Abstract
Objective:
Vulnerability indices use quantitative indicators and geospatial data to examine the level of vulnerability to morbidity in a community. The Centers for Disease Control and Prevention (CDC) uses 3 indices for the COVID-19 response: the CDC Social Vulnerability Index (CDC-SVI), the US COVID-19 Community Vulnerability Index (CCVI), and the Pandemic Vulnerability Index (PVI). The objective of this review was to describe these tools and explain the similarities and differences between them.
Methods:
We described the 3 indices, outlined the underlying data sources and metrics for each, and discussed their use by CDC for the COVID-19 response. We compared the percentile score for each county for each index by calculating Spearman correlation coefficients (Spearman ρ).
Results:
These indices have some, but not all, component metrics in common. The CDC-SVI is a validated metric that estimates social vulnerability, which comprises the underlying population-level characteristics that influence differences in health risk among communities. To address risk specific to the COVID-19 pandemic, the CCVI and PVI build on the CDC-SVI and include additional variables. The 3 indices were highly correlated. Spearman ρ for comparisons between the CDC-SVI score and the CCVI and between the CCVI and the PVI score was 0.83. Spearman ρ for the comparison between the CDC-SVI score and PVI score was 0.73.
Conclusion:
The indices can empower local and state public health officials with additional information to focus resources and interventions on disproportionately affected populations to combat the ongoing pandemic and plan for future pandemics.
Keywords: COVID-19, vulnerability, social vulnerability index, GIS, geographic information systems
As of January 2022, more than 887 000 COVID-19–related deaths had been reported, making COVID-19 one of the leading causes of death in the United States. 1 Strong evidence exists that rates of COVID-19 infection are not evenly distributed in the population, with demographic, social, and clinical risk factors associated with increased risk for the disease.2,3 To make equitable decisions on allocating resources, addressing subpopulations vulnerable to COVID-19 morbidity, and implementing interventions, it is necessary to understand community-level vulnerabilities to health risks. 2 Vulnerability indices represent an approach to understanding the factors that make communities vulnerable to health risks.4,5
During the past 2 decades, vulnerability indices have emerged as quantitative measures of vulnerability. 5 Vulnerability refers to the potential negative effects on communities caused by external stresses on human health, such as disease outbreaks or natural disasters. 6 In response to the COVID-19 pandemic and its impacts in the United States, several indices of vulnerability are emerging as online tools.
The Centers for Disease Control and Prevention (CDC) is currently using 3 vulnerability indices for the COVID-19 pandemic response: the CDC Social Vulnerability Index (CDC-SVI), the Pandemic Vulnerability Index (PVI), and the US COVID-19 Community Vulnerability Index (CCVI). Developed in 2011, the CDC-SVI is a validated metric of social vulnerability intended to help public health officials prepare for, respond to, and recover from emergencies and is widely used in research.6,7 An independent effort to validate several social vulnerability indices found the CDC-SVI compared well with other indices, especially in explaining property losses and fatalities. 8 Other validation efforts by CDC are ongoing and have found that the CDC-SVI has translational, convergent, and discriminant validity and is associated with various disaster outcomes.7-11 For example, after Hurricane Katrina, communities in New Orleans, Louisiana, with high CDC-SVI scores were slow to recover regardless of whether they incurred heavy flood damage. 12 The PVI and the CCVI build on the CDC-SVI. The CCVI adds 4 themes that address population density and epidemiologic, health care system, and high-risk environmental factors that may affect COVID-19 outcomes. The PVI adds variables to capture data on COVID-19 infection rates, intervention measures, and health care systems to the CDC-SVI. These indices can be found on CDC’s COVID Data Tracker (CDT), a website that allows users to explore and understand COVID-19 through maps, charts, and data. 1 The CDT combines information from the CDC-SVI, PVI, and CCVI to provide a comprehensive view of COVID-19, its impacts on communities, and trends.
The objective of this study was to describe the 3 indices, outline their underlying data sources and the metrics used, and discuss their current use by CDC for the COVID-19 response.
