ABSTRACT
Background
Ultra-processed foods contribute to risks of obesity and cardiometabolic disease, and higher intakes have been observed in low-income populations in the United States. Consumption of ultra-processed foods may be particularly higher among individuals experiencing food insecurity and participating in the Supplemental Nutrition Assistance Program (SNAP).
Objectives
Using data from the 2007–2016 NHANES, we examined the associations between food insecurity, SNAP participation, and ultra-processed food consumption.
Methods
The study population comprised 9190 adults, aged 20–65 y, with incomes ≤300% of the federal poverty level (FPL). Food insecurity was assessed using the Household Food Security Survey Module and SNAP participation over the past 12 mo was self-reported. Dietary intake was measured from two 24-h dietary recalls. Ultra-processed food consumption (percentage of total energy intake) was defined using the NOVA food classification system. Linear regression models were used to examine the associations between food insecurity, SNAP participation, and ultra-processed food consumption, adjusting for sociodemographic and health characteristics.
Results
More severe food insecurity was associated with higher intakes of ultra-processed foods (P-trend = 0.003). The adjusted means of ultra-processed food intake ranged from 52.6% for adults with high food security to 55.7% for adults with very low food security. SNAP participation was also associated with higher intakes of ultra-processed foods (adjusted mean: 54.7%), compared with income-eligible participants (adjusted mean: 53.0%). Furthermore, the association between food insecurity and ultra-processed foods was modified by SNAP participation (P-interaction = 0.02). Among income-eligible nonparticipants and income-ineligible nonparticipants, more severe food insecurity was associated with higher consumption of ultra-processed foods. Among SNAP participants, the association between food insecurity and consumption of ultra-processed foods was nonsignificant.
Conclusion
In a nationally representative sample of adults, food insecurity and SNAP participation were both associated with higher levels of ultra-processed food consumption.
Keywords: food insecurity, SNAP, ultra-processed food, NHANES, health disparities
Introduction
Food insecurity, defined as the “limited or uncertain availability of nutritionally adequate and safe foods or the limited or uncertain ability to acquire acceptable foods in socially acceptable ways,” is a critical social determinant of health (1). In 2019, it was estimated that 10.5% (or 13.7 million) US households experienced food insecurity (2). As a result of the ongoing COVID-19 pandemic, estimates of national food insecurity have more than tripled, which will likely result in widening diet and health disparities in marginalized groups (3, 4).
Food insecurity has been adversely associated with dietary intake in low-income adults (5). Across multiple studies, food insecurity has been associated with lower intakes of fruits and vegetables, higher intakes of red and processed meats and sugar-sweetened beverages, and lower scores on evidence-based diet quality indices, such as the Healthy Eating Index and the Alternate Healthy Eating Index (6–10). These findings suggest that dietary behaviors play an important role in mediating the observed associations between food insecurity and hypertension, diabetes, and other cardiometabolic conditions (11–14). However, the degree to which prior dietary studies have captured the spectrum of typical foods consumed by low-income populations is unclear.
The relation between food insecurity and dietary intake is further complicated by participation in the Supplemental Nutrition Assistance Program (SNAP), formerly known as the Food Stamp Program. SNAP is the largest of 15 federal nutrition assistance programs whose central goal is to alleviate food insecurity. In 2020, SNAP provided benefits to ∼40 million low-income individuals (≤130% of the FPL) at a total cost of $74 billion (15). SNAP benefits are distributed via Electronic Benefit Transfer (EBT) cards, which can be used to purchase most foods and beverages, with the exception of hot or prepared foods, alcohol, and dietary supplements. Despite the well-established effects of SNAP in alleviating food insecurity (16, 17), SNAP participants have poorer diet quality and cardiometabolic health outcomes than both their low- and higher-income nonparticipant counterparts (18, 19). SNAP participation may also positively or negatively modify the relation between household food security and dietary outcomes through its role as a policy intervention to improve food insecurity and poor nutrition, or as a proxy for individuals most vulnerable to poverty, food insecurity, and poor health. To our knowledge, few studies have examined this relation.
In the present study, we focused on the outcome of ultra-processed food consumption. According to NOVA, ultra-processed foods are formulations of ingredients, mostly of exclusive industrial use, that result from a series of industrial processes and typically contain high levels of added refined carbohydrates and/or fats. These foods include frozen and shelf-stable meals, breakfast cereals, sugar-sweetened beverages, baked desserts, and more (20). Ultra-processed foods comprise nearly 60% of total energy intake consumed in the United States, and higher intake rates have been observed in low-income populations (21). The current study of the relation between food insecurity and ultra-processed food consumption is distinct from prior studies of food insecurity and consumption of individual foods, food groups, or diet patterns because it focuses on the degree of food processing. Given that ultra-processed foods are aggressively marketed, widely accessible, more shelf stable than foods with less processing, and touted for their convenience (20), individuals from food-insecure households and those participating in SNAP may increase consumption of ultra-processed foods when monetary resources are low. Furthermore, ultra-processed foods contribute to excessive caloric intake (22) and overweight/obesity (23, 24), providing a plausible mechanism for the positive associations of diet-sensitive cardiometabolic outcomes with food insecurity and SNAP participation.
Our primary objectives were to examine associations of household food security and SNAP participation with ultra-processed food consumption. Our secondary objective was to examine the modifying role of SNAP participation in the association between household food security and ultra-processed food consumption. Based on prior studies, we hypothesized that food insecurity and SNAP participation would be positively associated with ultra-processed food consumption and that the association between food insecurity and ultra-processed food consumption would be more pronounced among low-income adults participating in SNAP.
Methods
Study population
NHANES is an ongoing, multistage survey representative of the civilian, noninstitutionalized United States population (25). NHANES collects information on demographics, dietary intake, and other health-related characteristics. NHANES study protocols were approved by the National Center for Health Statistics (NCHS) ethics review board and informed consent was obtained from all adult participants. The present study combines data from 2007 to 2016, including information from participants who completed two 24-h diet recalls, with information on household food security and other covariates of interest.
The analytic population comprised 9190 adults, ages 20–65 y, with family incomes ≤300% of the FPL at the time of data collection (Supplemental Figure 1). Individuals aged ≥65 y were excluded due to known differences in socioeconomic status, dietary behaviors, and the presence of existing health conditions, which may lead to differential associations between food insecurity and ultra-processed food consumption. Similar to prior studies, in the present study an income threshold was applied to focus on individuals at risk for food insecurity and to reduce the potential for residual confounding by income (8, 11, 26).
