Highlights
-
•
Seven chronic disease risks were analysed among community mental health consumers.
-
•
Latent class analysis identified three clusters of chronic disease risks.
-
•
Education level, gender, age and diagnosis were associated with cluster allocation.
-
•
Clustering patterns reinforce the importance of addressing multiple risks.
-
•
Findings can be used to assist the development of multi-risk interventions.
Keywords: Clustering, Chronic disease risks, Tobacco smoking, Alcohol consumption, Fruit and vegetable intake, Physical activity, Body Mass Index, Mental health conditions, Community mental health services
Abstract
This study identified clusters of chronic disease risks and explored associations between clusters and demographic characteristics and mental health conditions, among people accessing community mental health services. Data from a cross-sectional telephone survey of Australian mental health consumers (n = 567) were analysed. Clusters were identified based on tobacco smoking (53.5%), harmful chronic alcohol consumption (20.1%), harmful acute alcohol consumption (43.5%), inadequate fruit and vegetable intake (66.0%), inadequate physical activity (75.5%), inadequate strength activity (81.8%), and high body mass index (BMI) (67.9%), using latent class analysis. Multinomial logistic regression examined associations between cluster membership and participant characteristics. Three groups were identified: Cluster 1 (19.05%) had < 0.5 probabilities for most risks; Cluster 2 (34.04%) had high probabilities of all risks, particularly tobacco smoking and both types of harmful alcohol consumption; and Cluster 3 (46.91%) had high probabilities of both inadequate physical and strength activity, inadequate fruit and vegetable intake, and high BMI. Compared to Cluster 1 membership, participants with higher education were less likely to be in either Cluster 2 or 3, females or those over 55 were more likely to be in Cluster 3, those with a substance use disorder were more likely to be in Cluster 2, and those with a personality disorder were less likely to be in Cluster 3. The clustering patterns reinforce the importance of addressing multiple chronic disease risks for people with a mental health condition. Preventive care interventions targeting clusters of risks may help reduce the burden of chronic disease among this high-risk population.
1. Introduction
People with a mental health condition are more likely to have modifiable chronic disease risks relative to the general population internationally (Lê Cook et al., 2014, Di Florio et al., 2014, Teasdale et al., 2019, Vancampfort et al., 2017) and in Australia (Bartlem et al., 2015, Australian Bureau of Statistics, 2018), including tobacco smoking, harmful alcohol consumption, inadequate fruit and vegetable intake, inadequate physical activity, and overweight and obesity. The presence of any mental health condition is associated with elevated rates of each risk (Firth et al., 2019), and more severe mental health conditions, such as bipolar disorder and schizophrenia, are most strongly associated with risks (Jackson et al., 2015, Di Florio et al., 2014, Teasdale et al., 2019, Firth et al., 2018, Vancampfort et al., 2017) relative to other conditions. Whilst the presence of multiple risks is common among the general population (Meader et al., 2016, Noble et al., 2015), the likelihood of multiple risks is even higher for people with a mental health condition (Bartlem et al., 2021, Bartlem et al., 2015, Hahn et al., 2014). The presence of multiple risks increases the chance of chronic disease morbidity and mortality relative to one risk factor alone (Peters et al., 2019), and is a key contributor to the reduced life expectancy of up to 20 years experienced by people with a mental health condition compared to the general population (Campostrini et al., 2019, Chen et al., 2017, Firth et al., 2019).
Chronic disease risks are interrelated and measuring the prevalence of each, or multiple risks does not capture co-occurrence within individuals, nor allow exploration of risk patterns (McAloney et al., 2013). Cluster analysis can be used to examine clusters of risks that are likely to co-occur within individuals, enabling a more comprehensive understanding of risk patterns which may have important implications for the design of interventions. Further, exploration of associations between identified clusters and participant characteristics enables identification of groups who could most benefit from interventions. Most research that explores risk clustering has been undertaken with general population (Noble et al., 2015, Meader et al., 2016), vocational education students (Atorkey et al., 2021a), or child/adolescent samples (Whitaker et al., 2021). Among general population sample studies, cluster analysis has identified that tobacco smoking and harmful alcohol consumption cluster, as do inadequate nutrition and inadequate physical activity (Noble et al., 2015, Meader et al., 2016). Such data is valuable as it allows intervention approaches to consider the interactive nature of risks that are likely to cluster, rather than single-risk modification interventions (Prochaska, 2008, James et al., 2016). Studies suggest that interventions which simultaneously address clustered risks can potentially be more effective and cost-effective (Prochaska, 2008). Research also demonstrates that demographic factors such as lower socio-economic status and lower education tend to be associated with clusters characterised by a greater number of risks (Noble et al., 2015, Oftedal et al., 2019, Meader et al., 2016, Griffin et al., 2014, Paul et al., 2016).
To the authors’ knowledge, no studies have explored patterns of multiple risks using cluster analysis specifically among a sample of adults with mental health conditions. A small number of studies in general population samples have examined associations between cluster membership and presence of mental health variables (Griffin et al., 2014, Cao et al., 2020, Oftedal et al., 2019, Vermeulen-Smit et al., 2015, Ye et al., 2016, Jao et al., 2019), and have consistently found associations between membership of risk-dominant clusters and mental health condition presence or worse mental health symptoms (Oftedal et al., 2019, Jao et al., 2019, Ye et al., 2016, Vermeulen-Smit et al., 2015). For example, a large Australian study (n = 10,638) examined self-reported smoking status, diet quality, alcohol consumption, physical activity, and sleep quality, and identified four clusters: three of which were characterised by greater risk compared to one ‘healthy’ cluster (37% of sample) (Oftedal et al., 2019). Participants in each of the three risk-dominant clusters had significantly increased odds (OR = 2.14–6.02) of reporting frequent mental distress compared to participants in the ‘healthy’ cluster.
Given the identified higher prevalence of chronic disease and associated risks amongst people with a mental health condition, it is possible that the clustering of risks among this population may differ to that of the general population. However, no previous research has explored the clustering of risks specifically among a sample of people with a mental health condition. It is important to understand how, and to what extent chronic disease risks cluster among this population group, as the tendency for risks to aggregate and interact has important implications for preventive interventions and health policy. To address these evidence gaps, the aims of the current study were to conduct an exploratory analysis to: 1) identify clusters of key chronic disease risks (tobacco smoking, chronic alcohol consumption, acute alcohol consumption, fruit and vegetable intake, physical activity, strength activity, and body mass index (BMI) status) among a sample of people accessing community mental health services; and 2) explore possible associations between identified clusters and demographic characteristics and mental health conditions.
2. Methods
2.1. Design and setting
Cross-sectional surveys were undertaken with consumers of two government community mental health services in one Local Health District in a regional area of New South Wales (NSW), Australia. In Australia, government community mental health services are a major provider of mental health outpatient care (AIHW, 2020). The services provide specialised adult mental health care, that includes psychiatric rehabilitation, early diagnosis, and management to consumers with a range of mental health conditions (such as depression, anxiety, psychoses, bipolar disorder, eating disorders, comorbid substance-use) of varying severities.
Data were collected using Computer Assisted Telephone Interviews as part of a larger quasi-experimental controlled trial, involving consumers participating in two cross-sectional surveys: baseline in 2019 (April to October), and follow-up in 2020 (May to October). In the trial, one service received a practice change intervention and one continued to provide usual care. Included in the present study were all participants (from the control and intervention service) who completed a survey at baseline (prior to the intervention), and unique participants from the control service (i.e., not already identified in the baseline period) who completed a survey at follow-up (post intervention). The trial was approved by the Hunter New England Human Research Ethics Committee (Ref no. 18/11/21/4.06) and the University of Newcastle Human Research Ethics Committee (Ref no. H-2019–0108), and registered (ACTRN12619001379101).
2.2. Participants and data collection procedures
Adult consumers who had an in-person or telehealth appointment within the previous four months were identified via an electronic medical record system. Consumers were mailed a study information sheet that included a toll-free number to call if they did not wish to be contacted. Consumers were contacted approximately two weeks later via telephone by trained interviewers to assess further eligibility criteria (English speaking, mentally and physically capable of answering survey questions) and gain verbal consent to participate.
