Abstract
Local-level data on the health of populations are important to inform and drive effective and efficient actions to improve health, but such data are often expensive to collect and thus rare. Population Level Analysis and Community EStimates (PLACES) (www.cdc.gov/places/), a collaboration between the Centers for Disease Control and Prevention (CDC), the Robert Wood Johnson Foundation, and the CDC Foundation, provides model-based estimates for 29 measures among all counties and most incorporated and census-designated places, census tracts, and ZIP Code tabulation areas across the US. PLACES allows local health departments and others to better understand the burden and geographic distribution of chronic disease–related outcomes in their areas regardless of population size and urban–rural status and assists them in planning public health interventions. Online resources allow users to visually explore health estimates geographically, compare estimates, and download data for further use and exploration. By understanding the PLACES overall approach and using the easy-to-use PLACES applications, practitioners, policy makers, and others can enhance their efforts to improve public health, including informing prevention activities, programs, and policies; identifying priority health risk behaviors for action; prioritizing investments to areas with the biggest gaps or inequities; and establishing key health objectives to achieve community health and health equity.
Summary.
What is already known on this topic?
Local-level population health data are important for effective planning and resource allocation, yet such data are rarely available for most geographic areas below the state level.
What is added by this report?
The PLACES platform provides a set of 29 chronic disease–related measures for all US counties and most incorporated and census-designated places, census tracts, and ZIP Code tabulation areas using the same methodology.
What are the implications for public health practice?
By understanding the overall approach and using available resources and applications for PLACES, practitioners, policy makers, and other users can further support their efforts to improve health.
Introduction
Chronic diseases comprise 7 of the 10 leading causes of death in the US (1), and approximately half of US adults have at least 1 chronic condition (2). The extent of chronic disease in the population and recent public health emergencies, such as the COVID-19 pandemic and natural disasters (3–5), highlight the need for prevention and management efforts for people with chronic conditions and their risk factors.
Standardized and reliable health data for local areas across the US are critical to advancing health for all Americans, because implementing interventions and policies to promote health are largely driven at the local level. Effective planning and decision making rely on credible health information. Having detailed local information can identify patterns in the prevalence of disease as well as geographic disparities. Although planners in some areas of the US have access to geographically detailed data about chronic conditions and risk-related behaviors for their jurisdictions, most do not. One reason for the lack of local health data is the cost of directly collecting information to assess the health of populations, including data to assess and act on factors that differentially affect the health of population groups. In the absence of resources to directly collect information on the health of local populations, various statistical methods can provide alternative estimates of health measures and help conserve scarce resources for prevention activities. Beginning in 2015, the Centers for Disease Control and Prevention (CDC), with support from the Robert Wood Johnson Foundation and the CDC Foundation, implemented a small area estimation (SAE) approach that provided chronic disease–related health measures for large cities and their census tracts in the 500 Cities project (www.cdc.gov/places/about/500-cities-2016-2019/index.html). This effort was expanded in 2020 to cover all counties and all incorporated and census-designated places, census tracts, and ZIP Code Tabulation Areas (ZCTAs) with a population of 50 or more and renamed PLACES (Population Level Analysis and Community EStimates) (www.cdc.gov/places/). PLACES provides first-of-their-kind US population-level analyses and community estimates, including data for small cities and rural areas — data that were previously unavailable.
Approach to Small Area Estimation
SAE generally refers to a family of statistical procedures that estimates measures for a small geographic area by using the observed information collected for a larger area. The data for the large area can be survey data, vital statistics, or disease registry data. A variety of model-based SAE methods have been developed (6–8), and approaches vary based on the purpose of the analyses.