Household food security and SNAP participation
Household food security was measured using the 18-item US Household Food Security Survey Module (27). This “core module” is one of the most widely used instruments to measure food security status. Briefly, questions are ordered by severity and ask about experiences or behaviors related to inadequate resources to acquire food over the 12 mo prior to the time of collection of these data. Affirmative responses to the 18 questions are summed to create a score ranging from 0 to 18, with a higher score denoting more severe food insecurity. According to USDA guidelines, 0 affirmative responses indicates high food security, 1–2 affirmative responses indicates marginal food security, 3–5 affirmative responses in households without children or 3–7 affirmative responses in households with children indicates low food security, and 6–10 affirmative responses in households without children or 8–18 affirmative responses in households with children indicates very low food security.
SNAP participation was assessed using the question, “In the last 12 mo, did (you/you or any member of your household) receive Food Stamp benefits?” Beginning in 2013–2014, this question was rephrased to include “SNAP or Food Stamp benefits.” Individuals who responded affirmatively to this question and who had family incomes ≤130% FPL were categorized as SNAP participants. Individuals who responded negatively to this question and who had family incomes ≤130% FPL were categorized as income-eligible nonparticipants. Individuals who responded negatively to this question and had family incomes >130% FPL were considered income-ineligible nonparticipants because they would be financially ineligible to receive SNAP benefits. Individuals who responded affirmatively to receiving SNAP benefits and who had family incomes above the federal eligibility criteria for SNAP (i.e., >130% FPL) were excluded due to potential misclassification (n = 970). Information on the duration of SNAP participation was not collected in NHANES.
Ultra-processed food intake
Dietary intake was assessed using two 24-h dietary recalls using the Automated Multiple Pass Method, conducted by trained interviewers. The 24-h recall collects detailed information on all foods and beverages consumed from midnight to midnight of the previous day. The first recall is administered in-person in the Mobile Examination Center (28). The second recall is administered by telephone 3–10 d later (29). The validity of the 24-h recall method has been previously established (30, 31). We included recalls that were categorized as “reliable and met the minimum criteria” according to NCHS staff. Recalls with implausible total energy intakes (<500 or >5000 kcal) were excluded from analyses (n = 711) to reduce the potential for measurement error.
In the present analysis, all food and beverage items were categorized according to NOVA, a system that classifies each food item based on the extent and purpose to which the food item is industrially processed (32) into 4 mutually exclusive groups: 1) unprocessed or minimally processed foods, 2) processed culinary ingredients, 3) processed foods, and 4) ultra-processed foods. Ultra-processed foods are foods that contain the greatest degree of industrial processing, oftentimes containing cosmetic additives (e.g., coloring, flavoring, sweeteners, emulsifiers, etc.) and other substances of no or rare culinary use (e.g., modified starches, hydrogenated oils, protein isolates, etc.).
Foods were classified based on the following NHANES variables: “Main Food Description,” “Additional Food Description” (describing food codes), and “SR Code Description” (describing SR codes), as well as “Combination Food Type” and “Source of Food.” When foods were judged to be a hand-made recipe, the classification was applied to the underlying ingredients (SR codes) to ensure a more accurate classification. Details about the calculations for energy values are described in detail elsewhere (33). The energy contribution from all ultra-processed foods was summed and divided by the participant's total energy intake. Thus, the primary outcome for this analysis is the % of total energy (in kilocalories) from ultra-processed foods, averaging over 2 d of dietary recalls.
Study covariates
Sociodemographic and health covariates were included in the analyses because they were hypothesized to be common predictors of household food security and dietary intake. Sociodemographic covariates included age (in 5-y increments), sex, self-reported race/ethnicity (Non-Hispanic white, Non-Hispanic black, Hispanic, Other or multi-race/ethnicity), educational attainment (<12 y, high school diploma or equivalent, some college, college graduate or higher), family income to poverty ratio (as linear and quadratic terms), marital status (married or living with partner, never married, separated/widowed/divorced), and survey year (in 2-y NHANES cycles). Health covariates included smoking status (never smoker, former smoker, current smoker), vigorous physical activity (any, none), moderate physical activity (any, none), and total energy intake (as a linear term). Individuals with missing data on study covariates were also excluded from the analytic population: education (n = 11), marital status (n = 7), smoking status (n = 9), vigorous physical activity (n = 2), and moderate physical activity (n = 2).
Statistical analysis
Complex sampling weights were used to account for different sampling probabilities, nonresponse, and to make nationally representative estimates. Dietary weights were recalculated to reflect the probability of being sampled in the 10-y period according to NCHS guidelines and applied to all analyses.
First, we examined differences in sociodemographic and health characteristics by household food security status in adults with family incomes ≤300% FPL using χ2 tests and univariate linear regression models. Second, we evaluated the associations between household food security and ultra-processed food consumption using unadjusted and multivariate linear regression models. Unadjusted and adjusted means of ultra-processed food intake were computed using least squared means in the respective linear regression models. Trend tests were conducted by including household food security as an ordinal variable. Next, we examined the associations between SNAP participation and ultra-processed food consumption using unadjusted and multivariate linear regression models. In sensitivity analyses, we examined the associations between household food security and SNAP participation with individual categories of ultra-processed foods, adjusting for all study covariates. Finally, we examined whether the associations between household food security and ultra-processed food intake were modified by SNAP participation by including a multiplicative interaction term in the multivariate model. Where statistical interaction was found, least squared means of ultra-processed food intake were stratified by subgroups of interest.
All statistical tests were 2-sided and significance was considered at P < 0.05. Statistical analyses were performed using SAS 9.4 (SAS Institute Inc.).
Results
In the analytic population of 9190 adults with incomes ≤300% FPL, 56.1% of adults had full food security, 15.1% had marginal food security, 17.5% had low food security, and 11.3% had very low food security. Differences in sociodemographic and health covariates by food security status are shown in Table 1. Compared with food-secure adults, adults with marginal, low, or very low food security were more likely to be younger, of minority race/ethnicity, have lower incomes, have lower educational attainment, be a current smoker, be less likely to be married or partnered, and be or engage in any vigorous or moderate physical activity. Adults with more severe food insecurity were also more likely to be financially eligible for SNAP and report receiving SNAP benefits in the past 12 mo. For example, among adults with low food security, 42.6% participated in SNAP over the previous year and 28.0% were income-eligible but did not participate in SNAP. Among adults with very low food security, 50.0% participated in SNAP over the previous year and 28.2% were income-eligible but did not participate.
