Abstract
Acetabular component orientation and position are important factors in the short- and long-term outcomes of total hip arthroplasty.
Different definitions of inclination and anteversion are used in the orthopaedic literature and surgeons should be aware of these differences and understand their relationships.
There is no universal safe zone.
Preoperative planning should be used to determine the optimum position and orientation of the cup and assess spinopelvic characteristics to adjust cup orientation accordingly.
A peripheral reaming technique leads to a more accurate restoration of the centre of rotation with less variability compared with a standard reaming technique.
Several intraoperative landmarks can be used to control the version of the cup, the most commonly used and studied is the transverse acetabular ligament.
The use of an inclinometer reduces the variability associated with the use of freehand or mechanical alignment guides.
Keywords: cup, total hip, orientation
Introduction
Acetabular component orientation and position are important factors in the short- and long-term outcomes of total hip arthroplasty (THA). Therefore, it is crucial that the surgeon has accurate and precise control over the orientation and position of the implanted cup. Improper acetabular orientation and position can lead to: (i) limited range of motion (1); (ii) increased dislocation rate (2); (iii) accelerated wear of polyethylene (3), metal-on-metal (4) and ceramic-on-ceramic (5) bearings; (iv) fatigue fracture of highly cross-linked polyethylene (6); (v) squeaking of ceramic-on-ceramic bearings (7) and ceramic fracture (8); (vi) worse patient-reported outcomes (9); (vii) iliopsoas tendinitis (10); (viii) leg length discrepancy and poor biomechanics (11); (ix) increased osteolysis and aseptic loosening (12); (x) component migration (12); (xi) higher revision rates (13).
Despite advances in technique, the accuracy of cup placement remains variable, even in experienced hands. Suboptimal orientation of the acetabular component has been reported in several studies, with 20–70% of components placed outside the so-called ‘safe zone’ (Table 1) (9, 14, 15, 16, 17, 18, 19). This is due to the intrinsic relationship between cup inclination and version, variance in orientation of the pelvis both at the beginning of surgery and time of cup impaction, and lack of accuracy, reliability and consistency of the orientation of the cup introducer at the time of impaction (20). The optimal position of the centre of rotation (COR) of the cup depends on the anatomy of the patient, more specifically acetabular floor depth, and the reaming technique (21).
Table 1.
Results of freehand cup placement in the literature.
| Reference | Anteversion | Abduction | Inside safe zone |
|---|---|---|---|
| Bosker et al. (14) | 5–25° | 30–50° | 70.5% |
| Callanan et al. (15) | 5–25° | 30–45° | 47% |
| DiGioia et al. (16) | 5–25° | 30–50° | 20.3% |
| Grammatopoulos et al. (45) | 5–25° | 30–50° | 50% |
| Hassan et al. (17) | 5–25° | 30–50° | 58% |
| Leichtle et al | 10–30° | 35–55° | 65.5% |
| Reize et al. (18) | 5–25° | 30–50° | 41% |
| Saxler et al. (19) | 5–25° | 30–50° | 25.7% |
Terminology and mathematics
Different definitions of inclination and anteversion have been used in the orthopaedic literature. These different definitions of cup inclination and anteversion cause confusion and make it very difficult to directly compare reports in the literature. Murray’s (22) definitions are as follows: the acetabular axis passes through the centre of the cup and is perpendicular to the acetabular plane; anatomic inclination (AI) is the angle between the acetabular axis and the longitudinal axis of the body; operative inclination (OI) is the angle between the acetabular axis and the sagittal plane (the angle of abduction of the acetabular axis); radiographic inclination (RI) is the angle between the longitudinal axis of the body and the acetabular axis when projected onto the coronal plane; anatomic anteversion (AA) is the angle between the acetabular axis and the transverse axis of the body when the acetabular axis is projected onto the transverse plane; operative anteversion (OA) is the angle between the longitudinal axis of the patient and the acetabular axis when projected onto the sagittal plane; and radiographic anteversion (RA) is the angle between the acetabular axis and the coronal plane.
From a surgeon’s point of view, the most important relationships to comprehend are that of the radiographic and operative anteversion and inclination angles (Fig. 1). The relation between the OA and RA is determined by the RI angle. The equation connecting the operative and radiographic anteversion is: tan(RA) = tan(OA) x cos(RI). This implies that with bigger RI angles the difference between the OA and RA becomes greater. When surgeons are aiming for a RA of 15°, they should actually aim for an OA of ±20° if the RI is 35–50° provided that the pelvis is in a neutral position at the time of cup impaction (Fig. 2).
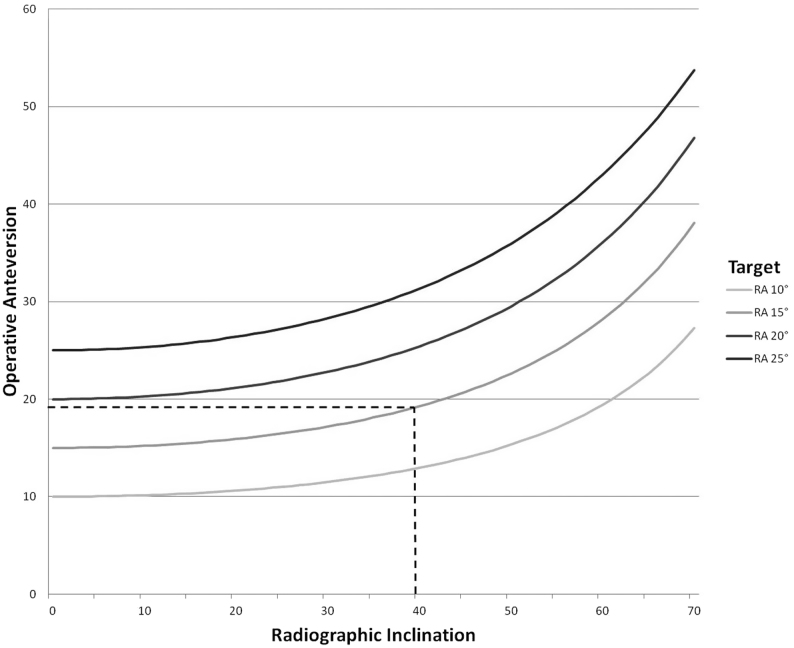
Figure 1.
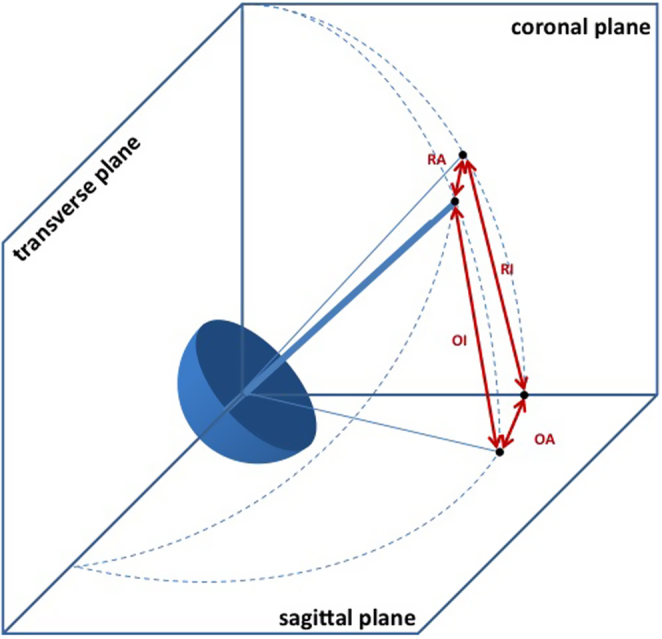
Anterior view of a 3D cup model implanted in the lateral decubitus position. The acetabular axis is represented by the thick blue line. OA, operative anteversion; OI, operative inclination; RA, radiographic anteversion; RI, radiographic anteversion.