Methods
We studied 3 vulnerability indices used in CDC’s CDT: the CDC-SVI, the CCVI, and the PVI. We summarized the main features of each index and performed a crosswalk of the variables included in each index to determine overlap between the metrics. We calculated Spearman rank-order correlation coefficients (Spearman ρ) between the 3 indices. Spearman ρ is a measure of the association of ranks between 2 indices, which can be used to assess the consistency (inter-rater reliability) of the different indices. Spearman ρ values range from −1 to +1. A Spearman ρ of +1 indicates a perfect positive association between ranks (ie, index y increases as index x increases), while a Spearman ρ of −1 indicates a perfect negative association between ranks (ie, index y decreases as index x increases). A Spearman ρ of 0 indicates no association between ranks. We used the 11.2.1 model of the PVI, accessed on February 24, 2021, and we accessed the 2018 CDC-SVI and CCVI from their websites on February 24, 2021.
Results
Social Vulnerability Index
In 2011, the Geospatial Research, Analysis, and Services Program at CDC/Agency for Toxic Substances and Disease Registry created the CDC-SVI to assist disaster management officials in identifying the locations of socially vulnerable populations and quantifying the sizes of these populations. 6 CDC-SVI is constructed at the census-tract level, a geographic scale commonly used to analyze community data for policy and planning in government and public health, and at the county level. The CDC-SVI database comprises 15 variables based on the US Census Bureau’s Decennial Census or American Community Survey (Table). 6 These variables are divided into 4 domains:
Table.
Comparison of variables among the 3 vulnerability indices used by the Centers for Disease Control and Prevention for the COVID-19 response
| Variable | CDC-SVI a | CCVI b | PVI c |
|---|---|---|---|
| Percentage of individuals living below the federal poverty level | x | x | x |
| Percentage of civilians aged ≥16 y who are unemployed | x | x | x |
| Per-capita income | x | x | x |
| Percentage of individuals aged ≥25 y with no high school diploma | x | x | x |
| Percentage of individuals aged ≥65 y | x | x | x |
| Percentage of individuals aged ≤17 y | x | x | |
| Percentage of the civilian noninstitutionalized population with a disability | x | x | |
| Percentage of single-parent households with children aged <18 y | x | x | |
| Percentage of individuals who belong to racial and ethnic minority groups (everyone except non-Hispanic White people) | x | x | |
| Percentage of individuals aged ≥5 y who speak English “less than well” | x | x | |
| Percentage of housing in structures with ≥10 units | x | x | x |
| Percentage of mobile homes | x | x | x |
| Percentage of crowded households (households with more people than rooms) | x | x | x |
| Percentage of households with no vehicle available | x | x | x |
| Percentage of individuals living in group quarters | x | x | x |
| Percentage of the population that has no health insurance | x | x | |
| Percentage of households without access to indoor plumbing | x | ||
| Annual cancer incidence per 100 000 population | x | ||
| Number of individuals living with HIV per 100 000 population | x | ||
| Percentage of adults diagnosed with high cholesterol | x | ||
| Percentage of adults diagnosed with a stroke | x | ||
| Percentage of adults diagnosed with heart disease | x | ||
| Percentage of adults diagnosed with chronic obstructive pulmonary disease, emphysema, or chronic bronchitis | x | ||
| Percentage of adults reporting being obese | x | x | |
| Percentage of adults ever diagnosed with diabetes | x | x | |
| Percentage of adults who report smoking cigarettes | x | x | |
| Intensive care unit beds per 100 000 population | x | ||
| Hospital beds per 100 000 population | x | x | |
| Epidemiologists per 100 000 population | x | ||
| Agency for Healthcare Research and Quality Prevention Quality Indicator overall composite score | x | ||
| State-level health spending per capita | x | ||
| Aggregate cost of medical care | x | ||
| Percentage of population with a primary care physician | x | ||
| Public Health Emergency Preparedness cooperative agreement total funding per capita | x | ||
| Health laboratories per 100 000 population | x | ||
| Emergency services per 100 000 population | x | ||
| Long-term care facility residents per 100 000 population | x | ||
| Prison population per 100 000 population | x | ||
| Percentage of the population employed in an industry in which frequent contact with other people in the workplace occurs | x | ||
| Population density or estimated daytime population | x | x | |
| Number of transmissible cases of COVID-19 | x | ||
| COVID-19 disease spread | x | ||
| Average traffic volume per meter of major roadway in the county | x | ||
| Numerical score based on social distancing scoreboard | x | ||
| Population divided by the number of COVID-19 tests performed | x | ||
| Percentage of population that self-identifies as Black or African American | x | ||
| Percentage of population that self-identifies as American Indian or Alaska Native | x | ||
| Average daily density of fine particulate matter in µg per cubic m | x | ||
| Years of potential life lost before age 75 y per 100 000 population (age-adjusted) | x |
Abbreviations: CCVI, COVID-19 Community Vulnerability Index; CDC-SVI, Centers for Disease Control and Prevention Social Vulnerability Index; PVI, Pandemic Vulnerability Index.
