Summary
Background
This evaluation of doula care emerges at a time when maternal mortality in the U.S. outranks every country in the developed world. Study objectives were to: 1) examine when over the maternity care continuum and with whom (i.e., clinical providers) doula care provides the greatest benefits to clinical health outcomes and health care utilization; and 2) evaluate whether women gain differential benefits from doulas depending upon race/ethnicity and health status.
Methods
We conducted a retrospective cohort study using Medicaid medical claims from California, Florida, and a northeastern state (USA) to compare maternal health outcomes between women who did and did not receive doula care between January 1, 2014 and December 31, 2020. We used propensity score matching and logistic regression models to calculate associations between selected health outcomes and doula care. Our analysis included 298 pairs of women matched on age, race/ethnicity, state, socioeconomic status, and hospital type (teaching or non-teaching).
Findings
Women who received doula care had 52.9% lower odds of cesarean delivery (OR: 0.471 95% CI: 0.29–0.79) and 57.5% lower odds of postpartum depression/postpartum anxiety (PPD/PPA) (OR: 0.425 95% CI: 0.22–0.82). Doulas who provided care with a clinical team that included a midwife most consistently showed a reduction in odds of cesarean delivery, regardless of the trimester when doula care was received. Women who received doula care during labor and birth, but not necessarily during pregnancy, showed a 64.7% reduction in odds of PPA/PPD (OR: 0.353 95% CI: 0.16–0.78) of PPA/PPD.
Interpretation
The use of doulas appears an effective strategy for improving maternal health, especially among socioeconomically vulnerable and marginalized minority populations. Future studies could address research gaps through focusing on the relationship between doula care received in the postpartum period and postpartum health.
Funding
No sources of funding were used to assist in the preparation of this manuscript. Research was completed as part of the usual employment obligations to Anthem, Inc.
Keywords: Doulas, Maternal health, Medicaid, Maternal morbidity
Research in context.
Evidence before this study
Doula care has received increasing attention recently as a promising, yet underutilized, strategy for advancing maternal health equity. We searched PubMed and Google Scholar to investigate the available evidence on the association between doulas and health outcomes between Jan 1, 2002 and Jan 1, 2022. Our search terms included the following: “doula” AND “maternal health” OR (“maternal” AND “health”) OR “women's health” OR “pregnancy.” We identified 199 unique studies, including two randomized controlled trials and one Cochrane review on “continuous support for women during childbirth.” Of these records, 26 publications included either a review or an empirical investigation of the association of doula care with maternal health. Studies were mostly descriptive in nature and often extracted data from surveys, interviews, and focus groups. With the exception of the RCTs, most studies did not account for selection bias. Although the significance of associations between doulas and health outcomes varied by study, results converged on the association between doula care and reduction in cesarean delivery.
Added value of this study
Our analytical methods and data source were relatively unique attributes that strengthened the methodological rigor of our study. To our knowledge, only one other study has used PSM to address the issue of selection bias. Our utilization of medical claims data was another relatively unique methodological attribute of our study, which helped us minimize the potentially confounding effects of reporting bias. Only one other study that we know of has relied upon claims data in their analysis of doulas and maternal health. Claims data also enabled us to assess the impact of provider-related factors and evaluate the timing in which health utilization and events occurred, which hasn't previously been investigated in the study of doula care and maternal health. Our findings indicate, in sum, that women who received doula care showed lower odds of cesarean section and of postpartum depression or anxiety, relative to women with similar sociodemographic and clinical characteristics but with no doula care. We found, however, that the timing in which doula care and the clinical team doulas interacted with affected the magnitude and significance of these statistical associations.
Implications of all the available evidence
Evidence collectively suggests that doulas can decrease risk of adverse maternal health outcomes, particularly among women whose sociodemographic and clinical characteristics place them at higher risk for maternal morbidity and mortality. Although further research is needed to explore the effects of race and cultural competence on the relationship between doulas and maternal health outcomes, our study findings suggest that integrating doulas into maternity care may help reduce maternal health disparities.
Alt-text: Unlabelled box
Introduction
Black women have faced longstanding challenges in improving maternal health equity. Race disparities have been documented in maternal morbidity and mortality since 1935, when national public health legislation (Title V of the Social Security Act) was implemented to improve the health for all mothers.1 While disparities have decreased over time, contemporary data show that Black women are still 1.3 times more likely to experience severe pregnancy complications and three times more likely to die from pregnancy and childbirth compared to White women.2,3 Black women are also twice as likely to experience postpartum depressive symptoms relative to White women, which is noteworthy because almost 10% of pregnancy-related deaths are due to mental health conditions.4,5 Research has previously implicated socioeconomic status (SES) for racial health disparities,6,7 but the influence of race on maternal health appears unique and independent of social and economic factors.8
The disparity in pregnancy-related mortality between Black and White women, for example, remains not only after adjusting for such factors as education, the gap widens with increasing education. Black women with a college education or higher have over five times the risk of maternal mortality compared to White women with the same educational attainment. Black women with less than a high school diploma, however, have a 1.6 times higher rate of pregnancy-related mortality relative to similarly educated White women.9 Research also has demonstrated the relationship between insurance status and maternal health, but the odds of severe maternal morbidity is approximately 1.5 times higher for Black women regardless of their insurance status (e.g., commercial insurance, Medicaid).10
The persistence and complexity of racial/ethnic disparities in maternal health can make efforts to reduce disparities appear Herculean at best and Sisyphean at worst. Members of the National Council on Patient Safety in Women's Health Care suggest, however, that some risk factors are modifiable and could reduce maternal health disparities if addressed at a systems level.11 In their Patient Safety Bundle for the Reduction of Peripartum Racial and Ethnic Disparities, the Council emphasized the importance of improving patient-provider communication to remediate disparities in maternal health. Effective communication is vital for quality care and patient safety, but it can be hampered by various barriers, including language differences between patient and provider, implicit bias, and lack of cultural competency.11
Research suggests that doulas, trained professionals who provide physical, emotional, and informational support to mothers during pregnancy, childbirth, and postpartum,12 can reduce health disparities through facilitating communication and serving as intermediaries between pregnant women and their providers. Studies show that doulas mitigate the pervasive influence of social determinants of health for at-risk pregnant women,13 and research has linked doula care utilized by socioeconomically vulnerable women with a reduction in odds of cesarean section, preterm birth, and low birthweight babies.14, 15, 16, 17
A growing amount of evidence has begun to converge on the association between doula care and improvements to maternal health. Evaluations have minimally explored, however, the contextual factors related to the broader health services environment in which doulas operate. No studies have demonstrated, for example, how timing or quantity of doula services received affects odds of health outcomes previously established in the literature. We evaluated a national insurer's pilot programs to provide doula services to Medicaid women in a county in central California; women in a county in a state in the Northeast; and women throughout the state of Florida (USA). These doula programs are unique because they provide coverage for women who traditionally would have financial difficulty accessing doula care. Additionally, these programs have integrated efforts from community-based organizations to enroll women at higher risk for adverse maternal health outcomes due to their sociodemographic characteristics and their health conditions.
