Abstract
Introduction
Control of tuberculosis (TB) is hampered by suboptimal case detection and subsequent delays in treatment, which is worsened by the COVID-19 pandemic. The community pharmacy is reported as the place for first aid medication among patients with TB. We, therefore, analysed knowledge, attitude and practice (KAP) on TB patient detection (TBPD) of community pharmacy personnel, aiming to find innovative strategies to engage community pharmacies in TBPD.
Methods
A multicentre cross-sectional study was performed in four areas of Indonesia’s eastern, central and western parts. Pharmacists and pharmacy technicians who worked in community pharmacies were assessed for their characteristics and KAP related to TBPD. Descriptive analysis was used to assess participant characteristics and their KAP, while multivariable regression analyses were used to analyse factors associated with the KAP on TBPD.
Results
A total of 1129 participants from 979 pharmacies, comprising pharmacists (56.6%) and pharmacy technicians (43.4%), were included. Most participants knew about TB. However, knowledge related to TB symptoms, populations at risk and medication for TB were still suboptimal. Most participants showed a positive attitude towards TBPD. They believed in their professional role (75.1%), capacity in TB screening (65.4%) and responsibility for TBPD (67.4%). Nevertheless, a lack of TBPD practice was identified in most participants. Several factors significantly associated with performing the TBPD practice (p<0.05), such as TB training experience (p<0.001), provision of a drug consultation service (p<0.001), male gender (p<0.05), a positive attitude towards TBPD (p<0.001), short working hours (p<0.001) and central city location of the pharmacy (p<0.05).
Conclusions
Most participants had good knowledge and attitude, which did not translate into actual TBPD practice. We identified that TB educational programmes are essential in improving the KAP. A comprehensive assessment is needed to develop effective strategies to engage the community pharmacy in TBPD activities.
Keywords: tuberculosis, infection control, public health
Strengths and limitations of this study.
This is the first study that explicitly analyses tuberculosis (TB) patient detection knowledge, attitude and practice among pharmacists and pharmacy technicians in community pharmacies in Indonesia.
A large number of 1129 participants from 979 pharmacies were included in this study, obtained from Indonesia’s western, central and eastern parts.
Relevant stakeholders were involved in developing the research question, the study’s methodology and its execution, which helped to assure the quality of the project and provided support for follow-up studies and interventions.
This was a self-reported study that may have been biased by socially desirable responses.
No causal relations can be inferred between factors related to patient characteristics, knowledge and attitude on the one hand and TB patient detection practice on the other hand since the nature of the cross-sectional study does not consider the time difference between the causal factors and the effect
Introduction
Tuberculosis (TB), a disease caused by Mycobacterium tuberculosis, remains an immense global health problem. The most recent TB report of the WHO estimated that its global incidence is about 9.9 million people, with total mortality around 1.3 million people in 2020.1 The global treatment coverage is still low, with great concern about multidrug-resistant TB (MDR-TB), that is, the pathogen’s resistance to at least two powerful anti-TB drugs (isoniazid and rifampicin). Global data showed that the success rate of MDR-TB treatment is only about 59%.1
The TB problem gets more complex when it is considered that the COVID-19 pandemic affects TB patient detection (TBPD). Globally, TB notifications significantly decreased from 7.1 million (2019) to 5.8 million (2020).1 The high-burden TB countries, such as India, Indonesia, Philippines, China, Bangladesh and Pakistan, contributed most to the global shortfall in TB notification. Indonesia is ranked third among the high TB burden countries, with around 824 thousand people who contracted TB in 2020.1 TB patient notification in Indonesia significantly dropped from 566.8 thousand (2019) to 393.3 thousand (2020) due to the COVID-19 pandemic.1
The community pharmacy is a potential facility that can help detect patients with TB.2 Studies in high-burden TB countries showed that most patients with TB initially present at the pharmacy for their first aid medication.3–8 However, improper management of patients with TB in pharmacies can lead to delayed diagnosis and inappropriate treatment.9 10 A study in Indonesia estimated that the total delay is caused by various reasons, including visiting a pharmacy for the initial aid medication.3 A qualitative study also showed that delayed TB diagnosis occurred when the patient with TB received inappropriate treatment recommendations from a pharmacy.11 Improper TB patient management in the pharmacy might be due to poor TB knowledge, attitude and practices (KAP) of the pharmacy personnel. All this information suggests that improving TB care in the community pharmacy is needed to enhance the practice of TB screening and refer a presumptive TB patient to the healthcare facility to support TBPD.
However, there is still limited or no systematic and comprehensive guidance on the involvement of pharmacies in TBPD, including in Indonesia. As a base for such guidance, a first study is needed to analyse the current situation and determinants for practising TBPD among community pharmacies. Therefore, we conducted a multicentre cross-sectional study to analyse the characteristics, KAP of the pharmaceutical personnel in the community pharmacy regarding TBPD in Indonesia. To the best of our knowledge, this is the first study on this topic for the setting, and it will be beneficial to develop innovative strategies to increase TBPD in Indonesia and other high-burden TB countries.
Methods
Study design and setting
A cross-sectional study was performed in four areas in Indonesia’s western, central and eastern parts. The three areas are the capital of provinces, while one area is a peripheral area outside the province capital. Thus, four areas were defined as the study location, that is, Makassar, Medan, the city of Bandung and the county of Bandung. Makassar is the capital of South Sulawesi, located in the eastern part of Indonesia, with a population of 2 847 754 persons,12 while Medan is the capital of North Sumatera, located in the western part of Indonesia with 2 681 830 inhabitants.12 In the central part, the city of Bandung, West Java’s capital, was selected as the study setting with a total population of 2 510 103 persons.12 In addition, the county of Bandung, with a total population of 3 831 505,12 located around 50 km from the city of Bandung, was included as a representation of the peripheral area in this study.
