Abstract
Background
The literature demonstrated a positive impact of medication therapy management (MTM) services provided by the pharmacists to improve the overall health outcomes. Nevertheless, limited data is available with regard to MTM service implementation by community pharmacists and its associated factors in Jordan.
Objective
To evaluate community pharmacists’ knowledge, attitude and practice of MTM service and to explore the challenges and barriers for its implementation.
Methods
The present cross-sectional study utilized a validated online survey which was filled by community pharmacists in different areas across Jordan. In addition to the socio-demographic variables, the study questionnaire evaluated pharmacists’ knowledge and attitudes towards MTM service, extent of MTM implementation and its associated challenges and barriers.
Results
A total of 250 pharmacists completed the survey. The study pharmacists showed moderate knowledge level (median of the total knowledge score = 6 (4–7) out of 10) and positive attitude (median of the attitude score was 23 (19–26) out of 30) towards MTM services. The participating pharmacists recognized performing or obtaining necessary assessments of patient’s health status as the most frequently provided MTM service (84.8%), while the least one was documenting the care delivered and communicating essential information to other healthcare providers (62%). Furthermore, collecting patient-related information was the most commonly recognized challenge to MTM service provision (36.8%), followed by referring the patient to a physician or consultant (36%) and collaboration with them (35.6%). The most reported barrier was negative physician attitudes (40.4%), followed by the lack of training on MTM provision (38.4%), and lack of adequate support staff (37.2%).
Conclusion
Efforts are needed to enhance collaboration between pharmacists and other health care professional, to develop documentation systems that would preserve and facilitate access to patient information, and to implement appropriate training programs which aim to overcome the challenges and barriers for MTM implementation.
Keywords: Medication therapy management, Pharmacists, Knowledge, Attitudes, Barriers, Jordan
1. Introduction
Medication therapy management (MTM) is defined as “a distinct service or group of services that optimize therapeutic outcomes for individual patients“ (McGivney et al. 2007). The MTM is a pharmacist-led service which involves medication therapy review (MTR), personal medication record, medication-related action plan (MAP), intervention or referral and documentation and follow-up (APhA and the NACDS 2008). MTM services were developed by the Medicare prescription drugs, improvement and Modernization Act of 2003 (MMA) (MacIntosh et al. 2009). The MMA recognized enhancing medication adherence, providing education on medication therapy and detecting any adverse drug reaction as the main goals of the MTM service. According to the Medicare part D report in January 2006 (Urmie et al., 2007, Touchette et al., 2006), MTM goals necessitate a collaboration between pharmacists, physicians and other healthcare providers (Pellegrino et al. 2009). Although MMA does not designate pharmacists as the primary providers of MTM services, many published studies suggested that community pharmacists are uniquely providers of MTM services (Group et al., 2005, Cranor and Christensen, 2003, Doucette et al., 2005, MacIntosh et al., 2009, Moczygemba et al., 2008). A study conducted by Touchette et al reported that almost all of the MTM services were provided by pharmacists (Touchette et al. 2006). Another cross-sectional survey showed high knowledge and positive attitudes toward MTM service by the participating pharmacists in Malaysia (Al-Tameemi and Sarriff 2019).
Although MTM implementation could improve the overall health outcomes, several barriers and challenges to the MTM were reported in previous studies. An American study reported that lack of time and lack of supporting pharmacists personnel were the most challenging barriers to providing MTM (Shah and Chawla 2011). Lack of time and trained personnel, in addition to limited reimbursement were also reported as barriers to MTM implementation in previous studies (Law et al., 2009, MacIntosh et al., 2009). The most frequently identified barriers to MTM in a Malaysian study were lack of training, need for high budget, and lack of time (Al-Tameemi and Sarriff 2019).
The literature demonstrated a positive impact of pharmacist-led MTM services on different health outcomes. Earlier studies reported improved medication adherence, reduction in hospital admissions, more identification of drug-related problems, and better clinical outcomes in patients with type 2 diabetes (Erku et al. 2017) and chronic obstructive pulmonary disease (Detoni et al. 2016) after receiving pharmacist-led MTM services. Other study showed significant improvement in blood pressure, blood glucose and lipid profile control following a pharmacist-led MTM service (De et al. 2016). Another observational study reported decreased therapeutic duplication, drug-drug interactions, and underuse of effective medication or having incorrect or unclear instructions for medication use after a pharmacist-led MTM services (SJ et al. 2014). Nevertheless, limited data is available to evaluate the awareness and implementation of MTM services in community pharmacies in Jordan. The present study is the first one to evaluate community pharmacists’ knowledge, practice and attitudes toward MTM service, in addition to the barriers and challenges they might face when implementing these services in Jordan. Findings of the present study could be utilized to improve pharmaceutical care and the health service provided for the patients in the community pharmacies.
