Abstract
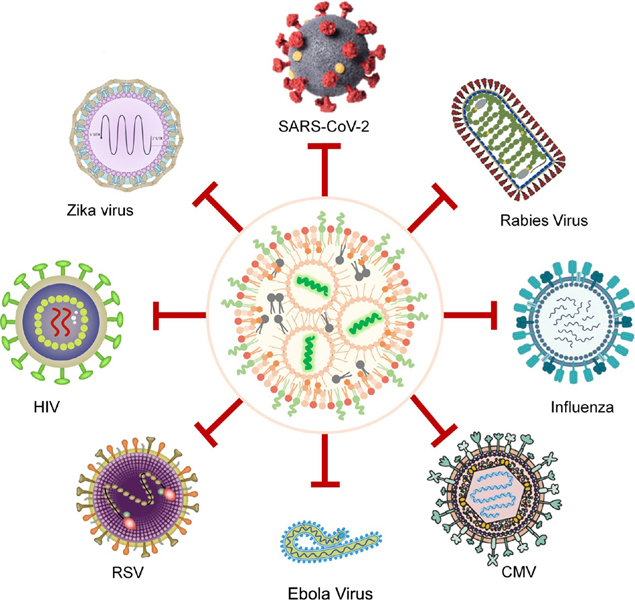
The novel coronavirus disease 2019 (COVID-19) is still rampant all over the world, causing incalculable losses to the world. Major pharmaceutical organizations around the globe are focusing on vaccine research and drug development to prevent further damage caused by the pandemic. The messenger RNA (mRNA) technology has got ample of attention after the success of the two very effective mRNA vaccines during the recent pandemic of COVID-19. mRNA vaccine has been promoted to the core stage of pharmaceutical industry, and the rapid development of mRNA technology has exceeded expectations. Beyond COVID-19, the mRNA vaccine has been tested for various infectious diseases and undergoing clinical trials. Due to the ability of constant mutation, the viral infections demand abrupt responses and immediate production, and therefore mRNA-based technology offers best answers to sudden outbreaks. The need for mRNA-based vaccine became more obvious due to the recent emergence of new Omicron variant. In this review, we summarized the unique properties of mRNA-based vaccines for infectious diseases, delivery technologies, discussed current challenges, and highlighted the prospects of this promising technology in the future. We also discussed various clinical studies as well preclinical studies conducted on mRNA therapeutics for diverse infectious diseases.
Keywords: messenger RNA (mRNA) vaccine, lipid-nanoparticle, infectious disease, drug delivery, coronavirus disease 2019 (COVID-19), virus
Acknowledgements
This work was supported by the Natural Science Foundation of Guangdong Province (No. 2019A1515010776), the Beijing-Tianjin-Hebei Basic Research Cooperation Project (No. 19JCZDJC64100), the National Key Research and Development Program of China (Nos. 2021YFE0106900, 2021YFA1201002, and 2021YFC2302402), the National Natural Science Foundation of China (Nos. 31871003 and 3217100573), and the Beijing Nova Program from Beijing Municipal Science & Technology Commission (No. Z201100006820005). The authors thank Biological & Medical Engineering Core Facilities (Beijing Institute of Technology) for providing advanced equipment.
Contributor Information
Abid Hussain, Email: abidrph@bit.edu.cn.
Yuanyu Huang, Email: yyhuang@bit.edu.cn.
References
- [1].Richner J M, Himansu S, Dowd K A, Butler S L, Salazar V, Fox J M, Julander J G, Tang W W, Shresta S, Pierson T C, et al. Modified mRNA vaccines protect against Zika virus infection. Cell. 2017;168:1114–1125.e10. doi: 10.1016/j.cell.2017.02.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Wolff J A, Malone R W, Williams P, Chong W, Acsadi G, Jani A, Felgner P L. Direct gene transfer into mouse muscle in vivo. Science. 1990;247:1465–1468. doi: 10.1126/science.1690918. [DOI] [PubMed] [Google Scholar]
- [3].Pardi N, Hogan M J, Porter F W, Weissman D. mRNA vaccines—A new era in vaccinology. Nat. Rev. Drug Discov. 2018;17:261–279. doi: 10.1038/nrd.2017.243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Weng Y H, Li C H, Yang T R, Hu B, Zhang M J, Guo S, Xiao H H, Liang X J, Huang Y Y. The challenge and prospect of mRNA therapeutics landscape. Biotechnol. Adv. 2020;40:107534. doi: 10.1016/j.biotechadv.2020.107534. [DOI] [PubMed] [Google Scholar]
- [5].Wykes M, Pombo A, Jenkins C, MacPherson G G. Dendritic cells interact directly with naive B lymphocytes to transfer antigen and initiate class switching in a primary T-dependent response. J. Immunol. 1998;161:1313–1319. doi: 10.4049/jimmunol.161.3.1313. [DOI] [PubMed] [Google Scholar]
- [6].Rybakova Y, Kowalski P S, Huang Y X, Gonzalez J T, Heartlein M W, DeRosa F, Delcassian D, Anderson D G. mRNA delivery for therapeutic anti-HER2 antibody expression in vivo. Mol. Ther. 2019;27:1415–1423. doi: 10.1016/j.ymthe.2019.05.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Sahin U, Muik A, Derhovanessian E, Vogler I, Kranz L M, Vormehr M, Baum A, Pascal K, Quandt J, Maurus D, et al. COVID-19 vaccine BNT162b1 elicits human antibody and TH1 T cell responses. Nature. 2020;586:594–599. doi: 10.1038/s41586-020-2814-7. [DOI] [PubMed] [Google Scholar]
- [8].Corbett K S, Edwards D K, Leist S R, Abiona O M, Boyoglu-Barnum S, Gillespie R A, Himansu S, Schäfer A, Ziwawo C T, DiPiazza A T, et al. SARS-CoV-2 mRNA vaccine design enabled by prototype pathogen preparedness. Nature. 2020;586:567–571. doi: 10.1038/s41586-020-2622-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Shin M D, Shukla S, Chung Y H, Beiss V, Chan S K, Ortega-Rivera O A, Wirth D M, Chen A, Sack M, Pokorski J K, et al. COVID-19 vaccine development and a potential nanomaterial path forward. Nat. Nanotechnol. 2020;15:646–655. doi: 10.1038/s41565-020-0737-y. [DOI] [PubMed] [Google Scholar]
- [10].Ding J X, Xiao H H, Chen X S. Advanced biosafety materials for prevention and theranostics of biosafety issues. Biosaf. Health. 2022;4:59–60. doi: 10.1016/j.bsheal.2022.03.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Sahin U, Karikó K, Türeci Ö. mRNA-based therapeutics—Developing a new class of drugs. Nat. Rev. Drug Discov. 2014;13:759–780. doi: 10.1038/nrd4278. [DOI] [PubMed] [Google Scholar]