TABLE 1.
Sociodemographic and health characteristics of 9190 adults with family incomes ≤300% of the FPL, NHANES 2007–20161
| Food security | ||||||
|---|---|---|---|---|---|---|
| Overall (n = 9190) | Secure (n = 4671) | Marginal (n = 1490) | Low (n = 1859) | Very low (n = 1170) | P value | |
| Age, y | 39.6 ± 0.4 | 40.1 ± 0.5 | 39.3 ± 0.6 | 38.2 ± 0.5 | 39.8 ± 0.7 | 0.01 |
| Income to poverty ratio | 1.43 ± 0.02 | 1.65 ± 0.03 | 1.35 ± 0.04 | 1.10 ± 0.03 | 0.99 ± 0.04 | <0.0001 |
| Sex | 0.12 | |||||
| Male | 4199 (46.3) | 2205 (47.7) | 642 (43.2) | 830 (44.9) | 522 (46.0) | |
| Female | 4991 (53.7) | 2466 (52.3) | 848 (56.8) | 1029 (55.1) | 648 (54.0) | |
| Race/ethnicity | <0.0001 | |||||
| Non-Hispanic white | 3300 (54.2) | 1892 (61.7) | 426 (43.8) | 538 (41.9) | 444 (49.9) | |
| Non-Hispanic black | 2052 (15.0) | 943 (12.1) | 370 (18.4) | 443 (18.2) | 296 (20.0) | |
| Hispanic | 3024 (22.9) | 1356 (17.8) | 566 (28.7) | 747 (33.7) | 355 (24.3) | |
| Other or multi-race | 814 (7.8) | 480 (8.5) | 128 (9.0) | 131 (6.2) | 75 (5.9) | |
| Educational attainment | <0.0001 | |||||
| <12 y | 2784 (24.0) | 1177 (18.6) | 443 (23.4) | 738 (36.1) | 426 (32.5) | |
| High school diploma or equivalent | 2377 (27.0) | 1173 (26.2) | 406 (29.0) | 492 (26.3) | 306 (29.9) | |
| Some college | 2801 (33.2) | 1474 (33.8) | 462 (34.6) | 499 (30.6) | 366 (31.9) | |
| College graduate or higher | 1228 (15.9) | 847 (21.4) | 179 (13.0) | 130 (7.1) | 72 (5.7) | |
| Marital status | <0.0001 | |||||
| Married or living with partner | 5043 (54.1) | 2657 (56.2) | 822 (55.2) | 1021 (52.9) | 543 (43.8) | |
| Never married | 2304 (27.7) | 1165 (28.1) | 363 (25.8) | 471 (27) | 305 (29.3) | |
| Separated, widowed, or divorced | 1843 (18.3) | 849 (15.7) | 305 (19.1) | 367 (20.1) | 322 (26.9 | |
| Smoking status | <0.0001 | |||||
| Never smoker | 4898 (51.9) | 2627 (54.8) | 832 (52.9) | 946 (51.4) | 493 (37.4) | |
| Former smoker | 1680 (8.7) | 916 (20.7) | 268 (19.0) | 321 (14.8) | 175 (14.4) | |
| Current smoker | 2612 (29.4) | 1128 (24.5) | 390 (28.1) | 592 (33.8) | 502 (48.2) | |
| Vigorous physical activity (any) | 1883 (23.9) | 1026 (26.2) | 313 (23.2) | 327 (20.2) | 217 (19.3) | 0.001 |
| Moderate physical activity (any) | 3334 (40.2) | 1830 (44.5) | 510 (37.8) | 610 (33.3) | 384 (32.5) | <0.0001 |
| Survey year | <0.0001 | |||||
| 2007–08 | 1851 (19.6) | 1086 (22.4) | 258 (14.4) | 334 (19.5) | 173 (12.6) | |
| 2009–10 | 2063 (19.3) | 1020 (19.9) | 329 (18.2) | 434 (18.6) | 280 (19.2) | |
| 2011–12 | 1805 (20.4) | 896 (19.5) | 313 (21.3) | 350 (19) | 246 (25.9) | |
| 2013–14 | 1790 (20.6) | 910 (20.6) | 279 (19.3) | 363 (21.6) | 238 (20.7) | |
| 2015–16 | 1681 (20.2) | 759 (17.7) | 311 (26.8) | 378 (21.3) | 233 (21.6) | |
| SNAP participation status | <0.0001 | |||||
| Participant | 2744 (25.4) | 879 (14.5) | 473 (27.7) | 815 (42.6) | 577 (50.0) | |
| Income-eligible nonparticipant | 2585 (25.4) | 1264 (23.7) | 428 (26.4) | 544 (28.0) | 349 (28.2) | |
| Income-ineligible nonparticipant | 3861 (49.2) | 2528 (61.7) | 589 (45.9) | 500 (29.5) | 244 (21.8) | |
Values are presented as mean ± SD or n (%). FPL, Federal Poverty Level; SNAP, Supplemental Nutrition Assistance Program.
From univariate linear regression or chi-squared.
The associations between household food security and ultra-processed food intake are shown in Table 2. Across food security groups, the unadjusted means for percentage energy intake from ultra-processed foods ranged from 56.0% to 60.1%. After adjusting for sociodemographic and health characteristics, adults with very low food security consumed 55.7% energy intake from ultra-processed foods (95% CI: 54.1%, 57.4%), ∼3.1% more than adults with high food security (P = 0.002). There was a dose-response relation, such that more severe food insecurity was associated with higher ultra-processed food intake (P-trend = 0.003). Sensitivity analysis of individual ultra-processed food categories showed significant associations between more severe food insecurity and higher intakes of pizza (P-trend = 0.002) and soft drinks (P-trend = 0.02) (Supplemental Table 1).
TABLE 2.