The objectives of this study were to: 1) evaluate the integration of doulas with different types of clinical providers during labor and delivery to understand how different combinations of provision of care relate to maternal health outcomes; 2) assess when, over the care continuum (from the first trimester through childbirth), doulas provide the greatest benefit to maternal health; and 3) evaluate whether women gain differential benefits from doulas depending upon certain risk factors, including race/ethnicity and certain chronic conditions.
Methods
Study design and data
We conducted a retrospective cohort study using claims data from the HealthCore Integrated Research Database (HIRD). The HIRD contains medical and pharmacy claims from a large, commercial health insurer that is geographically dispersed across the United States. This study was conducted in compliance with the Health Insurance Portability and Affordability Act. Patient consent was not required because only de-identified data was used, and the study was exempt from review by an Institutional Review Board.
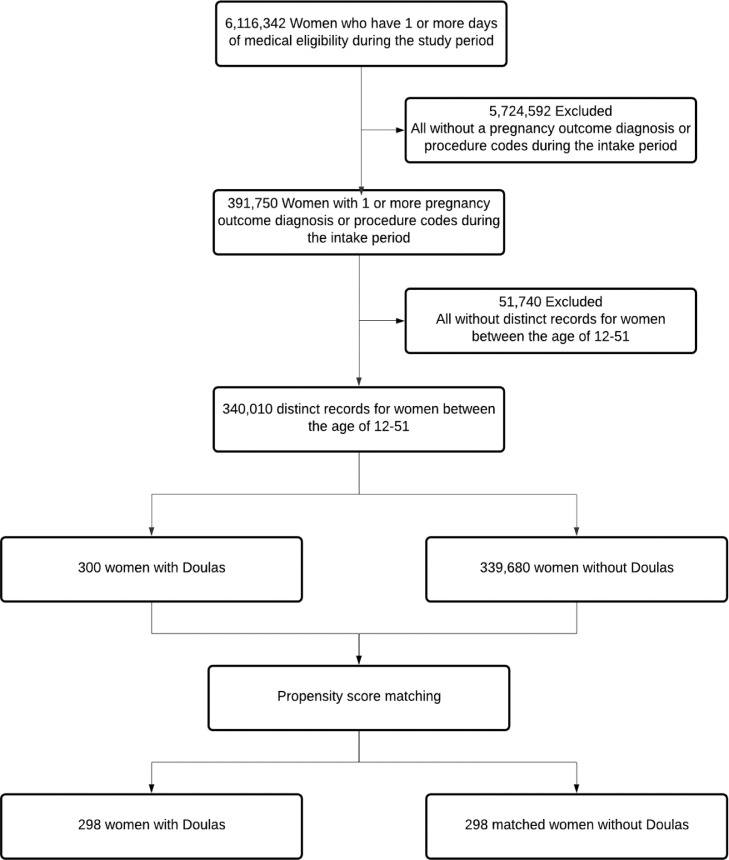
Our study population was comprised of 340,010 expectant mothers. Women with at least one claim for a pregnancy outcome diagnosis or procedure (ICD-9 or ICD-10) and at least one day of medical eligibility in Medicaid between January 1, 2014 and December 31, 2020 were eligible for study inclusion. Participants were restricted to those between the ages of 12–51 (see Figure 1). In total we identified 330 mothers utilizing doula care. Doula care was identified using the Center for Medicare & Medicaid Services (CMS) Taxonomy code for doula services (374J00000X) and unique National Provider Identifier (NPI) codes associated with the doulas participating in the programs in CA, FL, and the northeastern state.
Figure 1.
Study population flow chart of women who used doulas during their pregnancies and women who did not use doulas during their pregnancies. Of the 300 women we identified that used a doula during their pregnancy, 298 were included in propensity score matching analyses. These women were matched to 298 women (from a pool of 339,680) who did not use a doula.
Participants for the doula programs—especially in CA and the northeastern state—were often referred from community-based programs that identified women with health-related social needs and at high risk for adverse maternal health outcomes or those with health-related social needs. The scope of services for all women included at least four prenatal visits, support during labor and childbirth, and up to and including four postpartum visits. Doulas were reimbursed via Medicaid, although the specific reimbursement rate varied by state.
Outcomes
We assessed maternal outcomes during pregnancy (from the estimated start of pregnancy until delivery), at delivery, and during the postpartum period (up to 84 days after delivery). Outcomes included severe maternal morbidity (defined by the presence of at least one of the 21 conditions (see Supplemental Table 1) the CDC has indicated can result in significant or short-or long-term consequences to women's health), behavioral health (diagnosis of postpartum depression (PPD) or anxiety (PPA)), cesarean delivery, labor induction, rehospitalization within 60 days of delivery, emergency room (ER) visit from pregnancy complication within 30 days of delivery, and health care utilization (e.g., prenatal visits and postnatal visits). We did not evaluate maternal mortality because there were too few cases to evaluate. Outcomes were identified in claims using relevant ICD-9, ICD-10, CPT, and HCPCS codes (see Supplemental Table 2).
