Abstract
The objective of this review was to quantify the association between diabetes, hyperglycemia, and outcomes in patients hospitalized for community-acquired pneumonia (CAP) prior to the COVID-19 pandemic by conducting a systematic review and meta-analysis. Two investigators independently screened records identified in the PubMed (MEDLINE), EMBASE, CINAHL, and Web of Science databases. Cohort and case–control studies quantitatively evaluating associations between diabetes and in-hospital hyperglycemia with outcomes in adults admitted to hospital with CAP were included. Quality was assessed using the Newcastle-Ottawa Quality Assessment Scale, effect size using random-effects models, and heterogeneity using I2 statistics. Thirty-eight studies met the inclusion criteria. Hyperglycemia was associated with in-hospital mortality (adjusted OR 1.28, 95% CI 1.09 to 1.50) and intensive care unit (ICU) admission (crude OR 1.82, 95% CI 1.17 to 2.84). There was no association between diabetes status and in-hospital mortality (adjusted OR 1.04, 95% CI 0.72 to 1.51), 30-day mortality (adjusted OR 1.13, 95% CI 0.77 to 1.67), or ICU admission (crude OR 1.91, 95% CI 0.74 to 4.95). Diabetes was associated with increased mortality in all studies reporting >90-day postdischarge mortality and with longer length of stay only for studies reporting crude (OR 1.50, 95% CI 1.11 to 2.01) results. In adults hospitalized with CAP, in-hospital hyperglycemia but not diabetes alone is associated with increased in-hospital mortality and ICU admission. Diabetes status is associated with increased >90-day postdischarge mortality. Implications for management are that in-hospital hyperglycemia carries a greater risk for in-hospital morbidity and mortality than diabetes alone in patients admitted with non-COVID-19 CAP. Evaluation of strategies enabling timely and effective management of in-hospital hyperglycemia in CAP is warranted.
Keywords: diabetes mellitus, type 2; infections; hospitalization; hyperglycemia
Introduction
Diabetes mellitus increases the risk of developing multisystem complications predominantly through hyperglycemia-mediated adverse effects on the vasculature, immune system, and end organs. Among these complications is an increased risk of infections1 contributing to an increased frequency of hospitalization for infectious diseases in people with diabetes.2 Community-acquired pneumonia (CAP) contributes significantly to the burden of infection-related hospitalization, with significant consequential healthcare expenditure.3 As the prevalence of diabetes continues to increase, it is expected that hospitalizations due to CAP will also increase.4 Better understanding and quantification of the morbidity and mortality of patients with diabetes requiring hospitalization for CAP might alleviate the burden of diabetes on communities and healthcare systems.
While several studies have considered the relationship between diabetes and CAP, contextual and temporal heterogeneities prevent estimations of the contribution of diabetes to CAP morbidity and mortality in hospitalized patients. Given the marked discrepancies between clinical definitions employed in prior studies, it is also unclear on a prima facie basis what proportion of diabetes-related morbidity in CAP can be attributed to inpatient hyperglycemia, an important distinction given that this may be a potentially modifiable risk factor. Furthermore, hyperglycemia in the absence of diagnosed diabetes as a contributor to CAP hospital outcomes is seldom reported and thus incompletely understood.
Since the onset of the COVID-19 pandemic, multiple studies considering the relationship between diabetes, glycemia, COVID-19 infection, and pneumonia have been published. Both diabetes and new hyperglycemia have been associated with increased risk of adverse outcomes in patients hospitalized with COVID-19 in international cohorts (although not universally), with ORs for mortality conferred by pre-existing diabetes ranging from 1.49 to 3.64.5–9 The increased morbidity and mortality conferred by hyperglycemia independent of the contribution of diabetes are less well characterized. One study found hyperglycemia in those without previously diagnosed diabetes to confer an HR of 5.38 (95% CI 3.46 to 8.35) for intensive care unit (ICU) admission compared with those without hyperglycemia or diabetes.8
During the COVID-19 pandemic, there was a reduction in non-COVID-19 CAP, likely through infection control measures such as mask wearing and social distancing reducing CAP of viral etiology.10 11 Bacterial etiologies were thought to have remained largely unaffected by these measures. However, as rising vaccination rates and public health measures begin to reduce the burden and severity of COVID-19 infections leading to hospitalization, and non-vaccine infection control measures are relaxed, endemic causes of CAP may re-emerge as precipitants of hospitalization for those with CAP. In this context, prepandemic data establishing the associations between diabetes and hyperglycemia with CAP outcomes will again become relevant. We therefore conducted a systematic review and meta-analysis to determine the impact of both diabetes alone and of hyperglycemia on outcomes in hospitalized patients with CAP.
Methods
This review was conducted according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) and the Meta-analysis of Observational Studies in Epidemiology (MOOSE) guidelines for design, conduct, and reporting.12 13 The review protocol was not registered.
Eligibility criteria
This review sought published studies that quantitatively assessed associations between both ‘diabetes’ and ‘in-hospital hyperglycaemia’ on outcomes in adults admitted to hospital with CAP. Outcomes considered included mortality, length of stay, and ICU admission. Cohort studies and case-control studies were eligible while case reports and series were excluded. Cross-sectional studies also were excluded due to uncertain temporal relationships between exposures and outcomes. Included studies assessed participants aged 18 years or older, as the management of pneumonia in children and young adolescents differs from that in adults. Eligible studies were reported in English, with full text available.
