Abstract
Native patellar tendon injuries are seen in younger patients compared to quadriceps tendon ruptures.
Up to a third of the patients may have local (antecedent tendinopathy and cortisone injections) or systemic risk factors (obesity, diabetes, hyperparathyroidism, chronic renal failure, fluoroquinolone or statin use) of injury, these are more frequent in bilateral disruptions.
Complete extensor mechanism disruptions should be repaired surgically. Although isolated primary repair has been reported to have good outcomes in younger patients with acute tears and good tendon quality, augmentation of the repair with autograft, allograft or synthetic material should be considered in patients with poor tendon quality, chronic tears or tendon defects.
High rates of return to work/sports have been reported in native patellar and quadriceps tendon tears, with re-rupture rates <5%.
Extensor mechanism disruptions in patients with a total knee arthroplasty are challenging due to older age, systemic co-morbidities and poor local conditions, resulting in inferior outcomes compared to native extensor mechanism injuries. Some form of augmentation with autograft, allograft or synthetics is advisable in all cases. Salvage procedures such as whole extensor mechanism allografts provide acceptable outcomes in multiply operated knees with extensive bone and soft tissue deficits.
Keywords: knee extensor mechanism, patellar tendon rupture, quadriceps tendon rupture, total knee arthroplasty
Extensor mechanism disruptions are serious knee injuries resulting in considerable loss of function and morbidity. The injury may present itself in three main settings, namely, primary ruptures of the tendon, disruptions in patients with a knee replacement and finally patellar tendon ruptures associated with multi-ligament injuries of the knee. Early surgical repair with or without augmentation in the first few weeks following injury is advisable in acute injuries as delayed treatment results in inferior outcomes and may require more complex reconstructions (1). The postoperative recovery takes several months and requires extended rehabilitation programs. A recent systematic review of 48 studies has reported re-rupture rates of 0.3% for patellar and 2.6% for quadriceps tendon repairs (2). Although satisfactory patient-reported outcomes are possible after repair, loss in muscle volume and electromyographic changes may persist even 10 years after surgery (3). This paper will review the epidemiology, clinical presentation, imaging and treatment options of this serious knee injury.
Patellar tendon ruptures
Injury mechanism
Three main injury mechanisms resulting in patellar tendon ruptures are:
Indirect low-energy trauma is the most common tear type, occurring after eccentric contraction of the quadriceps muscle.
Indirect high-energy trauma: patellar tendon rupture may be a part of multi-ligamentous injury of the knee and may be accompanied by meniscus and cartilage injuries, avulsion fractures and neurovascular injury.
Direct injury to the tendon: possible injury mechanisms include penetrating trauma, iatrogenic injuries or dislocation of the tibial bearing after knee replacement.
Epidemiology
The incidence of patellar tendon ruptures has been reported to be 0.68 per 100,000 person-years in the general population (4). The peak incidence of low-energy patellar tendon tears is seen in the third and fourth decades of life in non-arthroplasty patients.
A variety of risk factors including age > 40, steroid injections (5), previous patellar tendinopathy, diabetes, obesity, inflammatory arthritis (systemic lupus erythematosus, gout and rheumatoid arthritis) and osteogenesis imperfecta have been reported. Systemic conditions such as hyperparathyroidism, chronic renal failure and dialysis and Ehlers–Danlos syndrome may increase the risk of bilateral tendon injuries (6). Repetitive micro-trauma in athletes leading to patellar tendinopathy may play a role (7). The use of fluoroquinolones has been associated with an increased risk of tendon ruptures (8). However, a recent study of over 1 million cases could find no association of tendon ruptures with fluoroquinolones except for levofloxacin (9).
Clinical presentation
The injury is quite dramatic with acute pain followed by swelling and inability to bear weight. A palpable defect may be observed if the tear is complete and the patella has migrated proximally. The hallmark of patellar tendon injury is weakness or loss of active extension. This may be difficult to appreciate in the acutely painful and swollen knee, and a high index of suspicion is warranted.
Imaging
Plain radiographs may depict avulsion fractures from the inferior pole of the patella or rarely the tibial tuberosity. Unilateral patella alta compared to the uninjured knee may be observed in complete tears. An Insall–Salvati index over 1.2 is indicative of a patellar tendon tear (Fig. 1). Changes in the inferior pole of the patella or the tibial tuberosity may be clues for antecedent tendinopathy.
Figure 1.
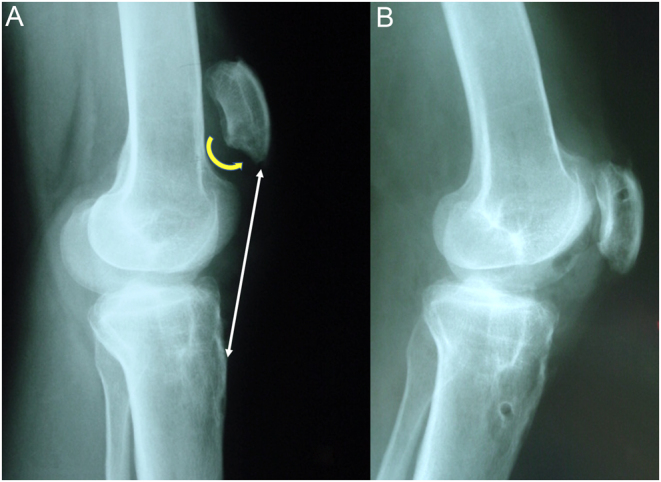
(A) Lateral X-ray of a patient with patellar tendon rupture, note patella alta and anterior prominence of the inferior patella pole; (B) Correction of patellar height after primary repair and augmentation with hamstring tendon grafts through bone tunnels.
Ultrasound diagnosis of patellar tendon tears is relatively inexpensive and readily available but is operator-dependent. A high rate of false-positive results (up to 33%) has been reported in some studies, particularly for quadriceps tendon tears in obese or muscular patients (10).
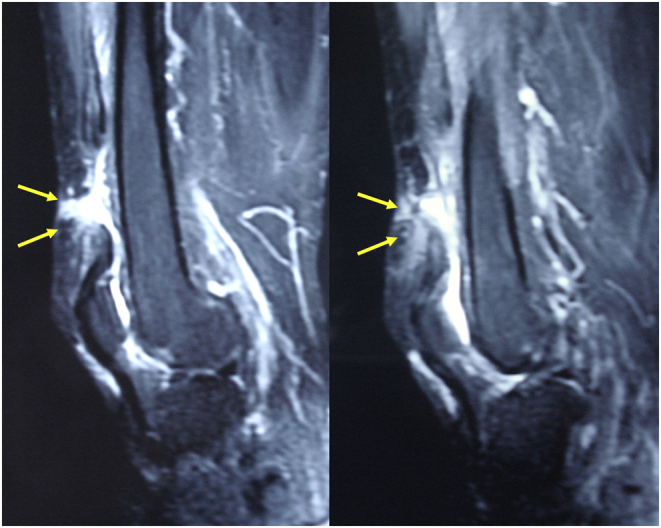
The gold standard in imaging of patellar tendon tears is MRI. Undulating appearance of the tendon with discontinuity at the tear site is typical for complete tears (Fig. 2). Partial tears may appear as increased signal intensity at the patella-tendon interface and thickening of the tendon (11).
Figure 2.
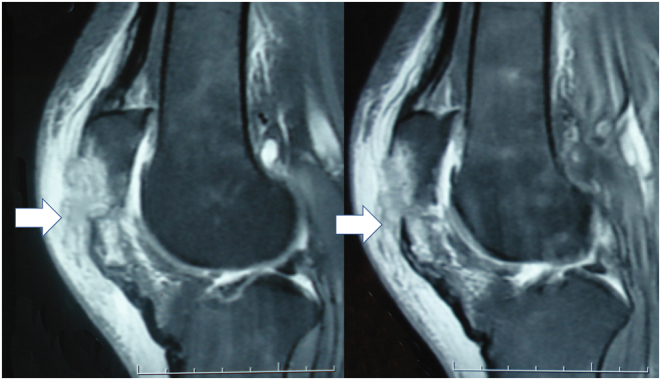
MRI of a patient with avulsion of the patellar tendon from the patella. Hyperintense defect at the injury site (white arrow) with undulation of the tendon is visible.
