To the Editor: The polarizing nature of vaccination against coronavirus disease 2019 (Covid-19) within the United States threatens public health and has contributed to variable statewide vaccine uptake that ranged from 50 to 80% as of January 2022.1 Given the divided national landscape and anecdotal evidence from our own patients, we hypothesized that low Covid-19 vaccination rates would be associated with decreases in influenza vaccination rates.
Using nationally representative data from the Centers for Disease Control and Prevention,2 we calculated changes in influenza vaccine uptake at the state-population level during the pandemic after Covid-19 vaccines became widely available (September 2021 through January 2022) relative to before the pandemic (September 2019 through January 2020). To account for pandemic-related factors unrelated to Covid-19 vaccines that might affect changes in influenza vaccine uptake (e.g., worsening inequities in access to care3,4 or employment), we also compared September 2020 through January 2021 (the first influenza season during the pandemic but before widespread Covid-19 vaccine availability) to before the pandemic. We stratified changes in influenza vaccine uptake according to quartile of state-level cumulative Covid-19 vaccine uptake through January 2022. We used mixed-effects linear regressions (difference-in-differences analyses) to examine whether changes in influenza vaccine uptake during influenza seasons before as compared with during the pandemic differed between states with high as compared with low Covid-19 vaccine uptake. Details and sensitivity analyses are provided in the Supplementary Appendix, available with the full text of this letter at NEJM.org.
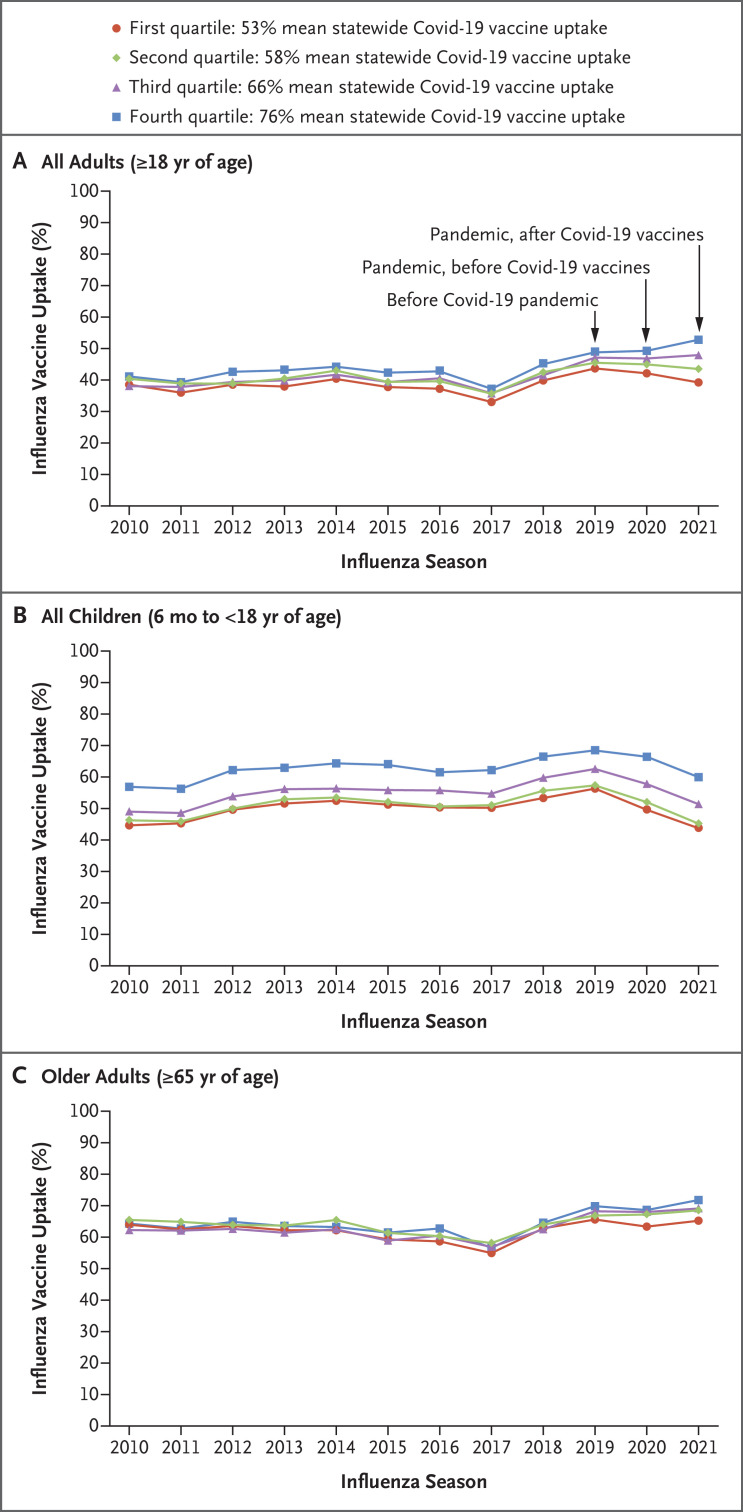
Influenza vaccine uptake remained relatively stable during the first influenza season of the pandemic (Figure 1). In contrast, after Covid-19 vaccines became widely available (2021–2022 season), adult influenza vaccine uptake decreased within states in the bottom two quartiles of Covid-19 vaccine uptake (quartile 1, from 43.7% [95% confidence interval {CI}, 41.8 to 45.6] to 39.2% [95% CI, 37.0 to 41.5]; quartile 2, from 45.5% [95% CI, 42.8 to 48.2] to 43.5% [95% CI, 40.4 to 46.7]) and increased within states in the top two quartiles (quartile 3, from 46.9% [95% CI, 45.1 to 48.8] to 47.7% [95% CI, 45.1 to 50.4]; quartile 4, from 49.0% [95% CI, 46.7 to 51.4] to 52.8% [95% CI, 50.2 to 55.3]) (Table S1 in the Supplementary Appendix). Differences between each quartile in the 2021–2022 season as compared with the 2019–2020 season are shown in Table S2. The sensitivity analysis comparing the 2020–2021 season with the 2019–2020 season showed that influenza vaccine uptake was stable before widespread Covid-19 vaccine availability, which suggests that other pandemic-related effects such as changes in access to care were unlikely to have affected influenza vaccine uptake. During the 2020–2021 and 2021–2022 influenza seasons, influenza vaccine uptake decreased uniformly among children but remained stable among older adults, regardless of Covid-19 vaccine uptake.
