ABSTRACT
Background
Little is known about the role of emerging plant-based dietary patterns in cardiovascular disease (CVD) risk at the national population level.
Objectives
The objectives of this research were to assess the validity and reliability of newly established plant-based dietary indices, and to evaluate their associations with CVD risk among Canadian adults.
Methods
Data were obtained from repeated 24-h dietary recalls of adult participants in the cross-sectional, nationally representative Canadian Community Health Survey cycle 2004 linked to health administrative databases (n = 12,323) and cycle 2015 (n = 14,026). Plant-based diet quality was assessed with a revised Plant-based Dietary Index (PDI), EAT–Lancet Reference Diet (ERD) score, and the latest Dietary Guidelines for Americans Adherence Index (DGAI) 2020. Weighted multivariate analyses were used for testing associations between diet quality and lifestyle characteristics, and weighted multivariable-adjusted Cox proportional hazards models for associations with CVD risk.
Results
Construct validity was confirmed for the revised PDI and DGAI 2020 (but not the ERD) because participants in the highest (healthiest) quartile, compared to those in the lowest (least healthy), were more likely to be female (mean ± SE: 52.63% ± 1.27% compared with 44.80% ± 1.65% for revised PDI; 59.37% ± 2.01% compared with 40.84% ± 1.71% for DGAI 2020), older (mean ± SE: 50.55 ± 0.39 y compared with 45.56 ± 0.43 y for revised PDI; 51.57 ± 0.39 y compared with 46.35 ± 0.54 y for DGAI 2020), to have postsecondary education (mean ± SE: 32.36% ± 1.55% compared with 21.12% ± 1.31% for revised PDI; 34.17% ± 2.69% compared with 17.87% ± 0.98% for DGAI 2020), and less likely to be daily smokers (mean ± SE: 8.21% ± 1.0% compared with 17.06% ± 1.45% for revised PDI; 7.36% ± 1.71% compared with 21.53% ± 1.58% for DGAI 2020) (P-trend < 0.0001). No significant associations were observed between dietary index scores and CVD risk.
Conclusions
The revised PDI and DGAI 2020 provided valid and meaningful measures of plant-based eating among Canadians, whereas the validity of the ERD was not directly confirmed. Adherence to the plant-based dietary patterns was not associated with CVD risk. Future large-scale studies are necessary to further evaluate the role of plant-based eating in CVD prevention.
Keywords: cardiovascular disease (CVD), dietary patterns, plant-based diet, guidelines, validity, reliability, dietary index, a priori methods, incidence, mortality
Introduction
Cardiovascular disease (CVD) is the leading driver of noncommunicable disease burden in the world, with trends revealing an almost double increase in CVD prevalent cases and a steady rise in the number of deaths over the past 30 y (1). Poor diet is the one of the most prevalent preventable behavioral risk factors for CVD, accounting for more than half of all CVD-related deaths globally (2).
In recent years, the focus of international dietary guidelines for CVD prevention has largely shifted to plant-based dietary patterns, which have been proven essential for the regulation of blood lipid concentrations, oxidative stress, inflammation, visceral adiposity, and hyperglycemia (3–5). Adherence to a plant-based eating approach has also become a major public health priority in response to global food insecurity and environmental degradation. In an extensive report on healthy diets and sustainable food production, the 2019 EAT–Lancet Commission (6) concluded that a universal reference diet—high in plant protein, fruit, and vegetables and very low in animal products—was associated with the lowest risk of CVD incidence and mortality and with the least harmful environmental effects. Similarly, the need for a shift toward plant-based dietary patterns was echoed in the 2020–2025 Dietary Guidelines for Americans (DGA) (7), which strongly recommend “obtaining the majority of energy from plant-based foods, while limiting intakes of added sugars, solid fats, and sodium” for optimal cardiovascular health.
Although a growing number of studies have utilized various indices to measure adherence to plant-based eating patterns (8–10), only a few have explored associations with CVD risk in a general population (11–13) even though without an examination of performance of plant-based dietary indices. Using the Canadian national nutritional surveys linked with health administrative databases, the objectives of this research were: 1) to evaluate the validity and reliability of the emerging plant-based dietary indices, namely revised Plant-based Dietary Index (PDI) (14), the EAT–Lancet Reference Diet (ERD) score (15), and the Dietary Guidelines for Americans Adherence Index (DGAI) 2020 (16); and 2) to assess whether adherence to these dietary indices was associated with a lower risk of CVD incidence and mortality in a national sample of Canadian adults. We hypothesized that all dietary indices were valid and reliable measures of diet quality among Canadians, and that index scores would be significantly associated with CVD risk. To our knowledge, this is the first population-based study to update the 2015 DGAI (16) using the recently released 2020 DGA (7), and to compare the performance of emerging plant-based dietary indices in relation to CVD risk at the national population level.
Methods
Study population
Data used in this research were from the 2004 and 2015 cycles of the Canadian Community Health Survey (CCHS)-Nutrition (17, 18). The CCHS is a nationally representative cross-sectional survey, which collects information on health status, health determinants, and eating habits across Canada (19). Additional information on sampling design and survey procedures can be found elsewhere (17, 18). Data were collected in accordance with the Statistics Act of Canada with ethical approval granted by Statistics Canada. All participants gave informed consent to have their data shared and linked to health administrative databases.
The following exclusion criteria were applied to the CCHS-Nutrition 2015 cycle: individuals <18 y of age, breastfeeding women, individuals with invalid dietary recalls (as defined by Statistics Canada), and those with missing data on energy intake and physical activity. Exclusion criteria for CCHS-Nutrition 2004 included individuals <45 y and >80 y (for survival models), pregnant and breastfeeding women, individuals with invalid dietary recalls (as defined by Statistics Canada), residents of Quebec (for hospitalization records), those with heart diseases at baseline, and individuals with missing data on energy intake (Supplemental Methods). Pregnant women were excluded from cycle 2004 but retained for cycle 2015 analyses because the 2015 Public Use Microdata File (PUMF) has pregnancy status masked to protect confidentiality (20). Missing measured height and weight data were handled by using self-reported anthropometric measurements and applying a correction factor determined by Statistics Canada (21). The final analytical samples for CCHS-Nutrition 2004 and 2015 were comprised of 12,323 and 14,026 Canadian adults, respectively (Supplemental Figure 1).
All descriptive analyses on validity and reliability of the dietary indices, as well as population adherence, were conducted on CCHS-Nutrition 2015, whereas the longitudinal associations between dietary indices and CVD outcomes were attained using CCHS-Nutrition 2004 linked to health administrative databases (Supplemental Methods).
Exposure and outcome measurement
Dietary assessment
In both CCHS-Nutrition cycles, data on sociodemographic and lifestyle characteristics were captured through administration of a general health questionnaire. Detailed dietary intake data were collected using two 24-h dietary recalls (17, 18) via the Automated Multiple-Pass Method (AMPM) (22). Nutrient and energy compositions of reported foods were retrieved from Health Canada's Canadian Nutrient File (CNF) (23, 24).
Outcome ascertainment
The primary outcomes of interest were CVD incidence and mortality, which were represented by a single variable—CVD events—defined as CVD incident hospitalization cases or deaths. CVD events were defined by a group of disorders of the heart and blood vessels coded according to the International Statistical Classification of Diseases and Related Health Problems, 10th revision [ICD-10 (25)] as described previously (26, 27).
Dietary index scores used
Dietary Approaches to Stop Hypertension (DASH) index (28) (0–90 points) was chosen as a robust, widely used index with substantial known benefits for cardiovascular health to serve primarily as a reference tool for assessing the performance of the emerging plant-based dietary indices in this research (Supplemental Table 1). Unlike other DASH indices, the index developed by Matsunaga et al. (28) depends on calorie-based standards in equivalent units with 0–10 scores assigned to every component, in accordance with the energy levels recommended in the DASH eating plan (7, 29). The PDI by Satija et al. (14) (0–90 points) provides a scoring system that distinguishes between plant-based and animal-based products, consisting of 18 food groups which are further ranked into quintiles based on distributions of respondents’ intake (Supplemental Table 2). To address the differences in distribution of intake due to using 24-h dietary recalls in this research, as opposed to FFQs used in the original research by Satija et al. (14), scoring criteria of the original index were modified as follows: continuous proportional scores were assigned for consumptions >0 but below the 5th quintile, and a maximum score of 5 was assigned to individual intakes above the 5th quintile. The ERD score (0–14 points) was developed by Knuppel et al. (15) and reflects recommended consumption amounts in the ERD (6) (Supplemental Table 3). Finally, the DGAI 2020 (0–19 points) was devised by updating the 2015 DGAI (16) to assess adherence to the food-based energy recommendations and nutrient requirements laid out in the DGA 2020 and USDA Food Patterns (7) (Supplemental Table 4). We evaluated adherence to the DGA 2020 (7) instead of Canada's Food Guide 2019 (30) because the former uniquely provides quantitative dietary pattern recommendations for 12 energy levels based on age, sex, and daily physical activity. In the present study, the DGAI 2020 included 19 components owing to insufficient data on trans fat (one of the DGA nutrient components) in the CNF (23,24). A penalty of ≤0.5 points for overconsumption amounts ≥1.25 times higher than the recommended intake was exercised for energy-dense food groups, including dairy, proteins, starchy vegetables, and grains (31).
Statistical analyses
Statistical analyses were carried out using SAS software (version 9.4; SAS Institute Inc.). The complex sampling framework of the CCHS was addressed by using bootstrap balanced repeated replication method for variance estimation (32). To ensure national representativeness of findings, the sample survey weights provided by Statistics Canada were applied to all statistical analyses. All a priori diet quality indices were normally distributed and divided into quartiles on the basis of population distributions. Weighted and covariate-adjusted associations between dietary scores and lifestyle and sociodemographic characteristics were explored using multivariable linear regression and least-squares means for continuous and categorical variables, respectively. Statistical significance was defined by a 2-tailed P value < 0.05. Descriptive analyses focused on the first 24-h dietary recall from CCHS-Nutrition 2015.
Handling measurement errors in dietary intake reporting
In line with previous studies, systematic measurement error (misreporting) was accounted for by comparing estimated energy requirements (EERs) with energy intakes (EIs) (33). To calculate EERs, the Institute of Medicine (IOM) factorial equations were applied, based on age, sex, BMI, height, weight, and physical activity level. Under-reporters were represented by an EI <70% of EER, plausible reporters by 70% ≥ EI ≤ 142% of EER, and over-reporters by an EI >142% of EER (34, 35). Random measurement error was addressed using the National Cancer Institute (NCI) method (36) for estimating usual dietary intake (Supplemental Methods).