In response to frequent requests for population health data at multiple geographic or administrative levels (eg, county, health services area, congressional districts, cities, metropolitan areas) in a uniform and efficient manner, the CDC Division of Population Health, beginning in the 2000s, adapted an SAE approach called multilevel regression and post stratification (MRP), which was initially developed to estimate state-level voter preference by using national polls (9). The program extended this approach to the census-block level, which could then be aggregated to any larger geographic unit on the basis of census blocks by using state-level health data from the Behavioral Risk Factor Surveillance System (BRFSS) (10). After several years of refining and validating the approach (11–14), the program collaborated with the Robert Wood Johnson Foundation and the CDC Foundation to produce estimates for adult chronic disease–related measures, initially for the 500 largest US cities and their census tracts, covering 33.4% of the US adult population. In 2020 the project was expanded and renamed PLACES to provide prevalence estimates at 4 geographic levels across the US: county, place (incorporated and census-designated), census tract, and ZCTA.
Estimates are currently available for 29 health measures (Table): 13 health outcomes, 4 health risk behaviors, 9 prevention practices, and 3 health status measures, capturing risk factors, behaviors, and conditions that have a substantial impact on population health. Measures of diagnosed depression and general health status were added with the 2021 data release. The measures were chosen because they contribute substantially to chronic disease morbidity and mortality rates and are amenable to intervention. Other factors, such as how often a particular BRFSS question was asked, were also considered when choosing these measures. The measure definitions reflect the work of the Chronic Disease Indicators Project, a collaboration of CDC, the Council of State and Territorial Epidemiologists, and the National Association of Chronic Disease Directors, to develop a uniform set of data measurement definitions (15,16).
Table. Chronic Disease–Related Measures Included in PLACESa, 2021.
| Health outcomes | Health risk behaviors | Preventive services | Health status |
|---|---|---|---|
|
|
|
|
Abbreviation: PLACES, Population Level Analysis and Community EStimates.
Here, we provide a background to understanding the data, discuss available tools for exploring the data, and provide some examples of how the data can be used for action.
Current Estimation Approach
Modeling approach. A multilevel logistic regression model is constructed for each outcome, which includes individual-level age (13 categories), sex (2 categories), race or ethnicity (8 categories), and education (4 categories) from BRFSS; county-level percentage of adults below 150% of the federal poverty level from the 5-year American Community Survey (17); and state- and county-level random effects. To estimate the predicted probability for the risk of each measure, model parameters are applied to the same age–race or ethnicity–sex categories (n = 208) for each small area by using the multilevel logistic model formula. The predicted probability for each measure is multiplied by the corresponding population for each area to produce its estimated (or expected) prevalence. Concurrent population estimates were used to create the county estimates (18), and the 2010 decennial population counts were used to create estimates for incorporated and census-designated places, census tracts, and ZCTAs (19). Because these population estimates or counts cross-tabulated by education level are not available, a bootstrapping method assigns education level to each population category for each small area. To obtain the distribution of the estimate, a Monte Carlo simulation is used to draw 1,000 samples of the model parameters from their estimated conditional distributions to generate a sample of 1,000 SAEs for each small area; the final estimate for each measure is reported as the mean and 95% CI (2.5th and 97.5th percentile) of these 1,000 samples for all 3,142 US counties and for 28,484 incorporated and census-designated places, 72,337 census tracts, and 32,409 ZCTAs.
Strengths. PLACES provides a uniformly developed set of local-level chronic disease estimates based on standardized definitions that can be used for health planning. Our approach combines both individual and area-specific information relevant to small area estimation of population health outcomes. Modeling nationally and predicting locally can help fill the need for local data, especially where direct local data are unavailable. PLACES data can be used by state and local health officials, policy makers, nonprofit organizations, and others to advance health by:
Informing the development and implementation of effective and tailored prevention activities, programs, and policies
Identifying emerging health problems and priority health risk behaviors for action
Understanding the prevalence and geographic distribution of health-related issues and prioritizing investment in areas with the biggest gaps or inequities
Establishing key health objectives that the community can focus on to improve health
Limitations and cautions. First, the modeling process does not control for known potential biases in self-reported surveys such as BRFSS, including recall or social desirability biases. BRFSS is the largest telephone-based (landline and cellular telephone) survey of health behaviors and factors in the world (10). BRFSS has been shown to produce estimates generally comparable to national surveys (20-22) and is a critical — and, in many cases, a primary — data source for state-level estimates of many chronic disease–related measures. Second, detailed population count data with the relevant stratifications needed for implementing our approach are available only for the decennial census year. Therefore, incorporated and census-designated place, census tract, and ZCTA-level estimates are currently based on 2010 census population counts. For county-level estimates, vintage population estimates released by the US Census Bureau (18) that match the year of the BRFSS data are used. Third, the model does not consider any local policy or intervention effects that may affect area-specific estimates.