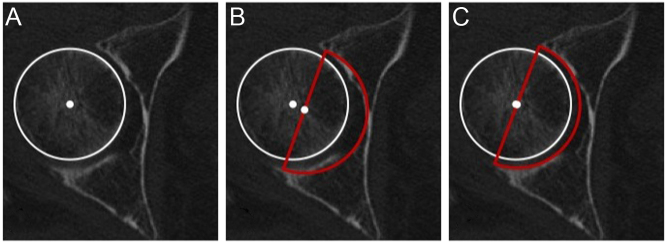
Figure 2.
Relationship between the targeted radiographic anteversion and the operative anteversion with regards to the radiographic inclination. When the radiographic inclination is 40° and the target is a 15° radiographic anteversion angle, the operative anteversion should be 19° (dotted line). RA, radiographic anteversion.
The equation connecting the OI and RI is: tan(OI) = tan(RI) x cos(OA). This implies that if a surgeon wants to achieve a specific RI they should aim for a smaller OI depending on the OA. Because the anteversion of the cup is numerically smaller, this difference is smaller compared with the difference between the OA and RA (Fig. 3). This is providing that the pelvis does not move during surgery and is positioned perfectly parallel to the vertical and horizontal plane of the operating table, this means with the sagittal plane parallel to the floor in lateral decubitus position.
Figure 3.
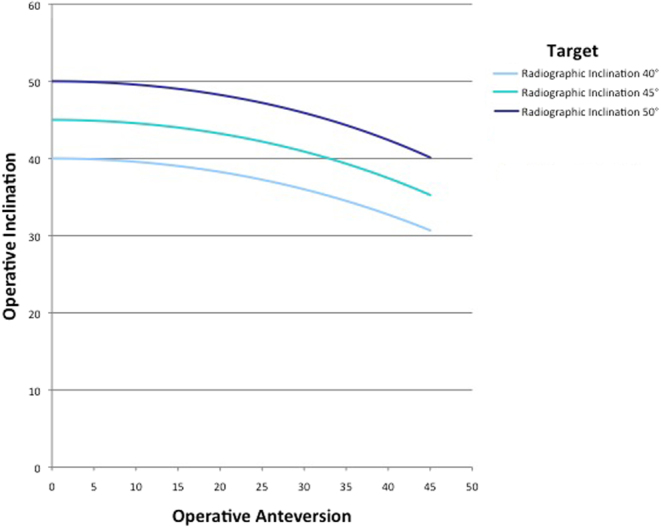
Relationship between the targeted radiographic inclination and the operative inclination with regards to the operative anteversion. RA, radiographic anteversion.
Safe zone
There is limited consensus in the literature as to what constitutes the optimum orientation of the acetabular component. Differences in reference systems, surgical techniques and measurement systems make objective comparisons of published studies difficult. Greater understanding of the optimal acetabular cup orientation would reduce the risk of revision surgery and alleviate the economic burden of revision surgery.
Although Lewinnek’s safe zone (40° ± 10° and 15° ± 10°) is still frequently used, the original paper does not stand up to our current scientific standard (23). In this study, conclusions were drawn based on only nine cases of dislocation of which six had revision THA. Only one case involved treatment of primary osteoarthritis. Three of the dislocations that did occur involved acetabular components within the safe zone and only 113 of 291 patients without dislocation had radiographs of sufficient quality to determine acetabular inclination and anteversion. More recent studies have confirmed the poor accuracy of the Lewinnek safe zone to predict mechanical complications after THA, including dislocation (24, 25, 26, 27, 28, 29).
These studies have demonstrated, that dislocations occur, despite cup orientation being within so-called ‘safe zones’. Having a cup within an acceptable cup orientation zone is associated with reduced risk of dislocation but the risk is not fully eliminated (9). This is because other factors (patient-, surgical- and implant-related) also contribute to THA stability, emphasizing the importance of surgical diligence in this multi-faceted issue.
Risk factors for malorientation
Surgeon factors
Callanan et al. (15) investigated the risk factors for cup malorientation in a tertiary hospital. The surgical approach was the only factor indicating cup malorientation in every analysis. The posterolateral approach was 20% more accurate than all other approaches. The minimally invasive approaches were the least accurate. This could be caused by a more constrained working space and decreased direct vision. The volume of surgeries performed was an indicator of malpositioning in inclination and anteversion and inclination combined. High-volume surgeons who performed an average of 164 THAs per year were 16% more accurate than the low-volume surgeons who performed an average of 13 THAs per year.
There only have been a few studies looking at the learning curve for optimal positioning of the acetabular component in primary THA. Bosker et al. (14) found a significant difference in inclination and anteversion of acetabular components in patients operated by an orthopaedic surgeon compared with a resident under the supervision of one of the surgeons. Reize et al. (18) found no difference in cup orientation when comparing surgeons with different levels of surgical experience. Biau et al. (30) demonstrated that implementing a system to monitor surgical performance in a teaching hospital improves the quality of THA. The most frequent reason why the performance of a primary THA was considered as inadequate was the malpositioning of the acetabular component. In a follow-up study, the proportion of failed acetabular components increased significantly with the use of a new cup design compared with those that had been used before (17 failures in 63 hips (27%) vs 15 failures in 137 hips (11%); P = 0.0064) (31). In a more recent study, the same authors found with the use of learning curve-cumulative summation test analysis that a substantial learning period (50 cases) is necessary for the optimal orientation of an acetabular cup (32). The results found in this latter study correspond to the ones found in another study with lower acetabular cup angle placements documented in the second cohort of 50 cases receiving an uncemented cup (33).
Patient factors
BMI was another indicator of increased risk of cup malpositioning. More specifically, obesity had a greater risk of malpositioning than the other BMI categories of underweight to overweight. In previous studies with smaller sample sizes this effect was not found (14, 34). In obese patients, there is a relatively smaller field for a given incision size due to the increased amount of adipose tissue. A large depth of fat can also influence the angle of the acetabular component inserter if it is forced against a deep wound edge. Furthermore, in obese patients, it is more difficult to get the pelvis well positioned at the beginning of surgery and there could be more intraoperative pelvic motion.
Pre-operative planning
The primary goal of total hip arthroplasty is the anatomic reconstruction of the hip joint, resulting in favourable prosthetic joint load and function. Mechanically, the goals are to create a stable articulation with an optimized range of motion, restore biomechanics for muscular efficiency and equalise limb lengths. This begins with a thorough analysis of the hip with comparison to the contralateral side in anteroposterior and lateral projections.
After determining the magnification of the X-ray, the orientation of the pelvic axis is drawn using the interteardrop line. True limb-length discrepancy due to abnormal anatomy of the proximal femur (e.g. femoral head collapse, old slipped capital femoral epiphysis, Perthes disease) is measured using the interteardrop line and the top of the lesser trochanter (35). If the limb lengths are clinically equal and correction of a limb-length discrepancy is not needed, this step can be omitted.
