Abstract
Squamous cell carcinoma of oral cavity has a high prevalence in our region. Upper alveolar cancers are uncommon but present with locally advanced disease extending to infra temporal fossa. The outcome of treatment in these tumors is poor. Surgery followed by adjuvant therapy is the mainstay of treatment. We are presenting a retrospective analysis of outcome of treatment in 20 patients with locally advanced (T4b) upper alveolar carcinoma treated by infra-structure maxillectomy with compartment resection of infra-temporal fossa and neck dissection followed by adjuvant radiotherapy or radiotherapy with chemotherapy. Study period was from 2013 to 2018. Minimum follow up was 12 months and mean follow up 30 months. 12 patients are alive and disease free, 6 patients had local recurrence and 2 patients had regional recurrence with one having pulmonary metastasis. We observed that positive or close margins (< 5 mm after formalin fixation) predisposed to early recurrence. Erosion of pterygoid plates was a poor prognostic factor. Cervical lymph node metastasis occurred late in disease, but carried poor prognosis. Compartment resection of infra temporal fossa gave better outcome compared to other studies which reported outcome of treatment in upper alveolar cancers.
Keywords: Squamous cell carcinoma, Upper alveolus, Infra-temporal fossa, Resection margins, Local recurrence, Infra-structure maxillectomy, Compartment resection
Introduction
Head and neck cancer is the sixth most prevalent cancer across the globe. However, in our country, head and neck malignancies account for 30% of all malignancies. 50% of the head and neck cancers in our region are oral cancers particularly among women [1]. Among them, upper alveolar cancers are relatively uncommon. Majority of these patients present with locally advanced disease extending to infra-temporal fossa. Surgery which is the treatment of choice is challenging in such patients, when the mandible and orbital floor are preserved. This is due to limited exposure and access, vascularity and spread along the muscles of mastication. Inadequate margins of resection predispose to early recurrence [2–6]. Infra temporal fossa was considered inoperable until recently and very few surgeons venture into this area even now. Compartment resection of masticator muscles in patients with infra-temporal fossa disease has improved the oncological outcome in such patients. [7–9] We are presenting the outcome in 20 cases of locally advanced upper alveolar squamous cell carcinoma extending to infra-temporal fossa, who underwent infra-structure maxillectomy with compartment resection of infra-temporal fossa and supra-omohyoid neck dissection followed by adjuvant treatment in our hospital—tertiary care hospital in rural area, between 2013 and 2018. All patients in our series had minimum follow up of 1 year.
Objectives
To document the outcome of surgery in locally advanced squamous cell carcinoma of upper alveolus extending to infra-temporal fossa.
To correlate the outcome with margins of resection in infra-temporal fossa.
Methodology
This study involved retrospective analysis of case sheets and histopathology reports of 20 patients diagnosed and treated for locally advanced upper alveolar carcinoma extending to infra-temporal fossa from June 2013 to July 2018 in our institution. All these patients were staged T4b due to involvement of infra-temporal fossa (Figs. 1, 2). All patients underwent infrastructure maxillectomy with coronoidectomy and compartment resection of infra-temporal fossa along with a supra-omohyoid neck dissection (Fig. 3) and reconstruction. Three of these patients underwent marginal mandibulectomy and two patients underwent segmental mandibulectomy to have adequate access for disease clearance. All patients underwent postoperative adjuvant treatment in form of radiotherapy or chemotherapy with radiotherapy. Post-operative chemotherapy with radiotherapy was given to those patients who had positive or close margins or extra-nodal spread from metastatic lymph node or multiple metastatic lymph nodes. The mean follow up period was 30 months and minimum follow up was 12 months. The medical case records were analysed for depth of invasion, bone erosion, lymph node metastasis, margins of resection particularly in infra-temporal fossa, loco-regional control and disease free survival. Documentation of all adverse factors on histopathological examination of the resected specimen was done in patients who had recurrence in order to implicate the histopathological factors that predispose to recurrence.
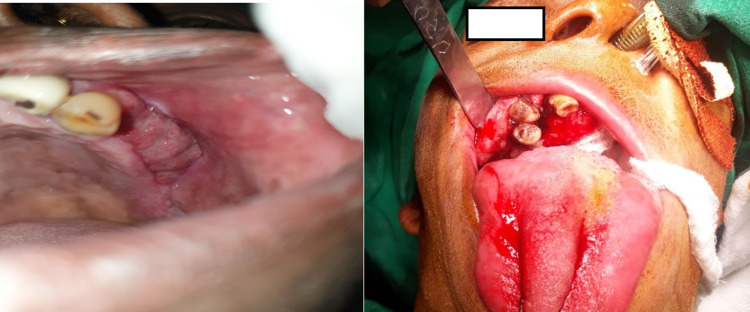
Fig. 1.