The lack of comparable local health data prohibits extensive validation of the PLACES MRP approach, particularly for areas smaller than counties. However, validation studies have observed that the PLACES model-based estimates show strong correlations with direct survey estimates from both BRFSS data and local survey data at the state, county, and city levels (11–14). These studies suggest that correlations are acceptable but vary by geographic level and indicator when assessed against comparable data from sources other than BRFSS, which should be expected because of different methods and measurement errors in other data sets (13,14). Where reliable, directly measured data are available, such data should be considered.
Because the model relies on decennial census data for small geographies, we caution against using the estimates for assessing changes or evaluating intervention effects over time. Also, because the statistical approach incorporates age, race or ethnicity, sex, education, and poverty to generate the estimates, others using these estimates should use caution when including PLACES estimates in other models, because some statistical collinearity is possible. Although PLACES shows geographic disparities in health, currently it does not display estimates by race or ethnicity or sex within or across geographies. However, assessing population health needs by examining the demographic composition within and across areas is appropriate. For example, PLACES estimates can be used to broadly assess health disparities across geographic areas and then examine the demographic composition of those areas to describe the populations to whom the estimates may apply, for example, whether an area is poorer, older, or has a large minority population. In addition to mapping functions such as highlighting rural and urban areas, other visualizations such as charts and graphs can complement maps. Although a focus may be on poor health, comparing healthy populations to maintain or promote health is also appropriate.
PLACES Applications and Online Resources
The PLACES website provides resources, including measure definitions, methodology, references to publications, frequently asked questions, communication tools such as fact sheets and multimedia graphics, and help pages for using the website and applications. To meet the diverse needs of users, data can be obtained, visualized, or downloaded by using various tools and applications. CDC data hosted by Socrata on CDC.gov has a feature that allows users to easily embed PLACES data on their own website.
Compare Counties Report. This report allows users to compare data between the US and up to 3 counties. By default, all categories (health outcomes, prevention, health risk behaviors, health status) display fully expanded to show data for all measures at the national level (default location is the US). Crude and age-adjusted prevalence and their corresponding CIs appear for each measure. For example, Figure 1 shows a Compare Counties Report of 3 neighboring counties in the Atlanta area. In addition to the crude and age-adjusted estimates for each measure, the population size for each county is listed. A more in-depth help section for using the Compare Counties Report is provided (www.cdc.gov/places/help/explore-compare-counties-report/index.html).
Figure 1.
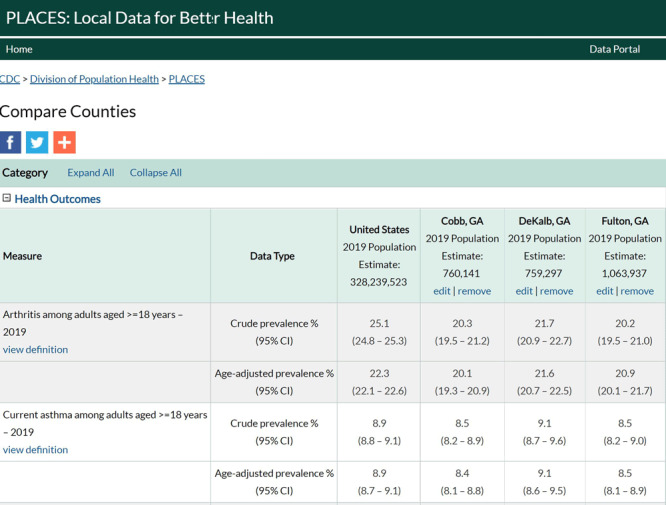
Screen shot of a PLACES Compare Counties Report comparing data for 3 Georgia counties and the US overall. Users can choose and compare data between the US and up to 3 counties.