The COR of the hip joint is determined by placing the digital acetabular component template centrally within the confines of the acetabulum. At this stage, it is important to check the depth of the native acetabular floor and take this into account to avoid inadvertent medialization of the COR (36). When the acetabular component template is placed at an angle that is approximately 40–45° to the pelvic axis, the amount of lateral overhang can be used as an anatomical reference for inclination of the acetabular component (37). Because the amount of lateral overhang is influenced by the amount of medialization of the acetabular component and the inclination angle, the intraoperative measurement can be different from that preoperatively templated.
Spinopelvic motion
Recent studies have demonstrated a significantly higher risk for dislocation in patients with abnormal spinopelvic characteristics (25, 38, 39). Spinopelvic mobility describes the interaction of the lumbar spine, the pelvis and hip joint, whereas these three parts are acting as a kinetic chain. A decrease of mobility of one part may be compensated by a different part and vice versa. Therefore, a thorough understanding and preoperative workup of the relationship between the spine and pelvis, spinopelvic parameters, and normal and pathologic spinopelvic motion is critical to the prevention of instability after THA.
The position of the spine has an effect on the relative position of the pelvis, which in turn has a significant effect on acetabular orientation. Pelvic tilt (movement in the sagittal plane) significantly alters cup anteversion. A change in the sagittal pelvic tilt of 1° affects functional cup anteversion by approximately 0.7° (40). Functional cup inclination is also affected by the change in pelvic tilt, however, to a lesser degree. Thus, cup inclination and anteversion depend on pelvic tilt, which itself depends on the posture of the patient.
Pelvic tilt, among other parameters, is typically measured with conventional lateral radiographs or bi-planar radiographs (EOS) provided the images include the lumbar spine, pelvis and proximal femur. Hip surgeons typically assess pelvic tilt by measuring the angle between the anterior pelvic plane and a vertical or horizontal plane as this is more applicable for navigation- and robotically assisted surgery. Spine surgeons typically assess pelvic tilt by measuring the angle between a line connecting the centre of femoral heads and the middle of S1 vertebrae in the sagittal plane and the vertical; the 'pelvic incidence' (PI) more accurately reflects the relative position of the hip to the axial skeleton and is this more applicable to sagittal balance and the body’s biomechanics. Both ways are equally suited to measure the change in pelvic tilt in degrees between different postures. Different body positions have been described on how best to assess spinopelvic characteristics (standing, relaxed seated or deep seated). The standing position provides significant information. If dynamic assessment is desired, the transition between the standing to the deep-seated position is a more reliable assessment.
The authors have investigated spinopelvic mobility of hip OA patients pre- and post THA compared to a healthy control group in several studies (41, 42, 43, 44, 45, 46). Before THA, the range of motion of the hip joint is commonly decreased due to degenerative changes. Thus, when moving from a standing to a seated position, the reduced ability to flex the hip results in an increased posterior pelvic tilt, to accommodate for the inability of the arthritic hip to flex. After THA, the range of motion of the hip joint is commonly increased compared to preoperatively indicating successful treatment by THA. Thus, when moving from a standing to a seated position, the pelvis has to tilt less posteriorly, because the hip can be properly flexed. Thus, post-THA, spinopelvic characteristics become ‘more physiological’ akin to what is expected of healthy volunteers matched for age and sex (42, 46). Due to these changes in spinopelvic characteristics, the preoperative pelvic tilt or sacral slope is poorly suited to predict postoperative spinopelvic mobility, functional cup orientation or even the risk of dislocation. However, there are other preoperative radiographic parameters alerting surgeons of the increased risk of dislocation post-THA. These are static spinopelvic characteristics that change little or not at all following arthroplasty, increasing their reliability (44, 46).
The two characteristics that are reliable predictors for identifying patients at risk are (i) Spinopelvic imbalance (also called lumbar spine flatback deformity, defined as a difference of more than 10° between pelvic incidence and the lumbar lordosis angle in the standing position (PI - LL >10°)) and (ii) Spinal stiffness defined as a difference in lumbar lordosis of less than 20° when patients undergo dynamic spinopelvic investigations (between standing and deep-seated positions) (Fig.4). Such patients have degenerate spines that contribute little to the overall sagittal movement and often have abnormal tilt (relative position of the hips to the spine – hip relative extended when standing). Thus, these patients demand more from their hips during day-to-day activities and are at increased risk of dislocation.
Figure 4.
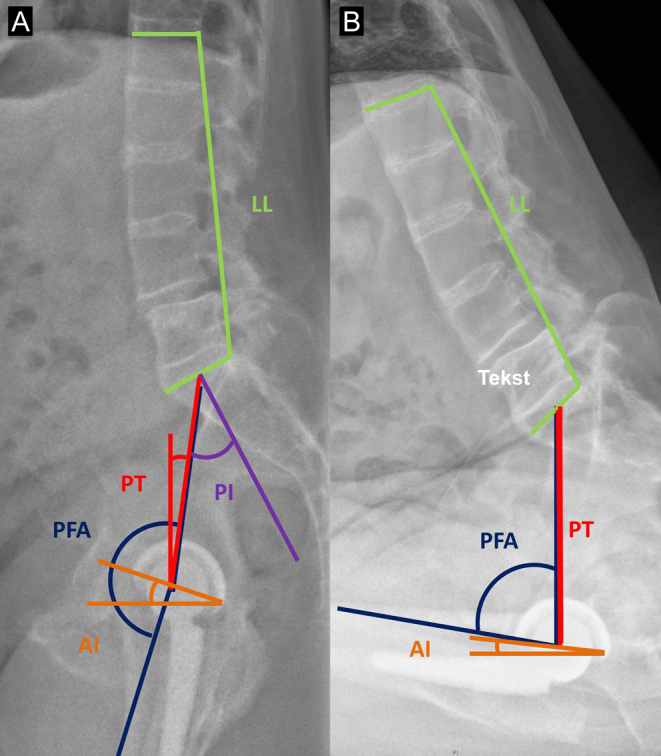
Lateral standing (A) and deep-seated (B) spinopelvic views of a 61 year old patient with Bechterew’s disease prior to his left total hip replacement, having undergone right total hip replacement earlier. The radiographs show all measurements that can be performed as part of pre- and post-op assessments. In this patient the change in LL between positions was 4° and his PI-LL value was 15° indicating that he is at a higher risk of instability post-THA due to a lumbar spine flat-back deformity and stiff lumbar spine. LL, lumbar lordosis angle; PI, pelvic incidence; PT, pelvic tilt; PFA, pelvic femoral angle as a measure of hip flexion; AI, ante-inclination
The authors have proposed an algorithm on how to incorporate spinopelvic characteristics into practice in determining optimum cup orientation and identifying patients with smaller ‘safe-zones’ of cup orientation. The combined sagittal index (CSI) is a valuable tool. It is the sum of the pelvic femoral angle (PFA) and cup anteinclination (AI). PFA is a measure of the patient’s standing hip flexion angle and does not change significantly with surgery (about 2–3°). AI is the sagittal orientation of the cup and is dependent on the orientation the surgeon implants the component. A standing CSI of 205–245°, is associated with a reduced dislocation risk. For patients at increased dislocation risk due to spinopelvic imbalance (PI - LL >10°), the range for the optimum CSI is however narrower (215–235°). Thus, knowing what the patient’s pre-operative PFA is can help surgeons determine what the range of AI should be. Nomograms have been developed to help guide surgeons for this in pre-operative planning, whilst aiming to satisfy both coronal (inclination and anteversion) and sagittal (anteinclination) targets. Whether reproducing the native version as per TAL and aiming for a 40° radiographic inclination increases the chances of being within the narrower CSI target is a topic of further study.
