Abstract
Background
The COVID-19 pandemic presented challenges for simulation programs including American College of Surgeons Accredited Education Institutes and American Society of Anesthesiologists Simulation Education Network. American College of Surgeons Accredited Education Institutes and American Society of Anesthesiologists Simulation Education Network leadership were surveyed to identify opportunities to enhance patient safety through simulation.
Methods
Between January and June 2021, surveys consisting of 3 targeted domains: (I) Changing practice; (II) Contributions and recognition; and (III) Moving ahead were distributed to 100 American College of Surgeons Accredited Education Institutes and 54 American Society of Anesthesiologists Simulation Education Network centers. Responses were combined and percent frequencies reported.
Results
Ninety-six respondents, representing 51 (51%) American College of Surgeons Accredited Education Institutes, 17 (31.5%) American Society of Anesthesiologists Simulation Education Network, and 28 dually accredited centers, completed the survey. Change of practice. Although 20.3% of centers stayed fully operational at the COVID-19 onset, 82% of all centers closed: 32% were closed less than 3 months, 28% were closed 3 to 6 months, 8% were closed 7 to 9 months, and 32% remained closed as of June 6, 2021. Most impacted activities were large-group instruction and team training. Sixty-nine percent of programs converted in-person to virtual programs. Contributions. The top reported innovative contributions included policies (80%), curricula (80%), and scholarly work (74%), Moving ahead. The respondents’ top concerns were returning to high-quality training to best address learners’ deficiencies and re-engagement of re-directed training programs. When asked “How the American College of Surgeons/American Society of Anesthesiologists Programs could best assist your simulation center goals?” the top responses were “facilitate collaboration” and “publish best practices from this work.”
Conclusion
The Pandemic presented multiple challenges and opportunities for simulation centers. Opportunities included collaboration between American College of Surgeons Accredited Education Institutes and the American Society of Anesthesiologists Simulation Education Network to identify best practices and resources needed to enhance patient safety through simulation.
Introduction
As the COVID-19 (or SARS-CoV-2) outbreak rapidly became a worldwide pandemic, the health care teams around the country mobilized to plan and act to best serve our patients and the health care system. Health care workers, particularly physicians in the acute care fields of anesthesiology, critical care medicine, and surgical critical care were particularly involved deploying to care for the surgery of severely ill patients. Many leaders in simulation-based education are also physicians in those fields. COVID-19 caused a shift in health care and resulted in significant changes in allocation of resources to COVID-19 patient care.1 , 2 Nonurgent, noncancer related procedures were stopped to reallocate personnel and resources to face the COVID-19 emergency. Medically necessary, time sensitive scoring system described by Prachand et al was endorsed by the American College of Surgeons (ACS) to triage and determine elective surgery urgency during the pandemic.3 Outpatient and emergency surgery visits were dramatically reduced. The deployment of large numbers of attending and resident physicians to COVID units and the considerable increase in inpatient volume led to significant decreases in educational opportunities. This caused a decrease in all simulation-based educational programs including procedural and nontechnical skills training. In addition, because of the highly contagious nature of COVID-19 and the severely limited supplies of personal protective equipment (PPE), decisions were made to limit the treatment team members to necessary personnel only, further significantly disrupting training programs and educational opportunities—for surgeons4 and anesthesiologists, alike.5
Surgical and anesthesiology trainees have been uniquely impacted. The need to limit use of PPE and spread of infection led to cancellation of in-person educational didactics and conferences, limited hands-on surgical training, and restriction of personnel in patient rooms. These restrictions hindered the development of trainee, patient, and family communications. Additional educational strain was experienced by COVID-19 infected residents experiencing health issues as well as long absences from the hospital.
Epicenters for surgical and anesthesiology education are the American College of Surgeons Accredited Education Institutes (ACS AEIs) and American Society of Anesthesiologists Simulation Education Network (ASA SEN) centers. An early response to the extraordinary, unprecedented demands for additional health care personnel because of the COVID-19 pandemic was cessation of educational activities. As the leadership of most of these centers are also physician leaders, they were deployed to care for COVID-19 patients. The simulation centers faced a significant challenge, and initially many paused their educational efforts. Generally, these centers were not equipped with a medical education disaster plan and the response of centers was improvisational and reactive.
