Abstract
BACKGROUND:
The impact of a stoma on long-term health-related quality of life in people living with ileostomies is not clear.
OBJECTIVE:
This study aimed to describe important patient-reported outcomes and health-related quality of life in people with ileostomies.
DESIGN:
This is a population-based, cross-sectional study. Patients were invited to answer questionnaires estimating stoma-specific and generic health-related quality of life (EQ-5D-5L and the Major Depression Inventory). Danish norms were retrieved from reference literature.
SETTINGS:
This study was conducted at the major stoma clinic at Aarhus University Hospital, Denmark.
PATIENTS:
We invited all patients with ileostomies who were in contact with the clinic between 2012 and 2017.
MAIN OUTCOME MEASURES:
The primary outcomes measured were patient-reported outcomes specific to people with ileostomies.
RESULTS:
Of 621 identified patients (50% women), 412 (67%) responded to the survey. Among the responders, 178 (43%) reported that they still had an ileostomy at the time of the survey and were included in the analysis. Fatigue was frequent; 68% (95% CI 60%–75%) reported being tired and 26% (95% CI 20%–33%) answered that they were “always tired,” whereas 43% (95% CI 36%–51%) lacked energy, 62% (95% CI 54%–69%) reported poor sleep, and 59% (95% CI 52%–66%) needed to rest during the day. Fifty-six percent (95% CI 48%–63%) needed to know the immediate location of the nearest toilet, and 58% (95% CI 51%–66%) felt sexually unattractive because of their ileostomy. Health-related quality of life measured with generic questions indicated 0.124 points lower health-related quality of life than the Danish norm (p < 0.001), and 18% (95% CI 13%–25%) scored above the threshold for depression, which is 2.6 times higher than the background population (7%, 95% CI 6%–9%; p < 0.001).
LIMITATIONS:
This study was limited by potential selection bias, and all participants did not answer all items.
CONCLUSIONS:
Fatigue and low health-related quality of life is common in people living with ileostomies. Addressing fatigue and stoma-specific challenges in patients with an ileostomy is warranted. See Video Abstract at http://links.lww.com/DCR/B803.
DESENLACES INFORMADOS POR PACIENTES Y CALIDAD DE VIDA RELACIONADA CON LA SALUD EN PERSONAS QUE VIVEN CON ILEOSTOMÍAS: UN ESTUDIO TRANSVERSAL POBLACIONAL
ANTECEDENTES:
El impacto de un estoma en la calidad de vida relacionada con la salud a largo plazo en personas que viven con ileostomías no está claro.
OBJETIVO:
Describir desenlaces importantes informados por pacientes y la calidad de vida relacionada con la salud en personas con ileostomías.
DISEÑO:
Estudio transversal poblacional. Se invitó a los pacientes a responder cuestionarios que estiman la calidad de vida relacionada con la salud general y específica del estoma (EQ-5D-5L y el Inventario de depresión mayor). Las normas danesas se recopilaron de la literatura de referencia.
AJUSTES:
El estudio se llevó a cabo en la clínica principal de estomas del Hospital Universitario de Aarhus, Dinamarca.
PACIENTES:
Invitamos a todos los pacientes con ileostomías que estuvieron en contacto con la clínica entre 2012 y 2017.
PRINCIPALES MEDIDAS DE RESULTADO:
Resultados informados por el paciente específicos para personas con ileostomías.
RESULTADOS:
De 621 pacientes identificados (50% mujeres), 412 (66%) respondieron la encuesta. Entre los que respondieron, 178 (43%) informaron que todavía tenían una ileostomía en el momento de la encuesta y fueron incluidos en el análisis. La fatiga era frecuente; el 68% (intervalo de confianza del 95%: 60–75%) informó estar cansado y el 26% (20–33%) respondió “siempre cansado”, mientras que el 43% (36–51%) carecía de energía, el 62% (54–69%)) refirieron dormir mal y el 59% (52–6%) necesitaba descansar durante el día. El cincuenta y seis por ciento (48–63%) necesitaba saber la ubicación inmediata del baño más cercano y el 58% (51–66%) se sentía sexualmente poco atractivo debido a su ileostomía. La calidad de vida relacionada con la salud medida con preguntas genéricas indicó una calidad de vida relacionada con la salud 0,124 puntos más baja que la norma danesa (p < 0,001), y el 18% (13–25%) puntuó con depresión, que es 2.6 veces más alta que la población de base (7%, 6–9%, p < 0,001).
