Abstract
The COVID-19 pandemic is a major chronic stressor affecting all societies and almost all individuals. Consequently, research demonstrated a negative impact of COVID-19 on mental health in parts of the general population. However, not all people are affected equally thus making the identification of resilience factors modulating the pandemic's impact on mental health an important research agenda. One of these factors is sense of coherence (SOC), the key component of the salutogenesis framework. The current study aimed at investigating the long-term relationship between SOC and psychopathological symptoms, and the impact of COVID-19-related rumination as its moderator. The prospective observational study assessed psychopathological symptoms and SOC before the COVID-19 outbreak in Germany (February 2020) and at six critical time points during the pandemic in an online panel (n = 1,479). Bivariate latent change score models and latent growth mixture modeling were used to analyze changes in psychopathological symptoms and SOC along with their interaction and to differentiate trajectories of COVID-19-related rumination. A model allowing for unidirectional coupling from SOC to psychopathological symptoms demonstrated best fit. In the total sample, psychopathological symptoms increased significantly over time. Previous SOC predicted later changes in psychopathological symptoms, whereby a stronger SOC was associated with a decrease in symptoms over time. The same pattern of results was evident in the high-rumination (17.2%) but not in the low-rumination group (82.8%). Our findings demonstrate that SOC is an important predictor and modulator of psychopathological symptoms during the COVID-19 pandemic, particularly in those respondents that ruminate about the pandemic.
Keywords: COVID-19, Mental health, Sense of coherence, Rumination, Resilience
1. Introduction
The coronavirus disease (COVID-19) pandemic has substantially altered the lives of people throughout the world (Stratton, 2020). As of July 2022, the death toll associated with SARS-CoV-2 (severe acute respiratory syndrome coronavirus type 2) stands at 6.4 million (Dong et al., 2020). COVID-19-related stress not only resulted from the fear of the virus (Şimşir et al., 2022) but also from measures to contain the pandemic. To reduce the spread of the virus, many governments have put in place restrictions on public and private life. A large number of countries curbed their economies by repeatedly closing all non-essential businesses, schools, and recreational facilities (Ehnts and Paetz, 2021). Despite governmental aid, many companies had to cut jobs, leaving numerous people exposed to financial hardship (Nicola et al., 2020). Although physical distancing was held to be one of the most important measures to slow down the spread of SARS-CoV-2, it resulted for some people in harmful social isolation (Banerjee and Rai, 2020). Together with the fear of the virus or loss of loved ones, these factors are among the stressors making the pandemic a major global stressor, which resulted in increased risk for stressor-related mental health problems in many people (Pfefferbaum and North, 2020).
However, despite fears of a ‘second pandemic’ of mental disorders, a large proportion of the population continues to report good mental health (Kunzler et al., 2021, 2022; Prati and Mancini, 2021; Robinson et al., 2022), and mental health consequences were found to depend on individual levels of perceived stress (Ahrens et al., 2021). This is in line with earlier theoretical considerations that expected resilience, that is, in this case conceptualized as maintenance or regain of low levels of psychopathological symptoms, to be the main mental health outcome of the pandemic (Chen and Bonanno, 2020; PeConga et al., 2020). Building on this outcome-oriented approach to resilience, recent research into resilience conceptualizes resilience as a process of adapting well in the face of significant sources of stress (Horn et al., 2016). Within this framework, resilience factors represent resources that protect individuals from potentially aversive effects of stressor exposure. These protective effects are assumed to emerge because resilience factors are associated with, for example, adaptive appraisal styles (Kalisch et al., 2019; 2015) and/or higher levels of regulatory flexibility (Bonanno, 2021; Bonanno and Burton, 2013) as mediating mechanisms, and in turn, with more successful coping. Therefore, it is crucial to identify factors that predict changes in psychopathological symptoms during the COVID-19 pandemic.
Sense of coherence (SOC) as the key factor of the salutogenesis framework may be such a resilience factor (Antonovsky, 1979, 1987). Due to its focus on health and well-being, the salutogenesis framework represents a change in perspective as compared to pathogenic models that focus on illness and disease (Mittelmark and Bauer, 2022). SOC represents a global orientation that “expresses the extent to which one has a pervasive, enduring though dynamic feeling of confidence that one's internal and external environments are predictable and that there is a high probability that things will work out as well as can reasonably be expected” (Antonovsky, 1979). Within the salutogenesis framework, SOC as a trait-like variable modulates one's position on the continuum between health (ease) and disease. Individuals with stronger SOC tend to enjoy better health and are assumed to cope more successfully (Eriksson and Lindström, 2006; Schäfer et al., 2019). When being exposed to a stressor, those with a stronger SOC may also experience a shift of mental health in the direction of disease but are likely to bounce back faster and stronger in the direction of ease.
However, despite a large number of cross-sectional studies (Fossion et al., 2014; Schäfer et al., 2018; Streb et al., 2014), there is less longitudinal evidence showing that SOC predicts mental health or changes in mental health when individuals are exposed to significant stressors. One study by Engelhardt et al. (2003) demonstrated that early pregnancy SOC (pre-stressor) was predictive of psychopathological symptoms one month after pregnancy loss. Correspondingly, a study reported SOC to be predictive of depression onset among Japanese workers (Sairenchi et al., 2011), while another study did not find (post-stressor) SOC to be predictive of posttraumatic stress disorder at one- and three-year follow-up after serious accidental injuries (Hepp et al., 2008). However, the latter studies did not comprise an assessment of pre-stressor SOC. Other studies, mostly conducted in Israel, examined the impact of chronic stressor exposure on SOC. For instance, Braun-Lewensohn and Sagy (2010) examined the impact of missile attacks in South Israel on adolescents’ SOC using a repeated cross-sectional design, finding that exposure to chronic stress resulted in reduced levels of SOC during the 3-year study period. Similarly, adolescents experiencing involuntarily displacement from the Gaza Strip, were found to report lower levels of SOC after displacement, which went back to baseline after five years (Braun-Lewensohn et al., 2013).
This research provided evidence for the interplay between SOC and mental health in face of significant stressor exposure that also inspired several studies that investigated SOC in the context of the COVID-19 pandemic (e.g., Braun-Lewensohn et al., 2021a; Tanaka et al., 2021), with the pandemic constituting a qualitatively new stressor for research into resilience and salutogenesis (Kunzler et al., 2022). In contrast to previous research into individual stressors that occur in all societies (e.g., pregnancy loss; Engelhard et al., 2003), the pandemic evolved from an acute stressor in March 2020 to a chronic stressor still impacting the lives of many two years later. At the same time, the pandemic is not comparable to previous studies on chronic stressor exposure (e.g., displacement, missile attacks; Braun-Lewensohn et al., 2013; Braun-Lewensohn and Sagy, 2010) since it is not specific to a population or region. That is, the COVID-19 pandemic represents a global stressor affecting almost all societies and almost all individuals to some extent synchronously, making it a unique use case for longitudinal research into resilience and SOC. However, so far, research into SOC during the pandemic has mostly being limited to cross-sectional studies, with a recent study finding a robust relationship between SOC and mental health across six countries during the first wave of the pandemic (Mana et al., 2021). This finding is supported by a large number of cross-sectional studies conducted during the first wave (Schmuck et al., 2021; Tanaka et al., 2021). Critically, to the best of our knowledge, the current study is the first with a pre-outbreak assessment that investigates the longitudinal relationship between SOC and psychopathological symptoms.