Associations between household food security and percentage energy intake (in kcal) from ultra-processed foods, NHANES 2007–2016 (n = 9190)1
| Household food security | n | Unadjusted mean (95% CI) | Adjusted mean (95% CI) |
|---|---|---|---|
| High | 4671 | 56.0 (54.9, 57.2) | 52.6 (51.6, 53.7) |
| Marginal | 1490 | 56.4 (54.9, 57.8) | 53.6 (52.2, 55.0) |
| Low | 1859 | 57.2 (55.6, 58.7) | 53.7 (52.3, 55.1) |
| Very low | 1170 | 60.12 (58.5, 61.7) | 55.72 (54.1, 57.4) |
| P-trend3 | 0.002 | 0.003 |
Least squared means from multivariable linear regression models were used to estimate mean % energy from ultra-processed foods adjusting for age (in 5-y increments), sex, race/ethnicity, educational attainment, family income to poverty ratio (continuous and squared term), marital status, smoking status, vigorous physical activity, moderate physical activity, survey year, and total energy intake.
2Significantly different from high food security.
3 P values for trend were obtained from linear regression models including household food security as an ordinal variable.
The associations between SNAP participation and ultra-processed food intake are shown in Table 3. Compared with both income-eligible nonparticipants (55.6%) and income-ineligible nonparticipants (56.0%), SNAP participants had higher unadjusted means (59.3%) of energy intake from ultra-processed foods. After adjustment for sociodemographic and health characteristics and household food security, the data indicated that compared with income-eligible nonparticipants, SNAP participants consumed 1.7% more of their energy intake from ultra-processed foods (P = 0.04). The contrast in adjusted means between SNAP participants and income-ineligible nonparticipants was not statistically significant (P > 0.05). Sensitivity analysis of individual ultra-processed food categories showed that the difference in ultra-processed food intake between SNAP participants and income-eligible nonparticipants was driven by higher intakes of salty snacks and soft drinks (Supplemental Table 2).
TABLE 3.
Associations between SNAP participation status and percentage energy intake (in kcal) from ultra-processed foods, NHANES 2007–2016 (n = 9190)1
| SNAP participation | n | Unadjusted mean (95% CI) | Adjusted mean (95% CI) |
|---|---|---|---|
| SNAP participants | 2744 | 59.3 (58.1, 60.5) | 54.7 (53.0, 56.3) |
| Income-eligible nonparticipants | 2585 | 55.62 (54.2, 57.1) | 53.02 (51.5, 54.5) |
| Income-ineligible nonparticipants | 3861 | 56.02 (54.8, 57.1) | 53.9 (52.4, 55.3) |
Least squared means from multivariable linear regression models were used to estimate mean percentage of energy from ultra-processed foods (adjusting for age in 5-y increments), sex, race/ethnicity, educational attainment, family income to poverty ratio (continuous and squared term), marital status, smoking status, vigorous physical activity, moderate physical activity, survey year, total energy intake, and household food security status. SNAP, Supplemental Nutrition Assistance Program.
Significantly different from SNAP participants.
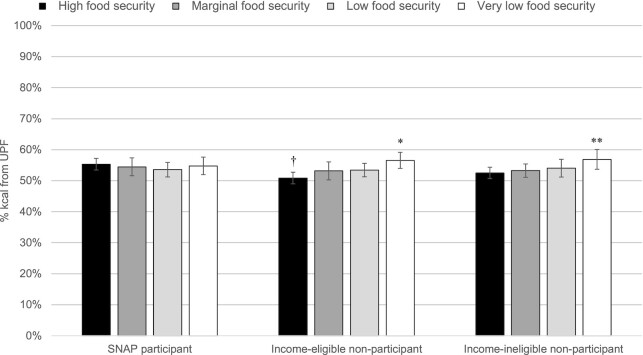
Furthermore, SNAP participation status modified the associations between household food security and ultra-processed food consumption (P-interaction = 0.02). The least squared means of ultra-processed food consumption in relation to household food security and SNAP participation status are shown in Figure 1. Among income-eligible nonparticipants, adults with very low food security consumed 5.4% more of their energy intake from ultra-processed foods than adults with high food security (P = 0.0002). Similarly, among income-ineligible nonparticipants, compared with adults with high food security adults with very low food security consumed 4.0% more of their energy intake from ultra-processed foods (P = 0.03). Among SNAP participants, the associations were attenuated; there were no significant associations between household food security and ultra-processed food consumption. However, among adults with full food security, SNAP participants had significantly higher intake of ultra-processed foods than income-eligible nonparticipants (P = 0.002). No other comparisons within household food security groups by SNAP participation status were statistically significant.
FIGURE 1.
Least squared means from multivariable linear regression models of ultra-processed food intake by household food security status and SNAP participation adjusted for sociodemographic and health characteristics, NHANEs 2007–2016 (n = 9190). P-interaction between household food security and SNAP participation was 0.02. *Significant difference from income-eligible nonparticipants with high food security P = 0.0002; **significant difference from income-ineligible nonparticipants with high food security P = 0.03; †significant difference from SNAP participants with high food security P = 0.002. SNAP, Supplemental Nutrition Assistance Program.
Discussion
In recent decades, there have been stark increases in the availability and consumption of ultra-processed foods on a global scale (34–40). Ultra-processed foods now comprise over half of all Americans’ daily calories (21), and their intake has contributed to increased risks of obesity, type 2 diabetes, cardiovascular disease, and even depression (41, 42). To our knowledge, this is the first study to examine the associations between household food security and SNAP participation with ultra-processed food consumption. We provide evidence of a graded relation between food insecurity and ultra-processed food consumption in a large, national sample of adults with family incomes ≤300% FPL, and this result furthered differed by SNAP participation status. These findings corroborate prior studies of food insecurity and diet quality, and further suggest that higher consumption of ultra-processed foods may contribute to the observed disparities in cardiometabolic health outcomes by food insecurity and SNAP participation status (5, 14).
It has been posited that the high cost of fruits, vegetables, and other healthful and less processed foods and the limited availability of these foods in the surrounding food environment can explain the inverse associations between socioeconomic status and diet quality (43). However, the contribution of economic and environmental factors to the observed disparities has been challenged by additional research (44–46). We hypothesize that psychological, neurological, and behavioral pathways are potentially important mediators of the associations between food insecurity and ultra-processed food consumption (and by association, overall diet quality). Specifically, we elaborate below on the intersecting and compounding roles of psychological distress specific to food insecurity, the addictive potential of ultra-processed foods, and the coping strategies used during periods of food insecurity in the context of the observed associations.