Definitions
Standard definitions of CAP included either a clinical diagnosis comprising clinical features and consistent radiological findings, with onset prior to or within 48 hours of hospitalization in the absence of recent inpatient healthcare contact, or discharge coding consistent with CAP. Standard definitions of diabetes mellitus included treatment with glucose-lowering medications, biochemical diagnosis consistent with prevalent guidelines, discharge coding, and patient self-report. It should be noted that there are issues with each of these definitions, for example, treatment with glucose-lowering medications may be instituted for conditions other than diabetes including pre-diabetes, while patient self-report is subject to recall bias. However, few studies use only a single definition. Given the marked heterogeneity in definitions of hyperglycemia, included definitions were glucose concentrations of 7.0 mmol/L (126 mg/dL) or greater. Studies of admitted patients with hyperglycemia were included regardless of whether participants had or did not have a diagnosis of diabetes.
Search strategy and data sources
The following databases were searched from inception (1950) to 4 June 2019: PubMed (MEDLINE), EMBASE, CINAHL, and Web of Science. MeSH and free-text terms were used to search PubMed. We searched for the MeSH headings ‘Pneumonia’, ‘Diabetes Mellitus’, ‘Hyperglycemia’ and the text strings ‘pneumoni*’, ‘diabet*’, ‘hyperglyc*’. MeSH headings were exploded and text strings were searched for in titles, abstracts, subject headings, and keyword headings. EMTREE and free-text terms were used to search EMBASE. Free-text terms were used to search CINAHL and Web of Science. The strategies sought publications referring to both pneumonia and either diabetes mellitus or hyperglycemia, or derivations thereof.
Study selection
Title and abstract screening was performed independently by two investigators (RDB, NC), who then reviewed full-text publications. Review-specific eligibility forms were created in PRISMA-compliant review software (Covidence systematic review software, Veritas Health Innovation, Melbourne, Australia) for each step of the review process with forms available on request. Discordance was resolved by case review with both investigators seeking consensus and a third investigator (LJW) consulted when this was not achieved.
Data extraction
Publication data were extracted independently by two investigators (RDB, NC) who then performed simultaneous comparisons to verify the accuracy of extracted data. Extracted data included first author, journal citation, year of publication, study location, funding, study design, data source, duration, population characteristics, and study-specific data including: inclusion and exclusion criteria, definitions, measures of association, and statistical methods.
Quality assessment
Quality was assessed using the Newcastle-Ottawa Quality Assessment Scale (NOS)14 according to recommended procedures by two investigators (RDB, NC). Discordance was resolved by case review with both investigators seeking consensus and a third investigator consulted when this was not achieved. The NOS allocates a maximum of nine stars across three domains: participant selection (four stars); group comparability (two stars); and ascertainment of either the exposure or outcome (three stars). If any item is not reported, a zero score is applied. We classified study quality according to the study score into low (score 0–3), moderate (score 4–6) and high quality (score 7–9).
Data synthesis and analysis
Characteristics of included studies were described in multiple publication and data-related domains. Where equivalence of measures allowed, meta-analysis was performed. Crude and adjusted results were pooled separately. Crude data meta-analyses use the Mantel-Haenszel method and the DerSimonian-Laird random-effects model with Hartung-Knapp adjustment. Adjusted measures included were the most adjusted statistical model from each study (covariates vary and are described in online supplemental tables 2 and 3). Adjusted data meta-analyses use the inverse variance method and the DerSimonian-Laird random-effects model. Summary measures were reported as ORs. Heterogeneity was assessed with Higgins and Thompson’s I2.15
bmjdrc-2022-002880supp001.pdf (474.5KB, pdf)
To account for variability in definitions of hyperglycemia, published study data were categorized with data-derived cut-points. Category A was defined as a study-defined hyperglycemia cut-point of ≤7.8 mmol/L, category B as 7.9–11.0 mmol/L, category C as ≥11.1 mmol/L and category D as not defined. Where a study defined hyperglycemia as a range with an upper boundary and lower boundary, the lower boundary was used to define the category. Studies with multiple grades of definitions of hyperglycemia, for which outcome data were reported separately, were thus able to contribute data to more than one hyperglycemia category.
All statistical analyses were performed in R V.3.6.0 (R Project for Statistical Computing). Non-base packages used for the analyses included meta version 4.15-1 and metafor version 2.4-0.
Results
Study selection in PRISMA format is shown in figure 1 with 38 studies included: 36 cohort studies and 2 case–control studies. Study characteristics including NOS quality assessment summary score are described in online supplemental table 1. Studies were conducted in a variety of contexts with a mean duration of 4.8 years (median: 4.0 years, range: 0.3–15.5 years).
Figure 1.
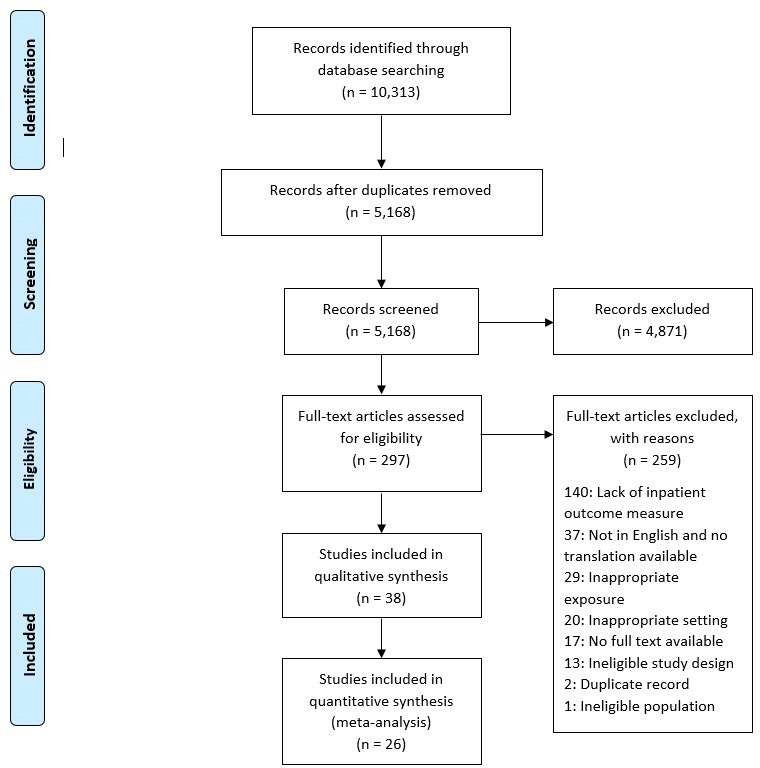
Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) flow diagram of study selection.