- [12].Miao L, Zhang Y, Huang L. mRNA vaccine for cancer immunotherapy. Mol. Cancer. 2021;20:41. doi: 10.1186/s12943-021-01335-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Schlake T, Thess A, Fotin-Mleczek M, Kallen K J. Developing mRNA-vaccine technologies. RNA Biol. 2012;9:1319–1330. doi: 10.4161/rna.22269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Karikó K. In vitro-transcribed mRNA therapeutics: Out of the shadows and into the spotlight. Mol. Ther. 2019;27:691–692. doi: 10.1016/j.ymthe.2019.03.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Kristie B, Fiona V D B, Patrick A, et al. Self-amplifying RNA vaccines for infectious diseases. Nature Gene Therapy. 2021;28:117–129. doi: 10.1038/s41434-020-00204-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Anna K B, Shell I, Andrew J G. An update on self-amplifying mRNA vaccine development. Vaccines (Basel) 2021;9:97. doi: 10.3390/vaccines9020097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Vogel A B, Lambert L, Kinnear E, Busse D, Erbar S, Reuter K C, Wicke L, Perkovic M, Beissert T, Haas H, et al. Self-amplifying RNA vaccines give equivalent protection against influenza to mRNA vaccines but at much lower doses. Mol. Ther. 2018;26:446–455. doi: 10.1016/j.ymthe.2017.11.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Richner J M, Jagger B W, Shan C, Fontes C R, Dowd K A, Cao B, Himansu S, Caine E A, Nunes B T D, Medeiros D B A, et al. Vaccine mediated protection against Zika virus-induced congenital disease. Cell. 2017;170:273–283.e12. doi: 10.1016/j.cell.2017.06.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Arunachalam P S, Scott M K D, Hagan T, Li C F, Feng Y P, Wimmers F, Grigoryan L, Trisal M, Edara V V, Lai L, et al. Systems vaccinology of the BNT162b2 mRNA vaccine in humans. Nature. 2021;596:410–416. doi: 10.1038/s41586-021-03791-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Wadman M. The overlooked superpower of mRNA vaccines. Science. 2021;373:479. doi: 10.1126/science.373.6554.479. [DOI] [PubMed] [Google Scholar]
- [21].Huang X, Xu W G, Li M Q, Zhang P, Zhang Y S, Ding J X, Chen X S. Antiviral biomaterials. Matter. 2021;4:1892–1918. doi: 10.1016/j.matt.2021.03.016. [DOI] [Google Scholar]
- [22].Selmi A, Vascotto F, Kautz-Neu K, Türeci Ö, Sahin U, von Stebut E, Diken M, Kreiter S. Uptake of synthetic naked RNA by skin-resident dendritic cells via macropinocytosis allows antigen expression and induction of T-cell responses in mice. Cancer Immunol. Immunother. 2016;65:1075–1083. doi: 10.1007/s00262-016-1869-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Granstein R D, Ding W H, Ozawa H. Induction of anti-tumor immunity with epidermal cells pulsed with tumor-derived RNA or intradermal administration of RNA. J. Invest. Dermatol. 2000;114:632–636. doi: 10.1046/j.1523-1747.2000.00929.x. [DOI] [PubMed] [Google Scholar]
- [24].Sahin U, Derhovanessian E, Miller M, Kloke B P, Simon P, Löwer M, Bukur V, Tadmor A D, Luxemburger U, Schrörs B, et al. Personalized RNA mutanome vaccines mobilize polyspecific therapeutic immunity against cancer. Nature. 2017;547:222–226. doi: 10.1038/nature23003. [DOI] [PubMed] [Google Scholar]
- [25].Kreiter S, Selmi A, Diken M, Koslowski M, Britten C M, Huber C, Türeci Ö, Sahin U. Intranodal vaccination with naked antigen-encoding RNA elicits potent prophylactic and therapeutic antitumoral immunity. Cancer Res. 2010;70:9031–9040. doi: 10.1158/0008-5472.CAN-10-0699. [DOI] [PubMed] [Google Scholar]
- [26].Kowalski P S, Rudra A, Miao L, Anderson D G. Delivering the messenger: Advances in technologies for therapeutic mRNA delivery. Mol. Ther. 2019;27:710–728. doi: 10.1016/j.ymthe.2019.02.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Kaczmarek J C, Patel A K, Kauffman K J, Fenton O S, Webber M J, Heartlein M W, DeRosa F, Anderson D G. Polymer-lipid nanoparticles for systemic delivery of mRNA to the lungs. Angew. Chem., Int. Ed. 2016;55:13808–13812. doi: 10.1002/anie.201608450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Guimaraes P P G, Zhang R, Spektor R, Tan M, Chung A, Billingsley M M, El-Mayta R, Riley R S, Wang L L, Wilson J M, et al. Ionizable lipid nanoparticles encapsulating barcoded mRNA for accelerated in vivo delivery screening. J. Control. Release. 2019;316:404–417. doi: 10.1016/j.jconrel.2019.10.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Yan H M, Hu Y, Akk A, Rai M F, Pan H, Wickline S A, Pham C T N. Induction of WNT16 via peptide-mRNA nanoparticle-based delivery maintains cartilage homeostasis. Pharmaceutics. 2020;12:73. doi: 10.3390/pharmaceutics12010073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Jiang Y H, Lu Q, Wang Y H, Xu E, Ho A, Singh P, Wang Y F, Jiang Z Z, Yang F, Tietjen G T, et al. Quantitating endosomal escape of a library of polymers for mRNA delivery. Nano Lett. 2020;20:1117–1123. doi: 10.1021/acs.nanolett.9b04426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Sharifnia Z, Bandehpour M, Hamishehkar H, Mosaffa N, Kazemi B, Zarghami N. In-vitro transcribed mRNA delivery using PLGA/PEI nanoparticles into human monocyte-derived dendritic cells. Iran. J. Pharm. Res. 2019;18:1659–1675. doi: 10.22037/ijpr.2019.1100872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [32].Vaidyanathan S, Azizian K T, Haque A K M A, Henderson J M, Hendel A, Shore S, Antony J S, Hogrefe R I, Kormann M S D, Porteus M H, et al. Uridine depletion and chemical modification increase Cas9 mRNA activity and reduce immunogenicity without HPLC purification. Mol. Ther. Nucleic Acids. 2018;12:530–542. doi: 10.1016/j.omtn.2018.06.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [33].Lee A S Y, Kranzusch P J, Doudna J A, Cate J H D. eIF3d is an mRNA cap-binding protein that is required for specialized translation initiation. Nature. 2016;536:96–99. doi: 10.1038/nature18954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34].Martin S A, Paoletti E, Moss B. Purification of mRNA guanylyltransferase and mRNA (guanine-7-) methyltransferase from vaccinia virions. J. Biol. Chem. 1975;250:9322–9329. doi: 10.1016/S0021-9258(19)40646-7. [DOI] [PubMed] [Google Scholar]