Treatment
Partial tears of the patellar tendon may be treated non-operatively (12). No clear guidelines exist, but a few weeks of immobilization in extension followed by gradually increasing passive flexion has been advocated. Strengthening exercises can be started after 6 weeks.
Primary repair is indicated for acute complete patellar tendon ruptures with good tissue quality (13). Transosseous tunnels or suture anchors are the most common methods of fixation. Suture anchor repair has demonstrated similar or superior biomechanical properties compared to the traditional technique of trans osseous repair. Less gapping at the repair site and better resistance to cyclic loading have been proposed as advantages of suture anchor repairs (14, 15).
The addition of metal cables or synthetic tapes to protect the primary repair increases the stability of the construct, decreases gapping at the repair site and may allow for earlier motion (11, 16). Historically, metal cable or cerclage wires have been used to protect the repair; however, these have been associated with material breakage, infection, skin necrosis and may necessitate a second surgery for implant removal. Ultra-high molecular weight polyethylene cables/wires (17, 18) and polyester tapes (19) and PDS cords (20) have also been used to augment the repair, avoiding most of the complications of metal cables or wires.
Although satisfactory outcomes can be achieved in acute patellar tendon repairs without augmentation in younger athletes (21), biological augmentation with autologous tissues may improve the outcomes if the quality of the tendon or strength of the repair is found to be inadequate during primary repair (22). Hamstring tendons are readily available, close to the repair site and can be harvested with minimal morbidity. These tendons may be passed through transpatellar tunnels or routed around the proximal patellar pole and sutured onto each other to increase stability. This author prefers to use two transverse tunnels, one in the patella and the other at the level of tibial tuberosity if an adequate length of hamstring tendons can be harvested. The tendons are weaved through the lateral and medial retinaculae and fixed in the boney tunnels using biodegradable interference screws (Fig. 3). Restoration of correct patellar height is critical and can be verified radiologically.
Figure 3.
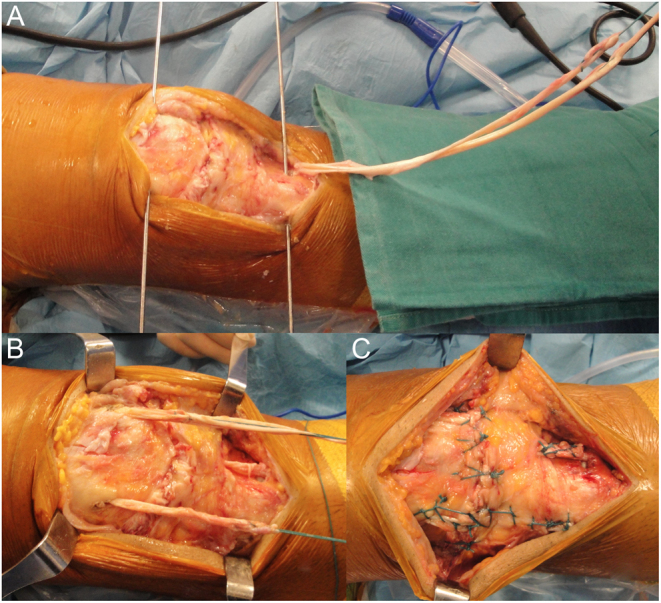
Augmentation of primary repair of the patellar tendon with hamstring tendons; (A) Both hamstrings have been harvested with their distal insertions intact, guide wires are placed in the patella and tibial tuberosity for bone tunnels; (B) Hamstring tendons are placed through these tunnels in a rectangular fashion and sutured on to each other; (C) Final appearance of the construct.
Chronic or neglected patellar tendon tears need to be augmented with auto or allograft tendons. The outcomes of chronic reconstructions are inferior to acute repairs due to muscle atrophy, scarring and chronic proximal migration of the patella. The most commonly used tendons are the hamstrings with their tibial attachments left intact (23) or as free grafts (12, 24). The tendon grafts are placed in transpatellar and trans-tibial tunnels in an X or rectangular configuration, tensioned and fixed with interference screws or non-absorbable sutures. The patellar tunnel for the tendon graft may be vertical or transverse depending on the technique employed. The use of reversed quadriceps tendon grafts with bone blocks (25) and contra-lateral central third bone-patellar tendon grafts (26) have also been reported.
Allografts are indicated in patients with chronic patellar tendon defects with poor native tissue, significant retraction or failed primary repairs. Fresh-frozen Achilles tendon with bone block or bone-patellar tendon-bone grafts are the most frequently used allografts. The outcomes of these patients are satisfactory with good range of motion and return to activities of daily living; however, residual extensor lag may be present up to a third of the cases (12) and return to high-impact activities may not be possible (27).
Partial or complete extensor mechanism allografts comprising the quadriceps tendon, patella, patellar tendon and tibial tuberosity may be utilized for chronic disruptions with poor tissue quality. Better outcomes have been reported in patients with primary chronic patellar tendon disruptions compared to patients having a total knee arthroplasty in place (28).
Return to sports
High rates of return to sports (RTS) 6–12 months following patellar tendon repair have been reported. A recent systematic review of 33 studies including 757 patients found an overall rate of return to play of 88.9%, with 80.8% returning to the same level of sports (2). Age over 40 years and BMI > 25 have been associated with lower rates of RTS (29).
Quadriceps tendon tears
Epidemiology
Quadriceps tendon tears are usually seen in older patients compared to patellar tendon tears. Garner et al. found the median age of patients with quadriceps tendon tears to be 61, compared to 39.5 for patellar tendon ruptures (30). Reported risk factors for quadriceps tendon tears are obesity, diabetes mellitus, rheumatoid arthritis, chronic tendinopathy with bone spurs (31), amyloidosis and systemic or local corticosteroids (32). A third of the cases have been reported to have systemic co-morbidities associated with tendinopathy (30). The prevalence of systemic risk factors is higher in bilateral quadriceps tendon ruptures with almost two-thirds of these cases having a predisposing factor (33). Otherwise healthy patients may also experience quadriceps tendon tears due to forceful eccentric contraction of the muscle. The use of statins is associated with an increased risk of quadriceps tendon rupture, probably by the inhibition of matrix metalloproteinases interfering with tendon remodeling (34).
Clinical presentation
Acute pain with a tearing sensation after eccentric quadriceps contraction is typical for acute tears. The hallmark of complete distal quadriceps tendon tears is loss of active extension strength. Some patients may still be able to perform a weak extension against gravity if the medial and lateral retinaculae are intact. A palpable defect may be present on the superior pole of the patella.
Imaging
Plain radiographs may depict avulsion of small fragments from the patella (Fig. 4). Spurs and calcifications in the bone-tendon junction indicating antecedent tendinopathy may be observed in two-thirds of these patients (35). Patella infera may not always be seen, only 39% of the cases had a Caton–Deschamps index <0.8 in one series (32).
Figure 4.
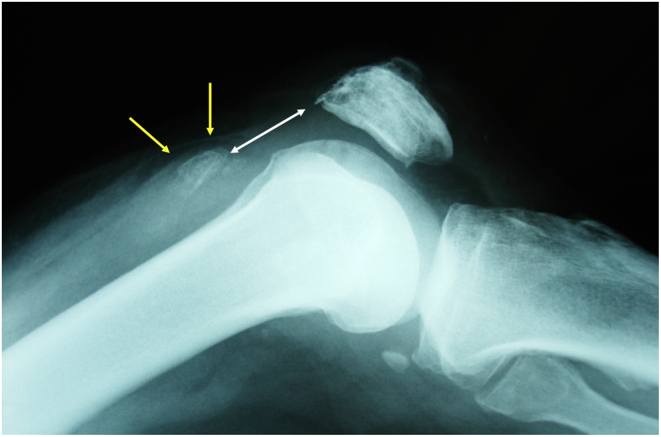
Lateral X-ray of a patient with quadriceps tendon avulsion from the proximal pole of the patella. Arrows indicate the boney fragment.