2. Methods
2.1. Study subjects
The present cross-sectional study included an online survey, which was distributed via Facebook Messenger and WhatsApp applications using snowball sampling technique. The survey was completed by community pharmacists who work in independent, chain or hospital pharmacy setting. Inclusion criteria included pharmacists and pharmacy technicians who graduated from Jordanian Universities and other Universities recognized by the Ministry of Higher Education, and were authorized by the Ministry of Health and the Jordanian Pharmaceutical Association to practice as community pharmacists in Jordan. Those who had less than one year of work experience were excluded from the study.
2.2. Study instrument construct and validation
The survey included a short paragraph describing the study and its objectives, with emphasis on the right for not participating or not completing the study questionnaire. The survey questionnaire was conducted in English and consisted of six domains assessing socio-demographics, knowledge, attitudes, practice, challenges, and barriers for providing MTM services. A literature review of relevant published studies identified some studies and survey instruments which evaluated community pharmacists’ knowledge, attitudes, and practice of MTM service, in addition to the challenges and barriers associated with MTM implementation. The 10-item knowledge and the 6-item attitudes domains were adapted from an earlier validated questionnaire (Al-Tameemi and Sarriff 2019). The third section consisted of 8 items which evaluated pharmacists’ utilization of different MTM services. The 11-item challenges domain was adapted from Blake et al (Blake et al. 2009) and the 9-item barriers questionnaire was adapted from Al-Tameemi NK (Al-Tameemi and Sarriff 2019) and Blake et al (Blake et al. 2009). The 10-item knowledge domain consisted of two true/false and two multiple choice questions. Each correct answer scored 1 point, while wrong answer scored 0. Then a sum score was calculated for each participant with a minimum of “0″ to a maximum of “10. A 5-likert scale from strongly disagree to strongly agree was used for responses on attitude, challenges and barriers domains. The strongly disagree choice was scored 1 and strongly agree was scored 5 with a maximum possible score of 30 for attitude and 55 for challenges. Similarly, a 5-likert scale was used to evaluate MTM practice which ranged from never (1 point) to always (5 points) with a maximum possible score of 40. Finally, each domain was classified into high or low based on the median of the calculated scores. After combining the four parts together, the questionnaire was sent to four experts in clinical pharmacy and pharmaceutical care for face and content validity. Then the validated instrument was piloted on fifteen pharmacists who were asked to provide their feedback at the end of the survey and changes including rewording and rephrasing were implemented when appropriate.
2.3. Ethics
No patient or public involved in the study. The study received Ethical approval from the Institutional Review Board at Jordan University of Science and Technology (Ref. No. 12/123/2021).
2.4. Statistical analysis
The data was coded and analyzed using statistical package for the social sciences (SPSS) version 22. Kolmogorov–Smirnov test indicated that the data was not normally distributed. Therefore, categorical variables were expressed as frequencies and percentages, while continuous variables were expressed as medians and (25–75 quartiles). Descriptive statistics were used to describe pharmacists’ demographics, knowledge, attitudes, barriers, and challenges for MTM implementation in clinical practice. Spearman’s rank correlation was conducted to evaluate the correlations between knowledge, attitudes, barriers, and challenges scores. Quantile regressions with dummy variables were constructed to identify the variables associated with the four calculated scores. The quantile regression models included age, gender, material status, pharmacy practice settings, years in experience, education, and monthly income as predictors. A P value of < 0.05 was considered statistically significant.