1.1. The present study
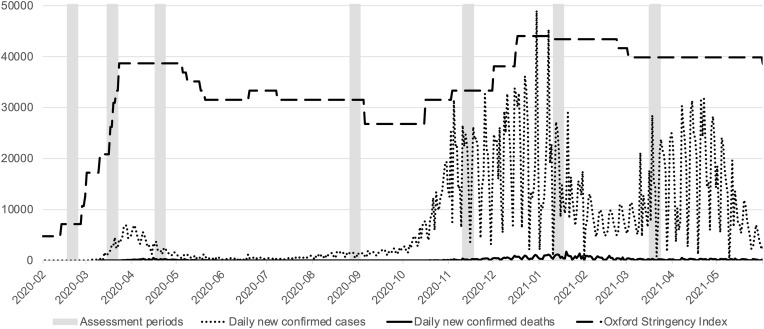
Our study was based on a project conducted in February 2020, immediately prior to the outbreak of the COVID-19 pandemic in Germany on the factorial structure of resilience measures. As participants were part of an online panel, we had the opportunity to repeatedly contact them after the outbreak of COVID-19. Thereby, we were able to compare pre-to-post outbreak mental health and examine a potential buffering effect of SOC in different stages of the pandemic. Findings on the pre-to-post outbreak comparison of psychopathological symptoms in this sample were published immediately after the outbreak of the pandemic (Schäfer et al., 2020b). There was no overall change in psychopathological symptoms from pre-to-post outbreak in the total sample, but we found a significant increase in a subsample reporting high levels of COVID-19-related distress. Significant decreases in symptom levels were evident for a subsample reporting below average COVID-19-related distress. The latter subsample was also characterized by lower levels of psychopathological symptoms, stronger SOC, and better sleep quality that was assessed as transdiagnostic indicator of mental health (Fairholme et al., 2013; Harvey et al., 2011). Most importantly, SOC was found to predict pre-to-post outbreak changes in psychopathological symptoms in the total sample and both subsamples. Stronger SOC was related to smaller changes in psychopathological symptoms. Thus, it seems plausible that SOC buffered the impact of COVID-19 as a multidimensional stressor on psychopathological symptoms. However, causal interpretation of these findings was limited as only two time points were assessed, which only captured responses to the outbreak of the pandemic (see Fig. 1 ). To provide conclusive findings on the long-term relationship between SOC and psychopathological symptoms, it is essential to examine their relationship in the course of the pandemic.
Fig. 1.
Course of the COVID-19 pandemic in Germany and assessment periods of the present study
Note. Data were published by John Hopkins University (Dong et al., 2020), University of Oxford (Hale et al., 2021) and was downloaded via Our World in Data (Odajima et al., 2017). For purpose of visualization, Oxford Stringency Indices were multiplied by 500.
The current study followed the rationale of our previous analyses (Schäfer et al., 2020b) and aimed at extending these findings by examining the relationship between SOC and psychopathological symptoms in the first year post-outbreak based on six critical time points during the pandemic in Germany. Building on systematic reviews on mental health consequences of COVID-19 in the general population (Kunzler et al., 2021, 2022; Prati and Mancini, 2021; Robinson et al., 2022), we expected small yet significant increases of psychopathological symptoms over time in the total sample. We had no hypothesis regarding changes in SOC in the total sample, as we did not expect COVID-19 to be perceived as equally stressful among all respondents (Flesia et al., 2020), that is, changes of SOC were expected to vary depending on individual levels of stressor exposure. Therefore, our analyses included COVID-19-related rumination as indicator of subjective stressor severity (Kovács et al., 2021). Building on previous research (Flett et al., 2002; Nikolova et al., 2021), we assumed that ruminative thoughts would occur when stressors are perceived as unsolvable and overpowering, and that the occurrence of rumination was predictive of psychopathological symptoms (Vanderhasselt et al., 2016). Following the rationale that resilience factors are of importance in more stressful situations (Kalisch et al., 2019; 2015), we assumed SOC to be particularly important in those who experience high levels of COVID-19-related rumination. In line with the results of the first wave of this study (Schäfer et al., 2020b) and previous findings on the negative impact of stressors on SOC levels (Braun-Lewensohn et al., 2013; Braun-Lewensohn and Sagy, 2010; Volanen et al., 2007), we expected SOC to decrease and psychopathological symptoms to increase over time in this group. Moreover, we expected psychopathological symptoms and sleep problems to be more severe as well as the proportion of respondents above cut-off criteria for psychopathological symptoms to be larger in the high-rumination group during the pandemic.
2. Methods
2.1. Study design and sample recruitment
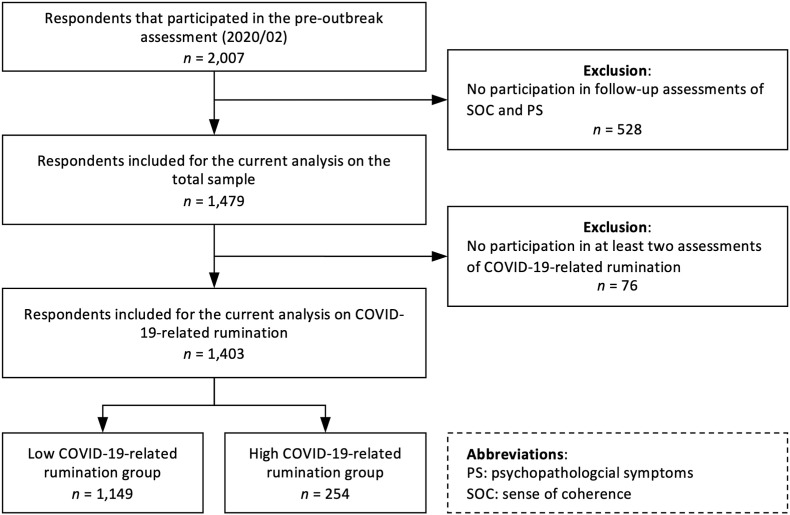
The current study derived from a cross-sectional online study on resilience factors conducted in February 2020. In March 2020, the study team decided to enlarge the scope of the project and to investigate the resilience factor SOC and its association with psychopathological symptoms during the COVID-19 pandemic. Follow-up assessments were conducted in April, August, and November 2020 as well as in January and March 2021 (see Fig. 1). Assessment points were chosen to capture critical points of the course of the pandemic in Germany (see Online Supplementary Material 1). For sample recruitment, we used the WiSo Panel (https://www.wisopanel.net; Göritz et al., 2021). The panel holds N = 14,369 German-speaking adult respondents who live in Germany, Austria, Switzerland, or border regions in neighboring countries. The panel is not representative of the German general population but holds socioeconomically diverse people. Individuals with heterogeneous demographic backgrounds interested in taking part in web-based studies are enrolled in the panel. Of the total panel, 2,007 respondents had participated in the baseline assessment in February 2020. Those were contacted for the follow-up assessments (see Fig. 2 ). Data were collected via the online platform SoSci Survey (Leiner, 2019) and respondents gave written informed consent according to the Declaration of Helsinki. The study was conducted in accordance with the ethical standards of the ethics committee of Saarland University.
Fig. 2.
Study flow chart.
2.2. Measures
Sense of coherence. SOC was assessed using the 9-item German short version (SOC-L9) of the Orientation to Life Questionnaire (Antonovsky, 1993; Singer and Brähler, 2007). SOC-L9 uses a bipolar 7-point scale with a verbal anchor at each pole. Across all time points, SOC showed internal consistency ranging from Cronbach's alpha (α) of 0.89 (2020/03) to 0.92 (2020/08). Temporal stability ranged between rtt = 0.80 (2020/02–2020/08) and r tt = 0.83 (2020/02–2020/03; see Online Supplementary Material 1 for details on retest-reliability).
Psychopathological symptoms. General psychopathological symptom burden was measured using the Mini-Symptom Checklist (BSI-18; Franke, 2017), a brief version of the Brief Symptom Checklist (BSCL; Franke, 2017). The 18-item scale is a measure of global psychopathological symptom burden. All items are rated on a 5-point scale, and higher scores indicate more severe psychopathological symptoms. In the current study, internal consistency ranged from 0.95 (2020/02, 2020/04, 2020/08, 2020/11) to 0.96 (2020/03, 2021/01, 2021/03). Temporal stability ranged between rtt = 0.67 (2020/02–2021/03) and r tt = 0.73 (2020/02–2020/04). For a comparison with the (pre-pandemic) German general population, we used norm data collected in 2009 (Franke et al., 2017). To note, this study also included adolescents (≥14 years) that tended to report lower levels of psychopathological symptoms. However, as no other German norm population was available for a similar age range, we deemed the comparison acceptable. To examine the number of respondents with substantial levels of psychopathological symptoms, we used cut-off scores of 13 and 10 for women and men respectively, which have been used in previous studies (Franke et al., 2010; Zabora et al., 2001). Individuals with above cut-off scores show increased psychopathological symptom burden that may - in some but not all cases - reflect symptoms of a mental disorder.
Sleep quality. Sleep quality during the last week was assessed at all post-outbreak assessments using a German version of the Single-Item Sleep Quality Scale (Snyder et al., 2018). Higher scores on the 11-point scale indicate better sleep quality. Temporal stability ranged between r tt = 0.56 (2020/02–2020/08, 2020/11) and r tt = 0.63 (2020/03–2020/04).