First, food insecurity is an inherently stressful experience. Studies have found that food insecurity is associated with greater perceived stress, trait anxiety, depressive symptoms, and serious psychological distress in low-income adults (47–52). Chronic stress is known to activate the hypothalamus–pituitary–adrenal axis, stimulating the release of cortisol, which alters certain metabolic processes. Chronic stress drives consumption of ultra-processed foods high in fat and sugar, which dampens the stress response in the short term but promotes visceral fat accumulation and increases chronic disease risk in the long term (53, 54). Health psychologists have termed this model “reward-based stress eating” or “comfort eating” (53, 54)—a paradigm that food-insecure populations may be counterintuitively more vulnerable to in response to the chronic stress they experience, as suggested by our findings.
Second, this issue is compounded by the way in which the consumption of ultra-processed foods activates neural reward pathways (55) and is associated with behavioral patterns indicative of addictive disorders, including diminished control over consumption, continued use despite negative consequences, and withdrawal (56). Individuals with low incomes and/or those experiencing food insecurity may be especially vulnerable to the addictive consumption of ultra-processed foods due to the dominance of these foods in their food environment and targeted marketing by the food industry (57). Further, psychological distress can increase the appeal of addictive substances, which further increases the vulnerability of low-income individuals to the addictive nature of ultra-processed foods (58).
And finally, coping strategies for food insecurity may reinforce consumption of ultra-processed foods. Studies have found that food-insecure families tend to keep ultra-processed microwavable or frozen meals in the home and feed their children more grains, mixed dishes, and processed meats as a strategy to cope with food insecurity (59, 60). These and other studies suggest that low-income adults may selectively seek out ultra-processed foods to ensure sufficient food for their household during food-related hardship. Future research should focus on examining the psychological and neurological mechanisms that reinforce the observed associations (61, 62).
We further found that compared with income-eligible nonparticipants and income-ineligible nonparticipants, SNAP participants had the highest level of ultra-processed food intake. Although this finding is consistent with prior studies of SNAP participation and diet quality (18, 63), the association is likely not causal. Some of this difference may be attributable to selective participation in the program, such that individuals who participate in the program are already at higher risk of food insecurity, poverty, and poor health. However, it is widely known that SNAP benefits are inadequate, leading to difficulties in food procurement and heightened coping strategies toward the end of the month (64–66). According to a recent USDA report, nearly 9 out of 10 SNAP participants reported challenges in eating a healthy diet, with cost, time, and transportation representing key barriers (67). Compared with income-eligible nonparticipants, the higher levels of ultra-processed food consumption among SNAP participants may be indicative of the coping strategies used to manage food insecurity, further magnified by the constraints of insufficient SNAP benefits and other structural barriers to healthy eating.
Furthermore, SNAP participation modified the association between food insecurity and ultra-processed food consumption. Among both income-eligible and income-ineligible nonparticipants, greater severity of food insecurity was associated with higher consumption of ultra-processed food in a graded fashion. Although this pattern was not observed among SNAP participants, SNAP participants with high food security had higher intakes of ultra-processed foods than their nonparticipant counterparts at the same level of food security. Further research examining the eating patterns of SNAP participants over the monthly benefit cycle and at varying levels of benefit issuance are needed to better understand this nuanced association.
These findings have important policy implications. Given the reality that ultra-processed foods will remain ubiquitous in the food environment and, in the United States, few limits on marketing such products are viable options, policies that increase access to and affordability of less processed and unprocessed products are important to minimize obstacles to accessing alternatives to ultra-processed foods. In the last decade, nutrition-related interventions for SNAP have focused on incentivizing and increasing the purchasing power for fruits and vegetables. Results from these interventions and related projects have demonstrated that financial incentives are successful in increasing fruit and vegetable intake (68). A simulation study estimated that incentivizing fruits and vegetable intake would prevent >300,000 cardiovascular events and save $6.8 billion in healthcare costs (69). Another recent USDA proposed rule would have also strengthened the stocking standards for SNAP-authorized food stores, mandating a greater array of fresh and shelf-stable foods (70). However, this rule was relaxed prior to being finalized (71). Changing SNAP stocking standards could be another important policy mechanism in shifting the availability toward minimally processed foods and away from ultra-processed foods in low-income communities. These strategies are also aligned with the growing national focus on nutrition insecurity and opportunity to use SNAP as a lever to alleviate the dual burden of food insecurity and cardiometabolic disease in low-income populations (72).
Our study is strengthened by the use of a large and representative sample of lower-income adults surveyed over a recent 10-y period. The primary limitation of our study is the cross-sectional nature of the data, which precludes the ability to understand how patterns in food insecurity or SNAP participation influence dietary intake over time. Despite the inclusion of several sociodemographic characteristics, there remains the possibility of unmeasured confounding by contextual factors, such as neighborhood socioeconomic status and food availability, family structure, and other individual-level traits that might influence food insecurity, desire to receive federal assistance, and health behaviors. Another limitation is the use of 24-h dietary recalls, which may be subject to social desirability bias and lead to an underestimation of the dietary contribution of ultra-processed foods. However, this bias is unlikely to affect the observed differences across categories of household food security and SNAP participation status. The standardized approach to collecting 24-h dietary recalls has also been shown to produce accurate intake estimates with minimal measurement error or bias (73, 74). Although NHANES collects some information indicative of food processing, these data are not consistently determined for all food items, which could lead to modest over- or underestimation of the consumption of ultra-processed foods. There are also other food processing classification systems, such as those developed by the International Food Information Council and University of North Carolina at Chapel Hill (75). Results of investigations of associations between household food security and SNAP participation with ultra-processed food consumption may differ depending on the classification system used. And finally, household food security was assessed over 12 mo preceding this report, which limits our understanding of how chronic or episodic food insecurity relates to ultra-processed food consumption. If the behavioral consequences of food insecurity are more likely to manifest toward the end of the month shortly before income or SNAP benefits are replenished, then this situation may lead to changes in dietary coping mechanisms. Future studies that incorporate repeated assessments of household food security and dietary intake throughout the weeks of a month are needed to tease out these associations.
Ultra-processed food consumption is a risk factor for cardiometabolic and mental health outcomes. Our findings showed that food-insecure adults and adults receiving SNAP have greater consumption of ultra-processed foods than their counterparts, suggesting that ultra-processed food consumption may help to explain the diet-related health disparities observed in these populations. SNAP participation further modified the association between food insecurity and ultra-processed food consumption, such that this association was more pronounced for income-eligible and income-ineligible nonparticipants, and nonsignificant for SNAP participants. These findings support the need for robust programs and policies to simultaneously improve food and nutrition insecurities in low-income populations.