The COVID-19 pandemic presented opportunities and challenges for ACS AEIs and ASA SEN simulation centers. In a collaborative effort to identify and mitigate challenges faced by the simulation centers that support these training programs, a multi-professional team of the leadership of both associations, surgeon and anesthesiologist directors of simulation centers, researchers, educators, and critical administrators created and disseminated a survey to identify where to best focus efforts to support our mission: to enhance patient safety through simulation education.
Methods
Survey dissemination
A ‘Simulation Centers Contributions and Lessons Learned During the SARS-CoV-2’ web-based survey was initially developed in the Fall of 2020 by the ACS AEI Surgical Summit program committee and the ACS Division of Education and reviewed for appropriateness by ASA leadership team. The 20-item survey consisted of three primary domains: (I) Changes in Practice–7 pull-down, checkbox and fill-in-the-blank items used to evaluate the short-term impact of the COVID-19 pandemic on simulation centers’ operations; (II) Contributions and Recognition–6 checkbox and fill-in-the-blank items used to identify different innovation and contributions that may be employed by AEI and SEN centers; and (III) Moving Ahead–4 fill-in the blank items used to identify concerns, ACS and ASA areas of needed support. The survey was disseminated to the directors of 100 ACS AEI centers in Winter of 2020 and Spring of 2021. A parallel survey was also sent to ASA SEN directors, faculty, educators, researchers, and administrators of the 55 SEN centers the Spring of 2021.
Data analysis
Data were collected and combined, and following the deletion of incomplete responses, frequency counts of pull-down and checkbox responses were tallied by AEI researcher-author (D.M.R.). The same author, who was familiar with data and experienced in traditional thematic analysis approaches,6 reviewed the fill-in-the-blank responses, and coded and categorized themes, noting differences in responses across AEI and SEN centers. The SEN administrator-author (S.H.), also familiar with the data and the thematic analysis method performed, independently tallied counts and reviewed themes for agreement across AEIs and SENs. No discrepancies were identified. Analyses were performed using traditional inductive reasoning methods with no supplemental analyses by thematic/text analyzer tools.
Results
A total of 96 respondents completed the survey. The sample represented 51 AEIs including 10 international AEIs from 6 countries, 17 SENs, and 28 centers who reported dual accreditation/endorsement. This sample represented a total of 79 AEI (79.0% of all 100 AEIs) and 45 (83.3% of all 54 SEN) simulation centers.
Domain I: Change of practice
COVID-19 pandemic’s impact on simulation center closures
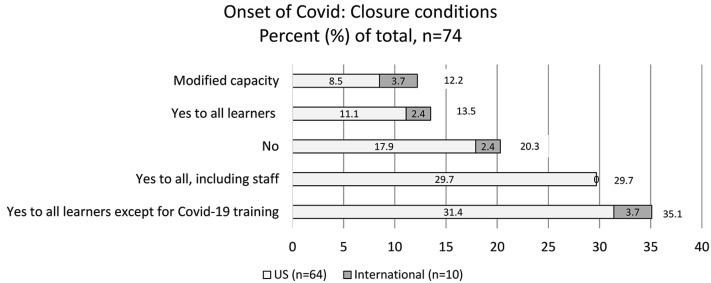
When asked about the conditions of centers’ closing, 15 of the 64 US (23.4%) and 2 of the 10 (20.0%) international centers did not close, while the remainder closed with varying degrees (Figure 1 ).
Figure 1.
Summary of all simulation centers’ initial degrees of closure reported by percent (%) response frequencies (Question: Did you center close at onset of COVID-19?), n = 74.
Of those that closed, 29.7% were fully closed to everyone, including staff, whereas 35.1% were closed to all learners not engaged in COVID-19 training programs. More than 20% of centers remained open, and of these, approximately 12% stayed open with modified capacity (eg, reduced group sizes, conversion to independent and virtual training). The remaining nearly 8% stayed open for the purpose of facilitating various aspects of institutional pandemic preparation. Although responses from the 10 international centers paralleled those from US centers for most closure conditions, none reported fully closing during the COVID-19 pandemic.