LIMITACIONES:
Posible sesgo de selección, y no todos los participantes respondieron a todos los ítems.
CONCLUSIONES:
La fatiga y la baja calidad de vida relacionada con la salud es común en las personas que viven con ileostomías. Se justifica abordar la fatiga y los desafíos específicos del estoma en pacientes con una ileostomía. Consulte Video Resumen en http://links.lww.com/DCR/B803. (Traducción—Juan Carlos Reyes)
Keywords: Fatigue, Ileostomy, Inflammatory bowel disease, Patient-reported outcome measures, Quality of life
The long-term health-related quality of life (HRQoL) of people living with ileostomies is rarely a health care focus area. Having a stoma affects the patient’s daily life, and adaptation to a stoma is both physical and psychosocial. Although patients needing an ileostomy are closely monitored in the postoperative period, follow-up visits become fewer or are omitted entirely once patients are biochemically stable. Little is known about the long-term consequences of living with an ileostomy on HRQoL and about factors that may affect HRQoL.
Previous studies have found that most people living with ileostomies seem to cope well but can experience low HRQoL.1–5 The specific causes influencing low HRQoL have been explored only briefly. Nutrition deficiencies and stoma-related morbidity may be part of the reason,1 but the literature lacks systematic investigations of which factors patients perceive as troublesome. Patient-reported outcomes (PROs) are measurements that stem directly from the patients without any interpretations, and they can be used to assess nonobservable outcomes.6 These measurements hold key information that can contribute to identifying the difficulties experienced by patients and can guide clinical management.
In this study, we aimed to describe important PROs affecting HRQoL in people living with ileostomies.
MATERIALS AND METHODS
In this population-based, cross-sectional study, we invited patients with temporary or permanent ileostomies to answer questionnaires covering generic and stoma-specific HRQoL. The patients were identified from an internal electronic register. We included all patients who had been in contact with the Outpatient Stoma Clinic at Aarhus University Hospital, Denmark, between 2012 and 2017 and who had been coded for an ileostomy (DZ932) in the Danish version of the International Classification of Diseases, 10th Revision, diagnostic database. This approach allowed us to identify all people living with an ileostomy from the Central Denmark Region because the clinic is responsible for prescription of stoma-related equipment.
The identified people received an invitation and a link to the survey in their electronic letterbox (e-Boks). e-Boks is a secure online mailbox, linked to all Danes’ unique civil registration number, and it is used by national authorities or hospitals. If patients consented to participation, they could fill out the questionnaires electronically. The questionnaires were sent with regular postal mail to patients without e-mail access. The invitations were sent in June 2017 and a reminder was sent to nonresponders 3 weeks after the first invitation.
Questionnaires
The first item in the questionnaire confirmed whether the responder currently had an ileostomy; if not, their participation ended. The remainder of the questionnaire for patients with a current ileostomy included 3 validated questionnaires and questions about demographics, HRQoL in relation to their stoma, bag-emptying, and smoking and drinking habits.
Stoma-QoL is a stoma-specific instrument with 20 questions rated on a 4-point Likert scale (“always,” “sometimes,” “rarely,” and “not at all”) describing current well-being. The results are transformed into a scale from 0 to 100 points, with higher scores indicating higher HRQoL.7
The EQ-5D-5L is a generic HRQoL questionnaire with 5 questions regarding perceived current problems regarding mobility, self-care, usual activities, pain/discomfort, and anxiety/depression. Each domain is answered on a 5-point Likert scale: “no problems,” “slight problems,” “moderate problems,” “severe problems,” and “extreme problems.” The answers are combined into a 5-digit number, which is translated into an index score describing health status, where higher scores indicate higher HRQoL.8 We compared our results with the Danish population norm9 using the Crosswalk10 value set provided by the developers (https://euroqol.org). The EQ-5D-5L also includes a self-perceived health visual analog scale (VAS), scoring from 1 to 100, where 100 expresses the best possible health.