Diabetes studies
The relationship between diabetes status and CAP outcomes was reported in 31 studies. Study details are described in online supplemental table 2.
Mortality
Mortality was reported in various ways: in-hospital mortality was assessed in 14 studies, 30-day mortality in 10 studies, 90-day mortality in 1 study, 1-year mortality in 2 studies, and end-of-trial mortality in 4 studies.
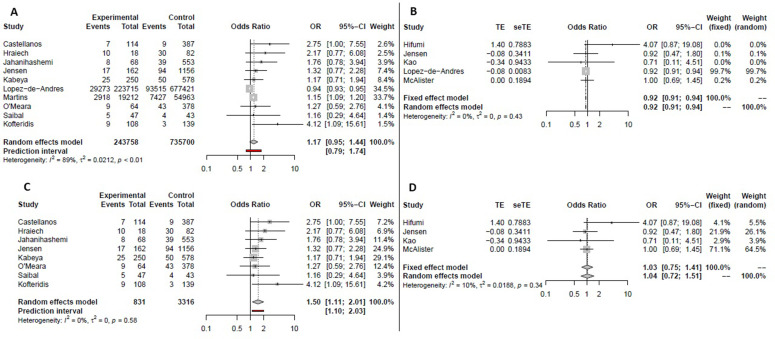
When considering all studies reporting in-hospital mortality there was no association shown for diabetes status. The pooled crude OR for in-hospital mortality with diabetes was 1.17 (95% CI 0.95 to 1.44, I2=89%) while the adjusted OR was 0.92 (95% CI 0.91 to 0.94, I2=0%) (figure 2A, B). Two studies used discharge coding data only to establish a diagnosis of diabetes. While this is a valid definition of diabetes it is likely to identify fewer and a substantively different subset of patients to clinical definitions, especially in more contemporary data sets,16 17 which can affect comparisons between studies using coding or clinical definitions. These studies also contributed the largest numbers of patients to the analyses. To explore their contributions to the results, analyses were repeated with these two studies removed. Meta-analysis of the remaining studies yielded both an increased crude OR of 1.50 (95% CI 1.11 to 2.01, I2=0%) and an increased adjusted OR of 1.04 (95% CI 0.72 to 1.51, I2=10%) (figure 2C, D).
Figure 2.
Meta-analyses of the association between diabetes and in-hospital mortality in hospitalized patients with community-acquired pneumonia. Pooled crude (A) and adjusted (B) ORs including all eligible studies. Pooled analyses after removal of studies that used coding data only in establishing a diagnosis of diabetes for crude (C) and adjusted (D) ORs.
Diabetes status was not associated with 30-day mortality (pooled crude OR 1.37, 95% CI 0.92 to 2.04, I2=41%; pooled adjusted OR 1.13, 95% CI 0.77 to 1.67, I2=62%) (online supplemental figure S1). One study reported this outcome as an HR of 1.29 (95% CI 1.01 to 1.65, p<0.001) and was not included in the meta-analysis.18
Other mortality outcomes were reported in a manner or with frequency unsuitable for meta-analysis. Ninety-day mortality was found by one study to be associated with diabetes (HR 2.47, 95% CI 2.05 to 2.98, p<0.001)18 as was 1-year mortality (OR 2.13, 95% CI 1.28 to 3.54, p=0.00419 and HR 1.3, 95% CI 1.03 to 1.65, p=0.0220). An association between diabetes and end-of-trial mortality was found, with HR of 2.84 (95% CI 1.35 to 5.99, p=0.006),21 1.26 (95% CI 1.04 to 1.54, p=0.02),18 and a relative risk of 1.5 (95% CI 1.05 to 2.14, p=not reported) but was not quantified in a study that reported crude event numbers.22
ICU admission
ICU admissions were no different between those with and without diabetes. The pooled crude OR for this outcome in those with diabetes for the five studies reporting it was 1.91 (95% CI 0.74 to 4.95, I2=84%) (online supplemental figure S2, panel A). The OR for ICU admission in those with diabetes was elevated in two studies, and not significantly different in three studies.
Length of stay
Length of hospital stay was generally longer for those with diabetes. Variable reporting of summary measures and crude continuous data or significance testing alone notwithstanding, of the six studies that assessed this, five found a statistically significant longer length of stay in those with diabetes versus those without23–27 while the last found no difference.28 Two studies reported a test of difference, being an HR of 0.68 (95% CI 0.51 to 0.89) for discharge in patients with diabetes compared with those without25 and an incidence rate ratio for longer length of stay in patients with diabetes of 1.19 (95% CI 1.06 to 1.33).27
Clinical outcomes
There was no association between diabetes status and the development of pleural effusion with a pooled crude OR from the three studies that assessed this outcome of 2.91 (95% CI 0.17 to 48.5, I2=83%) (online supplemental figure S2, panel B).