Ultrasound (US) diagnosis of quadriceps tears yields over 95% rates of sensitivity and specificity in expert hands (36). However, the accuracy of US is operator-dependent and may be lower in morbidly obese or heavily muscular patients.
MRI is the gold standard in the diagnosis of quadriceps tendon injuries. Discontinuity of the tendon fibers and gap formation at the proximal pole of the patella may be observed (Fig. 5). Signs of previous enthesopathy were found in 66% of the cases in a recent series (37).
Figure 5.
MRI of a patient with mid-tendon injury. Discontinuity of the tendon fibers and undulation of the tendon are seen.
Treatment
Repair in the first 3 weeks following trauma is the treatment of choice for acute tears of the quadriceps tendon. Delay in the diagnosis and treatment leads to inferior functional outcomes and may necessitate augmentation/reconstruction procedures. Both transosseous sutures and suture anchors have been used for primary repair.
Two high-strength sutures are passed through the quadriceps tendon in a continuous Krackow type locking stitch for transosseous repair. These are passed through three longitudinal transpatellar tunnels and tied over the inferior pole of the patella under appropriate tension. Anchor repair of the quadriceps tendon requires at least three anchors placed in the superior pole of the patella, taking care to avoid damaging the articular surface. The suture limbs are weaved through the tendon and tied under appropriate tension. Biomechanical comparisons of the two techniques report conflicting results, with some studies finding stronger fixation with transpatellar tunnels (38), while others reporting superior fixation strength with suture anchors (39, 40). New generation strengthened tapes are superior to sutures (39). The proposed advantages of anchors are a smaller incision, less dissection and avoidance of fracture risk; however, there are increased costs related to the use of these implants. Nevertheless, both transosseous and suture anchor repairs report satisfactory outcomes in non-arthroplasty patients with high rates of return to activities of daily living and work (32, 41) with no major difference in clinical outcomes (42) or gait analysis parameters (43). A recent systematic review of eight clinical studies has shown similar functional outcomes and re-rupture rates with transosseous sutures and suture anchors (44).
The need for augmentation of the repair with synthetics or autogenous tendon grafts for acute repairs is debatable, since good outcomes have been reported in patients without augmentation (45). Augmentation may offer advantages in early mobilization and protection of the repair site in patients with poor tendon quality. This author prefers to augment the repair with a non-rigid tape material passed around the patella and tied onto itself in obese patients, previous tendinopathy and predisposing factors (46). The safe range of motion (i.e. no tension and gapping at the repair site) is tested intra-operatively, determining the limits of knee motion in the early postoperative period.
Cast immobilization up to 10 weeks has been used in the postoperative period in the past. This has been associated with muscle atrophy, stiffness and delay in return to work and sports. At the other end of the spectrum, some surgeons advocate unrestricted, brace-free weight-bearing and full range of motion immediately after surgery (47). Most programs are between the two philosophies with protected weight-bearing and incremental passive range of motion for 6 weeks. The rehabilitation protocol used by the author employs an adjustable knee brace with partial weight-bearing for 6 weeks. Passive knee flexion is started within the safe limits of motion determined intra-operatively. The goal is to achieve 90° of flexion at 6 weeks and full flexion at 8 weeks. Active extension is delayed for 4–6 weeks depending on the strength of the repair and quality of tissues. Active and resistive exercises can be started after 6–8 weeks complemented with stationary bike and pool exercises. Running is permitted at 4 months along with sports-specific exercises. Return to sports is around 5–6 months.
Chronic tendon tears with retraction of the tendon need a variety of techniques to reconstruct the continuity of the extensor mechanism. Local turndown flaps created from the quadriceps tendon (Codivilla technique) and Scuderi type V-Y plasty to lengthen the tendon may be needed (48). Autogenous hamstring tendon grafts can be utilized in patients with poor tendon quality (Fig. 6). The postoperative rehabilitation program is slower compared to primary repairs. Synthetic mesh augmentation may be used in failed primary repairs of the quadriceps tendon, especially in patients with systemic comorbidities and poor tendon quality (49).
Figure 6.
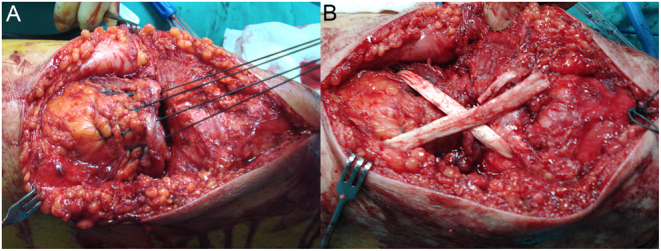
Augmentation of transosseous repair of a chronic quadriceps tendon injury with (A) placement of three rows of Krackow type sutures; (B) augmentation of the repair with a crossed hamstring tendon graft passing through the patella and proximal tendon.
A systematic review of 319 quadriceps repairs found that the worst results were noted in delayed repairs (50). Reported complications included heterotopic ossification (6.9%), deep venous thrombosis or pulmonary embolism (2.5%), superficial infection (1.2%) and deep infection (1.1%). The overall rate of re-rupture was 2% (50).
Return to sports
In a meta-analysis of 18 studies including 378 patients, Haskel et al. have found an overall rate of return to play of 89.8%, with 70 % of the athletes returning to the same level of play (2). Return to work was possible in 95.9% of the cases. This study reported that mean time to return to play was 4.6 months with a low re-rupture rate (2.6%).
Extensor mechanism disruptions in knee arthroplasty
The incidence of extensor mechanism disruptions after TKA has been reported to be in the range of 0.17–2.5% (51). This disruption may be due to patellar or quadriceps tendon rupture, patellar fracture or dehiscence of the repaired arthrotomy site. The patients are older and many have medical co-morbidities. The quality of the soft tissues may be attenuated due to infection, multiple surgical procedures, osteoporosis and loss of patellar bone stock. The vascularity of the extensor mechanism may be altered due to the arthrotomy, fat pad resection, lateral release or tibial tubercle osteotomy (52). Extensive dissection, over-resection of the patella, joint line elevation causing impingement of the tendon and multiple revisions may worsen this situation (52, 53). Manipulation under anesthesia for stiff knees is another risk factor, especially if performed later than 3 months (53). The outcomes of surgical repair of extensor mechanism in patients with TKA are worse than native tendon injuries. The risks of soft-tissue complications, infection and residual extensor lag are higher.
Patellar tendon disruptions in knee arthroplasty
Intra-operative injuries
Intra-operative peel-off of the patellar tendon from the patella or tibial tubercule may occur in patients with severe osteoporosis or stiff knees. Previously operated knees with scarring around the tendon or loss of proximal tibial metaphyseal bone stock have an increased risk for patellar tendon avulsion. When patellar tendon disruption is diagnosed intra-operatively, primary repair with suture anchors and transosseous sutures should be performed before cementing the final implants. This repair may be augmented with autogenous hamstring tendons and wire/cable/strengthened tape constructs (54). There are no clear guidelines on the use of postoperative braces, limitation of motion and weight-bearing after intra-operative repair, and the decision should be individualized according to the quality of soft tissues and stability of repair.
