Abstract
Background
Telemedicine use has increased significantly during the COVID-19 pandemic. It remains unclear if its rapid growth exacerbates disparities in healthcare access. We aimed to characterize telemedicine use among a large oncology population in the Deep South during the COVID-19 pandemic.
Materials and Methods
A retrospective cohort study was performed at the only National Cancer Institute designated-cancer center in Alabama March 2020 to December 2020. With a diverse (26.5% Black, 61% rural) population, this southeastern demographic uniquely reflects historically vulnerable populations. All non-procedural visits at the cancer center from March to December 2020 were included in this study excluding those with a department that had fewer than 100 visits during this time period. Patient and clinic level characteristics were analyzed using t-test and Chi-square to compare characteristics between visit types (in-person versus telemedicine, and video versus audio within telemedicine). Generalized estimating equations were used to identify independent factors associated with telemedicine use and type of telemedicine use.
Results
There were 50 519 visits and most were in-person (81.3%). Among telemedicine visits, most were phone based (58.3%). Black race and male sex predicted in-person visits. Telemedicine visits were less likely to have video among patients who were Black, older, male, publicly insured, and from lower income areas.
Conclusions
Telemedicine use, specifically with video, is significantly lower among historically vulnerable populations. Understanding barriers to telemedicine use and preferred modalities of communication among different populations will help inform insurance reimbursement and interventions at different socioecological levels to ensure the continued evolution of telemedicine is equitable.
Keywords: telemedicine, healthcare disparities, minority health, health services accessibility
The COVID-19 pandemic has caused an increase in the use of telemedicine. This article reports on the use of telemedicine at the only NCI-designated cancer center in Alabama, focusing on potential disparities in health care access.
Implications for Practice.
Alabama represents a uniquely diverse (26.5% Black, 61% rural) population with some of the highest cancer-related mortality, poverty rate, and uninsured rate. Healthcare disparities and the digital divide both disproportionately affect these populations. In this comprehensive study, we found that patients with cancer in Alabama suffer from disparities in telemedicine utilization. Vulnerable patients were less likely to use telemedicine and, when telemedicine was used, were generally using telephone visits. Helping patients navigate technologically complex interactions, such as video-based telemedicine, and reimbursing providers phone-based communication with some of our most vulnerable patients will help ensure the distributive justice of telemedicine.
Introduction
During the COVID-19 pandemic, telehealth use has exponentially increased to minimize in-person encounters, with the Department of Health and Human Services, among others, promoting video visits to reach patients at home.1 Patients with cancer are particularly vulnerable to COVID-19 infection,2 with greater rates of hospitalization and more severe outcomes. Cancer populations are older compared with other patient populations3 and benefit greatly from telemedicine visits, permitting remote and routine visitation with multidisciplinary healthcare providers.4 Many patients prefer telehealth to traditional in-person visits, largely due to its convenience.5 Telemedicine allows for patients’ healthcare needs to be met without time for travel, parking frustrations, lost productivity, or the additional involvement of a caretaker’s entire workday. Additionally, family members can conveniently be involved in care conversations, which are especially integral to cancer care 6. Telemedicine’s success for cancer care during the pandemic will likely lead to its expansion after the pandemic subsides 7. Therefore, it is critical to understand the patterns of telemedicine usage during the pandemic to ensure equity moving forward after COVID-19.
Barriers to using telemedicine use may exacerbate disparities due to the digital divide. Users of telemedicine have historically been young (average age 38 years) and from urban areas (83.3%) 8. However, half of all cancer cases are not diagnosed until after the age of 65.9 In that age group, about 13 million (38%) adults are unprepared for video visits due to disability, technologic restrictions, and inexperience.10 This telemedicine unreadiness is particularly prevalent among patients who are older; male; not married; Black or Hispanic; reside in non-metropolitan areas; and have less education, lower-income, and poorer self-reported health.10 Older patients often have multiple medical comorbidities and lower digital literacy.11 Patients from marginalized backgrounds have less access to broadband and digital infrastructures that would facilitate telemedicine use.12,13 Disparities in cancer outcomes have similarly been demonstrated across race and socioeconomic factors.14 Black patients and those with less wealth have later presentation, more aggressive tumors, and worse outcome.15
Alabama’s patients with cancer are particularly affected by the growing digital divide. Alabama has the sixth largest proportion of Black patients in the US,16 with 26.5% of the population identifying as Black. Many parts of the state are some of the poorest in the country and 95% of the land has rural status with 59% of the population living in urban settings 17. With most counties having an uninsured rate greater than the national average,18 this Southeastern population uniquely reflects historically vulnerable populations.
Starting in March 2020, our institution established an internal policy for all clinic visits to be virtual unless a procedure or in-person examination was needed. Visits would be video based with possible conversion to audio-only due to technology issues or patient-provider preference. Prior to March 2020, minimal use of telemedicine had been deployed across a minority of Divisions. This rapid development of telemedicine implementation was seen at institutions across the country, with a high risk of exacerbating disparities at the intersection of health and technology. Although telemedicine may help overcome many barriers and disparities, we hypothesized that those who experience the digital divide would similarly have less access to the age of telemedicine. Specifically, we hypothesize that patients who are older, Black, publicly insured, and from lower income areas will not be proportionally represented in the surge in telemedicine usage. We therefore conducted a retrospective review of telemedicine use in patients with cancer at the largest healthcare center in Alabama to determine whether there is an equitable distribution of patients benefiting from the rise in telemedicine use.
Materials and Methods
Telemedicine Implementation
Telemedicine implementation began before the COVID-19 pandemic but was not yet widely used. EW served led the telemedicine initiative across the institution and retrofitted the electronic medical record to be integrated with the telemedicine system. As demand for telemedicine increased with the pandemic, a HealthStream module was created to train regulatory and billing professionals, as well as nurses and providers. Completing regulatory training in HealthStream was required in order for schedulers to grant telehealth appointments to providers. Through a train-the-trainer framework, about 98% of billable providers received telemedicine training and were able to have scheduled telemedicine visits. Initially, the system was implemented using American Well and Doximity, which no longer required downloading of an app in May 2020. Patients were sent a link to join the appointment through either email or SMS.
Implementing a telemedicine infrastructure was predominantly costly for video-based visits, as phone visits utilized pre-existing technology and infrastructure. Video-based telemedicine required retrofitting existing clinics with camera capabilities, fortifying institutional broadband access, and paying for the video platform itself. Additionally, telemedicine visits were reimbursed less than in-person visits due to a lower facility fee ($0 for phone visits, $20-$25 for video visits, $80 for in-person visits). However, reduced costs for insurance companies and patients.
Visits during 2020 were reimbursed with parity due to the public health emergency which allowed for CMS to reimburse both phone and video visits for all specialties19. However, this has since changed to only permit mental health telemedicine services to be reimbursed with parity. Phone visits are now reimbursed based on time spent with the patient, while video visits have greater reimbursement due to the inclusion of components of the physical exam.
