Abstract
Objectives
The literature on the gendered differences of mental health as a result of grandchild care has shown mixed results. Research on grandchild care further suggests that nonresidential grandchild care improves mental health outcomes, while residential grandchild care arrangements decrease mental health outcomes in grandparents. The moderating or buffering role of social engagement remains understudied in the grandchild care–mental health relationship. This study examines mental health effect differences between caregiving grandmothers and grandfathers and the moderating effects of social engagement.
Methods
Using 2002–2012 data from the Health and Retirement Study, a nationally representative sample of U.S. adults aged 50 and older, I examine the mental health effects of grandchild care and the moderating effect of social engagement in fixed effects models.
Results
Grandfathers experience particularly worsened mental health outcomes when providing grandchild care in a skipped-generation household. Both grandmothers and grandfathers experience mental health improvements from increased social engagement. Social engagement, particularly for grandmothers, serves as a buffer or produces role enhancement for grandmothers in skipped-generation care arrangements.
Discussion
Nonresidential and residential grandchild care affects mental health outcomes differently for grandmothers and grandfathers. However, social engagement consistently serves as a buffer or mental health improvement for all grandparents. Findings further encourage the continued study of social engagement and gender differences in older adults more broadly.
Keywords: Gender, Grandparenting, Mental health, Social engagement
With demographic, social, and economic changes in the United States, grandparents have increasingly stepped into the role of childcare provider for their grandchildren. In response to wage stagnation, women joining the labor force, and increased longevity among older adults the prevalence of multigenerational households and noncustodial grandchild care have increased in recent decades (Cherlin, 2010; U.S. Census Bureau, 2004).
Substantial attention has been paid to the differential health outcomes of grandmothers and grandfathers, producing varied results. Independently, social engagement improves mental health for older adults, but has been understudied in terms of moderating the grandchild care–mental health relationship. This study examines grandchild care and mental health and how social engagement serves as a buffer effect for stressful care arrangements.
Background
Grandchild Care
Studies on the effects of grandchild care on health provide mixed results. Care-providing grandparents can experience increased physical stress (Musil & Ahmad, 2002), mental and emotional stress, and depressive symptoms (Baker & Silverstein, 2008; Szinovacz et al., 1999). This research is consistent with the role strain hypothesis, in which grandparents who serve as caregivers on top of other roles, such as spouse, coworker, or friend, experience negative mental and physical health outcomes (Goode, 1960; Rozario et al., 2004).
In contrast, role accumulation or role enhancement argues that fulfilling multiple roles provides psychological benefits (Di Gessa et al., 2016; Sieber, 1974). This is the case for grandparents who provide childcare in addition to occupying other roles and experience increased self-worth, increased interactions with their support systems (Rozario et al., 2004), and positive long-term physiological effects (Holmes & Joseph, 2011). While grandchild care may add a burden or stress to grandparents, increased contact with social networks has a buffer effect, contributing to role enhancement (Jang & Tang, 2016).
With regard to the gendered effects of grandchild care on mental health, results also vary. Care-providing grandmothers may experience more stress or depressive symptoms and reduced well-being compared to grandfathers (Blustein et al., 2004; Muller & Litwin, 2011; Szinovacz et al., 1999). More so, grandmothers experience fewer depressive symptoms or no change in life satisfaction after becoming first-time grandparents (Sheppard & Monden, 2019) or providing grandchild care (Hughes et al., 2007). Furthermore, Szinovacz and Davey (2006) found that retired grandfathers who provided child care experienced a sense of “spoiled retirement” and worse outcomes compared to grandmothers. Alternatively, Arpino and Bordone (2014) found no gender differences in cognitive function as a result of grandchild care.
Gender differences arise due to the type of childcare and the grandparents’ sense of satisfaction with the role (Winefield & Air, 2010). Grandmothers typically take on an “extension of their maternal” role, providing care, feeding, clothing, changing diapers, etc., for their grandchildren. Meanwhile, grandfathers are more likely to play with their grandchildren and be responsible for entertaining the children. Grandmothers taking on the care role experience more of the “burdens” of grandchild care and role strain, while grandfathers experience the joys of grandchild care or role enhancement (Blustein et al., 2004). Counter to much of the literature, Muller and Litwin (2011) and Waldrop and Weber (2001) provide evidence that grandparents experience both an increase in role satisfaction and an increase in stress and depressive symptoms.
Alternatively, grandmothers can experience more satisfaction from the grandparent role from their deeper, more emotional relationships with their grandchildren (Somary & Stricker, 1998; Thomas, 1989). They perform a continuation of their maternal role, while grandfathers have less experience interacting with children and expect to retire un-“spoiled” (Szinovacz & Davey, 2006). Grandmothers are often responsible for the formation and maintenance of social and kin networks and have more frequent contact with their grandchildren (Uhlenberg & Hammill, 1998) and spend more time with their grandchildren (Silverstein & Marenco, 2001), from which they derive increased satisfaction.
Another consideration in the effects of grandchild care is the childcare arrangement: the intensity of childcare and whether the arrangement is custodial or residential. More intensive grandchild care is often associated with worse health outcomes, while supplemental/occasional care is associated with positive emotional and physical health outcomes (Chen & Liu, 2012; Musil & Ahmad, 2002; Triadó et al., 2014).
Nonresidential childcare, which is often more leisurely and sporadic, reduces stress and improves mental and physical health for grandparents. Hughes et al. (2007) found that babysitting provided some health benefit for grandmothers. Residential childcare, in which grandparents coreside with their grandchildren in a multigenerational household (with children and grandchildren) or a skipped-generational household (with only grandchildren), increases stress and worsens mental health (Blustein et al., 2004). Furthermore, Chen and Liu (2012) argue that when grandchild care is less intensive, the benefits of the role’s emotional rewards and social support are highlighted and improve health; meanwhile, a heavier care responsibility worsens health.
Grandmothers are likely to provide grandchild care under these more stressful circumstances, in skipped-generation households (Luo et al., 2012; Minkler & Fuller-Thomson, 2001). Bowers and Myers (1999) found that full-time grandmothers with more responsibilities experienced less satisfaction in the grandparenting role and more stress than grandmothers who provided less intensive care.
