Abstract
Chemical injuries can severely damage the ocular surface. We present the case of a man in his 40s with severe periocular chemical injury with total lid loss and severe exposure keratopathy. He sustained burns to 45% of his body surface area and needed tracheostomy and multiple full-thickness skin grafts. Both eyes required surgery, Boston type 1 keratoprosthesis and penetrating keratoplasty for the right and left eye, respectively. There was melting in the right eye and a persistent epithelial defect in the left eye. Eventually, we suggested 18 mm diameter scleral contact lenses for both eyes to aid in ocular surface stabilisation. His best corrected visual acuity improved significantly with the scleral lenses to 20/100 and 20/320 in the right and left eyes, respectively. This case demonstrates that scleral lenses can treat the complications of exposure keratopathy and can improve vision. Therefore, they may be considered for rehabilitation of the ocular surface in eyes with severe chemical periocular injuries.
Keywords: Eye, Anterior chamber
Background
Cases of vitriolage or acid attacks are on the rise worldwide.1 These attacks are life-altering, and survivors, especially women, have to deal with lifelong physical disabilities and the many social, psychological and economic consequences associated with such debilitation. As these chemical substances are thrown on the face, damage to the eyes is inevitable in many cases. The resultant ocular injuries are among the few acute ophthalmic emergencies. Although the targets of vitriolage are usually young women, cases have also been reported in men.2 Even with timely management, severe injuries can lead to marked visual impairment and disfigurement, affecting quality of life and resulting in long-term disabilities. Stabilising the ocular surface is of utmost importance to prevent further degradation leading to permanent visual loss. Such stabilisation becomes extremely challenging with associated severe periocular injuries, such as cicatricial entropion/ectropion, lagophthalmos, and partial or total lid loss. Definitive surgical interventions, including full-thickness skin grafting and eyelid reconstructive procedures, are often delayed due to the accompanying systemic debilitation. This case report demonstrates the role of scleral lenses in stabilising the ocular surface, preventing desiccation and eventual perforation, and providing visual rehabilitation in conditions with total lid loss.
Case presentation
We report the case of a man in his 40s with severe acid burns who presented to our eye hospital with decreased vision and total lid loss in both eyes following an acid attack. The man survived a sulfuric acid attack at his workplace, scalding his face, neck, trunk, arms and abdomen. He sustained burns to 45% of his total body surface area and underwent multiple life-saving emergency procedures at a multispecialty hospital, where he received full-thickness skin grafting of the scalp, abdomen and arms. He had bilateral periorbital burns with total lid loss and total lagophthalmos, which led to exposure keratopathy. Multiple failed surgical attempts were made to achieve lid closure and stabilise the ocular surface. He underwent surgery with Boston type 1 keratoprosthesis in the right eye and penetrating keratoplasty in the left eye (figure 1). The best corrected visual acuity (BCVA) in both eyes was that the patient was able to count fingers close to his face. There was no orbicularis function with poor Bell’s response, which is the normal protective reflexive upward movement of the front portion of the eyeball during eye closure or blinking.3 The right eye had pericylinder melting and the left eye had a persistent epithelial defect with loss of graft clarity.
Figure 1.

Digital image of the patient 2 weeks post severe chemical injury showing charred skin of the face, severe periocular injury with bilateral loss of eyelashes, cicatricial lagophthalmos and severe exposure keratopathy in both eyes.
Intensive treatment with lubricants was started started using a combination of hourly hydroxypropyl methylcellulose (HPMC) 0.3%, dextran 0.1%, glycerine 0.2% eye-drops, and HPMC 0.3% gel three times per day and ofloxacin 0.3% eye ointment at bedtime. He was advised to use scleral contact lenses (BostonSight SCLERAL (BSS), Boston, Massachusetts, USA) for both eyes to stabilise the ocular surface and prevent further damage from continuous exposure caused by lagophthalmos due to lid loss. A large 18 mm diagnostic scleral lens with an 8 mm base curve and front surface eccentricity option 1 (FSE1) was fitted in both eyes. The sagittal heights were 3200 μm and 3020 μm in the right and left eyes, respectively. Both lenses had 360° steep haptics. The right eye lens had a toricity of −0.15 at 12 o’clock, –0.15 at 6 o’clock and −0.25 at 9 o’clock positions, and the left eye lens had −0.15 at 12 o’clock, –0.20 at 3 o’clock and −0.25 at 6 o’clock positions. A spherical over scleral lens acceptance with −7.00 Dioptre Sphere (DS) and −9.00 DS improved his vision to 20/100 p and 20/320 p in the right and left eyes, respectively. The patient’s attendant was trained to insert and remove the lenses with non-preserved normal saline safely and confidently. The procedure for cleaning the lens using Crystal RGP Plus multipurpose solution (Classic, India) was explained to the patient and his attendant. The patient and his caretakers were also informed about the potential risks of mid-day fogging and infection.