COVID-19-related rumination. COVID-19-related rumination was assessed at all post-outbreak assessments using a modified German version of the Perseverative Thinking Questionnaire (PTQ; Ehring et al., 2011). The 15-item instrument assesses core characteristics of rumination (i.e., repetitiveness, intrusiveness, difficulties to disengage) and was modified to assess COVID-19-related rumination (see the Supplementary Material of Schäfer et al., [2020b] for items). Each item was rated on a 5-point scale, and higher scores indicated more intense rumination. In the current sample, internal consistency ranged from 0.96 (2020/03) to 0.98 (2020/11). Temporal stability ranged between r tt = 0.57 (2020/03–2021/03) and r tt = 0.68 (2020/03–2020/04).
2.3. Data analyses
Analyses were conducted using RStudio version 2021.09.2 (2020), the lavaan package (Rosseel, 2012) and the RBtest package (Rouzinov and Berchtold, 2020). Latent class growth analysis (LCGA), a type of growth mixture modeling, was performed using MPlus version 8.8 (Muthén and Muthén, 2017). Comparisons with sociodemographic data of the German general population were based on data from Census 2011 (Bechtold, 2016). Patterns of missing data were investigated using a regression-based approach (Little, 1988). To analyze latent changes in psychopathological symptoms and SOC as well as the ability of SOC to predict changes in psychopathological symptoms and vice versa, we applied bivariate latent change score (BLCS) models (Grimm et al., 2016; Kievit et al., 2018). To ensure sound parameter estimates, respondents that participated in fewer than two assessments of SOC and psychopathological symptoms were excluded from analyses. Models were estimated using full information maximum likelihood (FIML) and maximum likelihood estimations with robust standard errors and scaled test statistics (MLR) to account for non-normal distributed data (Finney and DiStefano, 2006). Model fit was assessed using the comparative fit index (CFI) and Tucker-Lewis index (TLI; good fit: ≥ 0.97) and the standardized root-mean-square residual (SRMR; good fit: ≤ 0.05; Schermelleh-Engel et al., 2003). To compare nested models, we used Δχ2 difference tests to examine improvement of model fit. The equations proposed by Jajodia (2012) were used to illustrate coupling effects from SOC to psychopathological symptoms. To identify different trajectories of COVID-19-related rumination, we used unconditional LCGA with FIML to handle missing data. Respondents who participated in fewer than two assessments of COVID-19-related rumination were excluded from these analyses. Criteria for model selection followed guidelines for LCGA (van de Schoot et al., 2017), and the best fitting model was selected through multiple criteria. These were reduction in Akaike Information Criteria (AIC) and Bayesian Information Criteria (BIC), sample-size adjusted Bayesian Information Criterion (SSBI), entropy, and smallest class (≥100). Significance of fit differences was indicated by the Vuong-Lo-Mendell-Rubin Likelihood test (VRLT) and the Lo-Mendell-Rubin Adjusted LRT test (LRT). Subgroup analyses used the results from LGCA and were performed by means of multigroup models. Analysis code is available at osf.io/h5vky (Schäfer et al., 2022).
3. Results
3.1. Sample characteristics
The mean age of respondents who were included in the analyses (n = 1,479) was 55.3 years (SD = 13.34; range: 20–95 years) at baseline, and 52.8% were women. The large majority lived in Germany (96.3%), 2.2% in Austria, 1.1% in Switzerland, and 0.4% in other countries (e.g., French-German border area). The current sample did not differ in gender from the general population, p = .052, but respondents were significantly older, t(1478) = 11.86, p < .001, d = 0.62. Moreover, compared with the Census data the current sample was more educated: 0.3% versus 7.6% had not (yet) graduated from school, 31.4% versus 55.7% reported ten years of formal education, 2.3% versus 32.5% in the Census sample completed their A-level. Moreover, compared to 17.6% in the general population, 32.7% had a university degree, and 2.9% versus 1.2% held a doctoral degree. When comparing mean levels of psychopathological symptoms at all timepoints to a German norm population collected in 2009 (Franke et al., 2017), z tests yielded no significant differences, z ≥ −0.70, p ≥ .487. Thus, levels of psychopathological symptoms were comparable to the pre-pandemic German general population throughout the total study period. The regression-based test showed that missing data for all variables included in the following analyses was at least missing at random allowing for the use of FIML. Missing data ranged between 0% at the pre-outbreak assessment (2020/02) and 33% (2020/11). For bivariate correlations see Online Supplementary Material 2.
3.2. Dropout analyses
Respondents who were excluded from analysis were younger, t(2005) = −6.15, p < .001, d = −0.31, more likely to be male, χ2(1) = 18.49, p < .001, Cramer's V = 0.10, but did not differ in educational level, p = .642, r rb = −0.01, from the study sample. They reported lower levels of SOC, t(2005) = 2.66, p = .008, d = 0.14, but did not differ in psychopathological symptoms at pre-outbreak assessment, t(2005) = −1.54, p = .123, d = 0.08. The comparison between those who were included and excluded from the analysis on COVID-19-related rumination revealed the same pattern of results: Excluded respondents were significantly younger, t(1477) = −5.42, p < .001, d = −0.64, more likely to be male, χ2(1) = 9.22, p = .002, Cramer's V = 0.08, but equally educated, p = .106, r rb = −0.11. They reported significantly lower levels of SOC, t(1434) = −2.33, p = .020, d = 0.28, but comparable levels of psychopathological symptoms at pre-outbreak assessment, t(1433) = 1.60, p = .110, d = −0.19.
3.3. Model selection
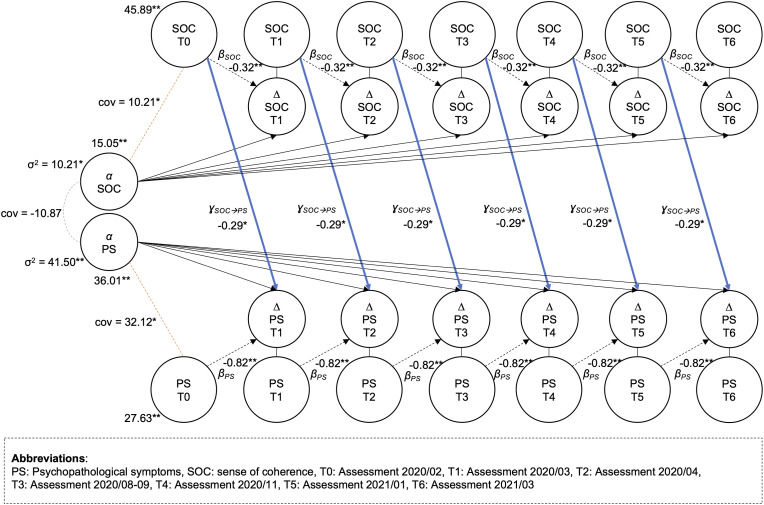
The model selection process is shown in Table 1 . Compared to a model without coupling effects between SOC and psychopathological symptoms only a model allowing for unidirectional coupling from SOC to psychopathological symptoms (see Fig. 3 ) significantly improved model fit, Δχ2(1) = 78.70, p < .001. By contrast, a model allowing for bidirectional coupling did not improve model fit compared to both unidirectional models, Δχ2(1) = 1.76, p = .185.
Table 1.
Fit statistics for all models and model comparisons.
| #pa | (Δ)χ2 | p | CFI | TLI | SRMR | AIC | BIC | ||
|---|---|---|---|---|---|---|---|---|---|
| Model 1 | No coupling between SOC and psychopathological symptoms | 98 | 117.95 | .083 | .992 | .992 | .022 | 108,868 | 108,979 |
| Model 2 | Unidirectional coupling from psychopathological symptoms to SOC | 97 | 115.18 | .100 | .992 | .993 | .025 | 108,861 | 108,978 |
| Model 1 vs. Model 2 | df = 1 | 1.99 | .159 | ||||||
| Model 3 | Unidirectional coupling from SOC to psychopathological symptoms | 97 | 112.39 | .136 | .992 | .993 | .023 | 108,860 | 108,977 |
| Model 1 vs. Model 3 | df = 1 | 78.70 | < .001 | ||||||
| Model 4 | Bidirectional coupling between SOC and psychopathological symptoms | 96 | 110.07 | .155 | .992 | .993 | .024 | 108,855 | 108,976 |
| Model 3 vs. Model 4 | df = 1 | 1.76 | .185 | ||||||
| Model 5 | Multigroup model (Unidirectional coupling from SOC to psychopathological symptoms) | 194 | 282.21 | < .001 | .984 | .985 | .034 | 104,899 | 105,130 |
| Model 3 vs. Model 5 | df = 97 | 194.54 | < .001 |
Note. AIC: Akaike Information Criterion, BIC: Bayesian information criterion, CFI: Comparative Fit Index, #pa: number of parameters, df: degrees of freedom, SRMR: Standardized Root-Mean-Square Residual, TLI: Tucker-Lewis Index.