Simulation centers’ ability to fully reopen after the COVID-19 pandemic onset
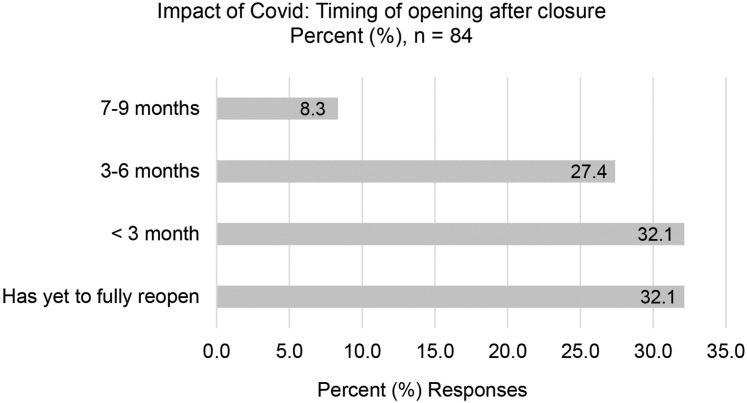
When asked about the timing of centers’ full reopening following their initial closure owing to the COVID-19 pandemic, 27 of 84 (32.1%) fully opened within 3 months (Figure 2 ).
Figure 2.
Summary of all simulation centers’ reopening times, reported by percent (%) response frequencies (Question: How soon after closure did your center fully re-open?), n = 84.
Approximately 32% centers remained closed, 11 months after initiation of closure owing to the COVID-19 pandemic.
COVID-19 Pandemic’s impact to simulation centers’ activities
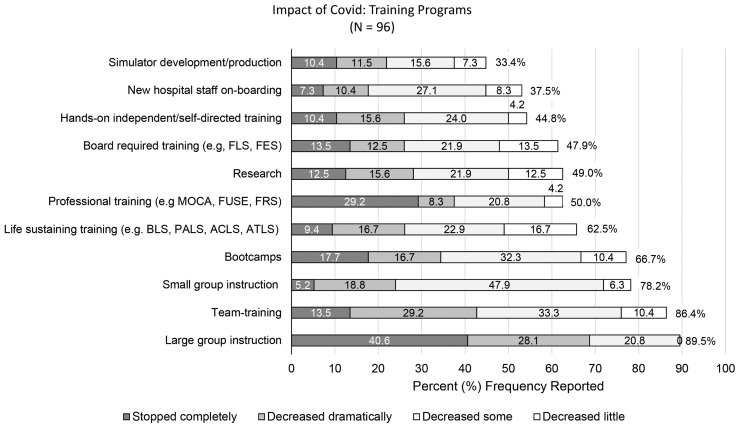
When asked about the greatest impact of the COVID-19 pandemic on simulation centers’ activities the most impacted activity was large-group instruction with 89.5% respondents reporting negative impact, and 40.6% of those programs “stopped completely” (Figure 3 ).
Figure 3.
Summary of all simulation centers’ activities impacted, and their degree of impact reported by percent (%) response frequencies (Question: How has COVID-19 impacted your Sim Center activities?), n = 96.
Other programs that were highly negatively impacted were team training (86.4%), small group instruction (78.2%), and bootcamps (66.7%). Professional training (eg, maintenance of certification, Fundamental Use of Surgical Energy, Fundamentals of Robotic Surgery) was associated with 50% of respondents reporting negative impact, with 29.2% reporting those programs as “stopped completely.”
Domain II: Contributions
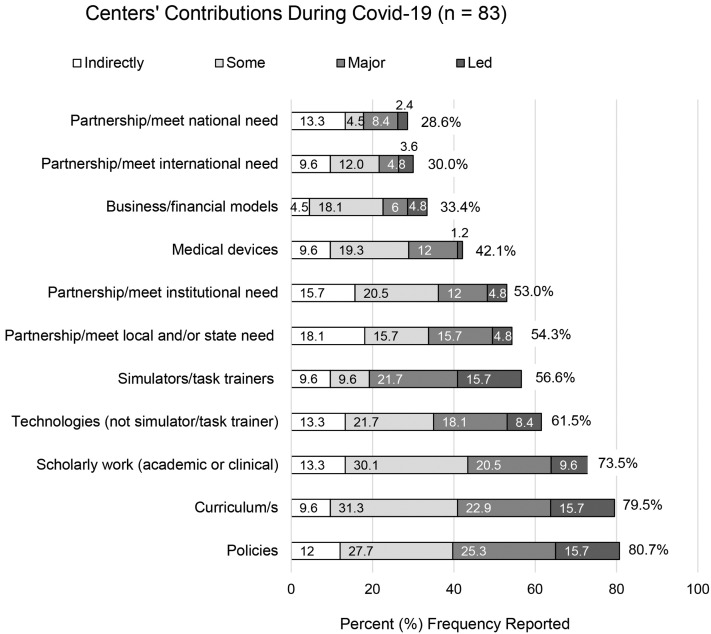
Fifty-four (65%) respondents reported innovative contributions, including policies (80.7%), curricula (79.5%), scholarly work (73.5%), technologies (61.5%), and simulators (56.6%) (Figure 4 ).