Interactive mapping. Users can examine and visualize health estimates across different geographic levels by using the interactive mapping application. For example, the map in Figure 2A displays estimates of chronic obstructive pulmonary disease (COPD) at the county level. By clicking a specific location, the estimate for that location will appear. The map shows that the county-level prevalence of COPD is 5.8% in DeKalb County, Georgia. The mean county-level prevalence of COPD is 8.65%, as shown in the figure legend. By zooming in and clicking on a particular geographic area, users can view the estimate for smaller geographic units. Figure 2B displays COPD prevalence estimates at the ZCTA level, which can be discerned by looking at the layer tool. Estimated COPD prevalence for ZCTA 30341 is 4.8%. A more in-depth help section for using the interactive map is provided (www.cdc.gov/places/help/explore-interactive-map/index.html).
Figure 2.
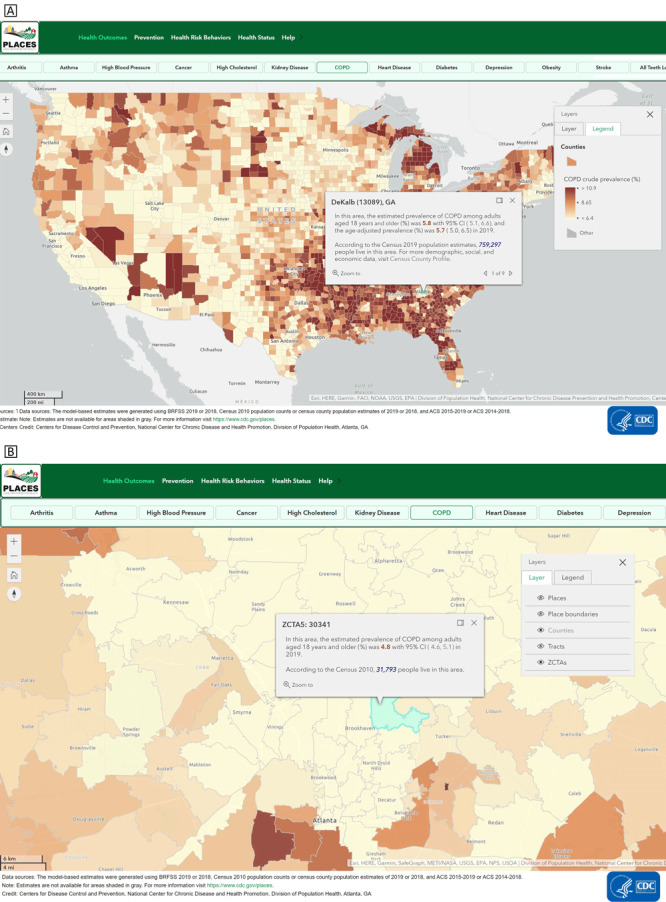
PLACES interactive map application (www.cdc.gov/PLACES). Users can examine and visualize health data estimates across different geographic levels by using the PLACES interactive mapping application. By clicking a specific location, the selected measure (eg, estimated prevalence and crude prevalence) will appear for the selected chronic disease at that location. By zooming in and clicking on a particular geographic area, users can view the estimate for smaller geographic units. In Figure 2A, the county-level prevalence of COPD in Dekalb County, Georgia, is shown. Figure 2B displays COPD prevalence estimates at the ZIP Code tabulation area (ZTCA), which can be discerned by looking at the layer tool. Abbreviations: COPD, chronic obstructive pulmonary disease; PLACES, Population Level Analysis and Community EStimates.
Advanced users can access ArcGIS Online service (Esri) and the individual maps for each measure available in CDC’s gallery of the ArcGIS Living Atlas of the World (23). Most measures have a single map, except for the core preventive services use measure, which has separate maps for older men and women. These web maps allow users to zoom to specific areas, filter data, use analysis tools, and overlay with other data available on the ArcGIS Living Atlas of the World (for example, American Community Survey socioeconomic data) or their own data.