Statistical analyses
We fit multivariate logistic regression models with maternal health as the dependent outcome and doula care as the primary exposure. Potential confounding variables were selected based on a priori reasoning, as well as whether the doula and non-doula groups showed sizeable differences in a characteristic that could potentially affect both the decision to use a doula and experience a health outcome. The following variables were ultimately included as confounders, based on a priori reasoning or if their inclusion into the adjusted models changed the unadjusted odds ratio by more than 10%:18 women's state of residence; race (reported in Medicaid enrollment records, which we categorized as either Asian/Pacific Islander, Black, Hispanic, White, or Other); delivery hospital type (hospital data from Enclarity's provider database and was categorized as either “teaching” or “non-teaching”); maternal comorbidity index (MCI), which is a validated index ranging from 0 to 45 that predicts occurrence of “maternal end-organ injury or death during the delivery hospitalization through 30 days postpartum;19 (see Supplemental Table 1 for conditions), prenatal anxiety, obesity, and socioeconomic status index (SES) quartile. The SES score was adapted from the AHRQ Social-Economic Status (SES) and ranges from 0 to 100, with higher index scores indicating higher SES based on the following American Community Survey variables: unemployment rate, percentage of people living below the poverty level, median household income, median value of owner-occupied dwellings, percentage of people ≥25 years of age with less than a 12th-grade education, percentage of people ≥25 years of age with at least four years of college, and percentage of households with ≥1 person per room (crowding). We subsequently categorized individuals to a SES index category by the census block group of a patient's residence, where quartile 1 includes the bottom 25% of block groups across the US (the lowest socio-economic status), and quartile 4 includes the top 25% of block groups in the US (the highest socio-economic status).
Due to several differences in baseline characteristics between women who received and women who did not receive doula care, we ran a second set of models using propensity score matching (PSM). One of the benefits of using PSM is that it enabled us to make more targeted comparisons of the two groups of women (ensuring a more balanced distribution of confounders), versus if we had compared women who used doulas to a much broader population of pregnant women. PSM also reduces the effects of potential selection bias, which we considered a potential threat as an unmeasurable confounder. We matched on the following characteristics: age at the time of the pregnancy outcome, patient's state of residence, race, delivery hospital type, and socioeconomic status index (SES) quartile. We used logistic regression to estimate the propensity score for receiving doula care. Beta coefficients and p-values for the variables in the full propensity score model are included in Supplemental Table 3.
We matched women who used doulas to women who did not use doulas using a 1:1 case-control match greedy algorithm, without replacement.20 This algorithm first creates the “best” matches possible based on the propensity score (i.e., matching on eight digits of the propensity score), followed by “next-best” matches (i.e., matching on seven digits of the propensity score), in a hierarchical sequence until no further matches can be made. Once a mother who utilized doulas was matched to one who did not utilize a doula, the untreated subject (those who did not utilized was no longer eligible for matching to another treated subject. Additionally, only one pregnancy per woman (their last) were included into the matching algorithm (i.e., a woman could not be matched more than once with different pregnancies). We assessed the balance of covariates before and after matching with the standardized mean differences. Differences <0.1 were considered as indications of good balance between the groups.
We ran logistic regression models to calculate odds ratios (OR) of the association between health outcomes associated with doula care. We further adjusted regression models for MCI; we did not match on MCI because it significantly reduced the quality and quantity of successful matches. Mothers without doula care were used as the referent category in all regression analyses. All statistical analyses were performed using SAS Enterprise Guide, version 9.3 (SAS Institute Inc., Cary, NC).
Role of funding source
The funder had no role in the study design, methods, analysis, or preparation of the paper. AMF, SGB, and WC had full access to the data. All authors agreed to submit the study for publication.
Results
We identified 330 women in in the three states who received doula care during the study period (2014–2020). Most women (n = 265) came from Florida, since their doula program was in place starting in 2014. The doula pilot in the northeastern state began enrolling women in 2019 and the doula pilot in California began enrolling women in 2020; they contributed 47 and 18 women to the doula group, respectively. The non-doula group was comprised of 339,680 women across the three states.
Demographic and clinical characteristics
Overall, relatively more Black women were enrolled in doula programs (35.8%) compared to the proportion of Black women in the non-doula population (17.3%). Women who received doula care also appeared older, with an average of 28.2, compared to the non-doula population average age of 27.7. Relatively more women with health conditions were enrolled in the doula group compared to the non-doula group. Specifically, 23.0% of women who used doulas had “any pregnancy complication” (defined as a diagnosis of any of the following: gestational diabetes, gestational hypertension, pre-eclampsia, thrombocytopenia, placenta previa, short cervix, depression, anxiety, or anemia) compared to 18.7% of non-doula women; 9.0% of women who used doulas had preeclampsia vs. 6.0% of women without doulas; and 5.5% of women who used a doula had anemia, compared to 2.5% of non-doula women. These differences were statistically significant at p < 0.05 (Table 1). Many of these differences were by design, because women who were at higher risk for adverse pregnancy or birth outcomes were targeted in doula program outreach efforts. A greater proportion of women who utilized doulas, however, attended a postnatal visit (61.5%), compared to 35.9% of non-doula women. (A higher proportion of women with doulas showed greater attendance at prenatal visits as well, although this observation was expected because many women were not made aware of the doula programs until they attended their prenatal appointment.)
Table 1.
Baseline demographic and clinical characteristics (Unmatched and PSM).