3. Results
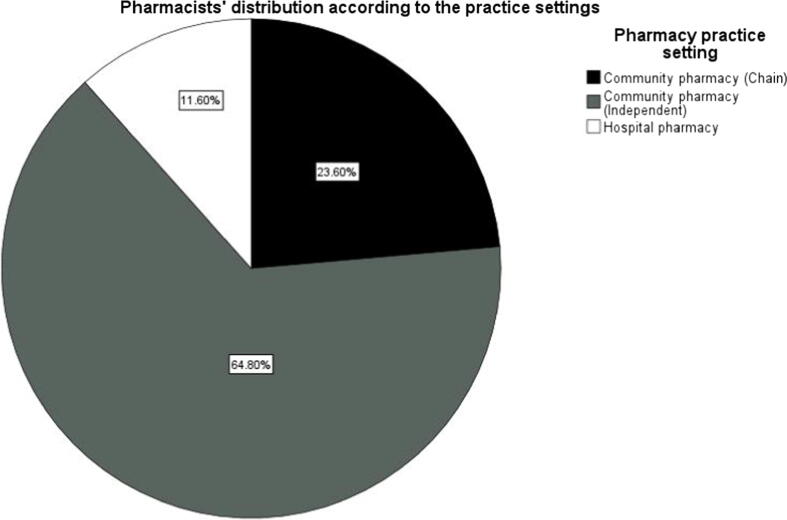
The study questionnaire was completed by 250 pharmacists from several hospitals and community pharmacies in different locations in Jordan. The median age of the participants was 26 (24–30) and ranged between 23 and 55 years. Most of the participants were females (n = 193;77.2%), with 1 to 5 years of experience (n = 184;73.6%), and had intermediate monthly income (n = 129;51.6%). Some of the participants were pharmacy technicians who had a Diploma degree in Pharmacy (n = 30;12%). Participants’ demographic characteristics are presented in Table 1, and pharmacists’ distribution according to pharmacy practice setting is shown in Fig. 1.
Table 1.
Pharmacists’ characteristics and demographics.
| Variables |
Median (25–75) Frequency (%) |
|
|---|---|---|
| Age | 26 (24–30) | |
| Gender |
Female | 193 (77.2%) |
| Male | 57 (22.8%) | |
| Marital status | Married | 92 (36.8%) |
| Single, divorced, separated, widowed | 158 (63.2%) | |
| Years in practice | 1–5 years | 184 (73.6%) |
| 6–10 years | 34 (13.6%) | |
| >10 years | 32 (12.8%) | |
| Education | Diploma | 30 (12.0%) |
| Bachelors of pharmacy | 169 (67.6%) | |
| PharmD* | 31 (12.4%) | |
| Master's or PhD* in Pharmacy | 20 (8.0%) | |
| Monthly income (JD*) | <300 | 87 (34.8%) |
| 300–600 | 129 (51.6%) | |
| >600 | 34 (13.6%) | |
JD: Jordanian Dinar, Pharm D: Doctor of pharmacy degree, PhD: Doctor of Philosophy degree.
Fig. 1.
Pharmacists’ distribution according to the pharmacy practice setting.
As shown in Table 2, the median of the total knowledge score was 6 (4–7) out of 10 indicating moderate knowledge level. The first question was about the elements of MTM services, the most identified elements by the pharmacist were medication therapy review (68%), followed by medication-related action plan (58.4%), while the least identified was documentation (29.2%). When asked about the goals of MTM, most of the pharmacists (n = 186;74.4%) recognized that improving patient outcomes is among the goals of MTM. However, only (n = 141;56.4%) of the pharmacists identified detection of medication-related problems as a goal. The majority of the pharmacists knew that MTM service can benefit any patient who is taking prescription or nonprescription medication (n = 216;86.4%), and that improving patients’ adherence and disease state management is a primary role of MTM service (n = 216;86.4%). Table 2 shows the knowledge of the participating pharmacists about MTM services.
Table 2.
Pharmacists’ knowledge about providing medication therapy management (MTM) services.
| Statements | Frequency (%) |
|---|---|
| The core element(s) of MTM service is/are: (You can select more than one answer) | |
| Documentation | 73 (29.2%) |
| Intervention | 81 (32.4%) |
| Medication-related action plan | 146 (58.4%) |
| Medication Therapy review | 170 (68%) |
| Personal medication record | 124 (49%) |
| Which of the following is/are the goals of medication therapy management services? (You can select more than one answer) | |
| Detection | 141 (56.4%) |
| Enhance | 159 (63.6%) |
| Improves | 186 (74.4%) |
| Any patient who uses prescription and nonprescription medication herbal products or other dietary Supplement could potentially benefit from MTM service? | |
| True | 216 (86.4% |
| primary role of MTM service is aid with adherence and disease state management | |
| True | 215 (86%) |
A shown in Table 3, the median of the attitude score was 23 (19–26) out of 30, indicating moderate attitude level. The most frequently agreed to sentence was “beside the processes of normal dispensing functions, reviewing patient’s medication profile and providing interventions are important roles of pharmacist to prevent adverse effects” (69.2%), while the least agreed with sentence was “providing MTM service is a unique opportunity for pharmacists to participate in patient care at a broader spectrum” (62%).