Downloading data. Estimates can be downloaded, enabling users to view, search, filter, and further use and analyze the data. Data can be downloaded for all 4 geographic levels by using the data portal (https://chronicdata.cdc.gov/browse?category=500+Cities+%26+Places). Data are available in 2 formats: 1 measure per row (open data) or all measures per row (GIS-friendly). In addition to downloading data, estimates can be viewed as tables and searched or filtered through the data portal. A more in-depth help section for using the data portal is provided (www.cdc.gov/places/help/explore-data-portal/index.html).
PLACES Methods and Data in Action
In the first year (December 7, 2020–December 3, 2021), PLACES received more than 200,000 page views from approximately 64,000 unique visitors. To illustrate the usefulness of PLACES, we provide some examples of how the PLACES approach and data are being used to support public health action.
The PLACES MRP approach has been applied to several public health issues (24-32). The COVID-19 pandemic highlighted the susceptibility of people with chronic conditions to severe illness and outcomes from other diseases like COVID-19. People with certain chronic conditions were observed to have higher risks of severe outcomes from COVID-19 (33). By using the PLACES MRP methods, the number and percentage of US adults with specific chronic conditions (heart disease, COPD, diabetes, chronic kidney disease, obesity) and with at least 1 of those conditions were estimated. The county level prevalence of at least 1 of these 5 conditions ranged from almost 1 in 4 adults to as many as 2 in 3 adults (3). Estimates were provided on the CDC COVID Data Tracker (34) as a visual tool to help local mitigation efforts. Findings highlighted the need for prevention and control of chronic conditions and the importance of chronic conditions and risk factors in prevention and mitigation efforts for infectious disease outbreaks such as COVID-19. Providing the estimates in an interactive format allows local decision makers to identify areas at high risk for severe COVID-19 illness in their jurisdictions and guide resource allocation and implementation of community mitigation strategies.
PLACES data have been combined with other data to identify and plan for at-risk populations, including before, during, and after natural disasters or other emergencies. The prevalence of most chronic conditions does not change quickly over time, so estimates such as those provided in PLACES could be used in a near real-time manner when combined with other data that may change quickly over time. For example, it was demonstrated that the estimated number and percentage of people with COPD residing in census tracts within 50, 100, and 200 miles of the path of Hurricane Florence that struck the Carolinas in 2018 could be quickly calculated and re-calculated as the predicted hurricane path changed; such information can help to anticipate, respond to, and ameliorate health threats in preparedness and response efforts (5).
PLACES estimates are incorporated into multiple CDC websites (35-37) and have been incorporated into other external applications, including County Health Rankings and Roadmaps (38) and the City Health Dashboard (39). These platforms bring together PLACES data with other data sources while also providing guidance on actions to address health. For example, the County Health Rankings and Roadmaps website provides tools and guidance on taking action, information on evidence-informed policies and programs, and tips on identifying and working with partners. PLACES data also have been incorporated into specific state- and local-level websites. For example, PLACES data are included as part of the Hawai’i Health Matters website, a one-stop source of information about community health on the islands (40).
Finally, PLACES has been used to prioritize investment to areas with the largest health gaps or inequities. CDC’s Division of Nutrition, Physical Activity, and Obesity used 2015 county-level estimates of obesity derived from the PLACES approach to determine eligibility for the High Obesity Program (41).
PLACES of the Future
PLACES provides previously unavailable local-level health estimates through a standardized and validated SAE approach with the goal of supporting public health planning and action.
Beyond identifying geographic health disparities, PLACES data can be particularly useful when combined with data related to social determinants of health (SDOH) to understand community health and to promote health equity and equal access to health (https://www.cdc.gov/chronicdisease/programs-impact/sdoh.htm). When examined together, users can identify which health and SDOH issues overlap in a community to inform and shape public health actions. For example, identifying communities with high rates of chronic disease and high social vulnerability can highlight geographic areas especially in need of strategies tailored for the conditions and risks residents experience. Combining and overlaying data can inform planning activities for partners across sectors like education, transportation, and housing that have the shared goal of improving the conditions in people’s environments.