Fig. 3.
Schematic illustration of the final model.
3.4. Unidirectional coupling from SOC to psychopathological symptoms
In the total sample, there was a constant increase in SOC, α = 15.05, z = 4.03, p < .001, and psychopathological symptoms, α = 36.01, z = 3.45, p < .001, along with a proportional change of SOC, β = −0.32, z = −4.04, p < .001, and psychopathological symptoms, β = −0.82, z = −4.11, p < .001. Higher levels of SOC were related to larger constant changes in SOC, and higher psychopathological symptoms levels were associated with larger constant changes in psychopathological symptoms. Constant changes in SOC and psychopathological symptoms were not significantly interrelated. Previous SOC levels predicted later changes in psychopathological symptoms, ɣ SOC→PS= −0.29, z = −1.99, p = .048. Stronger SOC was related to smaller changes in psychopathological symptoms. This translates to the following estimations: For individuals with relatively low levels of SOC (−1 SD) and average levels of pre-outbreak psychopathological symptoms, one would expect psychopathological symptoms to increase by 3.04 (scale range: 72), while for those with relatively strong SOC (+1 SD), one would expect a symptom decrease of −2.93.
3.5. Trajectories of COVID-19-related rumination
Using LGCA we identified two trajectories of COVID-19-related rumination across six waves: A smaller group (n = 254), the high-rumination group, showed consistently high levels of rumination and a larger group, the low-rumination group, showed consistently low levels of rumination (n = 1,149; for details on the LGCA results, see Online Supplementary Material 1). There were no differences between the groups with respect to age, t(1401) = 1.71, p = .088, d = 0.12, gender, χ2(1) = 0.52, p = .470, Cramer's V = 0.02, and educational level, p = .366, r rb = 0.06. However, the high-rumination group displayed higher levels of psychopathological symptoms, F(1, 647) = 275.43, p < .001, ηp = .17, lower sleep quality, F(1, 654) = 17.91, p < .001, ηp = .02, and weaker SOC, F(1, 656) = 66.48, p < .001, ηp = .08, than the low-rumination group. As can be seen in Table 2 , the proportion of participants with above cut-off psychopathological symptoms scores differed between the high- and the low-rumination group ranging from 24.4% (2020/11) to 27.0% (2021/01) in the low-rumination group, and from 53.9% (2020/02) to 59.8% (2020/11) in the high-rumination group, χ2(1) ≥ 101.97, p < .001.
Table 2.
Psychopathological symptoms by COVID-19-related rumination group.
| Assessment period | |||||||
|---|---|---|---|---|---|---|---|
| 2020/02 | 2020/03 | 2020/04 | 2020/08–09 | 2020/11 | 2021/01 | 2021/03 | |
| Low rumination(n) | 1,149 | 1,122 | 998 | 927 | 821 | 902 | 859 |
| n of respondents above cut-off | 239 | 224 | 189 | 173 | 142 | 186 | 159 |
| % respondents above cut-off |
20.8 |
20.0 |
18.9 |
18.7 |
17.3 |
20.6 |
18.5 |
| High rumination(n) | 254 | 245 | 226 | 201 | 164 | 204 | 175 |
| n of respondents above cut-off | 137 | 140 | 135 | 111 | 98 | 113 | 96 |
| % respondents above cut-off |
53.9 |
57.1 |
59.7 |
55.2 |
59.8 |
55.4 |
54.9 |
| Total sample(n) | 1,403 | 1,367 | 1,224 | 1,128 | 985 | 1,106 | 1,034 |
| n of respondents above cut-off | 376 | 364 | 324 | 284 | 240 | 299 | 255 |
| % respondents above cut-off | 26.8 | 26.6 | 26.5 | 25.2 | 24.4 | 27.0 | 24.7 |
Note. Cut-off scores: 10 (men), 13 (women).
3.6. COVID-19-related rumination as moderator
To examine the impact of COVID-19-related rumination on the relationship between SOC and psychopathological symptoms, we compared the BLCS model between high and low rumination groups (see Online Supplementary Material 1). The multigroup model improved model fit significantly, Δχ2(97) = 194.54, p < .001 (see Table 1). In the low-rumination group SOC constantly increased over time, α = 16.75, z = 4.19, p < .001, and SOC changes depended on previous levels of SOC, β = −0.34, z = −4.16, p < .001, while psychopathological symptoms did not show constant or proportional changes, p ≥ .537. In this group there was no coupling between SOC and psychopathological symptoms, ɣ SOC→PS=−.17, z = −0.53, p = .593. In the high-rumination group SOC constantly decreased over time, α = −21.28, z = −2.13, p < .001, and SOC changes depended on previous levels of SOC, β = 0.51, z = 2.07, p < .001. At the same time, psychopathological symptoms increased constantly over time, α = 81.94, z = 2.76, p = .006, and changes depended on previous symptom levels, β = −0.98, z = −3.08, p < .001. In both groups, constant changes in SOC and psychopathological symptoms were not significantly related. In contrast to the low-rumination group, changes in psychopathological symptoms were predicted by previous SOC strength, ɣ SOC→PS= −1.12, z = −2.15, p = .032, in the high-rumination group, that is, stronger SOC was related to smaller changes in psychopathological symptoms. In the high-rumination group, one would expect a symptom increase of 10.51 (scale range: 72) for individuals with low levels of SOC (−1 SD) and average psychopathological symptom burden at pre-outbreak assessment (2020/02), while symptoms would be expected to decrease by 9.78 for individuals with high levels of SOC (+1 SD).
4. Discussion
In this prospective observational study, we found a small yet significant increase of psychopathological symptoms in the general population. However, our multigroup model revealed that mental health consequences of the pandemic were heterogeneous: The majority of the sample (82.8%) did not experience significant changes in psychopathological symptom levels, while symptom increases were pronounced in a subgroup of respondents experiencing high levels of COVID-19-related rumination (17.2% of the total sample). In the total sample and in the high-rumination group, previous SOC significantly predicted changes in psychopathological symptoms at subsequent assessments. Those with stronger SOC at previous assessment were more likely to experience a decrease in symptoms, while those with weaker SOC were at higher risk for an increase in symptoms. Thus, in line with our preliminary analysis during the first wave (Schäfer et al., 2020b), our findings support a buffering effect of SOC.
Our results in the total sample are in line with systematic reviews and meta-analyses on long-term mental health consequences of COVID-19 (Kunzler et al., 2022, 2021; Prati and Mancini, 2021; Robinson et al., 2022) that show a small yet significant increase in psychopathological symptoms in the general population. However, by showing that 82.8% of the sample did experience no changes in psychopathological symptoms, our study also supports the notion that most people will show resilient responses to the pandemic (Chen and Bonanno, 2020; Kunzler et al., 2022). At the same time, our results also underline that there is a vulnerable subgroup that is at risk for clinically meaningful symptoms. These results are accordant with previous research demonstrating that high levels of rumination represent a particularly important transdiagnostic risk factor for the onset of depression and anxiety symptoms in the context of stressful events (McLaughlin and Nolen-Hoeksema, 2011). Correspondingly, ≥ 53.9% of the respondents in the high-rumination group showed above cut-off psychopathological symptom burden (vs. ≤ 2.8% in the low-rumination group). We did not find a constant increase of these shares over time - however shares peaked at the end of the first wave and when case number (newly detected cases per day) started to increase massively during the second wave.