2.3. Measures
Survey items were based on previous surveys undertaken by the research team with mental health consumers (Bartlem et al., 2015, Fehily et al., 2020a, Fehily et al., 2020b) and validated items from recommended assessment tools (ABS, 2019):
2.3.1. Risk factors
Participants were asked to self-report: how often they currently smoke cigarettes or any other type of tobacco product; their alcohol consumption using items from the AUDIT-C (Bush et al., 1998); the number of serves of fruit, and vegetables, typically consumed each day; physical activity level using the International Physical Activity Questionnaire-Short Form (Craig et al., 2003); and their current weight and height which was used to calculate BMI (WHO, 2000) (see Table 1).
Table 1.
Health risk measures and definition of ‘at risk’ variables included in cluster analysis.
| Risk Variable | Measures [response options]c | Definition of ‘at risk’ |
|---|---|---|
| Tobacco smoking | How often they currently smoke cigarettes or any other type of tobacco product [daily; at least once a week; less than once a week; not at all (quit<4 months ago); not at all (quit 4 months or more ago); never smoked] | Smoked in the last four months, or quit within the last four months |
| Harmful chronic alcohol consumption | How often they consumed alcohol [never, monthly or less, 2–4 times a month, 2–3 times a week, 4 + times a week]; How many days per week they would have a drink containing alcohol [0–7 days]; How many standard drinks they would have on a typical drinking day [1 or 2; 3 or 4; 5 or 6; 7 to 9; 10 +] | >10 standard drinks/week |
| Harmful acute alcohol consumption | How often they would consume five or more standard drinks on one occasion [never; less than monthly; monthly; weekly; daily or almost daily] | >4 standard drinks/day on any day |
| Inadequate fruit & vegetable intake | Number of serves of fruit typically consumed each day [0; 1; 2; 3; 4; 5; 6 or more]; Number of serves of vegetables typically consumed each day [0; 1; 2; 3; 4; 5; 6 or more] |
<2 serves/day of fruit and < 5 serves/day of veg |
| Inadequate moderate to vigorous physical activity | How many days, during the last seven days, they did vigorous physical activity (e.g. running, jogging, gym classes, boxing, soccer or squash) [0–7 days]; How many days, during the last seven days, they did moderate physical activity (e.g. fast walking, baseball, tennis, easy bicycling, volleyball, easy swimming), for at least ten minutes at a time [0 –7 days]; Participants who engaged in vigorous and/or moderate activity on at least one day were asked to report, respectively, how many minutes per session on average they spent doing these activities [open numerical] | <150 min moderate activity or, <75 min vigorous activity or, less than an equivalent combination of botha |
| Inadequate strength activity | Strength activity was measured by asking participants to report the number of days during the last week they engaged in any type of muscle strengthening activities (e.g. exercises using free weights, body weight exercises or gym-based strength exercises) [0 –7 days] | <2 days/week of including strength/resistance in physical activity |
| High BMIb | Current weight (kg or lbs) [open numerical]; Current height (cm or feet/inches) [open numerical] | BMI >= 25 (Overweight or Obese) |
an equivalent combination of moderate and vigorous activity was calculated by dividing the number of moderate activity minutes per week by two, then adding the number of vigorous activity minutes per week. If this total was<75, then considered inadequate (i.e. at risk).
Overweight (25.0–29.9) and Obese (30.0 + ) BMI levels were classified as high BMI, representing the BMI risk variable. BMI calculated as weight in kilograms divided by height in metres squared) (WHO, 2000).
all items included a ‘don’t know’ and ‘refused’ option.
2.3.2. Demographic characteristics and mental health conditions
Gender, age, marital status, highest level of education achieved, employment status and identification as Aboriginal and/or Torres Strait Islander were assessed. Participants also reported the mental health condition/s they were receiving care for from the service (depression, anxiety, schizophrenia, bipolar disorder, Post Traumatic Stress Disorder (PTSD), personality disorder, substance use disorder and other).
2.4. Statistical analysis
Statistical analyses were conducted using SAS v9.4 (SAS Institute, Cary, North Carolina, USA); p < 0.05 (two-tailed) was used to indicate statistical significance. Consistent with previous research exploring clustering of multiple risks (Champion et al., 2018, Kwan et al., 2016, Oftedal et al., 2019), prevalence of each risk was represented by a categorical variable reflecting adherence to Australian National Guidelines (see Table 1) with seven risk variables calculated for the cluster analysis. Six dichotomous variables were calculated (at risk/non-adherence to guideline, vs not at risk/adherence to guideline): (1) tobacco smoking; (2) harmful chronic alcohol consumption; (3) harmful acute alcohol consumption; (4) inadequate fruit and vegetable intake; (5) inadequate physical activity; and (6) inadequate strength activity. Acute and chronic alcohol consumption, and inadequate physical activity and strength activity were considered separately based on the Australian national guidelines (Australian Government Department of Health, 2014, National Health and Medical Research Council, 2020) and their distinct impact on health and chronic conditions (Westcott, 2012, Churilla et al., 2012). For the seventh risk variable, BMI calculations were classified into four levels: underweight (<18.5); healthy weight (18.5–24.9); overweight (25.0–29.9), and obese (30.0+), where (7) high BMI was classified as overweight or obese (see Table 1). Behavioural risk variables were calculated as at risk if participants responded with ‘don’t know’ for any items in the variable calculation (Table 2 footnote j) (Bartlem et al., 2015, McElwaine et al., 2013, Tremain et al., 2017, Metse et al., 2017), and BMI was considered missing if participants responded to either height or weight items with’don’t know’. Descriptive statistics summarised demographic characteristics, mental health conditions, and risk variables.
Table 2.
Demographic characteristics, mental health conditions and risks.
| Variable | N (Total N = 567) | % |
|---|---|---|
| Gender | ||
| Female | 345 | 60.8 |
| Male | 220 | 38.8 |
| Transgender or gender non-conforming | 2 | 0.4 |
| Age | ||
| 18 – 34 | 206 | 36.3 |
| 35 – 54 | 257 | 45.3 |
| 55+ | 104 | 18.3 |
| Employment Status | ||
| Employedb | 136 | 24.0 |
| Unemployed | 120 | 21.2 |
| Unable work due to health reasons | 231 | 40.7 |
| Otherc | 80 | 14.1 |
| Marital Status | ||
| Never married | 285 | 50.3 |
| Married or living together in a relationship | 136 | 24.0 |
| Otherd | 146 | 25.7 |
| Education Level | ||
| Some high school or lesse | 210 | 37.0 |
| Completed high school certificate | 92 | 16.2 |
| Technical and further education (TAFE) certificate or diploma | 212 | 37.4 |
| Diploma, University degree or higher | 53 | 9.3 |
| Aboriginal or Torres Strait Islander | 77a | 13.6 |
| Mental Health Conditionfg | ||
| Depression | 343 | 60.5 |
| Anxiety | 302 | 53.3 |
| Schizophrenia or other psychotic disorder | 150 | 26.5 |
| Bipolar disorder | 119 | 21.0 |
| Post-traumatic stress disorder | 87 | 15.3 |
| Personality disorder | 83 | 14.6 |
| Substance use disorder | 36 | 6.3 |
| Eating disorder | 29 | 5.1 |
| Obsessive-compulsive disorder | 9 | 1.6 |
| Otherh | 17 | 3.0 |
| Behavioural Risk Variables i, j | ||
| Tobacco smoking | 303 | 53.5 |
| Harmful chronic alcohol consumption | 114 | 20.1 |
| Harmful acute alcohol consumption | 246 | 43.5 |
| Inadequate fruit and vegetable intakek | 355 | 66.0 |
| Inadequate moderate to vigorous physical activity | 428 | 75.5 |
| Inadequate strength activity | 464 | 81.8 |
| BMIi | ||
| Underweight (<18.5) | 23 | 4.6 |
| Healthy weight (18.5 – 24.9) | 137 | 27.5 |
| High BMIl (25.0 + ) | 339 | 67.9 |
n = 1 Torres Strait Islander.
includes full time, part time, casual, on maternity leave.
includes home duties, student, retired, other.
includes separated, divorced, widowed.
includes never attended school, some primary school, completed primary school, some high school, school certificate.
participants could report one or more mental health conditions.
N = 18 report did not report a mental health condition.
other conditions reported included ADHD, Autism and Epilepsy.
there was some variability in total n sizes for each variable (n BMI = 499; n fruit and vegetable intake = 538; n smoking = 566; n both alcohol = 566; and n both activity = 567) due to missing data.
the proportion of participants at risk due to ‘‘don’t know’ responses, ranged from 0% (smoking) to 4.3% (chronic alcohol consumption).