Post-operative patellar tendon disruptions
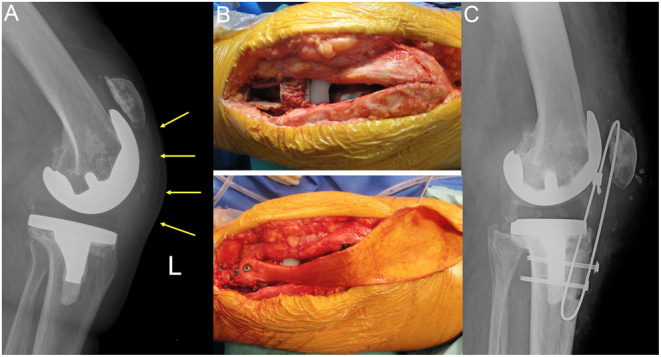
Patellar tendon injury after TKA usually occurs with falls on a hyper flexed knee or eccentric contraction of the quadriceps muscle. The risk factors associated with native patellar tendon injuries are also associated with an increased risk of tendon ruptures in patients with TKA (52). Dislocation of the polyethylene insert in either fixed or mobile-bearing implants may damage the patellar tendon (Fig. 7). Failure of fixation of tibial tubercle osteotomy during primary or revision TKA is another cause of active extension loss.
Figure 7.
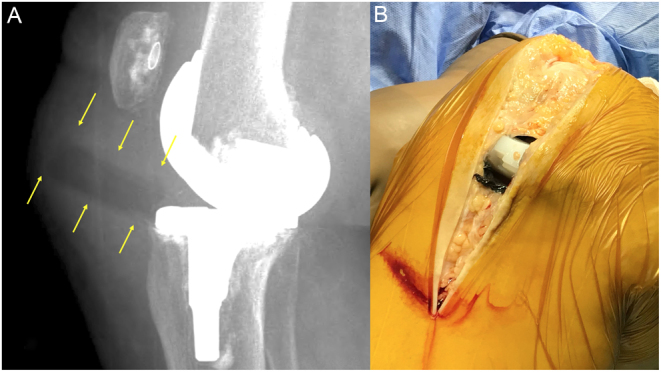
Dislocation of the tibial bearing and damage to the patellar tendon; (A) Arrows depict the dislocated insert in the lateral X-ray. (B) The defect in the patellar tendon caused by the insert and metallosis is discernible after surgical exposure.
Clinical presentation
Patients with patellar tendon disruptions typically present with an inability to extend the knee, pain and instability during walking or descending stairs. An infra-patellar defect may be palpable in chronic cases and a high riding patella on the injured side can be observed. Proximal migration of the patella is identified in lateral X-rays (Fig. 8), and avulsion fractures from the tibial tuberosity are uncommon. Ultrasound diagnosis may be helpful if clinical examination is inconclusive. MRI of the knee with metal artifact reduction sequences may also be utilized.
Figure 8.
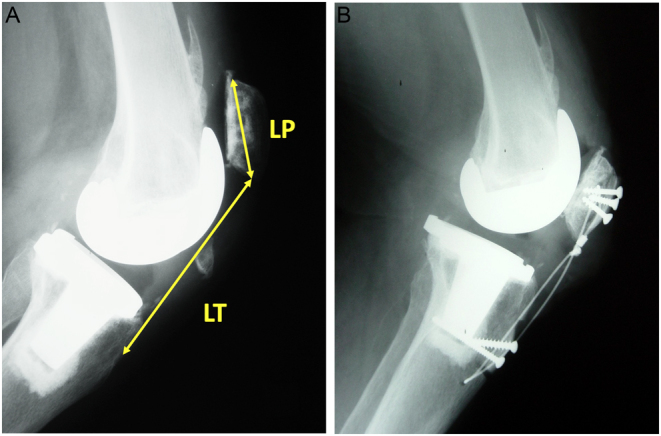
Lateral X-rays of a patient with a chronic patellar tendon rupture after TKA. (A) Pre-operative view demonstrates patella alta with an Insall Salvati index (LT/LP) of 1.8 and proximal migration of the patella. (B) Patellar height is restored after reconstruction with bone-patellar tendon-bone allograft fixed with screws to the patella and tibial tuberosity.
Treatment options
Conservative treatment with bracing is indicated only for low demand/high-risk patients who are not candidates for surgery. Primary repair with suture anchors is associated with a high risk of failure (55) and some form of biologic augmentation is advocated. Hamstring tendons are the most common grafts. Achilles tendon with a bone block or bone-patellar tendon-bone allografts may be used in patients with poor tissue quality and multiply operated knees. Synthetic meshes are proposed as a cheaper alternative to allografts with the added benefit of avoiding the risk of disease transmission. Whole extensor mechanism allografts should be reserved for patients with patellar bone loss or when the proximally migrated patella cannot be brought distally within 4 cm of the joint line.
The outcome of surgery for patellar tendon disruptions is variable and dependent on the quality of the tissues and type of surgery. Patient with good tissue quality and augmented repair can expect a good outcome with minimal extensor lag and adequate strength. Failure, extensor lag and increased rates of infection are seen more commonly in patients needing extensor mechanism allografts, soft tissue flaps and synthetic mesh augmentation.
Primary repair and hamstring tendon augmentation
Primary repair and hamstring tendon augmentation for patellar tendon ruptures after TKA are indicated in younger patients with adequate remaining tendon quality. Either the semitendinosus alone or both hamstrings may be used to augment the repair. The distal insertion is left intact and the tendon is passed through a transverse patellar tunnel sutured onto itself in patients with good patellar bone stock or unresurfaced patella. The grafts may be passed around the superior pole of the patella, weaving through the quadriceps tendon in patients with poor bone stock or patellar resurfacing. Spoliti et al. have reported good functional outcomes with a mean extensor lag of 5° in nine patients with hamstring graft augmentation (56). In a meta-analysis investigating nine different techniques, Gilmore et al. found primary repair augmented with autografts to have the best outcomes (57).
Fresh-frozen allografts
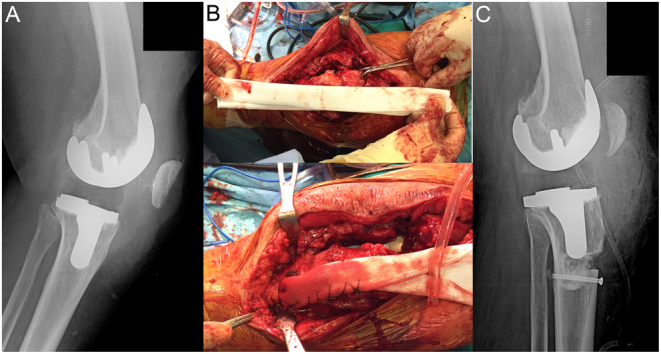
Achilles tendon allograft with bone block has been widely used to reconstruct the patellar tendon defects in patients with TKA. A rectangular boney trough is created at the level of tibial tuberosity, and the allograft bone block is securely fixed with cerclage wires or screws. The free end of the Achilles tendon is secured to the patella and the quadriceps tendon under tension in full extension (Fig. 9). A variety of techniques passing through, over or around the patella have been described (52, 58, 59). The knee is placed in an immobilizer in full extension for 6 weeks, followed by gradual increase in knee range of motion and strengthening. Onlay techniques with simple suturing to the quadriceps tendon carry a risk of stretching out and causing extensor lag. Efforts should be made to pass at least one limb of the allograft through or around the patella.
Figure 9.
Reconstruction of chronic patellar tendon rupture after TKA with Achilles allograft; (A) Pre operative lateral X-ray depicts proximal migration of the patella. (B) Achilles tendon allograft is placed in the bone trough created on the tibial tubercule and fixed with two screws. (C) Post-operative lateral X-ray showing normal patellar height, a cerclage wire was added for protection.
Recent studies using fresh-frozen Achilles tendon allografts of patellar tendon ruptures have reported favorable outcomes. Wise et al. reported ten patients with 45 months follow-up (58). The average extensor lag was 9.6° with a final flexion of 105°. Llombart-Blanco et al. reported seven patients with 25 months follow-up (59). KSS knee scores improved from 26 to 82, mean extensor lag was 5°, and final knee ROM was 95°. Lamberti et al. compared three techniques for the reconstruction of chronic patellar tendon disruption in 21 patients; namely Achilles tendon allograft, primary repair with autogenous hamstring augmentation and total extensor mechanism allografts (60). Mean extensor lag decreased from 50° to 3°. The best Knee Society Knee Scores were seen in patients with Achilles allograft reconstruction.