| Unmatched |
Matched |
|||||
|---|---|---|---|---|---|---|
| Doula n = 330 |
No Doula n = 339,680 |
Standardized bias | Doula n = 298 |
No Doula n = 298 |
Standardized bias | |
| Characteristics | ||||||
| Age (mean SD) | 28·2 (5·44) | 27·7 (6·31) | 0·086 | 28·4 (5·4) | 28·4 (5·4) | 0.000 |
| State | ||||||
| California | 18 (5·5%) | 177,758 (52·3%) | 0·086 | 17 (5·7%) | 17 (5·7%) | 0.000 |
| Florida | 265 (80·3%) | 69,405 (20·4%) | 0·086 | 238 (79·8%) | 236 (79·1%) | 0.000 |
| Northeastern state | 47 (14·2%) | 92,517 (27·2%) | 0·086 | 43 (14·4%) | 45 (15·1%) | 0.000 |
| Patient's race | ||||||
| % Asian/Pacific Islander | 13 (3·9%) | 33,785 (9·9%) | 0·086 | 13 (4·4%) | 13 (4·4%) | 0.000 |
| % Black | 118 (35·8%) | 58,723 (17·3%) | 0·086 | 102 (34·2%) | 102 (34·2%) | 0.000 |
| % Hispanic/Latino | 56 (17·0%) | 93,946 (27·7%) | 0·086 | 49 (16·4%) | 49 (16·4%) | 0.000 |
| % White | 119 (36·1%) | 76,176 (22·4%) | 0·086 | 112 (37·5%) | 109 (36·5%) | 0.000 |
| % Other | 24 (1·2%) | 77,500 (16·3%) | 0·086 | 22 (7·4%) | 25 (8·4%) | 0.000 |
| Socio-economic status (SES) index | ||||||
| Q1 (worst) | 132 (42·7%) | 142,329 (45·4%) | 0·086 | 120 (40·2%) | 120 (40·2%) | 0.000 |
| Q2 | 76 (23·0%) | 76,858 (22·6%) | 0·086 | 73 (24·5%) | 71 (23·8%) | 0.000 |
| Q3 | 77 (23·3%) | 59,758 (17·6%) | 0·086 | 67 (22·5%) | 67 (22·5%) | 0.000 |
| Q4 (best) | 24 (7·3%) | 34,753 (10·2%) | 0·086 | 21 (7·0% | 21 (7·0%) | 0.000 |
| Missing/unknown | 21 (6·4%) | 25,982 (7·6%) | 0·086 | 17 (5·7%) | 19 (6·4%) | 0.000 |
| Comorbid conditions n(%) | ||||||
| Obesity | 37 (11·2%) | 33,721 (9·9%) | 0·071 | 34 (11·4%) | 34 (11·4%) | 0.000 |
| Hypertension | 7 (2·4%) | 9877 (4·1%) | 0·024 | 7 (2·3%) | 14 (4·7%) | 0·022 |
| Substance use disorder | 5 (1·5%) | 6649 (2·0%) | 0·132 | 9 (3·0%) | 4 (1·3%) | 0·132 |
| Smoking | 4 (1·2%) | 6738 (2·0%) | 0·073 | 11 (3·7%) | 4 (1·3%) | 0·073 |
| Maternal comorbidity index score (mean SD) | 0·6 (1·27) | 0·4 (1·04) | 0·086 | 0·6 (1·3) | 0·7 (1·4) | 0.000 |
| 0 | 227 (68·8%) | 249,429 (73·4%) | 0·073 | 201 (67·5%) | 204 (68·5%) | 0·073 |
| 1–2 | 79 (23·9%) | 76,807 (22·6%) | 0·073 | 72 (24·2%) | 71 (23·8%) | 0·073 |
| 3+ | 24 (7·3%) | 13,444 (4·0%) | 0·073 | 25 (8·4%) | 23 (7·7%) | 0·073 |
| Complications during pregnancy | ||||||
| Gestational diabetes | 16 (4·8%) | 18,367 (5·4%) | 0·062 | 13 (4·4%) | 18 (6·0%) | 0·062 |
| Gestational hypertension | 15 (4·5%) | 12,704 (3·7%) | 0·043 | 15 (5·0%) | 15 (5·0%) | 0.000 |
| Pre-eclampsia | 26 (9·0%) | 14,273 (6·0%) | 0·0323 | 26 (8·7%) | 16 (5·4%) | 0·032 |
| Placental abruption | 3 (0·9%) | 2302 (0·7%) | 0·023 | 3 (1·0%) | 3 (1·0%) | 0.000 |
| Anxiety | 7 (2·1%) | 11,328 (3·3%) | 0·014 | 6 (2·0%) | 15 (5·0%) | 0·014 |
| Depression | 8 (2·4%) | 7574 (2·2%) | 0·129 | 7 (2·3%) | 11 (3·7%) | 0·129 |
| Anemia | 18 (5·5%) | 8449 (2·5%) | 0·143 | 16 (5·4%) | 12 (4·0% | 0·143 |
| Any pregnancy complication | 76 (23·0%) | 63,646 (18·7%) | 0·143 | 69 (23·2%) | 74 (24·8%) | 0·143 |
| Health service utilization | ||||||
| Prenatal visit | 327 (99·1%) | 318,560 (82·3%) | 0·185 | 291 (97·65%) | 243 (81·54%) | 0·149 |
| Postnatal visit | 203 (61·5%) | 121,897 (35·9%) | 0·169 | 184 (61·74%) | 152 (51·01%) | 0·169 |
All characteristics are presented as n(%), except for age and maternal comorbidity index, which are presented as mean (standard deviation)· Conditions are defined using ICD-9, ICD-10, and HCPCS codes, which are included in the Appendix·
PSM results
With propensity score matching, we identified 298 pairs of women who received doula care matched to a control. Sixteen women were not matched because they were duplicates (i.e., they had multiple pregnancies with a doula) and were excluded from analysis. An additional sixteen women were not matched because they did not have complete data with respect to all covariates; therefore, they were dropped from analysis and a propensity score was not calculated. Analysis of the data missingness show that those with missing data appeared slightly younger, a higher prevalence delivered at a teaching hospital, and a larger proportion belonged to highest socioeconomic class. With only 16 women (5% of sample), however, we lacked power to determine whether any of these differences were statistically significant. A proportion of 5% missingness also suggested a minimal impact on study findings.
In the matched sample, women who used doulas during their pregnancies showed lower odds of cesarean delivery (OR: 0·47, 95% CI: 0·29–0·79) and lower odds of a PPA/PPD diagnosis (OR: 0·43, 95% CI: 0·22–0·82). No significant differences were observed between the doula and non-doula groups with respect to their odds of labor induction, preterm birth, emergency room utilization, or inpatient admissions within 30-days postpartum due to a delivery complication, severe maternal morbidity or mortality, or hospital readmission postpartum (Table 2).
Table 2.