Using health data such as PLACES with SDOH factors can better align population-based public health approaches and tie in the social factors that contribute to both the causes of health problems and the success of solutions for population health. Beyond the built environment, SDOH includes assessing how structural policies and practices differentially affect the health of populations. With an important public health focus on SDOH and health equity (www.cdc.gov/places/social-determinants-of-health-and-places-data/index.html), further data on social and structural factors that underlie health may become available in future PLACES releases. For example, recent BRFSS surveys include modules on SDOH and on Reactions to Race, which can be assessed and made available if validated. However, PLACES is already in a format for use with such data to explore this critical area.
Conclusion
The multiple available tools and resources for PLACES allow public health practitioners and others to visualize local chronic disease–related estimates and to download data sets directly from the data portal for health planning and action. By understanding the PLACES approach and improving awareness of the easy-to-use PLACES applications, practitioners, policy makers, and other users can employ these data and tools to inform actions to improve health.
Acknowledgments
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of CDC. PLACES is funded in part by the National Foundation of the CDC (CDC Foundation, Project #1106) from a grant by the Robert Wood Johnson Foundation (Grant ID #77448). The content was not influenced, reviewed, or directed by the donors. No copyrighted material was used in this article.
Footnotes
The opinions expressed by authors contributing to this journal do not necessarily reflect the opinions of the U.S. Department of Health and Human Services, the Public Health Service, the Centers for Disease Control and Prevention, or the authors' affiliated institutions.
Suggested citation for this article: Greenlund KJ, Lu H, Wang Y, Matthews KA, LeClercq JM, Lee B, et al. PLACES: Local Data for Better Health. Prev Chronic Dis 2022;19:210459. DOI: https://doi.org/10.5888/pcd19.210459.
References
- 1. Kochanek KD, Xu J, Arias E. Mortality in the United States, 2019. NCHS Data Brief 2020;(395):1–8. [PubMed] [Google Scholar]
- 2. Buttorff C, Ruder T, Bauman M. Multiple chronic conditions in the United States. Santa Monica (CA): RAND Corporation; 2017. https://www.rand.org/pubs/tools/TL221.html. 10.7249/TL221 [DOI] [Google Scholar]
- 3. Razzaghi H, Wang Y, Lu H, Marshall KE, Dowling NF, Paz-Bailey G, et al. Estimated county-level prevalence of selected underlying medical conditions associated with increased risk for severe COVID-19 illness — United States, 2018. MMWR Morb Mortal Wkly Rep 2020;69(29):945–50. 10.15585/mmwr.mm6929a1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Ko JY, Danielson ML, Town M, Derado G, Greenlund KJ, Kirley PD, et al. ; COVID-NET Surveillance Team. Risk factors for coronavirus disease 2019 (COVID-19)-associated hospitalization: COVID-19-Associated Hospitalization Surveillance Network and Behavioral Risk Factor Surveillance System. Clin Infect Dis 2021;72(11):e695–703. 10.1093/cid/ciaa1419 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Holt JB, Matthews KA, Lu H, Wang Y, LeClercq JM, Greenlund KJ, et al. Small area estimates of populations with chronic conditions for community preparedness for public health emergencies. Am J Public Health 2019;109(S4):S325–31. 10.2105/AJPH.2019.305241 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Pfeffermann D. New important developments in small area estimation. Stat Sci 2013;28(1):40–68. 10.1214/12-STS395 [DOI] [Google Scholar]
- 7. Kong AY, Zhang X. The use of small area estimates in place-based health research. Am J Public Health 2020;110(6):829–32. 10.2105/AJPH.2020.305611 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Ghosh M, Rao JNK . Small area estimation: an appraisal. Stat Sci 1994;9(1):55–93. [Google Scholar]
- 9. Gelman A, Little TC. Poststratification into many categories using hierarchical logistic regression. Surv Methodol 1997;23:127–35. http://www.stat.columbia.edu/~gelman/research/published/poststrat3.pdf [Google Scholar]
- 10. Centers for Disease Control and Prevention. Behavioral Risk Factor Surveillance System. 2021. https://www.cdc.gov/brfss/. Accessed October 26, 2021.