- [35].Stepinski J, Waddell C, Stolarski R, Darzynkiewicz E, Rhoads R E. Synthesis and properties of mRNAs containing the novel “anti-reverse” cap analogs 7-methyl(3′-O-methyl)GpppG and 7-methyl (3′-deoxy)GpppG. RNA. 2001;7:1486–1495. [PMC free article] [PubMed] [Google Scholar]
- [36].von Niessen A G O, Poleganov M A, Rechner C, Plaschke A, Kranz L M, Fesser S, Diken M, Löwer M, Vallazza B, Beissert T, et al. Improving mRNA-based therapeutic gene delivery by expression-augmenting 3′ UTRs identified by cellular library screening. Mol. Ther. 2019;27:824–836. doi: 10.1016/j.ymthe.2018.12.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [37].Stefanovic B, Hellerbrand C, Brenner D A. Regulatory role of the conserved stem-loop structure at the 5′ end of collagen α1(I) mRNA. Mol. Cell. Biol. 1999;19:4334–4342. doi: 10.1128/MCB.19.6.4334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [38].Wu X Y, Brewer G. The regulation of mRNA stability in mammalian cells: 2.0. Gene. 2012;500:10–21. doi: 10.1016/j.gene.2012.03.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [39].Choi Y H, Hagedorn C H. Purifying mRNAs with a high-affinity eIF4E mutant identifies the short 3′ poly(A) end phenotype. Proc. Natl. Acad. Sci. USA. 2003;100:7033–7038. doi: 10.1073/pnas.1232347100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [40].Jalkanen A L, Coleman S J, Wilusz J. Determinants and implications of mRNA poly(A) tail size-does this protein make my tail look big? Semin. Cell Dev. Biol. 2014;34:24–32. doi: 10.1016/j.semcdb.2014.05.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [41].Zhong Z F, Portela Catani J P, Mc Cafferty S, Couck L, Van Den Broeck W, Gorlé N, Vandenbroucke R E, Devriendt B, Ulbert S, Cnops L, et al. Immunogenicity and protection efficacy of a naked self-replicating mRNA-based Zika virus vaccine. Vaccines. 2019;7:96. doi: 10.3390/vaccines7030096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [42].Li W, Meng J L, Ma X H, Lin J Q, Lu X G. Advanced materials for the delivery of vaccines for infectious diseases. Biosaf. Health. 2022;4:95–104. doi: 10.1016/j.bsheal.2022.03.002. [DOI] [Google Scholar]
- [43].Qiu P, Ziegelhoffer P, Sun J, Yang N S. Gene gun delivery of mRNA in situ results in efficient transgene expression and genetic immunization. Gene Ther. 1996;3:262–268. [PubMed] [Google Scholar]
- [44].De Ravin S S, Reik A, Liu P Q, Li L H, Wu X L, Su L, Raley C, Theobald N, Choi U, Song A H, et al. Targeted gene addition in human CD34+ hematopoietic cells for correction of X-linked chronic granulomatous disease. Nat. Biotechnol. 2016;34:424–429. doi: 10.1038/nbt.3513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [45].Hu B, Li B, Li K, Liu Y Y, Li C H, Zheng L L, Zhang M J, Yang T R, Guo S, Dong X Y, et al. Thermostable ionizable lipid-like nanoparticle (iLAND) for RNAi treatment of hyperlipidemia. Sci. Adv. 2022;8:eab–1418. doi: 10.1126/sciadv.abm1418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [46].Li C H, Yang T R, Weng Y H, Zhang M J, Zhao D Y, Guo S, Hu B, Shao W X, Wang X X, Hussain A, et al. Ionizable lipid-assisted efficient hepatic delivery of gene editing elements for oncotherapy. Bioact. Mater. 2022;9:590–601. doi: 10.1016/j.bioactmat.2021.05.051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [47].Li C H, Zhou J H, Wu Y D, Dong Y L, Du L L, Yang T R, Wang Y H, Guo S, Zhang M J, Hussain A, et al. Core role of hydrophobic core of polymeric nanomicelle in endosomal escape of siRNA. Nano Lett. 2021;21:3680–3689. doi: 10.1021/acs.nanolett.0c04468. [DOI] [PubMed] [Google Scholar]
- [48].Yang T R, Li C H, Wang X X, Zhao D Y, Zhang M J, Cao H Q, Liang Z C, Xiao H H, Liang X J, Weng Y H, et al. Efficient hepatic delivery and protein expression enabled by optimized mRNA and ionizable lipid nanoparticle. Bioact. Mater. 2020;5:1053–1061. doi: 10.1016/j.bioactmat.2020.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [49].Zhang Y Q, Li Z Y, Essola J M, Ge K, Dai X Y, He H N, Xiao H H, Weng Y H, Huang Y Y. Biosafety materials: Ushering in a new era of infectious disease diagnosis and treatment with the CRISPR/Cas system. Biosaf. Health. 2022;4:70–78. doi: 10.1016/j.bsheal.2022.03.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [50].Ullah A, Chen G, Yibang Z, Hussain A, Shafiq M, Raza F, Liu D J, Wang K K, Cao J, Qi X Y. A new approach based on CXCR4-targeted combination liposomes for the treatment of liver fibrosis. Biomater. Sci. 2022;10:2650–2664. doi: 10.1039/D2BM00242F. [DOI] [PubMed] [Google Scholar]
- [51].Guo S, Li K, Hu B, Li C H, Zhang M J, Hussain A, Wang X X, Cheng Q, Yang F, Ge K, et al. Membrane-destabilizing ionizable lipid empowered imaging-guided siRNA delivery and cancer treatment. Exploration. 2021;1:35–49. doi: 10.1002/EXP.20210008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [52].Huang, C. G.; Zhang, H. L.; Hussain, A. Liposome formulation of fluticasone furoate and method of preparation. U. S. Patent 11304901, April 19, 2022.