Pre-operative photographs showing primary tumour in 2 different patients
Fig. 2.
Pre-operative CT scans showing erosion of upper alveolus and extension to infra-temporal fossa in 2 different patients
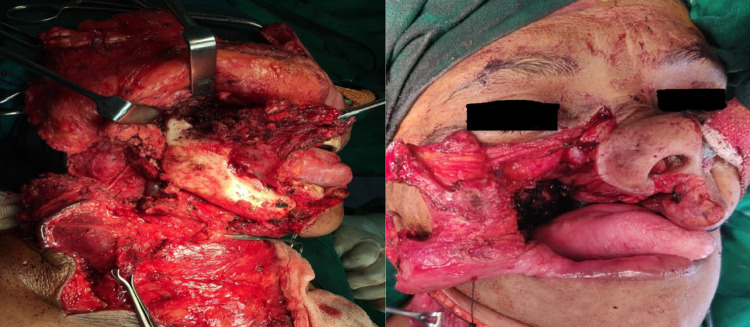
Fig. 3.
Infra structure maxillectomy with coronoidectomy and compartment resection of infra-temporal fossa, preserving mandible and orbital floor in 2 different patients
Results
In our series of 20 patients 16 were females and 4 males. The most common age group in our study was 60–70 years. All patients were found to have invasive squamous carcinoma extending to muscles of mastication in infratemporal fossa on imaging and histopathological examination. In all patients depth of invasion was more than 5 mm. In 2 patients depth of invasion was 10 mm and tumor was eroding the pterygoid plates. The margins of resection were clear (> 5 mm after formalin fixation) in 12 patients. However the superior margin was positive in one patient and there were dysplastic changes in the superior margin in two patients. The posterior margin of resection was positive in two patients. Superior margin was close (< 5 mm) in 2 patients. All patients were found have bone erosion in upper alveolus on histopathology. 3 patients were found to have metastatic lymph nodes in submandibular region. 2 of them had 2 metastatic nodes each and 1patient had a single metastatic lymph node. None of them had extra-nodal spread.
In our series of 20 patients 12 patients are alive and disease free after a mean follow up of 30 months and a minimum follow up of 12 months. 6 patients had local recurrence. Among them, 2 patients who recurred 4 months after treatment, died due to disease. 2 patients are receiving palliative chemotherapy and 1 patient defaulted after recurrence. 4 recurrences documented above were between 10 and 14 months after completion of treatment. Among them, 1 patient died due to local recurrence. 1 patient died due to lymph node and pulmonary metastasis. 1 patient died due to cerebro-vascular accident (Fig. 4).
Fig. 4.

Survival curve. All deaths occurred within 20 months of follow up but the median survival time was 19 months
Among the 6 patients who recurred locally, 5 patients had close margins i.e. less than 5 mm following formalin fixation and 1 patient who had early recurrence had positive superior margin in infra-temporal fossa and pterygoid plate erosion with depth of invasion > 10 mm. Among patients with close margins, 2 had dysplastic changes at superior margin of resection. All these 5 patients with close margins also had depth of invasion varying between 8 and 10 mm and 1 patient had pterygoid plate erosion. Only 2 patients among these recurrences had metastatic lymph nodes at level I and were staged pT4bN2bM0 (Table 1).
Table 1.
Local recurrences (n = 6)
| Time of recurrence after treatment | Clinical Staging at presentation | Margins of resection | Lymph node metastasis on histopathology (Level Ib) |
|---|---|---|---|
| 10 months | T4aN1M0 | Close posterior margin (2 mm) | Present |
| 14 months | T4aN1M0 | Close superior margin (4 mm) | Present |
| 6 months | T4aN0M0 | Close superior margin (2 mm) | Absent |
| 14 months | T4aN0M0 | Close superior margin (dysplastic) | Absent |
| 15 months | T4aN1M0 | Close superior margin (4 mm) | Absent |
| 4 months | T4aN0M0 | Positive superior margin | Absent |
In our series among the 4 patients with lymph node metastasis, 2 patients recurred. Among 3 patients who had pterygoid plate involvement on histopathology, 2 recurred (Table 2-survival statistics).
Table 2.
