Abstract
Objective
To assess the volume of deferred ophthalmic surgeries in Ontario associated with the COVID-19 pandemic from March to December 2020 and suggest strategies and time required to clear the backlog.
Design
Cross-sectional study.
Participants
Ontarians eligible for the Ontario Health Insurance Plan in 2017–2020.
Methods
Backlog and clearance time for ophthalmic surgeries associated with the COVID-19 pandemic were estimated from time-series forecasting models and queuing theory.
Results
From March 16 to December 31, 2020, the estimated ophthalmic surgical backlog needing operating rooms was 92,150 surgeries (95% prediction interval, 71,288–112,841). Roughly 90% of the delayed surgeries were cataract surgeries, and a concerning 4% were retinal detachment surgeries. Nearly half the provincial backlog (48%; 44,542 of 92,150) was in patients from the western health region. In addition, an estimated 23,755 (95% prediction interval, 14,656–32,497) anti–vascular endothelial growth factor injections were missed. Estimated provincial clearance time was 248 weeks (95% CI, 235–260) and 128 weeks (95% CI, 121–134) if 10% and 20% of operating room surgical capacity per week were added, respectively, based on the weekly ophthalmic surgical volume in 2019.
Conclusions
Ontario data demonstrate that the magnitude of the ophthalmic surgical backlog in 2020 alone raises serious concerns for meeting the ophthalmic surgical needs of patients. As the pandemic continues, the accrued backlog size is likely to increase. Planning and actions are needed urgently to better manage the collateral impacts of the pandemic on the ophthalmic surgical backlog.
In response to the COVID-19 pandemic,1 worldwide jurisdictions intermittently stopped or ramped down nonemergent surgeries,2, 3, 4 creating a global surgical backlog of unknown size. This unknown information limits the ability of administrators to develop strategies to effectively address the backlog.
In Ontario, the Ministry of Health directed hospitals/clinics to begin a measured “ramping down of elective surgeries and other nonemergent clinical activity” on March 15, 2020.2 In less than 3 months this directive resulted in 148,364 deferred surgeries, including cancer, cardiac, transplant, pediatric, vascular, and other (including ophthalmic) surgeries.5 The directive was lifted on May 26, 2020.6 Since then, hospital and clinic services in Ontario have gradually increased but have not returned to full capacity because of the ongoing pandemic, patient hesitancy, and new protocols to limit the impact of COVID-19.
In 2020, Wang et al.5 estimated that it will take 84 weeks to clear the backlog accrued in the first 3 months of the pandemic in Ontario, under the scenario of 717 weekly surgeries with 719 operating room hours, 265 hospital ward beds, and 9 intensive care unit beds available per week. Because ophthalmic surgeries are mostly day surgeries, clearing the ophthalmic surgical backlog is not constrained by available hospital and intensive care unit beds. The estimated clearance time by Wang et al.5 thus does not apply to ophthalmic surgeries, the most common adult surgery.
With global COVID-19 vaccination efforts,7, 8, 9 the impact of the pandemic will hopefully lessen. To assist with better comprehension of the magnitude of the ophthalmic surgical backlog and development of an evidence-based recovery plan, we analyzed population-based data to assess the volume of deferred ophthalmic surgeries associated with COVID-19 in March–December 2020 and suggest strategies and time required to clear the backlog in Ontario.
Methods
In Canada, medically necessary services are universally covered for all residents by publicly funded health insurance plans administered at the provincial level. In Ontario, the largest province in Canada by population (>14.7 million in 2020, 39.2% of Canada's population),10 ophthalmologists submit claims to the Ontario Health Insurance Plan (OHIP) for payment of insured services.
Ophthalmic surgeries were arranged into 9 subgroups using fee codes:11 retinal detachment (RD), intravitreal anti–vascular endothelial growth factor (anti-VEGF; code E147) injection, retina (other than RD and anti-VEGF), glaucoma, cataract, strabismus, pterygium, cornea (other than pterygium), and other. Surgeries for RD, retina, glaucoma, cataract, strabismus, and cornea typically require use of an operating room. These subgroups were analyzed separately and combined into 1 group—ophthalmic operating room surgeries. Anti-VEGF injections and pterygium surgery typically are done in clinics and were analyzed individually. We also analyzed data on ophthalmologists’ clinical visits and consults to assess the volumes of delayed nonsurgical services. We considered 5 health regions (Toronto, central, north, west, and east) in Ontario (Fig. 1 ) to examine geographic backlog distribution.12 , 13
Fig. 1.
Five health regions in Ontario in 2020.