Beyond insights on the impact of COVID-19 on mental health the present study is, to the best of our knowledge, the first to investigate the relationship between SOC and psychopathological symptoms throughout exposure to a global long-term stressor to some extend synchronously affecting all societies. Further, in contrast to previous longitudinal studies on SOC that used regression-based analyses and investigated rather acute or regionally specific stressors (Braun-Lewensohn et al., 2013; Braun-Lewensohn and Sagy, 2010; Engelhard et al., 2003; Hepp et al., 2008; Sairenchi et al., 2011), we examined the association between SOC and psychopathological symptoms by means of bivariate latent change score modeling, allowing to analyze the complex interplay between changes in SOC and psychopathological symptoms. Among the different models examined in the current study, the model allowing for unidirectional coupling from previous SOC to later psychopathological symptoms showed the best model fit. Thereby, SOC is the leading indicator of change in this relationship. This finding does not only corroborate earlier evidence identifying SOC as a predictor of changes in mental health (Engelhard et al., 2003; Schäfer et al., 2020a), but it further points out that SOC has a predictive value over a longer period. Thereby, our results challenge previous conceptual criticism of SOC as to being merely an inverse measure of psychopathological symptoms (Geyer, 1997; Gruszczynska, 2006). Interestingly, SOC's predictive value was particularly pronounced in a group showing high COVID-19-related rumination, higher levels of psychopathological symptoms, lower sleep quality, and weaker SOC. This may suggest that, in line with the salutogenic framework (Antonovsky, 1987, 1979), SOC has its strongest impact on mental health when individuals are exposed to stressors. According to the more recent Positive Appraisal Style Theory of Resilience (Kalisch et al., 2015), resilience factors come into play when aversive situations are strong enough to automatically trigger negative appraisal. In such situations stronger SOC may be associated with more positive reappraisal of the situation. From a regulatory flexibility point of view (Bonanno, 2021; Bonanno and Burton, 2013), it might be interesting to examine whether higher levels of SOC may be associated with greater regulatory flexibility or greater regulatory flexibility is associated with the use of SOC when facing specific contextual demands. Future studies will have to investigate SOC in the context of recent resilience theories and proposed mediating mechanisms.
Interestingly, we found SOC to increase over time in the total sample. This was even more pronounced in the low-rumination subgroup, while the high-rumination group showed a decrease in SOC, which is in line with other research (Braun-Lewensohn et al., 2013; Braun-Lewensohn and Sagy, 2010; Volanen et al., 2007). Thereby, our findings challenge the notion of SOC being a trait-like variable (Antonovsky, 1987, 1979; Schnyder et al., 2000) by showing substantial changes in level of SOC (without any intervention) over a relatively short period of 13 months. Increases in SOC in the total sample and the low-rumination group may reflect stressor-related personal growth that has also been described in other samples during the COVID-19 pandemic (Asmundson et al., 2021; Cheng and Liu, 2022; Vazquez et al., 2021) or gradual adaptation to uncertainty (Korkmaz and Güloğlu, 2021).
Importantly, SOC's instability may not only indicate a theoretical inconsistency within the salutogenesis framework but it may also represent an opportunity for clinical intervention. Given that previous findings show that SOC can be modified by interventions (Breslin et al., 2006; Schäfer et al., 2020a; Vastamaeki et al., 2009), and our results that underline SOC's predictive validity for mental health changes, it seems worthwhile to include SOC in resilience interventions. Resilience can be learned (PeConga et al., 2020; Riehm et al., 2021), and SOC may represent a component that should be targeted more often by resilience trainings that were found to have positive effects in different populations (Kunzler et al., 2020; Liu et al., 2020). Previous evaluations of SOC-targeting interventions in single studies have yielded promising results but often use unspecific interventions (Tan et al., 2016) and insufficient study designs (e.g., single-arm or non-randomized controlled trials; Odajima et al., 2017; Szovák et al., 2020). Future studies should investigate the efficacy of SOC-targeting interventions using more elaborated designs (Chmitorz et al., 2018). Given that a stronger SOC is also predictive of more stable mental health in our study, prevention programs could be useful to buffer adverse effects of future stressors (Pan et al., 2021).
Based on the findings of the current study, future research on SOC may take a multilevel view on resilience. While the present study focused on SOC as individual-level resilience factor, research into family, community or society-level resilience factors may contribute important information to the current state of research. For example, Braun-Lewensohn et al. (2021b) examined the association of community resilience with psychopathological symptoms and anger when Israel was facing the second lockdown. Community resilience was found to be associated with both outcomes even after controlling for sociodemographic variables and hope as individual level resilience factor. This approach is in line with other calls to take an ecological and systems perspective on resilience (Ioannidis et al., 2020). In case of salutogenesis, an assessment of community SOC has already been proposed and should be used in future studies to examine multilevel resilience factors (Elfassi et al., 2016). Such studies may make use of advances in psychological network modeling to examine the complex interplay between individual- and community-level resilience factors (Fritz et al., 2019, 2018).
4.1. Limitations
It is important to consider the limitations of the current study: First, the study used a nonrepresentative sample recruited online (WiSo panel; Göritz et al., 2021); and was observational. Therefore, we cannot exclude that changes in mental health found in the present study were not related to the COVID-19 pandemic, but reflected spontaneous fluctuations over time or seasons (Øverland et al., 2020), as we do not have a long-term pre-pandemic assessment of the sample. Moreover, a substantial number of respondents dropped out during the study (n = 658 completed all assessments). However, missing data was at least at random, and we aimed to account for potential biases by dropout analyses. Second, we conceptualized the COVID-19 pandemic as relatively homogeneous global chronic stressor and did not assess individual pandemic-related stressor exposure, as this was hampered by the dynamic course of the pandemic (i.e., as governmental policy and measures to contain the pandemic changed dynamically, also stressor assessment would have changed between assessments, which is not ideal for longitudinal data analyses). To account for individual differences in stressor exposure as best as possible, we included COVID-19-related rumination as an indicator of stress in our analyses. However, this does not compensate the lack of precise stressor assessment and future studies examining less dynamic stressors should include such assessments focusing on both objective and subjectively perceived stressor exposure (Kalisch et al., 2021). Such studies may also provide an opportunity to examine whether the importance of SOC differs between stressors (e.g., bereavement, job loss) and/or depends on the severity of stressor exposure. Research into (mis)matches between resilience factors, coping strategies and contextual demands would tie in with recent advances in resilience research (Bonanno, 2021) and add a flexibility perspective to research into salutogenesis.
5. Conclusions
Despite these limitations, the current study improves our understanding of the interaction between the resilience factor SOC and mental health during the COVID-19 pandemic. We found a small, yet significant increase of psychopathological symptoms in the total sample and identified a subgroup of respondents (17.2%) characterized by high COVID-19-related rumination, high levels of psychopathological symptoms and weaker SOC that was particularly burdened by the pandemic. In this subgroup, and in the total sample, previous levels of SOC were predictive of later changes in psychopathological symptoms. A stronger SOC was associated with smaller changes and a greater chance to experience symptom decreases over time. This predictive value hopefully inspires further research into mechanisms linking SOC and psychopathological symptoms and into interventions fostering resilience.
Author contributions
SKS: conceptualization (lead), formal analysis (lead), methodology (lead), writing – original draft preparation; MRS: conceptualization (supporting), methodology, writing – review and editing (equal); MK: formal analysis (supporting), methodology (supporting), visualization, writing – review and editing (equal); ASG: data curation, project administration, resources (lead), supervision (supporting), writing – review and editing (equal); TM: conceptualization (supporting), resources (supporting), supervision (lead), writing – review and editing (equal).
Role of the funding source
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Declaration of competing interest
All authors declare to have no conflict of interest.
Acknowledgments
The authors thank the Project RESPOND team for discussing the findings of our study. The Project RESPOND is funded by the EU RIA-call H2020-SC1-PHE474 CORONAVIRUS-2020-2-RTD (Grant number 101016127).
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.jpsychires.2022.07.004.