Figure 4.
Summary of all centers’ contributions during COVID-19 and degree of involvement by type of contribution, n = 83. AEI, accredited education institutes; SEN, simulation education networks.
Contributions that were most reported being led by simulation centers included policies, curricula, and simulators/task trainers (each 15.7%).
Domain III: Moving ahead
Simulation center directors’ concerns
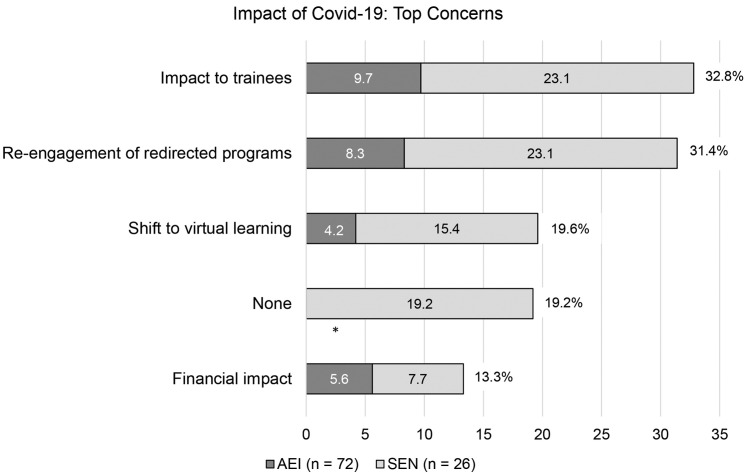
The respondents’ general concerns seemed to target the return to high-quality training to best address learners’ deficiencies. The top reported concerns are listed in decreasing order;
-
1.
Impact on trainees (32.8% of all respondents), with comments that included “Our resident's skill level is a concern we have owing to the fact they have not been able to come into the center for independent practice,” “We are most concerned about the loss of skills among employees,” and “Med students and residents with little sim training and fewer clinical encounters.” (Figure 5 ).
Figure 5.
Summary of all centers’ concerns during COVID-19 by center type. AEI, accredited education institutes; SEN, simulation education networks.
∗No relevant responses from ACS center respondants
-
2.
Re-engagement of redirected training programs was second highest concern (31.4%). Example comments associated with the re-engagement of redirected programs included “Learner groups adapted to different training modalities or got used to limited numbers in our center—we're actively working on re-engagement,” and “My concerns are that some education will not return to the simulation lab. Instructors have changed their education so that it does not include using the simulation lab because we can not gather in large groups.”
-
3.
Shift to virtual learning was third highest concern (19.6%). Associated resonses were varied in tone, and reflected mixed opinions. Sample responses varied, and included “Concerns about having the bandwidth to continue the virtual teaching along with simulations,” “The development of virtual simulation has enabled us to continue state-wide training in maternal health,” and “People have gotten use to virtual and there are both pros and cons to virtual activities.”
-
4.
No concerns was fourth highest noted category of commented ‘concerns’ (19.2%). Notably, the relevant comments were neutral-positive in tone, from SEN center respondants, and highlighted opportunities for improvements. Examples included “None” (x5), “I think COVID will and has changed the way we book programs and think out of the box to make some more Zoom-friendly/remote-friendly,” and “We have actually seen some benefit from the need to reduce occupancy in that learners receive more one on one feedback and instruction.”
-
5.
Financial impact was fifth noted concern identified by respondants (13.3%), with example comments that included “Loss of revenue due to reduction in external clients,” “Decreased support for the sim center,” and “Potential financial repercussions to try and balance a large institutional deficit.”
Addressing Concerns
When asked “How are you planning to address these concerns?” the top 3 common responses were “Restructure/Reorganize” (21.0), “Try harder/Make it work” (16.7%), and “Engage leadership/stakeholders” (16.0%) (Table I ).
Table I.