The patient was comfortable with the scleral lenses and reported significant improvement in symptoms. The average wearing time was 18–20 hours/day, with intermittent removal of the lenses for cleaning and replacement of the preservative-free 0.9% normal saline. In the interim, a combination of chloramphenicol, polymyxin and dexamethasone ointment was applied to the ocular surface to prevent desiccation and minimise surface inflammation. A drop of 0.5% moxifloxacin was also added to the reservoir of these lenses to reduce the risk of secondary infection. At a 1-month follow-up visit (figures 2A, B and 3A, B), BCVA in the right eye improved to 20/80 with the scleral lens; however, vision in the left eye only improved enough to see hand movements close to face. This was because the patient discontinued use of scleral lens in the left eye (preferring to use lenses only on the right eye as vision in the right eye was better), leading to the formation of a sterile dried plaque on the surface of the graft involving the visual axis.
Figure 2.
Digital image of the patient (A) at 1 year post chemical injury showing bilateral total lid loss and poor Bell’s phenomena with severe exposure keratopathy. (B) Right eye with BostonSight SCLERAL lens in situ with keratoprosthesis and pericylinder sterile infiltrate from 12 o’clock to 4 o’clock and left eye with penetrating keratoplasty with central sterile plaque of 5×5 mm.
Figure 3.
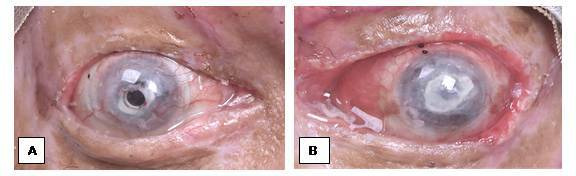
Digital image showing (A) the right eye with keratoprosthesis after 1 month of BSS use and (B) the left eye with failed graft and central plaque with BSS in situ. BSS, BostonSight SCLERAL lens.
Global health problem list
Epidemiology of acid attacks.
Morbidity caused by chemical injury.
Psychological effects of injury and associated disability.
Socioeconomic burden of the injury.
Medicolegal aspect of the injury.
Lack of rehabilitation services in rural and remote areas.
Availability of optimal care for acute and long-term burn management.
Financial and legal support.
Global health problem analysis
Epidemiology of acid attacks
Acid attacks are acts of violence where acid is thrown at an individual to disfigure and injure them.4 Sulfuric and nitric acid are commonly used for this purpose; however, the use of strong alkali such as sodium hydroxide has also been reported.5 Globally, approximately 1500 cases of acid attacks are reported every year.6 The highest number of cases was reported from the UK with cases increasing from 482 in 2017 to 501 in 2018.1 Colombia reports 100 cases per year.1 Reported cases of acid attacks were highest in Bangladesh.7 However, the cases dropped from 3000 in 1999 to 116 in 2009.7 In the last few years, there has also been a rise in the number of reported cases in South Asian countries.8–10 Pakistan reported 80 incidents of corrosive attacks in 2018.1 In the Indian subcontinent, 80% of patients are young women.11 Common reasons for such attacks are refusal of a marriage proposal, dowry demands, property or political disputes, revenge, jealousy, or domestic violence.2 12 Most of these cases occur in the rural areas of developing countries.13 According to the Acid Survivors Trust International,1 cases of acid attacks are often under-reported due to various reasons. Victims are mostly scared and ashamed of their injury. In developing countries, data for epidemiological analysis are inadequate14 and are usually gathered from urban areas, leading to an underestimation of cases from rural or remote parts. Of the 1500 cases reported globally, approximately 1000 cases were from India, although this still does not reflect the true numbers.6 Kumar15 mentioned the poor availability of resources to cope with this crime in rural areas of the country.