Supplementary Material
ACKNOWLEDGEMENTS
The authors’ responsibilities were as follows—CWL, APF, ANG, and JAW: designed the research; CWL and EM-S: performed statistical analysis; CWL, APF, LP, EM-S, ANG, and JAW: wrote the paper; CWL: had primary responsibility for final content; and all authors: read and approved the final manuscript. The authors report no conflicts of interest.
Notes
CWL was supported by the Eunice Kennedy Shriver National Institute for Child Health and Human Development (award #4R00HD084758). EM-S was supported by the Sao Paulo Research Foundation (FAPESP; Processo 2018/17972-9). JAW was supported by the National Institutes of Diabetes and Digestive and Kidney Diseases of the National Institutes of Health (award #K01DK119166).
Supplemental Figure 1 and Supplemental Tables 1–2 are available from the “Supplementary data” link in the online posting of the article and from the same link in the online table of contents at https://academic.oup.com/ajcn/.
Abbreviations used: EBT, Electronic Benefit Transfer; FPL, Federal Poverty Level; NCHS, National Center for Health Statistics; SNAP, Supplemental Nutrition Assistance Program.
Contributor Information
Cindy W Leung, Department of Nutritional Sciences, School of Public Health, University of Michigan, Ann Arbor, MI, USA.
Aarohee P Fulay, Department of Nutritional Sciences, School of Public Health, University of Michigan, Ann Arbor, MI, USA.
Lindsey Parnarouskis, Department of Psychology, College of Literature, Science, and Arts, University of Michigan, Ann Arbor, MI, USA.
Euridice Martinez-Steele, Center for Epidemiological Studies in Health and Nutrition, University of São Paulo, São Paulo, Brazil.
Ashley N Gearhardt, Department of Psychology, College of Literature, Science, and Arts, University of Michigan, Ann Arbor, MI, USA.
Julia A Wolfson, Department of International Health, Johns Hopkins Bloomberg School of Public Health, Baltimore, MD, USA.
Data Availability
Data described in the manuscript, code book, and analytic code are publicly and freely available without restriction at https://www.cdc.gov/nchs/nhanes/index.htm.
References
- 1. Bickel G, Nord M, Price C, Hamilton W, Cook J. Guide to measuring household food security. Food and Nutrition Service. US Department of Agriculture; 2000. [Google Scholar]
- 2. Coleman-Jensen A, Rabbitt MP, Gregory CA, Singh A. Household food security in the United States in 2019, ERR-275. US Department of Agriculture, Economic Research Service; 2020. [Google Scholar]
- 3. Wolfson JA, Leung CW. Food insecurity during COVID-19: an acute crisis with long-term health implications. Am J Public Health. 2020;110(12):1763–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Fitzpatrick KM, Harris C, Drawve G, Willis DE. Assessing food insecurity among US adults during the COVID-19 pandemic. J Hunger Environ Nutr. 2021;16(1):1–18. [Google Scholar]
- 5. Hanson KL, Connor LM. Food insecurity and dietary quality in US adults and children: a systematic review. Am J Clin Nutr. 2014;100(2):684–92. [DOI] [PubMed] [Google Scholar]
- 6. Bhattacharya J, Currie J, Haider S. Poverty, food insecurity, and nutritional outcomes in children and adults. J Health Econ. 2004;23(4):839–62. [DOI] [PubMed] [Google Scholar]
- 7. Robaina KA, Martin KS. Food insecurity, poor diet quality, and obesity among food pantry participants in Hartford. J Nutr Educ Behav. 2013;45(2):159–64. [DOI] [PubMed] [Google Scholar]
- 8. Leung CW, Epel ES, Ritchie LD, Crawford PB, Laraia BA. Food insecurity is inversely associated with diet quality of lower-income adults. J Acad Nutr Diet. 2014;114(12):1943–1953.e2. [DOI] [PubMed] [Google Scholar]
- 9. Leung CW, Tester JM. The association between food insecurity and diet quality varies by race/ethnicity: an analysis of National Health And Nutrition Examination Survey 2011–2014 results. J Acad Nutr Diet. 2019;119(10):1676–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Larson N, Laska MN, Neumark-Sztainer D. Food insecurity, diet quality, home food availability, and health risk behaviors among emerging adults: findings from the EAT 2010–2018 study. Am J Public Health. 2020;110(9):1422–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Seligman HK, Bindman AB, Vittinghoff E, Kanaya AM, Kushel MB. Food insecurity is associated with diabetes mellitus: results from the National Health Examination And Nutrition Examination Survey (NHANES) 1999–2002. J Gen Intern Med. 2007;22(7):1018–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Seligman HK, Laraia BA, Kushel MB. Food insecurity is associated with chronic disease among low-income NHANES participants. J Nutr. 2010;140(2):304–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Parker ED, Widome R, Nettleton JA, Pereira MA. Food security and metabolic syndrome in US adults and adolescents: findings from the National Health And Nutrition Examination Survey, 1999–2006. Ann Epidemiol. 2010;20(5):364–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Laraia B. Food insecurity and chronic disease. Adv Nutr. 2013;4(2):203–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. [Internet] [Accessed 2020 Jun 26]. Available from: https://fns-prod.azureedge.net/sites/default/files/resource-files/SNAPsummary-7.pdf. [Google Scholar]
- 16. Nord M. How much does the Supplemental Nutrition Assistance Program alleviate food insecurity? Evidence from recent programme leavers. Public Health Nutr. 2012;15(5):811–7. [DOI] [PubMed] [Google Scholar]
- 17. Nord M, Golla AM. Does SNAP decrease food insecurity? Untangling the self-selection effect. Economic Research Service, US Department of Agriculture, 2009. [Google Scholar]
- 18. Zhang FF, Liu J, Rehm CD, Wilde P, Mande JR, Mozaffarian D. Trends and disparities in diet quality among US adults by Supplemental Nutrition Assistance Program participation status. JAMA Network Open. 2018;1(2):e180237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Andreyeva T, Tripp AS, Schwartz MB. Dietary quality of Americans by Supplemental Nutrition Assistance Program participation status: a systematic review. Am J Prev Med. 2015;49(4):594–604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Jaime PC, Campello T, Monteiro CA, Bortoletto AP, Bomfim MYM. Ultra-processed food products: solutions for healthy and sustainable food systems. Sao Paulo (Brazil): Catedra Josue de Castro and Center for Epidemiological Research in Nutrition and Health (Nupens); 2021. [Google Scholar]