Initially, all visits were required to be by telemedicine to reduce in-person encounters unless there were clinical reasons the patient needed to be seen in person. Given the rapid expansion of telehealth, each provider was expected to have the ability to provide remote healthcare, but there were no departmental, division, or section requirements for certain visits to be remote. Telemedicine visits were a joint determination of provider preference, patient preference, and scheduling system requirements.
Study Design
A retrospective cohort study of all outpatient, non-procedural visits at the only National Cancer Institute-designated cancer center in Alabama were reviewed. Visits from March 17, 2020 to December 31, 2020 were characterized by patient and provider level characteristics derived from billing data. Patient characteristics included demographics (age, gender, and race), insurance provider, and home ZIP code. From patients’ ZIP code, distance to the hospital was calculated 20. Home ZIP was cross referenced with census data on median income21 and FCC data on broadband network access.22 Provider level characteristics included visit type (in-person vs telemedicine, and within telemedicine, video or audio) and Department (Medicine, Neurology, Obstetrics/Gynecology, Radiation Oncology, and Surgery). Visits with Divisions that had fewer than 100 visits were excluded (Dermatology, Otolaryngology).
General patient demographics of the cohort were determined based on each patient’s first visit, as some had multiple visits. Visits were analyzed to compare factors between visit type groups using Chi-square analysis and ANOVA. Multivariable generalized estimating equations (GEE) 23 with logit link were used to identify factors associated with telemedicine use as well as type of telemedicine use. GEE’s account for correlation in repeated patient observations and allow for estimation of population averaged effects. Our GEE implementation used an exchangeable correlations structure with clustering by patient and robust standard error. Data were analyzed using R (R Core Team, 2020)24 with P-values of <.05 considered significant.
Results
Population Description
A total of 50 519 visits for 19 692 unique patients occurred during the study period. Of these visits, 41 082 (81.3%) were in-person visits, and 9437 (18.7%) were telemedicine (Table 1). For the telemedicine visits, 5499 (58.3%) were phone visits, and 3938 (41.7%) were video visits. As shown in Table 1, most patients were white (68.1%) or Black (23.9%). Most patients identified as female (68.2%), and the median age was 61 years (mean: 58.6 years, min: 2 years, max: 102 years). Half of the patients had private insurance (49.4%) and over a third had Medicare (39.4%). The median annual household income based on ZIP code was $48 827 (mean: $52 834, SD: $21 314). The median distance from a patient’s home ZIP code to the cancer clinic was 40.3 mi (mean: 59.5 mi, SD: 89.9 mi). Most (54.7%) patients came from areas where 99%-100% of the population had access to Internet.
Table 1.
Patient characteristics.
| Factor | Patients (n = 19 692) | Visits | ||||||
|---|---|---|---|---|---|---|---|---|
| In-person (n = 41 082) | Telemedicine (n = 9437) | P-value | Phone (n = 5499) | Video (n = 3938) | P-value | |||
| Race | White | 13 404 (68.1%) | 28 143 (68.5%) | 6633 (70.3%) | <.001 | 3735 (67.9%) | 2898 (73.6%) | P < .001 |
| Black | 4697 (23.9%) | 9798 (23.8%) | 2143 (22.7%) | 1419 (25.8%) | 724 (18.4%) | |||
| Other | 879 (4.5%) | 1475 (3.6%) | 311 (3.3%) | 149 (2.7%) | 162 (4.1%) | |||
| Asian | 481 (2.4%) | 1154 (2.8%) | 282 (3.0%) | 157 (2.9%) | 125 (3.2%) | |||
| Hispanic | 231 (1.2%) | 512 (1.2%) | 68 (0.7%) | 39 (0.7%) | 29 (0.7%) | |||
| Sex | F | 13 422 (68.2%) | 27 715 (67.5%) | 6015 (63.7%) | .001 | 3529 (64.2%) | 2486 (63.1%) | .297 |
| M | 6270 (31.8%) | 13 967 (34.0%) | 3422 (36.3%) | 1970 (35.8%) | 1452 (36.9%) | |||
| Age, years | Mean (SD) | 58.6 (15.6) | 59.4 (14.7) | 60.0 (15.1) | .001 | 62.0 (14.3) | 57.3 (15.7) | .001 |
| Median (min, max) | 61 (2, 102) | 62 (2, 102) | 62 (3, 101) | 64 (11, 97) | 59 (3, 101) | |||
| <18 | 85 (0.4%) | 92 (0.2%) | 37 (0.4%) | .001 | 8 (0.1%) | 29 (0.7%) | .001 | |
| 18-29 | 929 (4.7%) | 1520 (3.7%) | 325 (3.4%) | 126 (2.3%) | 199 (5.1%) | |||
| 30-39 | 1618 (8.2%) | 3055 (7.4%) | 668 (7.1%) | 320 (5.8%) | 348 (8.8%) | |||
| 40-49 | 2554 (13.0%) | 5127 (12.5%) | 1142 (12.1%) | 581 (10.6%) | 561 (14.2%) | |||