Social Engagement and Grandchild Care
Social engagement, interaction, and support are important for older adults’ self-reported health, life satisfaction, and physical health outcomes (Ailshire & Crimmins, 2011; Ertel et al., 2008; Hayslip et al., 2015; Nelson et al., 2013), while loneliness or isolation worsens older adults’ quality of life and depressive symptoms (Domènech-Abella et al., 2017; Liu & Guo, 2007).
Different conceptualizations of social engagement have been examined, from social activities, formal and informal volunteering, contact with friends and family, and various forms of social and emotional support (Hayslip et al., 2015; Kohli et al., 2009). Specific to grandchild care and social activities, research has emphasized the relationship between these activities. Care-providing grandparents do not often substitute formal and informal social activities with grandchild care, but rather add on care responsibilities (Bulanda & Jendrek, 2016; Kohli et al., 2009). This is consistent with the cumulative hypothesis that suggests grandparents who provide childcare accumulate more activities. In contrast, some activities, such as religious activities, political activities, and others, may compete with grandchild care for the grandparents’ time in the competition hypothesis (Arpino & Bordone, 2017).
Social engagement has also been measured as social connectedness more generally, encompassing formal and informal, kin and non-kin interactions (Kohli et al., 2009). The Social Network Index (SNI) has been used in assessing social integration/isolation and health in mid- and later life and includes contact with children and parents, seeing friends or neighbors weekly, and volunteering (Ertel et al., 2008; Huisman & van Tilburg, 2021; Leigh-Hunt et al., 2017; Nelson et al., 2013; Yang et al., 2016). Many of these studies examine physical and mental health outcomes and do not examine engagement in conjunction with grandchild care. How social engagement moderates the grandchild care–mental health relationship remains understudied. Furthermore, research is limited on the relationships between grandchild care and social engagement or activities by gender. Thus, this study contributes to the literature by examining the gender differences in grandchild care and social engagement on mental health independently, as well as the moderating effect of social engagement on grandchild care.
The Present Study
Based on prior research, I ask the following questions:
1. Are there gender differences in the effects of social engagement and grandchild care on mental health?
I hypothesize that nonresidential grandchild care will positively affect mental health, and residential care arrangements, specifically the skipped-generation household arrangement, will worsen mental health outcomes. Furthermore, I expect these effects to be stronger for grandfathers. I also hypothesize that increases in social engagement will be associated with improved mental health outcomes across gender.
2. Does social engagement moderate the effect of grandchild care on mental health for grandmothers and grandfathers differently?
This question of the gender differences in the moderating effect of social engagement and grandchild care on mental health is more exploratory. I hypothesize that social engagement will serve as a buffer for stressful grandchild care arrangements (Gerard et al., 2006; Jang & Tang, 2016), and I further expect this effect to be greater for grandmothers.
Data and Empirical Strategy
Data and Sample
The data come from the Health and Retirement Study (HRS), a panel study surveying a representative sample of U.S. adults older than the age of 50 every 2 years. I use waves from 2002 to 2012. For this study, the sample has been limited to respondents who reported grandchildren, who had only nonmissing values for the variables of interest, and who have been observed in at least two waves. Descriptive statistics of the sample before limiting the sample are available in Supplementary Appendix Table 1.
Dependent Variable: Mental Health Index
The mental health index is derived from the Center for Epidemiologic Studies—Depression (CES-D) scale. The shorter, eight-item version used here is selected based on factor analysis and shows similar results to the original (Radlow, 1977; Radloff & Teri, 1986; Steffick, 2000). The CES-D is the sum of positive (depression, everything is an effort, sleep is restless, felt alone, felt sad, and could not get going) and negative (felt happy and enjoyed life) sentiments respondents have experienced in the previous 2 weeks, measured at every wave. The coding for this variable has been reversed from the original so that an increase is associated with improved health outcomes on a scale of 0–8.
Independent Variables
Childcare
Grandchild care is constructed from multiple HRS questions. In each wave, respondents are asked whether they have spent 100 h or more taking care of grandchildren in the previous 2 years. If yes, they estimated how many hours they had spent on grandchild care. Respondents also listed the people they lived with and identified their relationship to them. From these questions, I construct a comprehensive childcare variable: (0) less than 100 h of childcare and no residential grandchildren, (1) between 100 and 500 h of grandchild care and no residential grandchildren, (2) more than 500 h of grandchild care and no residential grandchildren, (3) grandparents live with at least one child and at least one grandchild (multigenerational household), and (4) grandparents who live with at least one grandchild but no children (skipped-generation household).
Social engagement
This version of the SNI is derived from multiple HRS questions. Respondents receive 1 point for each item: (1) being married or in a partnership, (2) having weekly contact with at least one parent or parent-in-law, (3) having weekly contact with friends, and (4) volunteering at least 1 h. Respondents without living parents were coded as 0. The resulting index is a scale from 0 to 4.
This index is a revised version of the SNI used in previous work, but omits seeing children weekly, as the directionality with its relationship with grandchild care is unclear. Thus, this variable is omitted from the index and is included as a covariate below. Other versions of this index use seeing neighbors instead of seeing friends. Due to data constraints, I use friends instead. Furthermore, while marriage likely mediates the grandchild care–mental health relationship for grandfathers (Hank & Buber, 2009), I include it in the index as an aspect of social support that improves mental health (Stokes & Moorman, 2018) and acts as a buffer against depressive symptoms (Helliwell et al., 2019). Similarly, I include seeing parents weekly in this operationalization of social engagement. Prior work has shown that providing care for both parents and children or grandchildren has negative effects for the middle generation and women in particular (DeRigne & Ferrante, 2012; Hammer & Neal, 2008). However, I include seeing parents, without instrumental care exchanged, as a measure of social engagement.
Covariates
The following time-variant covariates are included: age categories, income (logged), working status, whether respondents have any dependents, whether respondents see kids weekly, and a survey year indicator. Health measures are also included: self-reported health (0–4), limitations to activities of daily living (ADLs), limitations to instrumental activities of daily living (IADLs), and number of chronic health conditions (0–8).