The Major Depression Inventory (MDI) is a diagnostic instrument and a scale for measuring depression severity. It contains 10 items regarding depressive symptoms, compatible with the Diagnostic and Statistical Manual of Mental Disorders, 4th Edition, and International Classification of Diseases, 10th Revision, symptoms. Each item is scored on a 6-point Likert scale covering how much time the symptom has been present during the past 14 days (from not at all to all of the time), and higher scores indicate increasing depression severity.11 We compared our results with scores of a representative sample of the general Danish background population.12
Outcomes
The primary outcome was an exploration of PROs in people living with an ileostomy. Secondary outcomes were assessment of overall HRQoL and possible associations with PROs and descriptive parameters.
Data Handling and Statistics
Study data were collected and managed by using Research Electronic Data Capture (REDCap),13,14 an electronic data capture tool hosted at Aarhus University. The study was performed according to the Declaration of Helsinki, and the protocol was approved and registered by the Danish Data Protection Agency and the Central Denmark Regional Committee on Health Research Ethics (j.no. 1-10-72-290-16) before study initiation.
Descriptive and comparative statistics were performed using STATA 16 software (StataCorp, College Station, TX), and figures were made in GraphPad Prism 8.0.0 (GraphPad Software, San Diego, CA). Missing data were omitted, and questionnaire scores were reported only if all questions were answered. We performed sensitivity analyses with simple imputation of data to determine the robustness of this method for handling missing data. For participant with missing values, we applied the best possible choice (ie, toward high HRQoL or low depression score) and a derived mean score. No scores were imputed if the participant had more than 3 missing values per questionnaire.
Indications for ileostomy formation were stratified into IBDs (ulcerative colitis [UC] or Crohn’s disease [CD]), cancer, or miscellaneous indications. Results are presented as means (± SD) or percentage (95% CI) if data followed a normal distribution, otherwise they were reported as median, interquartile range (IQR), and range. When reporting proportions or comparing groups, 95% CIs are presented. Chi-squared/Fisher exact tests, Student t tests/Wilcoxon signed-rank tests, logistic regression, or Kruskal-Wallis tests were used according to distribution and data variables.
RESULTS
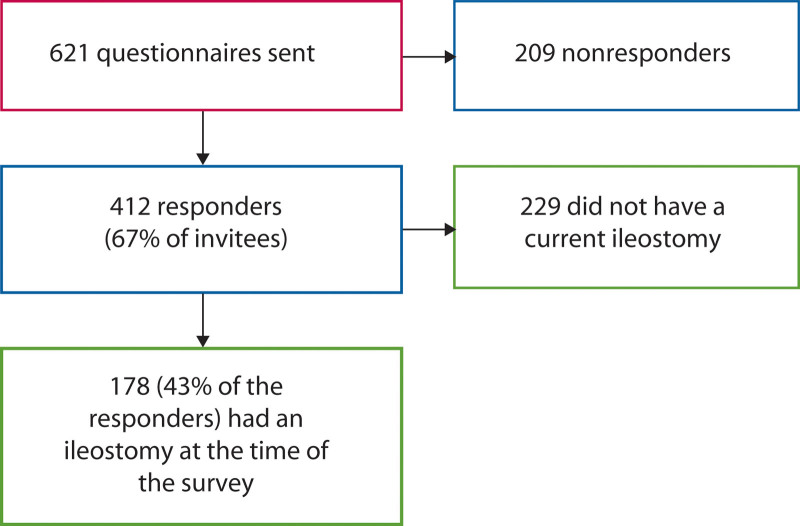
An invitation to participate was sent to 621 patients, of whom 89% had e-Boks; the remaining 11% received a paper questionnaire. Of the 621 invitees, 412 (67%) responded, and 178 (43% of the responders, 29% of all invitees) confirmed that they still had an ileostomy and completed all questionnaires (Fig. 1). The response rate for the electronic survey was 68% (95% CI 64%–72%) and for the paper survey 49% (95% CI 39%–63%). A higher proportion of the invited women (53%, 95% CI 48%–58%) than men responded (p = 0.03), and responders were a median 11 years older than nonresponders (p < 0.001). The characteristics of responders with ileostomies are presented in Table 1.