Appendix A. Supplementary data
The following are the Supplementary data to this article:
References
- Ahrens K.F., Neumann R.J., Kollmann B., Brokelmann J., von Werthern N.M., Malyshau A., Weichert D., Lutz B., Fiebach C.J., Wessa M., Kalisch R., Plichta M.M., Lieb K., Tüscher O., Reif A. Impact of COVID-19 lockdown on mental health in Germany: longitudinal observation of different mental health trajectories and protective factors. Transl. Psychiatry. 2021;11:392. doi: 10.1038/s41398-021-01508-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Antonovsky A. The structure and properties of the sense of coherence scale. Soc. Sci. Med. 1993;36:725–733. doi: 10.1016/0277-9536(93)90033-z. [DOI] [PubMed] [Google Scholar]
- Antonovsky A. The Jossey-Bass social and behavioral science series and the Jossey-Bass health series. Jossey-Bass; San Francisco, CA, US: 1987. Unraveling the Mystery of Health: How People Manage Stress and Stay Well. [Google Scholar]
- Antonovsky A. Jossey-Bass; San Francisco, CA, US: 1979. Health, Stress, and Coping. [Google Scholar]
- Asmundson G.J.G., Paluszek M.M., Taylor S. Real versus illusory personal growth in response to COVID-19 pandemic stressors. J. Anxiety Disord. 2021;81 doi: 10.1016/j.janxdis.2021.102418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Banerjee D., Rai M. Social isolation in Covid-19: the impact of loneliness. Int. J. Soc. Psychiatr. 2020;66:525–527. doi: 10.1177/0020764020922269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bechtold S. The 2011 census model in Germany. Comparative Population Studies-Zeitschrift für Bevölkerungswissenschaft. 2016;41:D1–D9. [Google Scholar]
- Bonanno G.A. The resilience paradox. Eur. J. Psychotraumatol. 2021;12 doi: 10.1080/20008198.2021.1942642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bonanno G.A., Burton C.L. Regulatory flexibility: an individual differences perspective on coping and emotion regulation. Perspect. Psychol. Sci. 2013;8:591–612. doi: 10.1177/1745691613504116. [DOI] [PubMed] [Google Scholar]
- Braun-Lewensohn O., Abu-Kaf S., Kalagy T. Hope and resilience during a pandemic among three cultural groups in Israel: the second wave of covid-19. Front. Psychol. 2021;12:340. doi: 10.3389/fpsyg.2021.637349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Braun-Lewensohn O., Abu-Kaf S., Kalagy T. What factors explain anger and mental health during the COVID-19 pandemic? The case of Israeli society. World J. Psychiatr. 2021;11:864. doi: 10.5498/wjp.v11.i10.864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Braun‐Lewensohn O., Sagy S. Sense of coherence, hope and values among adolescents under missile attacks: a longitudinal study. Int J Child Spirituality. 2010;15:247–260. [Google Scholar]
- Braun-Lewensohn O., Sagy S., Sabato H., Galili R. Sense of coherence and sense of community as coping resources of religious adolescents before and after the disengagement from the Gaza Strip. Isr Ann Psychiatr Relat Discip. 2013;50:110–116. [PubMed] [Google Scholar]
- Breslin F.C., Hepburn C.G., Ibrahim S., Cole D. Understanding stability and change in psychological distress and sense of coherence: a four-year prospective study. J. Appl. Soc. Psychol. 2006;36:1–21. [Google Scholar]
- Chen S., Bonanno G.A. Psychological adjustment during the global outbreak of COVID-19: a resilience perspective. Psychol Trauma. 2020;12:S51–S54. doi: 10.1037/tra0000685. [DOI] [PubMed] [Google Scholar]
- Cheng L., Liu L. Exploring posttraumatic growth after the COVID-19 pandemic. Tourism Manag. 2022;90 doi: 10.1016/j.tourman.2021.104474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chmitorz A., Kunzler A., Helmreich I., Tuescher O., Kalisch R., Kubiak T., Wessa M., Lieb K. Intervention studies to foster resilience - a systematic review and proposal for a resilience framework in future intervention studies. Clin. Psychol. Rev. 2018;59:78–100. doi: 10.1016/j.cpr.2017.11.002. [DOI] [PubMed] [Google Scholar]
- Dong E., Du H., Gardner L. An interactive web-based dashboard to track COVID-19 in real time. Lancet Infect. Dis. 2020;20:533–534. doi: 10.1016/S1473-3099(20)30120-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ehnts D., Paetz M. COVID-19 and its economic consequences for the Euro Area. Eurasian Econ Rev. 2021;11:227–249. [Google Scholar]
- Ehring T., Zetsche U., Weidacker K., Wahl K., Schönfeld S., Ehlers A. The Perseverative Thinking Questionnaire (PTQ): validation of a content-independent measure of repetitive negative thinking. J. Behav. Ther. Exp. Psychiatr. 2011;42:225–232. doi: 10.1016/j.jbtep.2010.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elfassi Y., Braun-Lewensohn O., Krumer-Nevo M., Sagy S. Community sense of coherence among adolescents as related to their involvement in risk behaviors. J. Community Psychol. 2016;44:22–37. [Google Scholar]
- Engelhard I.M., van den Hout M.A., Vlaeyen J.W. The sense of coherence in early pregnancy and crisis support and posttraumatic stress after pregnancy loss: a prospective study. Behav. Med. 2003;29:80–84. doi: 10.1080/08964280309596060. [DOI] [PubMed] [Google Scholar]
- Eriksson M., Lindström B. Antonovsky's sense of coherence scale and the relation with health: a systematic review. J. Epidemiol. Community Health. 2006;60:376–381. doi: 10.1136/jech.2005.041616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fairholme C.P., Nosen E.L., Nillni Y.I., Schumacher J.A., Tull M.T., Coffey S.F. Sleep disturbance and emotion dysregulation as transdiagnostic processes in a comorbid sample. Behav. Res. Ther. 2013;51:540–546. doi: 10.1016/j.brat.2013.05.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Finney S.J., DiStefano C. In: Structural Equation Modeling. Hancock G.r., Mueller R.O., editors. Information Age Publishing; Greenwich, CT, US: 2006. Non-normal and categorical data in structural equation modeling; pp. 269–314. [Google Scholar]
- Flesia L., Monaro M., Mazza C., Fietta V., Colicino E., Segatto B., Roma P. Predicting perceived stress related to the covid-19 outbreak through stable psychological traits and machine learning models. J. Clin. Med. 2020;9:3350. doi: 10.3390/jcm9103350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flett G.L., Madorsky D., Hewitt P.L., Heisel M.J. Perfectionism cognitions, rumination, and psychological distress. J. Ration. Emot. Cogn. Behav. Ther. 2002;20:33–47. [Google Scholar]
- Fossion P., Leys C., Kempenaers C., Braun S., Verbanck P., Linkowski P. Disentangling sense of coherence and resilience in case of multiple traumas. J. Affect. Disord. 2014:21–26. doi: 10.1016/j.jad.2014.02.029. [DOI] [PubMed] [Google Scholar]
- Franke G. Hogrefe Publishing Group; Germany: 2017. BSCL-53®-S. Brief Symptom-Checklist–Standard–Deutsches Manual. Göttingen. [Google Scholar]
- Franke G.H., Jaeger S., Glaesmer H., Barkmann C., Petrowski K., Braehler E. Psychometric analysis of the brief symptom inventory 18 (BSI-18) in a representative German sample. BMC Med. Res. Methodol. 2017;17:14. doi: 10.1186/s12874-016-0283-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Franke G.H., Jäger S., Morfeld M., Salewski C., Reimer J., Rensing A., Witzke O., Türk T. Eignet sich das BSI-18 zur Erfassung der psychischen Belastung von nierentransplantierten Patienten? Z. Med. Psychol. 2010;19:30–37. [Google Scholar]
- Fritz J., Fried E.I., Goodyer I.M., Wilkinson P.O., van Harmelen A.-L. A network model of resilience factors for adolescents with and without exposure to childhood adversity. Sc Rep. 2018;8 doi: 10.1038/s41598-018-34130-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fritz J., Stochl J., Fried E.I., Goodyer I.M., van Borkulo C.D., Wilkinson P.O., van Harmelen A.-L. Unravelling the complex nature of resilience factors and their changes between early and later adolescence. BMC Med. 2019;17:203. doi: 10.1186/s12916-019-1430-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Geyer S. Some conceptual considerations on the sense of coherence. Soc. Sci. Med. 1997;44:1771–1779. doi: 10.1016/s0277-9536(96)00286-9. [DOI] [PubMed] [Google Scholar]
- Göritz A.S., Borchert K., Hirth M. Using attention testing to select crowdsourced workers and research participants. Soc. Sci. Comput. Rev. 2021;39:84–104. [Google Scholar]
- Grimm K.J., Ram N., Estabrook R. Guilford Publications; New York, NY, US: 2016. Growth Modeling: Structural Equation and Multilevel Modeling Approaches. [Google Scholar]
- Gruszczynska E. What is measured by the orientation to life Questionnaire? Construct validity of the instrument for the sense of coherence measurement. Pol. Psychol. Bull. 2006;37:74–83. [Google Scholar]
- Hale T., Angrist N., Goldszmidt R., Kira B., Petherick A., Phillips T., Tatlow H. A global panel7 database of pandemic policies (Oxford COVID-19 Government Response Tracker) Nat. Human Behav. 2021;5(4):529–538. doi: 10.1038/s41562-021-01079-8. [DOI] [PubMed] [Google Scholar]
