Abstract
Single cell technologies allow the interrogation of tumor heterogeneity, providing insights into tumor evolution and treatment resistance. To better understand whether circulating tumor cells (CTCs) could complement metastatic biopsies for tumor genomic profiling, we characterized 11 single CTCs and 10 pooled CTC samples at the mutational and copy number aberration (CNA) levels, and compared these results with matched synchronous tumor biopsies from 3 metastatic breast cancer patients with triple-negative (TNBC), HER2-positive and estrogen receptor-positive (ER+) tumors. Similar CNA profiles and the same patient-specific driver mutations were found in bulk tissue and CTCs for the HER2-positive and TNBC tumors, whereas different CNA profiles and driver mutations were identified for the ER+ tumor, which presented two distinct clones in CTCs defined by mutations in ESR1 Y537N and TP53, respectively. Furthermore, de novo mutational signatures derived from CTCs described patient-specific biological processes. These data suggest that tumor tissue and CTCs provide complementary clinically relevant information to map tumor heterogeneity and tumor evolution.
Subject terms: Breast cancer, Translational research, Tumour heterogeneity
Introduction
Next-generation sequencing studies have demonstrated that cancer evolves over time and under the selective pressure of systemic treatment1. Temporal and spatial intratumor heterogeneity has now well been described in breast cancer (BC)2,3.
In the past years, the molecular assessment of circulating tumor cells (CTCs) hold the promise to become a valuable tool to map tumor heterogeneity and monitor tumor evolution4–6. In addition, the enumeration and characterization of CTCs offers several potential clinical applications, ranging from the early detection of cancer, the estimation of the risk of metastatic recurrence, the real-time monitoring of treatment efficacy as well as the identification of resistance mechanisms in different tumor types, including BC6. To date, CellSearch is the only Food and Drug Administration approved technology for the detection of CTCs, and together with the DEPArray system allows the isolation and genomic characterization of single CTCs7–9. Several technologies for enrichment, isolation and characterization of CTCs are currently under development and clinical validation4,5,10.
So far, few studies have used exome sequencing to analyze CTCs in BC and other tumor types11–19. Several studies have suggested that copy number aberrations (CNAs) profiles are usually consistent between CTCs and tumor tissue13,17, as well as among CTCs18. Using a targeted sequencing approach of 130 cancer-related genes, Paoletti et al. compared CTCs to tumor biopsies and detected at least one prioritized driver mutation in 85% of matched CTCs with higher discrepancy being observed for non-driver mutations17. Lohr et al. showed that mutations present in at least 3 CTCs were often present in the bulk tissue (70% of the cases) in two metastatic prostate cancer patients, while trunk mutations were found in 90% of the CTCs12. Furthermore, CTCs were found to mirror the clonal mutations of bone marrow tumor cells in multiple myeloma15,16. More recently, whole exome sequencing performed on 3 CTCs from one BC patient showed high genomic heterogeneity among the analyzed CTCs, with only few single-nucleotide variants (SNVs) shared by all CTCs19, whereas Su et al.18 showed that most of the mutations in the tumor tissue of small cell lung cancer patients were also present in CTCs. Importantly, the characterization of CTCs using whole genome sequencing may also guide treatment personalization14.
In this study, we investigated whether CTCs could complement metastatic biopsies for tumor genomic profiling allowing an optimized advanced stage BC patients’ care.
Results
Somatic mutations and copy number aberration landscape in CTCs from metastatic BC patients
We included in our study 11 single CTCs and 10 pooled CTC samples matched to 3 tumor biopsies as well as 3 pooled white blood cell (WBC) samples from 3 metastatic BC patients (Supplementary Table 1, Supplementary Fig. 1) representing the 3 major BC subtypes, namely triple-negative BC (TNBC) (patient #1), human epidermal growth factor receptor 2 (HER2)-positive/estrogen receptor (ER)-negative BC (patient #2) and ER-positive/HER2-negative BC (patient #3, luminal BC). Of note, time to metastatic relapse was 2.5 years and 8 years for patients with TNBC (#1) and ER+ (#3) tumors, respectively, whereas patient with HER2+ tumor (#2) presented de novo metastatic BC.
We interrogated the mutational landscape and copy number profiles of CTCs as well as matched bulk primary (#2) or metastatic (#1, #3) tumors. Tumor biopsies and CTC samples were taken synchronously. In the 21 evaluable CTC samples, we identified a median of 1395 high-confidence somatic SNVs (range = 203 to 3328 per sample) including a median of 573 nonsynonymous and nonsense SNVs (range = 75 to 1336). We also found a median of 105 CNAs (range = 32 to 149 per sample). In the 3 bulk tumors we identified 91, 144, and 323 high-confidence somatic SNVs including 32, 36, and 127 nonsynonymous and nonsense SNVs. We also found 80, 133, and 82 CNAs in the bulk tumor sample from patients with TNBC, HER2+ and ER+ tumors (#1, #2, and #3), respectively. Supplementary Table 2 provides information about the number of SNVs and CNAs identified for each patient.