FIGURE 1.
Flow chart.
TABLE 1.
Participant characteristics
| Characteristics | n | Subgroups | Stoma-QoL, mean (+SD) |
|---|---|---|---|
| Women, percentage (95% CI) | 178 | 57% (49%–64%) | 58.7 (±13) |
| Age, y, mean (±SD) | 178 | 58 (±16) | |
| Indication for ileostomy, percentage (95% CI) | 162 | ||
| IBD | 77% (69%–83%) | 59.3 (±13) | |
| Ulcerative colitis | 89 | 59.2 (±13) | |
| Crohn’s disease | 35 | 59.9 (±12) | |
| Cancer | 12% (8%–18%) | 59.2 (±11) | |
| Colorectal cancer | 19 | ||
| Cancer, other | 2 | ||
| Miscellaneous | 11% (7%–17%) | 55.6 (±11) | |
| Chronic constipation | 6 | ||
| Complications to other surgery | 5 | ||
| Ischemic bowel disease | 3 | ||
| Familial adenomatous polyposis | 2 | ||
| Other (diverticulitis, incarceration;) | 2 | ||
| BMI, kg/m2, median (IQR, range) | 173 | 24.8 (22–28, 17–46) | |
| Women | 100 | 24.5 (22–29, 17–46) | 58.7 (±13) |
| Men | 73 | 24.9 (22–28, 18–40) | 58.9 (±11) |
| Years with ileostomy, y, median (IQR, range) | 172 | 5 (2–17, 0–57) | |
| Education, percentage (95% CI) | 161 | ||
| Primary and lower secondary education (age 6–16 y) | 14% (9%–20%) | 57.9 (±10) | |
| Upper secondary education (typically age 16–19 y) | 22% (17%–30%) | 59.1 (±11) | |
| Higher education, short (typically 1–2 y) | 12% (8%–18%) | 58.4 (±15) | |
| Higher education, middle (typically 2-4 y) | 37% (30%–44%) | 57.6 (±13) | |
| Higher education, long (typically 4–6 y) | 16% (11%–22%) | 60.9 (±12) | |
| Job, percentage (95% CI) | 171 | ||
| Student | 2% (1%–6%) | 60.5 (±19) | |
| Full-time work | 23% (17%–30%) | 62.4 (±13) | |
| Part-time work | 5% (3%–10%) | 58.2 (±9) | |
| Unemployed | 4% (2%–8%) | 53.4 (±12) | |
| Sick leave | 5% (2%–9%) | 49.6 (±9) | |
| Incapacity benefit | 17% (12%–23%) | 53.7 (±13) | |
| Retirement/early retirement | 37% (31%–45%) | 61.8 (±9) | |
| Other (flex job, stay-at-home-parent, freelancer, etc) | 7% (4%–12%) | 52.3 (±15) | |
| Annual household incomea, % (95% CI) | 148 | ||
| <18,657 euro | 32% (25%–40%) | 55.6 (±13) | |
| 18,657–37,313 euro | 37% (30%–45%) | 61.3 (±12) | |
| 37,313–55,970 euro | 20% (15%–28%) | 57.1 (±11) | |
| >55,970 euro | 11% (7%–17%) | 64.6 (±12) | |
| Marital status, % (95% CI) | 170 | ||
| Single | 19% (14%–26%) | 57.1 (±14) | |
| Widow/widower | 7% (4%–11%) | 63.8 (±9) | |
| Married | 54% (46%–61%) | 58.8 (±12) | |
| Cohabiting | 14% (10%–20%) | 56.4 (±11) | |
| Partner, not living together | 7% (4%–11%) | 56.8 (±10) | |
| Alcohol consumptionb, (95% CI) | 167 | ||