In Indonesia, a pharmacy called apotek is a community pharmacy managed by the private sector. It can be a chain pharmacy or an independent pharmacy. According to the national regulation, a pharmacy is a facility where a pharmacist performs pharmaceutical practices in the community.13 Hence, a pharmacy must be under the authority of a pharmacist who holds a professional degree in pharmacy and a pharmaceutical license from the Ministry of Health, Republic of Indonesia. One or more pharmacy technicians support a responsible pharmacist in a pharmacy. A pharmacy technician should hold a pharmaceutical practice licence from the government and have a formal pharmaceutical education, at least in the pharmaceutical vocational school, equivalent to a senior high school education level.13
Questionnaire development and validation
A validated questionnaire was developed as the instrument for data collection. The questionnaire was developed based on the guideline for KAP survey in TB published by the WHO,14 the practice of survey research,15 the Indonesian national TB guideline,16 experts’ consensus on the psychological factors for implementing evidence-based practices17 and previous relevant studies.18–20
We defined four assessment domains, that is, the participant’s characteristics, KAP in TBPD. The domain for participant characteristics consisted of age, marital status, professional background, educational level, study site, working experience, an average of working hours per week, type of pharmacy (chain/ independent pharmacy), number of pharmacies for the pharmaceutical practice, availability of a physician practice in the pharmacy, providing drug consultation services and experience in TB training.
We assessed TB knowledge related to activities in TB detection, that is, TB pathogen, transmission, symptoms, risk population, diagnosis and medication. Given the experts’ consensus on the essential psychological determinants for implementing evidence based practice,17 the attitude domain was defined as the beliefs in the professional role, capability and consequences of the activities for TBPD. Finally, we defined practices of TBPD as the activities in the screening of TB signs and symptoms, communicating with TB healthcare workers, and referring a patient with presumptive TB to the health facility for further examination in the past 6 months.
The participant’s characteristics domain items were assessed using closed and short open questions, while the item of knowledge domain was measured on a nominal scale (‘true’, ‘false’ and ‘do not know’). Five Likert scales were used for the attitude, while rating scales were used for practice domain items. We used ‘strongly agree’, ‘agree’, ‘doubt’, ‘disagree’ and ‘strongly disagree’ for the attitude items, and ‘very often’, ‘often’, ‘sometimes’, ‘rarely’ and ‘never’ for the frequency of practice items. The TBPD practice was evaluated over the past 6 months. The 6 months were based on the results of our previous qualitative studies that there was the pharmacy personnel who provided the TBPD practice at least once 6 months.11 21 To have a clear definition and comprehensive duration assessment, we defined ‘very often’ as the practice performed at least every week; ‘often’ is the practice performed at least once a month; ‘sometimes’ is the practice performed at least once in 2–4 months; ‘rarely’ is the practice performed once in 5–6 months; and ‘never’ is never doing the practice in the last 6 months.
We assigned the questionnaire for face and content validation to experts with several backgrounds, that is, an epidemiologist, a pharmacist, an assistant pharmacist and a TB specialist. In light of the expert judgements, ISP (TB researcher) and EF (statistician and item developer) finalised the items. A pilot study involving 200 participants who were different from the participants was conducted for the validity and reliability test of the instrument.
Study size, participant and data collection
We included participants who had an educational background as a pharmacist or a pharmacy technician; were working as pharmaceutical workers at the community pharmacy; and had experience in the pharmacy for at least 6 months. The 6-month experience was defined considering that the study captured TBPD activities in the last 6 months. We excluded participants if they worked outside the pharmacy (eg, in a community health centre or hospital) or were underqualified according to the national regulation.
We used pharmacies as the unit sample in this study. An estimated 1800 pharmacies in all the study sites were defined as the sample frame, considering the government and professional organisation data.22 The study used an online Raosoft sample size estimator to identify a minimum sample size.23 In view of a 5% of margin error, 95% confidence level and 50% response distribution, we identified a total of 317 pharmacies as the minimum sample size in this study.
Data were obtained from July to October 2021. Considering that pharmacists and pharmacy technicians operate pharmacies, two responsible persons for data collection were appointed in each study site, that is, a data collector for the pharmacists and one for the pharmacy technicians. We collaborated with the two local professional organisations for data collection. The responsible data collector identified and distributed the questionnaire to the potential participants based on the participant eligibility, database, networking and geographical distribution at the district level. In light of the pandemic COVID-19 situation, we distributed the questionnaire using online and offline approaches. All the collected data were managed and analysed for eligibility of the data and achievement of the sample size by the researchers at each study site (ISP, KK, MAB and MNK).
Data analysis
In the pilot study, we tested the item validity using a correlation between the score of each item and the total score. A correlation between items was defined if the p value of the Pearson correlation coefficient (r) was below 0.05.24The reliability test was conducted by identifying Cronbach’s alpha, which should be more than 0.60 for an acceptably reliable item.25 26
Descriptive statistics were used to analyse the characteristics of participants. Categorical data were described as numbers and percentages. Median and IQR were used for continuous and non-normally distributed data. As to the knowledge domain, percentages of participants who had correct answers per item were reported, while in the attitude and practice domain, percentages referred to participants who chose a particular scale in the items.
We performed a multivariable regression analysis to identify factors associated with the practice of TBPD. The normality of the residual was identified by assessing the shape of the residual histogram and the probability-probability plot. Multicollinearity was evaluated by identifying the variance inflation factor less than 5.27 Subgroup analysis was performed to have a comprehensive picture from the multivariable analysis. We used logistic regression analysis in the subgroup analysis when the outcome was binary data, while linear regression analysis was used when the outcome data was numeric. We also analysed risk groups for poor TB knowledge and attitude as dependent variables. All significance levels were set at 5%, and 95% CIs were presented. Data management and analysis were performed anonymously, and the analyses were conducted using SPSS V.26.