| 50-59 | 3872 (19.7%) | 8409 (20.5%) | 1889 (20.0%) | 1023 (18.6%) | 866 (22.0%) | |||
| 60-69 | 5434 (27.6%) | 12077 (29.4%) | 2635 (27.9%) | 1629 (29.6%) | 1006 (25.5%) | |||
| 70-79 | 3973 (20.2%) | 8433 (20.5%) | 2080 (22.0%) | 1351 (24.6%) | 729 (18.5%) | |||
| 80+ | 1227 (6.2%) | 2369 (5.8%) | 661 (7.0%) | 461 (8.4%) | 200 (5.1%) | |||
| Distance to the hospital | Mean (SD) | 59.5 (89.9) | 54.2 (89.4) | 57.3 (86.2) | .002 | 52.3 (65.6) | 64.4 (108.2) | .001 |
| Median (min, max) | 40.3 (0, 4357) | 35.9 (0, 4357) | 28.8, (0, 2101) | 28.8 (0, 1152) | 30.2 (0, 2101) | |||
| 0-10 mi | 4646 (23.6%) | 9774 (23.8%) | 2325 (24.6%) | .001 | 1356 (24.7%) | 969 (17.6%) | .001 | |
| 10-25 mi | 3715 (18.9%) | 8384 (20.4%) | 2088 (22.1%) | 1258 (22.9%) | 830 (15.1%) | |||
| 25-50 mi | 2613 (13.3%) | 6034 (14.7%) | 1205 (12.8%) | 706 (12.8%) | 499 (9.1%) | |||
| 50-100 mi | 5022 (25.5%) | 10 252 (25.0%) | 2177 (23.1%) | 1321 (24.0%) | 856 (15.6%) | |||
| 100+ mi | 3433 (17.4%) | 6038 (14.7%) | 1544 (16.4%) | 803 (14.6%) | 741 (13.5%) | |||
| State | ||||||||
| AL | 18 342 (93.1%) | 38 818 (94.5%) | 8741 (92.6%) | .001 | 5179 (94.2%) | 3562 (90.5%) | .001 | |
| MS | 522 (2.7%) | 981 (2.4%) | 268 (2.8%) | 148 (2.7%) | 120 (3.0%) | |||
| FL | 449 (2.3%) | 699 (1.7%) | 237 (2.5%) | 98 (1.8%) | 139 (3.5%) | |||
| GA | 193 (1.0%) | 306 (0.7%) | 93 (1.0%) | 41 (0.7%) | 42 (1.1%) | |||
| TN | 81 (0.4%) | 139 (0.3%) | 36 (0.4%) | 14 (0.3%) | 22 (0.6%) | |||
| Other | 105 (0.5%) | 139 (0.3%) | 72 (0.8%) | 19 (0.3%) | 53 (1.3%) | |||
| Insurance | Private | 9724 (49.4%) | 19 370 (47.1%) | 4488 (47.6%) | .001 | 2390 (43.5%) | 2098 (53.3%) | .001 |
| Medicare | 7750 (39.4%) | 16 513 (40.2%) | 3987 (42.2%) | 2544 (46.3%) | 1443 (36.6%) | |||
| Medicaid | 1058 (5.4%) | 2524 (6.1%) | 499 (5.3%) | 311 (5.7%) | 188 (4.8%) | |||
| Other | 1159 (5.9%) | 2673 (6.5%) | 463 (4.9%) | 254 (4.6%) | 209 (5.3%) | |||
| Median income by ZIP | Mean (SD) | $52 834 ($21 314) | $52 506 ($21 148) | $53 929 ($21 700) | .001 | $52 274 ($21 332) | $56 338 ($22 006) | .001 |
| Median (min, max) | $48 827 ($11 741, $121 738) | $48 770 ($11 741, $121 738) | $49 570 ($12 863, $121 738) | $47 653 ($12 863, $121 738) | $52 175 ($12 863, $121, 38) | |||
| First quartile | 3557 (19.7%) | 7653 (19.9%) | 1603 (18.5%) | 1084 (21.2%) | 519 (14.7%) | |||
| Second quartile | 3609 (20.0%) | 7913 (20.6%) | 1654 (19.1%) | 1033 (20.2%) | 621 (17.6%) | |||
| Third quartile | 3644 (20.2%) | 7693 (20.0%) | 1711 (19.8%) | 1006 (19.6%) | 705 (20.0%) | |||
| Fourth quartile | 3619 (20.0%) | 7569 (19.7%) | 1776 (20.5%) | 983 (19.2%) | 793 (22.5%) | |||
| Fifth quartile | 3650 (20.2%) | 7545 (19.7%) | 1902 (22.0%) | 1019 (19.9%) | 883 (25.1%) | |||
| Percentage of population with Internet access | 0-50 | (0.0%) | 2743 (6.7%) | 584 (6.2%) | .001 | 360 (6.5%) | 224 (5.7%) | .169 |
| 50-75 | 1183 (6.0%) | 7050 (5.9%) | 565 (6.0%) | 316 (5.7%) | 249 (6.3%) | |||
| 75-90 | 3340 (17.0%) | 5520 (17.2%) | 1585 (16.8%) | 943 (17.1%) | 642 (16.3%) | |||
| 90-95 | 2848 (14.5%) | 22 895 (13.4%) | 1145 (12.1%) | 647 (11.8%) | 498 (12.6%) | |||
| 99-100 | 10 771 (54.7%) | 22 895 (55.7%) | 5450 (57.8%) | 3177 (57.8%) | 2273 (57.7%) | |||
| Department | Medicine | 21 109 (51.4%) | 5699 (60.4%) | .001 | 3674 (66.8%) | 2025 (51.4%) | .001 | |
| Neurology | 1414 (3.4%) | 374 (4.0%) | 228 (4.1%) | 146 (3.7%) | ||||
| Ob/Gyn | 6499 (15.8%) | 642 (6.8%) | 536 (9.7%) | 106 (2.7%) | ||||
| Radiation oncology | 3752 (9.1%) | 1591 (16.9%) | 462 (8.4%) | 1129 (28.7%) | ||||
| Surgery | 8308 (20.2%) | 1131 (12.0%) | 599 (10.9%) | 532 (13.5%) | ||||
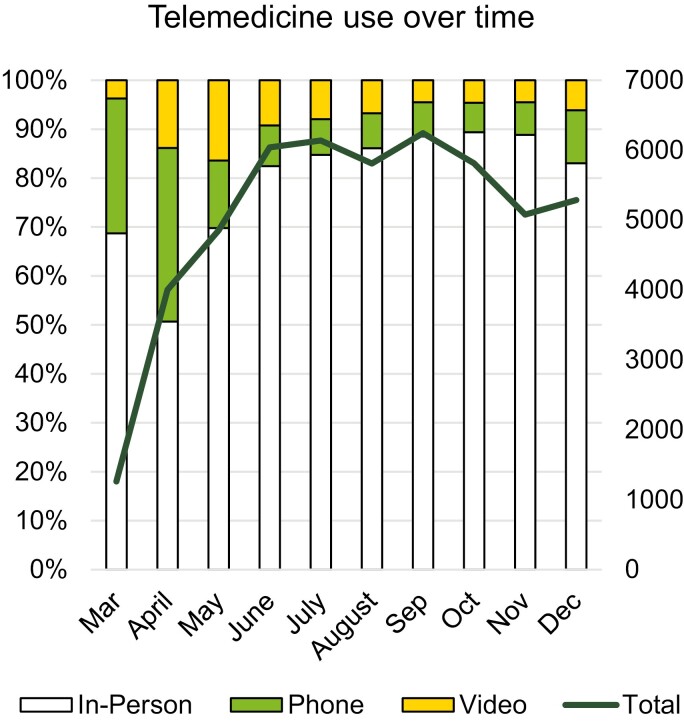
On average, there were 5052 visits each month (SD 1501) with the fewest visits in March 2020 (n = 1262) when the COVID-19 pandemic began and national shutdowns were occurring to decrease patient exposure in healthcare settings. As the infrastructure to conduct telemedicine visits was developed, clinic volume increased to 4000 per month and remained at 5000-6000 per month from June onward. Telemedicine adoption peaked in April 2020, consisting of 49% of clinic volume that month. Telemedicine use then stabilized, consisting of about 15% of visits each month (Fig. 1). Interestingly, while phone use peaked in April consisting of 72% of telemedicine volume, video use peaked in May, consisting of 54.4% of telemedicine volume that month. After initial adoption, phone and video use has stabilized as well with each modality consisting of about 50% of each month’s telemedicine visits.