Summary of themes emerging from responses to question “How are you planning to address these concerns?” Organized by simulation center type
| Action | Total percent (%) response | AEI (n = 70) percent (%) response | SEN (n = 27) percent (%) response |
|---|---|---|---|
| Restructure/Reorganization | 21.0 | 17.1 | 3.9 |
| Innovate/Expand services | 17.2 | 17.2 | – |
| Try harder/Make it work | 16.7 | 5.7 | 11.1 |
| Engage leadership/Stakeholders | 16.0 | 8.6 | 7.4 |
| Strategic planning | 14.8 | 7.1 | 7.7 |
| Maintain/Ensure safety protocols | 14.8 | – | 14.8 |
| Pending regulations/Policy/Guidance | 11.1 | – | 11.1 |
| Unsure | 10.5 | 2.8 | 7.7 |
| Improve VR offerings | 7.2 | 7.2 | – |
| Increase marketing | 5.7 | 5.7 | – |
AEI, accredited education institutes; SEN, simulation education networks; VR,virtual reality.
Some themes varied across and AEI and SEN respondants. For AEI respondants, the top responses were in decreasing order: “Innovate/expand services” (17.2%), “Improve virtual reality offerings” (7.2%), and “Increase marketing” (5.7%); whereas the top responses for SEN respondants’ were “Maintain safety protocols” (14.8%) and “Wait for regulations/ policies/guidelines” (11.1%).
When asked how ACS and ASA can help address these concerns, the responses were consistant across AEIs and SEN centers, with 3 primary themes, including; “Facilitate collaboration” (36.8%), “Publish best practices from this work” (32.3%), and “Provide support” (29.5%).
Discussion
We performed a survey of ACS AEI and SEN centers to assess the effects of the COVID-19 pandemic to gain an understanding of the landscape of experiences for both surgery and anesthesiology simulation training centers. This was done to identify the common challenges and opportunities to share best practices that may reliably support our mission: to enhance patient safety through simulation.
Findings from this work can be used to highlight the impact of the pandemic on simulation center closures. Although the survey disseminated did not capture specific rationale behind centers’ decisions to close, the work does provide general information on general patterns of closure, and how these closures impacted simulation centers’ training programs. A large majority of centers closed initially and therefore, severely limited the effectiveness of education. A third of the centers were closed completely, whereas another third reported remaining open to COVID-19 pandemic-related training. Importantly, almost a year after the onset of the pandemic another third of centers were fully open at 3 months, which demonstrated AEI and SEN flexibility and responsiveness to their institution’s needs.
This work also highlighted the contributions that AEIs and SENs have made during the COVID-19 pandemic. With 54 (65%) respondents reported innovative contributions, these range from new safety policies to novel curricula, and scholarly work to technologies and simulators.6 , 7
Responses captured from this survey also highlighted concerns from both surgical and anesthesiology training centers. The primary common concern targeted the pandemic’s impact on trainees, especially regarding the return to high-quality training, and the re-engagement of redirected training programs. Additionally, with the global shift to virtual and web-based training, respondents’ concerns ranged practical logistics (eg, creation and implementation of virtual training programs) to the potential long-term impact on training quality and center sustainability. Most importantly, findings from this joint work highlighted the opportunity to address the concerns and challenges reported by respondents from simulation centers that support both surgeon and anesthesiologist trainees. Identification of common solution is a powerful initial step for ASC and ASA to collaboratively work together to support AEI and SEN centers as they address theses challenges by restructuring/reorganizing, engaging leadership at their own institutions, and creating strategic plans.
There were limitations of this work to consider. First, although there was a high participating sample that represented 79.8% of AEIs and 83.3% of SEN centers, the responses may not have been representative of the nonparticipating centers, and any inferences made should not be generalized to all AEI and SEN centers. Additionally, differences in survey distribution that targeted ACS AEI and ASA SEN directors and a broader distribution ASA SEN faculty-educators and staff, may not fully represent the responses of surgical faculty-educators and staff, and surely does not reflect opinions of surgery or anesthesiology trainees, who may have different concerns regarding the impact of COVID-19 on training experience, which could be evaluated later. Additionally, the subgroup samples were small (eg, international centers, n = 10), limiting our ability to perform subgroup analyses. On this point, no international centers reported initial closures. We cannot fully ascertain if there were truly no closures, or the question was not interpreted as intended, which may have impacted the accuracy of these responses. Finally, the data review consisted of qualitative content analysis with thematic categorization, performed by a single educator-researcher (D.M.R.) with secondary review by an administrator (S.H.). An additional reviewer may have better ensured consensus and improved accuracy and reliability of thematic categorization.