In individual studies, diabetes was found to be associated with both cardiovascular events during follow-up (HR 1.92, 95% CI 1.18 to 3.14, p=0.009)22 and a lower likelihood of weaning from mechanical ventilation (OR 0.23, 95% CI 0.05 to 0.92, p=0.048).29
‘Complicated hospitalization’ and a ‘severe outcome’ were reported by five and three studies, respectively, with various definitions precluding meaningful meta-analysis. None of these showed a statistically significant association between diabetes and defined study outcomes.
Hyperglycemia studies
The relationship between hyperglycemia and pneumonia outcomes was reported in 17 studies. Study details are described in online supplemental table 3. One study was found to be a clear outlier in terms of effect size and its results were removed from the primary analyses reported.30 Analyses retaining this study are included in the online supplemental figures S5, S6 and S8. Of the 16 hyperglycemia studies, 12 included patients with and without diabetes, 2 were limited to patients with diabetes, while 2 only included patients without a diagnosis of diabetes.
Mortality
Similar to the studies assessing diabetes, mortality was reported in multiple ways: in-hospital mortality was assessed in seven studies, 30-day mortality in three studies, 90-day mortality in two studies, 1-year mortality in two studies, and end-of-trial mortality in one study.
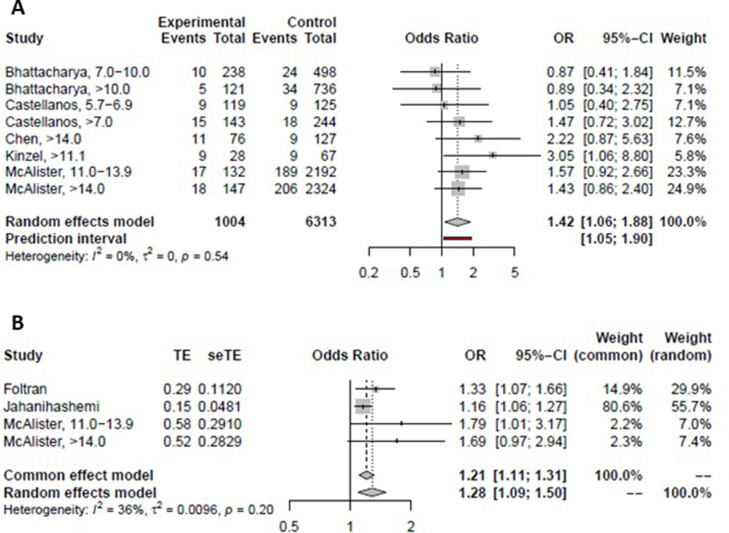
Hyperglycemia was associated with in-hospital mortality both for those studies reporting crude ORs (pooled crude OR 1.42, 95% CI 1.06 to 1.88, I2=0%) and adjusted ORs (pooled adjusted OR 1.28, 95% CI 1.09 to 1.50, I2=36%) (figure 3). When stratified by hyperglycemia cut-point categories using the mixed-effects model, there was no relationship seen between any individual cut-point category and in-hospital mortality point estimate for the crude OR. All but one category showed a relationship with in-hospital mortality for the adjusted OR; however, each category consisted of data from only a single study (online supplemental figure S3).
Figure 3.
Meta-analyses of the association between hyperglycemia and in-hospital mortality in hospitalized patients with community-acquired pneumonia. Pooled crude (A) and adjusted (B) ORs.
It is of interest to the clinician to differentiate the contribution of hyperglycemia to in-hospital mortality in patients with and without diabetes. Most studies31–35 included patients regardless of diabetes status and did not report the contribution of hyperglycemia to mortality separately in both of these groups. When studies including only patients with or without diabetes were excluded (relevant only to the pooled crude analysis), results were unchanged. The two studies to consider just patients with diabetes found hyperglycemia to not be associated with increased in-hospital mortality when hyperglycemia was defined as glucose >14.0 mmol/L (OR 2.22, 95% CI 0.87 to 5.63, p=0.18)36 or when risk was assessed per 1 mmol/L increase in glucose (OR 1.05, 95% CI 0.99 to 1.12, p=0.11).37 Similarly, both studies assessing the relationship between in-hospital mortality and hyperglycemia only in patients without diabetes found no association when hyperglycemia was defined as a glucose of ≥7.0 mmol/L (OR 1.98, 95% CI 0.32 to 12.4, p=0.46),38 or when assessing risk per 1 mmol/L increase in glucose (OR 1.10, 95% CI 0.99 to 1.23, p=0.09).37
Other mortality outcomes were reported in a manner unsuitable for meta-analysis. Hyperglycemia was not found to be associated with 30-day mortality in three studies,28 39 40 with 90-day mortality in one study,41 or with 1-year mortality in two studies.20 41 One study, the largest of the hyperglycemia-reporting studies, found 90-day mortality to be associated with an admission glucose of either 6.0–10.9, 11.0–13.9, or ≥14.0 mmol/L, with a progressively greater OR for each group respectively.18 Another study found new postprandial hyperglycemia in patients without diabetes to be associated with end-of-trial mortality (median surveillance duration of 5 years and 11 months) with an adjusted HR of 2.56 (95% CI 1.04 to 6.32).21
ICU admission
Three studies reported ICU admission, which was found to be associated with hyperglycemia (pooled crude OR 1.82, 95% CI 1.17 to 2.84, I2=16%) (online supplemental figure S4). In general, a higher glucose was associated with a greater OR of ICU admission, but this was not universally reported. One additional study found an association with hyperglycemia ≥11.1 mmol/L and ICU admission in those without diabetes,37 while another found none.40
Length of stay
Length of hospital stay was either longer or no different in those with hyperglycemia compared with those without. Of the six studies reporting this outcome, three found a statistically significant longer length of stay in those with hyperglycemia compared with those without,32 36 42 while the others reported no difference.31 33 38 The combination of summary measures and crude continuous data precluded meta-analysis.
