All nephrons are terminally differentiated at 36 weeks of gestation, but only a few are active soon after birth. Subsequently, nephrons become rapidly recruited, in the sequence in which they formed, until they asymptotically reach stable GFR at 18–24 months of age. It is important to assess kidney function in the neonate, but state-of-the-art measurements with exogenous markers (i.e., inulin) are challenging to perform, and the few published studies have small patient numbers.1 The most widely used endogenous biomarker, serum creatinine (sCr), crosses the placenta and reflects maternal kidney function.2 Cystatin C (cysC), the second most widely used endogenous marker of GFR, may cross the placenta in very small quantities, whereas beta-trace protein does not.3,4 Currently, no meta-analysis focuses on neonatal kidney function, so the study by Smeets et al. in this edition of JASN of 944 term neonates on the basis of measured GFR (mGFR)5 is of great interest.
The Study by Smeets et al.
Smeets’ team analyzed 50 studies published from 1947 to 2014, which included 1041 mGFR values from the 944 neonates. Individual participant data were available for 367, and 44 aggregated datapoints represented the other 577 neonates. The authors included exogenous GFR markers such as inulin (44% of studies, 28.4% of patients), mannitol (6% of studies and 6.3% of patients), or 51Cr-EDTA (2% of studies and 0.6% of patients), and 48% of studies (64.7% of patients) were on the basis of creatinine clearance, potentially skewing findings. Most of the studies were small (median numbers of participants were eight for inulin, 21 for creatinine clearance, and 11 for mannitol).
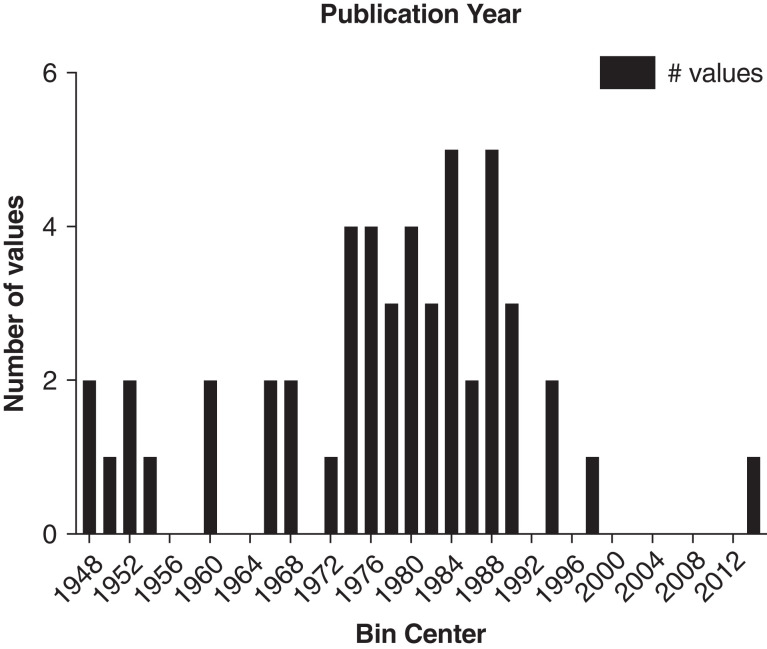
sCr methods have changed over the 67 years that the study encompasses, from the original Jaffe method to kinetic Jaffe, and then to isotope dilution mass spectrometry (IDMS) traceable enzymatic sCr. The older Jaffe method is more susceptible to interfering substances, including chromogens such as bilirubin and medications such as cephalosporins and dopamine.6 Therefore, enzymatic IDMS-traceable creatinine is the preferred method for neonates because of its reduced interference.6 In a study of 529 paired observations, 72% of measurements were discordant.7 As Figure 1 shows, only one study involved IDMS traceable creatinine and the majority of measurements would have used the Jaffe method. Moreover, sCr concentrations are sometimes as low as 10 µmol/L in neonates. Although both methods have the same limit of detection (10 µmol/L), the older Jaffe method has a much higher limit of quantitation, which results in much better performance of the enzymatic method at low creatinine levels.7
Figure 1.
Publications included in the study by Smeets et al. by year of publication. IDMS-traceable enzymatic creatinine would not have been available in any of the earlier studies.
Inclusion of 268 individual or aggregated inulin clearance studies provides considerable strength to the study. The authors also point out that mGFR on the basis of creatinine clearance did not differ in terms of postnatal age when compared with mGFR with exogenous markers. Their main finding was that mGFR doubled within the first 5 days of age from 19.6 (95% confidence interval, 14.7 to 24.6) ml/min per 1.73 m2 to 40.6 (95% confidence interval, 36.7 to 44.5) ml/min per 1.73 m2, and then rose more slowly to 59.4 (95% confidence interval, 45.9 to 72.9) ml/min per 1.73 m2 at 4 weeks of age. The undersigned believe that establishing the confidence intervals for renal function on the basis of mGFR is the most important finding by Smeets et al.5 and removes some of the uncertainties of small studies.
The second objective of the study by Smeets et al. was to optimize neonatal sCr-based GFR estimation in clinical care, introducing a new constant for the Schwartz bedside formula (constant*height/sCr ratio) of 0.31, using imperial units or 26.5 using the International System of Units (SI),5 replacing the constant of 0.45 from 1987. However, more work is necessary to evaluate this proposed new constant with appropriate enzymatic sCR measurements. Further limitations include the fact that the actual height was not measured in several newborns, but rather imputed, introducing another source of bias.