Data source: Centers for Disease Control and Prevention. 6
Data source: Surgo Ventures. 13
Data source: National Institute for Environmental Health Sciences. 14
Domain 1: Socioeconomic status. Percentage of individuals living below the federal poverty level, percentage of civilians aged ≥16 years who are unemployed, per-capita income, percentage of individuals aged ≥25 years with no high school diploma.
Domain 2: Household composition and disability. Percentage of individuals aged ≥65 years, percentage of individuals aged ≤17 years, percentage of the civilian noninstitutionalized population with a disability, percentage of single-parent households with children aged <18 years.
Domain 3: Racial and ethnic minority status and language. Percentage of individuals who belong to racial and ethnic minority groups (everyone except non-Hispanic White people), percentage of individuals aged ≥5 years who speak English “less than well.”
Domain 4: Housing type and transportation. Percentage of housing in structures with ≥10 units, percentage of mobile homes, percentage of crowded households (households with more people than rooms), percentage of households with no vehicle available, percentage of individuals living in group quarters.
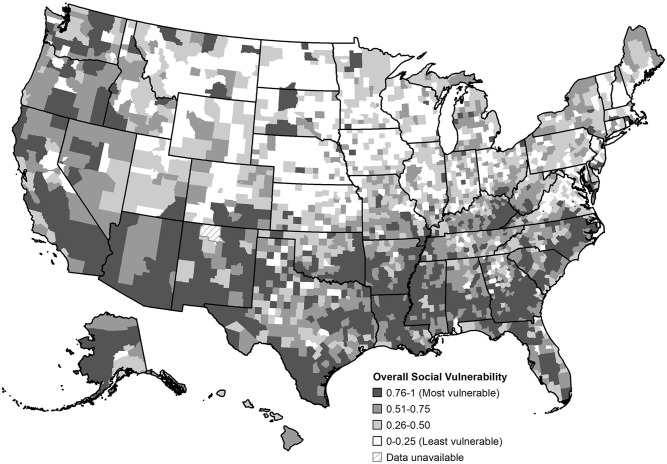
The CDC-SVI ranks all US census tracts and counties with a nonzero population from the lowest to highest vulnerability for each of these census variables, and a percentile rank is calculated for each CDC-SVI variable at the census-tract and county level. For each of the 4 themes, the CDC-SVI calculates a tract- and county-level percentile rank. Finally, an overall percentile rank is calculated for each tract and county as the composite variable ranking. All percentile ranks in the CDC-SVI range from 0 to 1, with 1 representing the highest level of vulnerability. A characteristic of the SVI is that the value with a percentile rank of 0 might not be significantly different from a value with a percentile rank of 1; however, percentile ranks for any data do not require significance, nor does significance need to be established. Data can be classified by quartiles, and classification ranges from least vulnerable to most vulnerable (Figure 1).
Figure 1.
Centers for Disease Control and Prevention (CDC) 2018 Social Vulnerability Index, by US county, generated February 24, 2021. Social vulnerability refers to the negative effects on communities caused by external stresses on human health. Data were mapped by using quartile classification. Data source: CDC. 6
In the CDT, the overall CDC-SVI score is provided in the county view of the Your Community tab. Several projects are using CDC-SVI to identify areas with high CDC-SVI scores and low COVID-19 vaccine access. 15
US COVID-19 Community Vulnerability Index
The Surgo Foundation, a nonprofit organization based in Washington, DC, constructed the CCVI to assess which US communities may be more susceptible than others to negative health, social, and economic impacts of the COVID-19 pandemic. 13 The CCVI adds 4 themes to the CDC-SVI themes that address population density and epidemiological, health care systems, and high-risk environment factors that may affect COVID-19 outcomes (Table). The CCVI uses data from many sources, such as the US Bureau of Labor Statistics and the Association of Public Health Laboratories. The CCVI comprises 40 variables grouped into the following 7 themes:
Theme 1: Socioeconomic status. Percentage of individuals living below the federal poverty level, percentage of civilians aged ≥16 years who are unemployed, per-capita income, percentage of individuals aged ≥25 years with no high school diploma, percentage of the population that is uninsured.
Theme 2: Racial and ethnic minority status and language. Percentage of individuals who belong to racial and ethnic minority groups (everyone except non-Hispanic White people), percentage of individuals aged >5 years who speak English “less than well.”