Table 3.
Pharmacists’ attitude toward medication therapy management (MTM) services.
| Attitude |
Agree/ Strongly agree Frequency (%) |
|---|---|
| Beside the processes of normal dispensing functions, reviewing patient’s medication profile and providing interventions are important roles of pharmacist to prevent adverse effects | 173 (69.2%) |
| By applying MTM service, patients would receive adequate and beneficial information about their chronic disease (s) and medication therapies from their providers | 168 (67.2%) |
| By considering the core elements of MTM service, do you agree that MTM service is valuable? | 156 (62.4%) |
| Patient’s health outcomes would be improved when medications are monitored by a pharmacist when compared to other health care providers | 152 (60.8%) |
| Applying MTM service requires more knowledge than basic information of pharmacy practice | 168 (67.2%) |
| Providing MTM service is a unique opportunity for pharmacists to participate in patient care at a broader spectrum | 155 (62.0%) |
As shown in Table 4, the median of the practice score was 24 (21–28) out of 40 indicating moderate level of practice. The most frequently provided service was performing or obtaining necessary assessments of the patient’s health status (84.8%) and the least was documenting the provided care and communicating essential information to other primary care providers (62%).
Table 4.
Pharmacists’ utilization of medication therapy management (MTM) services.
| MTM Service |
Always/Most of the times Frequency (%) |
|---|---|
| Performing or obtaining necessary assessments of the patient’s health status | 212 (84.8%) |
| Formulating a medication treatment plan | 171 (68.4%) |
| Selecting, initiating, modifying, or administering medication therapy | 183 (73.2%) |
| Monitoring and evaluating the patient’s response to therapy, including safety and effectiveness | 183 (73.2%) |
| Performing a comprehensive medication review to identify, resolve, and prevent medication-related problems, including adverse drug events | 188 (75.2%) |
| Documenting the care delivered and communicating essential information to the patient’s other primary care providers | 155 (62.0%) |
| Providing verbal education and training designed to enhance patient understanding and appropriate use of his/her medications | 192 (79.2%) |
| Providing information, support services, and resources designed to enhance patient adherence with his/her therapeutic regimens | 198 (69.2%) |
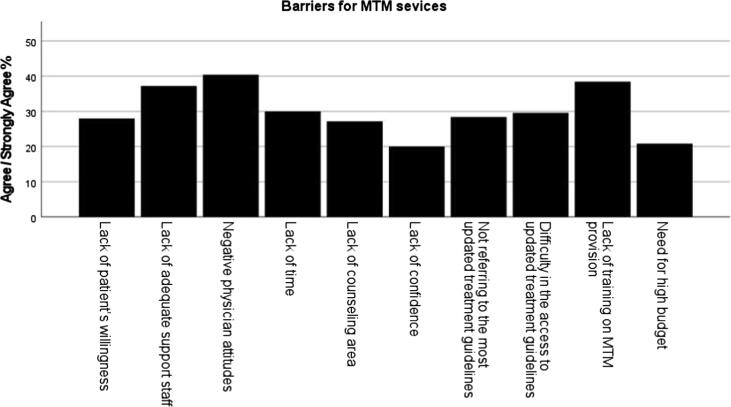
As shown in Table 5, the median of the challenges score was 33 (26–45) out of 55 indicating moderate level of challenges score. The most reported challenge was collecting patient-related information (36.8%), while providing drug related-information was the least reported challenge (25.2%). As shown in Fig. 2, the most reported barrier for MTM implementation was negative physician attitudes (40.4%), whereas, lack of confidence was the least reported barrier among the study participants (20%).
Table 5.