An unpublished protocol was developed prior to the study to provide better study planning and guidance for the research team. The Strengthening the Reporting of Observational Studies in Epidemiology guideline for a cross-sectional study was followed to achieve systematic and transparent study reporting.28
Patient and public involvement
The research question was developed considering the previous interviews and focus group discussions involving patients with TB, a non-governmental organisation, health service providers and pharmacists. We involved the representation of professional organisations in pharmacy for data collection.
Results
Questionnaire development and validation
In the phase of questionnaire development, all experts agreed that all items could be used for the research instrument. All items fulfilled the face and content validity with minor structural and content revisions. A total of 40 items were developed to assess participant characteristics (16), knowledge (17), attitude (4) and practice (3). After being revised, we distributed the items to 200 participants for the validity and reliability test.
The KAP items were significantly correlated with each total item (p<0.05). Similarly, all the KAP items were reliable since Cronbach’s alpha ranged from 0.63 to 0.79. The participants’ characteristics, validity and reliability test in the pilot study can be seen in online supplemental files 1–3, respectively.
bmjopen-2021-060078supp001.pdf (77.9KB, pdf)
Study size and participant characteristics
We successfully collected data from 979 pharmacies with 1242 subjects, from much more than the 317 pharmacies defined as the minimum sample size. However, we excluded 113 subjects due to an underqualified education level (4) and working outside of the community pharmacy (109). Finally, we included 1129 participants for further data analysis. We identified that the participant backgrounds were relative balance, that is, 56.6% were pharmacists, and 43.6% were pharmacy technicians. The flow diagram of the included participants is presented in figure 1.
Figure 1.
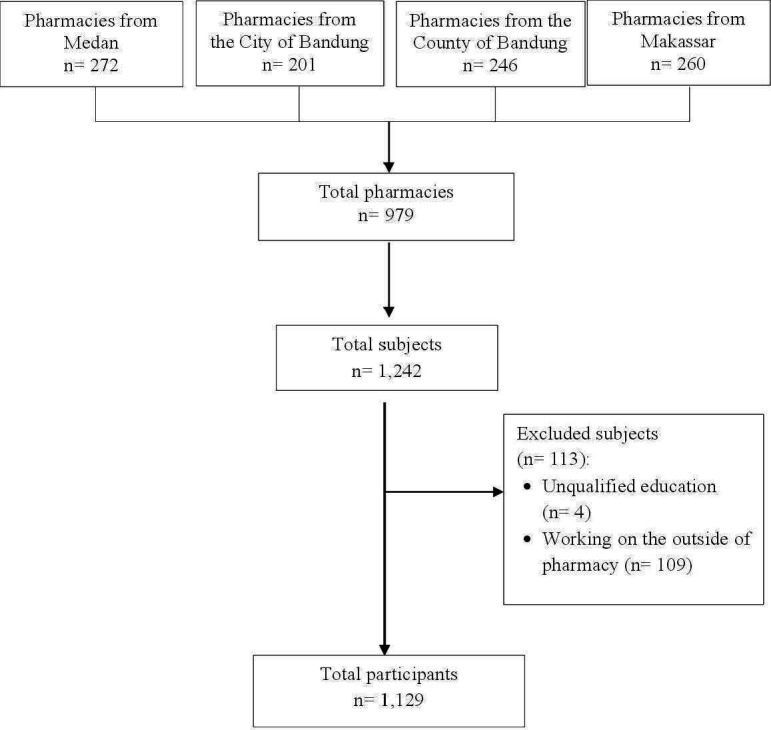
The flow diagram of the included participants.
We identified that the median age, working experience and average working hours were 29 years old (IQR: 9), 3 years (IQR: 4) and 40 hours per week (IQR: 48), respectively. The majority of participants had an educational level at the professional degree of pharmacist (48.7%), followed by senior high school or equivalent (17.8%) and the rest (33.5%). We assessed that only a small proportion of participants provided drug consultation services in their pharmacies (13.4%). In terms of TB training, almost half of the participants never had TB training (49.3%). The characteristics of the main study participants can be seen in table 1.
Table 1.
Characteristics of the study participants (n=1129)
| No | Characteristics | No |
| Sociodemographic characteristics | ||
| 1 | Female (no, %) | 910 (80.6) |
| 2 | Age in year (median, IQR) | 29 (9) |
| 3 | Marital status (no, %) | |
| Single | 480 (42.5) | |
| Married | 630 (55.8) | |
| Widow/widower | 19 (1.7) | |
| 4 | Educational level (no, %) | |
| Vocational pharmacy school or equivalent | 201 (17.8) | |
| Diploma | 142 (12.6) | |
| Bachelor | 147 (13.0) | |
| Pharmacist | 550 (48.7) | |
| Master | 81 (7.2) | |
| Doctor | 8 (0.7) | |
| 5 | No of participants surveyed (no, %) | |
| City of Bandung | 240 (21.3) | |
| County of Bandung | 285 (25.2) | |
| City of Makassar | 280 (24.8) | |
| City of Medan | 324 (28.7) | |
| Professional characteristics | ||
| 4 | Professional background (no, %) | |
| Pharmacy technicians | 490 (43.4) | |
| Pharmacists | 639 (56.6) | |
| 7 | Working experience in years (median, IQR) | 3 (4) |
| 8 | Average working time in hours per week (median, IQR) | 40 (28) |
| 9 | No of practice places (no, %) | |
| One pharmacy | 987 (87.4) | |
| Two pharmacies | 86 (7.6) | |
| Three pharmacies | 6 (0.5) | |
| More than three pharmacies | 50 (4.4) | |
| 10 | Providing drug consultation services (no, %) | 151 (13.4) |
| Pharmacy characteristics | ||
| 11 | Type of pharmacy (no, %) | |
| Chain pharmacy | 264 (23.4) | |
| Independent pharmacy | 865 (76.6) | |
| 12 | Availability of a physician practice in the pharmacy (no, %) | 464 (41.1) |
| TB-related characteristics | ||
| 13 | Experience in TB training (no, %) | |
| Never | 557 (49.3) | |
| More than 2 years ago | 225 (19.9) | |
| 1–2 years ago | 191 (16.9) | |
| 6 months to 1 year ago | 90 (8.0) | |
| Less than 6 months ago | 66 (5.8) | |
IQR, Interquartile range; TB, tuberculosis.