- 11. Zhang X, Holt JB, Yun S, Lu H, Greenlund KJ, Croft JB. Validation of multilevel regression and poststratification methodology for small area estimation of health indicators from the Behavioral Risk Factor Surveillance System. Am J Epidemiol 2015;182(2):127–37. 10.1093/aje/kwv002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Zhang X, Holt JB, Lu H, Wheaton AG, Ford ES, Greenlund KJ, et al. Multilevel regression and poststratification for small-area estimation of population health outcomes: a case study of chronic obstructive pulmonary disease prevalence using the behavioral risk factor surveillance system. Am J Epidemiol 2014;179(8):1025–33. 10.1093/aje/kwu018 [DOI] [PubMed] [Google Scholar]
- 13. Wang Y, Holt JB, Zhang X, Lu H, Shah SN, Dooley DP, et al. Comparison of methods for estimating prevalence of chronic diseases and health behaviors for small geographic areas: Boston validation study, 2013. Prev Chronic Dis 2017;14:E99. 10.5888/pcd14.170281 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Wang Y, Holt JB, Xu F, Zhang X, Dooley DP, Lu H, et al. Using 3 health surveys to compare multilevel models for small area estimation for chronic diseases and health behaviors. Prev Chronic Dis 2018;15:E133. 10.5888/pcd15.180313 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Holt JB, Huston SL, Heidari K, Schwartz R, Gollmar CW, Tran A, et al. ; Centers for Disease Control and Prevention (CDC). Indicators for chronic disease surveillance — United States, 2013. MMWR Recomm Rep 2015;64(RR-01):1–246. [PubMed] [Google Scholar]
- 16. Centers for Disease Control and Prevention. Chronic disease indicators. 2021. https://www.cdc.gov/CDI/. Accessed October 26, 2021.
- 17. US Census Bureau. American Community Survey. https://www.census.gov/programs-surveys/acs. Accessed May 9, 2021.
- 18. US Census Bureau. County population by characteristics: 2010–2019. 2021. https://www.census.gov/data/tables/time-series/demo/popest/2010s-counties-detail.html. Accessed October 26, 2021.
- 19. US Census Bureau. P12: Sex by age. 2010: DEC Summary File 1. https://data.census.gov. Accessed October 26, 2021.
- 20. Pierannunzi C, Xu F, Wallace RC, Garvin W, Greenlund KJ, Bartoli W, et al. A methodological approach to small area estimation for the Behavioral Risk Factor Surveillance System. Prev Chronic Dis 2016;13:E91. 10.5888/pcd13.150480 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Li C, Balluz LS, Ford ES, Okoro CA, Zhao G, Pierannunzi C. A comparison of prevalence estimates for selected health indicators and chronic diseases or conditions from the Behavioral Risk Factor Surveillance System, the National Health Interview Survey, and the National Health and Nutrition Examination Survey, 2007–2008. Prev Med 2012;54(6):381–7. 10.1016/j.ypmed.2012.04.003 [DOI] [PubMed] [Google Scholar]
- 22. Hsia J, Zhao G, Town M, Ren J, Okoro CA, Pierannunzi C, et al. Comparisons of estimates from the Behavioral Risk Factor Surveillance System and other national health surveys, 2011–2016. Am J Prev Med 2020;58(6):e181–90. 10.1016/j.amepre.2020.01.025 [DOI] [PubMed] [Google Scholar]
- 23. Esri. ArcGIS living atlas of the world: gallery for Centers for Disease Control and Prevention. https://cdcarcgis.maps.arcgis.com/home/gallery.html?view=grid&sortOrder=desc&sortField=modified. Accessed October 26, 2021.