88.5% (n = 476) were at risk for vegetable intake, and 66.5% (n = 358) were at risk for fruit intake. N = 29 not asked as had an eating disorder.
24.6% (n = 123) were overweight (25.0 – 29.9), and 43.3% (n = 216) were obese (30.0 + ).
The statistical approach used to examine clustering was latent class analysis (LCA), where participants were probabilistically allocated to latent clusters according to their pattern of the 7 risk variables. Latent Class models are parameterised according to 1) an assumed known number of classes, 2) the proportion of each class (class membership probabilities), and 3) the item response proportions within each class. The unknown parameters from this model were estimated using the Expectation-Maximisation algorithm in PROC LCA (Lanza et al., 2007). The number of latent classes was guided by comparing Akaike information criterion and Bayesian information criterion measures of fit between models with the number of latent classes varied between 2 and 10, as well as considering the interpretability of the resulting models. Participants were subsequently allocated a single class based on the highest-class membership probability produced for that individual; corresponding item-response probabilities were plotted accordingly to assist in the interpretation of the models. The item-response probability for risk ‘high BMI’ was calculated by adding the probability for the overweight level of BMI and the obese level of BMI.
Associations between best latent class membership and the following 13 participant characteristics were determined using separate univariate multinomial logistic regressions (age, gender, marital status, education, employment, Aboriginality, depression, anxiety, schizophrenia, bipolar disorder, personality disorder, PTSD, substance use disorder (yes/no for each mental health condition)). Chi-square odds ratios, 95% confidence intervals, number of observations used (N), pairwise p-values and overall Type III p-values were produced. Multivariable models were constructed using variables associated with the outcome (threshold p < 0.25) from corresponding univariate analyses; adjusted odds ratios, 95% confidence intervals, number of observations used (N), pairwise p-values and Type III p-values were presented with Cluster 1 as the reference category.
3. Results
3.1. Sample characteristics
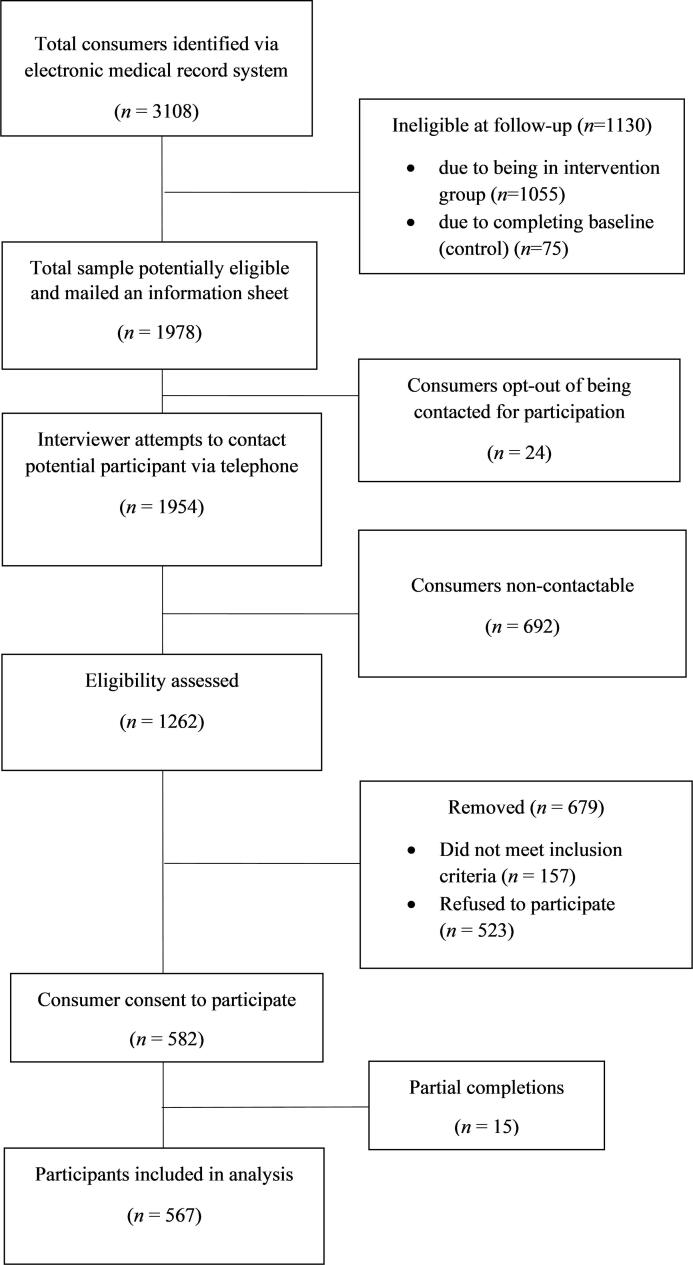
Fig. 1 illustrates the participant recruitment process. Of 1105 eligible consumers, 567 participants completed the survey (61% female; mean age = 40.8 years). Table 2 outlines the prevalence of demographic characteristics, mental health conditions and risks for the sample.
Fig. 1.
Flow diagram of participant recruitment.
3.2. Risk clusters
Three clusters were selected as appropriate based on the interpretability of the identified clusters in the LCA (see Fig. 2 which depicts the risk probability profiles of the clusters). Cluster 1 (19.1% of participants) was characterised by relatively lower risk overall (with four risks < 0.5 probability and three risks > 0.5 probability) whereas other clusters had higher probabilities for all risks, apart from harmful acute alcohol consumption in Cluster 3. Cluster 2 (34.0% of participants) was characterised by all risks (all risks > 0.5 probability): tobacco smoking (0.73); both harmful alcohol consumption variables (0.97 and 0.58 for acute and chronic, respectively); inadequate fruit and vegetable intake (0.73); both types of inadequate activity (0.79 and 0.80 for physical and strength, respectively); and high BMI (0.67). Cluster 3 (46.9% of participants) was characterised by inadequate fruit and vegetable intake (0.68), both types of inadequate activity (0.95 and 0.93 for physical and strength, respectively), and high BMI (0.72 probability).
Fig. 2.
Item-response probabilities for risks by latent class.
*Probabilities for BMI levels of overweight (C1: 0.28; C2: 0.31; C3: 0.19) and obesity (C1: 0.34; C2: 0.36; C3: 0.52) were added to reflect high BMI shown in the graph. See Supplementary material for individual item-response probabilities.
3.3. Cluster associations with demographic characteristics and mental health conditions
Univariate associations of clusters with demographic characteristics and mental health conditions are reported in Table 3. The univariate analysis found that 8 variables had a p-value of < 0.25 (age, gender, martial, education, employment, depression, personality disorder, and substance use disorder) and these were entered into the multinomial logistic regression model. In the multivariable model (reference category: Cluster 1), gender (p < 0.0001), age (p = 0.0125), presence of a personality disorder (p = 0.0036), education level (p = 0.0446) and presence of a substance use disorder (p = 0.0381) were found to be significantly associated with latent cluster membership based on respective type III p-values (Table 3). When examining pairwise comparisons, participants with a university degree or higher education level had lower odds of Cluster 2 membership than Cluster 1 (OR: 0.308) relative to those with some high school or less (p = 0.0092). People with a substance use disorder had higher odds of Cluster 2 membership than Cluster 1 (OR = 11.953), relative to those without a substance use disorder (p = 0.0168). No other pairwise associations were significant for Cluster 1 versus Cluster 2 membership (p > 0.05). Females had higher odds of Cluster 3 membership than Cluster 1 (OR = 2.907), relative to males (type-III p < 0.0001). Those aged over 55 also had higher odds of Cluster 3 membership than Cluster 1 (OR = 3.180), relative to those aged 18 to 34 (p = 0.0061). People who were unable to work due to health reasons had higher odds of Cluster 3 membership compared to Cluster 1 (OR = 2.766), relative to employed individuals (p = 0.0028), however interpretations here are cautious as the overall effect of employment on cluster membership (type III) was not significant. Participants with a personality disorder had lower odds of Cluster 3 membership than Cluster 1 (OR = 0.365), compared to those without a personality disorder (p = 0.0062). Those with a university degree or higher education level also had lower odds of Cluster 3 membership than Cluster 1 (OR = 0.392), relative to those who completed some high school or less (p = 0.0227).