Testing the validity and reliability of diet quality indices
Face validity and construct validity were assessed to test whether the 4 dietary indices could distinguish between population subgroups with known differences in dietary habits (37, 38), and to evaluate trends in the association of dietary scores with energy and nutrient intakes. Because higher quality diets have been previously reported among women, older individuals, and nonsmokers, we also explored concurrent-criterion validity through examining dietary index scores in these 3 groups. Weighted Pearson correlation coefficients were calculated to ensure that dietary indices could measure diet quality of Canadians irrespective of diet quantity (i.e., EI). Finally, internal consistency of indices was evaluated using Cronbach's coefficient α by determining the degree of association between the different components of an index (39).
Because of the role of obesity (defined by a BMI ≥30 kg/m2) as a known mediator in the relationship between diet and CVD, the association of diet quality indices with risk of obesity was also examined as an additional test for construct validity, using weighted multinomial logistic regression in 4 successive a priori–defined models. Because some obese individuals are shown to be “metabolically healthy” (40, 41), we further stratified regression models to study the associations between dietary index scores and obesity with and without chronic disease (i.e., self-reported heart disease, cancer, diabetes, and hypertension).
Examining the association of diet quality index scores with CVD outcomes
The NCI method (36) was applied to both 24-h dietary recalls available from CCHS-Nutrition 2004 to address random measurement error and generate respondents’ “usual” index score distributions (Supplemental Methods). Weighted Cox proportional hazards models with person-days as the main time-metric were fitted to evaluate associations between adherence to the 4 dietary indices and CVD risk. All Cox models tested for sex interaction. Because scores were treated as continuous in the models, HRs and 95% CIs were computed at the mid-point of each index quintiles, with the 10th percentile serving as a reference.
Results
Validity and reliability of diet quality indices
All index scores were normally distributed (data not shown). Estimated mean (± SE) DASH index, revised PDI, ERD, and DGAI 2020 scores were 41.19 ± 0.25 out of 90, 38.8 ± 0.17 out of 90, 8.94 ± 0.04 out of 14, and 8.80 ± 0.04 out of 19, respectively. These results indicate that Canadians adhered to <50% of the recommendations outlined in the DASH diet, plant-based dietary patterns, and DGA 2020, and to 64% of recommendations proposed in the ERD.
The face validity and construct validity of the DASH index, revised PDI, and DGAI 2020 were confirmed because the total scores were associated with a number of sociodemographic and lifestyle characteristics (Table 1, Supplemental Table 5). Respondents in the fourth quartile (highest diet quality) of these 3 index scores, compared with those in the first quartile (lowest diet quality), were more likely to be older and in the possession of higher education, and much less likely to be daily smokers and breakfast skippers (P-trend < 0.0001). As for the ERD score, significant positive associations with higher diet quality scores were found only for immigration status (P-trend = 0.0113). After adjusting for age, and sex, higher diet quality was significantly associated with higher percentage of energy from carbohydrates and densities of fiber, vitamin C, folate, folacin, magnesium, and iron across all indices (P-trend < 0.0001) (Table 2, Supplemental Table 6). Adjusting for misreporting status did not have a profound effect on the direction and significance of any of these trends. When individual index components were examined, respondents in the highest quartile categories of the DASH index, revised PDI, ERD, and DGAI 2020 had the highest individual component scores (Supplemental Tables 7–10).
TABLE 1.
Weighted sociodemographic and lifestyle characteristics by quartiles of the DASH index, revised PDI, ERD score, and DGAI 2020 among Canadian adults (≥18 y old) from CCHS-Nutrition 20151
| DASH index | Revised PDI | ERD score | DGAI 2020 | |||||
|---|---|---|---|---|---|---|---|---|
| Quartile 1 | Quartile 4 | Quartile 1 | Quartile 4 | Quartile 1 | Quartile 4 | Quartile 1 | Quartile 4 | |
| Median score2 | 26.75 | 54.94 | 29.20 | 48.25 | 6.32 | 10.0 | 6.38 | 11.23 |
| Female, % | 40.29 ± 1.50 | 61.40 ± 1.26** | 44.80 ± 1.65 | 52.63 ± 1.27* | 51.90 ± 3.42 | 51.87 ± 1.23 | 40.84 ± 1.71 | 59.37 ± 2.01** |
| Age, y | 45.83 ± 0.78 | 51.64 ± 0.43** | 45.56 ± 0.43 | 50.55 ± 0.39** | 50.17 ± 1.02 | 47.51 ± 0.50 | 46.35 ± 0.54 | 51.57 ± 0.39** |
| BMI, kg/m2 | 27.96 ± 0.21 | 26.68 ± 0.20** | 28.39 ± 0.23 | 26.52 ± 0.18** | 27.57 ± 0.30 | 27.07 ± 0.25 | 27.94 ± 0.24 | 26.74 ± 0.22* |
| Obesity, % | 29.77 ± 1.96 | 23.74 ± 2.03* | 26.69 ± 1.20 | 22.26 ± 1.63* | 24.94 ± 1.67 | 23.21 ± 0.95 | 26.02 ± 1.14 | 21.45 ± 0.98* |
| Obese with ≥1 chronic disease, % | 19.40 ± 1.61 | 14.25 ± 1.34* | 22.49 ± 2.99 | 14.44 ± 1.46 | 15.97 ± 1.98 | 16.44 ± 1.53 | 17.80 ± 1.49 | 14.50 ± 1.28 |
| Having ≥1 chronic disease, % | 55.56 ± 3.21 | 53.35 ± 2.02 | 61.34 ± 3.16 | 50.65 ± 2.44* | 55.05 ± 3.76 | 54.27 ± 2.75 | 56.74 ± 2.0 | 51.46 ± 4.37 |
| Met physical activity guidelines,3 % | 38.94 ± 2.48 | 47.81 ± 4.51* | 40.30 ± 2.46 | 45.38 ± 3.47 | 42.74 ± 2.27 | 44.77 ± 3.35 | 38.54 ± 1.78 | 48.15 ± 3.72** |
| Current daily smokers, % | 19.44 ± 1.63 | 6.48 ± 0.80** | 17.06 ± 1.45 | 8.21 ± 1.0** | 13.71 ± 1.38 | 12.75 ± 1.90 | 21.53 ± 1.58 | 7.36 ± 1.71** |
| Alcohol consumption,4 yes | 34.32 ± 1.54 | 32.13 ± 3.72 | 37.17 ± 3.57 | 34.77 ± 3.52 | 37.74 ± 1.99 | 36.23 ± 4.12 | 40.45 ± 1.66 | 29.37 ± 3.85* |
| Household education, % | ||||||||
| Less than secondary school graduation | 10.01 ± 0.97 | 4.76 ± 0.38** | 9.01 ± 0.69 | 5.18 ± 0.45** | 7.93 ± 1.71 | 6.81 ± 0.41 | 10.36 ± 1.14 | 4.50 ± 0.34** |
| Postsecondary education | 27.25 ± 2.03 | 45.47 ± 1.74** | 29.85 ± 1.55 | 43.55 ± 1.88** | 33.50 ± 4.97 | 37.26 ± 1.44 | 26.28 ± 2.26 | 46.64 ± 1.59** |
| Respondent education, % | ||||||||
| Less than secondary school graduation | 17.05 ± 0.99 | 8.76 ± 0.78** | 15.33 ± 0.78 | 9.20 ± 0.53** | 14.13 ± 1.98 | 11.48 ± 1.11 | 17.88 ± 1.01 | 8.36 ± 0.72** |
| Postsecondary education | 18.88 ± 0.95 | 33.26 ± 2.70** | 21.12 ± 1.31 | 32.36 ± 1.55** | 23.21 ± 2.34 | 27.73 ± 2.92 | 17.87 ± 0.98 | 34.17 ± 2.69** |
| Marital status, % | ||||||||
| Married | 50.68 ± 5.62 | 57.90 ± 6.18* | 49.35 ± 5.01 | 61.39 ± 5.31** | 56.74 ± 5.44 | 51.64 ± 9.28 | 45.25 ± 6.67 | 60.60 ± 6.92** |
| Single | 22.57 ± 4.69 | 17.89 ± 4.37* | 23.42 ± 4.37 | 15.78 ± 3.55** | 18.60 ± 3.97 | 21.92 ± 7.08 | 26.38 ± 6.04 | 16.14 ± 4.49** |
| Immigrant, % | 24.71 ± 3.63 | 33.55 ± 6.15* | 21.39 ± 5.12 | 34.34 ± 4.23** | 21.57 ± 6.16 | 28.88 ± 6.32* | 20.82 ± 2.76 | 36.17 ± 6.94** |
| Excellent self-perceived health status, % | 15.55 ± 1.04 | 23.85 ± 1.09** | 17.74 ± 1.17 | 22.78 ± 1.01* | 19.03 ± 1.11 | 19.99 ± 0.87 | 15.46 ± 0.97 | 23.88 ± 1.93* |
| Highest income, % | 12.46 ± 0.86 | 15.69 ± 1.30* | 15.09 ± 1.12 | 15.32 ± 1.05 | 15.72 ± 1.78 | 13.85 ± 1.26 | 11.39 ± 1.45 | 16.49 ± 1.26** |
| Breakfast skippers, % | 15.17 ± 1.67 | 4.79 ± 0.97** | 14.84 ± 2.19 | 4.98 ± 1.01** | 9.95 ± 3.35 | 10.15 ± 1.71 | 17.45 ± 2.27 | 1.65 ± 1.23** |
n = 14,026. A smaller sample size due to exclusion of “valid skip” and “not stated” responses in CCHS-Nutrition 2015 was used in the analyses of BMI (in kg/m2) (n = 9407); household education (%) (n = 13,996); respondent education (%) (n = 13,940); marital status (%) (n = 13,970); immigration status (%) (n = 14,015); self-perceived health status (%) (n = 14,007); and income (%) (n = 14,019). All values are weighted means or percentages with bootstrapped variances (determined with the use of the balanced repeated replication technique) ± SEs unless otherwise indicated. Covariate-adjusted associations between the scores and continuous and categorical variables were determined using weighted multivariable linear regression and least-squares means, respectively. Values were adjusted for age and sex unless otherwise noted. Age was adjusted for sex only, and sex was adjusted for age only. Only results for quartiles 1 and 4 are shown; see Supplemental Table 5 for results across all quartiles. CCHS, Canadian Community Health Survey; DASH, Dietary Approaches to Stop Hypertension; DGAI, Dietary Guidelines for Americans Adherence Index; ERD, EAT–Lancet Reference Diet; PDI, Plant-based Diet Index.
Higher scores indicated higher diet quality.
According to current physical activity guidelines, Canadian adults should perform 150 min moderate/vigorous-intensity physical activity per week.
Assessed as “alcohol intake from food sources (g)” and therefore representing any amount of alcohol consumed from the first 24-h dietary recall.
*,**Significant P-trend: *P-trend < 0.05; **P-trend < 0.0001.
TABLE 2.