Theme 3: Housing type, transportation, household composition, and disability. Percentage of housing in structures with ≥10 units, percentage of households with more people than rooms, percentage of households with no vehicle available, percentage of individuals living in group quarters, percentage of individuals aged ≤17 years, percentage of single-parent households with children aged <18 years, percentage of households without access to indoor plumbing, percentage of mobile homes, percentage of the civilian noninstitutionalized population with a disability.
Theme 4: Epidemiological factors. Percentage of adults diagnosed with high cholesterol; percentage of adults diagnosed with a stroke; percentage of adults ever diagnosed with heart disease; percentage of adults diagnosed with chronic obstructive pulmonary disease, emphysema, or chronic bronchitis; percentage of adults reporting smoking cigarettes; annual cancer incidence per 100 000 population; number of individuals living with an HIV diagnosis per 100 000 population; percentage of adults reporting being obese; percentage of adults ever diagnosed with diabetes; percentage of individuals aged ≥65 years.
Theme 5. Health care system factors. Intensive care unit beds per 100 000 population, hospital beds per 100 000 population, number of state-level epidemiologists per 100 000 population, Agency for Healthcare Research and Quality Prevention Quality Indicator overall composite score, state-level health spending per capita, aggregate cost of medical care, percentage of the population with a primary care physician, total state-level Public Health Emergency Preparedness cooperative agreement funding per capita, health laboratories per 100 000 population, state-level emergency services per 100 000 population (includes emergency and relief services and freestanding ambulatory surgical and emergency centers).
Theme 6: High-risk environments. These environments are generally defined as environments in which people are at high risk of exposure to disease because of proximity to and interaction with other people. For example, long-term care residents per 100 000 population, prison population per 100 000 population, percentage of the population employed in an industry at high risk of contact with other people in the workplace based on frequency and duration of contact.
Theme 7: Population density. Estimated total number of people per unit area.
To create the composite CCVI measure, percentiles of each variable are summed for each CCVI theme. 11 CCVI data can be classified by quartiles (Figure 2).
Figure 2.
The COVID-19 Community Vulnerability Index, by US county, generated February 24, 2021. Community vulnerability is defined as a limited ability to mitigate, treat, and delay transmission of virus and not withstand its secondary effects on health, economic, and social outcomes. Data were mapped by using quartile classification. Data source: Surgo Ventures. 13
The CCVI index score is provided in the Your Community/County View tab in the CDC CDT. 1 The CCVI is a free tool accessible online through Precision for COVID Data Explorer and allows users to explore data to plan, prepare, and respond to COVID-19. 11 Users can select the geographic unit (ie, state, county, or census tract) and indicators of interest and use the vulnerability filter to focus on data for specific populations (eg, counties highly vulnerable to the COVID-19 pandemic). Data are displayed in maps, histograms, and line graphs.
COVID-19 Pandemic Vulnerability Index
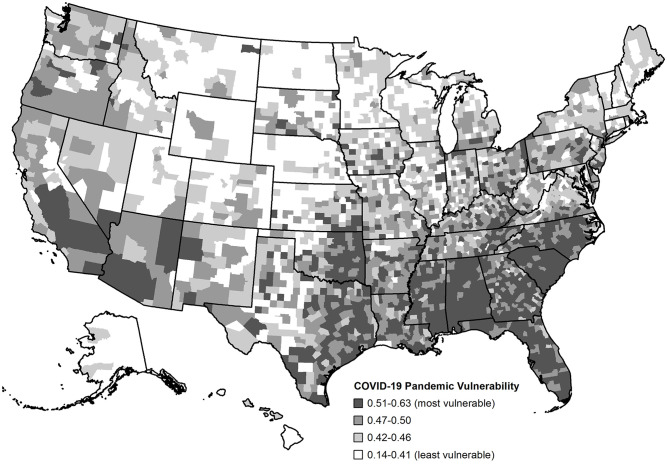
North Carolina State University, Texas A&M University, and the National Institute of Environmental Health Sciences developed the PVI and its scorecard visualization. The interactive PVI Dashboard provides a visual synthesis of dynamic information at the county level to monitor disease trajectories, communicate local vulnerabilities, forecast key outcomes, and guide informed responses. 2 The PVI integrates multiple data streams into an overall score derived from 12 key indicators, including vulnerability factors captured in CDC-SVI and emerging factors across 4 domains: current COVID-19 infection rates, baseline population concentration, current COVID-19 interventions, and health and environmental vulnerabilities (Table). The default view of the map (Figure 3) shows overall vulnerability, and interactive displays provide details on the components of the PVI Scorecard. The PVI Scorecard translates numerical results into a visual representation, with each vulnerability factor representing a slice of a radar chart. The dashboard provides additional visualization tools to help contextualize various measures of vulnerability. Data sources used in the version 11.2.1 model include CDC-SVI, 16 COVID-19 testing rates, 17 real-time social distancing metrics from mobile device data, 18 and dynamic measures of disease spread and case numbers. 19
Figure 3.