Morbidity caused by chemical injury
Acid attacks are mostly targeted at the face.16 These corrosive substances burn the face, melt the flesh and can penetrate deep into the bones, causing permanent damage and disfiguration.5 They can also destroy the skull bones, permanently damage the eyes and cause blindness, melt the cartilages of the ear, nose and mouth, and cause permanent contractures in the neck, chest and shoulders, leading to a lifetime of medical complications.2
Psychological effects of the injury and the associated disability
In many cases, these physical injuries are not fatal and therefore individuals must endure the psychological trauma of the attack and live in fear of another attack.17 Moreover, they suffer from headaches, weakness, depression, anxiety, insomnia, nightmares and a sense of worthlessness, and are often ashamed of their disfiguration.18 19
Socioeconomic burden of the injury
After surviving an acid attack, individuals often become dependent on their family for life. The wounds heal slowly and take months to close. Moreover, patients undergo multiple reconstructive procedures, adding to the financial burden of the family.17 20 Governments in many countries provide financial compensation, but is often inadequate. The Indian Supreme Court, for example, approved compensation payments of 300 000 rupees ($4760) to survivors,2 21 but the medical expenses can cost millions of rupees. Moreover, disability forces individuals to quit their jobs or schools and question their potential,2 17 making them financially dependent on their family and compromising their quality of life. This might lead to their family disowning them, resulting in victimisation.2 22 23
Legal aspects of the injury
The government can play an important role in curbing this problem. The Cruelty to Women and Children Act,24 the Prevention of Oppression Against Women and Children Act,25 and the Acid Offences Prevention Act 2002,26 which imposes the death penalty or life imprisonment with a fine of US$1185, are a few steps taken by the government of Bangladesh. The Domestic Violence Act of Cambodia 2005,26 27 where offenders may be charged with imprisonment for 10 years and which may be extended to over 20 years, strengthens attempts to curb acid attacks. The Indian government has also taken steps, such as restricting over-the-counter sale of acid. All sellers must maintain records of their buyers, their reasons and the quantity of purchase. India also has the Poisons Possession and Sales Rule.2 Amendments to the Indian Penal Code Sections 326A and 326B recognise acid violence as a separate offence26 and impose a minimum sentence of 10 years or imprisonment for life with a fine,22 26 while Section 357C directs all public or private hospitals to provide first aid and medical treatment free of cost to victims of acid attacks.26 The Rights of Persons with Disabilities Act revised in 2016 included ‘acid attack survivors’ as physically disabled and allowed them to receive education and employment benefits, with 3% of government jobs reserved for survivors.26 The government of India recommends other steps such as a zero-tolerance policy towards acid attacks and a generous compensation package for rehabilitation with strict implementation.2
Lack of rehabilitation services in rural and remote areas
Many of these attacks occur in rural and remote areas, and these survivors do not have access to emergency services to attend and treat such severe burns. Newberry et al28 stated that it takes a significantly long time for emergency services to transport burn patients to the nearest hospital, especially those from rural and remote areas. Moreover, the average distances travelled from tribal, rural and urban areas were 20 km, 17 km and 6 km, respectively.28 This shows the disparity in access to emergency services between patients in urban areas and those in tribal and rural areas. Only 27% of patients were transported to tertiary care hospitals, while 59% were taken to community or district hospitals.28 The authors also reported that most emergency medical technicians were unable to measure vital signs, either due to the severity of the injury, malfunctioning equipment or a lack of time. Most patients might die before reaching the nearest healthcare facility. The added expense of travelling to and residing in bigger cities for the duration of treatment results in additional difficulties.2 In India, 700 000 admissions are estimated annually; however, only 800–1000 specialised burn unit beds are available.29 Even in major cities, there are limited centres with expertise in treating burn cases and performing reconstructive procedures. It is difficult to access these services, even for those seeking rehabilitation, due to limited availability and a lack of awareness.2
Availability of optimal care for acute and long-term burn management
A multidisciplinary team is required for optimal management of acute injury, including specialised doctors and nursing staff trained in burn management, surgeons, anaesthesiologists, intensivists and dietitians.30 The healthcare facility should consist of intensive care units equipped with provisions for continuous respiration, fluid resuscitation and cardiovascular stabilisation.31 For optimal recovery, these patients need constant monitoring of haemodynamic stability, pain control, infection control, surgical debridement and wound closure, management of coagulopathy, thromboprophylaxis, and nutritional support to meet their altered metabolic demands.31
Ocular injuries account for 8%–22% of all traumatic ophthalmic injuries,32 including vitriolage. As per the National Crime Records Bureau, India reported 1483 cases of acid attack between 2014 and 2018.33 Tan et al34 reported that the face is the most common target in acid attack. The incidence of ocular chemical injuries among all ocular injuries was 14%,35 while in the UK it was 48%.36 The severity of damage depends on the type,37 concentration of the agent,37 and extent and duration of exposure.37 Acid can cause severe ocular surface damage without penetrating the deeper tissues.38 Therefore, management of acute ocular chemical injury37 requires thorough irrigation of the exposed eye with saline for 15–30 min or until the pH of the tears in the cul-de-sac neutralises. These rinsing solutions can be water, Ringer’s lactate, normal saline or phosphate buffer.39 Diphoterine, an amphoteric solution that has a non-specific binding for bases and acids, has been useful in ocular emergencies.39 This is followed by topical or systemic corticosteroids, prophylactic antibiotics, and cycloplegics with or without topical antiglaucoma therapy. Autologous serum, umbilical cord serum and amniotic membrane suspension are useful biological fluids that promote epithelialisation and accelerate wound healing.39 In cases of severe chemical injury, amniotic membrane transplantation or tenoplasty can aid in epithelial healing.39
There are 67 burn care centres in India. Among them, 30 are government-supported and the remaining 37 are private institutes. This translates to an availability of 0.1 inpatient beds per 100 000 population.40 The study also found that 75% of the population are within 2 hours of a designated burn centre with 1–10 physicians. However, not all centres are equipped to handle severe burn injuries. In addition to the inequitable geographical distribution of these centres, they have inadequate staffing and limited transportation facilities. Chamania41 describes the poor availability of these healthcare services in district hospitals. These hospitals lack junior doctors, medical staff and paramedical healthcare workers, with no facility for burn management. Even some state medical college hospitals lack the basic standard of care and protocols for burn management.