Odds ratios of health outcomes between women who received doula care compared with women who did not receive doula care.
| Unmatched |
Matched |
||||||
|---|---|---|---|---|---|---|---|
| Doula (n = 330) |
No Doula (n = 339,680) |
Doula (n = 298) |
No Doula (n = 298) |
Unadjusted odds ratio (95% confidence interval) |
Adjusted odds ratio* (95% confidence interval) |
PSM odds ratio (95% confidence interval) |
|
| Health Outcome | |||||||
| Labor induction | 37 (9·30%) | 21900 (6·50%) | 33 (11·07%) | 30 (10·07%) | 1·17 (0·80–1·72) | 1·38 (0.90–2·1) | 1·12 (0·66–1·90) |
| C-section | 36 (15·30%) | 51209 (27·66%) | 31 (10·40%) | 53 (17·79%) | 0·41 (0·27–0·63) | 0·40 (0·20–0·65) | 0·47 (0·24–0·65) |
| Pre term birth | 19 (5·76%) | 26586 (7·83%) | 16 (5·37%) | 26 (8·72%) | 0·52 (0·30–0·89) | 0·49 (0·16–1·16) | 0·59 (0·31–1·14) |
| ER visit or Inpatient admission due to delivery complication (30 days) | 11 (3·33%) | 15522 (4·57%) | 11 (3·69%) | 15 (5·03%) | 0·82 (0·46–1·46) | 0·47 (0·15–1·46) | 0·73 (0·33–1·61) |
| Severe maternal morbidity or mortality within 60 days of pregnancy outcome | 7 (2·10%) | 9123 (2·70%) | 6 (2·01%) | 7 (2·35%) | 0·70 (0·31–1·16) | 0·45 (0·11–1·83) | 0·87 (0·29–2·66) |
| Inpatient admission within 60 days of pregnancy outcome | 24 (7·27%) | 29120 (8·6%) | 22 (7·38%) | 27 (9·06%) | 0·72 (0·45–1·16) | 0·67 (0·33-1·36) | 0·81 (0·47–1·45) |
| Post partum anxiety or post partum depression | 25 (7·57%) | 42831 (13·45%) | 18 (6·04%) | 42 (14·09%) | 0·63 (0·36–1·07) | 0·93 (0·48–1·79) | 0·43 (0·22–0·82) |
PSM models were matched on maternal age, race, state of residence, socioeconomic status quartile, and delivery hospital type (teaching or non-teaching). PSM models were additionally adjusted for maternal comorbidity index (MCI). Logistic regressions were adjusted for race, SES index score, hospital type (teaching hospital or not teaching hospital), MCI, obesity, and prenatal anxiety. Conditions are defined using ICD-9, ICD-10, and HCPCS codes and are included in Supplemental Table 2.
The reduction in odds of cesarean delivery among women who received doula support was generally consistent regardless of differences in contextual factors surrounding their pregnancy and delivery. Analyses show, for example, that doulas are associated with a reduction in odds of cesarean delivery regardless of the trimester in which doula care was received or of the clinical provider present during childbirth (e.g., OB-GYN only, midwife (alone or present alongside an OB-GYN)). Women who received doula care during their first trimester, however, showed the greatest decrease in odds of cesarean delivery (OR: 0.38, 95% CI: 0.22–0.67). The association between doula support and odds of PPA/PPD diagnoses appeared more nuanced and dependent upon timing of doula care. Women showed a reduction in odds of PPA/PPD diagnoses, for example, when they received doula care during labor and childbirth but not necessarily during pregnancy (OR: 0.35, 95% CI: 0.16–0.78) (Table 3).
Table 3.
Odds ratios for c-section and PPA/PPD as a function of timing of doula utilization and clinical team.
| Health outcome | Clinical team | Trimester doula services received | Unadjusted odds ratio (95% confidence interval) |
Adjusted odds ratio* (95% confidence interval) |
PSM odds ratio (95% confidence interval) |
|---|---|---|---|---|---|
| Cesarean Delivery | All | 1 | 0·77 (0·39–1·50) | 0·79 (0·32–1·93) | 0·38 (0·22–0·67) |
| OB-GYN Only | 1 | 1·37 (0·63–2·97) | 1·68 (0·57–4·98) | 0·56 (0·29–1·08) | |
| OB-GYN + Midwife | 1 | 1·05 (0·36–3·02) | 2·04 (0·62–6·72) | 0·15 (0·04–0·55) | |
| All | 2 | 0·56 (0·33–0·95) | 0·44 (0·22–0·91) | 0·41 (0·21–0·77) | |
| OB-GYN Only | 2 | 0·85 (0·46–1·57) | 0·68 (0·29–1·59) | 0·48 (0·22–1·05) | |
| OB-GYN + Midwife | 2 | 0·81 (0·39–1·68) | 1·20 (0·47–3·07) | 0·10 (0·02–0·47) | |
| All | 3 | 0·43 (0·27–0·68) | 0·37 (0·20–0·70) | 0·44 (0·15–1·30) | |
| OB-GYN Only | 3 | 0·71 (0·42–1·20) | 0·46 (0·22–0·99) | 0·17 (0·03–0·83) | |
| OB-GYN + Midwife | 3 | 0·52 (0·27–0·98) | 0·86 (0·39–1·19) | – | |
| All | Delivery | 0·31 (0·17–0·55) | 0·25 (0·11–0·57) | 0·48 (0·28–0·84) | |
| OB-GYN Only | Delivery | 0·42 (0·20–0·88) | 0·22 (0·07–0·64) | 0·17 (0·03–0·84) | |
| OB-GYN + Midwife | Delivery | 0·46 (0·24–0·91) | 0·67 (0·27–1·66) | 0·21 (0·06–0·72) | |
| Post partum anxiety or post partum depression (PPA/PPD) | All | 1 | 0·35 (0.05–2.58) | 0·33 (0·05–2·44) | 0·52 (0·26–1·02) |
| OB-GYN Only | 1 | 0·72 (0.17–3.01) | 0·86 (0·11–6·07) | 0·56 (0·24–1·35) | |
| OB-GYN + Midwife | 1 | – | – | – | |
| All | 2 | 0·60 (0.28–1.27) | 0·52 (0·16–1·67) | 0·47 (0·21–1·06) | |
| OB-GYN Only | 2 | 0·34 (0.08–1.37) | 0·40 (0·06-2·97) | 0·69 (0·27–1·76) | |
| OB-GYN + Midwife | 2 | 0·79 (0.29–2.17) | 0·37 (0·05–2·28) | – | |
| All | 3 | 0·59 (0.32–1.08) | 0·86 (0·50–1·87) | 0·18 (0·02–1·31) | |
| OB-GYN Only | 3 | 0·69 (0.30–1.57) | 1·25 (0·49–3·18) | – | |
| OB-GYN + Midwife | 3 | 0·74 (0.34–1.59) | 0·66 (0·20–2·13) | – | |
| All | Delivery | 0·65 (0.35–1.24) | 0·76 (0·31–1·10) | 0·35 (0·16–0·78) | |
| OB-GYN Only | Delivery | 0·62 (0.23–1.70) | 0·94 (0·29–3·08) | 0·26 (0·08–0·87) | |
| OB-GYN + Midwife | Delivery | 0·63 (0.28–1.44) | 0·47 (0·11–1·96) | – |
PSM models were matched on maternal age, race, state of residence, socioeconomic status quartile, and delivery hospital type (teaching or non-teaching). PSM models were additionally adjusted for maternal comorbidity index (MCI). Logistic regressions were adjusted for race, SES index score, hospital type (teaching hospital or not teaching hospital), and MCI. Conditions are defined using ICD-9, ICD-10, and HCPCS codes and are included in the Appendix.