Patient positioning
It has been shown that the surgeons position the patients differently at the time of set-up for a THA and different pelvic supports provide varying levels of constraint to movement during surgery (47, 48) This has a significant effect on both cup inclination and version. Factors that influence pelvic position at the time of cup impaction are the position of the pelvis at the time of set-up, the approach, the procedure and the type of support (49). To avoid variability, patient set-up should be done in a standardized way and when operating in the lateral decubitus position two supports on the ipsi- and contralateral anterosuperior iliac spine should be used to minimize internal rotation of the pelvis during surgery. When operating in lateral decubitus irrespective of the support system used the key aim should be the same. Simply at the time of cup impaction, the pelvis should be neutral meaning that the pelvic sagittal plane is parallel to the floor.
Cup position
In the traditional Charnley approach, reaming of the acetabulum is started directly medial to the floor beginning with a small reamer and followed by sequentially larger reamers in the anticipated position of the implanted component (50). However, this could lead to inadvertent displacement of the COR and reduce global offset, which is the sum of femoral and acetabular offset.
The advantages of restoration of the COR are preservation of acetabular bone stock, decreased risk of bone or soft-tissue impingement (51, 52), improved kinematics (53), improved patient outcome scores (54), decreased wear (55), and decreased long-term loosening (13, 56). In order to avoid the adverse effects of displacement of the COR, it has been suggested that the COR should be restored <3 mm superiorly and <5 mm medially (57).
Several in vitro studies have demonstrated the large variability of acetabular anatomy in patients with primary osteoarthritis and the effect of reaming technique on displacement of the COR (36, 58, 59). Using a standard reaming technique, a substantial number of patients appear at risk for excessive cup medialization.
Clinical studies have reported displacement of the COR medially and superiorly and this displacement can be highly variable (Fig. 5) (57, 60, 61, 62). The level of surgical experience could play a role in the accuracy and consistency of cup placement (61). Furthermore, Benson et al. (62) used a navigation system to record the position of the COR intraoperatively and also found significant differences in antero-posterior displacement of the COR when stratified by the surgical approach, suggesting this displacement could be influenced by both patient positioning and reaming technique.
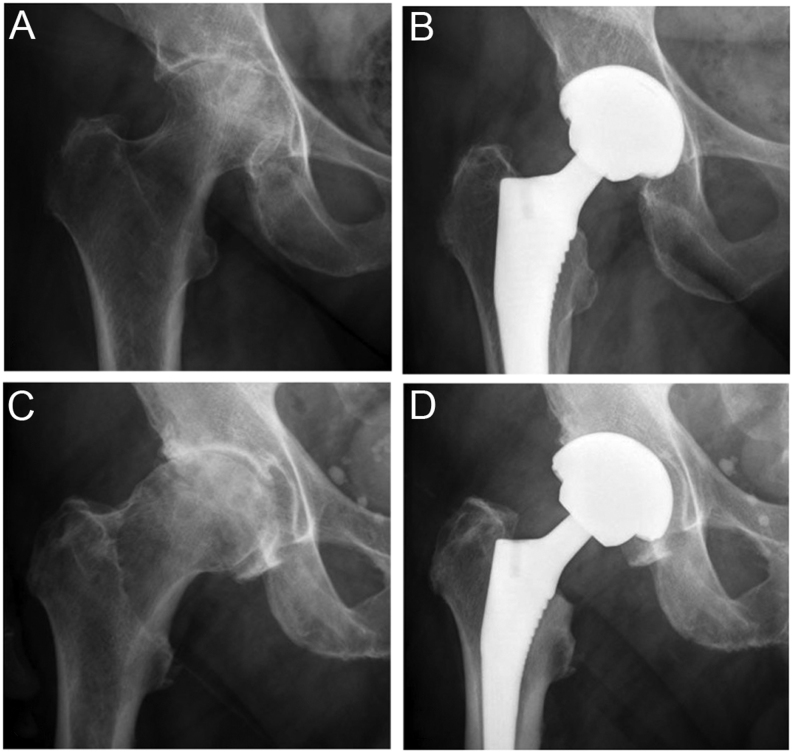
Figure 5.
(A) The centre of the femoral head. (B) When a cup is positioned flush with the true floor of the acetabulum (conventional technique) the centre of rotation is medialized. (C) When a cup is positioned using the anatomical technique the centre of rotation is maintained.
Therefore, some authors have advocated using a peripheral reaming technique which implies starting with a reamer the same size as the native femoral head followed by sequentially larger reamers until exposure of the subchondral bone. This leads to a more accurate restoration of the COR with less variability compared with a standard reaming technique (21). When using a standard reaming technique, medial and superior displacement of the COR is related to the pre-operative acetabular floor depth. In patients with a large acetabular floor depth, surgeons should be careful and adopt a technique to avoid excessive medial and superior displacement of the COR (Fig. 6).
Figure 6.
(A) Preoperative and (B) postoperative radiograph of a patient with low acetabular floor depth and (C) preoperative and (D) postoperative radiograph of a patient with high acetabular floor depth.
Cup orientation
Version
Highly anteverted cups correlate with an increased incidence of anterior dislocation while cups with too little anteversion and retroverted cups correlate with an increased risk of posterior dislocation. Currently, techniques used to improve the acetabular cup orientation include using patient-specific anatomical landmarks for acetabular cup placement. There are different methods to guide the placement of the acetabular component using anatomic landmarks without the need for special instruments. The landmarks are the sciatic notch (63), the bony landmarks encircling the acetabulum (37, 64), and the transverse acetabular ligament (65).
Archbold et al. (65) introduced a commonly used technique in which the plane of the transverse acetabular ligament (TAL) was used for cup anteversion (Fig. 7). With the use of this technique, they were able to reduce their primary dislocation rate from 3.7 to 0.6% (20). Although dislocation following THA is multifactorial and the cup version is not the only risk factor, other authors have found comparable low dislocation rates when using the TAL as a reference for the cup version (66, 67, 68).
Figure 7.
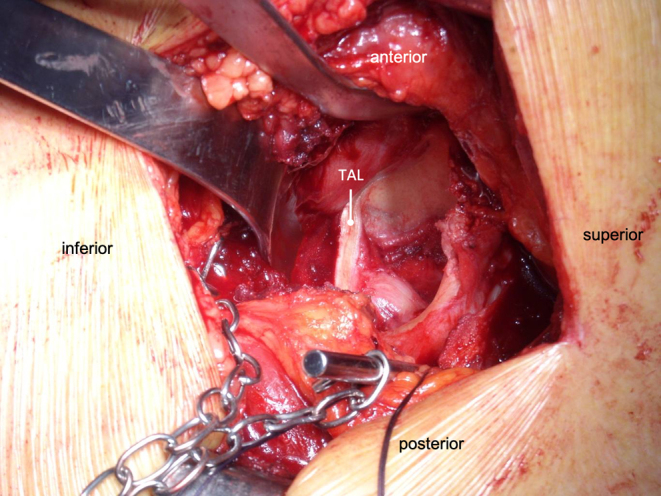
Intraoperative photographs of the use of the transverse acetabular ligament as a landmark for acetabular component version. TAL, transverse acetabular ligament.