- [53].Semple S C, Akinc A, Chen J X, Sandhu A P, Mui B L, Cho C K, Sah D W Y, Stebbing D, Crosley E J, Yaworski E, et al. Rational design of cationic lipids for siRNA delivery. Nat. Biotechnol. 2010;28:172–176. doi: 10.1038/nbt.1602. [DOI] [PubMed] [Google Scholar]
- [54].Maier M A, Jayaraman M, Matsuda S, Liu J, Barros S, Querbes W, Tam Y K, Ansell S M, Kumar V, Qin J, et al. Biodegradable lipids enabling rapidly eliminated lipid nanoparticles for systemic delivery of RNAi therapeutics. Mol. Ther. 2013;21:1570–1578. doi: 10.1038/mt.2013.124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [55].Kauffman K J, Dorkin J R, Yang J H, Heartlein M W, DeRosa F, Mir F F, Fenton O S, Anderson D G. Optimization of lipid nanoparticle formulations for mRNA delivery in vivo with fractional factorial and definitive screening designs. Nano Lett. 2015;15:7300–7306. doi: 10.1021/acs.nanolett.5b02497. [DOI] [PubMed] [Google Scholar]
- [56].Cheng Q, Wei T, Jia Y M, Farbiak L, Zhou K J, Zhang S Y, Wei Y L, Zhu H, Siegwart D J. Dendrimer-based lipid nanoparticles deliver therapeutic FAH mRNA to normalize liver function and extend survival in a mouse model of hepatorenal tyrosinemia type I. Adv. Mater. 2018;30:e1805308. doi: 10.1002/adma.201805308. [DOI] [PubMed] [Google Scholar]
- [57].Pardi N, Hogan M J, Pelc R S, Muramatsu H, Andersen H, DeMaso C R, Dowd K A, Sutherland L L, Scearce R M, Parks R, et al. Zika virus protection by a single low-dose nucleoside-modified mRNA vaccination. Nature. 2017;543:248–251. doi: 10.1038/nature21428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [58].Jayaraman M, Ansell S M, Mui B L, Tam Y K, Chen J X, Du X Y, Butler D, Eltepu L, Matsuda S, Narayanannair J K, et al. Maximizing the potency of siRNA lipid nanoparticles for hepatic gene silencing in vivo. Angew. Chem., Int. Ed. 2012;51:8529–8533. doi: 10.1002/anie.201203263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [59].Yanez Arteta M, Kjellman T, Bartesaghi S, Wallin S, Wu X Q, Kvist A J, Dabkowska A, Székely N, Radulescu A, Bergenholtz J, et al. Successful reprogramming of cellular protein production through mRNA delivered by functionalized lipid nanoparticles. Proc. Natl. Acad. Sci. USA. 2018;115:E3351–E3360. doi: 10.1073/pnas.1720542115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [60].Robinson E, MacDonald K D, Slaughter K, McKinney M, Patel S, Sun C, Sahay G. Lipid nanoparticle-delivered chemically modified mrna restores chloride secretion in cystic fibrosis. Mol. Ther. 2018;26:2034–2046. doi: 10.1016/j.ymthe.2018.05.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [61].DeRosa F, Guild B, Karve S, Smith L, Love K, Dorkin J R, Kauffman K J, Zhang J, Yahalom B, Anderson D G, et al. Therapeutic efficacy in a hemophilia B model using a biosynthetic mRNA liver depot system. Gene Ther. 2016;23:699–707. doi: 10.1038/gt.2016.46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [62].Yin H, Song C Q, Dorkin J R, Zhu L J, Li Y X, Wu Q Q, Park A, Yang J, Suresh S, Bizhanova A, et al. Therapeutic genome editing by combined viral and non-viral delivery of CRISPR system components in vivo. Nat. Biotechnol. 2016;34:328–333. doi: 10.1038/nbt.3471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [63].Cebecauer M, Amaro M, Jurkiewicz P, Sarmento M J, Šachl R, Cwiklik L, Hof M. Membrane lipid nanodomains. Chem. Rev. 2018;118:11259–11297. doi: 10.1021/acs.chemrev.8b00322. [DOI] [PubMed] [Google Scholar]
- [64].Xuexiang H, Hanwen Z, Kamila B, Kelsey L S, Mohamad G A, Drew W, Michael J M. An ionizable lipid toolbox for RNA delivery. Nature Communications. 2021;12:7233. doi: 10.1038/s41467-021-27493-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [65].Buschmann M D, Carrasco M J, Alishetty S, Paige M, Alameh M G, Weissman D. Nanomaterial delivery systems for mRNA vaccines. Vaccines. 2021;9:65. doi: 10.3390/vaccines9010065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [66].Li M, Zhao M N, Fu Y, Li Y, Gong T, Zhang Z R, Sun X. Enhanced intranasal delivery of mRNA vaccine by overcoming the nasal epithelial barrier via intra- and paracellular pathways. J. Control. Release. 2016;228:9–19. doi: 10.1016/j.jconrel.2016.02.043. [DOI] [PubMed] [Google Scholar]
- [67].Miyazaki T, Uchida S, Nagatoishi S, Koji K, Hong T, Fukushima S, Tsumoto K, Ishihara K, Kataoka K, Cabral H. Polymeric nanocarriers with controlled chain flexibility boost mRNA delivery in vivo through enhanced structural fastening. Adv. Healthc. Mater. 2020;9:e2000538. doi: 10.1002/adhm.202000538. [DOI] [PubMed] [Google Scholar]
- [68].Li M, Li Y, Peng K, Wang Y, Gong T, Zhang Z R, He Q, Sun X. Engineering intranasal mRNA vaccines to enhance lymph node trafficking and immune responses. Acta Biomater. 2017;64:237–248. doi: 10.1016/j.actbio.2017.10.019. [DOI] [PubMed] [Google Scholar]
- [69].Zhang M J, Weng Y H, Cao Z Y, Guo S, Hu B, Lu M, Guo W S, Yang T R, Li C H, Yang X Z, Huang Y Y. ROS-activatable siRNA-engineered polyplex for NIR-triggered synergistic cancer treatment. ACS Appl. Mater. Interfaces. 2020;12:32289–32300. doi: 10.1021/acsami.0c06614. [DOI] [PubMed] [Google Scholar]
- [70].Démoulins T, Milona P, Englezou P C, Ebensen T, Schulze K, Suter R, Pichon C, Midoux P, Guzmán C A, Ruggli N, et al. Polyethylenimine-based polyplex delivery of self-replicating RNA vaccines. Nanomedicine. 2016;12:711–722. doi: 10.1016/j.nano.2015.11.001. [DOI] [PubMed] [Google Scholar]