Population subgroup analyses
Analyses comparing outcomes among population subgroups (risk groups) who received doula care show that the odds of cesarean delivery for women with a pregnancy complication are 0.42 times the odds (95% CI: 0.24, 0.76) of cesarean delivery for women with pregnancy complication but who did not receive doula care. Women with a pregnancy complication who receive doula care also show lower odds of PPA/PPD (OR: 0.46, 95% CI: 0.23–0.92) compared to similar women without doula care. Doulas showed a similar association to health between Black and White women, as the odds of cesarean delivery and of a PPA/PPD diagnosis did not differ statistically between them (Table 4).
Table 4.
Odds ratios for c-section and for PPA/PPD, as a function of population risk subgroups.
| Health outcome | Unadjusted odds ratio (95% Confidence interval) |
Adjusted odds ratio* (95% Confidence interval) |
PSM odds ratio (95% Confidence interval) |
|---|---|---|---|
| Cesarean Delivery | |||
| Race: Black vs· WHITE | 0·93 (0·58–0·36) | 0·98 (0·88–1·58) | 0·66 (0·36–1·21) |
| Pregnancy complication: Yes vs· No | 0·94 (0·67–1·21) | 0·96 (0·57–1·35) | 0·42 (0·24–0·76) |
| Diagnosis of postpartum anxiety or postpartum depression | |||
| Race: Black vs· White | 0·80 (0·26–1·33) | 0·79 (0·26–1·33) | 0·50 (0·24–1·04) |
| Pregnancy complication: Yes vs· No | 0·95 (0·28–1·62) | 0·97 (0·28–1·66) | 0·46 (0·23–0·92) |
PSM models were matched on maternal age, race, state of residence, socioeconomic status quartile, and delivery hospital type (teaching or non-teaching). PSM models were additionally adjusted for maternal comorbidity index (MCI). Logistic regressions were adjusted for race, SES index score, hospital type (teaching hospital or not teaching hospital), and MCI. Conditions are defined using ICD-9, ICD-10, and HCPCS codes and are included in the Appendix.
A comparison of the results from the multivariate logistic regressions and the PSM analyses show similar findings. The magnitude of associations in the PSM analyses, however, were generally more modest, and the confidence intervals were narrower. These differences likely reflect differences in the sample sizes ultimately used in the two methodologies and because PSM women were more similar at baseline and therefore showed less variation. We also note that multivariate logistic regression (but not the PSM analysis) showed a significant reduction in odds of preterm birth for women who received doula care; this association has been found significant in other studies and previously published.15,21
Discussion
In this retrospective cohort study using claims data from three different states (CA, FL, and the northeastern state), we found that doula care provided to Medicaid enrollees was associated with salutary benefits. Analyses of propensity score matched expectant mothers show that women who received doula care had lower odds (52.9%) of cesarean delivery and of a PPA/PPD diagnosis (57.5%) relative to similar women who did not receive doula care. The link between doula care and reduction in cesarean delivery risk is consistent with findings published in previous literature. The reduction in risk of PPA/PPD was more novel, because the few studies that have explored the relationship between doula care and behavioral health either have been qualitative in nature or have shown no significant association.22,23 We were uncertain, therefore, whether we would be able to detect an association in claims.
Doulas do not operate in isolation, however, and their value to maternal health depends upon the composition of the mother's clinical provider team. The magnitude of the reduction in odds of cesarean delivery varied, for example, with the clinical provider present during childbirth. Results show that doula support received during different stages of pregnancy was more consistently associated with a reduction in odds of cesarean delivery when a midwife was present at delivery. The value of doula care also varied by the health outcome and timing in doula support was received. Women who initiated doula services during their first trimester, for example, showed the greatest reductions in odds cesarean delivery. This finding suggests the importance of establishing relationship with doulas early. Doulas are trained to help increase their patients’ understanding of their care, recognize health warning signs, and support coordination of ongoing care needs. Prior studies also have shown that pregnant women who interact with their doulas early in pregnancy are more engaged in their prenatal care and have better birth outcomes.24 Doula care received during early in pregnancy, therefore, may shift women into a trajectory that ultimately results in improved health outcomes during childbirth.
The relationship between doula care and PPA/PPD, however, showed a significant association only when doulas were present during labor and birth. The role doulas play in terms of reducing patient anxiety and feelings of isolation during labor and birth may be more critical to women's behavioral health postpartum, relative to benefits doulas provide with facilitating communication and coordination of care needs earlier in pregnancy. Doulas also are associated with greater patient engagement, which was reflected in our data by the greater prevalence of women who received doula care that attended their postnatal visits. This engagement in care beyond childbirth may also have contributed to the reduction in odds of PPA/PPD.
Results from this study provide important insight on the relationship between doula care and health by race and by high-risk medical conditions. The relatively small sample sizes of other studies have precluded such analyses, or relegated treatment of these factors as confounders adjusted for in analysis, rather than evaluating the relationships independently. Through stratification of analyses by race, we were able to determine that Black expectant mothers who received doula care enjoyed the same health benefits as White women who received doula care. Both groups of women showed lower odds of cesarean delivery and diagnoses of PPA/PPD relative to their non-doula counterparts.