Clinical outcomes
‘Complicated hospitalization’ was reported by three studies and variably defined. One study found hyperglycemia ≥14.0 mmol/L in patients with diabetes to be associated with complicated hospitalization, defined as a composite of 11 outcomes including in-hospital mortality.36 Another showed an association with hyperglycemia ≥11.0 mmol/L regardless of diabetes status, where complicated hospitalization was defined all inclusively as death, any non-metabolic complications, cardiac complications, and nosocomial infections.33 A third found complicated hospitalization, defined as an increase in oxygen requirements after 24 hours of admission or broadened antibiotic coverage, to be associated with glucose values >5.7 mmol/L in those without diabetes, but only for participants aged ≥65 years.38
A ‘severe outcome’ of the hospitalization was reported by three studies, with some definitions including mortality. Two studies found hyperglycemia to be associated with a severe outcome regardless of diabetes status for glucose values ≥11.1 mmol/L.37 40 A further study only found hyperglycemia of 5.7–6.9 mmol/L in those without diabetes and aged ≥65 years to be associated with a severe outcome, but in that same subset there was no association for hyperglycemia >7.0 mmol/L.38
Study quality and publication bias
Included studies were generally of high quality (7–9 points) on the NOS with two of moderate quality.
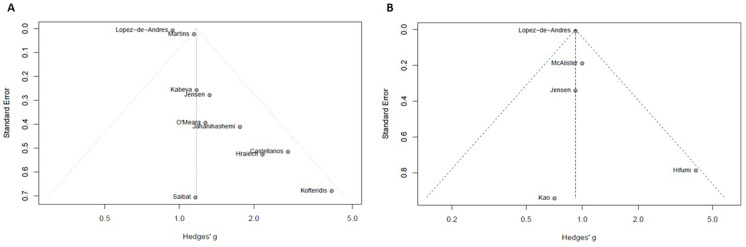
Funnel plots for the studies contributing data to the meta-analyses of in-hospital mortality, the most commonly reported outcome of pneumonia hospitalization, revealed significant publication bias for studies associating this outcome with both diabetes (figure 4) and hyperglycemia (online supplemental figure S7). Small studies (higher SE) with a small effect size (lower Hedges’ g) were missing in both cases. On the basis of clear outlier status in terms of effect size, one study reporting on hyperglycemia and pneumonia outcomes was removed (online supplemental figure S9).30
Figure 4.
Funnel plots of the association between diabetes and in-hospital mortality in hospitalized patients with community-acquired pneumonia for studies reporting crude (A) and adjusted (B) ORs.
Inter-rater reliability
For title and abstract screening, proportionate agreement between investigators was 0.94, random agreement 0.87, and Cohen’s kappa 0.56. For full-text review, proportionate agreement was 0.89, random agreement 0.73, and Cohen’s kappa 0.61.
Conclusions
While there is a clear pathological relationship between diabetes, hyperglycemia, and infection risk, patient and health service impacts of infection in diabetes and hyperglycemia are not well understood. Our review clarifies the nature of these relationships in a pre-COVID-19 pandemic context and identifies hyperglycemia as a stronger risk factor than diabetes for poor in-hospital outcomes in those admitted with CAP although diabetes is a greater risk factor for postdischarge mortality.
Individual studies revealed length of stay to be either no different or longer with both the presence of diabetes alone and with hyperglycemia. For both ICU admission and in-hospital mortality, however, on meta-analysis there appears to be a clear increase in risk associated with hyperglycemia but not with diabetes status. It is thus probable that hyperglycemia, at least in part, mediates the increased in-hospital mortality seen with diabetes in some individual studies assessing diabetes and mortality, especially as in-hospital hyperglycemia was reported in fewer than one-third of these studies. Indeed, the one study that reported adjusted ORs for both diabetes and hyperglycemia with in-hospital mortality found hyperglycemia but not diabetes to carry increased risk. Similarly, risks for composite outcomes termed complicated hospitalization and severe outcome, though variably defined, were universally increased with hyperglycemia but unchanged with diabetes status. These findings concur with the long-established increased risk for in-hospital adverse outcomes attributable to hyperglycemia in both those with and without diabetes.43 44
In contrast, postdischarge mortality outcomes were more strongly associated with diabetes than hyperglycemia, although heterogeneity precluded quantification of these effects through meta-analysis. For mortality reported as ≥90 days after discharge, diabetes was universally associated with increased risk in the six evaluable studies. In contrast, only two of five studies found hyperglycemia to increase the risk of ≥90-day mortality and in one of these studies it was new hyperglycemia in patients without previously diagnosed diabetes that was considered, which could thus represent diabetes newly detected during the admission for pneumonia. By 90 days after discharge, it is likely that any complications resulting from admission have been experienced and the risk of adversity stemming from hospitalization, amplified by acute hyperglycemia or not, has largely returned to baseline. These results are consistent with the known contribution of diabetes to mortality risk in ambulatory settings.45
The clear implications of these findings to clinicians managing adults hospitalized with pneumonia are that hyperglycemia during the hospital stay is a greater risk factor for in-hospital morbidity and mortality than diabetes status alone. Hyperglycemia is mechanistically linked to infection through immune dysfunction at multiple levels including impaired cytokine production,46 pathogen recognition,47 neutrophil function,48 and macrophage function.49 There is also long-standing evidence that in-hospital hyperglycemia is associated with a greater in-hospital mortality risk than diabetes.44 Our findings thus suggest that the effects of acute hyperglycemia are more important over the course of a hospital admission than the non-glycemic effects of the chronic condition of diabetes. These effects appear limited to the admission, however, and following discharge there does not appear to be a significant legacy effect of inpatient hyperglycemia, with medium-term outcomes such as mortality at ≥90 days associated to a greater degree with diabetes status.