Long-term management of these cases requires physical and occupational therapists for timely evaluation, prompt management of late complications such as wound contractures and graft loss, adequate nutritional replenishment, and psychosocial support for reintegrating the survivor into the society.42 They need psychological support to help deal with their scars, disfigurement, contractures and associated physical disabilities. The goal is to rehabilitate them enough to continue their education and/or employment.43 Patients with ocular damage are prone to dryness, scarring and forniceal shortening due to conjunctival inflammation and loss of goblet cells.44–46 Associated periocular injuries such as eyelid deformity with compromised Bell’s response can compromise the ocular surface and lead to corneal desiccation after exposure keratopathy, microbial keratitis and eventual globe perforation.47–49 These patients require aggressive treatments such as intensive lubrication, use of moisture chambers, lid taping, botulinum toxin, or surgical procedures such as human amniotic membrane grafting (hAM) with permanent tarsorrhaphy.47 49 However, the feasibility of hAM (cost and availability) and tarsorrhaphy (extensive lid loss) must be considered.50 51 Moreover, definitive procedures such as upper eyelid weight placement or other lid reconstructive procedures might be delayed due to severe systemic constraints, which warrant the need for an effective alternative. Therapeutic soft contact lenses can reduce discomfort and heal epithelial defects by acting as protective barriers; however, they might get displaced, lost or dry out in the absence of lid support. There are few case reports mentioning the use of scleral lenses in managing exposure keratopathy after lid loss caused by severe periocular thermal52 and chemical53 injuries.
Our patient had total lid loss with severe exposure keratopathy leading to pericylinder melt around the keratoprosthesis in the right eye and postkeratoplasty corneal graft melt in the left eye. We tried scleral contact lenses to prevent further deterioration and corneal perforation due to poor wound healing and repeated failed lid reconstructive procedures.
Scleral lenses are large-diameter, gas-permeable, custom-made lenses with a saline-filled reservoir in the vault between the cornea and the posterior surface of the lens. The fluid reservoir constantly bathes the ocular surface and helps protect it from desiccation and other lid-related mechanical factors.51 54 Moreover, the post-lens tear reservoir also corrects irregular astigmatism and significantly improves visual acuity.51 54 Therefore, in such cases, these lenses can be used for visual rehabilitation. An adequate vault height should be achieved while fitting the scleral lens in an eye with keratoprosthesis, keeping the limbus clear and ensuring that the lens rests on the sclera. Moreover, it is important to avoid air bubbles in the reservoir because they interfere with the visual axis and reduce vision. The reservoir ensures continuous fluid ventilation, avoids further desiccation, decreases suction effects and acts as a liquid bandage, promoting wound healing.
PROSE (prosthetic replacement of ocular surface ecosystem) and BSS lenses are available internationally at BostonSight, with local distributors in India. Moreover, other options for scleral and mini-scleral lenses are available through various national and international manufacturers.
The patient lost 1.5 years of his working life due to the attack and the associated poor healing of his physical wounds. The expenses stemming from the initial life-saving procedures, multiple skin grafting and failed eyelid reconstructive procedures amounted to 1.5 million rupees ($200 000), a tremendous financial burden for the patient. His condition required exploration of other management options to prevent further worsening of exposure keratopathy until he was ready for skin grafts or lid reconstructive procedures. Therefore, we felt scleral lenses were a viable option.
It is important to consider the possible risks associated with scleral lenses. Microbial keratitis is a well-documented risk of using scleral lenses55 56 and has an incidence ranging from 18%57 to 29%.58 Bacteria are common causative pathogens of microbial keratitis.59 60 Polania-Baron et al used preservative-free moxifloxacin (0.5%) as a reservoir to treat infectious keratitis,61 and others have mentioned a combination of sterile solution and preservative-free moxifloxacin in the reservoir in managing non-healing epithelial defects to prevent secondary infections.61–63
To the best of our knowledge, the use of scleral lenses in eyes with keratoprosthesis has not been reported previously. Our case demonstrates that scleral lenses are a safe and effective option to protect the ocular surface from exposure keratopathy, even in eyes with keratoprosthesis. They increase longevity by protecting them from further desiccation. It is important to consider that these patients might have associated contractures of the forelimbs, which can make insertion and removal of lenses challenging. It is the clinicians’ or optometrists’ responsibility to teach and motivate their caretakers to clean and maintain their scleral lenses. Moreover, patients should be informed about the risk of developing microbial keratitis and should be advised to use prophylactic antibiotics. Frequent use of lubricants over the scleral lenses helps keep the anterior surface of the lens wet and maintain good optical quality. Therefore, scleral contact lenses provide a reservoir of artificial tears and aid in wound healing, reduce symptoms and improve vision in complicated eyes without eyelids.