Empirical Strategy: Fixed Effects
Prior longitudinal research on grandchild care often do not provide causal estimates; or within-individual causal estimates do not hold up, thus providing evidence that there is no causal relationship between grandchild care and health outcomes (Ailshire & Crimmins, 2011; Danielsbacka et al., 2019; Ku et al., 2013). There might be selection into grandchild care, for example, in which healthier grandparents are more likely to provide grandchild care. There may be endogeneity with unobserved heterogeneity, in which unobserved characteristics bias the grandchild care effect on mental health, or reverse causality in which improved mental health causes increased grandchild care.
A fixed effects (FE) approach addresses some of these issues and improves the casual estimate because it measures the within-unit variation. Some studies used an FE approach to examine the effects of grandchild care and health outcomes (Ates, 2017; Danielsbacka et al., 2019; Ku et al., 2013; Sheppard & Monden, 2019). Ates (2017) finds positive associations between grandchild care and self-rated health. However, using FE to address unobserved heterogeneity, the relationship dissipates.
Similarly, I control for observable, time-variant characteristics that would affect childcare and well-being and I employ FE models to further address unobserved heterogeneity. The FE model controls for time-invariant characteristics, reducing omitted variable bias. I estimate the effect of childcare provision with an ordinary least squares FE model using the following equation:
in which is the person-wave health outcome, and the relationship between childcare provision and mental health. is an individual’s amount of childcare measured in time t. refers to the interaction term (Social engagement × Childcare arrangement). is individual-level, time-varying control variables. is the individual FEs and is the wave-year FEs, and is the error term.
For the main effects, positive coefficients indicate mental health improvement, and negative coefficients indicate mental health decline. Both grandchild care and social engagement are demeaned and refer to an increase or a decrease, or a deviation, from the individuals’ average experience with that characteristic.
To examine moderation, I interact social engagement with grandchild care arrangements. I use a moderation approach to examine individuals occupying multiple roles at once, as used in previous work (Szinovacz & Davey, 2006), and to examine the different effects of engagement by childcare arrangement. Before the interaction, I demean childcare arrangements and social engagement, producing a less biased estimate of the interaction in an FE model (Giesselmann & Schmidt-Catran, 2020). Giesselmann and Schmidt-Catran (2020) further suggest a double demeaning approach in which each factor variable is demeaned, and their interaction is also demeaned. Here, I present the single demeaning approach that produces the same results but with smaller standard errors and larger sample sizes (the double demeaning approach is provided in Supplementary Appendix Table 5). For interpretation, positive coefficients still mean health improvement, and negative coefficients still indicate health decline.
Lastly, this FE model does not address reverse causality. Prior work addressed reverse causality by accounting for health status at first observation or lagging the variables (Ku et al., 2013) or by reversing the model to predict childcare from health status (Danielsbacka et al., 2019). They have found that these sensitivity analyses supported the use of FEs. The timing of my measures reduces the potential of reverse causality because the dependent measure (mental health) asks respondents about the previous 2 weeks, while the independent measures of childcare and social engagement ask respondents to reflect on the previous 2 years. Reverse causality cannot be ignored completely but is attenuated by the temporal order of the measures.
Results
Descriptive Results
Table 1 displays the descriptive statistics for all characteristics of person-years by care arrangement. Women represent about 60% of the sample across the board. There is a higher proportion of grandmothers providing childcare in multigenerational households (69%) and in skipped-generation households (66%) than grandfathers. Grandparents who provide nonresidential childcare have slightly higher mental health scores than those grandparents who do not. Grandparents in residential grandchild care arrangements show slightly lower mental health scores.
Table 1.
Descriptive Statistics of Sample by Care Arrangements, Person-Years
| No care | <500 h care, nonresidential care | >499 h care, nonresidential care | Any care, multigenerational HH | Any care, skipped-generation HH | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | Mean | SD | Mean | SD | Mean | SD | |
| Mental health (0–8) | 6.48 | 2.00 | 6.89 | 1.73 | 6.85 | 1.74 | 6.02 | 2.23 | 6.08 | 2.24 |
| Women (%) | 61.48 | 58.86 | 60.64 | 69.10 | 66.20 | |||||
| Social engagement (0–4) | 1.54 | 0.90 | 1.82 | 0.87 | 1.86 | 0.87 | 1.36 | 0.92 | 1.53 | 0.91 |
| Sees kids weekly (%) | 1.61 | 2.39 | 3.03 | 0.00 | 2.18 | |||||
| Working (%) | 24.20 | 31.08 | 31.74 | 38.06 | 27.79 | |||||
| Any dependents (%) | 9.34 | 3.89 | 6.87 | 35.61 | 42.33 | |||||
| Self-reported health (0–4) | 2.11 | 1.09 | 2.42 | 1.02 | 2.35 | 1.01 | 1.87 | 1.10 | 1.93 | 1.09 |
| ADLs (0–5) | 0.31 | 0.85 | 0.14 | 0.54 | 0.15 | 0.56 | 0.37 | 0.87 | 0.40 | 0.95 |
| IADLs (0–3) | 0.11 | 0.42 | 0.05 | 0.25 | 0.04 | 0.22 | 0.11 | 0.41 | 0.12 | 0.44 |
| Health conditions (0–8) | 2.09 | 1.44 | 1.83 | 1.33 | 1.84 | 1.34 | 2.15 | 1.55 | 2.23 | 1.52 |
| Household income ($) | 55,477.85 | 89,704.74 | 77,311.70 | 92,938.25 | 93,918.31 | 726,998.60 | 46,190.78 | 62,039.97 | 49,457.92 | 55,638.97 |
| Age at first wave (years) | 68.77 | 10.58 | 65.29 | 7.74 | 64.53 | 7.57 | 62.33 | 8.65 | 65.07 | 8.33 |
| N | 66,418 | 4,392 | 2,505 | 1,466 | 1,148 | |||||
Notes: HH = household; SD = standard deviation; ADLs = activities of daily living; IADLs = instrumental activities of daily living. Units of analysis are person-years. Means and standard deviations for the sample are shown by care arrangement (columns). Variables here are not transformed. See Supplementary Appendix Table 2 for descriptive statistics for individuals in the final sample rather than in person-years.