Figure 1.
Stabilization of telemedicine uptake over time.
Half of the patients were seen once throughout the study period (47.0%), 20.8% were seen twice, and 9.1% were seen 3 times. Of the patients who had one type of visit throughout the studied time period (n = 15 448), most were in-person (n = 13 444), ranging from 1 (n = 8004, 59.5%) to 21 (n = n = 1, 0.0%) visits. Of the patients who only had phone visits throughout the studied time period (n = 1,095), most had 1 (n = 936, 85.5%) visit, with a maximum of 6 visits (n = 2, 0.0%). Of the patients who only had video visits throughout the studied time period (n = 909), most had 1 (n = 744, 81.8%) visit, with a maximum of 7 visits (n = 2, 0.0%).
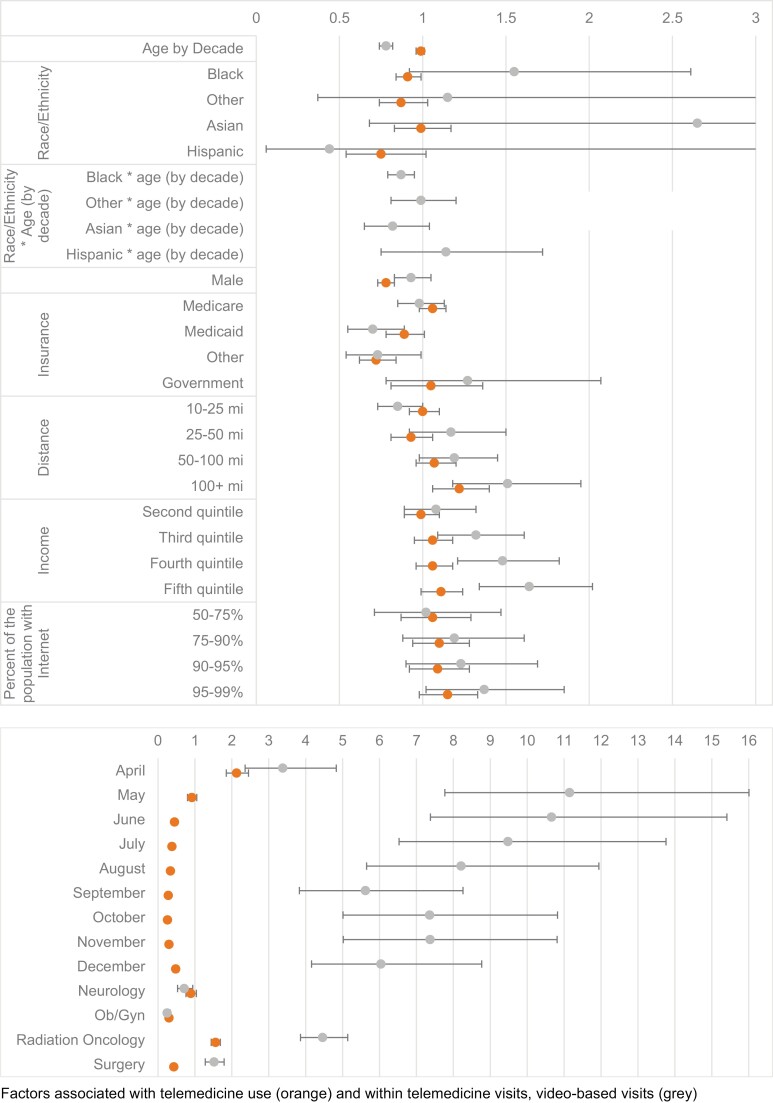
Primary Outcome: Telemedicine Visit
When comparing clinic visit modalities, most differences between those seen in-person and those seen via telemedicine on unadjusted analysis were statistically significant due to large sample sizes, but not clinically relevant as the differences were minimal (Table 1). On adjusted comparison, living 100+ mi from the hospital (OR 1.22, 95% CI 1.06-1.40) and having an appointment with Radiation Oncology (OR 1.56 95% CI 1.44-1.69) were associated with telemedicine use (Table 2; Fig. 2). While not statistically significant at the 95% confidence level, the highest levels of income and local Internet availability trended toward increased likelihood of telemedicine use. Black race (OR 0.91, 95% CI 0.84-0.99), male gender (OR 0.78, 95% CI 0.73-0.83), and visits with the Department of Obstetrics/Gynecology (OR 0.30, 95% CI 0.27-0.34) or Surgery (OR 0.43, 95% CI 0.40-0.47) were independently associated with in-person visits.
Table 2.
Logistic regression using generalized estimating equations.
| Telehealth visit versus in-person | Video versus phone visit | ||||||
|---|---|---|---|---|---|---|---|
| Odds ratios | CI | P | Odds ratios | CI | P | ||
| (Intercept) | 0.6 | 0.46–0.78 | <.001 | 0.29 | 0.17–0.50 | <.001 | |
| Race/ethnicity (ref: white) | Black | 0.91 | 0.84–0.99 | .03 | 0.69 | 0.60–0.81 | <.001 |
| Other | 0.87 | 0.74–1.03 | .105 | 1.06 | 0.78–1.45 | .705 | |
| Asian | 0.99 | 0.83–1.17 | .883 | 0.89 | 0.65–1.20 | .441 | |
| Hispanic | 0.75 | 0.54–1.02 | .069 | 0.76 | 0.41–1.43 | .4 | |
| Age | By decade | 0.99 | 0.96–1.01 | .269 | 0.74 | 0.71–0.78 | <.001 |
| Gender (ref: female) |
Male | 0.78 | 0.73–0.83 | <.001 | 0.93 | 0.83–1.05 | .223 |
| Insurance (ref: private) |
Medicare | 1.06 | 0.98–1.14 | .138 | 1.01 | 0.88–1.16 | .85 |
| Medicaid | 0.89 | 0.78–1.01 | .074 | 0.74 | 0.58–0.94 | .013 | |
| Other | 0.72 | 0.62–0.84 | <.001 | 0.74 | 0.55–1.00 | .049 | |
| Government | 1.05 | 0.81–1.36 | .735 | 1.24 | 0.76–2.03 | .379 | |
| Distance (ref: 0-10 mi) |
10-25 mi | 1 | 0.92–1.10 | .964 | 0.85 | 0.73–1.00 | .05 |
| 25-50 mi | 0.93 | 0.81–1.06 | .287 | 1.19 | 0.93–1.52 | .163 | |
| 50-100 mi | 1.07 | 0.96–1.20 | .196 | 1.21 | 0.99–1.47 | .061 | |
| 100+ mi | 1.22 | 1.06–1.40 | .006 | 1.54 | 1.19–1.98 | .001 | |
| Department (ref: Medicine) |
Neurology | 0.89 | 0.76–1.04 | .142 | 0.71 | 0.53–0.94 | .017 |
| Ob/Gyn | 0.3 | 0.27–0.34 | <.001 | 0.25 | 0.19–0.33 | <.001 | |
| Radiation Oncology | 1.56 | 1.44–1.69 | <.001 | 4.46 | 3.86–5.14 | <.001 | |
| Surgery | 0.43 | 0.40–0.47 | <.001 | 1.52 | 1.28–1.79 | <.001 | |
| Income (ref: first quintile) |