Data sources
We analyzed 3 population-based databases housed at ICES: OHIP physician billing database, ICES Physician Database, and Registered Persons Database (RPDB). The OHIP database provided physician services related information (e.g., surgery type, surgery date). The ICES Physician Database furnished physician-related information (e.g., physician specialty). The Registered Persons Database contained demographics information (e.g., age, sex, and location of residence) for OHIP-insured Ontarians. Database linkages were done using encrypted health card numbers in a protected environment by ICES analysts. Aggregated data were provided for analyses. This study was approved by the Research Ethics Board at the University of Toronto (No. 39901).
Estimating the backlog size
We estimated the backlog size as the difference between the expected and observed number of surgeries from March 16 to December 31, 2020, on a weekly basis. This backlog is the result of ramping down surgical services from the initial Ministry of Health announcement on March 15 to gradual reopening on May 26, 2020, up to December 31, 2020.2 , 6
The observed number of surgeries was the number of surgeries billed to OHIP by ophthalmologists. The expected number of surgeries was the number of surgeries expected to be performed by ophthalmologists as obtained from time-series forecasting models considering historical patterns and seasonal variations.14 , 15
Estimating clearance time
The clearance time was estimated as the backlog size divided by the weekly surgical volume that would be added, an adaptation of Little's law from queuing theory16 and used in prior publications.5 According to the Little's law, the average number of customers L in a queuing system is equal to the average arrival rate λ multiplied by the average time W that a customer spends in the system, that is, L = λW.5 , 16 Through algebraic manipulations, we can easily get W = L/λ. In our case, W is the average time spent waiting for surgery (clearance time), L is the surgical backlog (waiting in the queue), and λ is the weekly surgical volume being added.5 , 16 The weekly surgical volumes that would be added were estimated in 2 steps. First, we obtained the average weekly number of ophthalmic operating room surgeries in 2019 (e.g., 3177 for cataract surgeries). We then divided the weekly number by the conventional 40 working hours per week to estimate the number of surgeries per hour in Ontario (e.g., 3,177/40 = 79 cataract surgeries per hour). Second, the product of the hourly number of surgeries and additional operating hours added per week (assuming the status quo weekly volumes, i.e., no additional backlog) was used to calculate the clearance time. The added weekly additional operating hours divided by the conventional 40 weekly working hours was the percentage of increased surgical capacity, for example, adding 4 additional hours per surgical week divided by 40 hours per week equals a 10% increased surgical capacity.
Clearance time was estimated using various recovery scenarios between 2 extremes: 10% and 70% increase in weekly surgical time. The 10% increase is equivalent to adding half a day in the scenario of 8 hours in a day and 5 surgical days in a week; the 70% increase is equivalent to adding 8 operating hours on Saturday plus prolonging Monday to Friday from an 8-hour operating day to a 12-hour operating day. These 2 extremes represent potential additional surgical hours from a conservative to an aggressive approach. Clearance times in various scenarios between these 2 extremes were calculated. No clearance time was estimated for anti-VEGF injections because anti-VEGF injections are typically administered at a specific frequency. A missed injection would not result in an extra injection to catch up but rather a resumption of the injection frequency.
Statistical analysis
Time-series models were used to forecast the expected number of surgeries with data divided into 3 subsets: training set, validation set, and forecasting set. The training set included data from January 2, 2017, to March 11, 2019 (115 weeks), aiming to identify the weekly patterns of ophthalmic surgeries. The validation set included data from March 18, 2019, to March 9, 2020 (52 weeks), aiming to use the external data set to recognize which of several forecasting models performed best. The forecasting set included data from March 16, 2020, to December 31, 2020 (42 weeks), aiming to obtain the observed and expected number of surgeries for the pandemic period. Ophthalmic surgical volumes in Ontario displayed a clear seasonal variation (higher volumes in April and September and lower volumes in August and December in 2019; Fig. 2 ). We used the following models to take into account the effects of seasonal variations to improve the model performance in forecasting: seasonally naïve model, seasonal and trend decomposition model using locally estimated scatter-plot smoothing, dynamic harmonic regression with trigonometric terms for seasonality, and TBATS state-space models.14 , 15 Model selection was done using the root-mean-squared error during the validation period.15 Variability and uncertainty of the backlog estimation were dealt with the bootstrap technique with 1,000 trials. Uncertainty of the clearance time was taken into account with the Monte Carlo simulation with 1,000 trials at the provincial level and 10,000 trials at the regional level. All analyses were performed using SAS v9.4 (SAS Institute Inc, Cary, NC).