A similar pattern emerges with social engagement across care arrangements. Consistent with cumulative theory (Kohli et al., 2009) in which grandparents who participate in one activity accumulate more activities, grandparents who do not provide grandchild care have an average social engagement score of 1.54, which increases with nonresidential care amounts (1.82 and 1.86, respectively). However, consistent with resource or constraint theory (Arpino & Bordone, 2017), in which activities may be competing for grandparents’ energy, time, or resources: Grandparents in residential care arrangements have lower social engagement scores (1.36 in multigenerational households and 1.53 in skipped-generation households).
Grandparents who provide nonresidential care report better health, fewer ADLs and IADLs, and fewer chronic health conditions than grandparents who do not provide care. Meanwhile, grandparents in residential care arrangements report worse health, more ADLs and IADLs, and more chronic health conditions on average than grandparents who provide no care. Similarly, grandparents providing nonresidential care have higher household incomes, and those providing residential care report lower household incomes than those who provide no care, supporting prior work that has shown that multigenerational or skipped-generation households are also lower socioeconomic status households (Hayslip & Kaminski, 2005).
Table 2 displays within-individual changes for mental health, childcare, and social engagement, and individuals’ number of waves they are observed in the sample. Grandmothers in the sample experience on average 1.91 changes in mental health scores. In general, there are more within-individual changes for grandmothers than for grandfathers. Of note, on average, there is little change for grandmothers or grandfathers in terms of childcare arrangements. This small variability is usually of concern in the FE model, but is less so due to the single demeaning approach employed in the multivariate analyses (Giesselmann & Schmidt-Catran, 2020).
Table 2.
Descriptive Statistics of Within-Individual Changes
| All | Women | Men | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean | SD | Min | Max | N | Mean | SD | Min | Max | N | Mean | SD | Min | Max | N | |
| Mental health | 1.76 | 1.44 | 0 | 5 | 18,383 | 1.91 | 1.47 | 0 | 5 | 11,062 | 1.52 | 1.36 | 0 | 5 | 7,321 |
| Social engagement | 1.33 | 1.20 | 0 | 5 | 18,383 | 1.37 | 1.22 | 0 | 5 | 11,062 | 1.26 | 1.17 | 0 | 5 | 7,321 |
| Care arrangement | 0.54 | 0.98 | 0 | 5 | 18,383 | 0.56 | 1.00 | 0 | 5 | 11,062 | 0.52 | 0.96 | 0 | 5 | 7,321 |
| Waves present | 4.13 | 1.60 | 2 | 6 | 18,383 | 4.22 | 1.60 | 2 | 6 | 11,062 | 3.99 | 1.60 | 2 | 6 | 7,321 |
Notes: SD = standard deviation. Units of analysis are individuals. Means, standard deviations, minimums, maximums, and number of observations for within-individual changes for variables of interest are shown. Waves present refers to the number of waves a given individual appears in the sample.
FEs: Main Effects
Table 3 presents baseline models and models with the interactions for all grandparents, grandmothers, and grandfathers. I present the effects of childcare, social engagement, and the interaction between skipped-generation care arrangement and social engagement. The full models with controls are available in Supplementary Appendix Table 3. See Supplementary Appendix Table 4 for full models with all interactions between childcare and social engagement.
Table 3.
Multivariate Fixed Effects Models Predicting Mental Health Values for All Grandparents, Grandmothers, and Grandfathers
| All | Women | Men | ||||
|---|---|---|---|---|---|---|
| (1) | (2) | (3) | (4) | (5) | (6) | |
| <500 h nonresidential care, demeaned | 0.041+ (0.02) | 0.041+ (0.02) | 0.041 (0.03) | 0.041 (0.03) | 0.04 (0.03) | 0.041 (0.03) |
| >499 h nonresidential care, demeaned | 0.062* (0.03) | 0.062* (0.03) | 0.075+ (0.04) | 0.075+ (0.04) | 0.04 (0.04) | 0.039 (0.04) |
| Any care, multigenerational HH, demeaned | −0.029 (0.05) | −0.03 (0.05) | −0.036 (0.07) | −0.036 (0.07) | −0.008 (0.08) | −0.01 (0.08) |
| Any care, skipped-generation HH, demeaned | −0.146* (0.06) | −0.145* (0.06) | −0.106 (0.08) | −0.103 (0.08) | −0.221* (0.09) | −0.223* (0.09) |
| Social engagement, demeaned | 0.126*** (0.01) | 0.126*** (0.01) | 0.125*** (0.01) | 0.125*** (0.01) | 0.129*** (0.02) | 0.129*** (0.02) |
| Social engagement, demeaned × Any care, skipped-generation HH, demeaned | 0.315* (0.14) | 0.306+ (0.16) | 0.342 (0.24) | |||
| Constant | 5.416*** | 5.416*** | 5.064*** | 5.064*** | 5.972*** | 5.970*** |
| (0.12) | (0.12) | (0.15) | (0.15) | (0.17) | (0.17) | |
| Observations | 75,929 | 75,929 | 46,708 | 46,708 | 29,221 | 29,221 |
Notes: HH = household. Grandchild care arrangements and social engagement are demeaned. The interaction is the product of the demeaned skipped-generation care arrangement and demeaned social engagement. See Supplementary Appendix Table 3 for the complete models with all covariates. +0.10; *0.05; **0.01; ***0.001.
Grandparents who, on average, provide nonresidential care of less than 500 h experience an increase in mental health of about 0.04, significant at the 0.1 level. That is, for any individual grandparent, the estimated increase in mental health due to increasing their mean type of this care category by 1 is 0.04 on the mental health scale. Similarly, on average, providing more than 500 h of nonresidential care explains a 0.062 mental health increase for grandparents. While these effects are small in magnitude, they support the hypothesis that more nonresidential care is associated with better mental and physical health outcomes.
Findings further support prior work showing that residential grandchild care is negatively associated with mental health for grandparents, increasing symptoms of depression and stress. For all grandparents, a positive deviation in the skipped-generation household care provision is associated with a mental health score decrease of 0.146 (Model 1). A grandparent’s increase in a skipped-generation care arrangement that is more than their overall average negatively affects mental health.