Table 3.
Estimates of multivariable multinomial logistic regression model of latent cluster allocation (modelling probability of being in Cluster 1).
| Variable | Characteristic | Cluster 2 |
Cluster 3 |
Type III P-Value | ||
|---|---|---|---|---|---|---|
| Odds Ratio (95% CI) | Pairwise P-Value | Odds Ratio (95% CI) | Pairwise P-Value | |||
| Age | 35–54 vs. 18–34 | 1.273 (0.720, 2.251) | 0.4059 | 1.749 (0.995, 3.073) | 0.0519 | 0.0125* |
| 55 + vs. 18–34 | 1.229 (0.509, 2.970) | 0.6461 | 3.180 (1.392, 7.264) | 0.0061* | ||
| Gendera | Female vs. Male | 1.381 (0.815, 2.338) | 0.2303 | 2.907 (1.727, 4.891) | <0.0001* | <0.0001* |
| Marital | Married or living together in a relationship vs. Never married | 1.300 (0.687, 2.460) | 0.4199 | 1.544 (0.832, 2.862) | 0.1683 | 0.1711 |
| Other vs. Never married | 1.749 (0.881, 3.471) | 0.1100 | 1.146 (0.586, 2.241) | 0.6899 | ||
| Education | Completed HSC vs. Some high school or less | 1.492 (0.687, 3.239) | 0.3114 | 1.590 (0.734, 3.444) | 0.2394 | 0.0446* |
| TAFE certificate or diploma vs. Some high school or less | 0.952 (0.534, 1.700) | 0.8692 | 0.815 (0.461, 1.440) | 0.4804 | ||
| University degree or higher vs. Some high school or less | 0.308 (0.127, 0.747) | 0.0092* | 0.392 (0.175, 0.877) | 0.0227* | ||
| Employment | Other vs. Employed | 1.142 (0.524, 2.488) | 0.7385 | 1.160 (0.535, 2.514) | 0.7074 | 0.0572 |
| Unable to work due to health reasons vs. Employed | 1.518 (0.769, 2.993) | 0.2287 | 2.766 (1.419, 5.391) | 0.0028* | ||
| Unemployed vs. Employed | 1.293 (0.643, 2.600) | 0.4710 | 1.528 (0.758, 3.079) | 0.2360 | ||
| Depression | Yes vs. No | 0.987 (0.593, 1.643) | 0.9595 | 1.536 (0.930, 2.536) | 0.0933 | 0.0703 |
| Personality disorder | Yes vs. No | 0.874 (0.437, 1.747) | 0.7025 | 0.365 (0.177, 0.751) | 0.0062* | 0.0036* |
| Substance use disorder | Yes vs. No | 11.953 (1.563, 91.423) | 0.0168* | 7.504 (0.954, 59.014) | 0.0555 | 0.0381* |
*Asterix denotes (P=<0.05).
Gender included male and female, where transgender or gender non-conforming was excluded from the respective logistic regression model due to low numbers (n = 2).
4. Discussion
This study was the first to use cluster analysis to explore patterns of modifiable chronic disease risks among people accessing community mental health services. Three risk clusters were identified: Cluster 1, ‘lower risk overall’, exhibiting the lowest risk of the three clusters; and Cluster 2 and 3, ‘high overall risk and substance use’ and ‘inadequate activity and fruit and vegetable intake, and high BMI’, respectively, exhibiting higher risk. Four demographic variables and two mental health conditions were associated with the risk-dominant clusters when compared to the lower risk cluster.
4.1. Clusters
When compared to other clusters within this study, Cluster 1 was characterised by the relatively lowest probabilities of most risks, Cluster 2 was characterised by the relatively highest probabilities of tobacco smoking, both types of alcohol consumption and inadequate fruit and vegetable intake, and Cluster 3 was characterised by the relatively highest probabilities of both types of inadequate activity, inadequate fruit and vegetable intake, and high BMI. Prior research in general population samples has typically identified three to four clusters, of which one is ‘healthy’ (Noble et al., 2015, Vermeulen-Smit et al., 2015, Pettigrew et al., 2021, Jao et al., 2019, Cao et al., 2020, Di Benedetto et al., 2019, Oftedal et al., 2019), and one cluster characterised by elevated substance use (Noble et al., 2015, Jao et al., 2019, Vermeulen-Smit et al., 2015, Griffin et al., 2014, Noel et al., 2013, Funderburk et al., 2008).
The profile and proportion of Cluster 1 differs considerably to that typically found in general population research. Although identified as the ‘healthier’ cluster, Cluster 1 nevertheless evidenced considerable levels of risk with > 0.5 probability of three risks and almost 0.5 probability of tobacco smoking. In comparison, previous studies using cluster analysis in general population samples have reported ‘healthy’ clusters characterised by zero or one risks (Meader et al., 2016, Noble et al., 2015, Whitaker et al., 2021), and the probability of tobacco smoking is typically < 0.1 in such clusters (Hutchesson et al., 2021, Oftedal et al., 2019, Pettigrew et al., 2021). Additionally, studies in the Netherlands and Australia with general population and University samples report ‘healthy’ clusters to account for the largest proportion (54–80%) of the sample (Vermeulen-Smit et al., 2015, Oftedal et al., 2019, Di Benedetto et al., 2019). In contrast, the ‘healthy’ cluster (Cluster 1) accounts for the smallest proportion (19.05%) relative to Cluster 2 (34.04%) and Cluster 3 (46.91%). Although direct comparisons are not possible due to the lack of a comparison group, these findings provide support for existing evidence that multiple chronic disease risks are likely more prevalent among people with a mental health condition compared to the general population. Further research including a non-mental health comparison group would strengthen this finding. Regardless, these results reinforce the need for action to address multiple risks for this population.
A large proportion of the sample were allocated to clusters characterised by higher risk. Cluster 2 was distinguished based on the probabilities of substance-related risks, yet demonstrated > 0.5 probabilities for all risks. The current finding suggest people with a mental health condition engaging in substance-related risks are likely to also have inadequate physical and strength activity levels as well as inadequate fruit and vegetable consumption. Cluster 3 accounted for almost half of participants and had > 0.5 probabilities for both types of inadequate activity, inadequate fruit and vegetable intake, and high BMI. Clustering of such risks is supported by previous research suggesting that physical activity impacts diet and weight (Beaulieu et al., 2016, Fenton et al., 2021, Höchsmann et al., 2020), a potentially more salient association for people with a mental health condition due to health promoting barriers such as medication induced cravings and low motivation (Bailey et al., 2018, Scott and Happell, 2011). The probability of tobacco smoking in Cluster 3 (0.46) is typically higher than previous studies which have identified ‘unhealthy’ clusters that are not characterised by smoking (probabilities ranging from 0.04 to 0.29) (Atorkey et al., 2021b, Hutchesson et al., 2021, Oftedal et al., 2019, Pettigrew et al., 2021), evidence of tobacco smoking being a particularly prevalent risk among this population group, likely due to the perceived role of tobacco smoking in mental illness symptom management (Bailey et al., 2018, Keller-Hamilton et al., 2019).
Although it is difficult to make direct comparisons with previous studies due to various population groups and measurement approaches (such as different tools to measure risk and different combinations of risks included), the current study provides evidence of clustering of addictive behaviours requiring restraint or abstinence (smoking and alcohol in Cluster 2) and health promoting behaviours requiring active engagement (physical activity and fruit and vegetable consumption in Cluster 3) (de Vries et al., 2008, Noble et al., 2015). The clustering patterns identified, and the large proportion of participants (81%) in the risk-dominant clusters, highlights the need to target multiple risks. Despite conflicting points of view regarding multi-risk interventions, there is evidence to suggest that interventions targeting clustered risks may be more effective in aiding overall behaviour change than singular risk interventions (Cradock et al., 2017, Nigg and Long, 2012, Sweet and Fortier, 2010) as well as being less costly (Park et al., 2013, Fehily et al., 2020a, Fehily et al., 2020b, Ritzwoller et al., 2011), potentially due to the synergistic effects that change in one risk behaviour has on another (Hammami et al., 2020, Huang et al., 2012, Spring et al., 2012). However, to the authors’ knowledge, no studies have directly compared singular and multi-risk interventions among people with a mental health condition. Finding ways to develop and test multi-risk interventions for people with a mental health condition to understand the most acceptable and effective approaches to addressing multiple risks is warranted.