Fresh-frozen bone-patellar tendon-bone grafts may also be used for reconstruction of patellar tendon defects (61). The graft is placed in two grooves created in the patella and the tibial tuberosity and fixed with screws or cerclage wiring. Bone to bone healing is advantageous to prevent proximal migration of the patella, and the graft is less bulky compared to an Achilles allograft (Fig. 8).
Synthetic meshes
Synthetic polypropylene meshes have been proposed as an alternative to extensor mechanism allografts. These are readily available, relatively inexpensive and do not carry the risk of disease transmission. The mesh is fixed in a bone trough distal to the tibial tubercule with cement and screws if the implant is not to be revised (Fig. 10). For patients requiring a revision of the tibial baseplate, the mesh can be cemented under the revision implant. The mesh is then incorporated into the remaining viable host tissues and fixed to the quadriceps mechanism under tension. The knee is immobilized in a brace for 6–8 weeks in extension followed by gradual increase of flexion (62). Initially described by Browne and Hanssen, the technique has been used in patients with multiple operations, failed allografts, poor quality soft tissues and osteopenic bone (63). Abdel reported on the 4-year outcomes of 77 patients with polypropylene (Marlex) mesh reconstruction in patients with TKA (64). At the time of latest follow-up, 84% of the mesh reconstructions were still functioning with satisfactory clinical outcomes, with a mean 9° of extensor lag (64). The infection rate was 8%, lower than that reported for extensor mechanism allografts.
Figure 10.
Synthetic mesh reconstruction of the extensor mechanism in a patient with a failed primary repair of the quadriceps tendon. (A) Pre-operative X-ray depicting an everted patella; (B) placement of the mesh; (C) post-operative lateral X-ray showing the mesh placed in a bone trough distal to the tibial tuberosity fixed with cement and a screw.
Whole extensor mechanism allografts
These allografts comprise the tibial tuberosity bone block, patellar tendon, patella and the quadriceps tendon and are indicated for salvage cases with severe patellar bone loss and proximally retracted, immobile quadriceps/patellar tendon defects. The tibial tuberosity part of the graft is placed in a groove on the native tibia and the vastus medialis and lateralis are secured to the quadriceps tendon allograft in full extension under strong tension. Every effort should be made to preserve remaining host tissues and incorporate these into the repair. The allograft patella should be left unresurfaced.
Two recent systematic reviews comparing whole extensor mechanism allografts and synthetic meshes have found similar outcomes and complication rates. Deren et al.,analyzed 30 studies and found a success rate of 73% for allografts and 78% for synthetic mesh grafts (65). No significant difference in knee scores, infection and revision rates were found. In a meta-analysis of 14 studies involving 304 patients, success rates were 76% for allografts vs 74% mesh grafts, and no difference could be found in knee scores, range of motion, extensor lag and complications (54). Given the high cost and risk of disease transmission of allografts, synthetic meshes seem to provide the same outcomes with less expense.
Quadriceps tendon disruptions in knee arthroplasty
The typical presentation of the patient with quadriceps injury is pain and weakness in extension after a fall or eccentric muscle contraction (Fig. 11). Quadriceps peel-off from the patella may occur gradually in elderly patients with osteoporosis following knee replacement. Acute symptoms may be absent and these patients present with increasing loss of muscle strength and feelings of instability. The same is true for dehiscence of the arthrotomy repair following surgery, the patient may not remember an acute traumatic episode but describes pain, gradual loss of extension strength and rarely patellar instability.
Figure 11.
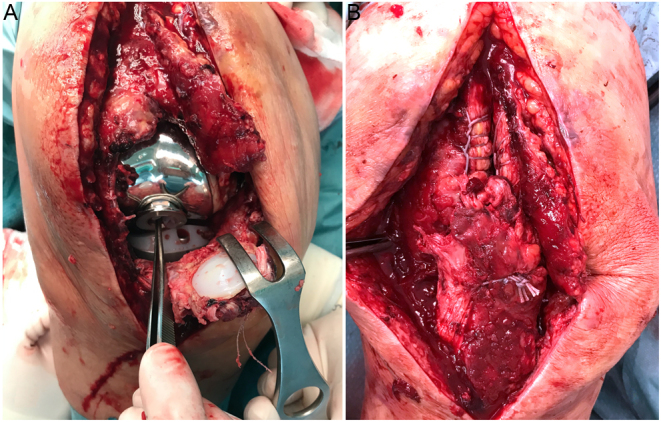
Complete rupture of the quadriceps tendon and traumatic dislocation of a hinge type total knee arthroplasty. (A) Intra-operative view depicting the extent of injury; (B) View after primary repair of the extensor mechanism.
The treatment of quadriceps tendon repairs after TKA may be challenging due to the older age, multiple operations, poor tendon and bone quality and the presence of patellar resurfacing. Transpatellar drill holes may not be possible and suture anchors can be used for fixation. Primary repair alone results in a significantly high rate of failure (66). The repair should be augmented either with flexible tape material and/or autogenous tissue in acute cases (67). While acceptable knee function can be achieved with surgery, some degree of extensor lag and loss of terminal flexion may be observed. In a series of 22 patients treated with primary repair and Scuderi type partial thickness V-Y quadriceps turndown augmentation, Miralles–Munoz et al. found a residual extensor lag of 7° and 8° loss of terminal flexion (68). Better outcomes were reported with the V-Y turndown technique by Shi et al.; who found 120° knee flexion and residual extensor lag in only 4° of the 24 repairs, with a mean KSS knee score of 88 (69). They proposed a preoperative gap of >6 cm as a limit to V-Y turndown and advocated other methods such as mesh or allografts in these extreme cases.
Chronic tears with retraction of the tendon require complex reconstructions. Treatment options are V-Y plasty lengthening and repair, augmentation with autogenous or allograft tendons, synthetic mesh repair and extensor mechanism allografts. The decision is based on the mobility and quality of the remaining tendon, availability of allografts, previous surgeries and type of implant.
Dehiscence of the arthrotomy
Dehiscence of the arthrotomy repair in the weeks following TKA is usually caused by a fall. The diagnosis may be difficult since active extension is weak but still possible. The chief complaints are pain, weakness and instability; frank patellar dislocation is rare. A longitudinal defect may be palpable in patients with dehiscence of the VMO from the quadriceps tendon. This defect becomes more pronounced with active quadriceps contraction. X-rays demonstrate no change in patellar height, tangential views may show a centered patella in the trochlear sulcus if no malrotation of the components is present. Surgical repair after verification of correct rotation of components is the treatment of choice. No augmentation is needed in acute repairs (Fig. 12).
Figure 12.
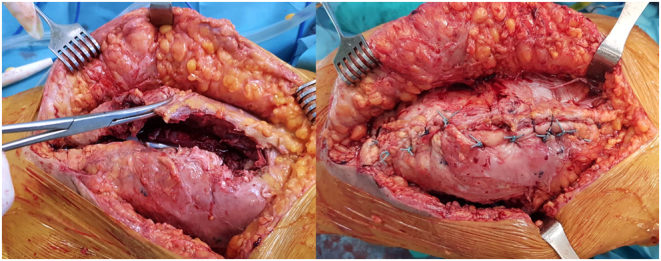
Dehiscence of the arthrotomy repair after a fall, primary repair resulted in satisfactory outcomes.
Conclusions
Extensor mechanism disruptions of the knee require early surgical repair. Primary repair should be augmented with autograft or allograft in patients with poor tendon quality and/or knee arthroplasty in place. The outcomes of early repairs are superior to late interventions which require complex reconstructions to restore the continuity of the extensor mechanism. Synthetic meshes and whole extensor mechanism allografts are salvage procedures with acceptable outcomes.