Survival statistics
| Time | Status | Cumulative proportion surviving at the time | N of cumulative events | N of remaining cases | ||
|---|---|---|---|---|---|---|
| Estimate | Std. error | |||||
| 1 | 4.000 | 1.00 | .944 | .054 | 1 | 17 |
| 2 | 6.000 | 1.00 | .889 | .074 | 2 | 16 |
| 3 | 10.000 | 1.00 | .833 | .088 | 3 | 15 |
| 4 | 11.000 | .00 | – | – | 3 | 14 |
| 5 | 12.000 | .00 | – | – | 3 | 13 |
| 6 | 14.000 | 1.00 | – | – | 4 | 12 |
| 7 | 14.000 | 1.00 | .705 | .112 | 5 | 11 |
| 8 | 14.000 | .00 | – | – | 5 | 10 |
| 9 | 18.000 | .00 | – | – | 5 | 9 |
| 10 | 20.000 | 1.00 | .627 | .124 | 6 | 8 |
| 11 | 20.000 | .00 | – | – | 6 | 7 |
| 12 | 22.000 | .00 | – | – | 6 | 6 |
| 13 | 26.000 | .00 | – | – | 6 | 5 |
| 14 | 28.000 | .00 | – | – | 6 | 4 |
| 15 | 36.000 | .00 | – | – | 6 | 3 |
| 16 | 40.000 | .00 | – | – | 6 | 2 |
| 17 | 60.000 | .00 | – | – | 6 | 1 |
| 18 | 60.000 | .00 | – | – | 6 | 0 |
| Meana | Median | ||||||
|---|---|---|---|---|---|---|---|
| Estimate | Std. error | 95% CI | Estimate | Std. error | 95% CI | ||
| Lower bound | Upper bound | Lower bound | Upper bound | ||||
| Means and medians for survival time | |||||||
| 42.080 | 5.893 | 30.529 | 53.631 | – | – | – | – |
aEstimation is limited to the largest survival time if it is censored
Mean survival time 42.08 Months with 95% confidence interval (30.529–53.631)
Discussion
Oral cancer has a high prevalence in our region (about 15% of all cancers), particularly among women [1]. This is due to the addiction to tobacco quid among women in this region. Upper alveolar cancers are relatively rare, accounting for 7% of oral cancers in our institution. Similar incidence has been observed in other studies [2–4]. However, majority of these patients (77%) presented with locally advanced disease extending to muscles of mastication in infra temporal fossa and were staged T4b. This could be due to lack of awareness and poor socio economic condition in this region. Other studies in Asia have also observed that upper alveolar squamous cell carcinoma is aggressive disease and a large proportion of patients present with locally advanced tumour [3–5].
Locally advanced disease extending to infra temporal fossa was considered inoperable till the last decade. This was due to difficult access, troublesome bleeding and positive margins in muscles of mastication. Compartment resection facilitates resection of muscles of mastication en-bloc [8–10]. In our series only patients with disease till the lateral pterygoid (on imaging) underwent compartment resection. 3 patients were found to have erosion of pterygoid plate and 2 patients among them recurred. Other studies have also observed that involvement of infra-temporal fossa above lateral pterygoid muscle carries poor prognosis [2, 3, 9]. In our study positive or close margins of resection carried poor prognosis [5, 6]. Out of 7 patients who had margins < 5 mm after formalin fixation, 5 had local recurrence. In our series, only superior or posterior margins were found to be close. Patients in our study were staged T4b only because they had erosion of upper alveolus and disease extending to muscles of mastication in infra- temporal fossa. However, patients who had disease extending above lateral pterygoid muscle on imaging were excluded from the study. Following compartment resection of infra-temporal fossa, we observed loco regional control in 60% of patients. Patients with pterygoid plate erosion on histopathology recurred early. Other local recurrences were observed within 18 months after completion of treatment. Other studies have observed 5 year survival varying between 20 and 49% in upper alveolar malignancies [2–6]. The better loco- regional control in our series (60%) could be due to the fact that majority of patients had disease below the lateral pterygoid muscle and all patients underwent compartment resection of infra-temporal fossa. All these patients had well differentiated squamous carcinoma. Aggressive resection of the tumor along with entire compartment of muscles of mastication may result in better loco-regional control. Other studies have also observed better control with surgery having adequate margins followed by adjuvant treatment. [3–5, 11] In our series lymph node metastasis was seen only in 15% of patients. This was in contrast with observations made by other authors where cervical lymph node metastasis was found to be higher [3–5, 11]. This could be because patients in our series had well differentiated carcinoma and had higher stage of disease owing to involvement of muscles of mastication though the tumor volume was less. However, patients having cervical lymph node metastasis in our series had early recurrence.
Conclusion
Upper alveolar tumors are uncommon and usually present with advanced disease due to extension into infra-temporal fossa. Anteriorly placed tumors have a better prognosis than posteriorly situated tumors. Other factors which are associated with poor prognosis are positive margins and lymph node metastasis. Adequate margins of resection of primary tumor along with compartment resection of muscles of mastication improves loco-regional control.