4.2. Associations
This study identified that people accessing community mental health services with higher education levels were less likely to be allocated the risk-dominant clusters, which is consistent with general population research (Noble et al., 2015, Oftedal et al., 2019, Pettigrew et al., 2021, Griffin et al., 2014, Hsu et al., 2013). Additionally, females and older people were more likely to be in Cluster 3 than Cluster 1, compared to males and those aged 18–34, respectively. As Cluster 3 exhibited the relatively lowest probability for harmful acute alcohol consumption and relatively highest probabilities for both types of inadequate activity, these findings are consistent with previous research demonstrating females and older people are less likely to binge drink (Pettigrew et al., 2021, Atorkey et al., 2021a, Atorkey et al., 2021b, Shaw and Agahi, 2012, Lee et al., 2012, Griffin et al., 2014, Paul et al., 2016, Noel et al., 2013) as well as engage in adequate physical activity (Alley et al., 2017, Bennie et al., 2016) than males and younger people, respectively. Understanding characteristics associated with certain clusters may provide additional considerations for tailoring multi-risk interventions.
The current sample included a broad range of mental health diagnoses, with only two conditions demonstrating significant associations. It is not surprising that substance use disorder had increased odds of Cluster 2 membership, given previously identified associations between substance use disorder, tobacco smoking, and alcohol consumption (Weinberger et al., 2017, Weinberger et al., 2016, Kelly et al., 2012). The finding that personality disorder had significantly lower odds of Cluster 3 membership is difficult to interpret, and no previous studies have assessed such an association. Future research should test associations between risk clusters and specific mental health conditions with larger sample sizes to allow stronger conclusions to be made. The number of participants with particular mental health conditions was limited (see Table 2), and therefore assessing associations with specific conditions was exploratory. Notwithstanding, findings of minimal differences across diagnoses are consistent with research suggesting that people with any mental health condition (i.e. not limited to depression or severe mental illness) experience high levels of chronic disease risk. Taken with previous meta-analyses demonstrating a life expectancy gap for all mental health conditions (Walker et al., 2015), the findings reinforce the importance of interventions focused on the prevention of chronic disease risks to be provided systematically and routinely to all people accessing community mental health services, in line with national and state health service guidelines (Australian Health Ministers’ Advisory Council, 2017, NSW Ministry of Health, 2021), and international recommendations (WHO, 2021).
4.3. Limitations
Some further study limitations should be acknowledged. Firstly, participants were people accessing community mental health services within NSW, Australia. It is unclear how generalisable the results are to people accessing other mental health care settings, or to people with a mental health condition not currently receiving care. Secondly, the data is self-report and therefore may under report risk as studies have found that the prevalence of risk factors in the community are higher according to gold standard data sources compared to self-report data (Althubaiti, 2016, Cronin et al., 2009, Newell et al., 1999, Prince et al., 2020, Spitzer and Weber, 2019). Additionally, some data collection coincided with the COVID-19 lockdowns (∼25%), the first experienced in this area of Australia. Research exploring the impact of COVID-19 lockdowns in Australia found the general population were more likely to engage in risks than before the lockdowns (Stanton et al., 2020, Brindal et al., 2021, Glenister et al., 2021, Arora and Grey, 2020, Phillipou et al., 2020). To the authors’ knowledge no research has been conducted with samples of people with a mental health condition, and whilst participants were prompted to respond with how they would normally engage in behaviours, it is unclear how the lockdowns impacted on reporting of risks. Further, characteristics of mental health conditions, such as severity and medications, may have an impact on risks however were not measured. Finally, due to the cross-sectional nature of the study, it is not possible to draw conclusions regarding the causality of the relationship between the clusters and mental health conditions examined.
5. Conclusion
Findings of this study strengthen previous research demonstrating people with a mental health condition have a high likelihood of engaging in multiple chronic disease risks, and adds a perspective of risk clustering. Minimal associations between clusters and participant characteristics suggest that regardless of demographics and diagnoses, this issue is important across all people with a mental health condition. Consistent with evidence and international health guidelines (World Health Organization, 2021, Kluge et al., 2020), the current findings can assist with planning intervention approaches to target multiple risk factors which commonly occur together and what factors to consider to adapt interventions accordingly. Further research could explore the effectiveness of multi-risk interventions and involve consumers and other stakeholders in their development (NSW Ministry of Health, 2018, Mental Health Commission of New South Wales, 2014). Understanding the most effective approaches to addressing the high prevalence and clustering of risks among people with a mental health condition may be an important step to redressing the physical health and life expectancy inequalities experienced.
CRediT authorship contribution statement
Casey Regan: Conceptualization, Methodology, Writing – original draft, Writing – review & editing, Project administration, Funding acquisition. Caitlin Fehily: Conceptualization, Methodology, Writing – review & editing, Supervision. Elizabeth Campbell: Conceptualization, Methodology, Writing – review & editing, Supervision. Jenny Bowman: Conceptualization, Methodology, Writing – review & editing, Supervision, Funding acquisition. Jack Faulkner: Conceptualization, Methodology, Formal analysis, Writing – review & editing. Christopher Oldmeadow: Conceptualization, Methodology, Formal analysis, Writing – review & editing. Kate Bartlem: Conceptualization, Methodology, Writing – review & editing, Supervision, Funding acquisition.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgements
The authors would like to thank the community mental health services and consumers for their support and contribution to the project. We would also like to acknowledge CATI interviewers who conducted the survey, and Christophe Lecathelinais for his statistical assistance in data management. Funding Financial support has been received by the Cancer Institute NSW: Community of Practice Implementation Science (Institution Number (G#): G1800812), Priority Research Centre of Health Behaviour (analysis costs), The Australian Prevention Partnership Centre (publication costs), and University of Newcastle higher degree research. Dr Kate Bartlem is supported by a National Health and Medical Research Council Early Career Fellowship (#1142272).
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.pmedr.2022.101870.
Appendix A. Supplementary data
The following are the Supplementary data to this article:
References
- Alley S.J., Duncan M.J., Schoeppe S., Rebar A.L., Vandelanotte C. 8-year trends in physical activity, nutrition, TV viewing time, smoking, alcohol and BMI: A comparison of younger and older Queensland adults. PLoS One. 2017;12(3) doi: 10.1371/journal.pone.0172510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Althubaiti A. Information bias in health research: definition, pitfalls, and adjustment methods. J. Multi. Healthcare. 2016;9:211. doi: 10.2147/JMDH.S104807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arora T., Grey I. Health behaviour changes during COVID-19 and the potential consequences: A mini-review. J. Health Psychol. 2020;25(9):1155–1163. doi: 10.1177/1359105320937053. [DOI] [PubMed] [Google Scholar]
- Atorkey P., Byaruhanga J., Paul C., Wiggers J., Bonevski B., Tzelepis F. Multiple Health Risk Factors in Vocational Education Students: A Systematic Review. Int. J. Environ. Res. Public Health. 2021;18(2):637. doi: 10.3390/ijerph18020637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Atorkey P., Paul C., Wiggers J., Bonevski B., Nolan E., Oldmeadow C., Mitchell A., Byrnes E., Tzelepis F. Clustering of multiple health-risk factors among vocational education students: a latent class analysis. Transl. Behav. Med. 2021;11(10):1931–1940. doi: 10.1093/tbm/ibab068. [DOI] [PubMed] [Google Scholar]
- Australian Bureau of Statistics, 2018. National Health Survey: First results. 2017-18. Table 5.1. Available from: https://www.abs.gov.au/statistics/health/health-conditions-and-risks/national-health-survey-first-results/2017-18.
- Australian Bureau of Statistics, 2019. National Health Survey: First Results, 2018-19. Australian Bureau of Statistics. Canberra.
- Australian Health Ministers’ Advisory Council, 2017. National Strategic Framework for Chronic Conditions. Australian Government. Canberra.
- Australian Institute of Health and Welfare, 2020. Mental health services in Australia. Australian Government.