Second quintile | 0.99 | 0.89–1.10 | .848 | 1.11 | 0.91–1.35 | .294 |
| Third quintile | 1.06 | 0.95–1.18 | .302 | 1.36 | 1.12–1.65 | .002 | |
| Fourth quintile | 1.06 | 0.96–1.18 | .256 | 1.53 | 1.25–1.87 | <.001 | |
| Fifth quintile | 1.11 | 0.99–1.24 | .084 | 1.72 | 1.40–2.11 | <.001 | |
| Percent of the population with Internet (ref: 0%-50%) |
50%-75% | 1.06 | 0.87–1.29 | .549 | 1.02 | 0.71–1.46 | .924 |
| 75%-90% | 1.1 | 0.94–1.28 | .253 | 1.19 | 0.88–1.61 | .258 | |
| 90%-95% | 1.09 | 0.92–1.28 | .323 | 1.23 | 0.90–1.68 | .203 | |
| 95%-99% | 1.15 | 0.98–1.33 | .08 | 1.37 | 1.02–1.85 | .039 | |
| Appointment month (ref: March) |
April | 2.13 | 1.85–2.45 | <.001 | 3.38 | 2.36–4.83 | <.001 |
| May | 0.92 | 0.80–1.05 | .219 | 11.15 | 7.77–16.01 | <.001 | |
| June | 0.45 | 0.39–0.51 | <.001 | 10.66 | 7.38–15.41 | <.001 | |
| July | 0.38 | 0.33–0.44 | <.001 | 9.48 | 6.53–13.76 | <.001 | |
| August | 0.34 | 0.29–0.39 | <.001 | 8.21 | 5.65–11.94 | <.001 | |
| September | 0.28 | 0.24–0.32 | <.001 | 5.62 | 3.83–8.26 | <.001 | |
| October | 0.26 | 0.22–0.30 | <.001 | 7.36 | 5.01–10.82 | <.001 | |
| November | 0.3 | 0.26–0.35 | <.001 | 7.37 | 5.02–10.81 | <.001 | |
| December | 0.48 | 0.41–0.55 | <.001 | 6.04 | 4.16–8.77 | <.001 | |
Figure 2.
Forest plot of factors predicting telemedicine use. Factors associated with telemedicine use (orange) and within telemedicine visits, video-based visits (grey).
Secondary Outcome: Video Telemedicine Visit
Patients using video visits were more likely to be White (73.6%) and less likely to be Black (18.4%) compared with those using phone visits (67.9% White, 25.8% Black; P < .001) on unadjusted analysis. Those who had video visits were more likely to live further from the hospital compared with those who had phone visits (mean distance 64.4 mi vs 52.3 mi, P < .001), with patients living greater than 100 mi from the hospital comprising 18.3% of those using video when compared with 14.7% of those who had phone visits (P < .001). There was no significant difference in use by gender. Patients who had phone visits were older compared with those who had video visits (mean age 62.0 vs 57.3 years, P < .001). Phone use varied significantly with age group (P < .001), with greater phone use among older users starting at the age of 60 (60-69 years: 61.7% of telemedicine visits by phone, 70-79 years: 65.0%, and 80+ years: 69.7%). Video adoption was greatest within the Departments of Radiation Oncology (71.0% of telemedicine visits) and Surgery (47%) and lowest in the Departments of Obstetrics/Gynecology (16.5%), Medicine (35.5%), and Neurology (39.0%; P < .001).
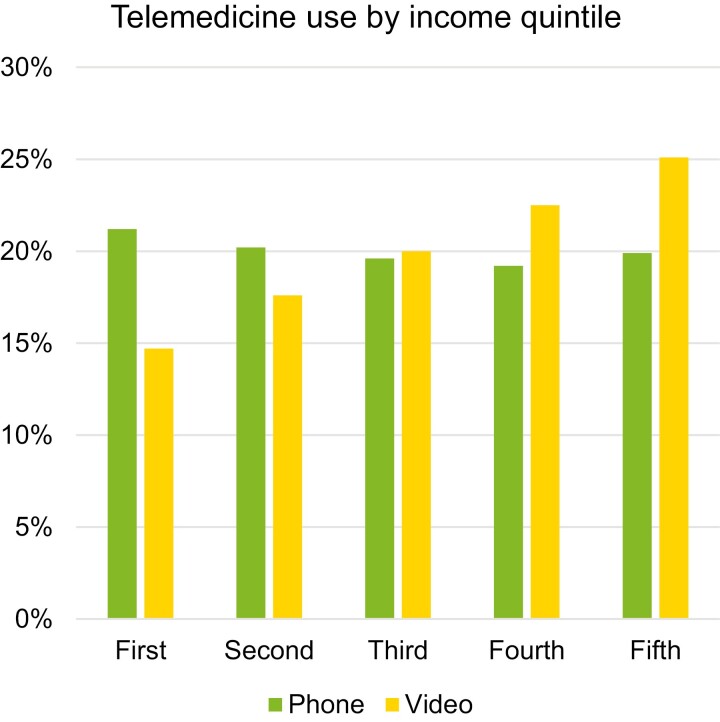
Those using video visits were more likely to be privately insured than those with phone visits (53.3% vs 43.5%, P < .001). Correspondingly, patients with video visits were less likely to have Medicare (36.6% vs 46.3%) or Medicaid (4.8% vs 5.7%;P < .001). Patients utilizing video visits were from ZIP codes with higher median incomes compared with those utilizing phone visits ($56 338 vs $52 274, P < .001; Fig. 3). Patients using phone visits are more likely to be in-state compared with those using video visits (94.2% vs 90.5%, P < .001) and live closer to the hospital (52.3 mi vs 64.4 mi, P < .001). There was no significant difference in local Internet availability.
Figure 3.
Increased video-based telemedicine use with increased median income of home ZIP.