Financial and legal support
The Indian government has launched various health organisations to aid these survivors. In addition to the Supreme Court ruling, the Prime Minister Relief Fund and the Central Victim Compensation Fund Scheme also provide financial assistance of 100 000 and 300 000 rupees ($1300 and $3919) to acid attack survivors, respectively.64 65 The Scheme for Relief and Rehabilitation of Offences (by Acids) on Women and Children by the National Commission for Women66 67 provides financial aid of 500 000 rupees ($6533) to survivors for medical assistance, another 500 000 rupees ($6533) for their rehabilitation and 200 000 rupees ($2613) to the legal heir in case of death. Similarly, many schemes have been launched by Indian state governments to support survivors financially.68 69 The ‘NALSA (Legal Services to Victims of Acid Attacks) Scheme’ strengthens the representation of these individuals at the national, state, district and taluka (subdistrict) levels in availing the various compensation schemes to patients, enables access to medical and rehabilitative services, and spreads awareness regarding entitlements to survivors.70 71
In terms of conviction rates, 90% of cases do not reach trial stage the same year,72 and those that reach court may take up to 10 years for disposal. This leads to low conviction rates,72 reported to be as low as 2.45% in 2016 and 3.36% in 2018.15 There is also a deficiency in aid reaching the survivors. The National Commission for Women stated that compensation paid to only 474 of the 1273 cases across the country.73 Similar instances where the government failed to provide help to these patients were also reported in Cambodia.74
Various non-governmental organisations (NGOs) support acid attack survivors by providing psychosocial counselling services, medical support, livelihood, and legal and educational support. These organisations provide financial help for their medical care and rehabilitation, including counselling and integration into society with vocational training, education and employment. These NGOs also conduct awareness campaigns about acid attacks and their survivors, supplementing government legislation.
Acid attacks are a global health problem that require a multidisciplinary approach to management. Preserving, maintaining and improving vision can be challenging in patients with severe ocular involvement. Scleral contact lenses can be very useful in such difficult situations.
Patient’s perspective.
TIP: I was very disheartened after the acid attack. Though I survived, it had very badly affected both my personal and professional life. I had given up the hope that I would ever see. Because of the severity of the damage to my eyes my left eye got perforated. Even after corneal transplantation for both my eyes, my cornea were melting and continued to deteriorate even after multiple failed attempts of lid closure. With Boston scleral lenses, I am comfortable, happy and now able to walk without being dependent on others and can confidently handle my daily chores.
Learning points.
Ocular damage is a common component of vitriolage as the face is frequently targeted.
Contracture of the eyelid skin can lead to severe exposure of the ocular surface and eventually a potentially blinding eye.
Scleral lenses can be used to treat eyes with severe periocular injury to protect against the sequelae of exposure keratopathy due to lid deformity or lid loss.
Scleral lenses can be safely advised to patients with keratoprosthesis to safeguard against exposure and improve vision.
Scleral lenses can be prescribed for round-the-clock use, with intermittent replacement of the reservoir fluid.
Acknowledgments
We would like to acknowledge Mr Tejah and Mr Abhinav for language editing.
Footnotes
Contributors: SChau drafted and edited the manuscript. SChat helped in data collection and managing the patient. NJ helped in editing reviews on acid attacks and different aspects of the victims. SB finalised the manuscript and assumes full responsibility for the case report.
Case reports provide a valuable learning resource for the scientific community and can indicate areas of interest for future research. They should not be used in isolation to guide treatment choices or public health policy.
Competing interests: The authors' institute is the sole distributor of BostonSight SCLERAL (BSS) and PROSE lenses in South Asia and South-East Asia.
Provenance and peer review: Not commissioned; externally peer reviewed.
Ethics statements
Patient consent for publication
Obtained.
References
- 1.ASTI. Available: https://www.asti.org.uk/a-worldwide-problem.html
- 2.Kaur N, Kumar A. Vitriolage (vitriolism) - a medico-socio-legal review. Forensic Sci Med Pathol 2020;16:481–8. 10.1007/s12024-020-00230-7 [DOI] [PubMed] [Google Scholar]
- 3.Resnick CM, Kaban LB. Padwa BL.62 - Hemifacial Microsomia: The Disorder and Its Surgical Management. In: Brennan PA, Schliephake H, Ghali GE, et al., eds. Maxillofacial surgery. 3rd Edn. Churchill Livingstone, 2017: 870–93. [Google Scholar]
- 4.Vij K. Textbook of forensic medicine and toxicology: principles and practice. 4th ed. Noida: Elsevier, 2008: p. 585. [Google Scholar]
- 5.Welsh J. “It was like burning in Hell”: A comparative exploration of acid attack violence (Doctoral dissertation, The University of North Carolina at Chapel Hill).
- 6.Nguyen K. India’s acid attack victims face long wait for justice. London: Reuters, 2015. Available: https://in.reuters.com/article/india-acid-attack-victims/indias-acid-attack-victims-face-long-wait-for-justice-idINKCN0RG1FO20150916
- 7.Kalantry S, Kestenbaum GJ. Combating acid violence in Bangladesh, India, and Cambodia (2011). Avon global center for women and justice and Dorothea S. Clarke program in feminist jurisprudence. paper 1. Available: http://scholarship.law.cornell.edu/avon_clarke/1
- 8.Dhar S. Acid attacks against women on the rise in India; survivors fight back. USA today, 2017. [Google Scholar]
- 9.Islam A. Why acid attacks are on the rise in India. Asia: DW made for minds, 2016. Available: https://www.dw.com/en/why-acid-attacks-are-on-the-rise-in-india/a-19313750
- 10.Kuriakose F, Mallick N, Iyer DK. Acid violence in South Asia: a structural analysis toward transformative justice. Antyajaa 2017;2:65–80. 10.1177/2455632717708717 [DOI] [Google Scholar]
- 11.Acid survivors Foundation, Bangladesh, annual report 2009:15, see also Bahl T and Syed MH. Encyclopaedia of the Muslim world. Delhi: Anmol publications, 2004:1163. Available: http://www.acidsurvivors.org/AR_2009.pdf [Accessed 11 Apr 2022].