- 21. Baraldi LG, Martinez Steele E, Canella DS, Monteiro CA. Consumption of ultra-processed foods and associated sociodemographic factors in the USA between 2007 and 2012: evidence from a nationally representative cross-sectional study. BMJ Open. 2018;8(3):e020574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Hall KD, Ayuketah A, Brychta R, Cai H, Cassimatis T, Chen KY, Chung ST, Costa E, Courville A, Darcey Vet al. . Ultra-Processed diets cause excess calorie intake and weight gain: an inpatient randomized controlled trial of ad libitum food intake. Cell Metabolism. 2019;30(1):226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Rauber F, Chang K, Vamos EP, da Costa Louzada ML, Monteiro CA, Millett C, Levy RB. Ultra-processed food consumption and risk of obesity: a prospective cohort study of UK Biobank. Eur J Nutr. 2021;60(4):2169–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Beslay M, Srour B, Mejean C, Alles B, Fiolet T, Debras C, Chazelas E, Deschasaux M, Wendeu-Foyet MG, Hercberg Set al. . Ultra-processed food intake in association with BMI change and risk of overweight and obesity: a prospective analysis of the French nutrinet-Sante cohort. PLoS Medicine. 2020;17(8):e1003256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. CDC . Home page. [Internet]. [Accessed 2021 Jul 5]. Available from: http://www.cdc.gov/nchs/nhanes.htm. [Google Scholar]
- 26. Gamba R, Leung CW, Guendelman S, Lahiff M, Laraia B. Household food insecurity is not associated with overall diet quality among pregnant women in NHANES 1999–2008. Matern Child Health J. 2016;20(11):2348–56. [DOI] [PubMed] [Google Scholar]
- 27. U.S. Household Food Security Survey Module: three-stage design, with screeners. Economic Research Service, US Department of Agriculture; 2012. [Google Scholar]
- 28. National Health and Nutrition Examination Survey (NHANES)—MEC in-person dietary interviewers procedures manual. National Center for Health Statistics; 2010. [Google Scholar]
- 29. National Health and Nutrition Examination Survey (NHANES)—phone follow-up dietary interviewer procedures manual. National Center for Health Statistics; 2010. [Google Scholar]
- 30. Ahluwalia N, Dwyer J, Terry A, Moshfegh A, Johnson C. Update on NHANES dietary data: focus on collection, release, analytical considerations, and uses to inform public policy. Adv Nutr. 2016;7(1):121–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Baranowski T. 24-Hour recall and diet record methods. In: Willett WC, editor. Nutritional Epidemiology. New York, NY: Oxford University Press; 2012, pp. 49–69. [Google Scholar]
- 32. Monteiro CA, Cannon G, Moubarac JC, Levy RB, Louzada MLC, Jaime PC. The UN decade of nutrition, the NOVA food classification and the trouble with ultra-processing. Public Health Nutr. 2018;21(1):5–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Martinez Steele E, Baraldi LG, Louzada ML, Moubarac JC, Mozaffarian D, Monteiro CA. Ultra-processed foods and added sugars in the US diet: evidence from a nationally representative cross-sectional study. BMJ Open. 2016;6(3):e009892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Moubarac JC, Batal M, Martins AP, Claro R, Levy RB, Cannon G, Monteiro C. Processed and ultra-processed food products: consumption trends in Canada from 1938 to 2011. Can J Diet Pract Res. 2014;75(1):15–21. [DOI] [PubMed] [Google Scholar]
- 35. Marron-Ponce JA, Tolentino-Mayo L, Hernandez FM, Batis C. Trends in ultra-processed food purchases from 1984 to 2016 in Mexican households. Nutrients. 2018;11(1):45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Juul F, Hemmingsson E. Trends in consumption of ultra-processed foods and obesity in Sweden between 1960 and 2010. Public Health Nutr. 2015;18(17):3096–107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Shim JS, Shim SY, Cha HJ, Kim J, Kim HC. Socioeconomic characteristics and trends in the consumption of ultra-processed foods in Korea from 2010 to 2018. Nutrients. 2021;13(4):1120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Vandevijvere S, Jaacks LM, Monteiro CA, Moubarac JC, Girling-Butcher M, Lee AC, Pan A, Bentham J, Swinburn B. Global trends in ultra-processed food and drink product sales and their association with adult body mass index trajectories. Obes Rev. 2019;20(S2):10–9. [DOI] [PubMed] [Google Scholar]
- 39. Juul F, Parekh N, Martinez-Steele E, Monteiro CA, Chang VW. Ultra-processed food consumption among US adults from 2001 to 2018. Am J Clin Nutr. 2021;115(1):211–21. [DOI] [PubMed] [Google Scholar]
- 40. Wang L, Martinez Steele E, Du M, Pomeranz JL, O'Connor LE, Herrick KA, Luo H, Zhang X, Mozaffarian D, Zhang FF. Trends in consumption of ultra-processed foods among US youths aged 2–19 years, 1999–2018. JAMA. 2021;326(6):519–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Elizabeth L, Machado P, Zinocker M, Baker P, Lawrence M. Ultra-processed foods and health outcomes: a narrative review. Nutrients. 2020;12(7):1955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Chen X, Zhang Z, Yang H, Qiu P, Wang H, Wang F, Zhao Q, Fang J, Nie J. Consumption of ultra-processed foods and health outcomes: a systematic review of epidemiological studies. Nutr J. 2020;19(1):86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Darmon N, Drewnowski A. Does social class predict diet quality?. Am J Clin Nutr. 2008;87(5):1107–17. [DOI] [PubMed] [Google Scholar]
- 44. Caspi CE, Sorensen G, Subramanian SV, Kawachi I. The local food environment and diet: a systematic review. Health Place. 2012;18(5):1172–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Variyam JN, Blaylock J, Smallwood D. USDA's Healthy Eating Index and Nutrition Information (Technical Bulletin No. 1866). Washington (DC): US Department of Agriculture; 1998. [Google Scholar]
- 46. Laraia BA, Leak TM, Tester JM, Leung CW. Biobehavioral factors that shape nutrition in low-income populations: a narrative review. Am J Prev Med. 2017;52(2):S118–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Lindow P, Yen IH, Xiao M, Leung CW. “You run out of hope:” an exploration of low-income parents’ experiences with food insecurity using photovoice. Public Health Nutr. 2022;25(4):987–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Laraia BA, Siega-Riz AM, Gundersen C, Dole N. Psychosocial factors and socioeconomic indicators are associated with household food insecurity among pregnant women. J Nutr. 2006;136(1):177–82. [DOI] [PubMed] [Google Scholar]