Challenges for providing medication therapy management (MTM) services.
| Challenge |
Agree/ Strongly agree Frequency (%) |
|---|---|
| Review medication profile for potential drug allergy, drug-drug interaction, and drug duplication | 80 (32.0%) |
| Providing drug related information | 63 (25.2%) |
| Collecting patient related information | 92 (36.8%) |
| Referring the patient to physician /consultant | 90 (36.0%) |
| Collaborating with physician /consultant | 89(35.6%) |
| Preparing medication action plan | 73 (29.2%) |
| Monitoring drug therapy effects | 86 (34.4%) |
| [Advising patients on monitoring drug therapy | 76 (30.4%) |
| Educating the patient on over-the-counter medication | 67 (26.8%) |
| Educating the patient on disease prevention | 72 (28.8%) |
| Educating the patient on disease state management | 71 (28.4%) |
Fig. 2.
Barriers for providing medication therapy management (MTM) services.
Spearman’s rank correlation showed positive significant association between knowledge score and both attitudes and challenges scores (r = 0.37, P < 0.01 and r = 0.22, P < 0.01 respectively), and a significant association between attitudes and challenges scores (r = 0.32, P < 0.01).
As shown in Table 6, results of quantile regression showed that age was positively associated with knowledge score (regression coefficient (B) = 0.12, 95 %CI: 0.052–0.187, P < 0.01). Low and moderate monthly income groups had significantly higher knowledge score than high monthly income group (B = 1.79, 95 %CI: 0.586–3.004, P < 0.01; B = 2.48, 95 %CI: 1.383–3.592, P < 0.01 respectively). Diploma holders had significantly less knowledge than masters and PhD holders (B = -2.3, 95 %CI: −3.705- −0.96, P < 0.01). Moreover, the results indicated that the participants who work in chain pharmacy or independent pharmacy had significantly less challenge score when compared with those who work in hospitals (B = -10.30, 95 %CI: −18.973- −1.64, P < 0.01; B = -8.34, 95 %CI: −16.287- −0.407, P < 0.01 respectively). Income level was also significantly associated with challenge score as the low and moderate monthly income groups had significantly higher challenge score than high monthly income group (B = 10.13, 95 %CI: 0.938–19.328, P < 0.01; B = 9.89, 95 %CI: 1.496–18.29, P < 0.01 respectively). Finally, Diploma holders had significantly less challenge score than Master and PhD holders (B = −11.38, 95 %CI: −21.818- −0.955, P < 0.01). The results showed no significant association between any of the studied variables and attitudes and practice scores.
Table 6.
Quantile regression results of the factors associated with knowledge and challenges scores.
|
Knowledge score | |||||
|---|---|---|---|---|---|
| Variable | Quantile regression coefficient (B) | P-value | 95% confidence interval (CI) |
||
| Lower | Upper | ||||
| Age | 0.12 | <0.01** | 0.052 | 0.187 | |
| Monthly income |
<300 JD* | 1.79 | <0.01** | 0.586 | 3.004 |
| 300–600 JD* | 2.48 | <0.01** | 1.383 | 3.592 | |
| >600 JD* | Reference | ||||
| Education degree | Diploma | −2.3 | <0.01** | −3.705 | −0.961 |
| Bachelor’s | −0.69 | 0.22 | −1.801 | 0.417 | |
| PharmD* | −0.41 | 0.544 | −1.740 | 0.919 | |
| Master or PhD* | Reference | ||||
| Challenges score | |||||
| Community pharmacy | Chain | −10.30 | <0.01** | −18.973 | −1.640 |
| Independent | −8.34 | <0.01** | −16.287 | −0.407 | |
| Hospital | Reference | ||||
| Monthly income | <300 JD* | 10.13 | <0.01** | 0.938 | 19.328 |
| 300–600 JD* | 9.89 | <0.01** | 1.496 | 18.290 | |
| >600 JD* | Reference | ||||
| Education degree | Diploma | −11.38 | <0.01** | −21.818 | −0.955 |
| Bachelor’s | −4.00 | 0.351 | −12.432 | 4.432 | |
| PharmD | −5.96 | 0.247 | −16.070 | 4.150 | |
| Master or PhD | Reference | ||||
JD: Jordanian dinar, Pharm D: Doctor of pharmacy degree, PhD: Doctor of Philosophy degree.
Significance at P < 0.01.