- Harvey A.G., Murray G., Chandler R.A., Soehner A. Sleep disturbance as transdiagnostic: consideration of neurobiological mechanisms. Clin. Psychol. Rev. 2011;31:225–235. doi: 10.1016/j.cpr.2010.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hepp U., Moergeli H., Büchi S., Bruchhaus-Steinert H., Kraemer B., Sensky T., Schnyder U. Post-traumatic stress disorder in serious accidental injury: 3-year follow-up study. Br. J. Psychiatry. 2008;192:376–383. doi: 10.1192/bjp.bp.106.030569. [DOI] [PubMed] [Google Scholar]
- Horn S.R., Charney D.S., Feder A. Understanding resilience: new approaches for preventing and treating PTSD. Exp. Neurol. 2016;284:119–132. doi: 10.1016/j.expneurol.2016.07.002. [DOI] [PubMed] [Google Scholar]
- Ioannidis K., Askelund A.D., Kievit R.A., van Harmelen A.-L. The complex neurobiology of resilient functioning after childhood maltreatment. BMC Med. 2020;18:32. doi: 10.1186/s12916-020-1490-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jajodia A. In: Longitudinal Data Analysis: A Practical Guide for Researchers in Aging, Health, and Social Sciences. Newsom J.T., Jones R.N., Hofer S.M., editors. Routledge/Taylor & Francis Group; London, UK: 2012. Dynamic structural equation models of change; pp. 291–328. [Google Scholar]
- Kalisch, R., Cramer, A.O.J., Binder, H., Fritz, J., Leertouwer, Ij, Lunansky, G., Meyer, B., Timmer, J., Veer, I.M., van Harmelen, A.-L., 2019. Deconstructing and reconstructing resilience: a dynamic network approach. Perspect. Psychol. Sci. 14, 765–777. [DOI] [PubMed]
- Kalisch R., Köber G., Binder H., Ahrens K.F., Basten U., Chmitorz A., Choi K.W., Fiebach C.J., Goldbach N., Neumann R.J., Kampa M., Kollmann B., Lieb K., Plichta M.M., Reif A., Schick A., Sebastian A., Walter H., Wessa M., Yuen K.S.L., Tüscher O., Engen H. The frequent stressor and mental health monitoring-paradigm: a proposal for the operationalization and measurement of resilience and the identification of resilience processes in longitudinal observational studies. Front. Psychol. 2021;12 doi: 10.3389/fpsyg.2021.710493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kalisch R., Müller M.B., Tüscher O. A conceptual framework for the neurobiological study of resilience. Behav. Brain Sci. 2015;38:e92. doi: 10.1017/S0140525X1400082X. [DOI] [PubMed] [Google Scholar]
- Kievit R.A., Brandmaier A.M., Ziegler G., Van Harmelen A.-L., de Mooij S.M., Moutoussis M., Goodyer I.M., Bullmore E., Jones P.B., Fonagy P. Developmental cognitive neuroscience using latent change score models: a tutorial and applications. Dev Cogn Neurosci. 2018;33:99–117. doi: 10.1016/j.dcn.2017.11.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Korkmaz H., Güloğlu B. The role of uncertainty tolerance and meaning in life on depression and anxiety throughout Covid-19 pandemic. Pers. Indiv. Differ. 2021;179 doi: 10.1016/j.paid.2021.110952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kovács L.N., Baksa D., Dobos D., Eszlári N., Gecse K., Kocsel N., Juhász G., Kökönyei G. Perceived stress in the time of COVID-19: the association with brooding and COVID-related rumination in adults with and without migraine. BMC Psychol. 2021;9:68. doi: 10.1186/s40359-021-00549-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kunzler A., Helmreich I., Chmitorz A., König J., Binder H., Wessa M., Lieb K. Psychological interventions to foster resilience in healthcare professionals. Cochrane Database Syst. Rev. 2020;7 doi: 10.1002/14651858.CD012527.pub2. CD012527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kunzler A., Schäfer S.K., Kalisch R., Tüscher O., Lieb K. 2022. Trajectories of Resilience and Mental Distress to Global Major Disruptions. Manuscript under revision. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kunzler A.M., Röthke N., Günthner L., Stoffers-Winterling J., Tüscher O., Coenen M., Rehfuess E., Schwarzer G., Binder H., Schmucker C., Meerpohl J.J., Lieb K. Mental burden and its risk and protective factors during the early phase of the SARS-CoV-2 pandemic: systematic review and meta-analyses. Glob. Health. 2021;17:34. doi: 10.1186/s12992-021-00670-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leiner D.J. 2019. SoSci Survey.http://www.soscisurvey.com [Computer software]. Available at. [Google Scholar]
- Little R.J.A. A test of missing completely at random for multivariate data with missing values. J. Am. Stat. Assoc. 1988;83:1198–1202. [Google Scholar]
- Liu J.J.W., Ein N., Gervasio J., Battaion M., Reed M., Vickers K. Comprehensive meta-analysis of resilience interventions. Clin. Psychol. Rev. 2020;82 doi: 10.1016/j.cpr.2020.101919. [DOI] [PubMed] [Google Scholar]
- Mana A., Bauer G.F., Meier Magistretti C., Sardu C., Juvinyà-Canal D., Hardy L.J., Catz O., Tušl M., Sagy S. Order out of chaos: sense of coherence and the mediating role of coping resources in explaining mental health during COVID-19 in 7 countries. SSM – Ment Health. 2021;1 doi: 10.1016/j.ssmmh.2021.100001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLaughlin K.A., Nolen-Hoeksema S. Rumination as a transdiagnostic factor in depression and anxiety. Behav. Res. Ther. 2011;49:186–193. doi: 10.1016/j.brat.2010.12.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mittelmark M.B., Bauer G.F. In: 11–17, the Handbook of Salutogenesis. Mittelmark M.B., Bauer G.F., Vaandrager L., Pelikan J.P., Sagy S., Eriksson M., Lindström B., Meier Magistretti C., editors. Springer; New York, NY, US: 2022. Salutogenesis as a theory, as an orientation and as the sense of coherence. [PubMed] [Google Scholar]
- Muthén L.K., Muthén B. Mplus user's guide: statistical analysis with latent variables, user's guide. 2017. https://www.statmodel.com/download/usersguide/MplusUserGuideVer_8.pdf Available from.
- Nicola M., Alsafi Z., Sohrabi C., Kerwan A., Al-Jabir A., Iosifidis C., Agha M., Agha R. The socio-economic implications of the coronavirus pandemic (COVID-19): a review. Int. J. Surg. 2020;78:185–193. doi: 10.1016/j.ijsu.2020.04.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nikolova I., Caniëls M.C.J., Curseu P.L. COVID-19 Rumination Scale (C-19RS): initial psychometric evidence in a sample of Dutch employees. Int. J. Health Plann. Manag. 2021;36:1166–1177. doi: 10.1002/hpm.3165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Odajima Y., Kawaharada M., Wada N. Development and validation of an educational program to enhance sense of coherence in patients with diabetes mellitus type 2. Nagoya J. Med. Sci. 2017;79:363–374. doi: 10.18999/nagjms.79.3.363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Øverland S., Woicik W., Sikora L., Whittaker K., Heli H., Skjelkvåle F.S., Sivertsen B., Colman I. Seasonality and symptoms of depression: a systematic review of the literature. Epidemiol. Psychiatr. Sci. 2020;29:e31. doi: 10.1017/S2045796019000209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pan K.-Y., Kok A.A.L., Eikelenboom M., Horsfall M., Jörg F., Luteijn R.A., Rhebergen D., Oppen P. van, Giltay E.J., Penninx B.W.J.H. The mental health impact of the COVID-19 pandemic on people with and without depressive, anxiety, or obsessive-compulsive disorders: a longitudinal study of three Dutch case-control cohorts. Lancet Psychiatr. 2021;8:121–129. doi: 10.1016/S2215-0366(20)30491-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- PeConga E.K., Gauthier G.M., Holloway A., Walker R.S.W., Rosencrans P.L., Zoellner L.A., Bedard-Gilligan M. Resilience is spreading: mental health within the COVID-19 pandemic. Psychol Trauma. 2020;12:S47–S48. doi: 10.1037/tra0000874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pfefferbaum B., North C.S. Mental health and the covid-19 pandemic. N. Engl. J. Med. 2020;383:510–512. doi: 10.1056/NEJMp2008017. [DOI] [PubMed] [Google Scholar]
- Prati G., Mancini A.D. The psychological impact of COVID-19 pandemic lockdowns: a review and meta-analysis of longitudinal studies and natural experiments. Psychol. Med. 2021;51:201–211. doi: 10.1017/S0033291721000015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Riehm K.E., Brenneke S.G., Adams L.B., Gilan D., Lieb K., Kunzler A.M., Smail E.J., Holingue C., Stuart E.A., Kalb L.G., Thrul J. Association between psychological resilience and changes in mental distress during the COVID-19 pandemic. J. Affect. Disord. 2021;282:381–385. doi: 10.1016/j.jad.2020.12.071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robinson E., Sutin A.R., Daly M., Jones A. A systematic review and meta-analysis of longitudinal cohort studies comparing mental health before versus during the COVID-19 pandemic in 2020. J. Affect. Disord. 2022;296:567–576. doi: 10.1016/j.jad.2021.09.098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosseel Y. Lavaan: an R package for structural equation modeling. J. Stat. Software. 2012;48:1–36. [Google Scholar]
- Rouzinov S., Berchtold A. Package RBtest. 2020. https://cran.r-project.org/web/packages/RBtest/RBtest.pdf Available from.