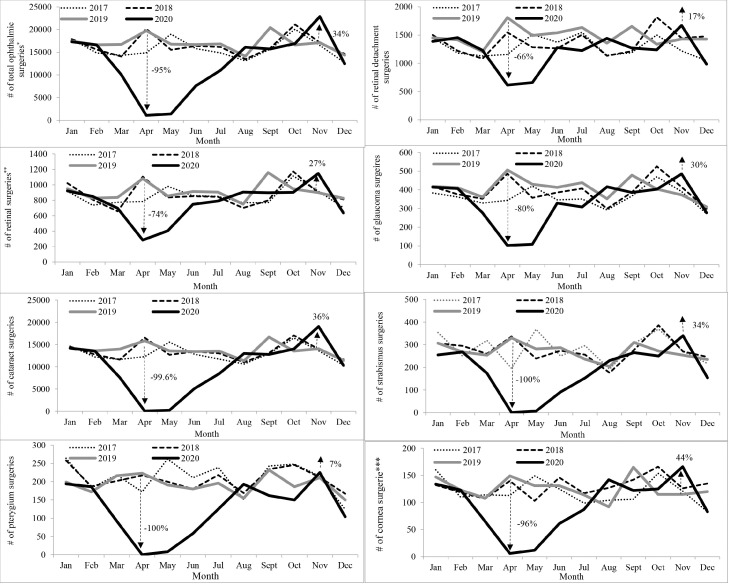
Fig. 2.
Monthly volume of ophthalmic surgeries in Ontario from 2017 to 2020.
*Not including anti-vascular endothelial growth factor injections and other less common ophthalmic surgeries that require use of an operating rooms.
†Excluding retinal detachment surgeries and anti-vascular endothelial growth factor injections.
‡Excluding pterygium surgeries.
Results
In 2018 and 2019, Ontario ophthalmologists provided 6.48 million and 6.60 million services, respectively. In 2020, services were reduced by 22% to 5.13 million. In 2019, 6.2% (411,823) of the services were procedures, including 203,567 ophthalmic operating room surgeries, 205,945 anti-VEGF injections, and 2,311 pterygium surgeries. In 2020, the number of operating room surgeries was 149,146 (26.7% decrease versus 2019), and the number of anti-VEGF injections was 193,921 (5.8% decrease versus 2019). The weekly mean number of surgeries and SD for Ontario and the 5 health regions in 2017–2020 are shown in Table 1 .
Table 1.
Weekly mean number and SD (in parenthesis) of ophthalmic surgeries in Ontario and health regions, 2017–2020
| Surgeries | 2017 | 2018 | 2019 | 2020 |
|---|---|---|---|---|
| Ontario | ||||
| Total ophthalmic surgeries* | 3649 (796) | 3738 (911) | 3915 (857) | 2868 (1663) |
| Pterygium | 49 (16) | 47 (16) | 44 (13) | 29 (20) |
| Anti-VEGF | 3441 (586) | 3685 (681) | 3960 (807) | 3729 (807) |
| Central | ||||
| Total ophthalmic surgeries* | 1092 (214) | 1135 (240) | 1198 (261) | 880 (497) |
| Pterygium | 23 (11) | 23 (9) | 22 (9) | 14 (11) |
| Anti-VEGF | 770 (142) | 834 (153) | 910 (184) | 848 (185) |
| East | ||||
| Total ophthalmic surgeries* | 986 (267) | 1007 (283) | 1030 (261) | 758 (460) |
| Pterygium | 10 (5) | 9 (4) | 9 (4) | 6 (4) |
| Anti-VEGF | 1031 (241) | 1109 (276) | 1196 (296) | 1097 (261) |
| North | ||||
| Total ophthalmic surgeries* | 246 (75) | 252 (83) | 251 (74) | 177 (110) |
| Pterygium | 2 (2) | 1 (1) | 1 (1) | 1 (1) |
| Anti-VEGF | 231 (62) | 244 (70) | 256 (82) | 260 (81) |
| Toronto | ||||
| Total ophthalmic surgeries* | 274 (64) | 281 (68) | 280 (55) | 222 (123) |
| Pterygium | 5 (3) | 5 (3) | 5 (3) | 3 (3) |
| Anti-VEGF | 232 (40) | 248 (47) | 263 (57) | 241 (62) |
| West | ||||
| Total ophthalmic surgeries* | 1052 (228) | 1062 (280) | 1155 (253) | 832 (489) |
| Pterygium | 8 (4) | 9 (5) | 8 (4) | 6 (5) |
| Anti-VEGF | 1177 (213) | 1251 (238) | 1336 (269) | 1285 (289) |
anti-VEGF = anti–vascular endothelial growth factor
Excluding anti–vascular endothelial growth factor and pterygium surgery.