4. Discussion
Despite the availability of various medications to treat different conditions, an optimal therapeutic plan is needed to reach the best clinical outcomes. Since pharmacists are medication experts, it is necessary to investigate their knowledge, practice and attitudes (KAP) towards MTM and to explore the challenges and the barriers that can hamper the implementation of such service.
The study results indicated that the most identified elements of MTM were MTR, followed by MAP, while the least identified element was documentation. Consistent results were found in an earlier study where most of the pharmacists were confident in providing MTR, somewhat confident in developing MAP, but they disagreed about the availability of adequate documentation systems for MTM service (Moczygemba et al. 2008). A study was conducted in America showed that more than half of the pharmacy managers strongly agreed that annual personal medication review would improve patient outcomes (MacIntosh et al. 2009).
Similar to what previously reported (MacIntosh et al. 2009), the results of the current study showed that most of the pharmacists recognized that improving patient outcomes is among the goals of MTM. However, only half of them identified detection of medication-related problems as a goal of MTM. In comparison, almost all of pharmacists surveyed in a Malaysian study identified all goals of MTM (Al-Tameemi and Sarriff 2019).
Consistent with an American study finding (Urmie et al. 2007), the current study pharmacists reported moderate knowledge level. Other studies reported a higher level of knowledge about MTM services among the participating pharmacists (Moczygemba et al., 2008, Al-Tameemi and Sarriff, 2019). On the other hand, a previous study reported that more than one third of the pharmacy technicians believed that they were less knowledgeable about MTM and they lack the skills necessary to provide MTM services when compared to pharmacists. However, they demonstrated more positive perceptions toward MTM and their ability to help pharmacists providing more MTM services (Adeoye et al. 2018). In comparison, Diploma holders who participated in the current study were found significantly less knowledgeable about MTM than participants who have a Master or PhD degree in pharmacy.
Consistent with what previously reported in a Malaysian study (Al-Tameemi and Sarriff 2019), the majority of the pharmacists in the present study agreed that MTM can benefit any patient receiving a prescription or over-the-counter medication and that the primary role of MTM was to assist with adherence and disease control.
The current study showed positive pharmacists’ attitude towards MTM services. Similar results were reported in several earlier studies (Herbert et al., 2006, Shah and Chawla, 2011, Blake et al., 2009, Al-Tameemi and Sarriff, 2019, Adeoye et al., 2018). The majority of the pharmacists in the present study believed that pharmacist’s role extends beyond merely dispensing medication and it should include reviewing patient’s medication profile to prevent adverse drug reactions. Similarly, most of the pharmacists believed that pharmacist’s role is more than dispensing medications in an earlier Malaysian study (Al-Tameemi and Sarriff 2019). Regarding the impact of MTM services on patients’ care, most of the pharmacists agreed that providing MTM service is a unique opportunity for pharmacists to participate in patient care at a broader spectrum, which is similar to what was reported by pharmacy students who indicated that participation in the MTM program would allow pharmacists to provide a higher level of patient care (Urmie et al. 2007).
The most frequently provided service in the present study was performing or obtaining necessary assessments of the patient’s health status. On the other hand, documenting the provided services and communicating essential information to other healthcare providers was the least recognized service, which is similar to an earlier study finding (Moczygemba et al. 2008).
Collecting patient- related information, referring the patient to a physician and collaborating with the physician or the consultant were the most common challenges to provide MTM service in the present study. The lack of pharmacist integration with other members of the healthcare team has been recognized as a recurring challenge affecting MTM services globally, and is a source of pharmacists frustration (Smith et al., 2017, Redmond et al., 2016). Therefore, it is necessary to enhance the collaboration between community pharmacists and other members of the healthcare team. The most reported barriers to provide MTM service in this study were negative physician attitudes, lack of training on MTM provision and lack of adequate support staff. Lack of training was the most reported barrier in an earlier Malaysian study (Al-Tameemi and Sarriff 2019). An earlier study showed that the majority of the pharmacists believed that additional training programs are needed to improve their experience in providing MTM services (Moczygemba et al. 2008). These findings shed the light on the importance of developing appropriate training programs that are capable of producing fully equipped pharmacists to provide MTM services. Furthermore, two earlier studies reported lack of adequate staff support as a barrier to provide MTM service (Law et al. 2009; Herbert et al. 2006), which is consistent with the current study findings.