Social engagement positively affects mental health outcomes for grandparents. Social engagement is also demeaned, so a positive deviation from an individual’s mean—an increase from their average level of social engagement—significantly improves mental health outcomes 0.126 units, significant at the 0.01 level. This supports prior research, which has shown that social engagement and reduced social isolation can provide a mental health benefit for older adults (Jang & Tang, 2016). Though these magnitudes are small, they show statistically significant relationships.
FEs: Main Effects by Gender
Next, I examine the effects of care arrangements and social engagement on mental health by gender. Here, there are slight differences in the effects of both nonresidential and residential care arrangements. First, the positive effect of increased nonresidential grandchild care in Model 1 is driven by women (Model 3). Providing over 500 h of nonresidential care significantly improves mental health for grandmothers (significant at the 0.1 level) but does not for grandfathers. Meanwhile, the negative effect of providing grandchild care in a skipped-generation care arrangement is primarily driven by grandfathers. For grandfathers, a positive deviation from their mean skipped-generation care provision experiences a 0.223 decline in mental health. Compared to the effects of other care arrangements for either grandmothers or grandfathers, this is a large, nonnegligible effect. This is consistent with the expectation that grandfathers, who are newer to childcare responsibilities, are more negatively affected by intensive grandchild care demands than grandmothers, who are more accustomed to childcare responsibilities and continue their maternal role (Winefield & Air, 2010).
The independent effects of social engagement on mental health do not differ between men and women. Controlling for other factors and grandchild care responsibilities, social engagement positively affects mental health for both grandmothers and grandfathers equally.
Moderation Effects: Grandchild Care and Social Engagement
To examine the moderation effect of social engagement on grandchild care, I include an interaction term of the demeaned skipped-generation care arrangement and social engagement. I present the models for all grandparents (Model 2) and by gender for women and men in Models 4 and 6, respectively.
For all grandparents, the positive, significant interaction term suggests role enhancement and is consistent with a cumulative theory of social engagement. Grandparents, who provide childcare in skipped-generation households and are engaged socially at once, experience a positive mental health effect of 0.347. While a positive deviation in the skipped-generation care arrangement is associated with negative mental health, social engagement independently improves mental health; and the two interacted further improve mental health outcomes, producing role enhancement. Care-providing grandparents who increase their social engagement with other family members, friends, and in volunteering activities show improvements to mental health. This is further indicative of a cumulative theory of social engagement, in which grandparents who provide grandchild care are also seeking out and attaining benefits from social connectedness in other forms.
There are only slight differences by gender when it comes to the joint experience of grandchild care and social engagement. Grandmothers experience a positive mental health boost as a result of increasing nonresidential grandchild care and increased social engagement (Model 4). Though the skipped-generation care arrangement is not significant for grandmothers, the interaction term between skipped-generation care and social engagement is significantly positive at 0.306, indicating role enhancement. Like all grandparents in Model 2, care-providing grandmothers who increase social engagement experience a positive mental health effect.
Grandfathers experience an independent mental health decline with increased skipped-generation care provision (−0.223) and an independent mental health improvement from increased social engagement (0.129). Occupying both roles produces a positive mental health effect of 0.342, though this interaction is not significant. The direction and magnitude suggest that social engagement counteracts the stress of grandchild care for grandfathers, but not significantly more so than for grandfathers in other care arrangements.
This also explains the difference in magnitude between the main effects and the moderation effects: While grandchild care independently produces small changes in mental health, social engagement independently produces an even greater effect. The interaction of larger magnitude further suggests that social engagement outside of the household is particularly beneficial to those grandparents who provide residential care in a skipped-generation household.
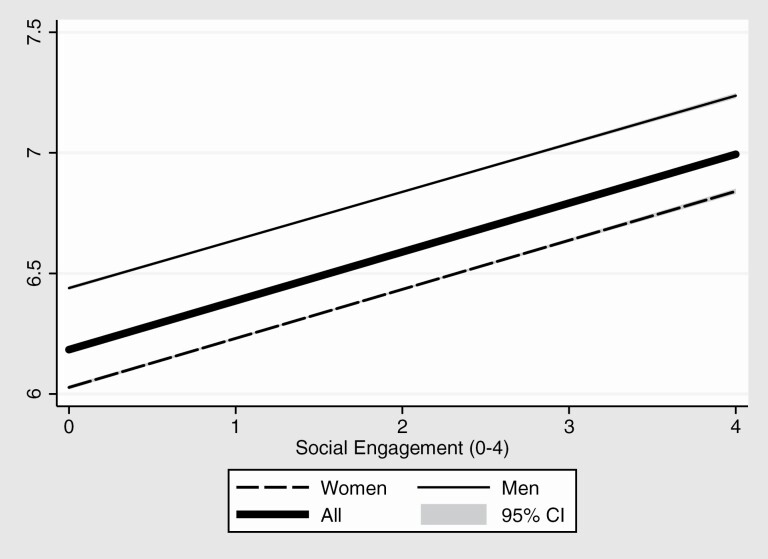
Figure 1 shows the predicted lines for mental health for women, men, and all grandparents, using the above equation with the interaction between skipped-generation grandchild care and social engagement. Though grandchild care may significantly decrease mental health, controlling for other factors, the moderation effect of social engagement improves mental health. There is little difference between grandmothers and grandfathers (save for significance) in the slopes of the lines, but grandfathers show higher mental health scores than grandmothers. The predicted value of mental health for one measure of social engagement for grandmothers is just less than 6.2, while for grandfathers it is closer to 6.5. Similarly, for grandmothers with four measures of social engagement, their predicted mental health is 6.9; for grandfathers, it is 7.3.
Figure 1.
Predicted mental health values for all grandparents. CI = confidence interval.
Discussion and Conclusion
I first asked how childcare and social engagement affect mental health for all grandparents. Consistent with prior work, nonresidential care significantly improves mental health, as does social engagement (Di Gessa et al., 2016; Hayslip et al., 2015). The skipped-generation care arrangement significantly worsens mental health for all grandparents. Furthermore, the interaction term between skipped-generation care provision and social engagement significantly improves mental health, indicating role enhancement in which social engagement serves as a buffer effect for those entering skipped-generation care arrangements. In this stressful arrangement, social connectedness is particularly important to care-providing grandparents.