The advantages of using intraoperative landmarks are that they are patient specific and are independent on patient position. Potential drawbacks to using anatomic landmarks include difficulty in locating certain features in diseased hips that have bony remodelling and osteophyte formation, and distortion secondary to trauma or dysplasia.
Inclination
In contrast to cup version, we have more proven boundaries when it comes to a target zone for cup inclination angles. It is widely acknowledged that radiographic inclination angles >50° are to be avoided.
Insertion of the acetabular component has traditionally been performed at an angle of 45° relative to the sagittal pelvic plane as judged by the surgeon’s eye (intra-operative inclination). However, orthopaedic surgeons are not always accurate in estimating angles (69, 70). Another commonly used technique involves attaching an alignment rod at 45° to the insertion rod on the presumption that it is easier for surgeons to evaluate a 90° angle than a 45° angle. These mechanical alignment guides are limited in that they can only achieve one target angle and lack accuracy (16, 17, 71). When operating with the patient in the lateral decubitus position, acetabular component orientation is influenced by pelvic motion during surgery which can be highly variable (72, 73).
To reduce the variability associated with the use of freehand or mechanical alignment guides, the use of an inclinometer is an attractive option as it can provide a more accurate means of measuring intraoperative acetabular component inclination than mechanical alignment guides but is simpler, more efficient and more cost-effective than computer navigation (74, 75, 76, 77, 78, 79, 80). Beacuse the relation between the RI and operative inclination (OI) is determined by the cosine of the operative anteversion and when operating in the lateral decubitus position the operated hemipelvis is commonly adducted and internally rotated, surgeons should aim for an angle of 30–35° of the cup introducer relative to the floor (20, 76). Overall, the use of an inclinometer resulted in a mean radiographic inclination angle closer to the target angle with less variation and outliers when compared with freehand and mechanical alignment techniques (81).
Conclusion
Total hip arthroplasty has become one of the most common and successful orthopaedic procedures. Correct cup orientation and position are critical to successful total hip replacements. It is important that surgeons are familiar with the different definitions of anteversion and inclinations, understand their relationship and are aware of the risk factors of cup malpositioning. Placing the acetabular component into an average position is not ideal for every patient. Differences in functional pelvic position, surgical approach, and femoral anteversion affect the optimal cup position for individual patients.
External guides are inconsistent and mistaken assumptions on their accuracy can lead to poor cup placement. Preoperative templating and anatomic landmarks can help guide acetabular placement. Computer navigation and robotics have been shown to improve accuracy, but are nowadays not widely used because of the additional costs, increase in operating time, and technical problems with the current systems in use. Patient-specific anatomy, rather than a generic safe zone, coupled with the use of quantitative technology such as computer navigation, may result in better short- and long-term outcomes and might be the future of cup placement in total hip arthroplasty.
ICMJE Conflict of Interest Statement
D E B reports receiving payment for lectures, travel, royalties from Depuy Synthes. G M reports receiving consultancy fees from Johnson & Johnson and institutional support from Zimmer-Biomet. Other authors have nothing to declare.
Funding Statement
The work reported here did not receive any specific grant from any funding agency in the public, commercial or not-for-profit sector.
References
- 1.Malik A, Maheshwari A, Dorr LD. Impingement with total hip replacement. Journal of Bone and Joint Surgery: American Volume 2007891832–1842. ( 10.2106/JBJS.F.01313) [DOI] [PubMed] [Google Scholar]
- 2.Jolles BM, Zangger P, Leyvraz PF. Factors predisposing to dislocation after primary total hip arthroplasty: a multivariate analysis. Journal of Arthroplasty 200217282–288. ( 10.1054/arth.2002.30286) [DOI] [PubMed] [Google Scholar]
- 3.Wan Z, Boutary M, Dorr LD. The influence of acetabular component position on wear in total hip arthroplasty. Journal of Arthroplasty 20082351–56. ( 10.1016/j.arth.2007.06.008) [DOI] [PubMed] [Google Scholar]
- 4.De Haan R, Campbell PA, Su EP, De Smet KA. Revision of metal-on-metal resurfacing arthroplasty of the hip: the influence of malpositioning of the components. Journal of Bone and Joint Surgery: Series B 2008901158–1163. ( 10.1302/0301-620X.90B9.19891) [DOI] [PubMed] [Google Scholar]
- 5.Al-Hajjar M, Leslie IJ, Tipper J, Williams S, Fisher J, Jennings LM. Effect of cup inclination angle during microseparation and rim loading on the wear of BIOLOX® delta ceramic-on-ceramic total hip replacement. Journal of Biomedical Materials Research: Part B, Applied Biomaterials 201095263–268. ( 10.1002/jbm.b.31708) [DOI] [PubMed] [Google Scholar]
- 6.Tower SS, Currier JH, Currier BH, Lyford KA, Van Citters DW, Mayor MB. Rim cracking of the cross-linked longevity polyethylene acetabular liner after total hip arthroplasty. Journal of Bone and Joint Surgery: Series A 2007892212–2217. ( 10.2106/JBJS.F.00758) [DOI] [PubMed] [Google Scholar]
- 7.Sexton SA, Yeung E, Jackson MP, Rajaratnam S, Martell JM, Walter WL, Zicat BA, Walter WK. The role of patient factors and implant position in squeaking of ceramic-on-ceramic total hip replacements. Journal of Bone and Joint Surgery: Series B 201193B439–442. ( 10.1302/0301-620X.93B4.25707) [DOI] [PubMed] [Google Scholar]
- 8.Traina F, De Fine M, Bordini B, Toni A. Risk factors for ceramic liner fracture after total hip arthroplasty. Hip International 201222607–614. ( 10.5301/HIP.2012.10339) [DOI] [PubMed] [Google Scholar]
- 9.Grammatopoulos G, Thomas GER, Pandit H, Beard DJ, Murray DW, Gill HS. The effect of orientation of the acetabular component on outcome following total hip arthroplasty with small diameter hard-on-soft bearings. Bone and Joint Journal 201597-B164–172. ( 10.1302/0301-620X.97B2.34294) [DOI] [PubMed] [Google Scholar]
- 10.Trousdale RT, Cabanela ME, Berry DJ. Anterior iliopsoas impingement after total hip arthroplasty. Journal of Arthroplasty 199510546–549. ( 10.1016/s0883-5403(0580160-3) [DOI] [PubMed] [Google Scholar]