This is noteworthy as while diabetes itself is not modifiable over the course of a hospital admission, hyperglycemia is. In patients admitted with CAP, outcomes may therefore potentially be improved through the identification and timely management of elevated plasma glucose concentrations, consistent with general hospital glucose management guidelines.50 A trial published in 2019 of proactive care to improve inpatient glycemia in the non-critical care setting showed reduced hyperglycemia and hospital-acquired infections, including pneumonia, in the intervention arm.51 The same intervention applied to adults hospitalized with pneumonia could similarly improve outcomes and is worthy of study, particularly to determine optimal glucose levels for prevention of CAP-related morbidity and mortality in admitted patients. This is especially important in our current context of different glycemic targets being recommended by different international groups.52 53
Methodological strengths of this review include a comprehensive search strategy and good inter-rater reliability suggesting consistent application of criteria. That the studies meeting the inclusion criteria were predominantly of high quality and represented a wide selection of geographic and temporal contexts is a further strength and confirms the reliability and broad applicability of the review findings. This review is limited by the observational nature of the source studies, which are by design necessarily susceptible to bias and confounding. Definitional heterogeneity of both diabetes and hyperglycemia is a source of error that is partially but not completely accounted for using random-effects model meta-analysis. Similarly, the reporting of different outcomes of CAP hospitalization resulted in a few data points for each, precluding meta-analysis for some outcomes. While it would be of interest to clinicians to differentiate the contribution of hyperglycemia to in-hospital mortality in patients with and without diabetes, most studies reporting on hyperglycemia outcomes pooled patients with and without diabetes and did not report on these associations separately. The presence of publication bias, as evidenced by the relative paucity of small studies with small effect size, may also impact on the strength of any conclusions drawn.
Future observational studies could improve the current state of knowledge summarized in this review by adopting standardized definitions for both hyperglycemia in patients admitted to hospital and clinical outcomes, which will enable direct comparisons between published studies. Studies considering the contribution of hyperglycemia to outcomes should additionally separately report on the effects of hyperglycemia on risk in patients with and without diabetes. Findings of our review highlight the need to evaluate whether early identification and treatment of hyperglycemia in individuals hospitalized with CAP can improve patient outcomes. Such an approach has shown promise for improved outcomes in a general population in a trial context.51 Future interventional studies, including randomized controlled trials, assessing the relationships between diabetes, hyperglycemia and CAP, offer the possibility of establishing euglycemia as a target for therapy, alongside appropriate antimicrobial therapy, as standardized treatment of CAP in hospitalized patients.
Footnotes
Contributors: RDB, NC, SF, and LJW conceived the study and wrote the research protocol. RDB and NC performed the search, study selection, data extraction, and quality assessment. RDB performed the data synthesis and statistical analysis. RDB and LJW wrote the initial manuscript. NC, SF, PBG, and PGC reviewed and edited the manuscript and contributed to the discussion. All authors reviewed the final manuscript and approved it for submission.
Funding: RDB was supported by the Australian Government Research Training Program Scholarship.
Disclaimer: The funders had no role in the study design, recruitment, data collection, analysis, interpretation, or writing of the report.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
No data are available.
Ethics statements
Patient consent for publication
Not required.
References
- 1.Abu-Ashour W, Twells L, Valcour J, et al. The association between diabetes mellitus and incident infections: a systematic review and meta-analysis of observational studies. BMJ Open Diabetes Res Care 2017;5:e000336. 10.1136/bmjdrc-2016-000336 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Shah BR, Hux JE. Quantifying the risk of infectious diseases for people with diabetes. Diabetes Care 2003;26:510–3. 10.2337/diacare.26.2.510 [DOI] [PubMed] [Google Scholar]
- 3.Fry AM, Shay DK, Holman RC, et al. Trends in hospitalizations for pneumonia among persons aged 65 years or older in the United States, 1988-2002. JAMA 2005;294:2712–9. 10.1001/jama.294.21.2712 [DOI] [PubMed] [Google Scholar]