Weighted mean daily intakes of macro- and micronutrients as percentage of energy or per 1000 kcal (nutrient density) by quartile category of dietary scores among Canadian adults (≥18 y old) from the CCHS-Nutrition1
| DASH index | Revised PDI | ERD score | DGAI 2020 | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Model | Quartile 1 | Quartile 4 | Quartile 1 | Quartile 4 | Quartile 1 | Quartile 4 | Quartile 1 | Quartile 4 | |
| Energy intake, kcal/d | a | 1903.24 ± 26.36 | 1742.80 ± 26.31** | 1801.31 ± 36.99 | 2008.51 ± 29.10** | 1967.20 ± 35.90 | 1790.45 ± 30.12** | 1983.92 ± 44.67 | 1806.05 ± 19.31* |
| b | 2282.71 ± 31.40 | 2231.45 ± 18.36 | 2276.92 ± 20.15 | 2292.11 ± 16.76 | 2315.41 ± 22.26 | 2229.68 ± 18.44** | 2306.78 ± 21.89 | 2256.37 ± 17.65* | |
| Carbohydrate, % of energy | a | 45.23 ± 0.33 | 51.48 ± 0.77** | 41.97 ± 1.10 | 51.93 ± 0.71** | 45.32 ± 0.66 | 49.17 ± 0.99** | 44.08 ± 0.65 | 50.71 ± 0.57** |
| b | 44.58 ± 0.35 | 50.60 ± 0.77** | 40.83 ± 1.05 | 51.39 ± 0.79** | 44.68 ± 0.67 | 48.33 ± 0.93** | 43.65 ± 0.56 | 50.07 ± 0.59** | |
| Fiber density, g/1000 kcal | a | 6.51 ± 0.13 | 13.61 ± 0.35** | 7.21 ± 0.14 | 12.42 ± 0.31** | 8.36 ± 0.37 | 10.68 ± 0.30** | 6.31 ± 0.15 | 13.57 ± 0.20** |
| b | 6.24 ± 0.14 | 13.24 ± 0.38** | 6.61 ± 0.16 | 12.14 ± 0.35** | 8.04 ± 0.37 | 10.26 ± 0.29** | 6.21 ± 0.15 | 13.40 ± 0.20** | |
| Added sugar,2 % of energy | a | 12.69 ± 0.32 | 6.74 ± 0.25** | 36.34 ± 2.43 | 47.69 ± 1.29** | 10.25 ± 0.47 | 8.32 ± 0.23** | 11.81 ± 0.45 | 6.51 ± 0.17** |
| b | 12.66 ± 0.34 | 6.73 ± 0.30** | 48.17 ± 3.26 | 54.67 ± 1.48 | 10.28 ± 0.49 | 8.36 ± 0.24** | 11.68 ± 0.46 | 6.35 ± 0.20** | |
| Total fat, % of energy | a | 33.78 ± 0.32 | 29.90 ± 0.45** | 34.27 ± 0.37 | 30.59 ± 0.52** | 34.07 ± 0.56 | 30.79 ± 0.49** | 35.46 ± 0.41 | 29.25 ± 0.35** |
| b | 34.48 ± 0.39 | 30.87 ± 0.54** | 35.34 ± 0.38 | 31.09 ± 0.67** | 34.71 ± 0.65 | 31.66 ± 0.52** | 35.90 ± 0.38 | 29.91 ± 0.46** | |
| Saturated fat, % of energy | a | 11.30 ± 0.20 | 9.09 ± 0.15** | 11.95 ± 0.12 | 9.15 ± 0.17** | 11.30 ± 0.32 | 9.84 ± 0.18** | 12.63 ± 0.18 | 8.60 ± 0.10** |
| b | 11.54 ± 0.22 | 9.43 ± 0.18** | 12.38 ± 0.14 | 9.33 ± 0.22** | 11.53 ± 0.34 | 10.16 ± 0.19** | 12.74 ± 0.16 | 8.78 ± 0.13** | |
| MUFAs, % of energy | a | 12.65 ± 0.11 | 11.16 ± 0.25* | 12.26 ± 0.14 | 11.85 ± 0.25 | 12.72 ± 0.23 | 11.39 ± 0.25** | 12.84 ± 0.15 | 11.13 ± 0.25** |
| b | 12.98 ± 0.13 | 11.60 ± 0.30* | 12.71 ± 0.14 | 12.09 ± 0.32 | 13.03 ± 0.27 | 11.79 ± 0.27** | 13.09 ± 0.15 | 11.49 ± 0.33** | |
| PUFAs, % of energy | a | 6.85 ± 0.08 | 6.89 ± 0.14 | 7.01 ± 0.21 | 6.81 ± 0.15 | 7.0 ± 0.12 | 6.73 ± 0.13* | 6.85 ± 0.15 | 6.77 ± 0.09 |
| b | 6.92 ± 0.10 | 7.0 ± 0.16 | 7.13 ± 0.20 | 6.84 ± 0.18* | 7.05 ± 0.12 | 6.81 ± 0.14* | 6.90 ± 0.15 | 6.85 ± 0.10 | |
| Linoleic acid, % of energy | a | 5.73 ± 0.07 | 5.84 ± 0.15 | 5.89 ± 0.18 | 5.81 ± 0.14 | 5.85 ± 0.10 | 5.74 ± 0.12 | 5.81 ± 0.12 | 5.66 ± 0.08 |
| b | 5.81 ± 0.09 | 5.96 ± 0.17 | 6.01 ± 0.18 | 5.84 ± 0.17* | 5.92 ± 0.11 | 5.83 ± 0.12 | 5.87 ± 0.12 | 5.75 ± 0.09 | |
| Linolenic acid, % of energy | a | 0.75 ± 0.01 | 0.79 ± 0.02 | 0.76 ± 0.02 | 0.76 ± 0.02 | 0.78 ± 0.04 | 0.75 ± 0.02 | 0.74 ± 0.01 | 0.78 ± 0.02* |
| b | 0.75 ± 0.91 | 0.79 ± 0.02 | 0.76 ± 0.02 | 0.76 ± 0.02 | 0.78 ± 0.03 | 0.75 ± 0.02 | 0.74 ± 0.01 | 0.78 ± 0.02* | |
| Protein, % of energy | a | 18.47 ± 0.35 | 15.88 ± 0.15** | 19.22 ± 0.21 | 15.13 ± 0.15** | 18.16 ± 0.22 | 16.08 ± 0.25** | 15.94 ± 0.21 | 18.26 ± 0.17** |
| b | 18.16 ± 0.28 | 15.43 ± 0.16** | 18.88 ± 0.21 | 15.01 ± 0.14** | 17.91 ± 0.21 | 15.71 ± 0.20** | 15.79 ± 0.23 | 18.02 ± 0.21** | |
| Alcohol, % of energy | a | 2.52 ± 0.18 | 2.73 ± 0.40 | 4.54 ± 0.88 | 2.34 ± 0.30* | 2.45 ± 0.27 | 3.96 ± 0.71* | 4.52 ± 0.36 | 1.78 ± 0.22** |
| b | 2.78 ± 0.24 | 3.10 ± 0.28 | 4.95 ± 0.73 | 2.51 ± 0.19** | 2.70 ± 0.22 | 4.30 ± 0.56* | 4.66 ± 0.28 | 2.0 ± 0.17** | |
| Cholesterol density, mg/1000 kcal | a | 190.68 ± 5.69 | 111.71 ± 4.27** | 200.89 ± 4.35 | 100.97 ± 3.60** | 199.46 ± 4.80 | 112.61 ± 2.86** | 174.79 ± 4.94 | 127.15 ± 3.98** |
| b | 189.04 ± 7.52 | 108.66 ± 5.99** | 200.99 ± 6.17 | 102.0 ± 5.51** | 198.52 ± 4.89 | 110.64 ± 4.13** | 173.11 ± 5.99 | 124.53 ± 5.28** | |
| Calcium density, mg/1000 kcal | a | 348.18 ± 6.26 | 500.96 ± 9.23** | 472.87 ± 9.65 | 402.69 ± 5.38** | 424.11 ± 11.31 | 439.91 ± 9.08* | 405.89 ± 7.36 | 457.12 ± 9.08** |
| b | 343.0 ± 6.03 | 493.05 ± 8.29** | 463.59 ± 9.16 | 399.03 ± 5.82** | 418.02 ± 10.51 | 431.26 ± 8.74* | 401.74 ± 7.56 | 450.66 ± 8.27** | |
| Vitamin A density in retinol activity equivalent, µg/1000 kcal | a | 289.47 ± 10.47 | 465.08 ± 27.10** | 361.72 ± 10.76 | 365.96 ± 13.87 | 382.89 ± 10.87 | 357.82 ± 12.72 | 288.47 ± 10.68 | 495.06 ± 19.57** |
| b | 279.51 ± 12.32 | 449.66 ± 28.99** | 343.91 ± 11.96 | 360.03 ± 18.59 | 372.50 ± 13.24 | 342.48 ± 15.82* | 285.21 ± 13.25 | 488.86 ± 24.40** | |
| Vitamin D density, µg/1000 kcal | a | 2.53 ± 0.18 | 2.75 ± 0.10 | 3.83 ± 0.18 | 2.04 ± 0.07** | 3.44 ± 0.19 | 2.13 ± 0.10** | 2.45 ± 0.18 | 2.87 ± 0.08* |
| b | 2.49 ± 0.16 | 2.68 ± 0.09 | 3.34 ± 0.16 | 2.03 ± 0.07** | 3.40 ± 0.17 | 2.06 ± 0.12** | 2.44 ± 0.15 | 2.83 ± 0.10* | |
| Vitamin C density, mg/1000 kcal | a | 38.30 ± 2.67 | 78.82 ± 1.96** | 38.10 ± 3.25 | 72.39 ± 1.70** | 49.88 ± 3.51 | 60.0 ± 2.18* | 30.2 ± 1.71 | 81.82 ± 3.10** |
| b | 36.66 ± 2.86 | 76.12 ± 2.0** | 34.01 ± 2.92 | 71.23 ± 1.79** | 48.09 ± 3.29 | 57.25 ± 2.64 | 29.94 ± 1.40 | 81.1 ± 3.56** | |
| Sodium density, g/1000 kcal | a | 1763.34 ± 27.86 | 1249.24 ± 13.55** | 1622.86 ± 20.99 | 1360.11 ± 14.97** | 1481.02 ± 25.79 | 1497.13 ± 23.80 | 1579.95 ± 29.55 | 1389.67 ± 20.24** |
| b | 1734.34 ± 27.70 | 1206.96 ± 14.48** | 1594.72 ± 21.50 | 1349.86 ± 15.53** | 1461.86 ± 25.17 | 1469.20 ± 24.91 | 1556.14 ± 29.92 | 1355.0 ± 17.50** | |
| Thiamin density, mg/1000 kcal | a | 0.84 ± 0.01 | 0.89 ± 0.02* | 0.88 ± 0.01 | 0.88 ± 0.03 | 0.81 ± 0.01 | 0.90 ± 0.04* | 0.79 ± 0.02 | 0.93 ± 0.01** |
| b | 0.82 ± 0.01 | 0.86 ± 0.02* | 0.85 ± 0.01 | 0.87 ± 0.03 | 0.79 ± 0.01 | 0.88 ± 0.04 | 0.78 ± 0.02 | 0.92 ± 0.01** | |