- [71].Kaczmarek J C, Kauffman K J, Fenton O S, Sadtler K, Patel A K, Heartlein M W, DeRosa F, Anderson D G. Optimization of a degradable polymer-lipid nanoparticle for potent systemic delivery of mRNA to the lung endothelium and immune cells. Nano Lett. 2018;18:6449–6454. doi: 10.1021/acs.nanolett.8b02917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [72].Fenton O S, Kauffman K J, McClellan R L, Kaczmarek J C, Zeng M D, Andresen J L, Rhym L H, Heartlein M W, DeRosa F, Anderson D G. Customizable lipid nanoparticle materials for the delivery of siRNAs and mRNAs. Angew. Chem., Int. Ed. 2018;57:13582–13586. doi: 10.1002/anie.201809056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [73].Ullah A, Chen G, Hussain A, Khan H, Abbas A, Zhou Z W, Shafiq M, Ahmad S, Ali U, Usman M, et al. Cyclam-modified polyethyleneimine for simultaneous TGFβ siRNA delivery and CXCR4 inhibition for the treatment of CCl4-induced liver fibrosis. Int. J. Nanomedicine. 2021;16:4451–4470. doi: 10.2147/IJN.S314367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [74].Akinc A, Maier M A, Manoharan M, Fitzgerald K, Jayaraman M, Barros S, Ansell S, Du X Y, Hope M J, Madden T D, et al. The Onpattro story and the clinical translation of nanomedicines containing nucleic acid-based drugs. Nat. Nanotechnol. 2019;14:1084–1087. doi: 10.1038/s41565-019-0591-y. [DOI] [PubMed] [Google Scholar]
- [75].Sedic M, Senn J J, Lynn A, Laska M, Smith M, Platz S J, Bolen J, Hoge S, Bulychev A, Jacquinet E, et al. Safety evaluation of lipid nanoparticle-formulated modified mRNA in the Sprague-Dawley rat and cynomolgus monkey. Vet. Pathol. 2018;55:341–354. doi: 10.1177/0300985817738095. [DOI] [PubMed] [Google Scholar]
- [76].Nabhan J F, Wood K M, Rao V P, Morin J, Bhamidipaty S, LaBranche T P, Gooch R L, Bozal F, Bulawa C E, Guild B C. Intrathecal delivery of frataxin mRNA encapsulated in lipid nanoparticles to dorsal root ganglia as a potential therapeutic for Friedreich’s ataxia. Sci. Rep. 2016;6:20019. doi: 10.1038/srep20019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [77].Ramaswamy S, Tonnu N, Tachikawa K, Limphong P, Vega J B, Karmali P P, Chivukula P, Verma I M. Systemic delivery of factor IX messenger RNA for protein replacement therapy. Proc. Natl. Acad. Sci. USA. 2017;114:e1941–e1950. doi: 10.1073/pnas.1619653114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [78].Kauffman K J, Mir F F, Jhunjhunwala S, Kaczmarek J C, Hurtado J E, Yang J H, Webber M J, Kowalski P S, Heartlein M W, DeRosa F, et al. Efficacy and immunogenicity of unmodified and pseudouridine-modified mRNA delivered systemically with lipid nanoparticles in vivo. Biomaterials. 2016;109:78–87. doi: 10.1016/j.biomaterials.2016.09.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [79].Oberli M A, Reichmuth A M, Dorkin J R, Mitchell M J, Fenton O S, Jaklenec A, Anderson D G, Langer R, Blankschtein D. Lipid nanoparticle assisted mRNA delivery for potent cancer immunotherapy. Nano Lett. 2017;17:1326–1335. doi: 10.1021/acs.nanolett.6b03329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [80].Sago C D, Lokugamage M P, Paunovska K, Vanover D A, Monaco C M, Shah N N, Gamboa Castro M, Anderson S E, Rudoltz T G, Lando G N, et al. High-throughput in vivo screen of functional mRNA delivery identifies nanoparticles for endothelial cell gene editing. Proc. Natl. Acad. Sci. USA. 2018;115:E9944–E9952. doi: 10.1073/pnas.1811276115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [81].Li B, Luo X, Deng B B, Giancola J B, McComb D W, Schmittgen T D, Dong Y Z. Effects of local structural transformation of lipid-like compounds on delivery of messenger RNA. Sci. Rep. 2016;6:22137. doi: 10.1038/srep22137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [82].Jain R, Frederick J P, Huang E Y, Burke K E, Mauger D M, Andrianova E A, Farlow S J, Siddiqui S, Pimentel J, Cheung-Ong K, et al. MicroRNAs enable mRNA therapeutics to selectively program cancer cells to self-destruct. Nucleic Acid Ther. 2018;28:285–296. doi: 10.1089/nat.2018.0734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [83].Fenton O S, Kauffman K J, McClellan R L, Appel E A, Dorkin J R, Tibbitt M W, Heartlein M W, DeRosa F, Langer R, Anderson D G. Bioinspired alkenyl amino alcohol ionizable lipid materials for highly potent in vivo mRNA delivery. Adv. Mater. 2016;28:2939–2943. doi: 10.1002/adma.201505822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [84].Fenton O S, Kauffman K J, Kaczmarek J C, McClellan R L, Jhunjhunwala S, Tibbitt M W, Zeng M D, Appel E A, Dorkin J R, Mir F F, et al. Synthesis and biological evaluation of ionizable lipid materials for the in vivo delivery of messenger RNA to B lymphocytes. Adv. Mater. 2017;29:1606944. doi: 10.1002/adma.201606944. [DOI] [PubMed] [Google Scholar]
- [85].Kowalski P S, Capasso Palmiero U, Huang Y X, Rudra A, Langer R, Anderson D G. Ionizable amino-polyesters synthesized via ring opening polymerization of tertiary amino-alcohols for tissue selective mRNA delivery. Adv. Mater. 2018;30:e1801151. doi: 10.1002/adma.201801151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [86].Jiang L, Berraondo P, Jericó D, Guey L T, Sampedro A, Frassetto A, Benenato K E, Burke K, Santamaría E, Alegre M, et al. Systemic messenger RNA as an etiological treatment for acute intermittent porphyria. Nat. Med. 2018;24:1899–1909. doi: 10.1038/s41591-018-0199-z. [DOI] [PubMed] [Google Scholar]
- [87].An D, Schneller J L, Frassetto A, Liang S, Zhu X L, Park J S, Theisen M, Hong S J, Zhou J, Rajendran R, et al. Systemic messenger RNA therapy as a treatment for methylmalonic acidemia. Cell Rep. 2017;21:3548–3558. doi: 10.1016/j.celrep.2017.11.081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [88].Li B, Luo X, Deng B B, Wang J F, McComb D W, Shi Y M, Gaensler K M L, Tan X, Dunn A L, Kerlin B A, et al. An orthogonal array optimization of lipid-like nanoparticles for mRNA delivery in vivo. Nano Lett. 2015;15:8099–8107. doi: 10.1021/acs.nanolett.5b03528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [89].Turnbull I C, Eltoukhy A A, Fish K M, Nonnenmacher M, Ishikawa K, Chen J Q, Hajjar R J, Anderson D G, Costa K D. Myocardial delivery of lipidoid nanoparticle carrying modRNA induces rapid and transient expression. Mol. Ther. 2016;24:66–75. doi: 10.1038/mt.2015.193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [90].Miller J B, Zhang S Y, Kos P, Xiong H, Zhou K J, Perelman S S, Zhu H, Siegwart D J. Non-viral CRISPR/cas gene editing in vitro and in vivo enabled by synthetic nanoparticle co-delivery of Cas9 mRNA and sgRNA. Angew. Chem., Int. Ed. 2017;56:1059–1063. doi: 10.1002/anie.201610209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [91].Jarzębińska A, Pasewald T, Lambrecht J, Mykhaylyk O, Kümmerling L, Beck P, Hasenpusch G, Rudolph C, Plank C, Dohmen C. A single methylene group in oligoalkylamine-based cationic polymers and lipids promotes enhanced mRNA delivery. Angew. Chem., Int. Ed. 2016;55:9591–9595. doi: 10.1002/anie.201603648. [DOI] [PubMed] [Google Scholar]