The current study had some limitations. Using the self-report method could make the obtained information prone to social desirability and recall biases. Nevertheless, online methodology can provide a safe and private environment that allows the participants to provide more accurate and honest answers (Cantrell and Lupinacci 2007). In addition, the online survey may only allow participation of community pharmacists who have access to online resources, which might enhance selection bias. Furthermore, it has been reported that with the increase of internet users, the socio-demographic characteristics of the recruited participants via web-based surveys reflect the general population (Im and Chee 2004).
5. Conclusion
Efforts are needed to enhance collaboration between pharmacists and other healthcare professional, to develop documentation systems that would preserve and facilitate access to patient information, and to implement appropriate training programs which aim to overcome challenges and barriers for MTM implementation.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Footnotes
Peer review under responsibility of King Saud University.
References
- Adeoye Omolola A., Lake Leslie M., Lourens Spencer G., Morris Rachel E., Snyder Margie E. What predicts medication therapy management completion rates? the role of community pharmacy staff characteristics and beliefs about medication therapy management. J. Am. Pharm. Assoc. 2018;58(4):S7–S15. doi: 10.1016/j.japh.2018.03.001. e5. [DOI] [PubMed] [Google Scholar]
- Al-Tameemi N.K., Sarriff A. Knowledge, attitude and practice of pharmacists on medication therapy management: a survey in hospital Pulau Pinang, Penang, Malaysia. J. Pharm. Health Care Sci. 2019;5(1):1–9. doi: 10.1186/s40780-019-0131-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- APhA and the NACDS Medication therapy management in pharmacy practice: core elements of an MTM service model (Version 2.0) J. Am. Pharm. Assoc.: JAPhA. 2008;48(3):341–353. doi: 10.1331/JAPHA.2008.08514. [DOI] [PubMed] [Google Scholar]
- Blake K.B., Madhavan S.S., Scott V.(., Meredith Elswick B.L. Medication therapy management services in west virginia: pharmacists’ perceptions of educational and training needs. Res. Social Administrative Pharm. 2009;5(2):182–188. doi: 10.1016/j.sapharm.2008.06.003. [DOI] [PubMed] [Google Scholar]
- Cantrell M.A., Lupinacci P. Methodological issues in online data collection. J. Adv. Nurs. 2007;60(5):544–549. doi: 10.1111/j.1365-2648.2007.04448.x. [DOI] [PubMed] [Google Scholar]
- Cranor C.W., Christensen D.B. The Asheville Project: short-term outcomes of a community pharmacy diabetes care program. J. Am. Pharm. Assoc. (Washington, D.C. : 1996) 2003;43(2):149–159. doi: 10.1331/108658003321480696. [DOI] [PubMed] [Google Scholar]
- De Simone, Mendonça Araújo Medina, Melo Angelita Cristine, Cristina Gabriela, Pereira Coelho, Souza Danielle Maria De, Dos Santos Serio. Clinical outcomes of medication therapy management services in primary health care. Braz. J. Pharm. Sci. 2016;52(3):365–373. [Google Scholar]
- Detoni K.B., Oliveira I.V., Nascimento M.M.G., Caux T.R., Alves M.R., Ramalho-de-Oliveira D. Impact of a medication therapy management service on the clinical status of patients with chronic obstructive pulmonary disease. Int. J. Clin. Pharm. 2016;39(1):95–103. doi: 10.1007/S11096-016-0402-6. [DOI] [PubMed] [Google Scholar]
- Doucette W.R., McDonough R.P., Klepser D., McCarthy R. Comprehensive medication therapy management: identifying and resolving drug-related issues in a community pharmacy. Clin. Ther. 2005;27(7):1104–1111. doi: 10.1016/S0149-2918(05)00146-3. [DOI] [PubMed] [Google Scholar]