I then asked how these effects vary by gender. While nonresidential childcare slightly improves mental health outcomes for grandmothers, the skipped-generation care arrangement decreases mental health outcomes for grandfathers. One interpretation is that grandchild care is akin to childcare, which is more commonly performed by women than men earlier in the life course and thus does not affect women as much later in the life course as they continue this role (Winefield & Air, 2010). If full-time childrearing is newer to grandfathers, they may experience role strain when confronted with grandchild care. Consistent with prior research, social engagement independently improves mental health for all grandparents (Domènech-Abella et al., 2017). Particularly for grandmothers, but also for all grandparents, social engagement serves as a buffer against the stress of residential care provision; and social connectedness is more beneficial for grandparents’ mental health in intensive care arrangements compared to grandparents in other care arrangements.
Taken together, I provide causal evidence that grandchild care and social engagement improve well-being outcomes, with only minimal differences by gender. I conclude that increased social engagement can serve as a buffer, particularly for grandparents who provide residential grandchild care.
This work is not without limitations and has implications for future research. First, social engagement has been proxied. Contact with kin and friends is often proxied by distance or coresidence, or by frequency of contact, as I do here. These proxies do not describe the nature of contact or interactions. Prior research has shown that different types of social activities should not be ignored when it comes to competition or accumulation with care responsibilities or by gender. For example, in additional analyses not presented here, and in prior work, volunteering and being married improve mental health for all grandparents providing care (Bulanda & Jendrek, 2016; Hank & Buber, 2009). Meanwhile, seeing friends regularly improves mental health for grandmothers but negatively affects mental health for grandfathers. This is unsurprising, given that women maintain relationships with kin and non-kin in later years more than men (Uhlenberg & Hammill, 1998); however, prior work provides little evidence as to why this may be the case only for men. Due to data constraints, various social activities were omitted from analyses. Instead, I present the results of a measure of social engagement or connectedness summing up measures of both kin and non-kin interactions and suggest future research to examine these relationships more in-depth.
Likewise, grandchild care is proxied by coresidence and number of hours of grandchild care within the previous 2 years, not portraying the activities performed during those hours, or the frequency or regularity of childcare, which may affect mental health differently. Future research should consider other conceptualizations of both social engagement and grandchild care, to provide more nuance as to which type of social engagement supports diverse grandchild care arrangements.
Furthermore, while I examine the possible gender differences in social support moderation of grandchild care, future research should also consider other intersections such as race and ethnicity or socioeconomic status. One limitation of this study is holding constant race and ethnicity through the FE approach, even though, like gender, there are racial and ethnic differences in grandchild care arrangements, social engagement, and the mental health effects thereof. For example, we know that most grandparent care providers are women, of lower income, and non-White, experiencing a disproportionate amount of caregiving and worsening mental health outcomes (Blustein et al., 2004). Future work should consider the increasing diversity in family and care arrangements and the disproportionate effects of care provision.
Third, this work has implications for health and well-being research on all older adults and the broader population. It supports that social connectedness independently improves mental health outcomes and significantly moderates the effects of stressful grandchild care arrangements. Research can be expanded to include a broader sample of older adults to address what these findings mean for nongrandparents and consider the role of social engagement in mental health for people of all ages in the face of other stressful events. In considering the increasingly aging U.S. population, future research should examine how to improve the social connectedness and well-being of older adults.
Supplementary Material
Acknowledgments
The author thanks Margot Jackson, Zhenchao Qian, and Emily Rauscher for their continued support throughout this project.
Funding
The author is grateful to the Population Studies and Training Center at Brown University, which receives funding from the National Institutes of Health (P2C HD041020), for general support.
Conflict of Interest
None declared.
References
- Ailshire, J. A., & Crimmins, E. M. (2011). Psychosocial factors associated with longevity in the United States: Age differences between the old and oldest-old in the Health and Retirement Study. Journal of Aging Research, 2011, 530534. doi: 10.4061/2011/530534 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arpino, B., & Bordone, V. (2014). Does grandparenting pay off? The effect of child care on grandparents’ cognitive functioning. Journal of Marriage and Family, 76(2), 337–351. doi: 10.1111/jomf.12096 [DOI] [Google Scholar]
- Arpino, B., & Bordone, V. (2017). Regular provision of grandchild care and participation in social activities. Review of Economics of the Household, 15(1), 135–174. doi: 10.1007/s11150-016-9322-4 [DOI] [Google Scholar]
- Ates, M. (2017). Does grandchild care influence grandparents’ self-rated health? Evidence from a fixed effects approach. Social Science & Medicine (1982), 190, 67–74. doi: 10.1016/j.socscimed.2017.08.021 [DOI] [PubMed] [Google Scholar]