| Riboflavin density, mg/1000 kcal | a | 1.05 ± 0.01 | 1.10 ± 0.01* | 1.16 ± 0.01 | 0.98 ± 0.01** | 1.11 ± 0.02 | 1.03 ± 0.02* | 1.03 ± 0.03 | 1.10 ± 0.02 |
| b | 1.02 ± 0.02 | 1.06 ± 0.01* | 1.12 ± 0.02 | 0.97 ± 0.01** | 1.09 ± 0.02 | 1.0 ± 0.01* | 1.01 ± 0.03 | 1.07 ± 0.02 | |
| Niacin density in niacin equivalents, mg/1000 kcal | a | 22.95 ± 0.40 | 19.94 ± 0.25** | 22.99 ± 0.30 | 19.51 ± 0.29** | 21.86 ± 0.50 | 20.64 ± 0.45* | 19.57 ± 0.29 | 22.95 ± 0.28** |
| b | 22.58 ± 0.35 | 19.35 ± 0.26** | 22.53 ± 0.28 | 19.39 ± 0.26** | 21.57 ± 0.49 | 20.19 ± 0.41** | 19.40 ± 0.25 | 22.67 ± 0.29** | |
| Vitamin B-6 density, mg/1000 kcal | a | 0.85 ± 0.02 | 1.04 ± 0.03** | 0.90 ± 0.02 | 0.94 ± 0.03* | 0.98 ± 0.04 | 0.91 ± 0.02* | 0.72 ± 0.02 | 1.15 ± 0.02** |
| b | 0.84 ± 0.02 | 1.0 ± 0.04** | 0.86 ± 0.02 | 0.94 ± 0.04** | 0.96 ± 0.04 | 0.88 ± 0.03* | 0.72 ± 0.02 | 1.14 ± 0.03** | |
| Vitamin B-12 density, µg/1000 kcal | a | 2.62 ± 0.09 | 1.94 ± 0.09** | 2.86 ± 0.09 | 1.75 ± 0.10** | 2.71 ± 0.10 | 1.89 ± 0.08** | 2.31 ± 0.07 | 2.20 ± 0.12 |
| b | 2.56 ± 0.12 | 1.86 ± 0.15** | 2.81 ± 0.10 | 1.71 ± 0.13** | 2.66 ± 0.10 | 1.83 ± 0.13** | 2.27 ± 0.10 | 2.13 ± 0.14 | |
| Naturally occurring folate density,3 µg/1000 kcal | a | 91.0 ± 3.17 | 157.84 ± 3.31** | 102.60 ± 1.80 | 141.38 ± 3.62** | 110.78 ± 5.66 | 125.35 ± 2.93* | 86.45 ± 2.06 | 157.82 ± 2.05** |
| b | 87.86 ± 3.15 | 153.17 ± 3.51** | 95.88 ± 1.92 | 138.78 ± 3.70** | 107.33 ± 5.64 | 120.44 ± 2.63* | 85.21 ± 1.64 | 155.64 ± 2.16** | |
| Folacin density from food sources,4 µg/1000 kcal | a | 161.27 ± 3.44 | 202.90 ± 3.61** | 165.40 ± 2.32 | 198.17 ± 3.01** | 157.84 ± 5.16 | 192.32 ± 4.32** | 157.88 ± 2.74 | 203.90 ± 2.36** |
| b | 157.81 ± 3.53 | 197.64 ± 4.27** | 158.72 ± 2.66 | 195.82 ± 3.39** | 154.63 ± 5.49 | 187.62 ± 4.37** | 155.94 ± 2.62 | 200.75 ± 2.34** | |
| Phosphorus density, mg/1000 kcal | a | 659.45 ± 6.56 | 745.53 ± 6.04** | 740.86 ± 11.55 | 671.67 ± 6.39** | 722.11 ± 8.42 | 683.52 ± 6.08* | 635.56 ± 6.67 | 766.62 ± 7.77** |
| b | 647.19 ± 6.50 | 728.30 ± 6.12** | 732.18 ± 12.01 | 663.38 ± 7.63** | 709.81 ± 8.77 | 666.79 ± 6.66* | 628.25 ± 8.0 | 755.49 ± 8.32** | |
| Magnesium density, mg/1000 kcal | a | 139.08 ± 3.41 | 214.15 ± 2.12** | 153.98 ± 1.80 | 192.97 ± 2.11** | 162.17 ± 3.99 | 178.26 ± 1.94** | 135.09 ± 2.19 | 210.88 ± 1.76** |
| b | 134.66 ± 3.53 | 207.68 ± 2.28** | 145.34 ± 1.97 | 189.50 ± 2.19** | 157.47 ± 3.91 | 171.67 ± 1.93* | 132.82 ± 1.83 | 207.18 ± 1.95** | |
| Iron density, mg/1000 kcal | a | 6.59 ± 0.89 | 7.06 ± 0.07** | 6.56 ± 0.06 | 7.09 ± 0.07** | 6.46 ± 0.10 | 6.99 ± 0.13* | 6.03 ± 0.09 | 7.45 ± 0.14** |
| b | 6.47 ± 0.09 | 6.89 ± 0.08* | 6.36 ± 0.07 | 7.0 ± 0.07** | 6.35 ± 0.10 | 6.83 ± 0.13* | 5.97 ± 0.08 | 7.35 ± 0.13** | |
| Zinc density, mg/1000 kcal | a | 5.84 ± 0.13 | 5.67 ± 0.10 | 5.96 ± 0.09 | 5.48 ± 0.08** | 5.96 ± 0.15 | 5.47 ± 0.06** | 5.10 ± 0.15 | 6.22 ± 0.18** |
| b | 5.73 ± 0.12 | 5.53 ± 0.13 | 5.83 ± 0.08 | 5.41 ± 0.10* | 5.86 ± 0.16 | 5.34 ± 0.07** | 5.04 ± 0.13 | 6.14 ± 0.21** | |
| Potassium density, mg/1000 kcal | a | 1282.15 ± 16.91 | 1804.70 ± 17.14** | 1369.28 ± 14.75 | 1637.84 ± 13.13** | 1555.38 ± 26.41 | 1515.58 ± 13.60 | 1198.37 ± 17.01 | 1831.62 ± 20.80** |
| b | 1247.95 ± 23.52 | 1751.16 ± 24.17** | 1301.36 ± 23.62 | 1616.15 ± 15.97** | 1519.36 ± 21.15 | 1462.19 ± 22.20 | 1183.80 ± 16.40 | 1805.73 ± 32.68** | |
| Caffeine density, mg/1000 kcal | a | 116.04 ± 6.20 | 96.03 ± 3.47* | 93.52 ± 4.40 | 94.80 ± 2.88 | 91.67 ± 3.98 | 102.62 ± 5.39 | 112.22 ± 13.65 | 86.37 ± 4.47* |
| b | 107.63 ± 6.05 | 82.81 ± 3.35** | 80.87 ± 4.30 | 91.38 ± 2.63 | 84.85 ± 3.47 | 92.11 ± 5.26 | 104.90 ± 12.39 | 75.24 ± 3.57* | |
| Moisture density,5 g/1000 kcal | a | 1387.53 ± 26.73 | 1731.01 ± 39.97** | 1534.38 ± 41.56 | 1487.13 ± 21.78 | 1382.12 ± 28.91 | 1605.48 ± 29.66** | 1455.71 ± 37.84 | 1658.0 ± 31.66** |
| b | 1285.84 ± 25.52 | 1567.88 ± 37.05** | 1366.86 ± 34.37 | 1443.19 ± 20.48 | 1294.74 ± 29.27 | 1469.33 ± 26.32** | 1378.56 ± 30.76 | 1536.44 ± 24.86** | |
| Glycemic index density,6 per 1000 kcal | a | 35.55 ± 0.66 | 32.98 ± 0.67* | 37.48 ± 1.21 | 28.65 ± 0.66** | 31.34 ± 0.75 | 35.71 ± 1.0** | 38.37 ± 1.41 | 29.88 ± 0.72** |
| b | 32.55 ± 0.67 | 27.98 ± 0.54* | 32.71 ± 1.23 | 27.73 ± 0.58** | 28.95 ± 0.72 | 31.79 ± 0.81* | 35.85 ± 1.43 | 25.92 ± 1.03** | |
| Energy density,7 per 1000 kcal | a | 1.29 ± 0.03 | 0.97 ± 0.01** | 1.40 ± 0.09 | 0.89 ± 0.01** | 1.09 ± 0.03 | 1.18 ± 0.05 | 1.52 ± 0.10 | 0.83 ± 0.01** |
| b | 1.20 ± 0.03 | 0.83 ± 0.01** | 1.27 ± 0.07 | 0.87 ± 0.01** | 1.02 ± 0.02 | 1.07 ± 0.05 | 1.43 ± 0.09 | 0.70 ± 0.03** | |
n = 14,026. All values are weighted means with bootstrapped variances (determined using the balanced repeated replication technique) ± SEs unless otherwise indicated. Covariate-adjusted associations between the scores and continuous variables were determined with the use of weighted multivariable linear regression. Values were adjusted for age and sex (model a), with the addition of misreporting status (model b). Only results for quartiles 1 and 4 are shown; see Supplemental Table 6 for results across all quartiles. CCHS, Canadian Community Health Survey; DASH, Dietary Approaches to Stop Hypertension; DGAI, Dietary Guidelines for Americans Adherence Index; ERD, EAT– Lancet Reference Diet; PDI, Plant-based Diet Index.
Because added sugars are not included in the Canadian Nutrient File, the method proposed by Brisbois et al. (59) was used to derive estimates of added sugars.
Naturally occurring folate included various forms of folate that are naturally present in food.
Sum of quantities of naturally occurring folate in addition to folic acid without consideration of their differing bioavailabilities.
Based on water content in food sources.
Estimated by assigning the mean values reported in the International Glycemic Index Table (60, 61) to each of the Bureau of Nutritional Sciences food categories (62), as described previously (63, 64).
The dietary energy density was calculated by dividing the total energy from foods (kcal) by the total weight of foods (g) (with the exclusion of beverages) (65, 66).
*,**Significant P-trend: *P-trend < 0.05; **P-trend < 0.0001.