- [92].Schrom E, Huber M, Aneja M, Dohmen C, Emrich D, Geiger J, Hasenpusch G, Herrmann-Janson A, Kretzschmann V, Mykhailyk O, et al. Translation of angiotensin-converting enzyme 2 upon liver- and lung-targeted delivery of optimized chemically modified mRNA. Mol. Ther. Nucleic Acids. 2017;7:350–365. doi: 10.1016/j.omtn.2017.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [93].Ball R L, Hajj K A, Vizelman J, Bajaj P, Whitehead K A. Lipid nanoparticle formulations for enhanced co-delivery of siRNA and mRNA. Nano Lett. 2018;18:3814–3822. doi: 10.1021/acs.nanolett.8b01101. [DOI] [PubMed] [Google Scholar]
- [94].Tanaka H, Nakatani T, Furihata T, Tange K, Nakai Y, Yoshioka H, Harashima H, Akita H. In vivo introduction of mRNA encapsulated in lipid nanoparticles to brain neuronal cells and astrocytes via intracerebroventricular administration. Mol. Pharm. 2018;15:2060–2067. doi: 10.1021/acs.molpharmaceut.7b01084. [DOI] [PubMed] [Google Scholar]
- [95].Sabnis S, Kumarasinghe E S, Salerno T, Mihai C, Ketova T, Senn J J, Lynn A, Bulychev A, McFadyen I, Chan J, et al. A novel amino lipid series for mRNA delivery: Improved endosomal escape and sustained pharmacology and safety in non-human primates. Mol. Ther. 2018;26:1509–1519. doi: 10.1016/j.ymthe.2018.03.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [96].Hassett K J, Benenato K E, Jacquinet E, Lee A, Woods A, Yuzhakov O, Himansu S, Deterling J, Geilich B M, Ketova T, et al. Optimization of lipid nanoparticles for intramuscular administration of mRNA vaccines. Mol. Ther. Nucleic Acids. 2019;15:1–11. doi: 10.1016/j.omtn.2019.01.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [97].Luo X, Li B, Zhang X, Zhao W, Bratasz A, Deng B, McComb D W, Dong Y. Dual-functional lipid-like nanoparticles for delivery of mRNA and MRI contrast agents. Nanoscale. 2017;9:1575–1579. doi: 10.1039/C6NR08496F. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [98].Jiang C, Mei M, Li B, Zhu X R, Zu W H, Tian Y J, Wang Q N, Guo Y, Dong Y Z, Tan X. A non-viral CRISPR/Cas9 delivery system for therapeutically targeting HBV DNA and pcsk9 in vivo. Cell Res. 2017;27:440–443. doi: 10.1038/cr.2017.16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [99].Badieyan Z S, Berezhanskyy T, Utzinger M, Aneja M K, Emrich D, Erben R, Schüler C, Altpeter P, Ferizi M, Hasenpusch G, et al. Transcript-activated collagen matrix as sustained mRNA delivery system for bone regeneration. J. Control. Release. 2016;239:137–148. doi: 10.1016/j.jconrel.2016.08.037. [DOI] [PubMed] [Google Scholar]
- [100].Hajj K A, Ball R L, Deluty S B, Singh S R, Strelkova D, Knapp C M, Whitehead K A. Branched-tail lipid nanoparticles potently deliver mRNA in vivo due to enhanced ionization at endosomal pH. Small. 2019;15:e1805097. doi: 10.1002/smll.201805097. [DOI] [PubMed] [Google Scholar]
- [101].Tanaka H, Watanabe A, Konishi M, Nakai Y, Yoshioka H, Ohkawara T, Takeda H, Harashima H, Akita H. The delivery of mRNA to colon inflammatory lesions by lipid-nano-particles containing environmentally-sensitive lipid-like materials with oleic acid scaffolds. Heliyon. 2018;4:e00959. doi: 10.1016/j.heliyon.2018.e00959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [102].McKinlay C J, Vargas J R, Blake T R, Hardy J W, Kanada M, Contag C H, Wender P A, Waymouth R M. Charge-altering releasable transporters (CARTs) for the delivery and release of mRNA in living animals. Proc. Natl. Acad. Sci. USA. 2017;114:e448–e456. doi: 10.1073/pnas.1614193114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [103].Patel A K, Kaczmarek J C, Bose S, Kauffman K J, Mir F, Heartlein M W, DeRosa F, Langer R, Anderson D G. Inhaled nanoformulated mRNA polyplexes for protein production in lung epithelium. Adv. Mater. 2019;31:e1805116. doi: 10.1002/adma.201805116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [104].Van der Jeught K, De Koker S, Bialkowski L, Heirman C, Tjok Joe P, Perche F, Maenhout S, Bevers S, Broos K, Deswarte K, et al. Dendritic cell targeting mRNA lipopolyplexes combine strong antitumor T-cell immunity with improved inflammatory safety. ACS Nano. 2018;12:9815–9829. doi: 10.1021/acsnano.8b00966. [DOI] [PubMed] [Google Scholar]
- [105].Weide B, Pascolo S, Scheel B, Derhovanessian E, Pflugfelder A, Eigentler T K, Pawelec G, Hoerr I, Rammensee H G, Garbe C. Direct injection of protamine-protected mRNA: Results of a phase 1/2 vaccination trial in metastatic melanoma patients. J. Immunother. 2009;32:498–507. doi: 10.1097/CJI.0b013e3181a00068. [DOI] [PubMed] [Google Scholar]