- 24. Samanic CM, Barbour KE, Liu Y, Wang Y, Fang J, Lu H, et al. Prevalence of self-reported hypertension and antihypertensive medication use by county and rural–urban classification — United States, 2017. MMWR Morb Mortal Wkly Rep 2020;69(18):533–9. 10.15585/mmwr.mm6918a1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Lin M, Zhang X, Holt JB, Robison V, Li CH, Griffin SO. Multilevel model to estimate county-level untreated dental caries among US children aged 6–9 years using the National Health and Nutrition Examination Survey. Prev Med 2018;111:291–8. 10.1016/j.ypmed.2017.11.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Eke PI, Zhang X, Lu H, Wei L, Thornton-Evans G, Greenlund KJ, et al. Predicting periodontitis at state and local levels in the United States. J Dent Res 2016;95(5):515–22. 10.1177/0022034516629112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Eke PI, Lu H, Zhang X, Thornton-Evans G, Borgnakke WS, Holt JB, et al. Geospatial distribution of periodontists and US adults with severe periodontitis. J Am Dent Assoc 2019;150(2):103–10. 10.1016/j.adaj.2018.09.021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Croft JB, Wheaton AG, Liu Y, Xu F, Lu H, Matthews KA, et al. Urban–rural county and state differences in chronic obstructive pulmonary disease — United States, 2015. MMWR Morb Mortal Wkly Rep 2018;67(7):205–11. 10.15585/mmwr.mm6707a1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Berkowitz Z, Zhang X, Richards TB, Sabatino SA, Peipins LA, Holt J, et al. Multilevel regression for small-area estimation of mammography use in the United States, 2014. Cancer Epidemiol Biomarkers Prev 2019;28(1):32–40. 10.1158/1055-9965.EPI-18-0367 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Berkowitz Z, Zhang X, Richards TB, Peipins L, Henley SJ, Holt J. Multilevel small-area estimation of multiple cigarette smoking status categories using the 2012 Behavioral Risk Factor Surveillance System. Cancer Epidemiol Biomarkers Prev 2016;25(10):1402–10. 10.1158/1055-9965.EPI-16-0244 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Berkowitz Z, Zhang X, Richards TB, Nadel M, Peipins LA, Holt J. Multilevel small-area estimation of colorectal cancer screening in the United States. Cancer Epidemiol Biomarkers Prev 2018;27(3):245–53. 10.1158/1055-9965.EPI-17-0488 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Barbour KE, Helmick CG, Boring M, Zhang X, Lu H, Holt JB. Prevalence of doctor-diagnosed arthritis at state and county levels — United States, 2014. MMWR Morb Mortal Wkly Rep 2016;65(19):489–94. 10.15585/mmwr.mm6519a2 [DOI] [PubMed] [Google Scholar]
- 33. Centers for Disease Control and Prevention. COVID-19 Information for people with medical conditions. 2021. https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/people-with-medical-conditions.html. Accessed October 26, 2021.
- 34. Centers for Disease Control and Prevention. Underlying medical conditions. 2021. https://covid.cdc.gov/covid-data-tracker/#underlying-med-conditions. Accessed October 26, 2021.
- 35. Centers for Disease Control and Prevention. US cancer statistics. The official federal cancer statistics. 2021. https://www.cdc.gov/cancer/uscs/index.htm. Accessed October 26, 2021.
- 36. Centers for Disease Control and Prevention. Interactive atlas of heart disease and stroke. 2020. https://www.cdc.gov/dhdsp/maps/atlas/index.htm. Accessed October 26, 2021.
- 37. Centers for Disease Control and Prevention. National environmental public health tracking network. 2020. https://ephtracking.cdc.gov/. Accessed October 26, 2021.
- 38.County Health Rankings. County health rankings and roadmaps. 2021. https://www.countyhealthrankings.org/. Accessed October 26, 2021.
- 39.NYU Langone Health. City health dashboard. 2021. https://www.cityhealthdashboard.com/. Accessed October 26, 2021.
- 40.Hawai'i Health Matters. Hawai'i health matters. 2021. http://www.hawaiihealthmatters.org/. Accessed October 26, 2021.
- 41. Centers for Disease Control and Prevention. High Obesity Program (HOP). 2021. https://www.cdc.gov/nccdphp/dnpao/state-local-programs/hop-1809/high-obesity-program-1809.html. Accessed October 26, 2021.