| <1 unit/wk | 47% (40%–54%) | 55.4 (±14) | |
| 1–3 units/wk | 22% (17%–29%) | 61.5 (±8) | |
| 4–6 units/wk | 13% (8%–19%) | 65.7 (±13) | |
| 7–9 units/wk | 8% (5%–14%) | 60.2 (±12) | |
| 10–12 units/wk | 4% (2%–9%) | 59.0 (±10) | |
| 13–15 units/wk | 3% (1%–7%) | 63.3 (±3) | |
| >15 units/wk | 3% (1%–7%) | 54.3 (±3) | |
| Smoking status, percentage (95% CI) | 169 | ||
| Nonsmoker | 88% (82%–92%) | 59.4 (±12) | |
| Smoking every day | 10% (6%–15%) | 51.8 (±13) | |
| Occasional smoking | 3% (1%–7%) | 67.2 (±7) |
IBD = Inflammatory bowel disease, IQR = interquartile range.
100 euro ≈ 756 Danish kroner.
1 unit = 12 g alcohol.
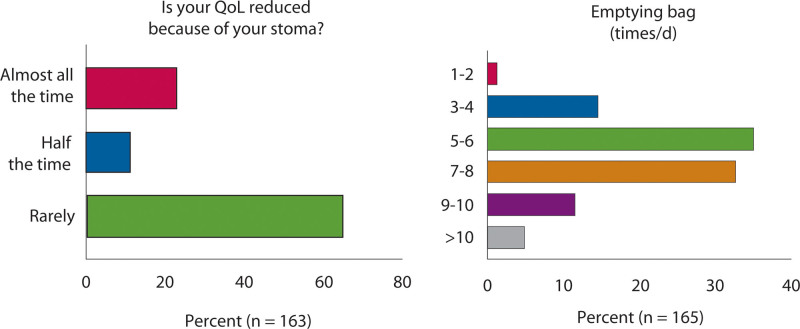
When asked directly if their stoma reduced their quality of life, 65% (95% CI 57%–72%) answered rarely, and 23% (95% CI 17%–30%) answered that it reduced their HRQoL almost all the time (Fig. 2A). This correlates well with their overall HRQoL score from both the stoma-specific (p < 0.001) and the generic questionnaire (p < 0.001), and there is a negative association between the number of times they have to empty their stoma bag and HRQoL (p < 0.001). Most (68%, 95% CI 60%–75%) respondents emptied their bag 5 to 8 times/day, and 5% (95% CI 2%–9%) emptied their bag more than 10 times/day (Fig. 2B). Thirty-one percent (24%–38%) of the responders always needed to know the location of the nearest toilet, 22% (95% CI 16%–29%) always worried that their bag would loosen, and 29% (95% CI 22%–36%) always felt less sexually attractive because of their ileostomy. Moreover, 23% (95% CI 17%–30%) always had poor sleep, 26% (95% CI 20%–33%) were always tired, and 28% (95% CI 22%–36%) needed to rest during the day (Fig. 3). When combining patients answering always or sometimes, 68% (60%–75%) were tired, 62% (95% CI 54%–69%) reported poor sleep, and 59% (95% CI 52%–66%) needed to rest during the day. Forty percent (95% CI 25%–59%) of the patients with CD and 39% (95% CI 19%–64%) of patients with miscellaneous indications answered that they always felt tired. Nineteen percent (95% CI 12%–29%) of patients with UC and 15% (95% CI 5%–40%) of patients with cancer felt tired all the time. Although patients with CD had numerically higher proportions of fatigue, differences in fatigue based on the indication for ileostomy formation did not reach statistical significance (p = 0.25). The participants had a mean Stoma-QoL score of 58.8 (± 12 SD), and there were no differences between men and women regarding the overall score or the individual PROs.