The Creatinine Enigma in the Neonatal Period
The shortcomings of sCr for the assessment of neonatal renal function have been reviewed extensively.1 sCr freely crosses the placenta and, for ≥72 hours, reflects maternal sCr.2 When using sCr to measure endogenous creatinine clearance, the clearance should be in steady state, because disagreement can arise in the nonsteady state.8 Therefore, sCr, even when used for creatinine clearance, is not a reliable marker of mGFR, especially not in the first few days of life.4
The Emerging Role of CysC
Low molecular weight markers of kidney function may be preferable.1 CysC is becoming more widely available and may be the endogenous marker of choice for estimating neonatal kidney function, but studies against gold-standard mGFR in neonates remain elusive. However, although assay variations are not as profound as with creatinine, they do exist, albeit the introduction of certified reference materials has improved the variability.1
Future Research
Smeets et al. have made a valuable contribution. Their studies establish normal mGFR values by postnatal day of life on the basis of a meta-analysis of individual and aggregated clearance data, including inulin clearance. The combined data remove some of the uncertainties of the previous small studies. The similar approach with the inclusion of several mGFR methods for the CKD Epidemiology Collaboration (CKD-EPI) formula, which sets the standard for estimation of GFR in adults, is a strength. However, mostly due to the methodological aspects of creatinine measurements over time and despite several (small) studies into measurement/estimation of GFR in the neonate, we still need new prospective neonatal studies using gold-standard mGFR methods1 against IDMS traceable enzymatic sCr and cysC. For children aged >18 months, adolescents, and young adults under age 25, the U25 formula by Pierce is recommended using both sCr and cys.9 The reason for not using the CKD-EPI in young adults is the poor agreement between a height creatinine ratio and CKD-EPI, and because <30 participants under 30 were in the CKD-EPI study.10 Beyond age 25, the CKD-EPI formula is recommended, again using both sCr and cysC.
The ability to accurately estimate eGFR in neonates and infants needs to be established. This is particularly important because of the high prevalence of AKI in the neonatal period and the long-term legacy of early nephron loss in life. The best estimator of neonatal kidney function clearly needs to be determined: sCr, cysC, or the combination.
Disclosures
G. Filler reports having consultancy agreements with Alnylam, Horizon, ProKidney, and Ultragenyx; reports receiving honoraria from and having an advisory or leadership role with Alnylam, Horizon, and Ultragenyx. All remaining authors have nothing to disclose.
Funding
None.
Acknowledgements
The authors thank Dr. Maria Esther Díaz-González de Ferris, MD, PhD MPH, for her extensive editing of the manuscript.
Footnotes
Published online ahead of print. Publication date available at www.jasn.org.
See related article, “Maturation of GFR in Term-Born Neonates: An Individual Participant Data Meta-Analysis,” on pages 1277–1292.
Author Contributions
J. Exantus and G. Filler conceptualized the study, and were responsible for the methodology and resources; G. Filler was responsible for the software and validation, provided supervision, and wrote the original draft; A. Sharma was responsible for the project administration; and J. Exantus, G. Filler, and A. Sharma reviewed and edited the manuscript.
References
- 1.Filler G, Ferris M, Gattineni J: Assessment of Kidney Function in Children, Adolescents, and Young Adults. In: Pediatric Nephrology, edited by Emma F, Goldstein S, Bagga A, Bates CM, Shroff R, Heidelberg, Springer, Berlin, 2021, 10.1007/978-3-642-27843-3_87-1 [DOI] [Google Scholar]
- 2.Bariciak E, Yasin A, Harrold J, Walker M, Lepage N, Filler G: Preliminary reference intervals for cystatin C and beta-trace protein in preterm and term neonates. Clin Biochem 44: 1156–1159, 2011 [DOI] [PubMed] [Google Scholar]
- 3.Filler G, Lopes L, Harrold J, Bariciak E: β-trace protein may be a more suitable marker of neonatal renal function. Clin Nephrol 81: 269–276, 2014 [DOI] [PubMed] [Google Scholar]
- 4.Kastl JT: Renal function in the fetus and neonate - the creatinine enigma. Semin Fetal Neonatal Med 22: 83–89, 2017 [DOI] [PubMed] [Google Scholar]
- 5.Smeets N, IntHout J, van der Burgh M, Schwartz G, Schreuder MF, de Wildt SN: Maturation of glomerular filtration rate in term-born neonates: An individual participant data meta-analysis [published online ahead of print]. J Am Soc Nephrol 2022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Allegaert K, Pauwels S, Smits A, Crevecoeur K, van den Anker J, Mekahli D, Vermeersch P: Enzymatic isotope dilution mass spectrometry (IDMS) traceable serum creatinine is preferable over Jaffe in neonates and young infants. Clinical Chem Lab Medic 52: e107–109, 2014. [DOI] [PubMed] [Google Scholar]
- 7.Schmidt RL, Straseski JA, Raphael KL, Adams AH, Lehman CM: A risk assessment of the Jaffe vs Enzymatic Method for creatinine measurement in an outpatient population. PLoS One 10: e0143205, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chen S, Chiaramonte R: Estimating creatinine clearance in the nonsteady state: The determination and role of the true average creatinine concentration. Kidney Med 1: 207–216, 2019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Pierce CB, Muñoz A, Ng DK, Warady BA, Furth SL, Schwartz GJ: Age- and sex-dependent clinical equations to estimate glomerular filtration rates in children and young adults with chronic kidney disease. Kidney Int 99: 948–956, 2021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Webster-Clark M, Jaeger B, Zhong Y, Filler G, Alvarez-Elias A, Franceschini N, et al. : Low agreement between modified-Schwartz and CKD-EPI eGFR in young adults: A retrospective longitudinal cohort study. BMC Nephrol 19: 194, 2018 [DOI] [PMC free article] [PubMed] [Google Scholar]