Knowledge of pharmacy personnel on TB
We assessed that most of the TB knowledge items were correctly answered by the participants. However, correct responses concerning TB signs and symptoms, risk population and TB medication were given by no more than 70% of the participants. The participants inappropriately answered about general signs of pulmonary TB (70.5%). The participants did not know that diabetes mellitus is a risk factor for TB disease (45%). Moreover, although the participants had a pharmaceutical background, they were not familiar with the TB treatment regimen for drug-sensitive TB and how to take the medication, either with or without food. The percentages of participants who correctly answered on the first-line regimen for drug-sensitive TB in the intensive treatment phase; the first-line regimen for drug-sensitive TB in the continuous treatment phase; and the preferable utilisation of the first-line anti-TB drugs on an empty stomach were only 62.4%, 54.5% and 45.3%, respectively. The proportion of the correct answers in the TB knowledge items is presented in table 2.
Table 2.
The items of TB knowledge (n=1129)
| No | Concept | Items | Correct answer (%) |
| 1 | The pathogen | TB is caused by virus | 70.9 |
| 2 | TB transmission | TB does not only spread into the lungs but also to other parts of the body, for example, eyes, joints and bone | 82.1 |
| TB can spread by droplets from coughing or sneezing of a pulmonary TB patient | 97.7 | ||
| The droplet containing the TB pathogen can stay longer in a room with minimum ventilation | 88.5 | ||
| 3 | TB sign and symptom | Coughing for more than equal 2 weeks is a general sign of pulmonary TB | 82.4 |
| An active TB patient can cough up blood | 95.9 | ||
| The general signs of pulmonary TB, that is, loss of body weight, chest pain, sweat at night and fever for more than a month | 29.5 | ||
| 4 | Risk population | Diabetes mellitus is a risk factor for having TB | 55 |
| HIV infection is a risk factor for having TB | 84.4 | ||
| Children under 5 years old is a risk group for TB disease | 75.6 | ||
| 5 | TB diagnosis procedure | A microscopic test of the TB patient’s sputum is a diagnostic approach for TB | 87.7 |
| A rapid molecular test of the TB patient’s sputum is a diagnostic approach for TB | 76.3 | ||
| 6 | TB medication and its use | The first-line anti-TB regimen for the intensive phase | 62.4 |
| The first-line anti-TB regimen for the continued phase | 54.5 | ||
| Taking anti-TB drugs without food | 45.3 | ||
| 7 | Adverse drug reaction and drug monitoring | Adverse drug reactions of isoniazid | 87.2 |
| Adverse drug reactions of rifampicin | 78.2 |
HIV, Human Immunodeficiency Virus; TB, Tuberculosis.
The attitude of pharmacy personnel towards TBPD
Most participants believed they had a role (75.1%) and capability (65.4%) to detect patients with TB in their pharmacy. The majority of participants also felt guilty if they did not make any effort to detect patients with TB (67.4%). On the other hand, 58.2% of participants believed they had significant barriers to finding patients with TB in their workplace. It highlighted that most participants realised they faced significant barriers to performing TBPD in their pharmacies. The attitude of the participant is presented in table 3.
Table 3.
The items of attitude for TB patient detection (n=1129)
| No | Concept | Items | % | ||||
| Strongly agree | Agree | Doubt | Disagree | Strongly disagree | |||
| 1 | The professional role | I have a role in finding TB patients in my workplace | 21 | 54.1 | 15.1 | 9.2 | 0.6 |
| 2 | The capability | I can screen TB signs and symptoms for presumptive TB patients who visit my workplace | 11.9 | 53.5 | 23.1 | 9.8 | 1.7 |
| I feel that there are no significant barriers to finding new TB patients in my workplace | 7 | 33.8 | 36.6 | 21.2 | 1.4 | ||
| 3 | The consequence | I feel guilty if I do not make any efforts to find new TB patients in my workplace | 21.2 | 46.2 | 19.1 | 20.6 | 1.8 |
TB, tuberculosis.
The practice of pharmacy personnel towards TBPD
Our study demonstrated that most participants did not always perform practice in TBPD. Only a small proportion of the participants routinely conducted TB screening (2%), suggested patients with presumptive TB for further examination (6.6%), and communicated with TB healthcare providers about referring patients with presumptive TB (1.8%) every week in the last 6 months. We assessed that more than 15% of the participants had never performed TBPD in their pharmacy in the last 6 months. The remaining participants stated that practising TBPD was performed once every 2–6 months. The practice of TBPD in the included participants is shown in table 4.
Table 4.