Comparison of SNVs between CTCs and synchronous bulk tumor tissue
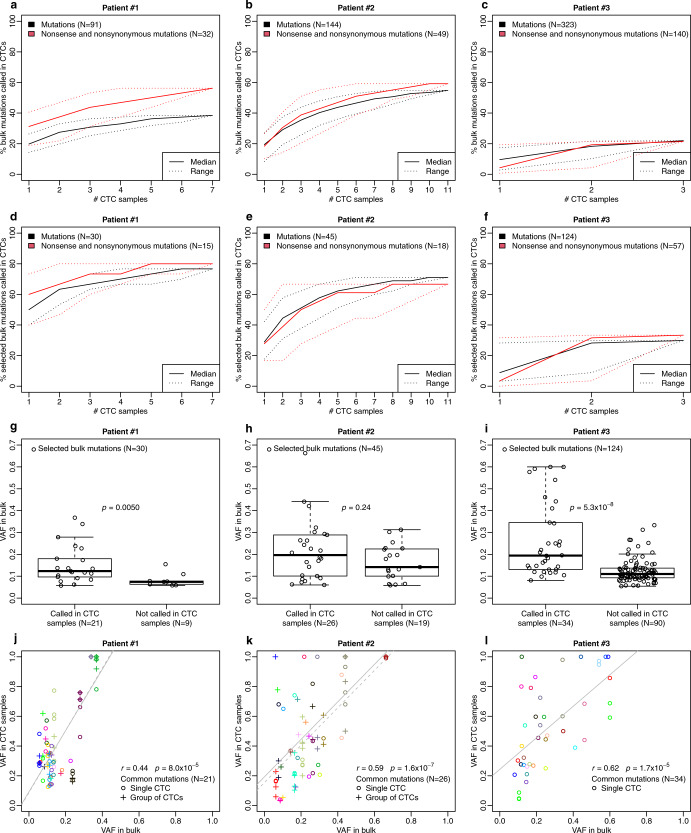
When comparing the mutational landscape of CTC samples to the matched, synchronous bulk tumor, we observed that 38% (TNBC patient #1), 55% (HER2+ patient #2), 22% (ER+ patient #3) of all bulk SNVs were found at least once in the CTC samples (Fig. 1a–c, Supplementary Tables 3–5). When focusing on selected bulk SNVs with adequate coverage on CTCs (at least 20 reads in the CTC samples), 79% (TNBC patient #1), 88% (HER2+ patient #2), 34% (ER+ patient #3) of all bulk SNVs were found at least once in the CTC samples (Fig. 1d–f; Supplementary Tables 3–5). When focusing only on SNVs in cancer driver genes, all SNVs identified in bulk were also identified in CTCs (Fig. 2). Of note, many SNVs that were not called in the CTC samples were actually present but were not called because of lack of sequencing depth or lack of read quality. In particular, the fractions of SNVs from the bulk that were covered with less than 5 reads in CTC samples were 60% (TNBC tumor #1), 64% (HER2+ tumor #2) and 41% (ER+ tumor #3). Interestingly, the percentage of bulk SNVs found in CTCs increased when considering nonsense/nonsynonymous SNVs only. Moreover, by increasing the number of CTC samples analyzed per patient, we recovered more SNVs in the CTC samples from the synchronous tumor tissue (Fig. 1a–f). Mutations present with a higher variant allele frequency (VAF) in the bulk tissue were detected more often in the CTC samples (Fig. 1g–i). Of note, low VAF mutations could be due to multiclonality, or having only one mutated allele in an amplified region, barring technical issues. However, as the VAFs in the bulk tumor were highly correlated with the VAFs in the CTC samples (Fig. 1j–l) multiclonality was not the predominant effect in our case.
Fig. 1. Comparison between single-nucleotide variation (SNVs) detected in bulk tumor and in CTCs.
a–c Percentage of bulk mutations called in CTCs, in patient #1, #2, and #3, respectively. Mutations in bulk and CTCs were independently called using the Strelka algorithm. The solid lines are the median, the dotted lines the range. Black: All mutations. Red: Nonsense and nonsynonymous mutations. d–f Percentage of selected bulk mutations called in CTCs, in patient #1, #2 and #3, respectively. Selected bulk mutations are defined as bulk mutations with 20X coverage in at least one CTC. Mutations in bulk and CTCs were independently called using the Strelka algorithm. The solid lines are the median, the dotted lines the range. Black: All mutations. Red: Nonsense and nonsynonymous mutations. g–i Distribution of the VAFs of selected bulk mutations according to whether they are called or not in CTC samples. Selected bulk mutations are defined as bulk mutations with 20× coverage in at least one CTC and are represented as black circles. Mutations in bulk and CTCs were independently called using the Strelka algorithm. P-value (two-sided) compares the distribution of the VAFs of selected bulk mutations in the two groups (called vs. not called in CTCs) using a Wilcoxon test. j–l Spearman correlation (r) between VAF in bulk and VAF in CTCs, for selected bulk mutations called in CTC samples (common mutations), in patient #1, #2, and #3, respectively. Each color represents a specific mutation. Single CTC samples are represented as circles (o) and group of CTC samples as crosses (+).