Compared with the monthly volumes of surgeries in 2019, the number of surgeries in April 2020 was the lowest, reduced by 95% for ophthalmic operating room surgeries, 66%–80% for emergent eye surgeries, and nearly 100% for nonemergent eye surgeries (Fig. 2). For anti-VEGF injections, the volume reduction in April 2020 was 42%. In November 2020, all types of ophthalmic surgical volumes increased (Fig. 2). For anti-VEGF injection, the volume increased by 25% in November 2020.
Results of the weekly time-series forecast for ophthalmic operating room surgeries are shown in Figure 3 . Weekly time-series forecasts for each surgery type can be found in Appendix A (available online). Between March 16 and December 31, 2020, the incremental provincial backlog was 92,150 operating room surgeries (95% prediction interval [PI], 71,288–112,841; Table 2 ). By health region, the largest backlog was among patients in the west (44,542), and the smallest was among patients in Toronto (4,132; Table 2). Weekly accumulation of the provincial backlog is illustrated in Figure 4 .
Fig. 3.
Weekly volumes versus forecasts for all ophthalmic surgeries that require use of an operating room in Ontario from January 2017 to December 2020. Shaded area: 95% prediction interval. Anti–vascular endothelial growth factor injections and other less common ophthalmic surgeries that require use of an operating room were not included.
Table 2.
Estimated backlog size and 95% prediction interval of ophthalmic surgeries in Ontario and health regions, 2020
| Surgery | Ontario | Central | East | North | Toronto | West |
|---|---|---|---|---|---|---|
| Cataracts | 83,561 (64,689–101,820) |
17,473 (11,576–23,554) |
15,960 (10,428–21,216) |
4927 (3645–6183) |
3369 (2060–4687) |
41,832 (36,891–46,899) |
| Retinal detachment | 3453 (2683–4448) | 860 (379–1343) | 550 (228–889) | 227 (133–321) | 275 (123–425) | 1540 (1395–1708) |
| Retina (other than RD and anti-VEGF) | 2195 (1432–3033) | 590 (274–894) | 646 (411–892) | 90 (20–156) | 235 (129–338) | 634 (418–853) |
| Glaucoma | 1276 (805–1739) | 763 (569–937) | 132 (18–281) | 46 (13–75) | 125 (54–194) | 210 (100–330) |
| Strabismus | 1063 (714–1429) | 409 (278–547) | 280 (159–399) | 64 (28–95) | 72 (24–118) | 239 (137–333) |
| Cornea (other than pterygium) | 602 (440–770) | 228 (158–297) | 201 (148–252) | 30 (17–43) | 57 (34–77) | 86 (29–142) |
| Total surgeries* | 92,150 (71,288–112,841) |
20,322 (13,347–27,312) |
17,769 (11,510–23,661) |
5,385 (3981–6745) |
4,132 (2585–5721) |
44,542 (39,199–49,974) |
| Pterygium | 758 (475–1035) | 414 (246–582) | 83 (20–141) | 21 (4–38) | 88 (52–123) | 153 (87–219) |
| Anti-VEGF injection | 23,755 (14,656–32,497) |
3774 (1853–5695) |
10,231 (6701–13,379) |
1107 (47–2261) | 1417 (811–1992) | 7226 (3798–10,754) |
RD = retinal detachment; anti-VEGF = anti–vascular endothelial growth factor
Not including other less common eye surgeries that require use of an operating room.
Fig. 4.
Week-over-week accumulation of the mean provincial backlog for all ophthalmic surgeries that require use of an operating room from March to December 2020. Anti–vascular endothelial growth factor injections and other less common ophthalmic surgeries that require use of an operating room were not included.