The National Institutes of Health COVID-19 Pandemic Vulnerability Index, by US county, generated February 24, 2021. Pandemic vulnerability refers to the susceptibility of populations to the pandemic and lack of coping resources to alleviate its impact. Data were mapped by using quartile classification. Data source: National Institute for Environmental Health Sciences. 14
Currently, the PVI comprises 4 domains (infection rate, population concentration, intervention measures, health and environment) with 12 slices, with each slice assigned a percentage of the total index score. 14 These domains include static measures of overall vulnerability and dynamic measures that are updated daily. Machine learning approaches were used to select the data streams and informed their relative weighting. 2
- Domain 1: COVID-19 infection rate (24% of total index score)
- Slice 1: Transmissible cases (20% of total index score). Population size divided by cases from the previous 14 days.
- Slice 2: Disease spread (4% of total index score). Percentage of total cases that are from the previous 14 days.
- Domain 2: Population concentration (16% of total index score)
- Slice 3: Population mobility (8% of total index score). Estimated daytime population and baseline traffic measured by the average traffic volume per meter of major roadway in the county. 20
- Slice 4: Residential density (8% of total index score). Percentage of housing in structures with ≥10 units, percentage of mobile homes, percentage of crowded households (households with more people than rooms), percentage of households with no vehicle available, and percentage of individuals living in group quarters. 21
- Domain 3: Intervention measures (16% of total index score)
- Slice 5: Social distancing (8% of total index score). Numerical score based on a social distancing scoreboard assigned by considering the change in overall distance traveled and the change in nonessential visits relative to a baseline (previous year) based on cell phone mobility data. 18
- Slice 6: Testing (8% of total index score). Population divided by the number of tests performed (statewide only due to the availability of data).
- Domain 4: Health and environment (44% of total index score)
- Slice 7: Population demographic characteristics (8% of total index score). Percentage of the population that self-identifies as Black or African American, American Indian, or Alaska Native.
- Slice 8: Air pollution (8% of total index score). Average daily density of fine particulate matter in micrograms per cubic meter. 22
- Slice 9: Age distribution (8% of total index score). Percentage of the population aged ≥65 years.
- Slice 10: Comorbidities (8% of total index score). Years of potential life lost before age 75 years per 100 000 population (age-adjusted), percentage of adults who are current smokers, 23 percentage of adults aged ≥20 years with diagnosed diabetes, 24 and percentage of the adult population (aged ≥20 years) reporting a body mass index ≥30 kg/m2.
- Slice 11: Health disparities (8% of total index score). Percentage of the population that is uninsured 21 and the CDC-SVI Socioeconomic Status domain, which integrates data on the percentage of the population living below the federal poverty level, percentage of civilians aged ≥16 years who are unemployed, per-capita income, and percentage of individuals aged ≥25 years with no high school diploma. 21
- Slice 12: Hospital beds (4% of total index score). Number of hospital beds for hospitals with open status and general medical and surgical designation.
The PVI is embedded in the CDC CDT 1 under the Your Community/Pandemic Vulnerability tab (which displays the PVI Dashboard). Data can be viewed by rank (from the top 20% to >80%) and by slices (low, medium, and high risk). This information is also available in a stand-alone PVI Dashboard on the National Institute of Environmental Health Sciences website. 25
Correlation Between 3 Indices
The 3 indices for all US counties were highly correlated (Figure 4). The Spearman ρ for comparisons between the CDC-SVI score and the CCVI and between the CCVI and the PVI score was 0.83 (P < .001) for both. The coefficient for the comparison between the CDC-SVI score and the PVI score was 0.73 (P < .001).
Figure 4.