ICMJE Conflict of Interest Statement
R N T declares receiving honoraria for lectures from Menarini pharma and consultancy fees from Stryker and Smith & Nephew. B V declares consultancy fees from Smith & Nephew and is a shareholder in Lento Medical Innovation. A K declares receiving honoraria for lectures from Menarini pharma and consultancy fees from Stryker. The other authors have nothing to disclose.
Funding Statement
This work did not receive any specific grant from any funding agency in the public, commercial or not-for-profit sector.
Author contribution statement
R T designed the structure and flow of the manuscript, wrote the article, provided and edited the images and reviewed the final version; E T performed the literature search and contributed to the writing of the paper; E G B contributed to the figures and critically reviewed the article, B V critically reviewed the article, A K contributed to the writing of the article. All authors read and approved the final version.
References
- 1.Bui CN, Learned JR, Scolaro JA. Treatment of patellar fractures and injuries to the extensor mechanism of the knee: a critical analysis review. JBJS Reviews 20186 e1. ( 10.2106/JBJS.RVW.17.00172) [DOI] [PubMed] [Google Scholar]
- 2.Haskel JD, Fried JW, Hurley ET, Mojica ES, Alaia MJ, Strauss EJ, Campbell KA. High rates of return to play and work follow knee extensor tendon ruptures but low rate of return to pre-injury level of play. Knee Surgery, Sports Traumatology, Arthroscopy 2021292695–2700. ( 10.1007/s00167-021-06537-4) [DOI] [PubMed] [Google Scholar]
- 3.Rosteius T, Jettkant B, Brinkemper A, Rausch V, Lotzien S, Geßmann J, Schildhauer TA, Königshausen M. Long-term follow up of extensor tendon ruptures of the knee using electromyography and three-dimensional gait analysis. Knee 202129251–261. ( 10.1016/j.knee.2021.02.011) [DOI] [PubMed] [Google Scholar]
- 4.Clayton RA, Court-Brown CM. The epidemiology of musculoskeletal tendinous and ligamentous injuries. Injury 2008391338–1344. ( 10.1016/j.injury.2008.06.021) [DOI] [PubMed] [Google Scholar]
- 5.Chen SK, Lu CC, Chou PH, Guo LY, Wu WL. Patellar tendon ruptures in weight lifters after local steroid injections. Archives of Orthopaedic and Trauma Surgery 2009129369–372. ( 10.1007/s00402-008-0655-1) [DOI] [PubMed] [Google Scholar]
- 6.Monroy A, Urruela A, Egol KA, Tejwani NC. Bilateral disruption of soft tissue extensor mechanism of knee: functional outcome and comparison to unilateral injuries. HSS Journal 2013912–16. ( 10.1007/s11420-012-9314-8) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Boublik M, Schlegel T, Koonce R, Genuario J, Lind C, Hamming D. Patellar tendon ruptures in National Football League players. American Journal of Sports Medicine 2011392436–2440. ( 10.1177/0363546511417083) [DOI] [PubMed] [Google Scholar]
- 8.Daneman N, Lu H, Redelmeier DA. Fluoroquinolones and collagen associated severe adverse events: a longitudinal cohort study. BMJ Open 20155 e010077. ( 10.1136/bmjopen-2015-010077) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Baik S, Lau J, Huser V, McDonald CJ. Association between tendon ruptures and use of fluoroquinolone, and other oral antibiotics: a 10-year retrospective study of 1 million US senior medicare beneficiaries. BMJ Open 202010 e034844. ( 10.1136/bmjopen-2019-034844) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Swamy GN, Nanjayan SK, Yallappa S, Bishnoi A, Pickering SA. Is ultrasound diagnosis reliable in acute extensor tendon injuries of the knee? Acta Orthopaedica Belgica 201278764–770. [PubMed] [Google Scholar]
- 11.Schliemann B, Grüneweller N, Yao D, Kösters C, Lenschow S, Roßlenbroich SB, Raschke MJ, Weimann A. Biomechanical evaluation of different surgical techniques for treating patellar tendon ruptures. International Orthopaedics 2016401717–1723. ( 10.1007/s00264-015-3003-4) [DOI] [PubMed] [Google Scholar]
- 12.Golman M, Wright ML, Wong TT, Lynch TS, Ahmad CS, Thomopoulos S, Popkin CA. Rethinking patellar tendinopathy and partial patellar tendon tears: a novel classification system. American Journal of Sports Medicine 202048359–369. ( 10.1177/0363546519894333) [DOI] [PubMed] [Google Scholar]
- 13.Carlson Strother CR, LaPrade MD, Keyt LK, Wilbur RR, Krych AJ, Stuart MJ. A strategy for repair, augmentation, and reconstruction of knee extensor mechanism disruption: a retrospective review. Orthopaedic Journal of Sports Medicine 2021923259671211046625. ( 10.1177/23259671211046625) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sherman SL, Black B, Mooberry MA, Freeman KL, Gulbrandsen TR, Milles JL, Evans L, Flood D, Pfeiffer F. Biomechanical evaluation of suture anchor versus transosseous tunnel patellar tendon repair techniques. Journal of Knee Surgery 201932825–832. ( 10.1055/s-0038-1669790) [DOI] [PubMed] [Google Scholar]
- 15.Ettinger M, Dratzidis A, Hurschler C, Brand S, Calliess T, Krettek C, Jagodzinski M, Petri M. Biomechanical properties of suture anchor repair compared with transosseous sutures in patellar tendon ruptures: a cadaveric study. American Journal of Sports Medicine 2013412540–2544. ( 10.1177/0363546513500633) [DOI] [PubMed] [Google Scholar]
- 16.Ravalin RV, Mazzocca AD, Grady-Benson JC, Nissen CW, Adams DJ. Biomechanical comparison of patellar tendon repairs in a cadaver model: an evaluation of gap formation at the repair site with cyclic loading. American Journal of Sports Medicine 200230469–473. ( 10.1177/03635465020300040301) [DOI] [PubMed] [Google Scholar]
- 17.Hasegawa M, Tone S, Naito Y, Sudo A. Reconstruction of patellar tendon rupture after total knee arthroplasty using polyethylene cable. Knee 20212963–67. ( 10.1016/j.knee.2021.01.008) [DOI] [PubMed] [Google Scholar]
- 18.Otsubo H, Kamiya T, Suzuki T, Kuroda M, Ikeda Y, Matsumura T, Yamashita T. Repair of acute patellar tendon rupture augmented with strong sutures. Journal of Knee Surgery 201730336–340. ( 10.1055/s-0036-1586725) [DOI] [PubMed] [Google Scholar]
- 19.Harrell RM, Tong J, Weinhold PS, Dahners LE. Comparison of the mechanical properties of different tension band materials and suture techniques. Journal of Orthopaedic Trauma 200317119–122. ( 10.1097/00005131-200302000-00007) [DOI] [PubMed] [Google Scholar]
- 20.Kasten P, Schewe B, Maurer F, Gösling T, Krettek C, Weise K. Rupture of the patellar tendon: a review of 68 cases and a retrospective study of 29 ruptures comparing two methods of augmentation. Archives of Orthopaedic and Trauma Surgery 2001121578–582. ( 10.1007/s004020100298) [DOI] [PubMed] [Google Scholar]
- 21.Marder RA, Timmerman LA. Primary repair of patellar tendon rupture without augmentation. American Journal of Sports Medicine 199927304–307. ( 10.1177/03635465990270030601) [DOI] [PubMed] [Google Scholar]