On adjusted analysis, patients with Black race (OR 0.69, 95%CI 0.60-0.81) and Medicaid insurance (OR 0.74, 95% CI 0.58-0.94) were less likely to have their telemedicine visit with video (Table 2; Fig. 2). Each decade increase of patient age decreased the odds of having video visits by 26% (OR 0.74, 95% CI 0.71-0.78). Those living closer to the hospital were more likely to use a phone visit (10-25 mi OR 0.85, 95% CI 0.73-1.00) while those living further from the hospital were more likely to have a video visit (100+ mi OR 1.54, 95% CI 1.19-1.98). Video visits were used most frequently by Radiation Oncology (OR 4.46, 95% CI 3.86-5.14) and Surgery (OR 1.52, 95% CI 1.28-1.79), while visits with Neurology (OR 0.71, 95% CI 0.53-0.94) and Ob/Gyn (OR 0.25, 95% CI 0.19-0.33) were more likely to be by phone. Increasing income quintile was predictive of video-based telemedicine (compared with the lowest quintile, odds of video use by increasing quintile: 1.11, 1.36, 1.53, 1.72). Living in a ZIP code where 95%-99% of the population had Internet access was also predictive of video use (OR 1.37, 95% CI 1.02-1.85).
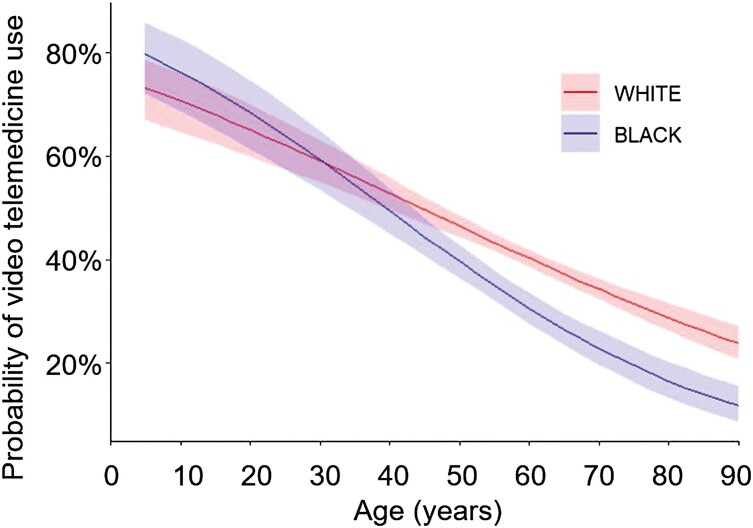
The interaction between age, race, insurance, and income reveals a complicated relationship between socioeconomic factors resulting in phone usage in the observed digital divide. In logistic regression with GEE, age was predictive of a phone visit (OR 0.81, 95% CI 0.79-0.84), which remained consistent when adjusting for race (OR 0.80, 95% CI 0.78-0.83; Table 3). Black race independently lowered odds of video use when adjusting for age (OR 0.61, 95% 0.54-0.68). When including an interaction between race and age, Black race by age independently predicted phone use (OR 0.89, 95%CI 0.82-0.96; Fig. 4).
Table 3.
Logistic regression using generalized estimating equations of age and race.
| Video versus phone visit | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Predictors | OR | CI | P | OR | CI | P | OR | CI | P | |
| Age | By decade | 0.81 | 0.79–0.84 | <.001 | 0.8 | 0.78––0.83 | <.001 | 0.83 | 0.80––0.86 | <.001 |
| Race (ref: white) | Black | 0.61 | 0.54––0.68 | <.001 | 1.18 | 0.76––1.85 | .458 | |||
| Asian | 0.94 | 0.72––1.22 | .641 | 2.66 | 0.81––8.67 | .106 | ||||
| Hispanic | 0.74 | 0.42––1.29 | .287 | 0.38 | 0.06––2.24 | .282 | ||||
| Other/PI/NA/mixed/Unknown | 1.35 | 1.05––1.73 | .021 | 0.96 | 0.37––2.54 | .941 | ||||
| Age and race (ref: white) | Black | 0.89 | 0.82––0.96 | .003 | ||||||
| Asian | 0.83 | 0.67––1.02 | .078 | |||||||
| Hispanic | 1.16 | 0.82––1.63 | .412 | |||||||
| Other/PI/NA/mixed/Unknown | 1.06 | 0.90––1.24 | .48 | |||||||
Figure 4.
Logistic regression of disparities in video-based telemedicine use among older patients exacerbated by race.
Discussion
In this study, we found that variations in telemedicine use exist by race, age, insurance type, and socioeconomic background. While older patients came from higher income backgrounds and were increasingly white, both predictors of video-based telemedicine use, increased age overcame those socioeconomic forces, resulting in decreased video-based telemedicine use. Patients that are more likely to have greater burden of disease and increased risk of severe illness with COVID-19 exposure are also not accessing telemedicine equitably.
This is the first analysis of patient with cancer utilization of telemedicine since the COVID-19 pandemic struck the United States. This is also a large study of over 19 000 patients and 50 000 patient visits with study demographics (white 68.0%, Black 24.3%) closely mirroring that of the state of Alabama (White 69.1%, Black 26.8%). Although 1 in 5 visits were through telemedicine, disparities by race, age, sex, and insurance provider exist in its utilization.
While many patients benefit from the convenience of telemedicine, the digital divide prevents some of the most vulnerable patient populations from equitable access. The disparate use in video telemedicine use as patients age is a crucial disparity to recognize and address. The visual component of video consultations offers distinct advantages over telephone consultations, specifically in providing visual cues and reassurance, building rapport, and improving communication.[21,25] Telemedicine provides time-saving alternatives to in-person appointments when formal physical examinations are not required, especially for those who are employed, but it is the visual component that allows for improve communication and rapport.
However, it is important for phone-based communication to be available to those who are not able to access video-based telemedicine, as for many this is the only source of remote healthcare access. Among Medicare beneficiaries, a majority of telehealth users report accessing care by phone only. These patients are mostly aged 75 and older, Hispanic, living in rural areas, and enrolled in both Medicare and Medicaid, closely mirroring the findings of this study.[22] It is important for insurance reimbursement to reflect the needs and access limitations of patients who are already at risk of greater disease burden and inequity in healthcare access while interventions are developed to allow for video-based telemedicine to become more accessible.
Disparities in telemedicine use have been observed in other access modalities. A study in New York including urgent care visits found that telemedicine use was similarly predominantly among white women. They also found that Black patients had the lowest odds of being seen via telemedicine in comparison to White patients.26 A study in Detroit for the Head and Neck Cancer Population had a largely male population, likely due to the male preponderance of that disease, and demonstrated telemedicine was more common among White patients, and phone visits more common among Black patients. Patients with Medicare and Medicaid were more likely to use phone than video visits, while those with private insurance were more likely to use video. Lower household income was associated with phone visits and higher household income was associated with video visits.27 These findings are all reflected in our Southeastern tertiary care population as well.