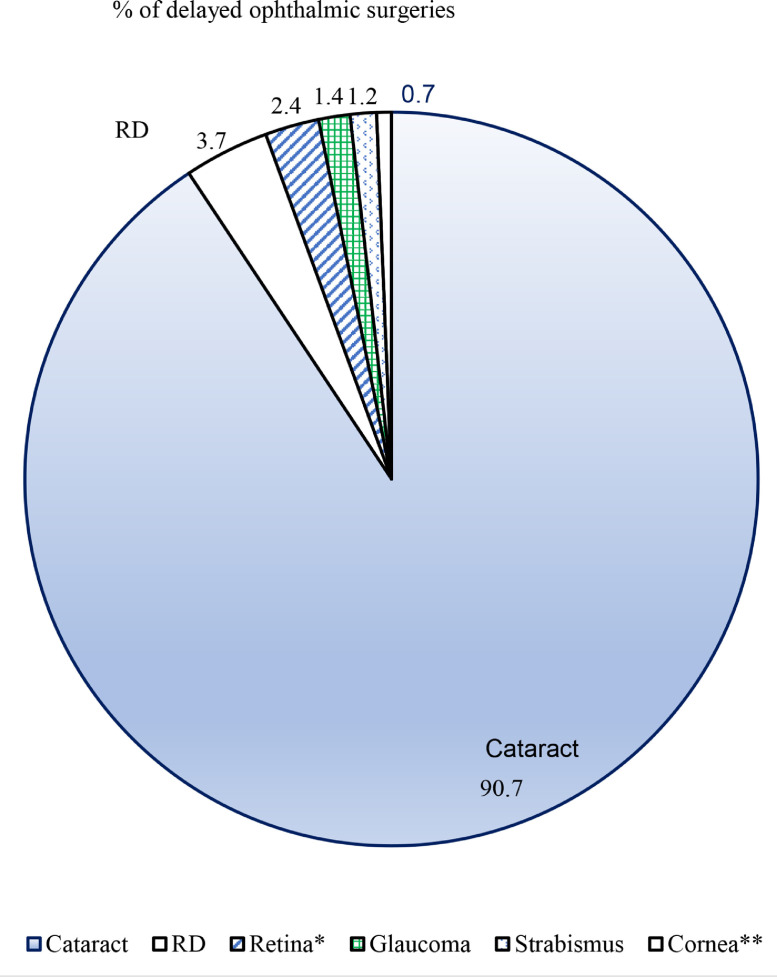
By surgery type, the largest backlog was cataract surgery (Table 2 and Fig. 5 ). This was followed by RD surgery. The smallest backlog was cornea surgery. The missed number of anti-VEGF injections was 23,755 (95% PI, 14,656–32,497; Table 2).
Fig. 5.
Percentage of delayed ophthalmic surgeries by surgery type.
*Excluding retinal detachment surgeries and anti-vascular endothelial growth factor injections.
**Excluding pterygium surgeries.
In 2020, assessments and consults decreased by 27% (510,571 fewer assessments) and 28% (157,413 fewer consults) compared with 2019, which was 5.5 and 1.7 times, respectively, greater than the delayed number of operating room surgeries. In 2019, 21% of patient assessments had a diagnosis of glaucoma, 21% had a cataract diagnosis, and 22% had a retinal diagnosis (Appendix B, available online). The percentages of diagnostic groups in ophthalmologist consults were 17% for glaucoma, 20% for cataract, and 15% for retina (Appendix B, available online).
Figure 6 shows the estimated clearance time for the ophthalmic operating room surgeries backlog. With a 10% increase in surgical time, it would take 248 weeks (4.8 years) to clear the provincial backlog. With a 70% increase in surgical time, it would require 36 weeks (0.7 year) to clear Ontario's 2020 backlog. Figure 6 also shows that increasing surgical capacity from 10% to 20% per week would shorten the clearance time by 120 weeks (248–128 weeks). However, increasing from 60% to 70% only decreases the clearance time by 6 weeks (42–36 weeks). In the west region, the estimated clearance time exceeds the estimated provincial clearance time in every additional surgical capacity added per week (Fig. 7 ).
Fig. 6.
Estimated clearance time for total number of ophthalmic surgeries that require use of an operating room at the provincial level. Not including anti–vascular endothelial growth factor injections and other less common ophthalmic surgeries that require use of an operating room. A 10% increase in surgical capacity is equivalent to adding half a day (4 hours) in the scenario of 8 hours in a day and 5 surgical days in a week [4/(8 × 5) = 10%]. Shaded area: 95% CI.
Fig. 7.
Estimated clearance time for total number of ophthalmic surgeries that require use of an operating room by health region in Ontario. Not including anti–vascular endothelial growth factor injections and other less common ophthalmic surgeries that require use of an operating room. A 10% increase in surgical capacity is equivalent to adding half a day (4 hours) in the scenario of 8 hours in a day and 5 surgical days in a week [4/(8 × 5) = 10%].
Discussion
This analysis estimated that 92,150 ophthalmic operating room surgeries were delayed in Ontario due to COVID-19 restrictions in March–December 2020 alone. Of these, the majority (90%) were cataract surgeries, and a concerning 4% were RD surgeries. However, emergency surgeries were allowed throughout the pandemic, suggesting possible delays in diagnosis due to issues with access to assessments or patient hesitancy, as demonstrated in Figure 2, where RD surgeries were reduced by 66% in April 2020. The backlog was unevenly distributed across the province, with the largest being among patients in the west region and the smallest in Toronto (Table 2). The estimated provincial clearance time was 248 and 128 weeks if an additional 10% and 20% surgical capacity per surgical week were added, respectively. In addition, 23,755 anti-VEGF injections were missed. Missed anti-VEGF injections may lead to worsening or permanent vision loss.17 In comparison to the surgical backlog, 5.5 times more ophthalmologist assessments and 1.7 times more consults were missed. Some of these missed assessments would be the result of cancelled surgeries. Overall, the impact of the ophthalmology backlog is large, and developing and implementing strategies to address this are required urgently to lessen the potential vision loss created by the reaction to the pandemic.