Fig. 2. Driver mutations and copy number aberrations for each CTC and bulk sample for the three patients.
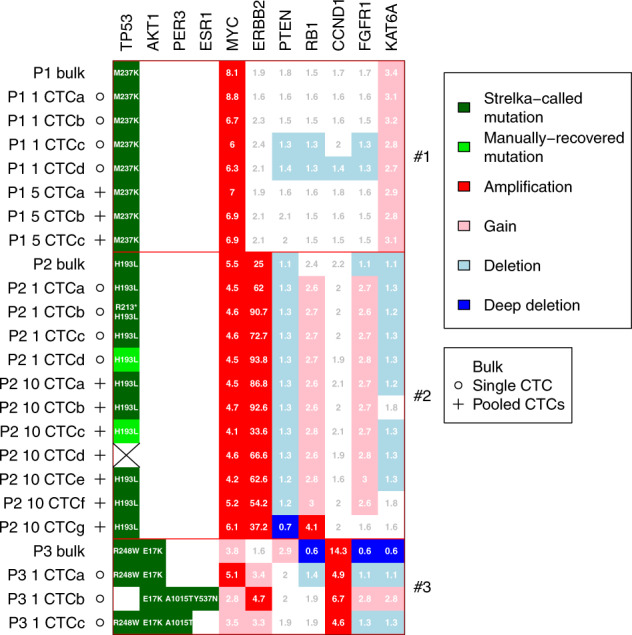
Mutations were called using the Strelka algorithm (dark green). Mutations that were not called by Strelka but were manually recovered after visual inspection with at least one read showing the alternative allele are shown in light green. The stricken cell had no read covering the H193L mutation. Copy numbers are relative to a normalized ploidy of 2.
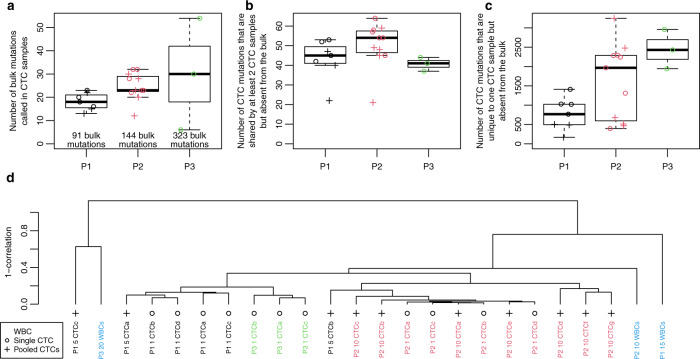
There were three types of mutations present in the CTC samples: 1. mutations that were also present in the bulk tumor (CTC bulk mutations, median = 23, range = 6 to 54), 2. mutations that were shared among at least 2 CTC samples and not present in the bulk (CTC shared mutations, median = 47, range = 21 to 64) and 3. mutations that were present in one CTC sample and absent in the bulk (CTC private mutations, median = 1309, range = 168 to 3250) (Fig. 3a–c and Supplementary Tables 6–8). It is difficult to assess for each mutation whether it is real or an artifact due to whole genome amplification12 or sequencing errors. Thus, the questions are whether a substantial proportion of those mutations is real, and if so, whether they could be clinically relevant. Since we found less than 100 private mutations on amplified WBCs, compared to 200 to 1500 on CTCs, this suggests that a large fraction of those mutations is not artifactual (Supplementary Tables 6–8). We reasoned that if those mutations were real, then they should be produced by processes that are to a certain extent patient-specific, and therefore should display a mutational pattern that is patient-specific as well. To verify this hypothesis, we calculated the number of mutations with specific context, as is done for mutational signature analysis, and used those to cluster the CTC and WBC samples (Fig. 3d). We found that CTC samples would mostly cluster by patient, with the exception of two samples from patient #1. The sample from the TNBC patient (#1) that did not fit the clustering at all (P1 5 CTCc) presented much less reads and mutations called (Supplementary Table 3), which may explain the discrepancy. The WBCs had few mutations which may explain why they did not cluster. Furthermore, there was no clear correlation between the mutational pattern of the WBCs, so it is not clear whether the mutations observed were real (e.g., due to ageing of immune stem cells)20 or technical artifacts.
Fig. 3. CTC mutation analysis.
a Number of bulk mutations called in CTC samples in patients #1, #2 and #3, respectively. b Number of CTC shared mutations in patients #1, #2, and #3, respectively. These are mutations shared among at least 2 CTC samples but absent from the bulk. c Number of CTC private mutations present in only one CTC sample and absent in the bulk, in patients #1, #2 and #3, respectively. Mutations in bulk and CTCs were independently called using the Strelka algorithm. Black circles represent CTC samples. d Clustering of the CTCs based on the mutational pattern.