These differences in utilization can be attributed to multiple socioecological determinants of health, and each level must be addressed to ensure equitable access and use of telemedicine resources. At the patient-provider level, technological readiness, patient-provider trust, and patient empowerment are integral, modifiable components to a therapeutic interaction 28. At the social network level, interventions to assist caregivers of patients with cancer in telemedicine navigation, such as counseling, navigation, and education, have been shown to improve psychosocial outcomes of caregivers 29,30. Toolkits for institutional digital literacy31 can address and facilitate telemedicine use on an organizational level.32,33 At the community level, establishment of trust between community hospitals and tertiary care centers is a key component to transitioning care and increasing access to major cancer centers34 through telemedicine. On the public policy level, insurance reimbursement for telemedicine visits, particularly audio-only, is crucial to incentivize institutions to provide care to patients that otherwise would not have access.35 Increasing digital and cellular access can significantly improve access equity among those lacking digital access—namely those with low socioeconomic status, age 85 or greater, and in communities of color.36
Telehealth interventions can provide independence and reassurance to patients with cancer. The convenience and independence stabilizes lives that have been disrupted by cancer with personalized care across a physical distance providing remote reassurance with a safety net of healthcare connection 37. Therefore, the development of multi-level interventions to address the various socioeconomic contributors to phone use is crucial for patients to receive equitable care. Additionally, given patient limitations in access to and readiness for telemedicine use, audio-only telephone visits must continue to be equally reimbursed by insurance companies, as currently is possible through the CARES act during the public health emergency of the COVID-19 pandemic. As vaccines continue to be distributed and the country reaches herd immunity, it is imperative to continue making healthcare accessible through efforts to allow patients the option of a more informative and meaningful healthcare interaction 38. Research on telemedicine moving forward will need to address each of these areas individually to see what impact each has on telemedicine adoption, satisfaction, and outcomes.
This study has several limitations. First, it is an observational study, with visit modalities determined by decisions made by patients, providers, and clinic scheduling offices. Furthermore, the visit type was determined based on billing documentation, and the conversion rate from video to phone calls is not known. However, converting failed video visits into phone visits is captured by the billing data, reflective of the video visits being unable to meet the needs of the patient. Provider and patient preferences play a large role in determining the visit type, and certain visits are not feasible for telemedicine in our health system. Changes in patient use of telemedicine and reasons for variations in use are not able to be characterized at a granular level. Because of these findings, our institution has begun qualitative interviews to determine patient, provider, and institutional barriers and facilitators to telemedicine utilization to adapt this rapidly expanding form of care to benefit all patients. This type of research will ensure all stakeholders play a role in identifying possible solutions to the different socioecological determinants of health levels. Concerns about low-value care39 warrant investigation of most appropriate indications and use of telemedicine, incorporating patient and provider preference into its clinical utility. Additionally, prioritizing barriers, such as technologic literacy versus broadband access, transportation to a local public health center versus a local library, etc. is needed to most effectually develop interventions that directly address the barriers most responsible for keeping patients from successfully using telemedicine. Some barriers may not be addressable; therefore, workaround solutions are paramount (e.g. using low bandwidth applications for patients with limited internet data plans).
Conclusions
Expansion of telemedicine use has increased significantly during the COVID-19 pandemic, with historically vulnerable patients disproportionately using audio-only visits. Multi-level interventions are imperative to make telemedicine, especially video-based, an accessible option for all patients.
Acknowledgments
Meeting presentations of this study include the American College of Surgeons Clinical Congress 2021 Oral Presentation, 27th Annual AHRQ NRSA Trainees Research Conference 2021 Podium Presentation, and AcademyHealth Annual Research Meeting 2021 Best Poster Award.
Contributor Information
Connie C Shao, University of Alabama at Birmingham Department of Surgery, Birmingham, AL, USA.
M Chandler McLeod, University of Alabama at Birmingham Department of Surgery, Birmingham, AL, USA.
Lauren T Gleason, University of Alabama at Birmingham Department of Surgery, Birmingham, AL, USA.
Isabel C Dos Santos Marques, University of Alabama at Birmingham Department of Surgery, Birmingham, AL, USA.
Daniel I Chu, University of Alabama at Birmingham Department of Surgery, Birmingham, AL, USA.
Eric L Wallace, University of Alabama at Birmingham Department of Medicine, Birmingham, AL, USA.
Mona N Fouad, University of Alabama at Birmingham Department of Medicine, Birmingham, AL, USA.
Sushanth Reddy, University of Alabama at Birmingham Department of Surgery, Birmingham, AL, USA.
Funding
Funding received from NIH (5T32HS013852), American College of Surgeons Research Resident Award.
Conflict of Interest
The authors indicated no financial relationships.
Author Contributions
Conception/design: C.S., D.C., E.W., M.F., S.R. Provision of study material/patients: M.F., S.R. Collection and/or assembly of data: C.S., S.R., E.W. Data analysis and interpretation: C.S., M.C. M., L.T., I.M. Manuscript writing: C.S., L.T., I.M. Final approval of manuscript: All authors.
Data Availability
The data underlying this article will be shared on reasonable request to the corresponding author.
References
- 1. CMS.gov. Trump administration issues second round of sweeping changes to support U.S. healthcare system during COVID-19 pandemic. Vol 2021: Baltimore, MD: Centers for Medicare & Medicaid Services; 2020. [Google Scholar]
- 2. Robilotti EV, Babady NE, Mead PA, et al. Determinants of COVID-19 disease severity in patients with cancer. Nat Med. 2020;26(8):1218-1223. 10.1038/s41591-020-0979-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Balducci L. Management of cancer in the elderly. Oncology (Williston Park). 2006;20(2):135-43; discussion 144, 146, 151. [PubMed] [Google Scholar]
- 4. Patt D, Wilfong L, Kanipe K, Paulson RS.. Telemedicine for cancer care: implementation across a multicenter community oncology practice. Am J Manag Care. 2020;26(10 Spec No):SP330-SP332. 10.37765/ajmc.2020.88560. [DOI] [PubMed] [Google Scholar]
- 5. Polinski JM, Barker T, Gagliano N, et al. Patients’ satisfaction with and preference for telehealth visits. J Gen Intern Med. 2016;31(3):269-275. 10.1007/s11606-015-3489-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Petursdottir AB, Sigurdardottir V, Rayens MK, Svavarsdottir EK.. The impact of receiving a family-oriented therapeutic conversation intervention before and during bereavement among family cancer caregivers: a nonrandomized trial. J Hosp Palliat Nurs 2020;22(5):383-391. 10.1097/NJH.0000000000000679. [DOI] [PubMed] [Google Scholar]
- 7. Abdel-Wahab M, Rosenblatt E, Prajogi B, Zubizarretta E, Mikhail M.. Opportunities in telemedicine, lessons learned after COVID-19 and the way into the future. Int J Radiat Oncol Biol Phys. 2020;108(2):438-443. 10.1016/j.ijrobp.2020.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Barnett ML, Ray KN, Souza J, Mehrotra A.. Trends in telemedicine use in a large commercially insured population, 2005-2017. JAMA 2018;320(20):2147-2149. 10.1001/jama.2018.12354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Surveillance, Epidemiology, and End Results. Bethesda, MD: SEER Cancer Statistics Review, 1975-2010. [Google Scholar]
- 10. Lam K, Lu AD, Shi Y, Covinsky KE.. Assessing telemedicine unreadiness among older adults in the United States during the COVID-19 pandemic. JAMA Intern Med 2020;180(10):1389-1391. 10.1001/jamainternmed.2020.2671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Seifert A, Batsis JA, Smith AC.. Telemedicine in long-term care facilities during and beyond COVID-19: challenges caused by the digital divide. Front Public Health. 2020;8:601595. 10.3389/fpubh.2020.601595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. York CoN. De Blasio Administration Releases Internet Master Plan For City’s Broadband Future. Web site. https://www1.nyc.gov/office-of-the-mayor/news/010-20/de-blasio-administration-releases-internet-master-plan-city-s-broadband-future. Published 2020. Updated.