Comparison of percentile scores of 3 vulnerability indices for each US county, 2021. 9 Vulnerability refers to the potential negative effects on communities caused by external stresses on human health, such as disease outbreaks or natural disasters. Each dot represents a US county. Percentile score for each county for each index was compared by calculating Spearman correlation coefficients. A, Comparison of CCVI and CDC-SVI. B, Comparison of PVI and CDC-SVI. C, Comparison of PVI and CCVI. Abbreviations and data sources: CCVI, US COVID-19 Community Vulnerability Index 13 ; CDC-SVI, Centers for Disease Control and Prevention Social Vulnerability Index 6 ; PVI, Pandemic Vulnerability Index (Model 11.2.1), 14 accessed February 24, 2021.
Discussion
Reducing vulnerability to COVID-19 and other diseases requires attention to social vulnerabilities. Vulnerability indices are useful for identifying and examining health disparities. Knowledge of these indices is an important part of understanding tools available to reveal geographic patterns of potential vulnerability to emergencies, disease outbreaks, and disparities, such as racial and ethnic inequalities. Understanding the differences among these indices helps to determine which tool is most appropriate for its intended purpose. Contextualizing data on racial and ethnic disparities highlights resource deficiencies related to low socioeconomic status, chronic stress, and place-based risks. 26 Vulnerability indices and the accompanying mapping can assist with COVID-19 intervention efforts by helping agencies identify areas in need of additional resources, such as places with high CDC-SVI scores and low vaccination rates to strengthen vaccine distribution efforts.
The 3 vulnerability indices reviewed here share many, but not all, constituent measures. The CCVI and PVI are modifications of the CDC-SVI. The CCVI adds indicators of COVID-19 vulnerability, such as access to health care. 13 In addition to adding indicators of COVID-19 vulnerability, the PVI data visualization tool supports dynamic monitoring by including both static drivers (eg, health care characteristics) and dynamic factors (eg, infection rate) and enabling the addition and removal of information layers. 2
Addressing social factors that contribute to poor health outcomes is essential to addressing inequities in health impacts of emergencies. Recent work has sought to understand associations between vulnerability factors and COVID-19 outcomes using social vulnerability indices. For instance, higher county-level CDC-SVI scores were associated with a higher case fatality rate but not COVID-19 incidence. 27 Another study assessed the relationship between COVID-19 cases and social vulnerability using CDC-SVI scores and COVID-19 case-count data. 28 The authors found that higher overall SVI score and percentile increases in racial and ethnic minority status and language were associated with increased COVID-19 case counts, highlighting the impact of social vulnerability factors during the pandemic. The relationship between social vulnerability and COVID-19 varied among US counties, as seen in previous studies, demonstrating the nonuniform distribution of social vulnerability during emergencies in the United States.7-12 Although the CDC-SVI was originally developed for natural disasters, many agencies and government bodies have used SVI indicators during the COVID-19 pandemic to assess vulnerability and assist with prioritizing the distribution of resources, such as COVID-19 testing sites and vaccinations to ensure effectiveness and equity. 29 A recent cross-sectional study examined the association between US county-level sociodemographic risk factors taken from the CDC-SVI database and COVID-19 incidence and mortality. The authors found a wide range of sociodemographic factors—including socioeconomic status, belonging to a racial or ethnic minority group, and environmental factors—that were significantly associated with weekly COVID-19 incidence and mortality. 30
Limitations
Our study had several limitations. First, all demographic and socioeconomic data included in the 3 indices are based on 2014-2018 American Community Survey 5-year estimates. Thus, the indices do not account for sociodemographic changes that occurred during the COVID-19 pandemic. The CDC-SVI and CCVI are static measures of social vulnerability, whereas the PVI includes dynamic COVID-19 epidemiologic data. However, the PVI was developed only for US counties, while data for the CDC-SVI and CCVI are accessible at the census-tract level and may be more easily mobilized for community-level COVID-19 prevention and mitigation efforts than county-based indices. Second, we did not conduct a full evaluation of each index, nor did we compare the indices with outcomes, such as COVID-19 case counts or death rates. Future research could examine these relationships. Karaye and Horney 28 found that SVI variables explained only 38.9% (R 2 = 0.389) of the variability in COVID-19 case counts, indicating further studies are warranted to explore additional factors to explain case counts of COVID-19 infection. Third, we did not examine all indices that quantitatively measure vulnerability. Many indices have emerged during the past 2 decades as quantitative measures of vulnerability, including those not discussed here, such as the US Census Community Resilience Estimates (CRE). 31 The CRE measures community resilience to disasters by using small-area estimation techniques and provides estimates of the total number of people living in a community by the number of risk factors. CDC and the US Department of Health and Human Services Office of Minority Health recently developed the Minority Health Social Vulnerability Index to enhance existing resources to support the identification of racial and ethnic minority communities at greatest risk for disproportionate impact and adverse outcomes of the COVID-19 pandemic. 32 This experimental product was released in late 2021 as a customization of the standard CDC-SVI. All indices are tools decisions makers can explore in addition to other data to make equitable decisions on allocating resources, addressing socially vulnerable subpopulations, and implementing interventions.