- Australian Government Department of Health . Commonwealth of Australia; 2014. Physical activity and exercise guidelines for all Australians. [Google Scholar]
- Bailey J.M., Hansen V., Wye P.M., Wiggers J.H., Bartlem K.M., Bowman J.A. Supporting change in chronic disease risk behaviours for people with a mental illness: A qualitative study of the experiences of family carers. BMC Public Health. 2018;18(1):1–13. doi: 10.1186/s12889-018-5314-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bartlem K.M., Bowman J.A., Bailey J.M., Freund M., Wye P.M., Lecathelinais C., McElwaine K.M., Campbell E.M., Gillham K.E., Wiggers J.H. Chronic disease health risk behaviours amongst people with a mental illness. Aust. N. Z. J. Psychiatry. 2015;49(8):731–741. doi: 10.1177/0004867415569798. [DOI] [PubMed] [Google Scholar]
- Bartlem K., Gibson L., Fehily C., Lodge S., Wiggers J., Bowman J. Multiple health behaviours and interest in change among people with a mental health condition: A brief report. Prevent. Med. Rep. 2021;22 doi: 10.1016/j.pmedr.2021.101383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beaulieu K., Hopkins M., Blundell J., Finlayson G. Does habitual physical activity increase the sensitivity of the appetite control system? A systematic review. Sports Med. 2016;46(12):1897–1919. doi: 10.1007/s40279-016-0518-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bennie J.A., Pedisic Z., van Uffelen, Charity M.J., Harvey J.T., Banting L.K., Eime R.M. Pumping iron in Australia: prevalence, trends and sociodemographic correlates of muscle strengthening activity participation from a national sample of 195,926 adults. PLoS One. 2016;11(4) doi: 10.1371/journal.pone.0153225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brindal E., Ryan J.C., Kakoschke N., Golley S., Zajac I.T., Wiggins B. Individual differences and changes in lifestyle behaviours predict decreased subjective well-being during COVID-19 restrictions in an Australian sample. J. Health (Oxford, England). 2021 doi: 10.1093/pubmed/fdab040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bush K., Kivlahan D.R., McDonell M.B., Fihn S.D., Bradley K.A., Ambulatory Care Quality Improvement Project (ACQUIP The AUDIT alcohol consumption questions (AUDIT-C): an effective brief screening test for problem drinking. Arch. Intern. Med. 1998;158(16):1789–1795. doi: 10.1001/archinte.158.16.1789. [DOI] [PubMed] [Google Scholar]
- Campostrini S., Dal Grande E., Taylor A.W. Increasing gaps in health inequalities related to non-communicable diseases in South Australia; implications towards behavioural risk factor surveillance systems to provide evidence for action. BMC Public Health. 2019;19(1):1–11. doi: 10.1186/s12889-018-6323-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cao R., Gao T., Hu Y., Qin Z., Ren H., Liang L., Li C., Mei S. Clustering of lifestyle factors and the relationship with depressive symptoms among adolescents in northeastern China. J. Affect. Disord. 2020;274:704–710. doi: 10.1016/j.jad.2020.05.064. [DOI] [PubMed] [Google Scholar]
- Champion K.E., Mather M., Spring B., Kay-Lambkin F., Teesson M., Newton N.C. Clustering of multiple risk behaviors among a sample of 18-year-old Australians and associations with mental health outcomes: a latent class analysis. Front. Public Health. 2018;6:135. doi: 10.3389/fpubh.2018.00135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen C.M., Lee I.C., Su Y.Y., Mullan J., Chiu H.C. The longitudinal relationship between mental health disorders and chronic disease for older adults: a population-based study. Int. J. Geriatric Psychiatry. 2017;32(9):1017–1026. doi: 10.1002/gps.4561. [DOI] [PubMed] [Google Scholar]
- Churilla J.R., Magyari P.M., Ford E.S., Fitzhugh E.C., Johnson T.M. Muscular strengthening activity patterns and metabolic health risk among US adults. J. Diabetes. 2012;4(1):77–84. doi: 10.1111/j.1753-0407.2011.00172.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cradock K.A., ÓLaighin G., Finucane F.M., Gainforth H.L., Quinlan L.R., Ginis K.A.M. Behaviour change techniques targeting both diet and physical activity in type 2 diabetes: A systematic review and meta-analysis. Int. J. Behav. Nutr. Phys. Activity. 2017;14(1) doi: 10.1186/s12966-016-0436-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Craig C.L., Marshall A.L., Sjöström M., Bauman A.E., Booth M.L., Ainsworth B.E., et al. International physical activity questionnaire: 12-country reliability and validity. Med. Sci. Sports Exerc. 2003;35(8):1381–1395. doi: 10.1249/01.MSS.0000078924.61453.FB. [DOI] [PubMed] [Google Scholar]
- Cronin K.A., Miglioretti D.L., Krapcho M., Yu B., Geller B.M., Carney P.A., Ballard-Barbash R. Bias associated with self-report of prior screening mammography. Cancer Epidemiology Biomarkers & Prevention. 2009;18(6):1699–1705. doi: 10.1158/1055-9965.EPI-09-0020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Vries H., van 't Riet J., Spigt M., Metsemakers J., van den Akker M., Vermunt J.K., Kremers S. Clusters of lifestyle behaviors: results from the Dutch SMILE study. Prev. Med. 2008;46(3):203–208. doi: 10.1016/j.ypmed.2007.08.005. [DOI] [PubMed] [Google Scholar]
- Di Benedetto M., Towt C.J., Jackson M.L. A Cluster analysis of sleep quality, self-care behaviors, and mental health risk in Australian university students. Behav. Sleep Med. 2019 doi: 10.1080/15402002.2019.1580194. [DOI] [PubMed] [Google Scholar]
- Di Florio A., Craddock N., Van den Bree M. Alcohol misuse in bipolar disorder. A systematic review and meta-analysis of comorbidity rates. Eur. Psychiatry. 2014;29(3):117–124. doi: 10.1016/j.eurpsy.2013.07.004. [DOI] [PubMed] [Google Scholar]
- Fehily C.MC., Bartlem K.M., Wiggers J.H., Wye P.M., Clancy R.V., Castle D.J., Wilson A., Rissel C.E., Wutzke S., Hodder R.K., Colyvas K., Murphy F., Bowman J.A. Effectiveness of embedding a specialist preventive care clinician in a community mental health service in increasing preventive care provision: A randomised controlled trial. Aust. N. Z. J. Psychiatry. 2020;54(6):620–632. doi: 10.1177/0004867420914741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fehily C., Ling R., Searles A., Bartlem K., Wiggers J., Hodder R., Wilson A., Colyvas K., Bowman J. An economic evaluation of a specialist preventive care clinician in a community mental health service: a randomised controlled trial. BMC Health Serv. Res. 2020;20(1) doi: 10.1186/s12913-020-05204-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fenton S., Burrows T.L., Collins C.E., Holliday E.G., Kolt G.S., Murawski B., Rayward A.T., Stamatakis E., Vandelanotte C., Duncan M.J. Behavioural mediators of reduced energy intake in a physical activity, diet, and sleep behaviour weight loss intervention in adults. Appetite. 2021;165 doi: 10.1016/j.appet.2021.105273. [DOI] [PubMed] [Google Scholar]
- Firth J., Stubbs B., Teasdale S.B., Ward P.B., Veronese N., Shivappa N., Hebert J.R., Berk M., Yung A.R., Sarris J. Diet as a hot topic in psychiatry: a population-scale study of nutritional intake and inflammatory potential in severe mental illness. World Psychiatry. 2018;17(3):365–367. doi: 10.1002/wps.20571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Firth J., Siddiqi N., Koyanagi A.i., Siskind D., Rosenbaum S., Galletly C., Allan S., Caneo C., Carney R., Carvalho A.F., Chatterton M.L., Correll C.U., Curtis J., Gaughran F., Heald A., Hoare E., Jackson S.E., Kisely S., Lovell K., Maj M., McGorry P.D., Mihalopoulos C., Myles H., O'Donoghue B., Pillinger T., Sarris J., Schuch F.B., Shiers D., Smith L., Solmi M., Suetani S., Taylor J., Teasdale S.B., Thornicroft G., Torous J., Usherwood T., Vancampfort D., Veronese N., Ward P.B., Yung A.R., Killackey E., Stubbs B. The Lancet Psychiatry Commission: a blueprint for protecting physical health in people with mental illness. Lancet Psychiatry. 2019;6(8):675–712. doi: 10.1016/S2215-0366(19)30132-4. [DOI] [PubMed] [Google Scholar]
- Funderburk J.S., Maisto S.A., Sugarman D.E., Wade M. The covariation of multiple risk factors in primary care: a latent class analysis. J. Behav. Med. 2008;31(6):525–535. doi: 10.1007/s10865-008-9176-1. [DOI] [PubMed] [Google Scholar]