- Baker, L. A., & Silverstein, M. (2008). Preventive health behaviors among grandmothers raising grandchildren. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 63(5), 304–311. doi: 10.1093/geronb/63.5.s304 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blustein, J., Chan, S., & Guanais, F. C. (2004). Elevated depressive symptoms among caregiving grandparents. Health Services Research, 39(6 Pt 1), 1671–1689. doi: 10.1111/j.1475-6773.2004.00312.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bowers, B. F., & Myers, B. J. (1999). Grandmothers providing care for grandchildren: Consequences of various levels of caregiving. Family Relations, 48(3), 303–311. doi: 10.2307/585641 [DOI] [Google Scholar]
- Bulanda, J. R., & Jendrek, M. P. (2016). Grandparenting roles and volunteer activity. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 71(1), 129–140. doi: 10.1093/geronb/gbu033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen, F., & Liu, G. (2012). The health implications of grandparents caring for grandchildren in China. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 67(1), 99–112. doi: 10.1093/geronb/gbr132 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cherlin, A. (2010). Demographic trends in the United States: A review of research in the 2000s. Journal of Marriage and the Family, 72(3), 403–419. doi: 10.1111/j.1741-3737.2010.00710.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Danielsbacka, M., Tanskanen, A. O., Coall, D. A., & Jokela, M. (2019). Grandparental childcare, health and well-being in Europe: A within-individual investigation of longitudinal data. Social Science & Medicine (1982), 230, 194–203. doi: 10.1016/j.socscimed.2019.03.031 [DOI] [PubMed] [Google Scholar]
- DeRigne, L., & Ferrante, S. (2012). The sandwich generation: A review of the literature. Florida Public Health Review, 9, 12. [Google Scholar]
- Di Gessa, G., Glaser, K., & Tinker, A. (2016). The health impact of intensive and nonintensive grandchild care in Europe: New evidence from SHARE. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 71(5), 867–879. doi: 10.1093/geronb/gbv055 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Domènech-Abella, J., Lara, E., Rubio-Valera, M., Olaya, B., Moneta, M. V., Rico-Uribe, L. A., Ayuso-Mateos, J. L., Mundó, J., & Haro, J. M. (2017). Loneliness and depression in the elderly: The role of social network. Social Psychiatry and Psychiatric Epidemiology, 52(4), 381–390. doi: 10.1007/s00127-017-1339-3 [DOI] [PubMed] [Google Scholar]
- Ertel, K. A., Glymour, M. M., & Berkman, L. F. (2008). Effects of social integration on preserving memory function in a nationally representative US elderly population. American Journal of Public Health, 98(7), 1215–1220. doi: 10.2105/AJPH.2007.113654 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gerard, J. M., Landry-Meyer, L., & Roe, J. G. (2006). Grandparents raising grandchildren: The role of social support in coping with caregiving challenges. International Journal of Aging & Human Development, 62(4), 359–383. doi: 10.2190/3796-DMB2-546Q-Y4AQ [DOI] [PubMed] [Google Scholar]
- Giesselmann, M., & Schmidt-Catran, A. W. (2020). Interactions in fixed effects regression models. Sociological Methods & Research. doi: 10.1177/0049124120914934 [DOI] [Google Scholar]
- Goode, W. J. (1960). A theory of role strain. American Sociological Review, 25(4), 483–496. doi: 10.2307/2092933 [DOI] [Google Scholar]
- Hammer, L. B., & Neal, M. B. (2008). Working sandwiched-generation caregivers: Prevalence, characteristics, and outcomes. The Psychologist-Manager Journal, 11(1), 93–112. doi: 10.1080/10887150801967324 [DOI] [Google Scholar]
- Hank, K., & Buber, I. (2009). Grandparents caring for their grandchildren: Findings from the 2004 Survey of Health, Ageing, and Retirement in Europe. Journal of Family Issues, 30(1), 53–73. doi: 10.1177/0192513X08322627 [DOI] [Google Scholar]
- Hayslip, B.Jr, Blumenthal, H., & Garner, A. (2015). Social support and grandparent caregiver health: One-year longitudinal findings for grandparents raising their grandchildren. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 70(5), 804–812. doi: 10.1093/geronb/gbu165 [DOI] [PubMed] [Google Scholar]
- Hayslip, B.Jr, & Kaminski, P. L. (2005). Grandparents raising their grandchildren: A review of the literature and suggestions for practice. The Gerontologist, 45(2), 262–269. doi: 10.1093/geront/45.2.262 [DOI] [PubMed] [Google Scholar]
- Health and Retirement Study. (n.d.). (Core public use files 2002–2012; RAND longitudinal files 2002–2012) Public use data set. Produced and distributed by the University of Michigan with funding from the National Institute on Aging (grant number NIA U01AG009740). Ann Arbor, MI (2020).
- Helliwell, J. F., Huang, H., Norton, M. B., & Wang, S. (2019). Happiness at different ages: The social context matters. In Rojas M. (Ed.), The economics of happiness: How the Easterlin paradox transformed our understanding of well-being and progress (pp. 455–481). Springer International Publishing. doi: 10.1007/978-3-030-15835-4_20 [DOI] [Google Scholar]
- Holmes, W. R., & Joseph, J. (2011). Social participation and healthy ageing: A neglected, significant protective factor for chronic non communicable conditions. Globalization and Health, 7, 43. doi: 10.1186/1744-8603-7-43 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hughes, M. E., Waite, L. J., LaPierre, T. A., & Luo, Y. (2007). All in the family: The impact of caring for grandchildren on grandparents’ health. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 62(2), 108–119. doi: 10.1093/geronb/62.2.s108 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huisman, M., & van Tilburg, T. G. (2021). Chapter 7—Social exclusion and social isolation in later life. In Ferraro K. F. & Carr D. (Eds.), Handbook of aging and the social sciences (9th ed., pp. 99–114). Academic Press. doi: 10.1016/B978-0-12-815970-5.00007-3 [DOI] [Google Scholar]
- Jang, H., & Tang, F. (2016). Effects of social support and volunteering on depression among grandparents raising grandchildren. International Journal of Aging & Human Development, 83(4), 491–507. doi: 10.1177/0091415016657561 [DOI] [PubMed] [Google Scholar]
- Kohli, M., Hank, K., & Künemund, H. (2009). The social connectedness of older Europeans: Patterns, dynamics and contexts. Journal of European Social Policy, 19(4), 327–340. doi: 10.1177/1350506809341514 [DOI] [Google Scholar]