Reduced surgical services during the pandemic have been a ubiquitous phenomenon worldwide.5 , 18 , 19 Estimates on the scale of cancelled surgeries during the initial COVID-19 peak disruption have been published.5 , 18 , 19 However, ophthalmic surgeries are often grouped into the “other” category.5 , 18 Recently, Felfeli et al.20 predicted the ophthalmic surgical backlog due to COVID-19 using the Ontario Wait Time Information System database and a microsimulation model. The authors reported that “by 2 years and 3 years since the start of the pandemic, the overall estimated number of patients awaiting surgery grew by 129% and 150%, respectively.” Due to differences in the database used (Wait Time Information System database vs physician billing database) and time period studied (2–3 years versus 10 months following the pandemic declaration), it is difficult to compare their findings with this study. Aggarwal et al.19 forecasted the volume of cataract surgery in U.S. Medicare beneficiaries due to COVID-19 using a linear regression model that ignores seasonal variations of ophthalmic surgeries. Compared with previous reports, our study not only focused on ophthalmic surgeries but also assessed anti-VEGF injections, office assessments, and new consults using population-based physician billing data and time-series forecasting models.
Physicians and allied health care workers are indispensable in clearing the surgical backlog. Physicians, including training physicians, have endured long working hours before COVID-19 compared with the general population (45–85 weekly working hours in practicing physicians and >50 hours in 87% of training physicians versus 40 hours in the general population).21, 22, 23, 24, 25 Physicians also experienced higher burnout rates before COVID-19.26 , 27 The pandemic has heightened existing challenges that physicians face and increased physician burnout.28, 29, 30 Adding additional operating hours is necessary to clear the backlog but may worsen existing burnout and other health issues in physicians and allied health care providers.
We propose 3 strategies to deal with the reported ophthalmic surgical backlog: (i) maximizing current surgical capacity will help to reduce the accrued backlog during the ongoing pandemic by carefully balancing patients’ needs, COVID-19 risk, and health care providers’ wellness; (ii) developing programs specifically targeting cataract surgery, the main contributor to the surgical backlog, will provide the greatest impact to reduce the ophthalmic surgical backlog and associated impact on quality of life; and (iii) Encouraging patients with retinal detachment and other urgent medical conditions to seek timely care. Retinal detachment is an emergency eye condition that requires timely surgical treatment to avoid permanent vision loss/blindness. Although emergency retinal detachment surgeries were allowed throughout the pandemic, the 4% retinal detachment surgical backlog suggests possible delays in diagnosis, including access to assessments or patient hesitancy. Public education is needed.
Study limitations include that the estimation of surgical backlog size and clearance time was focused on urgent and common ophthalmic surgeries only. This may result in an underestimation of the backlog size and clearance time for all ophthalmic surgeries. In dealing with massive backlog sizes, focusing on urgent and common surgeries is important. Second, our analysis included data up to December 2020 only and did not account for the backlog associated with COVID-19 in 2021 and beyond. Repeated shutdowns and reopenings and the surge in the omicron variant further compound the backlog and call for an analysis with updated data. Third, due to backlogs upstream in primary care, obtaining a consultation and patient hesitancy, it is possible that actual wait lists for ophthalmic surgery may be less. Fourth, we did not have information on where the surgeries were done (e.g., independent health facility, hospital, etc). Future studies are needed to understand whether the backlog was evenly distributed between independent health facilities and hospitals. Fifth, there is no differentiation between retinal redetachment surgery and new detachment surgery. Finally, the regional analysis was based on patient residence. This should be considered in the event of regional allocation of additional resources.
In conclusion, using population-based, single-payer, real-world physician billing data and time series models, we estimated that 92,150 ophthalmic surgeries were delayed in Ontario due to COVID-19 in 2020 alone. Roughly 90% of the delayed surgeries were cataract surgeries and a concerning 4% were RD surgeries. The estimated provincial clearance time ranged from 248 to 36 weeks if additional surgical capacity of 10%–70% per week were added. In addition, a much larger number of nonsurgical visits were missed that also may result in worsening of patient outcomes. Health administrators and ophthalmologists must react and plan now to treat patients effectively and safely while balancing physician wellness.