Our analyses by high-risk conditions indicate women who received doula care showed a 58% reduction in odds of cesarean delivery relative to women with pregnancy complications without doula care. Similarly, women with pregnancy complications who received doula care showed a 54% reduction in odds of PPA/PPD diagnosis, relative to similar women without doula care. Because Black women have a higher prevalence of some of the most common conditions women can acquire during pregnancy, including pre-eclampsia,25 anemia,26 and symptoms of depression or anxiety,27 doula care targeted toward Black women may help bridge the gap in health outcomes between White and Black women enrolled in Medicaid. Our study findings suggest that doulas help mitigate the effects of high risk pregnancy characteristics on maternal health outcomes.
We note that a limitation of the study is that we did not evaluate the extent that doula care received postnatally could have influenced postnatal outcomes, beyond the effects of factors we evaluated during pregnancy and occurring at birth. A qualitative study on the impact of doulas in the postpartum period indicate that social support provided postnatally from doulas is associated with improved maternal mental health and wellbeing.28 It is possible, therefore, that the reduction in odds of PPA/PPD we observed may in part be influenced by visits with doulas during the postpartum period. Future research, especially quantitative analyses, could address a research gap in the doula literature through focusing on the association between doula care received in the postpartum period and postpartum health outcomes.
Another limitation we note is that women were not representative of the broader population. Women were often referred to doula services because they were considered high risk due to their clinical or health-related social needs. Study findings may not be generalizable to women who receive doula care in Medicaid programs in states other than those included in our study, or to women with other types of insurance (i.e., non-Medicaid) or who pay for doula care out-of-pocket. Additionally, because the study sample was largely comprised of women residing in FL, the generalizability of findings to women in CA and the northeastern state may be limited. While data was assessed from a single area from a relatively smaller list of doulas within those states, respectively, women in Florida received doula care from a wider range of doulas across the state. The intent of this study, however, was to evaluate whether and how the doula pilot programs evaluated were associated with improved maternal health outcomes (in order to inform decision making about potential expansion of such programs into other areas.) Our study findings demonstrated that within the vulnerable population of women studied, doula care was associated with a reduction in cesarean births and in PPA/PPD diagnoses.
Although this study describes the clinical benefits associated with doula care, prior studies also have linked doula care with qualitative outcomes not found in claims—such as breastfeeding and improved patient satisfaction.16,29,30 We are presently interviewing some of the participants in the study population to gain a more comprehensive understanding of the patient experience with doula services. We also note that this study did not address the degree to which race concordance between doula and patient influences health outcomes. Some literature suggests that race concordance contributes to the quality of patient-provider communication,31 and is associated with birthing mortality among infants—but has no association with maternal mortality.32 Further research on this subject area could consider the importance of race concordance in the relationship between doula and women to maternal health.
Addressing or intervening upon maternal health disparities requires broad, systems’ level thinking focused on mitigating the social and structural factors that can perniciously influence health. Our study provides evidence on the benefit of the integration of doula care early in pregnancy and continuing postnatally. Study findings also demonstrate the success in integrating doula into maternity care networks. Doulas offer numerous benefits to expectant and postpartum mothers, especially among low-income and marginalized minority populations.
Contributors
AMF and WC designed the study and the analytical strategy. AMF and SGB obtained and analyzed the data. AMF and SGB wrote the first draft of the manuscript. AMF prepared the tables. SGB prepared the figure. AMF, SGB, and WC all had direct access to and verified the underlying data reported in the manuscript. All authors reviewed and edited the manuscript. TT, DM, DB, and SD supervised the study process.
Data sharing statement
Requests for data should be directed to the corresponding author. Some data can be made available upon reasonable request.
Declaration of interests
April M. Falconi, PhD, Samantha G. Bromberg, PhD, and Winnie Chi, PhD, Demetria Malloy, MD, Denae Blanco, RN, and Susan Disciglio, RN, all are employed by Anthem, Inc. Truc Tang, MPH was employed with Anthem during the evaluation of the study and writing of the manuscript but left Anthem while the manuscript was under review.
Acknowledgements
No sources of funding were used to assist in the preparation of this manuscript. Research was completed as part of the usual employment obligations to Anthem, Inc.
Footnotes
Supplementary material associated with this article can be found in the online version at doi:10.1016/j.eclinm.2022.101531.
Appendix. Supplementary materials
References
- 1.Singh GK. United States Health Resources and Services Administration; Washington, DC: 2010. Maternal Mortality in the United States, 1935–2007: Substantial Racial/Ethnic Socioeconomic, and Geographic Disparities Persis. [Google Scholar]
- 2.Leonard S, Main E, Scott K, Profit J, Carmichael S. Racial and ethnic disparities in severe maternal morbidity prevalence and trends. Ann Epidemiol. 2019;33:30–36. doi: 10.1016/j.annepidem.2019.02.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rossen LM, Womack LS, Hoyert DL, Anderson RN, Uddin SFG. The impact of the pregnancy checkbox and misclassification of maternal mortality trends in the United States, 1997-2017. Vital Health Stat. 2020;44:1–61. [PubMed] [Google Scholar]
- 4.Howell EA, Mora PA, Horowitz CR, Leventhal H. Racial and ethnic differences in factors associated with early postpartum depressive symptoms. Obstetr Gynecol. 2005;105:1442–1450. doi: 10.1097/01.AOG.0000164050.34126.37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Davis NL, Smoots AN, Goodman D. Centers for Disease Control and Prevention; 2019. Pregnancy-Related Deaths: Data from 14 U.S. Maternal Mortality Review Committees, 2008-2017.https://www.cdc.gov/reproductivehealth/maternal-mortality/erase-mm/MMR-Data-Brief_2019-h.pdf Accessed 6 July 2020. [Google Scholar]