- Glenister K.M., Ervin K., Podubinski T. Detrimental health behaviour changes among females living in rural areas during the COVID-19 pandemic. Int. J. Environ. Res. Public Health. 2021;18(2):722. doi: 10.3390/ijerph18020722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Griffin B., Sherman K.A., Jones M., Bayl-Smith P. The Clustering of health behaviours in older Australians and its association with physical and psychological status, and sociodemographic indicators. Ann. Behav. Med. 2014;48(2):205–214. doi: 10.1007/s12160-014-9589-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hahn L.A., Galletly C.A., Foley D.L., Mackinnon A., Watts G.F., Castle D.J., Waterreus A., Morgan V.A. Inadequate fruit and vegetable intake in people with psychosis. Aust. N. Z. J. Psychiatry. 2014;48(11):1025–1035. doi: 10.1177/0004867414553950. [DOI] [PubMed] [Google Scholar]
- Hammami N., Chaurasia A., Bigelow P., Leatherdale S.T. Gender differences in the longitudinal association between multilevel latent classes of chronic disease risk behaviours and body mass index in adolescents. Health Promotion & Chronic Disease Prevent. Canada: Res., Policy & Practice. 2020;40(9):259–266. doi: 10.24095/hpcdp.40.9.01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Höchsmann C., Dorling J.L., Apolzan J.W., Johannsen N.M., Hsia D.S., Martin C.K. Baseline habitual physical activity predicts weight loss, weight compensation, and energy intake during aerobic exercise. Obesity. 2020;28(5):882–892. doi: 10.1002/oby.22766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hsu H.C., Luh D.L., Chang W.C., Pan L.Y. Joint trajectories of multiple health-related behaviors among the elderly. Int. J. Public Health. 2013;58(1):109–120. doi: 10.1007/s00038-012-0358-9. [DOI] [PubMed] [Google Scholar]
- Huang D.Y.C., Lanza H.I., Murphy D.A., Hser Y.I. Parallel development of risk behaviors in adolescence: potential pathways to co-occurrence. Int. J. Behav. Dev. 2012;36:247–257. doi: 10.1177/0165025412442870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hutchesson M.J., Duncan M.J., Oftedal S., Ashton L.M., Oldmeadow C., Kay-Lambkin F., Whatnall M.C. Latent class analysis of multiple health risk behaviors among Australian university students and associations with psychological distress. Nutrients. 2021;13(2):425. doi: 10.3390/nu13020425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jackson J.G., Diaz F.J., Lopez L., de Leon J. A combined analysis of worldwide studies demonstrates an association between bipolar disorder and tobacco smoking behaviors in adults. Bipolar Disord. 2015;17(6):575–597. doi: 10.1111/bdi.12319. [DOI] [PubMed] [Google Scholar]
- James E., Freund M., Booth A., Duncan M.J., Johnson N., Short C.E., Wolfenden L., Stacey F.G., Kay-Lambkin F., Vandelanotte C. Comparative efficacy of simultaneous versus sequential multiple health behavior change interventions among adults: A systematic review of randomised trials. Prev. Med. 2016;89:211–223. doi: 10.1016/j.ypmed.2016.06.012. [DOI] [PubMed] [Google Scholar]
- Jao N.C., Robinson L.D., Kelly P.J., Ciecierski C.C., Hitsman B. Unhealthy behavior clustering and mental health status in United States college students. J. Am. Coll. Health. 2019;67(8):790–800. doi: 10.1080/07448481.2018.1515744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keller-Hamilton B., Moe A.M., Breitborde N.J., Lee A., Ferketich A.K. Reasons for smoking and barriers to cessation among adults with serious mental illness: A qualitative study. J. Commun. Psychol. 2019;47(6):1462–1475. doi: 10.1002/jcop.22197. [DOI] [PubMed] [Google Scholar]
- Kelly P.J., Baker A.L., Deane F.P., Kay-lambkin F.J., Bonevski B., Tregarthen J. Prevalence of smoking and other health risk factors in people attending residential substance abuse treatment. Drug Alcohol Rev. 2012;31(5):638–644. doi: 10.1111/j.1465-3362.2012.00465.x. [DOI] [PubMed] [Google Scholar]
- Kluge H.H.P., Wickramasinghe K., Rippin H.L., Mendes R., Peters D.H., Kontsevaya A., Breda J. Prevention and control of non-communicable diseases in the COVID-19 response. The Lancet. 2020;395(10238):1678–1680. doi: 10.1016/S0140-6736(20)31067-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kwan M.Y., Arbour-Nicitopoulos K.P., Duku E., Faulkner G. Patterns of multiple health risk–behaviours in university students and their association with mental health: application of latent class analysis. Health Promot. Chronic Dis. Prev. Can. 2016;36(8):163–170. doi: 10.24095/hpcdp.36.8.03. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lanza S.T., Collins L.M., Lemmon D.R., Schafer J.L. PROC LCA: A SAS procedure for latent class analysis. Struct. Equation Modeling. 2007;14(4):671–694. doi: 10.1080/10705510701575602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lê Cook B., Wayne G.F., Kafali E.N., Liu Z., Shu C., Flores M. Trends in smoking among adults with mental illness and association between mental health treatment and smoking cessation. JAMA. 2014;311(2):172–182. doi: 10.1001/jama.2013.284985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee Y., Back J.H., Kim J., Byeon H., Kim S., Ryu M. Clustering of multiple healthy lifestyles among older Korean adults living in the community. Geriatrics Gerontol. Int. 2012;12(3):515–523. doi: 10.1111/j.1447-0594.2011.00788.x. [DOI] [PubMed] [Google Scholar]
- McAloney K., Graham H., Law C., Platt L. A scoping review of statistical approaches to the analysis of multiple health-related behaviours. Prev. Med. 2013;56(6):365–371. doi: 10.1016/j.ypmed.2013.03.002. [DOI] [PubMed] [Google Scholar]
- McElwaine K.M., Freund M., Campbell E.M., Knight J., Bowman J.A., Doherty E.L., Wye P.M., Wolfenden L., Lecathelinais C., McLachlan S., Wiggers J.H. The delivery of preventive care to clients of community health services. BMC Health Serv. Res. 2013;13(1):1–11. doi: 10.1186/1472-6963-13-167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meader N., King K., Moe-Byrne T., Wright K., Graham H., Petticrew M., Power C., White M., Sowden A.J. A systematic review on the Clustering and co-occurrence of multiple risk behaviours. BMC Public Health. 2016;16(1) doi: 10.1186/s12889-016-3373-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mental Health Commission of New South Wales, 2014. Living well: A strategic plan for mental health in NSW 2014-2024. Mental Health Commission of New South Wales.
- Metse A.P., Wiggers J., Wye P., Wolfenden L., Freund M., Clancy R., Stockings E., Terry M., Allan J., Colyvas K., Prochaska J.J., Bowman J.A. Efficacy of a universal smoking cessation intervention initiated in inpatient psychiatry and continued post-discharge: a randomised controlled trial. Aust. N. Z. J. Psychiatry. 2017;51(4):366–381. doi: 10.1177/0004867417692424. [DOI] [PubMed] [Google Scholar]
- National Health and Medical Research Council . NHMRC; 2020. Australian guidelines to reduce health risks from drinking alcohol. [Google Scholar]
- Newell S.A., Girgis A., Sanson-Fisher R.W., Savolainen N.J. The accuracy of self-reported health behaviors and risk factors relating to cancer and cardiovascular disease in the general population: a critical review. Am. J. Preventive Med. 1999;17(3):211–229. doi: 10.1016/s0749-3797(99)00069-0. [DOI] [PubMed] [Google Scholar]
- Nigg C.R., Long C.R. A systematic review of single health behavior change interventions vs. multiple health behavior change interventions among older adults. Transl. Behav. Med. 2012;2(2):163–179. doi: 10.1007/s13142-012-0130-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Noble N., Paul C., Turon H., Oldmeadow C. Which modifiable health risk behaviours are related? A systematic review of the Clustering of Smoking, Nutrition, Alcohol and Physical activity (‘SNAP’) health risk factors. Prev. Med. 2015;81:16–41. doi: 10.1016/j.ypmed.2015.07.003. [DOI] [PubMed] [Google Scholar]
- Noel H., Denny S., Farrant B., Rossen F., Teevale T., Clark T., Fortune S. Clustering of adolescent health concerns: A latent class analysis of school students in NewZealand. J. Paediatr. Child Health. 2013;49(11):935–941. doi: 10.1111/jpc.12397. [DOI] [PubMed] [Google Scholar]
- NSW Ministry of Health, 2018. NSW Strategic Framework and Workforce Plan for Mental Health 2018–2022: A Framework and Workforce Plan for NSW Health Services.