Conclusion
In the United States, impacts of the COVID-19 pandemic vary widely based on geographic location and population-level social factors. Indices that summarize quantitative metrics to assess social vulnerabilities are used to understand these differential impacts. 5 Use of the CDC-SVI is helpful to determine communities with high levels of vulnerability. Modification of the index to include additional vulnerability factors, as with the CCVI and PVI, combined with sophisticated analysis and visualization tools, can empower public health officials with additional information to focus resources and interventions on disproportionately affected populations. Knowledge of available indices is important to combat the COVID-19 pandemic and future pandemics.
Footnotes
Declaration of Conflicting Interests: The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The authors received no financial support for the research, authorship, and/or publication of this article.
ORCID iDs: Amy Wolkin, DrPH  https://orcid.org/0000-0003-4307-7641
https://orcid.org/0000-0003-4307-7641
David Reif, PhD  https://orcid.org/0000-0001-7815-6767
https://orcid.org/0000-0001-7815-6767
Danielle Sharpe, MS  https://orcid.org/0000-0003-1898-6202
https://orcid.org/0000-0003-1898-6202
References
- 1. Centers for Disease Control and Prevention. COVID data tracker. Accessed September 9, 2021. https://covid.cdc.gov/covid-data-tracker/#datatracker-home
- 2. Marvel SW, House JS, Wheeler M, et al. The COVID-19 Pandemic Vulnerability Index (PVI) Dashboard: monitoring county-level vulnerability using visualization, statistical modeling, and machine learning. Environ Health Perspect. 2021;129(1):017701. doi: 10.1289/ehp8690 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Tan TQ, Kullar R, Swartz TH, et al. Location matters: geographic disparities and impact of coronavirus disease 2019 (COVID-19). J Infect Dis. 2020;222(12):1951-1954. doi: 10.1093/infdis/jiaa583 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Amram O, Amiri S, Lutz RB, Rajan B, Monsivais P. Development of a vulnerability index for diagnosis with the novel coronavirus, COVID-19, in Washington State, USA. Health Place. 2020;64:102377. doi: 10.1016/j.healthplace.2020.102377 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Tate E. Uncertainty analysis for a social vulnerability index. Ann Assoc Am Geogr. 2013;103(3):526-543. doi: 10.1080/00045608.2012.700616 [DOI] [Google Scholar]
- 6. Centers for Disease Control and Prevention. CDC Social Vulnerability Index. Accessed April 16, 2021. https://www.atsdr.cdc.gov/placeandhealth/svi/index.html
- 7. Flanagan BE, Hallisey EJ, Adams E, Lavery A. Measuring community vulnerability to natural and anthropogenic hazards: the Centers for Disease Control and Prevention’s Social Vulnerability Index. J Environ Health. 2018;80(10):34-36. [PMC free article] [PubMed] [Google Scholar]
- 8. Bakkensen LA, Fox-Lent C, Read LK, Linkov I. Validating resilience and vulnerability indices in the context of natural disasters. Risk Anal. 2017;37(5):982-1004. doi: 10.1111/risa.12677 [DOI] [PubMed] [Google Scholar]
- 9. Rufat S, Tate E, Emrich CT, Antolini F. How valid are social vulnerability models? Ann Am Assoc Geogr. 2019;109(4):1131-1153. doi: 10.1080/24694452.2018.1535887 [DOI] [Google Scholar]
- 10. Lehnert EA, Wilt G, Flanagan B, Hallisey E. Spatial exploration of the CDC’s Social Vulnerability Index and heat-related health outcomes in Georgia. Inter J Disaster Risk Reduct. 2020;46:101517. doi: 10.1016/j.ijdrr.2020.101517 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Fletcher KM, Espey J, Grossman MK, et al. Social vulnerability and county stay-at-home behavior during COVID-19 stay-at-home orders, United States, April 7-April 20, 2020. Ann Epidemiol. 2021;64:76-82. doi: 10.1016/j.annepidem.2021.08.020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Flanagan BE, Gregory EW, Hallisey EJ, Heitgerd JL, Lewis B. A social vulnerability index for disaster management. J Homeland Secur Emerg Manage. 2011;8(1):article 3. doi: 10.2202/1547-7355.1792 [DOI] [Google Scholar]