- 11.Clark CR, Huddleston HD, Schoch EP, Thomas BJ. Leg-length discrepancy after total hip arthroplasty. Journal of the American Academy of Orthopaedic Surgeons 20061438–45. ( 10.5435/00124635-200601000-00007) [DOI] [PubMed] [Google Scholar]
- 12.Kennedy JG, Rogers WB, Soffe KE, Sullivan RJ, Griffen DG, Sheehan LJ. Effect of acetabular component orientation on recurrent dislocation, pelvic osteolysis, polyethylene wear, and component migration. Journal of Arthroplasty 199813530–534. ( 10.1016/s0883-5403(9890052-3) [DOI] [PubMed] [Google Scholar]
- 13.Karachalios T, Hartofilakidis G, Zacharakis N, Tsekoura M. A 12- to 18-year radiographic follow-up study of Charnley low-friction arthroplasty: the role of the center of rotation. Clinical Orthopaedics and Related Research 1993296140–147. ( 10.1097/00003086-199311000-00026) [DOI] [PubMed] [Google Scholar]
- 14.Bosker BH, Verheyen CCPM, Horstmann WG, Tulp NJA. Poor accuracy of freehand cup positioning during total hip arthroplasty. Archives of Orthopaedic and Trauma Surgery 2007127375–379. ( 10.1007/s00402-007-0294-y) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Callanan MC, Jarrett B, Bragdon CR, Zurakowski D, Rubash HE, Freiberg AA, Malchau H. The john charnley award: risk factors for cup malpositioning: quality improvement through a joint registry at a tertiary hospital. Clinical Orthopaedics and Related Research 2011469319–329. ( 10.1007/s11999-010-1487-1) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.DiGioia AM, Jaramaz B, Plakseychuk AY, Moody JE, Nikou C, LaBarca RS, Levison TJ, Picard F. Comparison of a mechanical acetabular alignment guide with computer placement of the socket. Journal of Arthroplasty 200217359–364. ( 10.1054/arth.2002.30411) [DOI] [PubMed] [Google Scholar]
- 17.Hassan DM, Johnston GHF, Dust WNC, Watson G, Dolovich AT. Accuracy of intraoperative assessment of acetabular prosthesis placement. Journal of Arthroplasty 19981380–84. ( 10.1016/s0883-5403(9890079-1) [DOI] [PubMed] [Google Scholar]
- 18.Reize P, Geiger EV, Suckel A, Rudert M, Wülker N. Influence of surgical experience on accuracy of acetabular cup positioning in total hip arthroplasty. American Journal of Orthopedics 200837360–363. [PubMed] [Google Scholar]
- 19.Saxler G, Marx A, Vandevelde D, Langlotz U, Tannast M, Wiese M, Michaelis U, Kemper G, Grützner PA, Steffen Ret al. The accuracy of free-hand cup positioning – a CT based measurement of cup placement in 105 total hip arthroplasties. International Orthopaedics 200428198–201. ( 10.1007/s00264-004-0542-5) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Beverland DE, O’Neill CKJ, Rutherford M, Molloy D, Hill JC. Placement of the acetabular component. Bone and Joint Journal 201698-B (1 SupplementA) 37–43. ( 10.1302/0301-620X.98B1.36343) [DOI] [PubMed] [Google Scholar]
- 21.Meermans G, Van Doorn J, Kats JJ. Restoration of the centre of rotation in primary total hip arthroplasty the influence of acetabular floor depth and reaming technique. Bone and Joint Journal 201698-B1597–1603. ( 10.1302/0301-620X.98B12.BJJ-2016-0345.R1) [DOI] [PubMed] [Google Scholar]
- 22.Murray DW.The definition and measurement of acetabular orientation. Journal of Bone and Joint Surgery: Series B 199375228–232. ( 10.1302/0301-620X.75B2.8444942) [DOI] [PubMed] [Google Scholar]
- 23.Lewinnek GE, Lewis JL, Tarr R, Compere CL, Zimmerman JR. Dislocations after total hip-replacement arthroplasties. Journal of Bone and Joint Surgery: American Volume 197860217–220. ( 10.2106/00004623-197860020-00014) [DOI] [PubMed] [Google Scholar]
- 24.Abdel MP, von Roth P, Jennings MT, Hanssen AD, Pagnano MW. What safe zone? The vast majority of dislocated THAs are within the Lewinnek safe zone for acetabular component position. Clinical Orthopaedics and Related Research 2016474386–391. ( 10.1007/s11999-015-4432-5) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.DelSole EM, Vigdorchik JM, Schwarzkopf R, Errico TJ, Buckland AJ. Total hip arthroplasty in the spinal deformity population: does degree of sagittal deformity affect rates of safe zone placement, instability, or revision? Journal of Arthroplasty 2017321910–1917. ( 10.1016/j.arth.2016.12.039) [DOI] [PubMed] [Google Scholar]
- 26.Murphy WS, Yun HH, Hayden B, Kowal JH, Murphy SB. The safe zone range for cup anteversion is narrower than for inclination in THA. Clinical Orthopaedics and Related Research 2018476325–335. ( 10.1007/s11999.0000000000000051) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Sadhu A, Nam D, Coobs BR, Barrack TN, Nunley RM, Barrack RL. Acetabular component position and the risk of dislocation following primary and revision total hip arthroplasty: a matched cohort analysis. Journal of Arthroplasty 201732987–991. ( 10.1016/j.arth.2016.08.008) [DOI] [PubMed] [Google Scholar]
- 28.Seagrave KG, Troelsen A, Malchau H, Husted H, Gromov K. Acetabular cup position and risk of dislocation in primary total hip arthroplasty. Acta Orthopaedica 20178810–17. ( 10.1080/17453674.2016.1251255) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Timperley AJ, Biau D, Chew D, Whitehouse SL. Dislocation after total hip replacement – there is no such thing as a safe zone for socket placement with the posterior approach. Hip International 201626121–127. ( 10.5301/hipint.5000318) [DOI] [PubMed] [Google Scholar]
- 30.Biau DJ, Milet A, Thévenin F, Anract P, Porcher R. Monitoring surgical performance: an application to total hip replacement. Journal of Evaluation in Clinical Practice 200915420–424. ( 10.1111/j.1365-2753.2008.01029.x) [DOI] [PubMed] [Google Scholar]
- 31.Biau DJ, Meziane M, Bhumbra RS, Dumaine V, Babinet A, Anract P. Monitoring the quality of total hip replacement in a tertiary care department using a cumulative summation statistical method (CUSUM). Journal of Bone and Joint Surgery: Series B 201193B1183–1188. ( 10.1302/0301-620X.93B9.26436) [DOI] [PubMed] [Google Scholar]
- 32.Lee YK, Biau DJ, Yoon BH, Kim TY, Ha YC, Koo KH. Learning curve of acetabular cup positioning in total hip arthroplasty using a cumulative summation test for learning curve (LC-CUSUM). Journal of Arthroplasty 201429586–589. ( 10.1016/j.arth.2013.07.023) [DOI] [PubMed] [Google Scholar]
- 33.Callaghan JJ, Heekin RD, Savory CG, Dysart SH, Hopkinson WJ. Evaluation of the learning curve associated with uncemented primary porous-coated anatomic total hip arthroplasty. Clinical Orthopaedics and Related Research 1992282132–144. ( 10.1097/00003086-199209000-00017) [DOI] [PubMed] [Google Scholar]
- 34.Todkar M.Obesity does not necessarily affect the accuracy of acetabular cup implantation in total hip replacement. Acta Orthopaedica Belgica 200874206–209. [PubMed] [Google Scholar]