Comparison of CNA profiles between CTCs and synchronous bulk tumor tissue
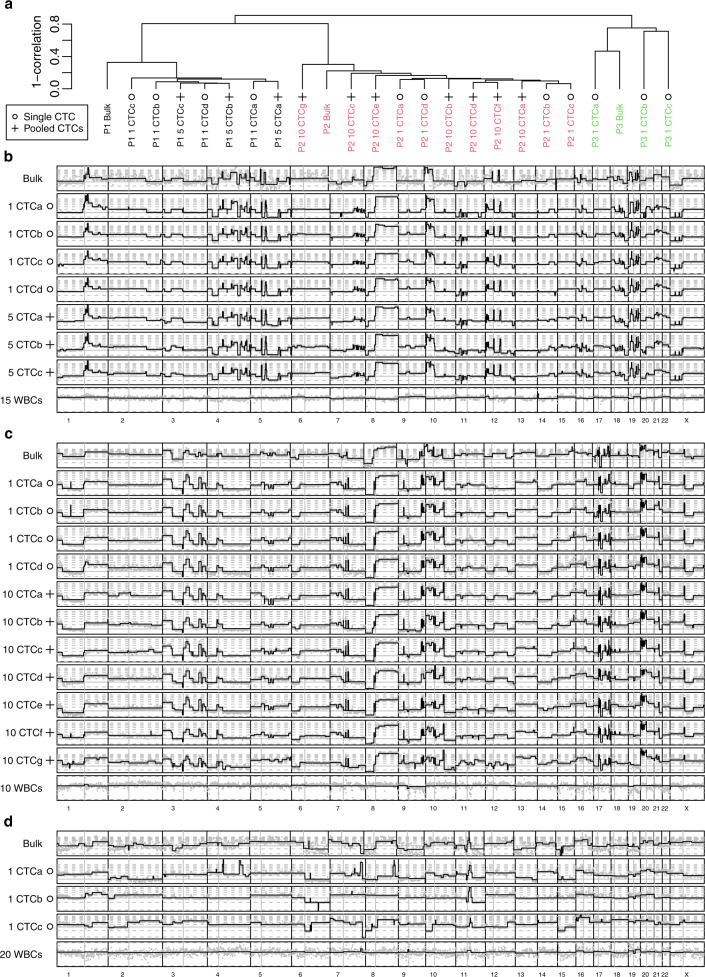
We then compared the CNA profiles from the CTC samples and synchronous bulk tumor and found mostly concordant profiles for the patients with TNBC (#1) and HER2+ tumors (#2), with correlations of CNA profiles between CTC samples ranging from 63 to 94%. The correlations between CTC samples and bulk ranged from 62 to 72% for the patient with TNBC (#1) and 73 to 83% for the patient with HER2+ tumor (#2) (Fig. 4a–c). Conversely, the differences were much larger for the patient with ER+ tumor (#3), for whom we identified 3 different patterns (Fig. 4a, d): one CTC had a moderate correlation of 53% with the bulk, while all other CTC to CTC as well as CTC to bulk correlations ranged between 21 and 32%. In a clustering analysis, CTC samples of a given patient were grouped together as well as with the matched bulk tumor tissue (Fig. 4a).
Fig. 4. Copy number aberration analysis in the bulk tumor and in CTCs.
a Clustering of all CTCs and bulk tumors, showing that samples cluster by patient. b–d Plot of the copy number by chromosome for all samples in patient #1, triple-negative (b), patient #2, HER2 positive (c) and patient #3 ER+/HER2− (d). Non-segmented estimates are given in light gray to show the estimate variance. ER Estrogen receptor, HER2 Human epidermal growth factor receptor 2.
The comparison of the CNA profiles showed that the evaluation for CTC samples was very reproducible, and less noisy than the corresponding profiles from bulk tissue (Fig. 4b–d). The noisier profiles for bulk tissues were due to the relatively low tumor purities (20 to 35% as determined by ABSOLUTE, Supplementary Table 9) which must be corrected for, and that amplify the random sampling variations. Of interest, CTC samples from the HER2+ BC (patient #2) did not show heterogeneity in terms of ERBB2 copy number and were all HER2-amplified.
SNVs and CNAs in known cancer driver genes
We identified SNVs and CNAs in known cancer driver genes including TP53, AKT, MYC, PTEN, and CCND1 (Fig. 2). Importantly, we identified similar CNA aberrations and SNVs in driver genes in matched bulk and CTC samples, consistent with high-quality CTC isolation and sequencing (Fig. 4). In particular, we found TP53 M237K mutation and MYC amplification in all samples from the TNBC patient (#1), TP53 H193L mutation as well as MYC and ERBB2 amplifications in all samples from the HER2+ patient (#2), AKT E17K mutation and CCND1 amplification in all samples from the ER+ patient (#3). At the same time heterogeneity was observed between bulk and CTC samples or among CTC samples from the same patient. For HER2+ patient #2, we observed an RB1 amplification in one CTC sample but not in the bulk. For ER+ patient #3, we observed an activating ESR1 Y537N mutation and an ERBB2 amplification in one CTC sample both absent in the bulk and the other CTC samples. Interestingly, this CTC sample was lacking a TP53 mutation that was present in the bulk and the other CTC samples. An A1015T mutation in PER3 (period circadian regulator) gene was observed in 2 CTC samples, while it was absent from the bulk and the other CTC sample. In this patient, a PTEN loss was also present in the bulk but absent from the CTC samples.