- 13. Surgo Ventures. The US COVID Community Vulnerability Index (CCVI). Vulnerability—how well a community handles the repercussions of a COVID-19 outbreak matters. Updated April 16, 2021. Accessed April 16, 2021. https://precisionforcovid.org/ccvi
- 14. National Institute for Environmental Health Sciences. Details for PVI maps. Accessed April 16, 2021. https://www.niehs.nih.gov/research/programs/coronavirus/covid19pvi/details/index.cfm
- 15. Hughes MM, Wang A, Grossman MK, et al. County-level COVID-19 vaccination coverage and social vulnerability—United States, December 14, 2020–March 1, 2021. MMWR Morb Mortal Wkly Rep. 2021;70(12):431-436. doi: 10.15585/mmwr.mm7012e1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Horney J, Nguyen M, Salvesen D, Dwyer C, Cooper J, Berke P. Assessing the quality of rural hazard mitigation plans in the southeastern United States. J Plann Educ Res. 2017;37(1):56-65. doi: 10.1177/0739456X16628605 [DOI] [Google Scholar]
- 17. Atlantic Monthly Group. The COVID Tracking Project. 2021. Updated March 7, 2021. Accessed April 16, 2021. https://covidtracking.com
- 18. Unacast. COVID-19 Toolkit Social Distancing Scoreboard. Accessed April 16, 2021. https://www.unacast.com/covid19/social-distancing-scoreboard
- 19. USA Facts. Understanding the COVID-19 pandemic. Accessed April 16, 2021. https://usafacts.org/issues/coronavirus
- 20. US Environmental Protection Agency. EJSCREEN: environmental justice screening and mapping tool. Accessed April 16, 2021. https://www.epa.gov/ejscreen
- 21. US Census Bureau. American Community Survey data tables. Accessed April 23, 2021. https://www.census.gov/acs/www/data/data-tables-and-tools
- 22. Centers for Disease Control and Prevention. National Environmental Public Health Tracking Network. Accessed April 23, 2021. https://ephtracking.cdc.gov
- 23. Centers for Disease Control and Prevention. Behavioral Risk Factor Surveillance System. Prevalence data & data analysis tools. Accessed April 23, 2021. https://www.cdc.gov/brfss/data_tools.htm
- 24. Centers for Disease Control and Prevention. Diagnosed diabetes. Accessed April 23, 2021. https://gis.cdc.gov/grasp/diabetes/diabetesatlas.html
- 25. National Institute of Environmental Health Sciences. COVID-19 Pandemic Vulnerability Index (PVI). Accessed April 16, 2021. https://covid19pvi.niehs.nih.gov
- 26. Chowkwanyun M, Reed AL. Racial health disparities and COVID-19—caution and context. N Engl J Med. 2020;383(3):201-203. doi: 10.1056/nejmp2012910 [DOI] [PubMed] [Google Scholar]
- 27. Nayak A, Islam SJ, Mehta A, et al. Impact of social vulnerability on COVID-19 incidence and outcomes in the United States. medRxiv. Preprint April 14, 2020. doi: 10.1101/2020.04.10.20060962 [DOI] [Google Scholar]
- 28. Karaye IM, Horney JA. The impact of social vulnerability on COVID-19 in the U.S.: an analysis of spatially varying relationships. Am J Prev Med. 2020;59(3):317-325. doi: 10.1016/j.amepre.2020.06.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Michigan Department of Health and Human Services. Social vulnerability & COVID-19. Accessed April 16, 2021. https://www.michigan.gov/documents/coronavirus/Social_Vulnerability_and_COVID-19-v4_715525_7.pdf
- 30. Karmakar M, Lantz PM, Tipirneni R. Association of social and demographic factors with COVID-19 incidence and death rates in the US. JAMA Netw Open. 2021;4(1):e2036462. doi: 10.1001/jamanetworkopen.2020.36462 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. US Census Bureau. Community resilience estimates. Accessed August 30, 2021. https://www.census.gov/programs-surveys/community-resilience-estimates.html
- 32. US Department of Health and Human Services, Office of Minority Health. Minority Health SVI. Accessed November 4, 2021. https://www.minorityhealth.hhs.gov/minority-health-svi