- 12.Baseline Report: Violence Against Women in Bangladesh. International Women’s rights action watch Asia Pacific, Kuala Lumpur, Malaysia.
- 13.Shahidul BM, Mahmud CM. Acid burns in Bangladesh. Ann Burn Fire Dis 2001;14:115–8. [Google Scholar]
- 14.Dissanaike S, Rahimi M. Epidemiology of burn injuries: highlighting cultural and socio-demographic aspects. Int Rev Psychiatry 2009;21:505–11. 10.3109/09540260903340865 [DOI] [PubMed] [Google Scholar]
- 15.Kumar V, Kumar V. Acid attacks in India: a Socio-Legal report. Dignity 2021;6:e5. 10.23860/dignity.2021.06.01.05 [DOI] [Google Scholar]
- 16.Ahmad N. Weak laws against acid attacks on women: an Indian perspective. Med Leg J 2012;80:110–20. 10.1258/mlj.2012.012020 [DOI] [PubMed] [Google Scholar]
- 17.Goswami S, Handa RK. The peril of acid attacks in India and susceptibility of women. J Victimol Victim Just 2020;3:72–92. 10.1177/2516606920927247 [DOI] [Google Scholar]
- 18.Chandrasekhar K. What is “acid” mark on Asia? An opinion of Dr K Chandrasekhar, Eenadu, Telugu News Daily, 21 July 2009. Also see Tang Chhin Sothy, Project Against Torture. Cambodian League for the Promotion & Defense of Human Rights (LICADHO), Phnom Penh, Cambodia. Available: http://www.licadho-cambodia.org/reports/files/41acid%20report%20English.pdf [Accessed 11 Apr 2022].
- 19.Patel M. A desire to disfigure: acid attack in India. Int J Criminol Sociol Theory 2014;7:1–11. [Google Scholar]
- 20.Ministry, National Commission for women in the dark. Available: http://www.thehindu.com/news/national/ministry-national-commission-for-women-in-the-dark/article4446923.ece
- 21.Actions to counter acid attacks: overview as on November 2016. Available: http://uphome.gov.in/writereaddata/Portal/Images/Acid-Attacks-Webpage.pdf
- 22.Bajpai M, Singh S. Acid attack: a burning issue in India. J Leg Stud 2015;2. [Google Scholar]
- 23.Jayakumar S. A brief analysis of acid attacks on women in India. India: legal service India.. Available: https://www.legalserviceindia.com/legal/article-5989-a-brief-analysis-of-acid-attacks-on-women-in-india.html
- 24.Huq SP. Bodies as sites of struggle: Naripokkho and the movement for women’s rights in Bangladesh. Bangladesh Dev Stud 2003;29:47–65. [Google Scholar]
- 25.Chowdhury EH. Rethinking patriarchy, culture and masculinity: transnational narratives of gender violence and human rights advocacy. J Int Women's Stud 2015;16:98–114. [Google Scholar]
- 26.Hameed S, Bhattacharya B. Scarred for life: thoughts on legal perspectives of acid attacks in selected countries with a focus on India. J Int Women's Stud 2022;23:131–9. [Google Scholar]
- 27.Welsh J. “It was like burning in Hell”: A comparative exploration of acid attack violence (Doctoral dissertation, The University of North Carolina at Chapel Hill), 2019. [Google Scholar]
- 28.Newberry JA, Bills CB, Pirrotta EA, et al. Timely access to care for patients with critical burns in India: a prehospital prospective observational study. Emerg Med J 2019;36:176–82. 10.1136/emermed-2018-207900 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Sachan D. India launches major programme to treat burn injuries. BMJ 2014;348:g1658. 10.1136/bmj.g1658 [DOI] [PubMed] [Google Scholar]
- 30.Song M, Armstrong A, Murray A. Acid attacks: broadening the multidisciplinary team to improve outcomes. Burns 2020;46:514–9. 10.1016/j.burns.2019.03.018 [DOI] [PubMed] [Google Scholar]
- 31.Gauglitz GG, Williams FN. Overview of the management of the severely burned patient. UpToDate, 2022. Available: https://www.uptodate.com/contents/overview-of-the-management-of-the-severely-burned-patient
- 32.Nagarajan M, Mohamed S, Asmar O, et al. Data from national media reports of 'Acid attacks' in England: A new piece in the Jigsaw. Burns 2020;46:949–58. 10.1016/j.burns.2019.10.027 [DOI] [PubMed] [Google Scholar]
- 33.India saw almost 1,500 acid attacks in five years. Available: https://www.indiatoday.in/diu/story/india-saw-almost-1500-acid-attacks-in-five-years-1636109-2020-01-12