Acknowledgements
We acknowledge the contribution of Dr. Manjunath G.N., Professor in Radiation Oncology, Sri Devaraj Urs Medical College, Kolar, India for his contribution in Adjuvant treatment of all the subjects included in this study.
Funding
There was no funding by any organisation or source for this study.
Compliance with Ethical Standards
Conflict of interest
There is no conflict of interest among the authors.
Ethical Approval
Institutional ethical committee clearance (SDUMC/KLR/IEC/85/2018-2019) was obtained for this study.
Human and Animal Rights
No animal or human experiments were done for this study.
Informed Consent
Consent for being included in this retrospective study without revealing the identity of the patient has been obtained from all study subjects.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
H. S. Brindha, Email: hsbrindha@gmail.com
S. M. Azeem Mohiyuddin, Email: azeem_hn@yahoo.co.in.
A. Sagayaraj, Email: sagayarj79@gmail.com
Kouser Mohammadi, Email: zamahmed1999@yahoo.com.
R. Kalyani, Email: drkalyanir@rediffmail.com
N. Harshitha, Email: twinkle.harshitha@gmail.com
D. Aishwarya Raj Pillai, Email: ash.raj21@gmail.com.
Ravishankar Suryanarayana, Email: suryasankya@gmail.com.
References
- 1.Kalyani R, Das S, Bindra MS, Kumar H. Cancer profile in Kolar: a ten year study. Indian J Cancer. 2010;47:160–165. doi: 10.4103/0019-509X.63011. [DOI] [PubMed] [Google Scholar]
- 2.Morris LG, Patel SG, Shah JP, Ganly I. High rates of regional failure in squamous cell Carcinoma of the hard palate and maxillary alveolus. Head Neck. 2011;33(6):824–830. doi: 10.1002/hed.21547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Pathak KA, Mathur N, Talole S, Deshpande MS, Chaturvedi P, Pai PS, et al. Squamous cell carcinoma of the superior gingival–buccal complex. Oral Oncol. 2007;43:774–779. doi: 10.1016/j.oraloncology.2006.09.009. [DOI] [PubMed] [Google Scholar]
- 4.Baishya N, Rahman T, Das AK, Kalita CR, Sharma JD, Krishnatreya M, et al. Squamous cell carcinoma of upper alveolus: an experience of a tertiary care centre of Northeast India. South Asian J Cancer. 2019;8:44–46. doi: 10.4103/sajc.sajc_66_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Vijay K, Sindhu VA, Shivaprakash R, Jaswant J, Japipalreddy RP, Naseem A, et al. Cancers of upper gingivobuccal sulcus, hard palate and maxilla: a tertiary care centre study in North India. Natl J of Maxillofac Surg. 2013;4:202–205. doi: 10.4103/0975-5950.127652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wang TC, Hua CH, Lin CC, Tsou YA, Tseng HC, Tsai MH. Risk factors affect the survival outcome of hard palatal and maxillary alveolus squamous cell carcinoma: 10-year review in a tertiary referral center. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2010;110:11–17. doi: 10.1016/j.tripleo.2009.11.035. [DOI] [PubMed] [Google Scholar]
- 7.Trivedi NP, Kekatpure V, Kuriakose MA. Radical (compartment) resection for advanced buccal cancer involving masticator space (T4b): our experience in thirty patients. Clinic Otolaryngol. 2012;37:470–496. doi: 10.1111/coa.12018. [DOI] [PubMed] [Google Scholar]
- 8.Liao CT, Chang JT, Wang HM, et al. Surgical outcome of T4a and resected T4b oral cavity cancer. Cancer. 2006;107:337–344. doi: 10.1002/cncr.21984. [DOI] [PubMed] [Google Scholar]
- 9.Mohiyuddin SMA, Pooja H, Shreeharsha M, Sumanth KR, Suresh TN, Manjunath GN, Sagayaraj A, et al. Outcome of compartment: a tertiary rural hospital experience. Eur Arch Otorhinolaryngol. 2018;275:2843–2850. doi: 10.1007/s00405-018-5124-z. [DOI] [PubMed] [Google Scholar]
- 10.Ota Y. Infratemporal surgery for oral cancer invaded to masticator space. Int J Oral Maxillofac Surg. 2017;46:372–373. doi: 10.1016/j.ijom.2017.02.1253. [DOI] [Google Scholar]
- 11.Lin HW, Bhattacharyya N. Survival impact of nodal disease in hard palate and maxillary alveolus cancer. Laryngoscope. 2009;119:312–315. doi: 10.1002/lary.20054. [DOI] [PubMed] [Google Scholar]