Discussion
High-throughput molecular profiling studies have revolutionized our understanding of BC heterogeneity. It is well established now that BC evolves over time under the selection pressure of various factors including treatments received by the patients2,3. New studies are increasingly focusing on the characterization of the metastatic disease for treatment selection21. However, metastatic tissue biopsies can often be challenging to obtain. The molecular characterization of CTCs therefore appears as a promising approach that can provide unique insights into tumor temporal and spatial heterogeneity through a minimally invasive procedure. In this pilot study of 3 metastatic BC patients, we investigated whether profiling of CTCs at the single cell level can complement the synchronous metastatic bulk tumor tissue analyses.
We showed that CTCs were able to capture about 40% of SNVs identified in the bulk tumor analysis. This proportion increased when focusing on bulk mutations that were well covered on CTCs for the patients with TNBC and HER2+ BC, but not for the ER+ patient. For this patient time from diagnosis of metastatic disease to samples collection was significantly longer compared to the other 2 patients, and that might partly explain the differences observed. Of note, we also showed that by increasing the number of CTCs analyzed we can increase the percentage of identified SNVs from synchronous tumor tissue analyses. Moreover, SNVs with high VAF in tumor tissue were detected significantly more often on CTCs. The heterogeneity between CTCs and tumor tissue in terms of mutational profiles has been previously described, with a higher concordance reported for clonal mutations12,15–18.
Importantly, when focusing on bulk mutations in cancer driver genes, all of them were recovered using single CTC analysis. In addition, CTC analysis revealed mutations in cancer driver genes that were not identified in bulk analysis. Of particular interest, an activating mutation of ESR1 in the ER+ patient, who previously progressed under endocrine therapy, was detectable only in one CTC and could not be identified by deep sequencing in the bulk tumor. The ESR1 Y537N mutation has been associated with endocrine resistance and potential sensitivity to specific estrogen receptor degraders22, and has been previously described in CTCs23. Since this patient received endocrine therapy in both the adjuvant and metastatic settings before entering the study, this finding is not surprising. Interestingly, the CTC that had an ESR1 mutation had no TP53 mutation, contrary to the other CTCs and the bulk from the same patient. The exclusion between ESR1 and TP53 mutations has previously been reported for metastatic BC24.
Furthermore, we identified many SNVs in CTCs that could not be found in the tumor tissue. These SNVs likely represent passenger mutations with little clinical significance. This result has to be interpreted carefully, as whole genome amplification may introduce artifacts12. However, the number of private mutations in the WBCs samples was at least one order of magnitude lower as compared to the CTCs (Supplementary Table 6–8). Furthermore, by comparing de novo mutational signatures derived from WBCs and CTCs, we demonstrated that the distribution of the signatures was different between the patients, as well as between CTCs and WBCs. This supports the hypothesis that those mutations are not an artifact due to whole genome amplification and are produced by distinct biological processes that are mostly shared by the CTCs from the same patient (with the exception of the patient with ER+ tumor). Thus, mutational signatures can be used to identify the common origin and mutational process across CTCs with very different SNV profiles.
By comparing bulk tumor and CTC samples for CNAs, we showed that CTCs and paired bulk tissue clustered together. Furthermore, the CNA profiles of the CTCs in each patient showed overall high concordance, also when compared with the bulk tumor tissue for the TNBC and HER2+ but not for the ER+ patient, as observed in the SNV analyses. This finding confirmed previous studies in which CNA patterns were found to be reproducible across CTCs and compared to the tumor tissue11,13,15–18. For the patient with ER+ BC, as it was the case with SNVs, at the CNA level heterogeneity was observed between the bulk tumor and CTCs. Interestingly, in this patient, ERBB2 copy number amplification was detected on a single CTC but not on bulk tumor analysis. Of note, the primary tumor diagnosed in 2005 presented a weak staining for HER2 by immunohistochemistry, while no staining was observed in the metastatic lesion. This exemplifies the power of single cell analysis to uncover subclonality. Further investigations aimed at evaluating the impact of ERBB2 copy number heterogeneity detected in CTCs on anti-HER2 treatment response is warranted, even in patients with tumors classified as HER2-negative and especially in the light of the recent introduction of the “HER2-low” category25. Indeed, we and others have shown that HER2-positive CTCs can be detected in patients with HER2-negative tumors26. The recently reported DETECT study that randomized 105 patients with HER2-negative metastatic BC and HER2-positive CTCs between standard chemotherapy with or without lapatinib showed promising preliminary results of improved OS with the addition of lapatinib. Further validation in larger patient cohorts is needed.
Our study has some notable limitations. First, the small sample size, although representative of the 3 main BC subtypes, prevented us to perform additional analyses comparing CTCs characteristics across patients with the same BC subtype. This is an exploratory study that needs further validation using additional patients. Second, having characterized a single biopsy from one tumor site, we cannot exclude that the concordance in terms of SNVs could have been higher if multiple tissue samples were analyzed.