- 34.Tan A, Bharj AK, Nizamoglu M, et al. Assaults from corrosive substances and medico legal considerations in a large regional burn centre in the United Kingdom: calls for increased vigilance and enforced legislation. Scars Burn Heal 2015;1:2059513115612945. 10.1177/2059513115612945 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Singh P, Tyagi M, Kumar Y, et al. Ocular chemical injuries and their management. Oman J Ophthalmol 2013;6:83. 10.4103/0974-620X.116624 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.White ML, Chodosh J, Jang J, et al. Incidence of Stevens-Johnson syndrome and chemical burns to the eye. Cornea 2015;34:1527–33. 10.1097/ICO.0000000000000646 [DOI] [PubMed] [Google Scholar]
- 37.Wagoner MD. Chemical injuries of the eye: current concepts in pathophysiology and therapy. Surv Ophthalmol 1997;41:275–313. 10.1016/s0039-6257(96)00007-0 [DOI] [PubMed] [Google Scholar]
- 38.Schrage NF, Langefeld S, Zschocke J, et al. Eye burns: an emergency and continuing problem. Burns 2000;26:689–99. 10.1016/S0305-4179(00)00044-9 [DOI] [PubMed] [Google Scholar]
- 39.Sharma N, Kaur M, Agarwal T, et al. Treatment of acute ocular chemical burns. Surv Ophthalmol 2018;63:214-235. 10.1016/j.survophthal.2017.09.005 [DOI] [PubMed] [Google Scholar]
- 40.Chamania S. Training and burn care in rural India. Indian J Plast Surg 2010;43:S216–130. 10.4103/0970-0358.70735 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Potokar T, Bendell R, Chamania S, et al. A comprehensive, integrated approach to quality improvement and capacity building in burn care and prevention in low and middle-income countries: an overview. Burns 2020;46:1756–67. 10.1016/j.burns.2020.05.029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Ranganathan K, Mouch CA, Chung M, et al. Geospatial mapping as a guide for resource allocation among burn centers in India. J Burn Care Res 2020;41:853–8. 10.1093/jbcr/irz210 [DOI] [PubMed] [Google Scholar]
- 43.Overview of the management of the severely burned patient. Available: https://www.uptodate.com/contents/overview-of-the-management-of-the-severely-burned-patient
- 44.Schneider JC, Bassi S, Ryan CM. Employment outcomes after burn injury: a comparison of those burned at work and those burned outside of work. J Burn Care Res 2011;32:294–301. 10.1097/BCR.0b013e31820aaf56 [DOI] [PubMed] [Google Scholar]
- 45.Schrage NF, Langefeld S, Zschocke J, et al. Eye burns: an emergency and continuing problem. Burns 2000;26:689–99. 10.1016/s0305-4179(00)00044-9 [DOI] [PubMed] [Google Scholar]
- 46.Fish R, Davidson RS. Management of ocular thermal and chemical injuries, including amniotic membrane therapy. Curr Opin Ophthalmol 2010;21:317–21. 10.1097/ICU.0b013e32833a8da2 [DOI] [PubMed] [Google Scholar]
- 47.Spector J, Fernandez WG, Chemical FWG. Chemical, thermal, and biological ocular exposures. Emerg Med Clin North Am 2008;26:125–36. 10.1016/j.emc.2007.11.002 [DOI] [PubMed] [Google Scholar]
- 48.Bizrah M, Yusuf A, Ahmad S. An update on chemical eye burns. Eye 2019;33:1362–77. 10.1038/s41433-019-0456-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Krachmer JH, Mannis MJ, Holland EJ. Perioheral corneal disease.Cornea. 3rd edn. Elsevier Health Sciences, 2010: p. 267. [Google Scholar]
- 50.Holland EJ, Mannis MJ, Lee WB. Ocular surface disease: cornea, conjunctiva and tear film: expert consult-online and print. Elsevier Health Sciences, 2013. [Google Scholar]
- 51.McIndoe AH. Total reconstruction of the burned face. The Bradshaw lecture 1958. Br J Plast Surg 1983;36:410–20. 10.1016/0007-1226(83)90119-4 [DOI] [PubMed] [Google Scholar]
- 52.Williams ZR, Aquavella JV. Management of exposure keratopathy associated with severe craniofacial trauma. J Cataract Refract Surg 2007;33:1647–50. 10.1016/j.jcrs.2007.04.035 [DOI] [PubMed] [Google Scholar]
- 53.Kalwerisky K, Davies B, Mihora L, et al. Use of the Boston ocular surface prosthesis in the management of severe periorbital thermal injuries: a case series of 10 patients. Ophthalmology 2012;119:516–21. 10.1016/j.ophtha.2011.08.027 [DOI] [PubMed] [Google Scholar]
- 54.Scanzera AC, Ahmad A, Shorter E. Adjunct use of therapeutic scleral lens for exposure keratopathy after severe chemical burn. Case Rep Ophthalmol 2021;12:243–7. 10.1159/000511223 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Barnett M, Johns LK, eds. Contemporary scleral lenses: theory and application. Bentham Science Publishers, 2017. [Google Scholar]