- 4.Korbel L, Spencer JD. Diabetes mellitus and infection: an evaluation of hospital utilization and management costs in the United States. J Diabetes Complications 2015;29:192–5. 10.1016/j.jdiacomp.2014.11.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Scheen AJ, Marre M, Thivolet C. Prognostic factors in patients with diabetes hospitalized for COVID-19: findings from the CORONADO study and other recent reports. Diabetes Metab 2020;46:265–71. 10.1016/j.diabet.2020.05.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cariou B, Hadjadj S, Wargny M, et al. Phenotypic characteristics and prognosis of inpatients with COVID-19 and diabetes: the CORONADO study. Diabetologia 2020;63:1500–15. 10.1007/s00125-020-05180-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Apicella M, Campopiano MC, Mantuano M, et al. COVID-19 in people with diabetes: understanding the reasons for worse outcomes. Lancet Diabetes Endocrinol 2020;8:782–92. 10.1016/S2213-8587(20)30238-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wang W, Chai Z, Cooper ME, et al. High fasting blood glucose level with unknown prior history of diabetes is associated with high risk of severe adverse COVID-19 outcome. Front Endocrinol 2021;12:791476. 10.3389/fendo.2021.791476 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bode B, Garrett V, Messler J, et al. Glycemic characteristics and clinical outcomes of COVID-19 patients hospitalized in the United States. J Diabetes Sci Technol 2020;14:813-821. 10.1177/1932296820924469 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Yamamoto T, Komiya K, Fujita N, et al. COVID-19 pandemic and the incidence of community-acquired pneumonia in elderly people. Respir Investig 2020;58:435–6. 10.1016/j.resinv.2020.09.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mandell LA, Zhanel GG, Rotstein C, et al. Community-acquired pneumonia in Canada during coronavirus disease 2019. Open Forum Infect Dis 2022;9:ofac043. 10.1093/ofid/ofac043 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Moher D, Liberati A, Tetzlaff J. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ Clinical research 2009;339:b2535. 10.1371/journal.pmed.1000097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Stroup DF, Berlin JA, Morton SC, et al. Meta-analysis of observational studies in epidemiology: a proposal for reporting. meta-analysis of observational studies in epidemiology (moose) group. JAMA 2000;283:2008–12. 10.1001/jama.283.15.2008 [DOI] [PubMed] [Google Scholar]
- 14.The Newcastle-Ottawa scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses, 2014. Available: http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp
- 15.Higgins JPT, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med 2002;21:1539–58. 10.1002/sim.1186 [DOI] [PubMed] [Google Scholar]
- 16.Campbell SE, Campbell MK, Grimshaw JM, et al. A systematic review of discharge coding accuracy. J Public Health Med 2001;23:205–11. 10.1093/pubmed/23.3.205 [DOI] [PubMed] [Google Scholar]
- 17.Burns EM, Rigby E, Mamidanna R, et al. Systematic review of discharge coding accuracy. J Public Health 2012;34:138–48. 10.1093/pubmed/fdr054 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lepper PM, Ott S, Nüesch E, et al. Serum glucose levels for predicting death in patients admitted to hospital for community acquired pneumonia: prospective cohort study. BMJ 2012;344:e3397. 10.1136/bmj.e3397 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Adamuz J, Viasus D, Jiménez-Martínez E, et al. Incidence, timing and risk factors associated with 1-year mortality after hospitalization for community-acquired pneumonia. J Infect 2014;68:534–41. 10.1016/j.jinf.2014.02.006 [DOI] [PubMed] [Google Scholar]
- 20.Yende S, van der Poll T, Lee M, et al. The influence of pre-existing diabetes mellitus on the host immune response and outcome of pneumonia: analysis of two multicentre cohort studies. Thorax 2010;65:870–7. 10.1136/thx.2010.136317 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Koskela HO, Salonen PH, Romppanen J, et al. Long-term mortality after community-acquired pneumonia-impacts of diabetes and newly discovered hyperglycaemia: a prospective, observational cohort study. BMJ Open 2014;4:e005715. 10.1136/bmjopen-2014-005715 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Cangemi R, Calvieri C, Falcone M, et al. Relation of cardiac complications in the early phase of community-acquired pneumonia to long-term mortality and cardiovascular events. Am J Cardiol 2015;116:647–51. 10.1016/j.amjcard.2015.05.028 [DOI] [PubMed] [Google Scholar]
- 23.Martins M, Boavida JM, Raposo JF, et al. Diabetes hinders community-acquired pneumonia outcomes in hospitalized patients. BMJ Open Diabetes Res Care 2016;4:e000181. 10.1136/bmjdrc-2015-000181 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Saibal MAA, Rahman SHZ, Nishat L, et al. Community acquired pneumonia in diabetic and non-diabetic hospitalized patients: presentation, causative pathogens and outcome. Bangladesh Med Res Counc Bull 2012;38:98–103. 10.3329/bmrcb.v38i3.14336 [DOI] [PubMed] [Google Scholar]
- 25.Suter-Widmer I, Christ-Crain M, Zimmerli W, et al. Predictors for length of hospital stay in patients with community-acquired pneumonia: results from a Swiss multicenter study. BMC Pulm Med 2012;12:21. 10.1186/1471-2466-12-21 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kofteridis DP, Giourgouli G, Plataki MN, et al. Community-acquired pneumonia in elderly adults with type 2 diabetes mellitus. J Am Geriatr Soc 2016;64:649–51. 10.1111/jgs.14011 [DOI] [PubMed] [Google Scholar]
- 27.Kabeya Y, Shimada A, Tsukada N, et al. Diabetes affects length of stay and hospital costs for elderly patients with pneumonia: an analysis of a hospital administrative database. Tokai J Exp Clin Med 2016;41:203–9. [PubMed] [Google Scholar]
- 28.Di Yacovo S, Garcia-Vidal C, Viasus D, et al. Clinical features, etiology, and outcomes of community-acquired pneumonia in patients with diabetes mellitus. Medicine 2013;92:42–50. 10.1097/MD.0b013e31827f602a [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Falguera M, Pifarre R, Martin A, et al. Etiology and outcome of community-acquired pneumonia in patients with diabetes mellitus. Chest 2005;128:3233–9. 10.1378/chest.128.5.3233 [DOI] [PubMed] [Google Scholar]
- 30.Iroezindu MO, Isiguzo GC, Chima EI, et al. Predictors of in-hospital mortality and length of stay in community-acquired pneumonia: a 5-year multi-centre case control study of adults in a developing country. Trans R Soc Trop Med Hyg 2016;110:445–55. 10.1093/trstmh/trw057 [DOI] [PubMed] [Google Scholar]