Acknowledgments
Footnotes and Disclosure
The authors have made the following disclosures: This study contracted ICES Data and Analytic Services (DAS) and used deidentified data from the ICES Data Repository, which is managed by ICES with support from its funders and partners: Canada's Strategy for Patient-Oriented Research (SPOR), the Ontario SPOR Support Unit, the Canadian Institutes of Health Research, and the Government of Ontario. The opinions, results, and conclusions reported are those of the authors. No endorsement by ICES or any of its funders or partners is intended or should be inferred.
Funding
This work was supported by the Ontario Ministry of Health for the COVID-19 Challenge Questions Initiative. The costs associated with preparing the data cut by ICES analysts for the study were provided by the Ministry of Health.
The authors thank Ms. Qi-Sheng Chen from the University of Waterloo, Canada, for preparation of Figure 1.
Conflicts of interest
The authors have no proprietary or commercial interest in any materials discussed in this article.
Footnotes
Supplementary material associated with this article can be found in the online version at doi:10.1016/j.jcjo.2022.06.020.
Appendix. Supplementary materials
References
- 1.World Health Organization. Timeline: WHO's COVID-19response. Available from: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/interactive-timeline#!. Accessed Jul. 26, 2022.
- 2.Ontario Ministry of Health . Ministry of Health and Long-Term Care; Toronto: 2020 Mar. 15. Ramping down elective surgeries and other non-emergent activities [memorandum to Ontario Health and hospitals]http://www.health.gov.on.ca/en/pro/programs/publichealth/coronavirus/docs/memos/DM_OH_CMOH_memo_COVID19_elective_surgery_March_15_2020.pdf Available from. Accessed Aug. 6, 2021. [Google Scholar]
- 3.Royal College of Ophtalmologists. Reopening and redeveloping ophthalmology services during Covid recovery – Interim guidance. Available from: https://www.rcophth.ac.uk/wp-content/uploads/2020/05/Reopening-Redeveloping-Ophthalmology-Services-During-COVID-Recovery-Interim-Guidance.pdf. Accessed Jul. 26, 2022.
- 4.COVIDSurg Collaborative Global guidance for surgical care during the COVID-19 pandemic. Br J Surg. 2020;107:1097–1103. doi: 10.1002/bjs.11646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wang J, Vahid S, Eberg M, et al. Clearing the surgical backlog caused by COVID-19 in Ontario: a time series modelling study. CMAJ. 2020;192:E1347–E1356. doi: 10.1503/cmaj.201521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Williams DC. Ministry of Health and Long-Term Care; Toronto: 2020. COVID-19 directive #2 for health care providers (regulated health professionals or persons who operate a group practice of regulated health professionals), issued under Section 77.7 of the Health Protection and Promotion Act (HPPA), R.S.O. 1990, c. H.7 [yyyy mon dd]https://www.oha.com/Bulletins/CMOH%20Directive%202%20-%20Health%20Care%20Providers%20-%20April%2020%202021%20FINAL%20AODA.pdf Available from. Accessed Aug. 6, 2021. [Google Scholar]
- 7.Health Canada. COVID-19 vaccination in Canada [yyyy mon dd]. Available from: https://health-infobase.canada.ca/covid-19/vaccination-coverage/. Accessed Aug. 6, 2021.
- 8.Centers for Disease Control and Prevention. COVID-19 Vaccinations in the United States. Available at https://covid.cdc.gov/covid-data-tracker/#vaccinations_vacc-total-admin-rate-total Accessed Aug 6, 2021.
- 9.Our World in Data. Coronavirus (COVID-19) vaccinations [yyyy mon dd]. Available from: https://ourworldindata.org/covid-vaccinations?country=OWID_WR. Accessed Aug. 6, 2021.
- 10.Statistics Canada. Table 17-10-0005-01: population estimates on July 1st, by age and sex [yyyy mon dd]. Available from: https://www150.statcan.gc.ca/t1/tbl1/en/tv.action?pid=1710000501. Accessed Nov. 18, 2021.
- 11.Ontario Ministry of Health and Long-Term Care. Ocular and aural surgical procedures [yyyy mon dd]. Available from: https://www.health.gov.on.ca/en/pro/programs/ohip/sob/physserv/y_specia.pdf. Accessed Feb. 15, 2022.
- 12.Dapasoft. 14 LHINs reorganized into 5 transitional regions in Ontario [yyyy mon dd]. Available from: https://www.dapasoft.com/14-lhins-reorganized-ontario/. Accessed Aug. 6, 2021.