- 35.Meermans G, Malik A, Witt J, Haddad F. Preoperative radiographic assessment of limb-length discrepancy in total hip arthroplasty. Clinical Orthopaedics and Related Research 20114691677–1682. ( 10.1007/s11999-010-1588-x) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Bonnin MP, Archbold PHA, Basiglini L, Fessy MH, Beverl DE. Do we medialise the hip centre of rotation in total hip arthroplasty? Influence of acetabular offset and surgical technique. Hip International 201222371–378. ( 10.5301/HIP.2012.9350) [DOI] [PubMed] [Google Scholar]
- 37.Sotereanos NG, Miller MC, Smith B, Hube R, Sewecke JJ, Wohlrab D. Using intraoperative pelvic landmarks for acetabular component placement in total hip arthroplasty. Journal of Arthroplasty 200621832–840. ( 10.1016/j.arth.2005.12.001) [DOI] [PubMed] [Google Scholar]
- 38.Heckmann N, McKnight B, Stefl M, Trasolini NA, Ike H, Dorr LD. Late dislocation following total hip arthroplasty: spinopelvic imbalance as a causative factor. Journal of Bone and Joint Surgery: American Volume 20181001845–1853. ( 10.2106/JBJS.18.00078) [DOI] [PubMed] [Google Scholar]
- 39.Esposito CI, Carroll KM, Sculco PK, Padgett DE, Jerabek SA, Mayman DJ. Total hip arthroplasty patients with fixed spinopelvic alignment are at higher risk of hip dislocation. Journal of Arthroplasty 2018331449–1454. ( 10.1016/j.arth.2017.12.005) [DOI] [PubMed] [Google Scholar]
- 40.Ranawat CS, Ranawat AS, Lipman JD, White PB, Meftah M. Effect of spinal deformity on pelvic orientation from standing to sitting position. Journal of Arthroplasty 2016311222–1227. ( 10.1016/j.arth.2015.11.035) [DOI] [PubMed] [Google Scholar]
- 41.Innmann MM, Reichel F, Schaper B, Merle C, Beaulé PE, Grammatopoulos G. How does spinopelvic mobility and sagittal functional cup orientation affect patient-reported outcome 1 year after THA? – A prospective diagnostic cohort study. Journal of Arthroplasty 2021362335–2342. ( 10.1016/j.arth.2021.02.014) [DOI] [PubMed] [Google Scholar]
- 42.Innmann MM, Merle C, Phan P, Beaulé PE, Grammatopoulos G. Differences in spinopelvic characteristics between hip osteoarthritis patients and controls. Journal of Arthroplasty 2021362808–2816. ( 10.1016/j.arth.2021.03.031) [DOI] [PubMed] [Google Scholar]
- 43.Innmann MM, Weishorn J, Beaule PE, Grammatopoulos G, Merle C. Pathologic spinopelvic balance in patients with hip osteoarthritis: preoperative screening and therapeutic implications. Der Orthopade 202049860–869. ( 10.1007/s00132-020-03981-x) [DOI] [PubMed] [Google Scholar]
- 44.Grammatopoulos G, Falsetto A, Sanders E, Weishorn J, Gill HS, Beaulé PE, Innmann ME, Merle C. Integrating the combined sagittal index reduces the risk of dislocation following total hip replacement. Journal of Bone and Joint Surgery 2022104397–411. ( 10.2106/JBJS.21.00432) [DOI] [PubMed] [Google Scholar]
- 45.Grammatopoulos G, Gofton W, Jibri Z, Coyle M, Dobransky J, Kreviazuk C, Kim PR, Beaulé PE. 2018 Frank Stinchfield Award: spinopelvic hypermobility is associated with an inferior outcome after THA: examining the effect of spinal arthrodesis. Clinical Orthopaedics and Related Research 2019477310–321. ( 10.1097/CORR.0000000000000367) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Innmann MM, Verhaegen JCF, Reichel F, Schaper B, Merle C, Grammatopoulos G. Spinopelvic characteristics normalize 1 year after total hip arthroplasty: a prospective, longitudinal, case-controlled study. Journal of Bone and Joint Surgery: American Volume 2022104675––683.. ( 10.2106/JBJS.21.01127) [DOI] [PubMed] [Google Scholar]
- 47.Grammatopoulos G, Pandit HG, Da Assunção R, McLardy-Smith P, De Smet KA, Gill HS, Murray DW. The relationship between operative and radiographic acetabular component orientation: which factors influence resultant cup orientation? Bone and Joint Journal 201496-B1290–1297. ( 10.1302/0301-620X.96B10.34100) [DOI] [PubMed] [Google Scholar]
- 48.Grammatopoulos G, Pandit HG, da Assunção R, Taylor A, McLardy-Smith P, De Smet KA, Murray DW, Gill HS. Pelvic position and movement during hip replacement. Bone and Joint Journal 201496-B876–883. ( 10.1302/0301-620X.96B7.32107) [DOI] [PubMed] [Google Scholar]
- 49.Grammatopoulos G, Gofton W, Cochran M, Dobransky J, Carli A, Abdelbary H, Gill HS, Beaulé PE. Pelvic positioning in the supine position leads to more consistent orientation of the acetabular component after total hip arthroplasty. Bone and Joint Journal 2018100-B1280–1288. ( 10.1302/0301-620X.100B10.BJJ-2018-0134.R1) [DOI] [PubMed] [Google Scholar]
- 50.Charnley J.Low Friction Arthroplasty of the Hip. Berlin,Heidelberg: Springer, 1979. [Google Scholar]
- 51.Kurtz WB, Ecker TM, Reichmann WM, Murphy SB. Factors affecting bony impingement in hip arthroplasty. Journal of Arthroplasty 201025624, .e1–63. ( 10.1016/j.arth.2009.03.024) [DOI] [PubMed] [Google Scholar]
- 52.García-Rey E, García-Cimbrelo E. Abductor biomechanics clinically impact the total hip arthroplasty dislocation rate. A prospective long-term study. Journal of Arthroplasty 201631484–490. ( 10.1016/j.arth.2015.09.039) [DOI] [PubMed] [Google Scholar]
- 53.Stief F, van Drongelen S, Brenneis M, Tarhan T, Fey B, Meurer A. Influence of hip geometry reconstruction on frontal plane hip and knee joint moments during walking following primary total hip replacement. Journal of Arthroplasty 2019343106–3113. ( 10.1016/j.arth.2019.07.027) [DOI] [PubMed] [Google Scholar]
- 54.Mahmood SS, Mukka SS, Crnalic S, Wretenberg P, Sayed-Noor AS. Association between changes in global femoral offset after total hip arthroplasty and function, quality of life, and abductor muscle strength. A prospective cohort study of 222 patients. Acta Orthopaedica 20168736–41. ( 10.3109/17453674.2015.1091955) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Little NJ, Busch CA, Gallagher JA, Rorabeck CH, Bourne RB. Acetabular polyethylene wear and acetabular inclination and femoral offset. Clinical Orthopaedics and Related Research 20094672895–2900. ( 10.1007/s11999-009-0845-3) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Callaghan JJ, Salvati EA, Pellicci PM, Wilson PD, Ranawat CS. Results of revision for mechanical failure after cemented total hip replacement, 1979 to 1982. A two to five-year follow-up. Journal of Bone and Joint Surgery: Series A 1985671074–1085. [PubMed] [Google Scholar]
- 57.Dastane M, Dorr LD, Tarwala R, Wan Z. Hip offset in total hip arthroplasty: quantitative measurement with navigation. Clinical Orthopaedics and Related Research 2011469429–436. ( 10.1007/s11999-010-1554-7) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Merle C, Innmann MM, Waldstein W, Pegg EC, Aldinger PR, Gill HS, Murray DW, Grammatopoulos G. High variability of acetabular offset in primary hip osteoarthritis influences acetabular reaming – a computed tomography-based anatomic study. Journal of Arthroplasty 2019341808–1814. ( 10.1016/j.arth.2019.03.065) [DOI] [PubMed] [Google Scholar]