- 31.Bhattacharya RK, Mahnken JD, Rigler SK. Impact of admission blood glucose level on outcomes in community-acquired pneumonia in older adults. Int J Gen Med 2013;6:341–4. 10.2147/IJGM.S42854 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kinzel T, Smith M. Hyperglycemia as a predictor for mortality in veterans with pneumonia. Exp Aging Res 1988;14:99–102. 10.1080/03610738808259730 [DOI] [PubMed] [Google Scholar]
- 33.McAlister FA, Majumdar SR, Blitz S, et al. The relation between hyperglycemia and outcomes in 2,471 patients admitted to the hospital with community-acquired pneumonia. Diabetes Care 2005;28:810–5. 10.2337/diacare.28.4.810 [DOI] [PubMed] [Google Scholar]
- 34.Foltran F, Gregori D, Caropreso A, et al. Is blood glucose on admission a predictor of mortality in adult acute pneumonia? Clin Respir J 2013;7:276–80. 10.1111/crj.12003 [DOI] [PubMed] [Google Scholar]
- 35.Jahanihashemi H, Babaie M, Bijani S, et al. Poverty as an independent risk factor for in-hospital mortality in community-acquired pneumonia: a study in a developing country population. Int J Clin Pract 2018;72:e13085. 10.1111/ijcp.13085 [DOI] [PubMed] [Google Scholar]
- 36.Chen P-C, Liao W-I, Wang Y-C, et al. An elevated glycemic gap is associated with adverse outcomes in diabetic patients with community-acquired pneumonia. Medicine 2015;94:e1456. 10.1097/MD.0000000000001456 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Jensen AV, Egelund GB, Andersen SB, et al. The impact of blood glucose on community-acquired pneumonia: a retrospective cohort study. ERJ Open Res 2017;3. 10.1183/23120541.00114-2016. [Epub ahead of print: 19 06 2017]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Castellanos MR, Szerszen A, Saifan C, et al. Fasting hyperglycemia upon hospital admission is associated with higher pneumonia complication rates among the elderly. Int Arch Med 2010;3:16. 10.1186/1755-7682-3-16 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Rueda AM, Ormond M, Gore M, et al. Hyperglycemia in diabetics and non-diabetics: effect on the risk for and severity of pneumococcal pneumonia. J Infect 2010;60:99–105. 10.1016/j.jinf.2009.12.003 [DOI] [PubMed] [Google Scholar]
- 40.Schuetz P, Friedli N, Grolimund E, et al. Effect of hyperglycaemia on inflammatory and stress responses and clinical outcome of pneumonia in non-critical-care inpatients: results from an observational cohort study. Diabetologia 2014;57:275–84. 10.1007/s00125-013-3112-9 [DOI] [PubMed] [Google Scholar]
- 41.Eurich DT, Gamble JM, Marrie TJ, et al. Dysglycaemia and 90 day and 1 year risks of death or readmission in patients hospitalised for community-acquired pneumonia. Diabetologia 2010;53:497–503. 10.1007/s00125-009-1598-y [DOI] [PubMed] [Google Scholar]
- 42.Godar DA, Kumar DR, Schmelzer KM, et al. The impact of serum glucose on clinical outcomes in patients hospitalized with community-acquired pneumonia. WMJ 2011;110:14–20. [PubMed] [Google Scholar]
- 43.Bruno A, Gregori D, Caropreso A, et al. Normal glucose values are associated with a lower risk of mortality in hospitalized patients. Diabetes Care 2008;31:2209–10. 10.2337/dc08-0672 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Umpierrez GE, Isaacs SD, Bazargan N, et al. Hyperglycemia: an independent marker of in-hospital mortality in patients with undiagnosed diabetes. J Clin Endocrinol Metab 2002;87:978–82. 10.1210/jcem.87.3.8341 [DOI] [PubMed] [Google Scholar]
- 45.Li S, Wang J, Zhang B, et al. Diabetes mellitus and cause-specific mortality: a population-based study. Diabetes Metab J 2019;43:319–41. 10.4093/dmj.2018.0060 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Reinhold D, Ansorge S, Schleicher ED. Elevated glucose levels stimulate transforming growth factor-beta 1 (TGF-beta 1), suppress interleukin IL-2, IL-6 and IL-10 production and DNA synthesis in peripheral blood mononuclear cells. Horm Metab Res 1996;28:267–70. 10.1055/s-2007-979789 [DOI] [PubMed] [Google Scholar]
- 47.Gupta S, Maratha A, Siednienko J, et al. Analysis of inflammatory cytokine and TLR expression levels in type 2 diabetes with complications. Sci Rep 2017;7:7633. 10.1038/s41598-017-07230-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Stegenga ME, van der Crabben SN, Blümer RME, et al. Hyperglycemia enhances coagulation and reduces neutrophil degranulation, whereas hyperinsulinemia inhibits fibrinolysis during human endotoxemia. Blood 2008;112:82–9. 10.1182/blood-2007-11-121723 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Restrepo BI, Twahirwa M, Rahbar MH, et al. Phagocytosis via complement or Fc-gamma receptors is compromised in monocytes from type 2 diabetes patients with chronic hyperglycemia. PLoS One 2014;9:e92977. 10.1371/journal.pone.0092977 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Pasquel FJ, Lansang MC, Dhatariya K, et al. Management of diabetes and hyperglycaemia in the hospital. Lancet Diabetes Endocrinol 2021;9:174–88. 10.1016/S2213-8587(20)30381-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Kyi M, Colman PG, Wraight PR, et al. Early intervention for diabetes in medical and surgical inpatients decreases hyperglycemia and hospital-acquired infections: a cluster randomized trial. Diabetes Care 2019;42:832-840. 10.2337/dc18-2342 [DOI] [PubMed] [Google Scholar]
- 52.American Diabetes Association . Diabetes Care in the Hospital: Standards of Medical Care in Diabetes-2020. Diabetes Care 2020;43:S193–202. 10.2337/dc20-S015 [DOI] [PubMed] [Google Scholar]
- 53. JBDS-IP. Management of hyperglycaemia and steroid (glucocorticoid) therapy, 2021. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjdrc-2022-002880supp001.pdf (474.5KB, pdf)
Data Availability Statement
No data are available.