- [106].Armbruster N, Jasny E, Petsch B. Advances in RNA vaccines for preventive indications: A case study of a vaccine against rabies. Vaccines. 2019;7:132. doi: 10.3390/vaccines7040132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [107].Jarzebska N T, Lauchli S, Iselin C, French L E, Johansen P, Guenova E, Kündig T M, Pascolo S. Functional differences between protamine preparations for the transfection of mRNA. Drug Deliv. 2020;27:1231–1235. doi: 10.1080/10717544.2020.1790692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [108].Li M C, Wang H, Tian L L, Pang Z H, Yang Q K, Huang T Q, Fan J F, Song L H, Tong Y G, Fan H H. COVID-19 vaccine development: Milestones, lessons and prospects. Signal Transduct. Target. Ther. 2022;7:146. doi: 10.1038/s41392-022-00996-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [109].Hussain A, Yang H Y, Zhang M J, Liu Q, Alotaibi G, Irfan M, He H N, Chang J, Liang X J, Weng Y H, et al. mRNA vaccines for COVID-19 and diverse diseases. J. Control. Release. 2022;345:314–333. doi: 10.1016/j.jconrel.2022.03.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [110].Luk A, Clarke B, Dahdah N, Ducharme A, Krahn A, McCrindle B, Mizzi T, Naus M, Udell J A, Virani S, et al. Myocarditis and pericarditis after COVID-19 mRNA vaccination: Practical considerations for care providers. Can. J. Cardiol. 2021;37:1629–1634. doi: 10.1016/j.cjca.2021.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [111].Garcia-Beltran W F, St. Denis K J, Hoelzemer A, Lam E C, Nitido A D, Sheehan M L, Berrios C, Ofoman O, Chang C C, Hauser B M, et al. mRNA-based COVID-19 vaccine boosters induce neutralizing immunity against SARS-CoV-2 Omicron variant. Cell. 2022;185:457–466.e4. doi: 10.1016/j.cell.2021.12.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [112].Dong Y Z, Dorkin J R, Wang W H, Chang P H, Webber M J, Tang B C, Yang J, Abutbul-Ionita I, Danino D, DeRosa F, et al. Poly(glycoamidoamine) brushes formulated nanomaterials for systemic siRNA and mRNA delivery in vivo. Nano Lett. 2016;16:842–848. doi: 10.1021/acs.nanolett.5b02428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [113].Palmiero U C, Kaczmarek J C, Fenton O S, Anderson D G. Poly(β-amino ester)-co-poly(caprolactone) terpolymers as nonviral vectors for mRNA delivery in vitro and in vivo. Adv. Healthc. Mater. 2018;7:e1800249. doi: 10.1002/adhm.201800249. [DOI] [PubMed] [Google Scholar]
- [114].Li J H, Wang W D, He Y P, Li Y Z, Yan E Z, Zhang K T, Irvine D J, Hammond P T. Structurally programmed assembly of translation initiation nanoplex for superior mRNA delivery. ACS Nano. 2017;11:2531–2544. doi: 10.1021/acsnano.6b08447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [115].Li J H, He Y P, Wang W D, Wu C, Hong C, Hammond P T. Polyamine-mediated stoichiometric assembly of ribonucleoproteins for enhanced mRNA delivery. Angew. Chem., Int. Ed. 2017;56:13709–13712. doi: 10.1002/anie.201707466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [116].Haabeth O A W, Blake T R, McKinlay C J, Waymouth R M, Wender P A, Levy R. mRNA vaccination with chargealtering releasable transporters elicits human T cell responses and cures established tumors in mice. Proc. Natl. Acad. Sci. USA. 2018;115:e9153–e9161. doi: 10.1073/pnas.1810002115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [117].McKinlay C J, Benner N L, Haabeth O A, Waymouth R M, Wender P A. Enhanced mRNA delivery into lymphocytes enabled by lipid-varied libraries of charge-altering releasable transporters. Proc. Natl. Acad. Sci. USA. 2018;115:e5859–e5866. doi: 10.1073/pnas.1805358115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [118].Le Moignic A, Malard V, Benvegnu T, Lemiègre L, Berchel M, Jaffrès P A, Baillou C, Delost M, Macedo R, Rochefort J, et al. Preclinical evaluation of mRNA trimannosylated lipopolyplexes as therapeutic cancer vaccines targeting dendritic cells. J. Control. Release. 2018;278:110–121. doi: 10.1016/j.jconrel.2018.03.035. [DOI] [PubMed] [Google Scholar]
- [119].Yan Y F, Xiong H, Zhang X Y, Cheng Q, Siegwart D J. Systemic mRNA delivery to the lungs by functional polyester-based carriers. Biomacromolecules. 2017;18:4307–4315. doi: 10.1021/acs.biomac.7b01356. [DOI] [PubMed] [Google Scholar]
- [120].Dunn A W, Kalinichenko V V, Shi D L. Highly efficient in vivo targeting of the pulmonary endothelium using novel modifications of polyethylenimine: An importance of charge. Adv. Healthc. Mater. 2018;7:e1800876. doi: 10.1002/adhm.201800876. [DOI] [PubMed] [Google Scholar]
- [121].Uchida S, Kinoh H, Ishii T, Matsui A, Tockary T A, Takeda K M, Uchida H, Osada K, Itaka K, Kataoka K. Systemic delivery of messenger RNA for the treatment of pancreatic cancer using polyplex nanomicelles with a cholesterol moiety. Biomaterials. 2016;82:221–228. doi: 10.1016/j.biomaterials.2015.12.031. [DOI] [PubMed] [Google Scholar]
- [122].Chen Q X, Qi R G, Chen X Y, Yang X, Wu S D, Xiao H H, Dong W F. A targeted and stable polymeric nanoformulation enhances systemic delivery of mRNA to tumors. Mol. Ther. 2017;25:92–101. doi: 10.1016/j.ymthe.2016.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [123].Schumann C, Nguyen D X, Norgard M, Bortnyak Y, Korzun T, Chan S, Lorenz A S, Moses A S, Albarqi H A, Wong L, et al. Increasing lean muscle mass in mice via nanoparticle-mediated hepatic delivery of follistatin mRNA. Theranostics. 2018;8:5276–5288. doi: 10.7150/thno.27847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [124].Jiang Y H, Gaudin A, Zhang J W, Agarwal T, Song E, Kauffman A C, Tietjen G T, Wang Y H, Jiang Z Z, Cheng C J, et al. A “top-down” approach to actuate poly(amine-co-ester) terpolymers for potent and safe mRNA delivery. Biomaterials. 2018;176:122–130. doi: 10.1016/j.biomaterials.2018.05.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [125].Fornaguera C, Guerra-Rebollo M, Ángel Lázaro M, Castells-Sala C, Meca-Cortés O, Ramos-Pérez V, Cascante A, Rubio N, Blanco J, Borrós S. mRNA delivery system for targeting antigen-presenting cells in vivo. Adv. Healthc. Mater. 2018;7:e1800335. doi: 10.1002/adhm.201800335. [DOI] [PubMed] [Google Scholar]
- [126].Song Y, Wang M M, Li S Q, Jin H B, Cai X L, Du D, Li H, Chen C L, Lin Y H. Efficient cytosolic delivery using crystalline nanoflowers assembled from fluorinated peptoids. Small. 2018;14:e1803544. doi: 10.1002/smll.201803544. [DOI] [PubMed] [Google Scholar]