The items of the practice in TB patient detection (n=1129)
| No | Items | % | ||||
| Very often | Often | Sometimes | Rarely | Never | ||
| 1 | Practice in screening TB signs and symptoms for the presumptive TB patient | 2 | 10.9 | 27.1 | 35.2 | 24.8 |
| 2 | Practice in suggesting presumptive TB patients for further health examination to the community health centre or health facility | 6.6 | 26.8 | 24.4 | 25.8 | 16.4 |
| 3 | Practice communicating with TB healthcare providers in referring the presumptive TB patient to them | 1.8 | 11.1 | 16.5 | 26.5 | 44.2 |
Information: Very often: at least every week; often: at least every month; sometimes: at least once 2–4 months; rarely: at least once 5–6 months; never: never doing the activities in the last 6 months.
TB, tuberculosis.
Factors associated with TB practice and the exploratory analyses
We included all participant characteristics, TB knowledge and attitude items in a regression analysis to identify factors associated with the practice of TBPD. Multicollinearity was identified in the factors of education level and professional background. We, therefore, removed the determinant of the level of education in the regression analysis. After it had been removed, the regression assumption was fulfilled since the residual data were normally distributed and no multicollinearity occurred (online supplemental file 4)
The regression analysis showed that male gender (Beta coefficient, B=0.41; p<0.05; 95% CI 0.02 to 0.80), providing drug consultation services (B=0.68; p<0.05; 95% CI 0.23 to 1.14), experience in TB training (B=0.83; p<0.001; 95%CI 0.52 to 1.15), working hours per week (B=−0.16; p<0.05; 95%CI −0.03 to −0.01), being a participant from the county of Bandung (B=−0.52; p<0.05; 95% CI −0.99 to −0.05) and a positive attitude on TBPD (B=0.34; p<0.001; 95% CI 0.29 to 0.40) were significant factors for TBPD practice. Of note, the beta coefficients were negative for the factor of working hours and for being a participant from the county of Bandung, which means that the factors had negative effects on TBPD activities. A higher beta coefficient represented the more influential factors. To have a comprehensive picture of the association between gender and TBPD practice, we conducted a subgroup analysis of the gender variable. The subgroup analysis showed that age, providing drug consultation services and positive attitude towards TBPD were associated with the male gender. The multivariable regression analysis of the factors associated with the practice of TBPD and the gender analysis are presented in online supplemental files 4 and 5.
Assuming TB knowledge and attitude were associated with TBPD practice, we explored factors associated with TB knowledge and attitude. In terms of TB knowledge, we found that age (B=0.07; p<0.05; 95% CI 0.03 to 0.10), being a pharmacist (B=2.2; p<0.001; 95% CI 1.68 to 2.63), experience in TB training (B=0.65; p<0.001; 95% CI 0.25 to 1.04) and a positive attitude on TBPD (B=0.1: p<0.001; 95% CI 0.03 to 0.17) were positively associated with TB knowledge. Meanwhile, the factors of being a participant from the county of Bandung (B=−1.04; p<0.001; 95% CI −1.63 to −0.45) and from the city of Makassar (B=−1.13; p<0.001; 95% CI −1.70 to −0.55) were negatively associated with TB knowledge as compared with being a participant from the city of Bandung.
Regarding the attitude, the analysis demonstrated that factors positively associated with TB attitude were male gender (B=0.68; p<0.001; 95% CI 0.26 to 1.09), TB knowledge (B=0.74; p<0.001; 95% CI 0.02 to 0.12), provision of drug consultation services (B=0.91; p<0.001; 95% CI 1.40 to 0.68), experience in TB training (B=0.84; p<0.001; 95% CI 0.51 to 1.16), being a participant from the county of Bandung (B=0.93; p<0.001; 95% CI 0.44 to 1.43) and city of Makassar (B=0.51; p<0.05; 95% CI 0.02 to 0.99). Meanwhile, working in a chain pharmacy (B=−0.64; p<0.001; 95% CI −1.07 to −0.21) was negatively associated with TBPD attitude. The regression analyses on the factors associated with TB knowledge and attitude, are presented in online supplemental file 4.
Generally, our study demonstrated that exposure to TB training is strongly associated with improving TB knowledge (B=0.65; p<0.001; 95% CI 0.25 to 1.04), attitude (B=0.84; p<0.001; 95% CI 0.51 to 1.16), and practice (B=0.83; p<0.001; 95% CI 0.52 to 1.15) in TBPD.
Discussion
Our study demonstrated that knowledge of TB as a disease was present among pharmacists and pharmacy technicians. However, a minority had incorrect responses on TB knowledge items. Despite their pharmaceutical background, many participants were unfamiliar with the first-line treatment regimen for drug-susceptible TB. As to their attitude, most participants showed a role and capacity to detect patients with TB in their pharmacy, but they realised significant barriers in performing TBPD. In this respect, only a small proportion of participants already performed TBPD practices in their community pharmacies.
In terms of TB knowledge, our participants showed a high understanding of several topics, such as TB transmission, diagnostic procedures and potential adverse drug reactions. However, the participants should be strengthened in their knowledge about TB signs and symptoms, risk population, and medication since those knowledge scores were relatively low. Good knowledge was associated with participants who have a pharmacist background. This finding highlights the importance of exposing TB knowledge to the pharmacy technicians since they also have a role as the front line in pharmacy. Unintegrated pharmaceutical services in TB programmes and a lack of public–private collaboration with community pharmacies were reported in Indonesia.11 21 This potentially leads to the limited exposure of community pharmacy personnel to the educational programme from the national TB programme.
Insufficient TB knowledge was also reported by a private retail survey in Tanzania that demonstrated that the observed participants did not fully understand TB symptoms and the risk factors of TB.29 Although some items are slightly different across the studies, studies on community pharmacies in Peru,30 Tanzania29 and Pakistan20 showed that community pharmacy personnel has the basic knowledge of TB that can support them in conducting activities in TBPD.