- RStudio Team . PBC; Boston, MA: 2020. RStudio: Integrated Development for R. RStudio.http://www.rstudio.com/ URL. [Google Scholar]
- Sairenchi T., Haruyama Y., Ishikawa Y., Wada K., Kimura K., Muto T. Sense of coherence as a predictor of onset of depression among Japanese workers: a cohort study. BMC Publ. Health. 2011;11:205. doi: 10.1186/1471-2458-11-205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schäfer S.K., Becker N., King L., Horsch A., Michael T. The relationship between sense of coherence and post-traumatic stress: a meta-analysis. Eur. J. Psychotraumatol. 2019;10 doi: 10.1080/20008198.2018.1562839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schäfer S.K., Lass-Hennemann J., Groesdonk H., Volk T., Bomberg H., Staginnus M., Brueckner A.H., Holz E., Michael T. Mental health in anesthesiology and ICU staff: sense of coherence matters. Front. Psychiatr. 2018;9:440. doi: 10.3389/fpsyt.2018.00440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schäfer S.K., Schanz C.G., Sopp M.R., Lass-Hennemann J., Käfer M., Michael T. Pre-rehabilitation sense of coherence as a predictor of symptom change during rehabilitation. Stress Health. 2020;36:546–554. doi: 10.1002/smi.2949. [DOI] [PubMed] [Google Scholar]
- Schäfer S.K., Sopp M.R., Schanz C.G., Staginnus M., Göritz A.S., Michael T. Impact of COVID-19 on public mental health and the buffering effect of a sense of coherence. Psychother. Psychosom. 2020;89:386–392. doi: 10.1159/000510752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schäfer S.K., Sopp M.R., Koch M., Göritz A.S., Michael T. The long-term buffering effect of sense of coherence on psychopathological symptoms during the first year of the COVID-19 pandemic: A prospective observational study. J. Psychiatr. Res. 2022 doi: 10.1016/j.jpsychires.2022.07.004. Retrieved from osf.io/h5vky. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schermelleh-Engel K., Moosbrugger H., Müller H., others Evaluating the fit of structural equation models: tests of significance and descriptive goodness-of-fit measures. Meth Psychol Res. 2003;8:23–74. [Google Scholar]
- Schmuck J., Hiebel N., Rabe M., Schneider J., Erim Y., Morawa E., Jerg-Bretzke L., Beschoner P., Albus C., Hannemann J., Weidner K., Steudte-Schmiedgen S., Radbruch L., Brunsch H., Geiser F. Sense of coherence, social support and religiosity as resources for medical personnel during the COVID-19 pandemic: a web-based survey among 4324 health care workers within the German Network University Medicine. PLoS One. 2021;16 doi: 10.1371/journal.pone.0255211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schnyder U., Büchi S., Sensky T., Klaghofer R. Antonovsky's sense of coherence: trait or state? Psychother. Psychosom. 2000;69:296–302. doi: 10.1159/000012411. [DOI] [PubMed] [Google Scholar]
- Şimşir Z., Koç H., Seki T., Griffiths M.D. The relationship between fear of COVID-19 and mental health problems: a meta-analysis. Death Stud. 2022;46:515–523. doi: 10.1080/07481187.2021.1889097. [DOI] [PubMed] [Google Scholar]
- Singer S., Brähler E. Vandenhoeck & Ruprecht; Göttingen, Germany: 2007. Die»Sense of Coherence Scale«: Testhandbuch zur deutschen Version. [Google Scholar]
- Snyder E., Cai B., DeMuro C., Morrison M.F., Ball W. A new single-item sleep quality scale: results of psychometric evaluation in patients with chronic primary insomnia and depression. J. Clin. Sleep Med. 2018;14:1849–1857. doi: 10.5664/jcsm.7478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stratton S.J. COVID-19: not a simple public health emergency. Prehospital Disaster Med. 2020;35 doi: 10.1017/S1049023X2000031X. 119–119. [DOI] [PubMed] [Google Scholar]
- Streb M., Häller P., Michael T. PTSD in paramedics: resilience and sense of coherence. Behav. Cognit. Psychother. 2014;42:452–463. doi: 10.1017/S1352465813000337. [DOI] [PubMed] [Google Scholar]
- Szovák E., Varga K., Pelyva I.Z., Soós R., Jeges S., Kívés Z., Tóth Á.L. Insights gained in the aftermath of the COVID-19 pandemic: a follow-up survey of a recreational training program, focusing on sense of coherence and sleep quality. Int. J. Environ. Res. Publ. Health. 2020;17:9201. doi: 10.3390/ijerph17249201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tan K.K., Chan S.W.-C., Wang W., Vehviläinen-Julkunen K. A salutogenic program to enhance sense of coherence and quality of life for older people in the community: a feasibility randomized controlled trial and process evaluation. Patient Educ. Counsel. 2016;99:108–116. doi: 10.1016/j.pec.2015.08.003. [DOI] [PubMed] [Google Scholar]
- Tanaka K., Tahara M., Mashizume Y., Takahashi K. Effects of lifestyle changes on the mental health of healthcare workers with different sense of coherence levels in the era of COVID-19 pandemic. Int. J. Environ. Res. Publ. Health. 2021;18:2801. doi: 10.3390/ijerph18062801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van de Schoot R., Sijbrandij M., Winter S.D., Depaoli S., Vermunt J.K. The GRoLTS-checklist: guidelines for reporting on latent trajectory studies. Struct. Equ. Model. 2017;24:451–467. [Google Scholar]
- Vanderhasselt M.-A., Brose A., Koster E.H.W., De Raedt R. Co-variation between stressful events and rumination predicts depressive symptoms: an eighteen months prospective design in undergraduates. Behav. Res. Ther. 2016;87:128–133. doi: 10.1016/j.brat.2016.09.003. [DOI] [PubMed] [Google Scholar]
- Vastamaeki J., Moser K., Paul K.I. How stable is sense of coherence? Changes following an intervention for unemployed individuals. Scand. J. Psychol. 2009;50:161–171. doi: 10.1111/j.1467-9450.2008.00695.x. [DOI] [PubMed] [Google Scholar]
- Vazquez C., Valiente C., García F.E., Contreras A., Peinado V., Trucharte A., Bentall R.P. Post-Traumatic growth and stress-related responses during the COVID-19 pandemic in a national representative sample: the role of positive core beliefs about the world and others. J. Happiness Stud. 2021;22:2915–2935. doi: 10.1007/s10902-020-00352-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Volanen S.M., Suominen S., Lahelma E., Koskenvuo M., Silventoinen K. Negative life events and stability of sense of coherence: a five-year follow-up study of Finnish women and men. Scand. J. Psychol. 2007;48:433–441. doi: 10.1111/j.1467-9450.2007.00598.x. [DOI] [PubMed] [Google Scholar]
- Zabora J., Brintzenhofeszoc K., Jacobsen P., Curbow B., Piantadosi S., Hooker C., Owens A., Derogatis L. A new psychosocial screening instrument for use with cancer patients. Psychosomatics. 2001;42:241–246. doi: 10.1176/appi.psy.42.3.241. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.