- 56.Zimmerman AB, Marks A. Microbial keratitis secondary to unintended poor compliance with scleral gas-permeable contact lenses. Eye Contact Lens 2014;40:e1–4. 10.1097/ICL.0b013e318273420f [DOI] [PubMed] [Google Scholar]
- 57.Fernandes M, Sharma S. Polymicrobial and microsporidial keratitis in a patient using Boston scleral contact lens for Sjogren's syndrome and ocular Cicatricial pemphigoid. Cont Lens Anterior Eye 2013;36:95–7. 10.1016/j.clae.2012.10.082 [DOI] [PubMed] [Google Scholar]
- 58.Rosenthal P, Croteau A. Fluid-ventilated, gas-permeable scleral contact lens is an effective option for managing severe ocular surface disease and many corneal disorders that would otherwise require penetrating keratoplasty. Eye Contact Lens 2005;31:130–4. 10.1097/01.icl.0000152492.98553.8d [DOI] [PubMed] [Google Scholar]
- 59.Rosenthal P, Cotter JM, Baum J. Treatment of persistent corneal epithelial defect with extended wear of a fluid-ventilated gas-permeable scleral contact lens. Am J Ophthalmol 2000;130:33–41. 10.1016/s0002-9394(00)00379-2 [DOI] [PubMed] [Google Scholar]
- 60.Lakhundi S, Siddiqui R, Khan NA. Pathogenesis of microbial keratitis. Microb Pathog 2017;104:97–107. 10.1016/j.micpath.2016.12.013 [DOI] [PubMed] [Google Scholar]
- 61.Polania-Baron EJ, Santana-Cruz O, Lichtinger A, et al. Treatment of severe infectious keratitis with scleral contact lenses as a reservoir of moxifloxacin 0.5. Cornea 2021;40:831–6. 10.1097/ICO.0000000000002482 [DOI] [PubMed] [Google Scholar]
- 62.Ciralsky JB, Chapman KO, Rosenblatt MI, et al. Treatment of refractory persistent corneal epithelial defects: a standardized approach using continuous wear PROSE therapy. Ocul Immunol Inflamm 2015;23:219–24. 10.3109/09273948.2014.894084 [DOI] [PubMed] [Google Scholar]
- 63.Ling JD, Gire A, Pflugfelder SC. PROSE therapy used to minimize corneal trauma in patients with corneal epithelial defects. Am J Ophthalmol 2013;155:615–9. 10.1016/j.ajo.2012.09.033 [DOI] [PubMed] [Google Scholar]
- 64.PMNRF . Grant to acid attack victims. India: government of India, 2016. Available: https://pmnrf.gov.in/en/about/grant-to-acid-attack-victims
- 65.Kumar D. Central victim compensation fund scheme guidelines. India: Government of India, 2016. [Google Scholar]
- 66.Annual report 2008-09. Available: http://ncwapps.nic.in/AnnualReports/200809/Eng/Annexure4.pdf
- 67.Scheme for relief and rehabilitation of offences (by acids) on women and children national Commission for women. Available: https://nlrd.org/scheme-for-relief-and-rehabilitation-of-offences-by-acids-on-women-and-children-national-commission-for-women
- 68.Department of social security and woman & child development . Financial assistance to acid victims. Punjab: government of Punjab, 2017. Available: https://sswcd.punjab.gov.in/en/financial-assistance-to-acid-victims
- 69.H. department of social justice and empowerment. financial assistance to women and girls acid attack victims. Haryana: government of Haryana, 2019. Available: https://socialjusticehry.gov.in/financial-assistance-to-women-and-girls-acid-attack-victims
- 70.National legal service authorities. NALSA (Legal service to victims of acid attacks) scheme. India:National legal service authorities, 2016. Available: https://himachal.nic.in/WriteReadData/l892s/240_l892s/1500444109.pdf
- 71.NALSA (legal services to victims of acid attacks) scheme, 2016. Available: https://nalsa.gov.in/acts-rules/preventive-strategic-legal-services-schemes/nalsa-legal-services-to-victims-of-acid-attacks-scheme-2016
- 72.Gupta P. India is failing acid attack survivors, here is the data. shethepeople, 2020. Available: https://www.shethepeople.tv/top-stories/issues/india-acid-attacks-survivors-data
- 73.Compensation not paid to acid attack victims in 799 out of 1,273 cases: NCW. Available: https://economictimes.indiatimes.com/news/politics-and-nation/compensation-not-paid-to-acid-attack-victims-in-799-out-of-1273-cases-ncw/articleshow/79350842.cms?from=mdr
- 74.Acid attacks: Cambodia victims 'denied government aid'. Available: https://www.bbc.com/news/world-asia-47133728