Practising TBPD in the pharmacy was associated with experience in TB training, a positive attitude towards TBPD, provision of drug consultation services, male gender, short working hours per week and pharmacies located in central city areas. We finally found that experience in following TB training is essential for improving TB knowledge, forming a positive attitude and performing activities on TBPD. Our study thus emphasises the importance of TB training to gain TB knowledge and a positive attitude. The knowledge and attitude can then generate action for TBPD. It is in line with the KAP theory that states that the changes in human behaviour are divided into three successive processes, that is, knowledge acquisition, the generation of attitudes and the formation of behaviour.31 In the health belief model, knowledge plays a key role in generating action, and then belief and attitude drive behaviour change.32
Next to TB training and a positive attitude, we identified other factors relevant to the TBPD practice, such as male gender and providing drug consultation services. We identified that the proportion of females (80.6%) is higher than males (19.4%) in our study. It is in line with national data showing that females represent the majority of pharmaceutical personnel in Indonesia (80.6%).33 Although the proportion of females is higher than males, our study identified that males are more likely to perform TBPD practices. Our subgroup analysis explained that males have a more positive attitude towards TBPD and provide more drug consultation services than females (see online supplemental file 5). The positive attitude may drive them to provide the drug consultation service and lead them to perform TBPD activities as well. It can be explained that providing drug consultation services will give them more opportunities to meet patients directly, leading to the TBPD activities. However, further study is needed to have a more comprehensive picture of the associations that include other relevant variables.
Furthermore, we assessed that time available to perform TBPD activities is essential. Our study emphasised the need for workload assessment for the community pharmacies to be able to conduct TBPD activities. This conclusion is supported by a KAP study in Peru that showed that lack of time is the main problem in managing TB patient management among pharmacies.30 Supporting our findings, studies in India and Indonesia identified that patient volume and workload are the barriers to performing TBPD activities and pharmaceutical services in community pharmacies.34 35
In the geographical aspect, our study revealed that pharmacy personnel in a peripheral city area has fewer TBPD practices than the pharmacy personnel in the central city. However, the differences in knowledge and attitude between the areas cannot be analysed clearly. This finding underlines that unidentified factors other than knowledge and attitude may affect the practice of TBPD in a particular area. A systematic review describes that several factors can affect healthcare practices, such as guidelines, individual healthcare providers, patients, professional interaction, incentives and resources, capacity for organisational change, social, political and legal factors.36 Hence, a comprehensive analysis may be beneficial to analyse the geographical effect on the TBPD activities.
This study, however, has limitations. First, this is a self-reported study that may be biased by social desirability. This means that participants may respond in a socially acceptable way that contradicts the facts. Second, formally no causal relations can be inferred between factors related to patient characteristics, knowledge and attitude on the one hand and TBPD practice on the other hand since the nature of a cross-sectional study does not consider the time difference between the causal factors and the eventual effect. However, several efforts were made to minimise potential bias and increase this study’s validity and reliability. We stated in the questionnaire that data would be analysed and presented anonymously. This can minimise social desirability bias since the participant’s identity would be unknown. We also collaborated with professional organisations that have a broad network and a list of pharmacies in the study sites for data collection. Hence, we reached a high number of pharmacies and participants that could be considered highly representative of the target population.
We analysed that the community pharmacy is a potential facility to increase TBPD. It considers that most community pharmacy personnel already has certain basic knowledge and a positive attitude towards TBPD. Moreover, the evidence shows that they are indeed the main facility to seek first aid medication for patients with TB.3–8 Other evidence from India, Pakistan and Tanzania also supported that community pharmacies can help in detecting patients with TB in the community.37–39 However, a comprehensive strategy is required to follow up on this study to implement TBPD activities among pharmacy personnel.
First, further study is needed to comprehensively analyse the local determinants affecting TBPD activities, including guidelines, patients, professional interactions, incentives, resources, capacity for organisational change, and social, political, and legal factors. A qualitative study may be beneficial to explore in detail voices from the field related to the local determinants and partnership strategies from the relevant stakeholders. A future intervention can then be developed based on the identified local determinants and partnership strategies. Second, a TB training system for improving the KAP should be developed for pharmacy personnel. The training is not only for increasing TB awareness about case detection activities but also for minimising irrational dispense of TB drugs40 and raising awareness on the other potential roles of community pharmacy in TB (eg, treatment supporter, TB medication counsellor). As a treatment supporter, pharmacy personnel can potentially reduce the clinical and economic impacts of TB medication adherence.41–43 Third, integrating the role of community pharmacy in TB patient management within National Tuberculosis Programmes (NTPs) is essential to have the same vision and concept in accelerating TB elimination. Finally, technical guidance for performing TBPD in pharmacies and integrating the activities in NTPs should also be developed to have a successful community pharmacy engagement programme, especially in TBPD activities.
Conclusion
Our study showed that most Indonesian pharmacists and pharmacy technicians have a good knowledge and attitude related to TBPD. However, their knowledge and attitude do not align with their actual TBPD practice. We identified that a TB educational programme is essential in improving KAP among pharmacy personnel for TBPD activities. A systematic and comprehensive assessment is needed to develop an effective strategy for engaging the community pharmacy in sustainable TBPD activities.
Supplementary Material
Acknowledgments
We wish to thank Indonesian Pharmacist Association (IAI=Ikatan Apoteker Indonesia) and Pharmacy Technician Association (PAFI=Perhimpunan Ahli Farmasi Indonesia), who supported this study.