- [127].Chen G J, Ma B, Wang Y Y, Gong S Q. A universal GSH-responsive nanoplatform for the delivery of DNA, mRNA, and Cas9/sgRNA ribonucleoprotein. ACS Appl. Mater. Interfaces. 2018;10:18515–18523. doi: 10.1021/acsami.8b03496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [128].Thomas S J, Moreira E D, Jr, Kitchin N, Absalon J, Gurtman A, Lockhart S, Perez J L, Marc G P, Polack F P, Zerbini C, et al. Safety and efficacy of the BNT162b2 mRNA Covid-19 vaccine through 6 months. N. Engl. J. Med. 2021;385:1761–1773. doi: 10.1056/NEJMoa2110345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [129].El Sahly H M, Baden L R, Essink B, Doblecki-Lewis S, Martin J M, Anderson E J, Campbell T B, Clark J, Jackson L A, Fichtenbaum C J, et al. Efficacy of the mRNA-1273 SARS-CoV-2 vaccine at completion of blinded phase. N. Engl. J. Med. 2021;385:1774–1785. doi: 10.1056/NEJMoa2113017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [130].Xu, Z. P.; Liu, K. F.; Gao, G. F. Omicron variant of SARS-CoV-2 imposes a new challenge for the global public health. Biosaf. Health, in press, 10.1016/j.bsheal.2022.01.002. [DOI] [PMC free article] [PubMed]
- [131].Zhang, B.; Huo, J.; Huang, Y.; Teo, S. Y.; Li, Y. F.; Toh, L. K.; Lam, K. P.; Xu, S. mRNA booster vaccination enhances antibody responses against SARS-CoV2 Omicron variant in individuals primed with mRNA or inactivated virus vaccines. 2022. [DOI] [PMC free article] [PubMed]
- [132].Wu K, Choi A, Koch M, Elbashir S, Ma L Z, Lee D, Woods A, Henry C, Palandjian C, Hill A, et al. Variant SARS-CoV-2 mRNA vaccines confer broad neutralization as primary or booster series in mice. Vaccine. 2021;39:7394–7400. doi: 10.1016/j.vaccine.2021.11.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [133].Dolgin E. CureVac COVID vaccine let-down spotlights mRNA design challenges. Nature. 2021;594:483. doi: 10.1038/d41586-021-01661-0. [DOI] [PubMed] [Google Scholar]
- [134].Chen G L, Li X F, Dai X H, Li N, Cheng M L, Huang Z, Shen J, Ge Y H, Shen Z W, Deng Y Q, et al. Safety and immunogenicity of the SARS-CoV-2 ARCoV mRNA vaccine in Chinese adults: A randomised, double-blind, placebo-controlled, phase 1 trial. Lancet Microbe. 2022;3:e193–e202. doi: 10.1016/S2666-5247(21)00280-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [135].Chaudhary N, Weissman D, Whitehead K A. mRNA vaccines for infectious diseases:Principles, delivery and clinical translation. Nat. Rev. Drug Discov. 2021;20:817–838. doi: 10.1038/s41573-021-00283-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [136].Hekele A, Bertholet S, Archer J, Gibson D G, Palladino G, Brito L A, Otten G R, Brazzoli M, Buccato S, Bonci A, et al. Rapidly produced SAM® vaccine against H7N9 influenza is immunogenic in mice. Emerg. Microbes Infect. 2013;2:e52. doi: 10.1038/emi.2013.54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [137].Bahl K, Senn J J, Yuzhakov O, Bulychev A, Brito L A, Hassett K J, Laska M E, Smith M, Almarsson Ö, Thompson J, et al. Preclinical and clinical demonstration of immunogenicity by mRNA vaccines against H10N8 and H7N9 influenza viruses. Mol. Ther. 2017;25:1316–1327. doi: 10.1016/j.ymthe.2017.03.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [138].Bian J W, Li Z J. Angiotensin-converting enzyme 2 (ACE2): SARS-CoV-2 receptor and RAS modulator. Acta Pharm. Sin. B. 2021;11:1–12. doi: 10.1016/j.apsb.2020.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [139].Zhang P, Narayanan E, Liu Q B, Tsybovsky Y, Boswell K, Ding S L, Hu Z H, Follmann D, Lin Y, Miao H Y, et al. A multiclade env-gag VLP mRNA vaccine elicits tier-2 HIV-1-neutralizing antibodies and reduces the risk of heterologous SHIV infection in macaques. Nat. Med. 2021;27:2234–2245. doi: 10.1038/s41591-021-01574-5. [DOI] [PubMed] [Google Scholar]
- [140].Loomis R J, DiPiazza A T, Falcone S, Ruckwardt T J, Morabito K M, Abiona O M, Chang L A, Caringal R T, Presnyak V, Narayanan E, et al. Chimeric fusion (F) and attachment (G) glycoprotein antigen delivery by mRNA as a candidate nipah vaccine. Front. Immunol. 2021;12:772864. doi: 10.3389/fimmu.2021.772864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [141].Lamb, R. A. Paramyxoviridae: The viruses and their replication. Fields Virology2001.
- [142].Fugl A, Andersen C L. Epstein—Barr virus and its association with disease—A review of relevance to general practice. BMC Fam. Pract. 2019;20:62. doi: 10.1186/s12875-019-0954-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [143].Kozlov M. Monkeypox goes global: Why scientists are on alert. Nature. 2022;606:15–16. doi: 10.1038/d41586-022-01421-8. [DOI] [PubMed] [Google Scholar]
- [144].Oladoye M J. Monkeypox: A neglected viral zoonotic disease. Eur. J. Med. Educat. Technol. 2021;14:e–2108. [Google Scholar]
- [145].Nowak D, Jakubczyk E. The freeze-drying of foods—The characteristic of the process course and the effect of its parameters on the physical properties of food materials. Foods. 2020;9:1488. doi: 10.3390/foods9101488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [146].Huang Y Y, Zheng S Q, Guo Z D, de Mollerat du Jeu X, Liang X J, Yang Z W, Zhang H Y, Gao S, Liang Z C. Ionizable liposomal siRNA therapeutics enables potent and persistent treatment of Hepatitis B. Signal Transduct. Target. Ther. 2022;7:38. doi: 10.1038/s41392-021-00859-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [147].Ai, L. X.; Li, Y. F.; Zhou, L.; Zhang, H.; Yao, W. R.; Han, J. Y.; Wu, J. M.; Wang, R. Y.; Wang, W. J.; Xu, P. et al. Lyophilized mRNA-lipid nanoparticle vaccines with long-term stability and high antigenicity against SARS-CoV-2. 2022, bioRxiv 2022.02. 10.479867. [DOI] [PMC free article] [PubMed]
- [148].Muramatsu H, Lam K, Bajusz C, Laczkó D, Karikó K, Schreiner P, Martin A, Lutwyche P, Heyes J, Pardi N. Lyophilization provides long-term stability for a lipid nanoparticle-formulated, nucleoside-modified mRNA vaccine. Mol. Ther. 2022;30:1941–1951. doi: 10.1016/j.ymthe.2022.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]