To explore population adherence to dietary recommendations, multidimensional radar plots were used representing percentages of compliers, intermediate compliers, and noncompliers (Figure 1). Overall, none of the 4 dietary patterns were fully adhered to by Canadians. In fact, the ERD score was the only index with a good degree of compliance: >80% of respondents complied well with recommendations in 7 out of 14 component categories. Poor compliance was commonly observed for plant-based food categories, whereas the animal-based components “fish” and “eggs” appeared to be the main source of compliance. Concurrent-criterion validity was confirmed for the DASH index, revised PDI, and DGAI 2020 (Supplemental Table 11). After adjusting for age and sex, mean total scores were significantly higher in women than in men (P < 0.05), older respondents than in younger individuals (P < 0.0001), and in nonsmokers than in daily and occasional smokers (P < 0.0001). The ERD score did not display any significant linear trends among the different categories.
FIGURE 1.
Weighted percentages with bootstrapped variances (determined using the balanced repeated replication technique) of compliance for each of the components of the DASH index (A), revised PDI (B), ERD score (C), DGAI 2020 food intake subscore (D), and DGAI 2020 healthy choice subscore (E) among Canadian adults (≥18 y old) from the Canadian Community Health Survey 2015 (n = 14,026). Each spoke of the radar plot depicts an individual component and each line color represents a different category of compliance. Prevalence is expressed as 0%–100%. All differences between compliance groups across the dietary indices’ components were assessed with a chi-square test and were statistically significant (P < 0.0001). DASH, Dietary Approaches to Stop Hypertension; DGAI, Dietary Guidelines for Americans Adherence Index; ERD, EAT–Lancet Reference Diet; PDI, Plant-based Diet Index.
Lastly, internal consistency tests revealed standardized Cronbach's α coefficients of 0.73, 0.45, 0.35, and 0.23 for the DGAI 2020, DASH index, revised PDI, and ERD score, respectively. The DASH index, revised PDI, and ERD total scores had significant and positive correlations with their respective individual components (P < 0.05) (Supplemental Tables 12–15). To ensure diet quality was measured independently of diet quantity, the correlations between EI and the total scores of each index were explored. Results showed slightly negative correlations for the DASH index (r = −0.17) and DGAI 2020 (r = −0.15), and slightly positive correlations for the revised PDI (r = 0.07) and ERD score (r = 0.01). All correlation coefficients between EI and total and component scores were small.
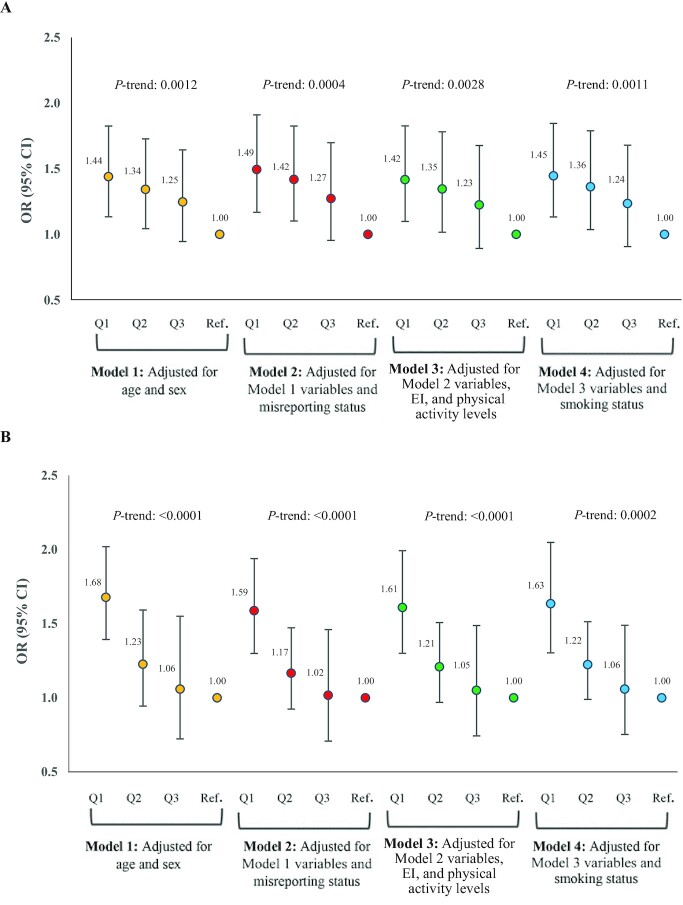
Adherence to the diet quality indices and risk of obesity
The multivariable-adjusted odds of being obese were significantly higher in the lowest (unhealthiest) quartiles than for those in the highest quartiles (healthiest, reference) of the DASH index (OR: 1.45; 95% CI: 1.13, 1.85), revised PDI (OR: 1.63; 95% CI: 1.30, 2.05), and DGAI 2020 scores (OR: 1.52; 95% CI: 1.24, 1.86) (all P-trends < 0.05) (model 4 in Figure 2A, B, D). Although the probability of being obese also increased in the lowest compared with the highest quartile of the ERD score across all models (Figure 2C), none of the trends reached statistical significance. Jointly stratifying respondents by weight and chronic disease status showed less clear trends (Figure 3). The ORs of being unhealthy and obese were significantly increased in quartile 1 compared with quartile 3 of the DASH index (Q1 OR: 1.54; 95% CI: 1.02, 2.34; Q3 OR: 1.13; 95% CI: 0.78, 1.62) and DGAI 2020 (Q1 OR: 1.53; 95% CI: 1.05, 2.23; Q3 OR: 1.36; 95% CI: 0.87, 2.14) (P-trends < 0.05). The probability of being obese without a chronic disease (healthy and obese), on the other hand, was significantly higher in the lowest as compared to the highest quartiles of the revised PDI (OR: 1.67; 95% CI: 0.92, 3.03) and DGAI 2020 (OR: 1.75; 95% CI: 1.18, 2.61) (P-trends < 0.05). High adherence to the EAT–Lancet planetary diet was not associated with a lower risk of obesity (with or without chronic disease) or decreased odds of a chronic disease without obesity (Figure 3C).
FIGURE 2.
Weighted multivariate-adjusted ORs (95% CIs) with bootstrapped variances (determined using the balanced repeated replication technique) for obesity risk [BMI (in kg/m2) ≥30] across quartile categories of the Dietary Approaches to Stop Hypertension index (A), revised Plant-based Diet Index (B), EAT–Lancet Reference Diet score (C), and Dietary Guidelines for Americans Adherence Index 2020 (D) in Canadian adults (≥18 y old) from the Canadian Community Health Survey-Nutrition 2015 (n = 14,026). Estimates were based on the multinomial logistic regression generalized logit model. P-trend was based on the logistic regression coefficient for the index scores as continuous variables. EI, energy intake; Q, quartile.
FIGURE 3.
Weighted multivariate-adjusted ORs (95% CIs) with bootstrapped variances (determined using the balanced repeated replication technique) for risk of obesity with and without ≥1 chronic disease across quartile categories of the Dietary Approaches to Stop Hypertension index (A), revised Plant-based Diet Index (B), EAT–Lancet Reference Diet score (C), and Dietary Guidelines for Americans Adherence Index 2020 (D) in Canadian adults (≥18 y old) from the Canadian Community Health Survey-Nutrition 2015 (n = 14,026). All models were adjusted for age, sex, misreporting, energy intake, physical activity levels, and smoking status. Estimates were based on the multinomial logistic regression generalized logit model. P-trends are shown in the following order: 1) obese with chronic disease; 2) obese without chronic disease; 3) nonobese with chronic disease. Q, quartile.
Adherence to the diet quality indices and risk of CVD
CCHS-Nutrition 2004 was used for evaluating the association of diet quality indices with CVD outcomes. Compliance to dietary patterns was relatively similar between the two Canadian national nutrition surveys (CCHS 2004 and CCHS 2015) (Supplemental Table 16). During a total of 80,529 person-years of follow-up, 748 incident CVD events were documented. After accounting for multiple potential confounders in the multivariable-adjusted models, there were no significant associations between usual dietary scores and CVD events (Table 3). Effect modification by sex was significant across all dietary scores in both the age- and multivariable-adjusted models (P-interaction < 0.0001 for all).
TABLE 3.