In conclusion, we showed that single CTC genomic analysis provides most of the information provided by the genomic analysis of the synchronous bulk metastatic tumors at least in terms of driver SNVs and CNAs. It additionally allows the identification of some driver aberrations that are not detected in the bulk and also provides information on the clonal/subclonal distribution of all aberrations identified. This information is not captured by ctDNA analysis, which does not inform us on the distribution of genomic aberrations in the different clones within the same patient. However, ctDNA analysis is easier to perform in the context of a clinical setting as compared to the tedious procedure of single CTC analysis, hence it remains the preferred liquid biopsy analyte tested in clinical trials and clinical practice. Indeed, multigene assays evaluating ctDNA are already approved for use in clinical practice, but it is not the case for CTCs. Nevertheless, we believe it is worth evaluating whether CTC heterogeneity provides clinically relevant information. The clinical value of this additional information provided by single CTC analysis including information on clonality needs to be prospectively evaluated in larger cohorts.
These data suggest that tumor tissue and single CTC exome sequencing analyses provide complementary information to map tumor heterogeneity and monitor tumor evolution. Further validation for potential clinical applications is needed.
Methods
Patients and samples
Three patients with metastatic BC treated at the Institut Jules Bordet were included in the study, one for each of the 3 major BC subtypes. For each patient, whole blood samples were collected simultaneously with the tissue biopsies. Samples’ collection was obtained after several lines of treatment for metastatic disease for patients #1 and #3, and at the time of diagnosis for de novo metastatic disease in patient #2. Detailed characteristics of the patients included in the study are provided in Supplementary Table 1. The study was approved by the Institut Jules Bordet ethics committee (internal number 1698) and was conducted in accordance with the Declaration of Helsinki, written informed consent being obtained from all participants.
Circulating tumor cell isolation
CTCs were enumerated and enriched from whole blood samples using the CellSearch system, according to the manufacturer’s recommendations (Janssens Diagnostics, LLC). CellSearch cartridges were processed to recover single and pools of CTCs using the DEPArrayTM technology (Menarini Silicon Biosystems). WBCs were isolated using the same procedure as the CTCs. Whole genome amplification (WGA) of the DNA from single and pools of CTCs and WBCs was performed using the Ampli1 kit (Menarini Silicon Biosystems), as previously described9. Quality control of the WGA was assessed using the Ampli1 QC kit.
Whole exome sequencing
DNA extraction was performed using the QIAamp DNA FFPE Tissue kit (Qiagen) and the DNeasy Blood and Tissue kit for the FFPE tumor tissues and whole blood samples respectively. Library preparation was performed using the Truseq Exome kit (Illumina). Whole exome library sequencing was performed using the Illumina HiSeq2000 platform with a 200× targeted coverage. Eleven single CTCs (4, 4 and 3 for patients #1, #2 and #3, respectively) and 10 pooled CTC samples (3 and 7 for patients #1 and #2, respectively) comprising 5 (patient #1) or 10 (patient #2) CTCs were sequenced (Supplementary Tables 6–8), for a total of 21 CTC samples, as well as 3 pools of WBCs (one for each patient).
Mutation analysis
Reads were trimmed using Trimmomatic (version 0.36)27 and aligned using bwa (version 0.7.17)28. Duplicates were removed using Picard tools (version 2.17)29. Variants were called with Strelka (version 2.9.2)30, using the whole blood as the normal. Mutations fitting the pattern TTAACTGACAGC were considered as artifacts and removed, as were mutations appearing in more than one patient. Mutations with a VAF below 20% were discarded, unless they were present in the corresponding bulk sample.
Bulk mutations were defined as mutations present in the bulk but absent from both whole blood normal DNA and amplified WBC from the same patient. CTC mutations were defined as mutations present in at least one CTC sample but absent from the WBC cells sample from the same patient. CTC shared mutations were defined as CTC mutations that are shared by at least 2 CTC samples but absent from the bulk. CTC private mutations were defined as CTC mutations that were unique to only one CTC sample but absent from the bulk.
Frequencies of mutations by context (flanking bases) were obtained with the R package deconstructSig31. Hierarchical clustering on those frequencies was done with complete linkage, using 1-cor(log(0.01 + f)) as the distance.
We selected to show on the Oncoplot genes that had at least 2 mutations across all samples that appeared at least 20 times in COSMIC, in addition to ESR1 and selected driver CNAs. Individual mutations shown appear at least 20 times in COSMIC, except for TP53 mutations for which the cutoff was set at 5 appearances in COSMIC.
Copy number assessment
CNAs were determined by counting reads in 10 kb windows. Those counts were normalized using WBC pools (for CTC/CTC pools) or normal blood (for bulk tumor). Segmentation was performed using circular binary segmentation from the DNAcopy32 R package. Correction for purity for bulk tumor sample was performed with ABSOLUTE33. Pairwise concordance of CNAs profiles was assessed using Spearman correlation of CNAs profiles across the whole genome. Using copy numbers normalized to a sample ploidy of 2, amplifications were defined as CN > 4, gains as CN > 2.5, deletions as CN < 1.5 and deep deletions as CN < 0.8.