Footnotes
Contributors: Main idea: ISP; Conception and design of the work: ISP, KK, MAB, EF; Data acquisition: ISP, KK, MAB, MNK; Data analysis and interpretation: ISP, EF, RR, RAa, RAb; Preparing the first draft: ISP; Guarantor: ISP; Substantial revision of the manuscript: all authors; approval for the final manuscript: all authors.
Funding: We acknowledge the collaborative research funding 2021 under the scheme of PPKI (Program Penelitian Kolaborasi Indonesia), Ministry of Education, Research, Technology and Higher Education, Republic of Indonesia, for Ivan S. Pradipta (Universitas Padjadjaran) and Kharunnisa (Universitas Sumatera Utara).
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were involved in the design, or conduct, or reporting, or dissemination plans of this research. Refer to the Methods section for further details.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
Data are available on reasonable request. Data are available on reasonable request. The data were managed at the Department of Pharmacology and Clinical Pharmacy, Universitas Padjadjaran, under the supervision of Ivan S. Pradipta, PhD.
Ethics statements
Patient consent for publication
Not applicable.
Ethics approval
This study involves human participants and was approved by Universitas Sumatera Utara, IndonesiaNo. 599/KEP/USU/2021. Participants gave informed consent to participate in the study before taking part.
References
- 1.WHO . Global tuberculosis report 2021. Geneva, 2021. [Google Scholar]
- 2.Miller R, Goodman C. Quality of tuberculosis care by pharmacies in low- and middle-income countries: gaps and opportunities. J Clin Tuberc Other Mycobact Dis 2020;18:100135. 10.1016/j.jctube.2019.100135 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lestari BW, McAllister S, Hadisoemarto PF, et al. Patient pathways and delays to diagnosis and treatment of tuberculosis in an urban setting in Indonesia. Lancet Reg Health West Pac 2020;5:100059. 10.1016/j.lanwpc.2020.100059 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Surya A, Setyaningsih B, Suryani Nasution H, et al. Quality tuberculosis care in Indonesia: using patient pathway analysis to optimize public-private collaboration. J Infect Dis 2017;216:S724–32. 10.1093/infdis/jix379 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lönnroth K, Uplekar M, Blanc L. Hard gains through soft contracts: productive engagement of private providers in tuberculosis control. Bull World Health Organ 2006;84:876–83. 10.2471/BLT.06.029983 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Daftary A, Jha N, Pai M. Enhancing the role of pharmacists in the cascade of tuberculosis care. J Epidemiol Glob Health 2017;7:1–4. 10.1016/j.jegh.2016.05.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kiwuwa MS, Charles K, Harriet MK. Patient and health service delay in pulmonary tuberculosis patients attending a referral Hospital: a cross-sectional study. BMC Public Health 2005;5:122. 10.1186/1471-2458-5-122 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sreeramareddy CT, Qin ZZ, Satyanarayana S, et al. Delays in diagnosis and treatment of pulmonary tuberculosis in India: a systematic review. Int J Tuberc Lung Dis 2014;18:255–66. 10.5588/ijtld.13.0585 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Satyanarayana S, Kwan A, Daniels B, et al. Use of standardised patients to assess antibiotic dispensing for tuberculosis by pharmacies in urban India: a cross-sectional study. Lancet Infect Dis 2016;16:1261–8. 10.1016/S1473-3099(16)30215-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Zawahir S, Le H, Nguyen TA, et al. Standardised patient study to assess tuberculosis case detection within the private pharmacy sector in Vietnam. BMJ Glob Health 2021;6:e006475. 10.1136/bmjgh-2021-006475 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Pradipta IS, Idrus LR, Probandari A, et al. Barriers and strategies to successful tuberculosis treatment in a high-burden tuberculosis setting: a qualitative study from the patient’s perspective. BMC Public Health 2021;21:1–12. 10.1186/s12889-021-12005-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Badan Pusat Statistik . Badan Pusat Statistik, 2017: 335–58. [Google Scholar]
- 13.Ministry of health Republic of Indonesia . Peraturan Menteri Kesehatan Republik Indonesia, 2011. [Google Scholar]
- 14.WHO . Advocacy, communication and social mobilization for TB control. A guide to developing knowledge, attitude and practice surveys, 2008. [Google Scholar]
- 15.Ruel E, Wagner III WE, Gillespie BJ. The practice of survey research: theory and applications, 2016. [Google Scholar]
- 16.Ministry of health Republic of Indonesia . Peraturan menteri kesehatan Republik Indonesia no 67 tahun 2016 tentang penanggulangan tuberkulosis, 2010. [Google Scholar]
- 17.Michie S, Johnston M, Abraham C, et al. Making psychological theory useful for implementing evidence based practice: a consensus approach. Qual Saf Health Care 2005;14:26–33. 10.1136/qshc.2004.011155 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wahab FA, Abdullah S, Abdullah JM, et al. Updates on knowledge, attitude and preventive practices on tuberculosis among healthcare workers. Malays J Med Sci 2016;23:25–34. 10.21315/mjms2016.23.6.3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Alotaibi B, Yassin Y, Mushi A, et al. Tuberculosis knowledge, attitude and practice among healthcare workers during the 2016 hajj. PLoS One 2019;14:e0210913. 10.1371/journal.pone.0210913 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mustafa T, Shahzad Y, Kiani A. A survey of knowledge, attitude, and practices of private retail pharmacies staff in tuberculosis care: study from Dera Ismail Khan City, Pakistan. J Pharm Policy Pract 2018;11:7. 10.1186/s40545-018-0134-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Pradipta IS, Idrus LR, Probandari A, et al. Barriers to optimal tuberculosis treatment services at community health centers: a qualitative study from a high prevalent tuberculosis country. Front Pharmacol 2022;13:936. 10.3389/fphar.2022.857783 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Jumlah Apotek Berdasarkan Kabupaten/Kota di Jawa Barat. Available: https://opendata.jabarprov.go.id/id/dataset/jumlah-apotek-berdasarkan-kabupatenkota-di-jawa-barat [Accessed 2 Nov 2021].
