In Vivo Monitoring of PV Reveals CA1 as a Potent Therapeutic Target
Current murine models of myeloproliferative neoplasms (MPN) cannot address how MPN can invade hematopoietic organs from a defined single anatomical origin as observed in patients. Murakami et al. developed an immunocompetent wild-type mouse model of Polycythemia Vera (PV) spreading from a single bone marrow site. PV development was abrogated in mice with splenectomy or lacking carbonic anhydrase 1 (CA1) in mutant hematopoietic progenitors. Increased expression of CA1 was found in CD34+ cells from PV patients, and its pharmacologic inhibition decreased variant allele frequency in colony-forming assays, suggesting CA1 as a potential therapeutic target for PV.
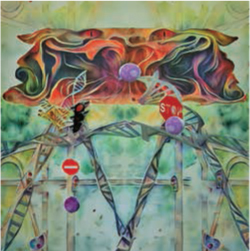
Type I CALR Mutations Activate the IRE1α/XBP1 Pathway to Drive MPNs
Approximately every fifth patient with myeloproliferative neoplasms (MPN) harbors a CALR mutation of either type I or type II, which differ in clinical features and outcomes. Ibarra et al. show that type I, but not type II, mutant CALR proteins lose Ca2+ binding, causing Ca2+ depletion from the endoplasmic reticulum and activation of the IRE1α/XBP1 pathway. IRE1α inhibition prevented type I-mutant CALR cell survival in culture and thrombocythemia development in mice. These results identify IRE1α/XBP1 as a potentially targetable dependency specific to type I CALR-mutated MPNs.
Multimodal Single-Cell Genomic Analysis of MDS Progression to sAML

By single-cell DNA, RNA and proteogenomic sequencing of matched patient samples, Guess et al. uncovered three clonal evolution patterns associated with clinical progression from myelodysplastic syndrome (MDS) to secondary acute myeloid leukemia (sAML). The Static pattern, characterized by minimal clonal change, had founding clones with mutations in DNA methylation genes and transitioned to sAML in the absence of further genomic aberrations, suggesting nongenetic evolution. Clonal architecture changed dramatically in Dynamic groups, often involving acquisition of mutations in signaling pathways (Dynamic-S) or progressive structural aberrations along with TP53 mutations (Dynamic-C). Collectively, these findings elucidate the interplay of genetic and nongenetic factors in leukemic transformation.
Signaling Genes Undergo Complex Patterns of Clonal Evolution during MDS Progression
To investigate patterns of subclone evolution during progression from myelodysplastic syndrome (MDS) to secondary acute myeloid leukemia (sAML), Menssen et al. sequenced paired MDS and sAML samples from a cohort of patients. Signaling gene mutations were found to occur universally in subclones and undergo complex patterns of clonal evolution, including acquisition, expansion, persistence, and contraction of mutations during progression, with multiple patterns often coexisting in the same patient. The presence of at least one signaling gene mutation at MDS was associated with future progression to sAML in patients with lower risk MDS.
The 5hmC Landscape and Dynamics of Human Hematopoiesis and TET2-Deficient HSPCs

Nakauchi et al. report the genome-wide landscape of DNA hydroxymethylation (5hmC) in human hematopoietic lineages. The authors map TET2-dependent 5hmC, epigenetic and transcriptional programs matched to competitive advantage, myeloid skewing, and reduced erythroid output in TET2-deficient hematopoietic stem and progenitor cells (HSPC). Vitamin C and azacitidine restore the 5hmC landscape and phenotypes in TET2-mutant HSPCs. These findings offer a comprehensive resource for TET-dependent transcriptional regulation of human hematopoiesis and shed light on the potential mechanisms by which TET deficiency contributes to clonal hematopoiesis and malignancies.