Weighted and multivariable-adjusted HRs and bootstrapped 95% CIs of cardiovascular disease events (incidence and mortality) according to the midpoints of quintiles of usual intake of the DASH index, revised PDI, revised hPDI, revised uPDI, ERD score, and DGAI 2020 in Canadian adults (45–80 y), CCHS-Nutrition 2004 linked to Canadian Vital Statistics—Death Database and Discharge Abstract Database, 2004–20171
| Midpoint of quintile of estimated usual dietary score, HR (95% CI) | |||||
|---|---|---|---|---|---|
| Dietary indices | 1 | 2 | 3 | 4 | 5 |
| DASH index | |||||
| Median score2 | 37.62 | 41.80 | 44.93 | 47.95 | 52.44 |
| Median score3 | 37.21 | 41.74 | 45.04 | 48.17 | 52.46 |
| Base model4 | |||||
| Women | 1 (Reference) | 0.86 (0.74, 1.00) | 0.77 (0.59, 1.00) | 0.67 (0.47, 0.99) | 0.58 (0.34, 0.99) |
| Men | 1 (Reference) | 0.89 (0.75, 1.05) | 0.81 (0.60, 1.09) | 0.74 (0.48, 1.13) | 0.65 (0.36, 1.19) |
| Multivariable-adjusted model5 | |||||
| Women | 1 (Reference) | 0.91 (0.76, 1.08) | 0.85 (0.62, 1.15) | 0.79 (0.52, 1.21) | 0.72 (0.40, 1.31) |
| Men | 1 (Reference) | 0.87 (0.72, 1.06) | 0.79 (0.57, 1.10) | 0.72 (0.45, 1.14) | 0.63 (0.33, 1.21) |
| Revised PDI | |||||
| Median score2 | 34.77 | 37.15 | 38.99 | 40.75 | 43.26 |
| Median score3 | 34.13 | 37.07 | 38.99 | 40.94 | 43.53 |
| Base model4 | |||||
| Women | 1 (Reference) | 0.97 (0.84, 1.13) | 0.95 (0.73, 1.24) | 0.94 (0.65, 1.35) | 0.91 (0.54, 1.54) |
| Men | 1 (Reference) | 0.92 (0.79, 1.07) | 0.86 (0.66, 1.12) | 0.81 (0.55, 1.18) | 0.74 (0.43, 1.26) |
| Multivariable-adjusted model5 | |||||
| Women | 1 (Reference) | 1.04 (0.86, 1.27) | 1.07 (0.78, 1.48) | 1.10 (0.70, 1.73) | 1.14 (0.61, 2.13) |
| Men | 1 (Reference) | 0.91 (0.75, 1.12) | 0.86 (0.61, 1.21) | 0.81 (0.51, 1.30) | 0.75 (0.39, 1.44) |
| Revised hPDI | |||||
| Median score2 | 39.14 | 41.87 | 43.74 | 45.62 | 48.32 |
| Median score3 | 38.33 | 41.42 | 44.06 | 46.04 | 49.23 |
| Base model4 | |||||
| Women | 1 (Reference) | 0.91 (0.80, 1.04) | 0.86 (0.68, 1.07) | 0.80 (0.59, 1.10) | 0.73 (0.47, 1.14) |
| Men | 1 (Reference) | 0.92 (0.79, 1.07) | 0.87 (0.67, 1.12) | 0.82 (0.57, 1.17) | 0.75 (0.45, 1.25) |
| Multivariable-adjusted model5 | |||||
| Women | 1 (Reference) | 0.96 (0.83, 1.11) | 0.93 (0.71, 1.22) | 0.91 (0.63, 1.31) | 0.88 (0.52, 1.46) |
| Men | 1 (Reference) | 0.91 (0.77, 1.08) | 0.84 (0.62, 1.15) | 0.79 (0.52, 1.21) | 0.72 (0.40, 1.30) |
| Revised uPDI | |||||
| Median score2 | 34.68 | 37.37 | 39.25 | 41.13 | 43.87 |
| Median score3 | 33.78 | 36.97 | 38.95 | 41.57 | 44.66 |
| Base model4 | |||||
| Women | 1 (Reference) | 1.10 (0.96, 1.25) | 1.17 (0.94, 1.46) | 1.25 (0.91, 1.70) | 1.37 (0.88, 2.13) |
| Men | 1 (Reference) | 1.09 (0.94, 1.26) | 1.15 (0.89, 1.48) | 1.22 (0.85, 1.74) | 1.33 (0.80, 2.21) |
| Multivariable-adjusted model5 | |||||
| Women | 1 (Reference) | 1.04 (0.89, 1.21) | 1.07 (0.83, 1.36) | 1.10 (0.76, 1.59) | 1.14 (0.68, 1.91) |
| Men | 1 (Reference) | 1.10 (0.93, 1.31) | 1.17 (0.88, 1.55) | 1.27 (0.83, 1.94) | 1.39 (0.77, 2.52) |
| ERD score | |||||
| Median score2 | 7.10 | 7.34 | 7.53 | 7.71 | 7.94 |
| Median score3 | 7.01 | 7.28 | 7.50 | 7.73 | 8.13 |
| Base model4 | |||||
| Women | 1 (Reference) | 0.92 (0.80, 1.07) | 0.87 (0.67, 1.13) | 0.82 (0.56, 1.19) | 0.76 (0.46, 1.27) |
| Men | 1 (Reference) | 0.76 (0.61, 0.96) | 0.62 (0.42, 0.93) | 0.51 (0.29, 0.90) | 0.40 (0.18, 0.87) |
| Multivariable-adjusted model5 | |||||
| Women | 1 (Reference) | 0.91 (0.71, 1.17) | 0.84 (0.54, 1.32) | 0.78 (0.41, 1.50) | 0.68 (0.25, 1.89) |
| Men | 1 (Reference) | 0.76 (0.57, 1.01) | 0.61 (0.36, 1.01) | 0.48 (0.23, 1.02) | 0.32 (0.10, 1.03) |
| DGAI 2020 | |||||
| Median score2 | 6.84 | 7.54 | 8.03 | 8.47 | 9.17 |
| Median score3 | 6.77 | 7.55 | 8.06 | 8.55 | 9.20 |
| Base model4 | |||||
| Women | 1 (Reference) | 0.91 (0.77, 1.07) | 0.85 (0.64, 1.12) | 0.80 (0.55, 1.17) | 0.73 (0.42, 1.24) |
| Men | 1 (Reference) | 1.15 (0.96, 1.39) | 1.27 (0.93, 1.74) | 1.39 (0.90, 2.14) | 1.60 (0.87, 2.95) |
| Multivariable-adjusted model5 | |||||
| Women | 1 (Reference) | 1.03 (0.85, 1.25) | 1.05 (0.76, 1.44) | 1.07 (0.69, 1.64) | 1.09 (0.60, 1.97) |
| Men | 1 (Reference) | 1.13 (0.92, 1.38) | 1.21 (0.87, 1.70) | 1.31 (0.82, 2.08) | 1.44 (0.76, 2.72) |
n = 6771. Weighted HRs were calculated using regression calibration (Cox proportional hazards model) and the 95% CIs calculated by bootstrapping the usual intake estimating models B = 500 times at each step. All Cox models used sex interaction to test for effect modification by sex (P-interaction < 0.0001 for all). CCHS: Canadian Community Health Survey; DASH, Dietary Approaches to Stop Hypertension; DGAI, Dietary Guidelines for Americans Adherence Index; ERD, EAT– Lancet Reference Diet; hPDI, healthful Plant-based Diet Index; PDI, Plant-based Diet Index; uPDI, unhealthful Plant-based Diet Index.
Weighted and error-adjusted usual intake median of the diet quality index score; corresponds to base model (midpoint of quintiles).
Weighted and error-adjusted usual intake median of the diet quality index score; corresponds to multivariable-adjusted model (midpoint of quintiles).
Base model: adjusted for day of the week on which 24-h dietary recall was collected [weekday/weekend (Friday–Sunday)], sequence of dietary recall (first or second), and baseline age (continuous).
Multivariable-adjusted model: adjusted for base model covariates in addition to education (less than secondary school graduation; secondary school graduation; some postsecondary; postsecondary graduation), smoking (daily/occasional smoker with 20 ≤ cigarettes/d < 90; daily/occasional smoker with <20 cigarettes/d; former daily/occasional smoker and those who smoked a total of ≥100 cigarettes in lifetime; never smoked), misreporting (under-reporter; plausible reporter and over-reporter), physical activity (daily energy expenditure ≥3; 1.5 ≤ daily energy expenditure < 3; and 0 ≤ daily energy expenditure < 1.5), marital status (married/common-law partner; widowed/separated/divorced/single; never married), immigrant (yes/no), and alcohol consumption (none; less than once a month/once a month/2–3 times a month; once a week/2–3 times a week; 4–6 times a week/every day).
Discussion
In a nationally representative sample of Canadian adults, our findings revealed consistent and strong evidence to support the validity of the DASH index, revised PDI, and DGAI 2020 for measuring diet quality, whereas the validity of the ERD score was not directly confirmed. In the multivariable-adjusted model, we found no significant associations between adherence to the dietary indices and CVD incidence and mortality.
To our knowledge, this is the first study to evaluate the validity and reliability of emerging plant-based dietary indices at the national population level. We confirmed the construct validity of the revised PDI and DGAI 2020 to be as robust as that of the DASH index, established through associations with sociodemographic and lifestyle characteristics. Furthermore, closer adherence to the revised PDI and DGAI 2020 was associated with higher nutrient quality (irrespective of quantity), higher index subcomponent scores, and a lower risk of obesity after adjusting for a number of confounders. These findings are supported by previous studies using PDIs and the DGAI, whereby higher index scores were significantly associated with lower risk of obesity (16, 42). Conversely, the ERD score displayed weak and inconsistent evidence to support its validity and reliability, which may be explained in light of its crude scoring system.
Our study did not find any significant associations between plant-based dietary patterns and CVD incidence and mortality. This is in line with a previous nationally representative study conducted in the United States (11), which revealed non-significant associations between PDIs and CVD mortality after stratifying analyses by sex. Nonetheless, mixed results were reported by the same group in a consecutive community-based analysis where CVD incidence and mortality were explored separately (13). More recently, Keaver et al. (12) extended the use of PDIs to further distinguish the quality of animal- and plant-based foods in another nationally representative study in the United States and found no significant associations with heart disease mortality. Whereas our findings are directly in line with previous nationally representative studies in the United States, they are in contrast with the majority of previous prospective cohort studies to have utilized PDIs (14, 43, 44) or overall diet quality indices such as the DASH index (44–47), although most of these involved smaller samples or specific populations. Such conflicting results could be attributed to inconsistencies in the definitions of CVD and plant-based dietary patterns, lack of uniform methodological and statistical approaches in the utilization of a priori dietary pattern scores, as well as the inclusion of highly variable confounders. Another plausible explanation is that a minimum level of adherence to plant-based eating is to be achieved before health benefits are observed (11, 48, 49) and because general populations tend to adhere less to plant-based dietary patterns, health benefits might be difficult to capture. As well, compared to nationally representative analyses, cohort studies are prone to selection bias, which could lead to higher scores (healthier dietary patterns). Importantly, the non-significant associations found in this study do not undermine the well-established role of plant-based eating patterns in reducing CVD events and mortality at the population level (14, 15, 50, 51).
Another important aspect of this study was inclusion of the ERD score as an emerging dietary index with a promising focus on the role of plant-based eating in health and environmental sustainability. So far, the role of the EAT–Lancet diet in cardiometabolic health has only been investigated in the EPIC (European Prospective Investigation into Cancer and Nutrition)-Oxford cohort study (15), whereby high ERD scores were significantly associated with 28% decrease in ischemic heart disease arguably due to the large proportion of vegetarians in the sample. Nonetheless, the global diet has largely been criticized for relying on suboptimal quantities of specific food groups, as well as for its limited applicability to countries with a high/middle sociodemographic index (52, 53). In our study, high ERD scores were associated with a nonsignificant but reduced risk of CVD incidence and mortality in both women and men, suggesting potential health benefits. Further nationally representative research is warranted to improve the inherent methodological limitations of the ERD score before its establishment as a robust plant-based dietary index in Canada.
A key novelty of our study was development and validation of the DGAI 2020, which was updated from the DGAI 2015 (16) with the release of the 2020 DGA (7). Compared to the previous version, the DGAI 2020 brings about an increase (by 0.5 servings) in the recommended intake of nuts, seeds, and soy, as well as substituting “protein foods” for a “meat and beans” subcomponent, combining all plant and animal protein into 1 category. In our study, the DGAI 2020 was non-significantly but positively associated with CVD incidence and mortality. To the best of our knowledge, the association of the DGAI with CVD risk has not been previously explored in nationally representative studies, even though observational research has confirmed positive associations between high adherence to previous versions of the DGAI and cardiovascular health (31, 51, 54, 55). A potential reason for the non-significant slightly elevated risks of CVD outcomes in the highest quintiles of the DGAI 2020 in our research could be the fact that the DGAI score does not distinguish healthy from unhealthy plant- and animal-based products as well as the revised PDI and ERD scores do. Indeed, the DGAI 2020 combines plant and animal proteins into 1 category—with a focus on meeting daily requirements rather than placing restrictions on meat intake—although replacement of as little as 3% of energy from animal sources with plant sources was recently reported to reduce CVD risk (56).