- 13.Ontario Ministry of Health and Long-Term Care. Connected care update [yyyy mon dd]. Available from: https://www.health.gov.on.ca/en/news/connectedcare/2019/CC_20191113.aspx. Accessed Feb. 10, 2022.
- 14.de Livera AM, Hyndman RJ, Snyder RD. Forecasting time series with complex seasonal patterns using exponential smoothing. J Am Stat Assoc. 2011;106:1513–1527. [Google Scholar]
- 15.Hyndman RJ, Athanasopoulos G. OTexts; Melbourne (AU): 2018. Forecasting: principles and practice.https://otexts.com/fpp2/ Available from. Accessed Aug. 6, 2021. [Google Scholar]
- 16.Little JDC. A proof for the queuing formula: L = λW. Oper Res. 1961;9:383–387. [Google Scholar]
- 17.Teo KYC, Nguyen V, Barthelmes D, Arnold JJ, Gillies MC, Cheung CMG. Extended intervals for wet AMD patients with high retreatment needs: informing the risk during COVID-19, data from real-world evidence. Eye (Lond) 2021;35:2793–2801. doi: 10.1038/s41433-020-01315-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.COVIDSurg Collaborative Elective surgery cancellations due to the COVID-19 pandemic: global predictive modelling to inform surgical recovery plans. Br J Surg. 2020;107:1440–1449. doi: 10.1002/bjs.11746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Aggarwal S, Jain P, Jain A. COVID-19 and cataract surgery backlog in Medicare beneficiaries. J Cataract Refract Surg. 2020;46:1530–1533. doi: 10.1097/j.jcrs.0000000000000337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Felfeli T, Ximenes R, Naimark DMJ, et al. The ophthalmic surgical backlog associated with the COVID-19 pandemic: a population-based and microsimulation modelling study. CMAJ Open. 2021;9:E1063–E1072. doi: 10.9778/cmajo.20210145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Slade S, Busing N. Weekly work hours and clinical activities of Canadian family physicians: results of the 1997/98 National Family Physician Survey of the College of Family Physicians of Canada. CMAJ. 2002;166:1407–1411. [PMC free article] [PubMed] [Google Scholar]
- 22.Chen KY, Yang CM, Lien CH, et al. Burnout, job satisfaction, and medical malpractice among physicians. Int J Med Sci. 2013;10:1471–1478. doi: 10.7150/ijms.6743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wegner R, Szadkowski D, Poschadel B, Simms M, Niemeyer Y, Baur X. Psychomental stress in doctors: the results of a questionnaire. Arbeitsmedizin Sozialmedizin Umweltmedizin. 2002;37:60–75. [Google Scholar]
- 24.Cohen JS, Leung Y, Fahey M, et al. The happy docs study: a Canadian Association of Internes and Residents well-being survey examining resident physician health and satisfaction within and outside of residency training in Canada. BMC Res Notes. 2008;1:105. doi: 10.1186/1756-0500-1-105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Statistics Canada. Total number of employed persons in Canada in 2017, by average usual weekly hours (in 1,000) [yyyy mon dd]. Available from: https://www.statista.com/statistics/438177/employment-level-in-canada-by-average-usual-weekly-hours/. Accessed Sep. 5, 2021.
- 26.Medscape. National physician burnout and suicide report 2020: the generational divide [yyyy mon dd]. Available from: https://www.medscape.com/slideshow/2020-lifestyle-burnout-6012460?src=WNL_physrep_200207_burnout2020_RM_int&uac=124881MT&impID=2269802&faf=1#4. Accessed Aug. 7, 2021.
- 27.Dyrbye LN, West CP, Satele D, et al. Burnout among U.S. medical students, residents, and early career physicians relative to the general U.S. population. Acad Med. 2014;89:443–451. doi: 10.1097/ACM.0000000000000134. [DOI] [PubMed] [Google Scholar]
- 28.Amanullah S, Ramesh Shankar R. The impact of COVID-19 on physician burnout globally: a review. Healthcare (Basel) 2020;8:421. doi: 10.3390/healthcare8040421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kannampallil TG, Goss CW, Evanoff BA, Strickland JR, McAlister RP, Duncan J. Exposure to COVID-19 patients increases physician trainee stress and burnout. PLoS One. 2020;15 doi: 10.1371/journal.pone.0237301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Physicians for Human Rights. Pandemic burnout: the toll of COVID-19 on health care workers and children [yyyy mon dd]. Available from: https://phr.org/our-work/resources/pandemic-burnout-the-toll-of-covid-19-on-health-care-workers-and-children/. Accessed Aug. 6, 2021.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.