- 13. Federal Communications Commission 2020 Broadband Deployment Report. Washington, DC; 2020. [Google Scholar]
- 14. Parikh-Patel A, Morris CR, Kizer KW.. Disparities in quality of cancer care: the role of health insurance and population demographics. Medicine (Baltim). 2017;96(50):e9125. doi: 10.1097/MD.0000000000009125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Patel MI, Lopez AM, Blackstock W, et al. Cancer disparities and health equity: a policy statement from the American Society of Clinical Oncology. J Clin Oncol. 2020;38(29):3439-3448. doi: 10.1200/JCO.20.00642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. ACS demographic and housing estimates. https://data.census.gov/cedsci/table?q=alabama&tid=ACSDP1Y2019.DP05. Published Updated.
- 17. Alabama: rural or urban? ‘It depends,’ according to UA analyst. Tuscaloosa, AL: The University of Alabama News Center; 2012. [Google Scholar]
- 18. Archibald R. One in 10 Alabamians is without health insurance. But rates vary by county. AL.com. New York, NY: Advance Local Media, LLC; 2020. [Google Scholar]
- 19. Medicare payment policies during COVID-19. https://www.telehealth.hhs.gov/providers/billing-and-reimbursement/medicare-payment-policies-during-covid-19/. Published 2021. Updated.
- 20. Latham J. How to calculate distance in excel. https://www.contextures.com/excellatitudelongitude.html. Published Updated Mar 3, 2021. Accessed Mar 21, 2021.
- 21. INCOME IN THE PAST 12 MONTHS (IN 2019 INFLATION-ADJUSTED DOLLARS). Web site. https://data.census.gov/cedsci/table?q=median%20income&g=0400000US01,01.050000&tid=ACSST1Y2019.S1901&hidePreview=true. Published Updated.
- 22. Commission FC. 2019 Broadband Deployment Report 2019. Washington, DC. [Google Scholar]
- 23. Huang S, Fiero MH, Bell ML.. Generalized estimating equations in cluster randomized trials with a small number of clusters: review of practice and simulation study. Clin Trials. 2016;13(4):445-449. doi: 10.1177/1740774516643498. [DOI] [PubMed] [Google Scholar]
- 24. R: A language and environment for statistical computing [computer program]. Vienna, Austria: R Core Team; 2020. [Google Scholar]
- 25. Donaghy E, Atherton H, Hammersley V, et al. Acceptability, benefits, and challenges of video consulting: a qualitative study in primary care. Br J Gen Pract. 2019;69(686):e586-e594. doi: 10.3399/bjgp19X704141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Chunara R, Zhao Y, Chen J, et al. Telemedicine and healthcare disparities: a cohort study in a large healthcare system in New York City during COVID-19. J Am Med Inform Assoc. 2021;28(1):33-41. doi: 10.1093/jamia/ocaa217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Darrat I, Tam S, Boulis M, Williams AM.. Socioeconomic disparities in patient use of telehealth during the coronavirus disease 2019 surge. JAMA Otolaryngol Head Neck Surg 2021;147(3):287-295. doi: 10.1001/jamaoto.2020.5161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Cimperman M, Brencic MM, Trkman P, Stanonik M de L.. Older adults’ perceptions of home telehealth services. Telemed J E Health. 2013;19(10):786-790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Carman KL, Dardess P, Maurer M, et al. Patient and family engagement: a framework for understanding the elements and developing interventions and policies. Health Aff (Millwood) 2013;32(2):223-231. doi: 10.1377/hlthaff.2012.1133. [DOI] [PubMed] [Google Scholar]
- 30. Chi NC, Demiris GA.. systematic review of telehealth tools and interventions to support family caregivers. J Telemed Telecare. 2015;21(1):37-44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Smith B, Magnani JW.. New technologies, new disparities: the intersection of electronic health and digital health literacy. Int J Cardiol. 2019;292:280-282. doi: 10.1016/j.ijcard.2019.05.066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Isibel D. Improving health literacy at the organizational level. J Dr Nurs Pract 2020;13(1):79-83. doi: 10.1891/2380-9418.JDNP-D-19-00028. [DOI] [PubMed] [Google Scholar]
- 33. Dunn P, Hazzard E.. Technology approaches to digital health literacy. Int J Cardiol. 2019;293:294-296. doi: 10.1016/j.ijcard.2019.06.039. [DOI] [PubMed] [Google Scholar]
- 34. Drahota A, Meza RD, Brikho B, et al. Community-academic partnerships: a systematic review of the state of the literature and recommendations for future research. Milbank Q. 2016;94(1):163-214. doi: 10.1111/1468-0009.12184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Contreras CM, Metzger GA, Beane JD, et al. Telemedicine: patient-provider clinical engagement during the COVID-19 pandemic and beyond. J Gastrointest Surg. 2020;24(7):1692-1697. doi: 10.1007/s11605-020-04623-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Roberts ET, Mehrotra A.. Assessment of disparities in digital access among medicare beneficiaries and implications for telemedicine. JAMA Internal Medicine 2020;180(10):1386-1389. doi: 10.1001/jamainternmed.2020.2666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Cox A, Lucas G, Marcu A, et al. Cancer survivors’ experience with telehealth: a systematic review and thematic synthesis. J Med Internet Res. 2017;19(1):e11. doi: 10.2196/jmir.6575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Shachar C, Engel J, Elwyn G.. Implications for telehealth in a postpandemic future: regulatory and privacy issues. JAMA 2020;323(23):2375-2376. doi: 10.1001/jama.2020.7943. [DOI] [PubMed] [Google Scholar]
- 39. O’Reilly-Jacob M, Mohr P, Ellen M, et al. Digital health and low-value care. Healthc (Amst) 2021;9(2):100533. doi: 10.1016/j.hjdsi.2021.100533. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data underlying this article will be shared on reasonable request to the corresponding author.