A notable strength of our study was the use of a national nutrition survey linked to health administrative databases to eliminate the challenges of cohort design (e.g., loss to follow-up, non-representative sample). Another considerable strength in our methodological approach was application of the NCI method for handling random measurement error while taking into consideration a number of confounders in a priori–defined analyses (57, 58). Furthermore, compared with previous studies, a unique feature of the present research was handling systematic error through controlling for misreporting bias (33). Despite the aforementioned strengths, our study is not without limitations. The relatively short follow-up time available in health administrative databases may have partially contributed to a lack of power to detect significant differences. Sex interaction (instead of sex stratification) was used in our regression analyses, which resulted in our inability to observe the individual effects from other lifestyle factors (model confounders). Lastly, lack of repeated dietary measurements, differencesi n methodology between the CCHS-Nutrition cycles, and the overall low adherence to healthy dietary patterns in the present study may have led to reduced sensitivity and specificity in detecting statistically significant differences.
In conclusion, in a nationally representative sample of Canadian adults, we confirmed the validity and reliability of the DGAI 2020 and revised PDI (but not the ERD score) as acceptable measures of diet quality. We observed no significant associations between dietary indices with CVD incidence and mortality. Nonetheless, close adherence to the dietary recommendations outlined in the 2020 DGA and the revised Plant-based Dietary pattern was associated with a higher diet quality and a lower risk of obesity. Future studies should continue exploring the potential benefits of emerging plant-based dietary patterns in relation to CVD outcomes in population-based settings, as well as addresing the lack of a uniform framework in scoring algorithms of dietary indices.
Supplementary Material
ACKNOWLEDGEMENTS
We thank the staff at Statistics Canada's Research Data Centre, especially Wendy Kei, for their technical support.
The authors’ responsibilities were as follows—MJ: designed the research and had primary responsibility for the final content; SVL and MJ: coded the data and conducted the research; SVL: analyzed the data and wrote the first draft; MJ, JMS and SVL: read, revised and approved the final manuscript. The authors report no conflicts of interest.
Notes
Supported by Canadian Institutes of Health Research Grant 378193 (to MJ), the Canada Research Chair Program, and Banting Foundation Discovery Award (to MJ). The funders had no role in the design, implementation, analysis, and interpretation of the data.
Supplemental Methods, Supplemental Figure 1, and Supplemental Tables 1–16 are available from the “Supplementary data” link in the online posting of the article and from the same link in the online table of contents at https://academic.oup.com/ajcn/.
Abbreviations used: CCHS, Canadian Community Health Survey; CNF, Canadian Nutrient File; CVD, cardiovascular disease; DASH, Dietary Approaches to Stop Hypertension; DGA, Dietary Guidelines for Americans; DGAI, Dietary Guidelines for Americans Adherence Index; EER, estimated energy requirement; EI, energy intake; ERD, EAT–Lancet Reference Diet; NCI, National Cancer Institute; PDI, Plant-based Dietary Index; Q, quartile.
Contributor Information
Svilena V Lazarova, Food, Nutrition and Health Program, Faculty of Land and Food Systems, The University of British Columbia, Vancouver, British Columbia, Canada.
Jason M Sutherland, Centre for Health Services and Policy Research, School of Population and Public Health, University of British Columbia, Vancouver, British Columbia, Canada.
Mahsa Jessri, Food, Nutrition and Health Program, Faculty of Land and Food Systems, The University of British Columbia, Vancouver, British Columbia, Canada; Centre for Health Services and Policy Research, School of Population and Public Health, University of British Columbia, Vancouver, British Columbia, Canada.
Data Availability
Data described in the article, code book, and analytic code will be made available upon request pending application and approval (By Statistics Canada).
References
- 1. Roth GA, Mensah GA, Johnson CO, Addolorato G, Ammirati E, Baddour LM, Barengo NC, Beaton AZ, Benjamin EJ, Benziger CPet al. Global burden of cardiovascular diseases and risk factors, 1990–2019: update from the GBD 2019 study. J Am Coll Cardiol. 2020;76(25):2982–3021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Afshin A, Sur PJ, Fay KA, Cornaby L, Ferrara G, Salama JS, Mullany EC, Abate KH, Abbafati C, Abebe Zet al. Health effects of dietary risks in 195 countries, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2019;393(10184):1958–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Aune D. Plant foods, antioxidant biomarkers, and the risk of cardiovascular disease, cancer, and mortality: a review of the evidence. Adv Nutr. 2019;10(Supplement_4):S404–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Hu FB. Plant-based foods and prevention of cardiovascular disease: an overview. Am J Clin Nutr. 2003;78(3):544S–51S. [DOI] [PubMed] [Google Scholar]
- 5. Satija A, Bhupathiraju SN, Rimm EB, Spiegelman D, Chiuve SE, Borgi L, Willett WC, Manson JE, Sun Q, Hu FB. Plant-based dietary patterns and incidence of type 2 diabetes in US men and women: results from three prospective cohort studies. PLoS Med. 2016;13(6):e1002039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Willett W, Rockström J, Loken B, Springmann M, Lang T, Vermeulen S, Garnett T, Tilman D, DeClerck F, Wood Aet al. Food in the Anthropocene: the EAT–Lancet Commission on healthy diets from sustainable food systems. Lancet. 2019;393(10170):447–92. [DOI] [PubMed] [Google Scholar]
- 7. Dietary Guidelines Advisory Committee . Scientific report of the 2020 Dietary Guidelines Advisory Committee: advisory report to the Secretary of Agriculture and the Secretary of Health and Human Services. Washington (DC): U.S. Department of Agriculture, Agricultural Research Service; 2020. [Google Scholar]
- 8. Chen Z, Schoufour JD, Rivadeneira F, Lamballais S, Ikram MA, Franco OH, Voortman T. Plant-based diet and adiposity over time in a middle-aged and elderly population: the Rotterdam Study. Epidemiology. 2019;30(2):303–10. [DOI] [PubMed] [Google Scholar]
- 9. Kim H, Rebholz CM, Garcia-Larsen V, Steffen LM, Coresh J, Caulfield LE. Operational differences in plant-based diet indices affect the ability to detect associations with incident hypertension in middle-aged US adults. J Nutr. 2020;150(4):842–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Martínez-González MA, Sánchez-Tainta A, Corella D, Salas-Salvadó J, Ros E, Arós F, Gómez-Gracia E, Fiol M, Lamuela-Raventós RM, Schröder Het al. A provegetarian food pattern and reduction in total mortality in the Prevención con Dieta Mediterránea (PREDIMED) study. Am J Clin Nutr. 2014;100(suppl_1):320S–8S. [DOI] [PubMed] [Google Scholar]
- 11. Kim H, Caulfield LE, Rebholz CM. Healthy plant-based diets are associated with lower risk of all-cause mortality in US adults. J Nutr. 2018;148(4):624–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Keaver L, Ruan M, Chen F, Du M, Ding C, Wang J, Shan Z, Liu J, Zhang FF. Plant- and animal-based diet quality and mortality among US adults: a cohort study. Br J Nutr. 2021;125(12):1405–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Kim H, Caulfield LE, Garcia-Larsen V, Steffen LM, Coresh J, Rebholz CM. Plant-based diets are associated with a lower risk of incident cardiovascular disease, cardiovascular disease mortality, and all-cause mortality in a general population of middle-aged adults. J Am Heart Assoc. 2019;8(16):e012865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Satija A, Bhupathiraju SN, Spiegelman D, Chiuve SE, Manson JE, Willett W, Rexrode KM, Rimm EB, Hu FB. Healthful and unhealthful plant-based diets and the risk of coronary heart disease in US adults. J Am Coll Cardiol. 2017;70(4):411–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Knuppel A, Papier K, Key TJ, Travis RC. EAT-Lancet score and major health outcomes: the EPIC-Oxford study. Lancet. 2019;394(10194):213–4. [DOI] [PubMed] [Google Scholar]
- 16. Jessri M, Lou WY, L'Abbé MR. The 2015 Dietary Guidelines for Americans is associated with a more nutrient-dense diet and a lower risk of obesity. Am J Clin Nutr. 2016;104(5):1378–92. [DOI] [PubMed] [Google Scholar]
- 17. Health Canada . Canadian Community Health Survey, Cycle 2.2, Nutrition (2004): a guide to accessing and interpreting the data. [Internet]. Ottawa (Ontario): Health Canada; 2006. [Cited 2021 Jul 9]. Available from: https://www.canada.ca/en/health-canada/services/food-nutrition/food-nutrition-surveillance/health-nutrition-surveys/canadian-community-health-survey-cchs/canadian-community-health-survey-cycle-2-2-nutrition-2004-guide-accessing-interpreting-data-health-canada-2006.html. [Google Scholar]
- 18. Health Canada . Reference guide to understanding and using the data: 2015 Canadian Community Health Survey—Nutrition. [Internet]. Ottawa (Ontario): Health Canada; 2017. [Cited 2021 Jul 9]. Available from: https://www.canada.ca/en/health-canada/services/food-nutrition/food-nutrition-surveillance/health-nutrition-surveys/canadian-community-health-survey-cchs/reference-guide-understanding-using-data-2015.html. [Google Scholar]
- 19. Béland Y, Dale V, Dufour J, Hamel M. The Canadian Community Health Survey: building on the success from the past. In: Proceedings of the American Statistical Association Joint Statistical Meetings 2005, Section on Survey Research Methods; 7–11; August 2005; Minneapolis, MN. Alexandria (VA): American Statistical Association; 2005. p. 2738–46. [Google Scholar]
- 20. Statistics Canada . Canadian Community Health Survey—Nutrition: Public Use Microdata File, 2015—archived. Ottawa (Ontario): Statistics Canada; 2018. [Google Scholar]
- 21. Shields M, Gorber SC, Janssen I, Tremblay MS. Bias in self-reported estimates of obesity in Canadian health surveys: an update on correction equations for adults. Health Rep. 2011;22(3):35–45. [PubMed] [Google Scholar]
- 22. USDA Agricultural Research Service (ARS) . AMPM—USDA Automated Multiple-Pass Method. [Internet]. Beltsville (MD): Food Surveys Research Group, USDA ARS; 2009. [Cited 2021 Jul 9]. Available from: http://www.ars.usda.gov/Services/docs.htm?docid=7710. [Google Scholar]
- 23. Health Canada . The Canadian Nutrient File. Nutrition Research Division. Ottawa (Ontario): Health Canada; 2001. [Google Scholar]
- 24. Health Canada . The Canadian Nutrient File. Ottawa (Ontario): Health Canada; 2015. [Google Scholar]
- 25. World Health Organization . International statistical classification of diseases and related health problems (ICD), 10th revision. 2019. [Cited Dec 2021] [Internet]. Available from:https://icd.who.int/browse10/2019/en.