- NSW Ministry of Health, 2021. Physical Health Care for People Living with Mental Health Issues - A Guideline.
- Oftedal S., Kolt G.S., Holliday E.G., Stamatakis E., Vandelanotte C., Brown W.J., Duncan M.J. Associations of health-behavior patterns, mental health and self-rated health. Prev. Med. 2019;118:295–303. doi: 10.1016/j.ypmed.2018.11.017. [DOI] [PubMed] [Google Scholar]
- Park A.L., McDaid D., Weiser P., Von Gottberg C., Becker T., Kilian R. Examining the cost effectiveness of interventions to promote the physical health of people with mental health problems: a systematic review. BMC Public Health. 2013;13(1):1–17. doi: 10.1186/1471-2458-13-787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paul C., Tzelepis F., Bisquera A., Noble N., Wiggers J. Just how high-risk are ongoing smokers? Exploring Clusters of health risk behaviours among current and ex-smokers. Prev. Med. 2016;93:70–75. doi: 10.1016/j.ypmed.2016.09.021. [DOI] [PubMed] [Google Scholar]
- Peters, R., Ee, N., Peters, J., Beckett, N., Booth, A., Rockwood, K., & Anstey, K. J., 2019. Common risk factors for major noncommunicable disease, a systematic overview of reviews and commentary: the implied potential for targeted risk reduction. Therapeutic advances in chronic disease, doi:10.1177/2040622319880392. [DOI] [PMC free article] [PubMed]
- Pettigrew S., Dana L.M., McAleese A., Bastable A., Drane C., Sapountsis N. Brief report: a latent class analysis of guideline compliance across nine health behaviors. Int. J. Behav. Med. 2021;1–6 doi: 10.1007/s12529-021-09988-8. [DOI] [PubMed] [Google Scholar]
- Phillipou A., Meyer D., Neill E., Tan E.J., Toh W.L., Van Rheenen T.E., Rossell S.L. Eating and exercise behaviors in eating disorders and the general population during the COVID-19 pandemic in Australia: Initial results from the COLLATE project. Int. J. Eat. Disord. 2020;53(7):1158–1165. doi: 10.1002/eat.23317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prince S.A., Cardilli L., Reed J.L., Saunders T.J., Kite C., Douillette K., Buckley J.P. A comparison of self-reported and device measured sedentary behaviour in adults: a systematic review and meta-analysis. International Journal of Behavioral Nutrition and Physical Activity. 2020;17(1):1–17. doi: 10.1186/s12966-020-00938-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prochaska J.O. Multiple health behavior research represents the future of preventive medicine. Prev. Med. 2008;46(3):281–285. doi: 10.1016/j.ypmed.2008.01.015. [DOI] [PubMed] [Google Scholar]
- Ritzwoller D.P., Sukhanova A.S., Glasgow R.E., Strycker L.A., King D.K., Gaglio B., Toobert D.J. Intervention costs and cost-effectiveness for a multiple-risk-factor diabetes selfmanagement trial for Latinas: economic analysis of ¡viva Bien! Transl. Behav. Med. 2011;1(3):427–435. doi: 10.1007/s13142-011-0037-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scott D., Happell B. The high prevalence of poor physical health and unhealthy lifestyle behaviours in individuals with severe mental illness. Issues Mental Health Nursing. 2011;32(9):589–597. doi: 10.3109/01612840.2011.569846. [DOI] [PubMed] [Google Scholar]
- Shaw B.A., Agahi N. A prospective cohort study of health behavior profiles after age 50 and mortality risk. BMC Public Health. 2012;12(1):1–10. doi: 10.1186/1471-2458-12-803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spitzer S., Weber D. Reporting biases in self-assessed physical and cognitive health status of older Europeans. PLoS One. 2019;14(10) doi: 10.1371/journal.pone.0223526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spring B., Moller A.C., Coons M.J. Multiple health behaviours: overview and implications. J. Public Health. 2012;34(suppl_1):i3–i10. doi: 10.1093/pubmed/fdr111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stanton R., To Q.G., Khalesi S., Williams S.L., Alley S.J., Thwaite T.L., Fenning A.S., Vandelanotte C. Depression, anxiety and stress during COVID-19: associations with changes in physical activity, sleep, tobacco and alcohol use in Australian adults. Int. J. Environ. Res. Public Health. 2020;17(11):4065. doi: 10.3390/ijerph17114065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sweet S.N., Fortier M.S. Improving physical activity and dietary behaviours with single or multiple health behaviour interventions? A synthesis of meta-analyses and reviews. Int. J. Environ. Res. Public Health. 2010;7(4):1720–1743. doi: 10.3390/ijerph7041720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Teasdale S.B., Ward P.B., Samaras K., Firth J., Stubbs B., Tripodi E., Burrows T.L. Dietary intake of people with severe mental illness: systematic review and meta-analysis. Br. J. Psychiatry. 2019;214(5):251–259. doi: 10.1192/bjp.2019.20. [DOI] [PubMed] [Google Scholar]
- Tremain D., Freund M., Wolfenden L., Wye P., Bowman J., Dunlop A., Gillham K., Bartlem K., McElwaine K., Gow B., Wiggers J. Modifiable health risk behaviours and attitudes towards behaviour change of clients attending community-based substance use treatment services. Drug Alcohol Rev. 2017;36(3):369–377. doi: 10.1111/dar.12439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vancampfort D., Firth J., Schuch F.B., Rosenbaum S., Mugisha J., Hallgren M., Probst M., Ward P.B., Gaughran F., De Hert M., Carvalho A.F., Stubbs B. Sedentary behavior and physical activity levels in people with schizophrenia, bipolar disorder and major depressive disorder: a global systematic review and meta-analysis. World Psychiatry. 2017;16(3):308–315. doi: 10.1002/wps.20458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vermeulen-Smit E., Ten Have M., Van Laar M., De Graaf R. Clustering of health risk behaviours and the relationship with mental disorders. J. Affect. Disord. 2015;171:111–119. doi: 10.1016/j.jad.2014.09.031. [DOI] [PubMed] [Google Scholar]
- Walker E.R., McGee R.E., Druss B.G. Mortality in mental disorders and global disease burden implications: a systematic review and meta-analysis. J. Am. Med. Assoc. Psychiatry. 2015;72(4):334–341. doi: 10.1001/jamapsychiatry.2014.2502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weinberger A.H., Funk A.P., Goodwin R.D. A review of epidemiologic research on smoking behavior among persons with alcohol and illicit substance use disorders. Prev. Med. 2016;92:148–159. doi: 10.1016/j.ypmed.2016.05.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weinberger A.H., Platt J., Esan H., Galea S., Erlich D., Goodwin R.D. Cigarette smoking is associated with increased risk of substance use disorder relapse: a nationally representative, prospective longitudinal investigation. J. Clin. Psychiatry. 2017;78(02) doi: 10.4088/JCP.15m10062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Westcott W.L. Resistance training is medicine: effects of strength training on health. Curr. Sports Med. Rep. 2012;11(4):209–216. doi: 10.1249/JSR.0b013e31825dabb8. [DOI] [PubMed] [Google Scholar]
- Whitaker V., Oldham M., Boyd J., Fairbrother H., Curtis P., Meier P., Holmes J. Clustering of health-related behaviours within children aged 11–16: a systematic review. BMC Public Health. 2021;21(1):1–12. doi: 10.1186/s12889-020-10140-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization, 2000. Obesity: preventing and managing the global epidemic. Report of a WHO consultation. WHO technical report series 894. Geneva. [PubMed]
- World Health Organization, 2021. Comprehensive mental health action plan 2013–2030. Geneva: World Health Organization.
- Ye Y.L., Wang P.G., Qu G.C., Yuan S., Phongsavan P., He Q.Q. Associations between multiple health risk behaviors and mental health among Chinese college students. Psychol., Health Med. 2016;21(3):377–385. doi: 10.1080/13548506.2015.1070955. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.