- 22.El-Desouky II, Mohamed MM, Al Assassi M. Primary repair of ruptured patellar tendon augmented by semitendinosus. Journal of Knee Surgery 201427207–213. ( 10.1055/s-0033-1360655) [DOI] [PubMed] [Google Scholar]
- 23.Maffulli N, Del Buono A, Loppini M, Denaro V. Ipsilateral hamstring tendon graft reconstruction for chronic patellar tendon ruptures: average 5.8-year follow-up. Journal of Bone and Joint Surgery: American Volume 201395e1231–e1236. (https:/doi/10.2106/JBJS.L.01462) [DOI] [PubMed] [Google Scholar]
- 24.Abdou YE.Reconstruction of a chronic patellar tendon rupture with semitendinosus autograft. Archives of Orthopaedic and Trauma Surgery 20141341717–1721. ( 10.1007/s00402-014-2080-y) [DOI] [PubMed] [Google Scholar]
- 25.Gomes JL, de Oliveira Alves JA, Zimmermann Jr JM. Reconstruction of neglected patellar tendon ruptures using the quadriceps graft. Orthopedics 201437527–529. ( 10.3928/01477447-20140728-04) [DOI] [PubMed] [Google Scholar]
- 26.Temponi EF, Camelo N, Tuteja S, Thaunat M, Daggett M, Fayard JM, de Carvalho Júnior LH, Sonnery-Cottet B. Reconstruction of chronic patellar tendon rupture with contralateral bone-tendon-bone autograft. Knee Surgery, Sports Traumatology, Arthroscopy 2017252468–2473. ( 10.1007/s00167-015-3951-7) [DOI] [PubMed] [Google Scholar]
- 27.Karas V, Sherman S, Hussey K, Baker C, Bach Jr B, Cole B, Bush-Joseph C. Allograft reconstruction for extensor mechanism injuries. Journal of Knee Surgery 201427489–496. ( 10.1055/s-0034-1370899) [DOI] [PubMed] [Google Scholar]
- 28.Fiquet C, White N, Gaillard R, Servien E, Neyret P, Lustig S. Partial extensor mechanism allograft reconstruction for chronic patellar tendon disruption shows superior outcomes in native knees when compared to same technique following total arthroplasty. International Orthopaedics 2018422591–2599. ( 10.1007/s00264-018-4119-0) [DOI] [PubMed] [Google Scholar]
- 29.Beranger JS, Kajetanek C, Bayoud W, Pascal-Mousselard H, Khiami F. Return to sport after early surgical repair of acute patellar tendon ruptures. Orthopaedics and Traumatology, Surgery and Research 2020106503–507. ( 10.1016/j.otsr.2020.01.010) [DOI] [PubMed] [Google Scholar]
- 30.Garner MR, Gausden E, Berkes MB, Nguyen JT, Lorich DG. Extensor mechanism injuries of the knee: demographic characteristics and comorbidities from a review of 726 patient records. Journal of Bone and Joint Surgery: American Volume 2015971592–1596. ( 10.2106/JBJS.O.00113) [DOI] [PubMed] [Google Scholar]
- 31.Pagliari M, Menna CR, Migliorini A, Molinari M. Atraumatic acute bilateral quadriceps tendon rupture in a patient with bilateral patella spurs. A case report and review of literature. Acta Bio-Medica 201890203–208. (https:/doi/10.23750/abm.v90i1-S.8008) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Boudissa M, Roudet A, Rubens-Duval B, Chaussard C, Saragaglia D. Acute quadriceps tendon ruptures: a series of 50 knees with an average follow-up of more than 6 years. Orthopaedics and Traumatology, Surgery and Research 2014100213–216. ( 10.1016/j.otsr.2013.09.014) [DOI] [PubMed] [Google Scholar]
- 33.Neubauer T, Wagner M, Potschka T, Riedl M. Bilateral, simultaneous rupture of the quadriceps tendon: a diagnostic pitfall? Report of three cases and meta-analysis of the literature. Knee Surgery, Sports Traumatology, Arthroscopy 20071543–53. ( 10.1007/s00167-006-0133-7) [DOI] [PubMed] [Google Scholar]
- 34.Deren ME, Klinge SA, Mukand NH, Mukand JA. Tendinopathy and tendon rupture associated with statins. JBJS Reviews 20164 e4. ( 10.2106/JBJS.RVW.15.00072) [DOI] [PubMed] [Google Scholar]
- 35.Ellanti P, Moriarity A, Wainberg N, Fhoghlu CN, McCarthy T. Association between patella spurs and quadriceps tendon ruptures. Muscles, Ligaments and Tendons Journal 2015588–91. [PMC free article] [PubMed] [Google Scholar]
- 36.Foley R, Fessell D, Yablon C, Nadig J, Brandon C, Jacobson J. Sonography of traumatic quadriceps tendon tears with surgical correlation. Journal of Ultrasound in Medicine 201534805–810. ( 10.7863/ultra.34.5.805) [DOI] [PubMed] [Google Scholar]
- 37.Falkowski AL, Jacobson JA, Hirschmann MT, Kalia V. MR imaging of the quadriceps femoris tendon: distal tear characterization and clinical significance of rupture types. European Radiology 2021317674–7683. ( 10.1007/s00330-021-07912-y) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Hart ND, Wallace MK, Scovell JF, Krupp RJ, Cook C, Wyland DJ. Quadriceps tendon rupture: a biomechanical comparison of transosseous equivalent double-row suture anchor versus transosseous tunnel repair. Journal of Knee Surgery 201225335–339. ( 10.1055/s-0031-1299656) [DOI] [PubMed] [Google Scholar]
- 39.Kindya MC, Konicek J, Rizzi A, Komatsu DE, Paci JM. Knotless suture anchor with suture tape quadriceps tendon repair is biomechanically superior to transosseous and traditional suture anchor-based repairs in a cadaveric model. Arthroscopy 201733190–198. ( 10.1016/j.arthro.2016.06.027) [DOI] [PubMed] [Google Scholar]
- 40.Petri M, Dratzidis A, Brand S, Calliess T, Hurschler C, Krettek C, Jagodzinski M, Ettinger M. Suture anchor repair yields better biomechanical properties than transosseous sutures in ruptured quadriceps tendons. Knee Surgery, Sports Traumatology, Arthroscopy 2015231039–1045. ( 10.1007/s00167-014-2854-3) [DOI] [PubMed] [Google Scholar]
- 41.Brossard P, Le Roux G, Vasse B. & Orthopedics, Traumatology Society of Western France (SOO). Acute quadriceps tendon rupture repaired by suture anchors: outcomes at 7 years’ follow-up in 25 cases. Orthopaedics and Traumatology, Surgery and Research 2017103597–601. ( 10.1016/j.otsr.2017.02.013) [DOI] [PubMed] [Google Scholar]
- 42.Plesser S, Keilani M, Vekszler G, Hasenoehrl T, Palma S, Reschl M, Crevenna R, Hajdu S, Widhalm HK. Clinical outcomes after treatment of quadriceps tendon ruptures show equal results independent of suture anchor or transosseus repair technique used – a pilot study. PLoS ONE 201813 e0194376. ( 10.1371/journal.pone.0194376) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Hasenoehrl T, Palma S, Keilani M, Reschl M, Vekszler G, Ambrozy C, Plesser S, Hajdu S, Crevenna R, Widhalm HK. Gait analysis and body composition after treatment of quadriceps tendon ruptures showed equal results independent of suture anchor or transosseus repair technique used: a pilot study. Disability and Rehabilitation 2020423833–3837. ( 10.1080/09638288.2019.1611951) [DOI] [PubMed] [Google Scholar]
- 44.Mehta AV, Wilson C, King TS, Gallo RA. Outcomes following quadriceps tendon repair using transosseous tunnels versus suture anchors: a systematic review. Injury 202152339–344. ( 10.1016/j.injury.2020.10.020) [DOI] [PubMed] [Google Scholar]