Figure 1. Trends in Influenza Vaccine Uptake Aggregated According to Quartile of Statewide Covid-19 Vaccine Uptake among All Adults, All Children, and Older Adults.
Each influenza season spans September of the indicated year through January of the following year (e.g., the 2021 influenza season was September 2021 through January 2022). An explanation of the decrease in influenza vaccine uptake during the 2017–2018 season, in addition to further interpretation of results, is available in the Discussion section in the Supplementary Appendix. Covid-19 denotes coronavirus disease 2019.
Although inferences about specific policies and messaging promoting Covid-19 vaccination are beyond the scope of this ecologic study, our findings suggest that after the widespread availability of Covid-19 vaccines, factors associated with Covid-19 vaccination rates (e.g., safety concerns and mistrust of Covid-19 vaccines or government5) may have spilled over to affect influenza vaccination rates.
Supplementary Appendix
Disclosure Forms
This letter was published on June 15, 2022, at NEJM.org.
Footnotes
Supported by grants from the National Institutes of Health (NIH), National Heart, Lung, and Blood Institute, Stimulating Access to Research in Residency program at UCLA (5R38HL143614-03, to Dr. Leuchter); the NIH, National Center for Advancing Translational Sciences UCLA Clinical and Translational Science Institute (UL1TR001881, to Dr. Sarkisian); the NIH, National Institute on Aging (1K76AG064392-01A1, to Dr. Mafi); and the NIH, National Institute on Aging Midcareer Award in Patient-Oriented Aging Research (2K24AG047899-06, to Dr. Sarkisian). Dr. Sarkisian was also supported with resources and the use of facilities at the Veterans Affairs Greater Los Angeles Healthcare Center.
Disclosure forms provided by the authors are available with the full text of this letter at NEJM.org.
References
- 1.Centers for Disease Control and Prevention. COVID-19 vaccinations in the United States, county. 2022. (https://data.cdc.gov/Vaccinations/COVID-19-Vaccinations-in-the-United-States-County/8xkx-amqh).
- 2.Centers for Disease Control and Prevention. FluVaxView: influenza (flu). 2021. (https://www.cdc.gov/flu/fluvaxview/index.htm).
- 3.Leuchter RK, Villaflores CWA, Norris KC, Sorensen A, Vangala S, Sarkisian CA. Racial disparities in potentially avoidable hospitalizations during the COVID-19 pandemic. Am J Prev Med 2021;61:235-239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mafi JN, Craff M, Vangala S, et al. Trends in US ambulatory care patterns during the COVID-19 pandemic, 2019–2021. JAMA 2022;327:237-247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Khairat S, Zou B, Adler-Milstein J. Factors and reasons associated with low COVID-19 vaccine uptake among highly hesitant communities in the US. Am J Infect Control 2022;50:262-267. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.