- 26. Manuel DG, Tuna M, Bennett C, Hennessy D, Rosella L, Sanmartin C, Tu JV, Perez R, Fisher S, Taljaard M. Development and validation of a cardiovascular disease risk-prediction model using population health surveys: the Cardiovascular Disease Population Risk Tool (CVDPoRT). CMAJ. 2018;190(29):E871–E882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. World Health Organization . Cardiovascular disease. About cardiovascular diseases. Geneva (Switzerland): WHO; 2017. [Google Scholar]
- 28. Matsunaga M, Hurwitz EL, Li D. Development and evaluation of a Dietary Approaches to Stop Hypertension dietary index with calorie-based standards in equivalent units: a cross-sectional study with 24-hour dietary recalls from adult participants in the National Health and Nutrition Examination Survey 2007–2010. J Acad Nutr Diet. 2018;118(1):62–73.e4. [DOI] [PubMed] [Google Scholar]
- 29. U.S. Department of Agriculture and U.S. Department of Health and Human Services . Dietary Guidelines for Americans. Washington (DC): U.S.Government Printing Office; 2010 [Internet]. Available from: https://health.gov/sites/default/files/2020-01/DietaryGuidelines2010.pdf. [Google Scholar]
- 30. Health Canada . Canada's Dietary Guidelines for health professionals and policy makers. Ottawa (Ontario): Health Canada; 2019. [Google Scholar]
- 31. Imamura F, Jacques PF, Herrington DM, Dallal GE, Lichtenstein AH. Adherence to 2005 Dietary Guidelines for Americans is associated with a reduced progression of coronary artery atherosclerosis in women with established coronary artery disease. Am J Clin Nutr. 2009;90(1):193–201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Yeo D, Mantel H, Liu T-P. Bootstrap variance estimation for the National Population Health Survey. In: American Statistical Association, proceedings of the Survey Research Methods Section. Alexandria (VA): American Statistical Association; 1999. p. 778–83. [Google Scholar]
- 33. Jessri M, Lou WY, L'Abbé MR. Evaluation of different methods to handle misreporting in obesity research: evidence from the Canadian national nutrition survey. Br J Nutr. 2016;115(1):147–59. [DOI] [PubMed] [Google Scholar]
- 34. Garriguet D. Impact of identifying plausible respondents on the under-reporting of energy intake in the Canadian Community Health Survey. Health Rep. 2008;19(4):47–55. [PubMed] [Google Scholar]
- 35. Garriguet D. Accounting for misreporting when comparing energy intake across time in Canada. Health Rep. 2018;29(5):3–12. [PubMed] [Google Scholar]
- 36. National Cancer Institute (NCI) . Usual dietary intakes: SAS macros for the NCI method. [Internet]. Bethesda (MD): NCI; 2018. [Cited 2021 Jul 21]. Available from: https://epi.grants.cancer.gov/diet/usualintakes/macros.html. [Google Scholar]
- 37. Anderson A, Bell A, Adamson A, Moynihan P. A questionnaire assessment of nutrition knowledge—validity and reliability issues. Public Health Nutr. 2002;5(3):497–503. [DOI] [PubMed] [Google Scholar]
- 38. Trochim WMK. Research methods knowledge base. Types of measurement validity. The Web Center for Social Research Methods. [Internet]. 2004. [Cited 2021 Jul 21]. Available from: https://conjointly.com/kb/. [Google Scholar]
- 39. Dennis LK, Snetselaar LG, Nothwehr FK, Stewart RE. Developing a scoring method for evaluating dietary methodology in reviews of epidemiologic studies. J Am Diet Assoc. 2003;103(4):483–7. [DOI] [PubMed] [Google Scholar]
- 40. Stefan N, Kantartzis K, Machann J, Schick F, Thamer C, Rittig K, Balletshofer B, Machicao F, Fritsche A, Häring H-U. Identification and characterization of metabolically benign obesity in humans. Arch Intern Med. 2008;168(15):1609–16. [DOI] [PubMed] [Google Scholar]
- 41. Wildman RP, Muntner P, Reynolds K, McGinn AP, Rajpathak S, Wylie-Rosett J, Sowers MR. The obese without cardiometabolic risk factor clustering and the normal weight with cardiometabolic risk factor clustering: prevalence and correlates of 2 phenotypes among the US population (NHANES 1999–2004). Arch Intern Med. 2008;168(15):1617–24. [DOI] [PubMed] [Google Scholar]
- 42. Wang YB, Shivappa N, Hébert JR, Page AJ, Gill TK, Melaku YA. Association between dietary inflammatory index, dietary patterns, plant-based dietary index and the risk of obesity. Nutrients. 2021;13(5):1536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Heianza Y, Zhou T, Sun D, Hu FB, Manson JE, Qi L. Genetic susceptibility, plant-based dietary patterns, and risk of cardiovascular disease. Am J Clin Nutr. 2020;112(1):220–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Shan Z, Li Y, Baden MY, Bhupathiraju SN, Wang DD, Sun Q, Rexrode KM, Rimm EB, Qi L, Willett WCet al. Association between healthy eating patterns and risk of cardiovascular disease. JAMA Intern Med. 2020;180(8):1090–100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Hu EA, Steffen LM, Coresh J, Appel LJ, Rebholz CM. Adherence to the Healthy Eating Index–2015 and other dietary patterns may reduce risk of cardiovascular disease, cardiovascular mortality, and all-cause mortality. J Nutr. 2020;150(2):312–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Schwingshackl L, Bogensberger B, Hoffmann G. Diet quality as assessed by the Healthy Eating Index, Alternate Healthy Eating Index, Dietary Approaches to Stop Hypertension Score, and health outcomes: an updated systematic review and meta-analysis of cohort studies. J Acad Nutr Diet. 2018;118(1):74–100.e11. [DOI] [PubMed] [Google Scholar]
- 47. Zhong VW, Ning H, Van Horn L, Carnethon MR, Wilkins JT, Lloyd-Jones DM, Allen NB. Diet quality and long-term absolute risks for incident cardiovascular disease and mortality. Am J Med. 2021;134(4):490–8.e24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Heidemann C, Schulze MB, Franco OH, van Dam RM, Mantzoros CS, Hu FB. Dietary patterns and risk of mortality from cardiovascular disease, cancer, and all causes in a prospective cohort of women. Circulation. 2008;118(3):230–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Kant AK, Graubard BI, Schatzkin A. Dietary patterns predict mortality in a national cohort: the National Health Interview Surveys, 1987 and 1992. J Nutr. 2004;134(7):1793–9. [DOI] [PubMed] [Google Scholar]
- 50. Salehi-Abargouei A, Maghsoudi Z, Shirani F, Azadbakht L. Effects of Dietary Approaches to Stop Hypertension (DASH)-style diet on fatal or nonfatal cardiovascular diseases—incidence: a systematic review and meta-analysis on observational prospective studies. Nutrition. 2013;29(4):611–8. [DOI] [PubMed] [Google Scholar]
- 51. Fresán U, Sabaté J, Martínez-Gonzalez MA, Segovia-Siapco G, de la Fuente-Arrillaga C, Bes-Rastrollo M. Adherence to the 2015 Dietary Guidelines for Americans and mortality risk in a Mediterranean cohort: the SUN project. Prev Med. 2019;118:317–24. [DOI] [PubMed] [Google Scholar]
- 52. Hirvonen K, Bai Y, Headey D, Masters WA. Affordability of the EAT–Lancet reference diet: a global analysis. Lancet Glob Health. 2020;8(1):e59–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Zagmutt FJ, Pouzou JG, Costard S. The EAT-Lancet Commission's dietary composition may not prevent noncommunicable disease mortality. J Nutr. 2020;150(5):985–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Fogli-Cawley JJ, Dwyer JT, Saltzman E, McCullough ML, Troy LM, Meigs JB, Jacques PF. The 2005 Dietary Guidelines for Americans and risk of the metabolic syndrome. Am J Clin Nutr. 2007;86(4):1193–201. [DOI] [PubMed] [Google Scholar]
- 55. Hosseini-Esfahani F, Jessri M, Mirmiran P, Bastan S, Azizi F. Adherence to dietary recommendations and risk of metabolic syndrome: Tehran Lipid and Glucose Study. Metabolism. 2010;59(12):1833–42. [DOI] [PubMed] [Google Scholar]
- 56. Huang J, Liao LM, Weinstein SJ, Sinha R, Graubard BI, Albanes D. Association between plant and animal protein intake and overall and cause-specific mortality. JAMA Intern Med. 2020;180(9):1173–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Kipnis V, Midthune D, Buckman DW, Dodd KW, Guenther PM, Krebs-Smith SM, Subar AF, Tooze JA, Carroll RJ, Freedman LS. Modeling data with excess zeros and measurement error: application to evaluating relationships between episodically consumed foods and health outcomes. Biometrics. 2009;65(4):1003–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Tooze JA, Kipnis V, Buckman DW, Carroll RJ, Freedman LS, Guenther PM, Krebs-Smith SM, Subar AF, Dodd KW. A mixed-effects model approach for estimating the distribution of usual intake of nutrients: the NCI method. Stat Med. 2010;29(27):2857–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Brisbois TD, Marsden SL, Anderson GH, Sievenpiper JL. Estimated intakes and sources of total and added sugars in the Canadian diet. Nutrients. 2014;6(5):1899–912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Atkinson FS, Foster-Powell K, Brand-Miller JC. International tables of glycemic index and glycemic load values: 2008. Diabetes Care. 2008;31(12):2281–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Foster-Powell K, Holt SH, Brand-Miller JC. International table of glycemic index and glycemic load values: 2002. Am J Clin Nutr. 2002;76(1):5–56. [DOI] [PubMed] [Google Scholar]
- 62. Health Canada . Bureau of Nutritional Sciences (BNS) food group codes and descriptions – 2015 Canadian Community Health Survey—nutrition. Ottawa (Ontario): Statistics Canada; 2015. [Google Scholar]
- 63. Flood A, Subar AF, Hull SG, Zimmerman TP, Jenkins DJ, Schatzkin A. Methodology for adding glycemic load values to the National Cancer Institute Diet History Questionnaire database. J Am Diet Assoc. 2006;106(3):393–402. [DOI] [PubMed] [Google Scholar]
- 64. Louie JC-Y, Flood V, Turner N, Everingham C, Gwynn J. Methodology for adding glycemic index values to 24-hour recalls. Nutrition. 2011;27(1):59–64. [DOI] [PubMed] [Google Scholar]
- 65. Johnson L, Wilks D, Lindroos A, Jebb S. Reflections from a systematic review of dietary energy density and weight gain: is the inclusion of drinks valid?. Obes Rev. 2009;10(6):681–92. [DOI] [PubMed] [Google Scholar]
- 66. Ledikwe JH, Blanck HM, Khan LK, Serdula MK, Seymour JD, Tohill BC, Rolls BJ. Dietary energy density determined by eight calculation methods in a nationally representative United States population. J Nutr. 2005;135(2):273–8. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data described in the article, code book, and analytic code will be made available upon request pending application and approval (By Statistics Canada).