Statistical analyses
Comparisons between groups for continuous variables (i.e., distribution of the VAFs of selected bulk mutations in two groups, called vs. not called in CTCs) were performed using a Wilcoxon test. P values were two-sided, no correction for multiple testing was performed. Correlations were Spearman, p values on correlations were obtained with the cor.test R function. Boxplots were standard R boxplots, so center lines are at the median, hinges are at the first and third quartiles, while the whiskers extend to the most extreme data point which is no more than 1.5 times the interquartile range from the box. Analyses were performed using the R software (version 3.5).
Supplementary information
Acknowledgements
The study was partly funded by the Breast Cancer Research Foundation (BCRF), MEDIC and “Les Amis de Bordet” foundations. C.S. is supported by the National Fund for Scientific Research (F.R.S.—FNRS). M.R. is supported by Télévie and the Fonds National de la Recherche Scientifique (F.R.S.—FNRS).
Author contributions
F.R. and M.I. conceived, designed and supervised the study. F.R., D.V., C.S., and M.I. contributed to develop the methodology. F.R., G.R., D.P., D.S., D.L., P.C., and L.D. contributed to data acquisition and provided technical support. F.R., D.V., C.S., and M.I. analyzed and interpreted the data. F.R., D.V., M.R., F.D., C.S., and M.I. wrote the first draft of the paper, which was edited and approved by all authors.
Data availability
The whole exome sequencing data from this publication have been deposited to the EGA database (https://ega-archive.org) and assigned the identifier EGAS00001005228.
Code availability
Open-source software were used for this study. The scripts used are available upon request.
Competing interests
All the authors declare no non-financial competing interests. The authors C.S. and M.I. declare the following competing financial interests. C.S.: advisory board (receipt of honoraria or consultations fees): Astellas, Cepheid, Vertex, Seattle genetics, Puma, Amgen, Exact Sciences; participation in company sponsored speaker’s bureau: Eisai, Prime Oncology, Teva, Foundation Medicine, Exact Sciences; other support (travel, accommodation expenses): Roche, Genentech, Pfizer. M.I: Consultant/Honoraria: Novartis, Seattle Genetics; research grant to his institution: Roche, Pfizer, Natera Inc. The remaining authors declare no financial competing interests.
Footnotes
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
These authors contributed equally: Françoise Rothé, David Venet.
These authors jointly supervised this work: Christos Sotiriou, Michail Ignatiadis.
Supplementary information
The online version contains supplementary material available at 10.1038/s41523-022-00445-7.
References
- 1.McGranahan N, Swanton C. Clonal heterogeneity and tumor evolution: past, present, and the future. Cell. 2017;168:613–628. doi: 10.1016/j.cell.2017.01.018. [DOI] [PubMed] [Google Scholar]
- 2.Yates LR, et al. Subclonal diversification of primary breast cancer revealed by multiregion sequencing. Nat. Med. 2015;21:751–759. doi: 10.1038/nm.3886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Yates LR, et al. Genomic evolution of breast cancer metastasis and relapse. Cancer Cell. 2017;32:169–184.e7. doi: 10.1016/j.ccell.2017.07.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Haber DA, Velculescu VE. Blood-based analyses of cancer: circulating tumor cells and circulating tumor DNA. Cancer Discov. 2014;4:650–661. doi: 10.1158/2159-8290.CD-13-1014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kilgour E, Rothwell DG, Brady G, Dive C. Liquid biopsy-based biomarkers of treatment response and resistance. Cancer Cell. 2020;37:485–495. doi: 10.1016/j.ccell.2020.03.012. [DOI] [PubMed] [Google Scholar]
- 6.Ignatiadis M, Sledge GW, Jeffrey SS. Liquid biopsy enters the clinic—implementation issues and future challenges. Nat. Rev. Clin. Oncol. 2021;18:297–312. doi: 10.1038/s41571-020-00457-x. [DOI] [PubMed] [Google Scholar]
- 7.Cristofanilli M, et al. Circulating tumor cells, disease progression, and survival in metastatic breast cancer. N. Engl. J. Med. 2004;351:781–791. doi: 10.1056/NEJMoa040766. [DOI] [PubMed] [Google Scholar]
- 8.Cristofanilli M, et al. Circulating tumor cells: a novel prognostic factor for newly diagnosed metastatic breast cancer. J. Clin. Oncol. 2005;23:1420–1430. doi: 10.1200/JCO.2005.08.140. [DOI] [PubMed] [Google Scholar]
- 9.Peeters DJE, et al. Semiautomated isolation and molecular characterisation of single or highly purified tumour cells from CellSearch enriched blood samples using dielectrophoretic cell sorting. Br. J. Cancer. 2013;108:1358–1367. doi: 10.1038/bjc.2013.92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ignatiadis M, Lee M, Jeffrey SS. Circulating tumor cells and circulating tumor DNA: challenges and opportunities on the path to clinical utility. Clin. Cancer Res. 2015;21:4786–4800. doi: 10.1158/1078-0432.CCR-14-1190. [DOI] [PubMed] [Google Scholar]