In spite of these limitations, this joint work highlights the critical value ACS AEI and ASA SEN simulation centers have on surgery and anesthesiology training programs especially in light of the significant negative impact COVID-19 pandemic has had on the well-being of residents and educational experiences.8 In examples from around the world, surgical trainee redeployment to roles outside of their training programs, and decreased elective surgery and outpatient activities, have resulted in reduced operative training opportunities.9, 10, 11 These unfortunate consequences of the pandemic offer opportunities for learning and behavioral change. In the remarkably short span of 6 months, the world changed radically. The COVID-19 pandemic has irrevocably opened opportunities for working remotely via electronic platforms including telemedicine, a greater ability to work from home, to hold even large meetings electronically, the expansion of virtual methods for training surgeons, and virtual site visits for programs needing ACS accreditation or re-accreditation. Amid stress, loss, and grief, there are also many future opportunities that the ACS and ASA are now striving to bring to fruition.
In conclusion, the pandemic presented opportunities and challenges for ACS and ASA simulation centers. Gaps in training for surgical and anesthesia providers resulted in skill decay. An established common goal is to identify best practices and resources to ensure reliable simulation-based education and training of surgeon, anesthesia service provider and other learners to provide high quality, safe patient care.
Funding/Support
This research did not receive any specific funding from any agencies in the public, commercial, or not-for-profit areas.
Conflict of interest/Disclosures
Deborah Rooney is founding partner of Arbor Simulation, LLC. This relationship is irrelvant to the content of this manuscript. No other authors have conflicts of interest to disclose
Footnotes
Presented at the American College of Surgeons Surgical Simulation Summit in March 2022.
References
- 1.Emanuel E.J., Persad G., Upshur R., et al. Fair allocation of scarce medical resources in the time of COVID-19. N Engl J Med. 2020;382:2049–2055. doi: 10.1056/NEJMsb2005114. [DOI] [PubMed] [Google Scholar]
- 2.White D.B., Lo B. A framework for rationing ventilators and critical care beds during the COVID-19 pandemic. JAMA. 2020;323:1773–1774. doi: 10.1001/jama.2020.5046. [DOI] [PubMed] [Google Scholar]
- 3.Prachand V.N., Milner R., Angelos P., et al. Medically necessary, time sensitive procedures: scoring system to ethically and efficiently manage resource scarcity and provider risk during the COVID-19 pandemic. J Am Coll Surg. 2020;231:281–288. doi: 10.1016/j.jamcollsurg.2020.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Aziz H., James T., Remulla E., et al. Effect of COVID-19 on surgical training across the United States: a national survey of general surgery residents. J Surg Educ. 2021;78:431–439. doi: 10.1016/j.jsurg.2020.07.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sneyd J.R., Mathoulin S.E., O'Sullivan E.P., et al. Impact of the COVID-19 pandemic on anaesthesia trainees and their training. Br J Anaesth. 2020;125:450–455. doi: 10.1016/j.bja.2020.07.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Andreae M.H., Dudak A., Cherian V., et al. Data and debriefing observations on healthcare simulation to prepare for the COVID-19 pandemic. Data Brief. 2020;31 doi: 10.1016/j.dib.2020.106028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Andreae M.H., Dudak A., Cherian V., et al. Healthcare simulation to prepare for the COVID-19 pandemic. J Clin Anesth. 2020;66 doi: 10.1016/j.jclinane.2020.109928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Braun V., Clarke V. Reflecting on reflexive thematic analysis. Qual Res Sport Exerc. 2019;11:589–597. [Google Scholar]
- 9.Andreae M.H., Dudak A., Cherian V., et al. Data and debriefing observations on healthcare simulation to prepare for the COVID-19 pandemic. Data Brief. 2020;31 doi: 10.1016/j.dib.2020.106028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hope C., Reilly J.J., Griffiths G., Lund J., Humes D. The impact of COVID-19 on surgical training: a systematic review. Tech Coloproctol. 2021;25:505–520. doi: 10.1007/s10151-020-02404-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.COVID-STAR Collaborative Study Group COVID-19 impact on Surgical Training and Recovery Planning (COVID-STAR) - A cross-sectional observational study. Int J Surg. 2021;88 doi: 10.1016/j.ijsu.2021.105903. [DOI] [PMC free article] [PubMed] [Google Scholar]