- 49. Laraia B, Vinikoor-Imler LC, Siega-Riz AM. Food insecurity during pregnancy leads to stress, disordered eating, and greater postpartum weight among overweight women. Obesity. 2015;23(6):1303–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Tsuchiya K, Leung CW, Jones AD, Caldwell CH. Multiple financial stressors and serious psychological distress among adults in the USA. Int J Public Health. 2020;65(3):335–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Myers CA. Food insecurity and psychological distress: a review of the recent literature. Curr Nutr Rep. 2020;9(2):107–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Wolfson JA, Garcia T, Leung CW. Food insecurity is associated with depression, anxiety, and stress: evidence from the early days of the COVID-19 pandemic in the United States. Health Equity. 2021;5(1):64–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Adam TC, Epel ES. Stress, eating and the reward system. Physiol Behav. 2007;91(4):449–58. [DOI] [PubMed] [Google Scholar]
- 54. Tomiyama AJ, Dallman MF, Epel ES. Comfort food is comforting to those most stressed: evidence of the chronic stress response network in high stress women. Psychoneuroendocrinology. 2011;36(10):1513–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Small DM, DiFeliceantonio AG. Processed foods and food reward. Science. 2019;363(6425):346–7. [DOI] [PubMed] [Google Scholar]
- 56. Schulte EM, Avena NM, Gearhardt AN. Which foods may be addictive? The roles of processing, fat content, and glycemic load. PloS One. 2015;10(2):e0117959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Nguyen KH, Glantz SA, Palmer CN, Schmidt LA. Transferring racial/ethnic marketing strategies from tobacco to food corporations: Philip Morris and Kraft General Foods. Am J Public Health. 2020;110(3):329–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Sinha R, Jastreboff AM. Stress as a common risk factor for obesity and addiction. Biol Psychiatry. 2013;73(9):827–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Nackers LM, Appelhans BM. Food insecurity is linked to a food environment promoting obesity in households with children. J Nutr Educ Behav. 2013;45(6):780–4. [DOI] [PubMed] [Google Scholar]
- 60. Burke MP, Martini LH, Blake CE, Younginer NA, Draper CL, Bell BA, Liese AD, Jones SJ. Stretching food and being creative: Caregiver responses to child food insecurity. J Nutr Educ Behav. 2017;49(4):296–303.e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Dong KR, Tang AM, Stopka TJ, Beckwith CG, Must A. Food acquisition methods and correlates of food insecurity in adults on probation in Rhode Island. PloS One. 2018;13(6):e0198598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Dachner N, Ricciuto L, Kirkpatrick SI, Tarasuk V. Food purchasing and food insecurity among low-income families in Toronto. Can J Diet Pract Res. 2010;71(3):e50–6. [DOI] [PubMed] [Google Scholar]
- 63. Leung CW, Ding EL, Catalano PJ, Villamor E, Rimm EB, Willett WC. Dietary intake and dietary quality of low-income adults in the Supplemental Nutrition Assistance Program. Am J Clin Nutr. 2012;96(5):977–88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Hamrick KS, Andrews M. SNAP participants’ eating patterns over the benefit month: a time use perspective. PloS One. 2016;11(7):e0158422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Whiteman ED, Chrisinger BW, Hillier A. Diet quality over the monthly Supplemental Nutrition Assistance Program cycle. Am J Prev Med. 2018;55(2):205–12. [DOI] [PubMed] [Google Scholar]
- 66. Sanjeevi N, Freeland-Graves J. Monthly variations in dietary intake of women participating in the Supplemental Nutrition Assistance Program. J Acad Nutr Diet. 2019;119(2):261–71. [DOI] [PubMed] [Google Scholar]
- 67. Gearing M, Dixit-Joshi S, May L. Barriers that constrain the adequacy of Supplemental Nutrition Assistance Program (SNAP) allotments. Westat, Inc., for the USDA. Food and Nutrition Service. 2021. [Google Scholar]
- 68. Bartlett S, Klerman J, Olsho L, Logan C, Blocklin M, Beauregard M, Enver A, Associates A. Evaluation of the Healthy Incentives Pilot (HIP): final report. Alexandria: Food and Nutrition Service. US Department of Agriculture; 2014. [Google Scholar]
- 69. Mozaffarian D, Liu J, Sy S, Huang Y, Rehm C, Lee Y, Wilde P, Abrahams-Gessel S, de Souza Veiga Jardim T, Gaziano Tet al. . Cost-effectiveness of financial incentives and disincentives for improving food purchases and health through the US Supplemental Nutrition Assistance Program (SNAP): a microsimulation study. PLoS Medicine. 2018;15(10):e1002661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. Enhancing retailer standards in the Supplemental Nutrition Assistance Program (SNAP)—proposed rule. In: Food and Nutrition Service USDA, ed., 2016:8015–21. [Google Scholar]
- 71. Enhancing retailer standards in the Supplemental Nutrition Assistance Program (SNAP) [FNS-2016–0018]. In: U.S. Department of Agriculture FaNS, ed., 2016:90675–99. [Google Scholar]
- 72. Mozaffarian D, Fleischhacker S, Andres JR. Prioritizing nutrition security in the US. JAMA. 2021;325(16):1605–6. [DOI] [PubMed] [Google Scholar]
- 73. Moshfegh AJ, Rhodes DG, Baer DJ, Murayi T, Clemens JC, Rumpler WV, Paul DR, Sebastian RS, Kuczynski KJ, Ingwersen LAet al. . The US department of agriculture automated multiple-pass method reduces bias in the collection of energy intakes. Am J Clin Nutr. 2008;88(2):324–32. [DOI] [PubMed] [Google Scholar]
- 74. Blanton CA, Moshfegh AJ, Baer DJ, Kretsch MJ. The USDA automated multiple-pass method accurately estimates group total energy and nutrient intake. J Nutr. 2006;136(10):2594–9. [DOI] [PubMed] [Google Scholar]
- 75. Bleiweiss-Sande R, Chui K, Evans EW, Goldberg J, Amin S, Sacheck J. Robustness of food processing classification systems. Nutrients. 2019;11(6):1344. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data described in the manuscript, code book, and analytic code are publicly and freely available without restriction at https://www.cdc.gov/nchs/nhanes/index.htm.