- 6.Vilda D, Wallace M, Dyer L, Harville E, Theall K. Income inequality and racial disparities in pregnancy-related mortality in the US. Soc Sci Med - Popul Health. 2019;9 doi: 10.1016/j.ssmph.2019.100477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Braveman B, Dominguez TP, Burke W, et al. Explaining the Black-White disparity in preterm birth: a consensus statement from a multi-disciplinary scientific work group convened by the March of Dimes. Front Reprod Health. 2021;3 doi: 10.3389/frph.2021.684207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wang E, Glazer K, Howell E. Social determinants of pregnancy-related mortality and morbidity in the United States: a systematic review. Obstetr Gynecol. 2020;135:896–915. doi: 10.1097/AOG.0000000000003762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Petersen EE, Davis NL, Goodman D, et al. Racial/ethnic disparities in pregnancy-related deaths — United States, 2007–2016. MMWR Morb Mortal Wkly Rep. 2019;68:762–765. doi: 10.15585/mmwr.mm6835a3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Howell E, Egorova N, Janevic T, et al. Race and ethnicity, medical insurance, and within-hospital severe maternal morbidity disparities. Obstetr Gynecol. 2020;235:285–293. doi: 10.1097/AOG.0000000000003667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Howell E, Brown H, Brumley J, et al. Reduction of peripartum racial and ethnic disparities. Obstetr Gynecol. 2018;131:770–782. doi: 10.1097/AOG.0000000000002475. [DOI] [PubMed] [Google Scholar]
- 12.Howard ED, Low L, Kane L. It's time to dial up doula care. J Perinat Neonatal Nurs. 2020;34:4–7. doi: 10.1097/JPN.0000000000000456. [DOI] [PubMed] [Google Scholar]
- 13.Kozhimannil K, Vogelsang CA, Hardeman R, Prasad S. Disrupting the pathways of social determinants of health: doula support during pregnancy and childbirth. J Am Board Fam Med. 2016;29:308–317. doi: 10.3122/jabfm.2016.03.150300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Thomas M-P, Ammann G, Brazier E, Noyes P, Maybank A. Doula services within a healthy start program: increasing access for an underserved population. J Matern Child Health. 2017;21:S59–S64. doi: 10.1007/s10995-017-2402-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gruber KJ, Cupito S, Dobson C. Impact of doulas on healthy birth outcomes. J Perinat Educ. 2013;22:1058–1243. doi: 10.1891/1058-1243.22.1.49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lee PH. Should we adjust for a confounder if empirical and theoretical criteria yield contradictory results? A simulation study. Sci Rep. 2014;6:6085. doi: 10.1038/srep06085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Thurstona LF, Abrams D, Dreher A, Ostrowski S, Wright J. Improving birth and breastfeeding outcomes among low resource women in Alabama by including dulas in the interprofessional care team. J Interprof Educ Pract. 2019;17 [Google Scholar]
- 18.Kozhimannil K, Attanasio L, Jou J, Joarnt L, Johnson P, Gjerdingen D. Potential benefits of increased access to doula support during childbirth. Am J Manag Care. 2014;20:e340–e352. [PMC free article] [PubMed] [Google Scholar]
- 19.Aoyama K, D'Souza R, Inada E, Lapinsky S, Fowler R. Measurement properties of comorbidity indices in maternal health research: a systematic review. BMC Pregnancy Childbirth. 2017;17:372–380. doi: 10.1186/s12884-017-1558-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Parsons L. SUGI 29 Proceedings. Ovation Research Group; Seattle, Washington: 2004. Performing a 1:N case-control match on propensity score. Paper 165-29. [Google Scholar]
- 21.Kozhimannil K, Hardeman R, Alarid-Escudero F, Vogelsang C, Blauer-Peterson C, Howell E. Modeling the cost-effectiveness of doula care associated with reductions in preterm birth and cesarean delivery. Birth. 2016;43:20–27. doi: 10.1111/birt.12218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Gordon N, Walton D, McAdam E, Derman J, Gallitero G, Garrett L. Effects of providing hospital-based doulas in health maintenance organization hospitals. Obstetr Gynecol. 1999;93:422–426. doi: 10.1016/s0029-7844(98)00430-x. [DOI] [PubMed] [Google Scholar]
- 23.Hans S., Edwards R, Zhang Y. Randomized controlled trial of doula-home-visiting services: impact on maternal and infant health. Matern Child Health J. 2018;22:105–113. doi: 10.1007/s10995-018-2537-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ogunwole S, Bennett W, Williams A, Bower K. Community-based doulas and COVID-19: addressing structural and institutional barriers to maternal health equity. Perspect Sexual Reprod Health. 2020;52:199–204. doi: 10.1363/psrh.12169. [DOI] [PubMed] [Google Scholar]
- 25.Zhang M, Wan P, Ng K, et al. Preeclampsia among African American pregnant women: an update on prevalence, complications, etiology, and biomarkers. Obstet Gynecol Surv. 2020;75:111–120. doi: 10.1097/OGX.0000000000000747. [DOI] [PubMed] [Google Scholar]
- 26.ACOG Anemia in pregnancy. Obstetr Gynecol. 2021;138:e55–e64. doi: 10.1097/AOG.0000000000004477. [DOI] [PubMed] [Google Scholar]
- 27.Ponting C, Mahrer N, Zelcer HD, Chavira D. Psychological interventions for depression and anxiety in pregnant Latina and Black women in the United States: a systematic review. Clin Psychol Psychother. 2020;27:249–265. doi: 10.1002/cpp.2424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.McLeish J, Redshaw M. “Being the best person that they can be and the best mum”: a qualitative study of community volunteer doula support for disadvantaged mothers before and after birth in England. BMC Pregnancy Childbirth. 2019;19 doi: 10.1186/s12884-018-2170-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Strauss N, Sakala C, Corry M. Overdue: Medicaid and private insurance. J Perinat Educ. 2016;25:145–149. doi: 10.1891/1058-1243.25.3.145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kozhimannil K, Attanasio L, Hardeman R, O'Brien M. Doula care supports near-universal breastfeeding initiation among diverse, low-income women. J Midwifery Women's Health. 2013;58:378–382. doi: 10.1111/jmwh.12065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Johnson Shen M, Peterson EB, Costas-Muniz R, et al. The effects of race and racial concordance on patient-physician communication: a systematic review of the literature. J Racial Ethnic Health Disparities. 2018;5:117–140. doi: 10.1007/s40615-017-0350-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Greenwood BN, Hardeman RR, Huang L, Sojourner A. Physician-patient racial concordance and disparities in birthing mortality for newborns. Proc Natl Acad Sci. 2019;117:21194–21200. doi: 10.1073/pnas.1913405117. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.