- Erku D.A., Ayele A.A., Mekuria A.B., Belachew S.A., Hailemeskel B., Tegegn H.G. The impact of pharmacist-led medication therapy management on medication adherence in patients with type 2 diabetes mellitus: a randomized controlled study. Pharm. Pract. 2017;15(3) doi: 10.18549/PHARMPRACT.2017.03.1026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Group, Lewin T., Burns A. Medication therapy management services: a critical review. J. Am. Pharm. Assoc. 2005;45(5):580–587. doi: 10.1331/1544345055001328. [DOI] [PubMed] [Google Scholar]
- Herbert K.E., Urmie J.M., Newland B.A., Farris K.B. Prediction of pharmacist intention to provide medicare medication therapy management services using the theory of planned behavior. Res. Social Administrative Pharm. 2006;2(3):299–314. doi: 10.1016/j.sapharm.2006.02.008. [DOI] [PubMed] [Google Scholar]
- Im E.-O., Chee W. Recruitment of research participants through the internet. Computers, Informatics, Nursing : CIN. 2004;22(5):289–297. doi: 10.1097/00024665-200409000-00009. [DOI] [PubMed] [Google Scholar]
- Law A.V., Okamoto M.P., Brock K. Ready, willing, and able to provide MTM services?: a survey of community pharmacists in the USA. Res. Social Administrative Pharm. 2009;5(4):376–381. doi: 10.1016/j.sapharm.2009.01.001. [DOI] [PubMed] [Google Scholar]
- MacIntosh C., Weiser C., Wassimi A., Reddick J., Scovis N., Guy M., Boesen K. Attitudes toward and factors affecting implementation of medication therapy management services by community pharmacists. J. Am. Pharm. Assoc. 2009;49(1):26–30. doi: 10.1331/JAPhA.2009.07122. [DOI] [PubMed] [Google Scholar]
- McGivney Melissa Somma, Meyer Susan M., Duncan-Hewitt Wendy, Hall Deanne L., Jean Venable R. Goode, Smith Randall B. Medication therapy management: its relationship to patient counseling, disease management, and pharmaceutical care. J. Am. Pharm. Assoc. : Japha. 2007;47(5):620–628. doi: 10.1331/JAPHA.2007.06129. [DOI] [PubMed] [Google Scholar]
- Moczygemba L.R., Barner J.C., Roberson K. Texas pharmacists’ opinions about and plans for provision of medication therapy management services. J. Am. Pharm. Assoc. 2008;48(1):38–45. doi: 10.1331/JAPhA.2008.07015. [DOI] [PubMed] [Google Scholar]
- Pellegrino A.N., Martin M.T., Tilton J.J., Touchette D.R. Medication therapy management services: definitions and outcomes. Drugs. 2009;69(4):393–406. doi: 10.2165/00003495-200969040-00001. [DOI] [PubMed] [Google Scholar]
- Redmond P., Carroll H., Grimes T., Galvin R., McDonnell R., Boland F., McDowell R., Hughes C., Fahey T. GPs’ and community pharmacists’ opinions on medication management at transitions of care in ireland. Fam. Pract. 2016;33(2):172–178. doi: 10.1093/fampra/cmw006. [DOI] [PubMed] [Google Scholar]
- Shah B., Chawla S. A needs assessment for development and provision of medication therapy management services in New York City. J. Pharm. Pract. 2011;24(3):339–344. doi: 10.1177/0897190010396584. [DOI] [PubMed] [Google Scholar]
- Kogut S.J., Goldstein E., Charbonneau C., Jackson A., Patry G. Improving medication management after a hospitalization with pharmacist home visits and electronic personal health records: an observational study. Drug, Healthcare Patient Saf. 2014;2014(default):1–6. doi: 10.2147/DHPS.S56574. https://doaj.org/article/d47f55b4702b4fd787949a65a75e2a53 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith M.A., Spiggle S., McConnell B. Strategies for community-based medication management services in value-based health plans. Res. Social Administrative Pharm. 2017;13(1):48–62. doi: 10.1016/j.sapharm.2016.01.005. [DOI] [PubMed] [Google Scholar]
- Touchette D.R., Burns A.L., Bough M.A., Blackburn J.C. Survey of medication therapy management programs under medicare part D. J. Am. Pharm. Assoc. 2006;46(6):683–691. doi: 10.1331/1544-3191.46.6.683.TOUCHETTE. [DOI] [PubMed] [Google Scholar]
- Urmie J.M., Farris K.B., Herbert K.E. Pharmacy students’ knowledge of the medicare drug benefit and intention to provide medicare medication therapy management services. Am. J. Pharm. Education. 2007;71(3):1–7. doi: 10.5688/aj710341. [DOI] [PMC free article] [PubMed] [Google Scholar]