- 23.Sample size calculator by Raosoft, Inc. Available: http://www.raosoft.com/samplesize.html [Accessed 26 Oct 2021].
- 24.Cohen S, Mark E., RJ. Psychological testing and assessment : an introduction to tests and measurement, 2018. [Google Scholar]
- 25.Taber KS. The Use of Cronbach’s Alpha When Developing and Reporting Research Instruments in Science Education. Res Sci Educ 2018;48:1273–96. 10.1007/s11165-016-9602-2 [DOI] [Google Scholar]
- 26.RALF vanG, van Eijck MW, Haste H. Global Patterns in Students’ Views of Science and Interest in Science. Res Sci Educ 2014;45:581–603. [Google Scholar]
- 27.Vatcheva KP, Lee M, McCormick JB, et al. Multicollinearity in regression analyses conducted in epidemiologic studies. Epidemiology 2016;6. 10.4172/2161-1165.1000227. [Epub ahead of print: 07 03 2016]. 10.4172/2161-1165.1000227 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.von Elm E, Altman DG, Egger M, et al. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. The Lancet 2007;370:1453–7. 10.1016/S0140-6736(07)61602-X [DOI] [PubMed] [Google Scholar]
- 29.Rutta E, Tarimo A, Delmotte E, et al. Understanding private retail drug outlet dispenser knowledge and practices in tuberculosis care in Tanzania. Int J Tuberc Lung Dis 2014;18:1108–13. 10.5588/ijtld.14.0020 [DOI] [PubMed] [Google Scholar]
- 30.García PJ, Hernández-Córdova G, Pourjavaheri P, et al. Knowledge, attitudes and practices related to tuberculosis in pharmacy workers in a cross-sectional survey in El Agustino, Peru. PLoS One 2018;13:e0196648. 10.1371/journal.pone.0196648 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Fan Y, Zhang S, Li Y, et al. Development and psychometric testing of the knowledge, attitudes and practices (KAP) questionnaire among student tuberculosis (TB) patients (STBP-KAPQ) in China. BMC Infect Dis 2018;18:213. 10.1186/s12879-018-3122-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Rosenstock IM. Historical origins of the health belief model. Health Educ Monogr 1974;2:328–35. 10.1177/109019817400200403 [DOI] [PubMed] [Google Scholar]
- 33.Ministry of health Republic of Indonesia . Health information system 2020. Jakarta, 2021. [Google Scholar]
- 34.Gayathri P, Shah PB, Rajanandh MG. Barriers of community pharmacists in identification and referral of presumptive tuberculosis cases in Tiruvallur district of Tamil Nadu. Indian J Tuberc 2020;67:560–3. 10.1016/j.ijtb.2020.07.018 [DOI] [PubMed] [Google Scholar]
- 35.Abdulah R, Barliana MI, Pradipta IS. Assessment of patient care indicators at community pharmacies in Bandung City, Indonesia. Southeast Asian J Trop Med Public Health 2014;45:1196–201. [PubMed] [Google Scholar]
- 36.Flottorp SA, Oxman AD, Krause J, et al. A checklist for identifying determinants of practice: a systematic review and synthesis of frameworks and taxonomies of factors that prevent or enable improvements in healthcare professional practice. Implement Sci 2013;8:35. 10.1186/1748-5908-8-35 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Daftary A, Satyanarayana S, Jha N, et al. Can community pharmacists improve tuberculosis case finding? a mixed methods intervention study in India. BMJ Glob Health 2019;4:e001417. 10.1136/bmjgh-2019-001417 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Ullah W, Almansour H, Fatima R, et al. Engaging community pharmacies in early detection of missing tuberculosis patients through public-private mix intervention in Pakistan. Am J Trop Med Hyg 2020;103:221–30. 10.4269/ajtmh.19-0939 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Colvin C, Mugyabuso J, Munuo G, et al. Evaluation of community-based interventions to improve TB case detection in a rural district of Tanzania. Glob Health Sci Pract 2014;2:219–25. 10.9745/GHSP-D-14-00026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Wulandari LPL, Khan M, Liverani M, et al. Prevalence and determinants of inappropriate antibiotic dispensing at private drug retail outlets in urban and rural areas of Indonesia: a mixed methods study. BMJ Glob Health 2021;6:e004993. 10.1136/bmjgh-2021-004993 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Chimeh RA, Gafar F, Pradipta IS, et al. Clinical and economic impact of medication non-adherence in drug-susceptible tuberculosis: a systematic review. Int J Tuberc Lung Dis 2020;24:811–9. 10.5588/ijtld.19.0754 [DOI] [PubMed] [Google Scholar]
- 42.Pradipta IS, Houtsma D, van Boven JFM, et al. Interventions to improve medication adherence in tuberculosis patients: a systematic review of randomized controlled studies. NPJ Prim Care Respir Med 2020;30:21. 10.1038/s41533-020-0179-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Ridho A, Alfian SD, van Boven JFM, et al. Digital health technologies to improve medication adherence and treatment outcomes in patients with tuberculosis: systematic review of randomized controlled trials. J Med Internet Res 2022;24:e33062. 10.2196/33062 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2021-060078supp001.pdf (77.9KB, pdf)
Data Availability Statement
Data are available on reasonable request. Data are available on reasonable request. The data were managed at the Department of Pharmacology and Clinical Pharmacy, Universitas Padjadjaran, under the supervision of Ivan S. Pradipta, PhD.