- 59.Messer-Hannemann P, Bätz J, Lampe F, Klein A, Püschel K, Campbell GM, Morlock M. The influence of cavity preparation and press-fit cup implantation on restoring the hip rotation center. Clinical Biomechanics 201963185–192. ( 10.1016/j.clinbiomech.2019.03.006) [DOI] [PubMed] [Google Scholar]
- 60.Bjarnason JA, Reikeras O. Changes of center of rotation and femoral offset in total hip arthroplasty. Annals of Translational Medicine 20153355. ( 10.3978/j.issn.2305-5839.2015.12.37) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Kim SC, Lim YW, Kwon SY, Jo WL, Ju SH, Park CJ, Lee CW, Kim YS. Level of surgical experience is associated with change in hip center of rotation following cementless total hip arthroplasty: a radiographic assessment. PLoS ONE 201712e0178300. ( 10.1371/journal.pone.0178300) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Benson JR, Govindarajan M, Muir JM, Lamb IR, Sculco PK. Surgical approach and reaming depth influence the direction and magnitude of acetabular center of rotation changes during total hip arthroplasty. Arthroplasty Today 20206414–421. ( 10.1016/j.artd.2020.04.003) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.McCollum DE, Gray WJ. Dislocation after total hip arthroplasty: causes and prevention. Clinical Orthopaedics and Related Research 1990261159–170. ( 10.1097/00003086-199012000-00019) [DOI] [PubMed] [Google Scholar]
- 64.Ha YC, Yoo JJ, Lee YK, Kim JY, Koo KH. Acetabular component positioning using anatomic landmarks of the acetabulum. Clinical Orthopaedics and Related Research 20124703515–3523. ( 10.1007/s11999-012-2460-y) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Archbold HAP, Mockford B, Molloy D, McConway J, Ogonda L, Beverland D. The transverse acetabular ligament: an aid to orientation of the acetabular component during primary total hip replacement. A preliminary study of 1000 cases investigating post-operative stability. Journal of Bone and Joint Surgery: Series B 200688883–886. ( 10.1302/0301-620X.88B7.17577) [DOI] [PubMed] [Google Scholar]
- 66.Epstein NJ, Woolson ST, Giori NJ. Acetabular component positioning using the transverse acetabular ligament: can you find it and does it help? Clinical Orthopaedics and Related Research 2011469412–416. ( 10.1007/s11999-010-1523-1) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Ho KWK, Whitwell GS, Young SK. Reducing the rate of early primary hip dislocation by combining a change in surgical technique and an increase in femoral head diameter to 36 mm. Archives of Orthopaedic and Trauma Surgery 20121321031–1036. ( 10.1007/s00402-012-1508-5) [DOI] [PubMed] [Google Scholar]
- 68.Miyoshi H, Mikami H, Oba K, Amari R. Anteversion of the acetabular component aligned with the transverse acetabular ligament in total hip arthroplasty. Journal of Arthroplasty 201227916–922. ( 10.1016/j.arth.2011.10.017) [DOI] [PubMed] [Google Scholar]
- 69.Dorr LD, Malik A, Wan Z, Long WT, Harris M. Precision and bias of imageless computer navigation and surgeon estimates for acetabular component position. Clinical Orthopaedics and Related Research 200746592–99. ( 10.1097/BLO.0b013e3181560c51) [DOI] [PubMed] [Google Scholar]
- 70.Moran KM, Ness K, Finkbeiner AA. Visual estimation of angles by orthopedic surgeons. American Journal of Orthopedics 200029361–362; discussion 363. [PubMed] [Google Scholar]
- 71.Minoda Y, Ohzono K, Aihara M, Umeda N, Tomita M, Hayakawa K. Are acetabular component alignment guides for total hip arthroplasty accurate? Journal of Arthroplasty 201025986–989. ( 10.1016/j.arth.2009.07.016) [DOI] [PubMed] [Google Scholar]
- 72.Asayama I, Akiyoshi Y, Naito M, Ezoe M. Intraoperative pelvic motion in total hip arthroplasty. Journal of Arthroplasty 200419992–997. ( 10.1016/j.arth.2004.03.013) [DOI] [PubMed] [Google Scholar]
- 73.Nishikubo Y, Fujioka M, Ueshima K, Saito M, Kubo T. Preoperative fluoroscopic imaging reduces variability of acetabular component positioning. Journal of Arthroplasty 2011261088–1094. ( 10.1016/j.arth.2011.05.011) [DOI] [PubMed] [Google Scholar]
- 74.Darrith B, Bell AJ, Valle CJD, Culvern C. Can the use of an inclinometer improve the positioning of the acetabular component in total hip arthroplasty? Bone and Joint Journal 2018100-B862–866. ( 10.1302/0301-620X.100B7.BJJ-2017-1607.R1) [DOI] [PubMed] [Google Scholar]
- 75.Hill JC, Gibson DP, Pagoti R, Beverland DE. Photographic measurement of the inclination of the acetabular component in total hip replacement using the posterior approach. Journal of Bone and Joint Surgery: Series B 2010921209–1214. ( 10.1302/0301-620X.92B9.24476) [DOI] [PubMed] [Google Scholar]
- 76.Meermans G, Goetheer-Smits I, Lim RF, Van Doorn WJ, Kats J. The difference between the radiographic and the operative angle of inclination of the acetabular component in total hip arthroplasty: use of a digital protractor and the circumference of the hip to improve orientation. Bone and Joint Journal 201597-B603–610. ( 10.1302/0301-620X.97B5.34781) [DOI] [PubMed] [Google Scholar]
- 77.O’Neill CKJ, Hill JC, Patterson CC, Molloy DO, Gill HS, Beverland DE. Reducing variability in apparent operative inclination during total hip arthroplasty: findings of a randomised controlled trial. Hip International 201828234–239. ( 10.1177/1120700018777485) [DOI] [PubMed] [Google Scholar]
- 78.Pongkunakorn A, Chatmaitri S, Diewwattanawiwat K. Use of smartphone to improve acetabular component positioning in total hip athroplasty: a comparative clinical study. Journal of Orthopaedic Surgery 2019272309499019825578. ( 10.1177/2309499019825578) [DOI] [PubMed] [Google Scholar]
- 79.Vendittoli PA, Duval N, Stitson DJ, Mâsse B. Vertical acetabular positioning with an inclinometer in total hip arthroplasty. Journal of Arthroplasty 200217936–941. ( 10.1054/arth.2002.34820) [DOI] [PubMed] [Google Scholar]
- 80.Vendittoli PA, Ganapathi M, Duval N, Lavoie P, Roy A, Lavigne M. Randomised controlled trial comparing two methods of acetabular cup positioning during total hip arthroplasty. Hip International 200717137–142. ( 10.5301/hip.2008.658) [DOI] [PubMed] [Google Scholar]
- 81.van Duren BH, Royeca JM, Cunningham CM, Lamb JN, Brew CJ, Pandit H. Can the use of an inclinometer improve acetabular cup inclination in total hip arthroplasty? A review of the literature. Hip International 202131609–617. ( 10.1177/1120700020946716) [DOI] [PMC free article] [PubMed] [Google Scholar]



 This work is licensed under a
This work is licensed under a