- Ku, L. J., Stearns, S. C., Van Houtven, C. H., Lee, S. Y., Dilworth-Anderson, P., & Konrad, T. R. (2013). Impact of caring for grandchildren on the health of grandparents in Taiwan. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 68(6), 1009–1021. doi: 10.1093/geronb/gbt090 [DOI] [PubMed] [Google Scholar]
- Leigh-Hunt, N., Bagguley, D., Bash, K., Turner, V., Turnbull, S., Valtorta, N., & Caan, W. (2017). An overview of systematic reviews on the public health consequences of social isolation and loneliness. Public Health, 152, 157–171. doi: 10.1016/j.puhe.2017.07.035 [DOI] [PubMed] [Google Scholar]
- Liu, L. J., & Guo, Q. (2007). Loneliness and health-related quality of life for the empty nest elderly in the rural area of a mountainous county in China. Quality of Life Research, 16(8), 1275–1280. doi: 10.1007/s11136-007-9250-0 [DOI] [PubMed] [Google Scholar]
- Luo, Y., LaPierre, T. A., Hughes, M. E., & Waite, L. J. (2012). Grandparents providing care to grandchildren: A population-based study of continuity and change. Journal of Family Issues, 33(9), 1143–1167. doi: 10.1177/0192513X12438685 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Minkler, M., & Fuller-Thomson, D. E. (2001). Physical and mental health status of American grandparents providing extensive child care to their grandchildren. Journal of the American Medical Women’s Association (1972), 56(4), 199–205. [PubMed] [Google Scholar]
- Muller, Z., & Litwin, H. (2011). Grandparenting and psychological well-being: How important is grandparent role centrality? European Journal of Ageing, 8(2), 109–118. doi: 10.1007/s10433-011-0185-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Musil, C. M., & Ahmad, M. (2002). Health of grandmothers: A comparison by caregiver status. Journal of Aging and Health, 14(1), 96–121. doi: 10.1177/089826430201400106 [DOI] [PubMed] [Google Scholar]
- Nelson, L. A., Noonan, C. J., Goldberg, J., & Buchwald, D. S. (2013). Social engagement and physical and cognitive health among American Indian participants in the Health and Retirement Study. Journal of Cross-Cultural Gerontology, 28(4), 453–453. doi: 10.1007/s10823-013-9213-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Radloff, L. S. (1977). The CES-D scale: A self-report depression scale for research in the general population. Applied Psychological Measurement, 1(3), 385–401. doi: 10.1177/014662167700100306 [DOI] [Google Scholar]
- Radloff, L. S., & Teri, L. (1986). Use of the Center for Epidemiological Studies—Depression scale with older adults. Clinical Gerontologist, 5(1–2), 119–136. doi: 10.1300/J018v05n01_06 [DOI] [Google Scholar]
- Rozario, P. A., Morrow-Howell, N., & Hinterlong, J. E. (2004). Role enhancement or role strain: Assessing the impact of multiple productive roles on older caregiver well-being. Research on Aging, 26(4), 413–428. doi: 10.1177/0164027504264437 [DOI] [Google Scholar]
- Sheppard, P., & Monden, C. (2019). Becoming a first-time grandparent and subjective well-being: A fixed effects approach. Journal of Marriage and Family, 81(4), 1016–1026.doi: 10.1111/jomf.12584 [DOI] [Google Scholar]
- Sieber, S. D. (1974). Toward a theory of role accumulation. American Sociological Review, 39(4), 567. doi: 10.2307/2094422 [DOI] [Google Scholar]
- Silverstein, M., & Marenco, A. (2001). How Americans enact the grandparent role across the family life course. Journal of Family Issues, 22(4), 493–522. doi: 10.1177/019251301022004006 [DOI] [Google Scholar]
- Somary, K., & Stricker, G. (1998). Becoming a grandparent: A longitudinal study of expectations and early experiences as a function of sex and lineage. The Gerontologist, 38(1), 53–61. doi: 10.1093/geront/38.1.53 [DOI] [PubMed] [Google Scholar]
- Steffick, D. (2000). Documentation of affective functioning measures in the Health and Retirement Study. Institute for Social Research, University of Michigan. doi: 10.7826/ISR-UM.06.585031.001.05.0005.2000 [DOI] [Google Scholar]
- Stokes, J. E., & Moorman, S. M. (2018). Influence of the social network on married and unmarried older adults’ mental health. The Gerontologist, 58(6), 1109–1113. doi: 10.1093/geront/gnx151 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Szinovacz, M. E., & Davey, A. (2006). Effects of retirement and grandchild care on depressive symptoms. International Journal of Aging & Human Development, 62(1), 1–20. doi: 10.2190/8Q46-GJX4-M2VM-W60V [DOI] [PubMed] [Google Scholar]
- Szinovacz, M. E., DeViney, S., & Atkinson, M. P. (1999). Effects of surrogate parenting on grandparents’ well-being. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 54(6), 376–388. doi: 10.1093/geronb/54b.6.s376 [DOI] [PubMed] [Google Scholar]
- Thomas, J. L. (1989). Gender and perceptions of grandparenthood. International Journal of Aging & Human Development, 29(4), 269–282. doi: 10.2190/H9XB-9VL6-KFCQ-L60E [DOI] [PubMed] [Google Scholar]
- Triadó, C., Villar, F., Celdrán, M., & Solé, C. (2014). Grandparents who provide auxiliary care for their grandchildren: Satisfaction, difficulties, and impact on their health and well-being. Journal of Intergenerational Relationships, 12(2), 113–127. doi: 10.1080/15350770.2014.901102 [DOI] [Google Scholar]
- Uhlenberg, P., & Hammill, B. G. (1998). Frequency of grandparent contact with grandchild sets: Six factors that make a difference. The Gerontologist, 38(3), 276–285. doi: 10.1093/geront/38.3.276 [DOI] [PubMed] [Google Scholar]
- U.S. Census Bureau. (2004). Table CH-7. Grandchildren living in the home of their grandparents: 1970–Present. http://www.census.gov/population/socdemo/hh-fam/tabCH-7.pdf
- Waldrop, D. P., & Weber, J. A. (2001). From grandparent to caregiver: The stress and satisfaction of raising grandchildren. Families in Society: The Journal of Contemporary Social Services, 82(5), 461–472. doi: 10.1606/1044-3894.177 [DOI] [Google Scholar]
- Winefield, H., & Air, T. (2010). Grandparenting: Diversity in grandparent experiences and needs for healthcare and support. International Journal of Evidence-Based Healthcare, 8(4), 277–283. doi: 10.1111/j.1744-1609.2010.00187.x [DOI] [PubMed] [Google Scholar]
- Yang, Y. C., Boen, C., Gerken, K., Li, T., Schorpp, K., & Harris, K. M. (2016). Social relationships and physiological determinants of longevity across the human life span. Proceedings of the National Academy of Sciences of the United States of America, 113(3), 578–583. doi: 10.1073/pnas.1511085112 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.