- 45.Mille F, Adam A, Aubry S, Leclerc G, Ghislandi X, Sergent P, Garbuio P. Prospective multicentre study of the clinical and functional outcomes following quadriceps tendon repair with suture anchors. European Journal of Orthopaedic Surgery and Traumatology 20162685–92. ( 10.1007/s00590-015-1710-6) [DOI] [PubMed] [Google Scholar]
- 46.Akgun RA, Tandogan RN, Sahin O. The outcome of acute quadriceps tendon rupture managed with primary repair and mersilene tape augmentation. Turkiye Klinikleri Journal of Medical Sciences 200929438–444. [Google Scholar]
- 47.West JL, Keene JS, Kaplan LD. Early motion after quadriceps and patellar tendon repairs: outcomes with single-suture augmentation. American Journal of Sports Medicine 200836316–323. ( 10.1177/0363546507308192) [DOI] [PubMed] [Google Scholar]
- 48.Ibounig T, Simons TA. Etiology, diagnosis and treatment of tendinous knee extensor mechanism injuries. Scandinavian Journal of Surgery 201610567–72. ( 10.1177/1457496915598761) [DOI] [PubMed] [Google Scholar]
- 49.Hartline BE, Wilson JM, Schwartz AM, Roberson JR, Guild 3rd GN. Synthetic mesh reconstruction of chronic, native quadriceps tendon disruptions following failed primary repair. Case Reports in Orthopedics 202120215525319. ( 10.1155/2021/5525319) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Ciriello V, Gudipati S, Tosounidis T, Soucacos PN, Giannoudis PV. Clinical outcomes after repair of quadriceps tendon rupture: a systematic review. Injury 2012431931–1938. ( 10.1016/j.injury.2012.08.044) [DOI] [PubMed] [Google Scholar]
- 51.Schoderbek Jr RJ, Brown TE, Mulhall KJ, Mounasamy V, Iorio R, Krackow KA, Macaulay W, Saleh KJ. Extensor mechanism disruption after total knee arthroplasty. Clinical Orthopaedics and Related Research 2006446176–185. ( 10.1097/01.blo.0000218726.06473.26) [DOI] [PubMed] [Google Scholar]
- 52.Bonnin M, Lustig S, Huten D. Extensor tendon ruptures after total knee arthroplasty. Orthopaedics and Traumatology, Surgery and Research 2016102 (1 Supplement) S21–S31. ( 10.1016/j.otsr.2015.06.025) [DOI] [PubMed] [Google Scholar]
- 53.Papalia R, Vasta S, D’Adamio S, Albo E, Maffulli N, Denaro V. Complications involving the extensor mechanism after total knee arthroplasty. Knee Surgery, Sports Traumatology, Arthroscopy 2015233501–3515. ( 10.1007/s00167-014-3189-9) [DOI] [PubMed] [Google Scholar]
- 54.Shau D, Patton R, Patel S, Ward L, Guild 3rd G. Synthetic mesh vs. allograft extensor mechanism reconstruction in total knee arthroplasty – a systematic review of the literature and meta-analysis. Knee 2018252–7. ( 10.1016/j.knee.2017.12.004) [DOI] [PubMed] [Google Scholar]
- 55.Rand JA, Morrey BF, Bryan RS. Patellar tendon rupture after total knee arthroplasty. Clinical Orthopaedics and Related Research 1989244233–238. ( 10.1097/00003086-198907000-00023) [DOI] [PubMed] [Google Scholar]
- 56.Spoliti M, Via AG, Padulo J, Oliva F, Del Buono A, Maffulli N. Surgical repair of chronic patellar tendon rupture in total knee replacement with ipsilateral hamstring tendons. Knee Surgery, Sports Traumatology, Arthroscopy 2016243183–3190. ( 10.1007/s00167-014-3448-9) [DOI] [PubMed] [Google Scholar]
- 57.Gilmore JH, Clayton-Smith ZJ, Aguilar M, Pneumaticos SG, Giannoudis PV. Reconstruction techniques and clinical results of patellar tendon ruptures: evidence today. Knee 201522148–155. ( 10.1016/j.knee.2014.10.007) [DOI] [PubMed] [Google Scholar]
- 58.Wise BT, Erens G, Pour AE, Bradbury TL, Roberson JR. Long-term results of extensor reconstruction using Achilles tendon allograft after total knee arthroplasty. International Orthopaedics 2018422367–2373. ( 10.1007/s00264-018-3848-4) [DOI] [PubMed] [Google Scholar]
- 59.Llombart Blanco R, Valentí A, Díaz de Rada P, Mora G, Valentí JR. Reconstruction of the extensor mechanism with fresh-frozen tendon allograft in total knee arthroplasty. Knee Surgery, Sports Traumatology, Arthroscopy 2014222771–2775. ( 10.1007/s00167-013-2688-4) [DOI] [PubMed] [Google Scholar]
- 60.Lamberti A, Balato G, Summa PP, Rajgopal A, Vasdev A, Baldini A. Surgical options for chronic patellar tendon rupture in total knee arthroplasty. Knee Surgery, Sports Traumatology, Arthroscopy 2018261429–1435. ( 10.1007/s00167-016-4370-0) [DOI] [PubMed] [Google Scholar]
- 61.Zanotti RM, Freiberg AA, Matthews LS. Use of patellar allograft to reconstruct a patellar tendon-deficient knee after total joint arthroplasty. Journal of Arthroplasty 199510271–274. ( 10.1016/s0883-5403(0580173-1) [DOI] [PubMed] [Google Scholar]
- 62.Buller LT, Warth LC, Deckard ER, Meneghini RM. Extensor mechanism reconstruction using marlex mesh: is postoperative casting mandatory? Journal of Arthroplasty 2020353747–3753. ( 10.1016/j.arth.2020.06.037) [DOI] [PubMed] [Google Scholar]
- 63.Browne JA, Hanssen AD. Reconstruction of patellar tendon disruption after total knee arthroplasty: results of a new technique utilizing synthetic mesh. Journal of Bone and Joint Surgery: American Volume 2011931137–1143. ( 10.2106/JBJS.J.01036) [DOI] [PubMed] [Google Scholar]
- 64.Abdel MP, Salib CG, Mara KC, Pagnano MW, Perry KI, Hanssen AD. Extensor mechanism reconstruction with use of marlex mesh: a series study of 77 total knee arthroplasties. Journal of Bone and Joint Surgery: American Volume 20181001309–1318. ( 10.2106/JBJS.17.01165) [DOI] [PubMed] [Google Scholar]
- 65.Deren ME, Pannu TS, Villa JM, Firtha M, Riesgo AM, Higuera CA. Meta-analysis comparing allograft to synthetic reconstruction for extensor mechanism disruption after total knee arthroplasty. Journal of Knee Surgery 202134338–350. ( 10.1055/s-0039-1696656) [DOI] [PubMed] [Google Scholar]
- 66.Dobbs RE, Hanssen AD, Lewallen DG, Pagnano MW. Quadriceps tendon rupture after total knee arthroplasty. Prevalence, complications, and outcomes. Journal of Bone and Joint Surgery: American Volume 20058737–45. ( 10.2106/JBJS.D.01910) [DOI] [PubMed] [Google Scholar]
- 67.Jimenez A, Bedeir YH, Hasselfeld KA, Hasselfeld KA, Branam BR. Novel repair of a quadriceps tendon rupture after a total knee arthroplasty using gracilis and semitendinosus autografts. Knee 2020271446–1450. ( 10.1016/j.knee.2020.07.090) [DOI] [PubMed] [Google Scholar]
- 68.Miralles-Muñoz FA, Rubio-Morales M, Ruiz-Lozano M, Martinez-Mendez D, Gonzalez-Parreño S, Lizaur-Utrilla A. V-Y turndown flap augmentation for acute quadriceps rupture after total knee arthroplasty: a prospective matched cohort study. International Orthopaedics 2021451501–1507. ( 10.1007/s00264-021-04939-0) [DOI] [PubMed] [Google Scholar]
- 69.Shi SM, Shi GG, Laurent EM, Ninomiya JT. Modified V-Y turndown flap augmentation for quadriceps tendon rupture following total knee arthroplasty: a retrospective study. Journal of Bone and Joint Surgery: American Volume 20191011010–1015. ( 10.2106/JBJS.18.01098) [DOI] [PubMed] [Google Scholar]



 This work is licensed under a
This work is licensed under a