- 11.Ni X, et al. Reproducible copy number variation patterns among single circulating tumor cells of lung cancer patients. Proc. Natl Acad. Sci. U.S.A. 2013;110:21083–21088. doi: 10.1073/pnas.1320659110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lohr JG, et al. Whole-exome sequencing of circulating tumor cells provides a window into metastatic prostate cancer. Nat. Biotechnol. 2014;32:479–484. doi: 10.1038/nbt.2892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gao Y, et al. Single-cell sequencing deciphers a convergent evolution of copy number alterations from primary to circulating tumor cells. Genome Res. 2017;27:1312–1322. doi: 10.1101/gr.216788.116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gulbahce N, et al. Quantitative whole genome sequencing of circulating tumor cells enables personalized combination therapy of metastatic cancer. Cancer Res. 2017;77:4530–4541. doi: 10.1158/0008-5472.CAN-17-0688. [DOI] [PubMed] [Google Scholar]
- 15.Mishima Y, et al. The mutational landscape of circulating tumor cells in multiple myeloma. Cell Rep. 2017;19:218–224. doi: 10.1016/j.celrep.2017.03.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Manier S, et al. Whole-exome sequencing of cell-free DNA and circulating tumor cells in multiple myeloma. Nat. Commun. 2018;9:1691. doi: 10.1038/s41467-018-04001-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Paoletti C, et al. Comprehensive mutation and copy number profiling in archived circulating breast cancer tumor cells documents heterogeneous resistance mechanisms. Cancer Res. 2018;78:1110–1122. doi: 10.1158/0008-5472.CAN-17-2686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Su Z, et al. Inferring the evolution and progression of small-cell lung cancer by single-cell sequencing of circulating tumor cells. Clin. Cancer Res. 2019;25:5049–5060. doi: 10.1158/1078-0432.CCR-18-3571. [DOI] [PubMed] [Google Scholar]
- 19.Yin J, et al. Characterization of circulating tumor cells in breast cancer patients by spiral microfluidics. Cell Biol. Toxicol. 2019;35:59–66. doi: 10.1007/s10565-018-09454-4. [DOI] [PubMed] [Google Scholar]
- 20.Welch JS, et al. The origin and evolution of mutations in acute myeloid leukemia. Cell. 2012;150:264–278. doi: 10.1016/j.cell.2012.06.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lefebvre C, et al. Mutational profile of metastatic breast cancers: a retrospective analysis. PLoS Med. 2016;13:e1002201. doi: 10.1371/journal.pmed.1002201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Jeselsohn R, Buchwalter G, De Angelis C, Brown M, Schiff R. ESR1 mutations—a mechanism for acquired endocrine resistance in breast cancer. Nat. Rev. Clin. Oncol. 2015;12:573–583. doi: 10.1038/nrclinonc.2015.117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Paolillo C, et al. Detection of activating estrogen receptor gene (ESR1) mutations in single circulating tumor cells. Clin. Cancer Res. 2017;23:6086–6093. doi: 10.1158/1078-0432.CCR-17-1173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bertucci F, et al. Genomic characterization of metastatic breast cancers. Nature. 2019;569:560–564. doi: 10.1038/s41586-019-1056-z. [DOI] [PubMed] [Google Scholar]
- 25.Tarantino P, et al. HER2-low breast cancer: pathological and clinical landscape. J. Clin. Oncol. 2020;38:1951–1962. doi: 10.1200/JCO.19.02488. [DOI] [PubMed] [Google Scholar]
- 26.Ignatiadis M, et al. HER2-positive circulating tumor cells in breast cancer. PLoS ONE. 2011;6:e15624. doi: 10.1371/journal.pone.0015624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Bolger AM, Lohse M, Usadel B. Trimmomatic: a flexible trimmer for Illumina sequence data. Bioinformatics. 2014;30:2114–2120. doi: 10.1093/bioinformatics/btu170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Li H, Durbin R. Fast and accurate short read alignment with Burrows-Wheeler transform. Bioinformatics. 2009;25:1754–1760. doi: 10.1093/bioinformatics/btp324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Picard Tools—By Broad Institute. http://broadinstitute.github.io/picard/.
- 30.Saunders CT, et al. Strelka: accurate somatic small-variant calling from sequenced tumor-normal sample pairs. Bioinformatics. 2012;28:1811–1817. doi: 10.1093/bioinformatics/bts271. [DOI] [PubMed] [Google Scholar]
- 31.Rosenthal R, McGranahan N, Herrero J, Taylor BS, Swanton C. DeconstructSigs: delineating mutational processes in single tumors distinguishes DNA repair deficiencies and patterns of carcinoma evolution. Genome Biol. 2016;17:31. doi: 10.1186/s13059-016-0893-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Seshan, V. E. & Olshen, A. DNAcopy: DNA copy number data analysis. 10.18129/B9.bioc.DNAcopy (2014).
- 33.Carter SL, et al. Absolute quantification of somatic DNA alterations in human cancer. Nat. Biotechnol. 2012;30:413–421. doi: 10.1038/nbt.2203. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The whole exome sequencing data from this publication have been deposited to the EGA database (https://ega-archive.org) and assigned the identifier EGAS00001005228.
Open-source software were used for this study. The scripts used are available upon request.