FIGURE 2.
Single patient-reported outcomes. Single questions investigating potentially relevant patient-reported outcomes. QoL = quality of life.
FIGURE 3.
Stoma-specific quality of life (Stoma-QoL). Proportions of individual answers to the Stoma-QoL questionnaire.
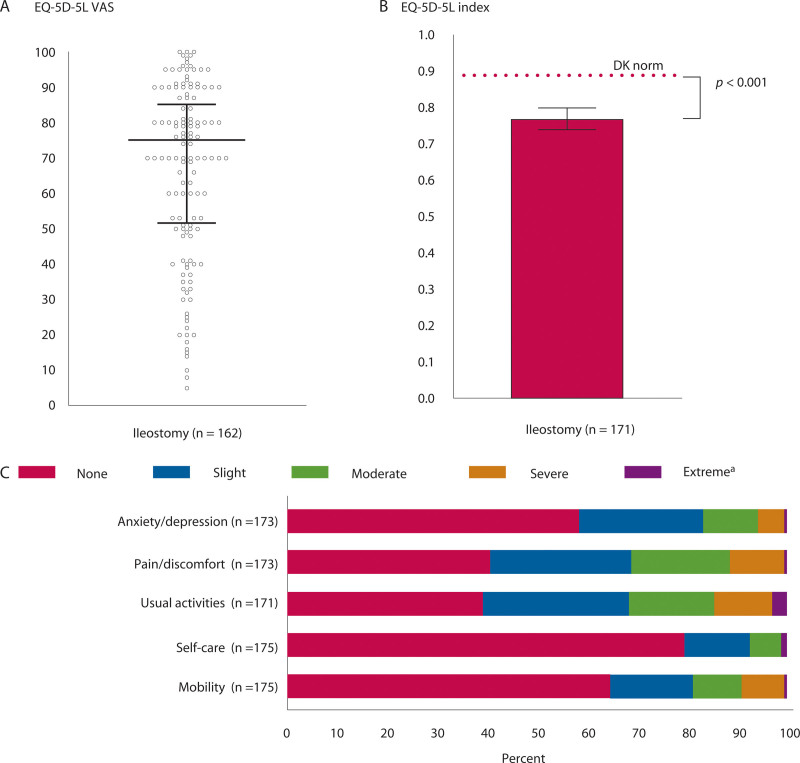
The participants rated their current health to be a median of 75 (IQR 52–85, range 5–100) on the EQ-5D-5L VAS (Fig. 4A). The EQ-5D-5L HRQoL index score was a median of 0.79 (IQR 0.66–0.87, range 0.053–1) and 0.124 points lower than the overall Danish norm (p < 0.001; Fig. 4B). The mean index scores were also lower than the Danish norms after stratifying for sex and age, but the difference was smaller for women aged ≥70 and men aged ≥60 years. The individual PROs indicated that 32% (95% CI 25%–39%) experienced more than slight difficulties performing their usual activities, 31% (95% CI 25%–39%) reported more than slight pain/discomfort, and 17% (95% CI 12%–23%) experienced more than slight anxiety/depression. Furthermore, 19% (95% CI 14%–25%) and 7% (95% CI 4%–12%) reported more than slight problems with mobility and self-care, respectively (Fig. 4C). There were no statistically significant differences in the generic (p = 0.21) or the stoma-specific (p = 0.75) HRQoL scores between different ileostomy indications.
FIGURE 4.
Generic health-related quality of life (EQ-5D-5L). A, The participants’ self-perceived health on a VAS (median and IQR). B, EQ-5D-5L scores from people living with ileostomies compared with a Danish normative score9 (mean, 95% CI). C, Proportions of individual answers to the EQ-5D-5L questionnaire. aFor mobility/self-care/usual activities, “extreme” expresses that the participant is unable to walk/wash or dress themselves/do usual activities. DK = Danish; HRQoL = health-related quality of life; IQR = interquartile range; VAS = visual analog scale.
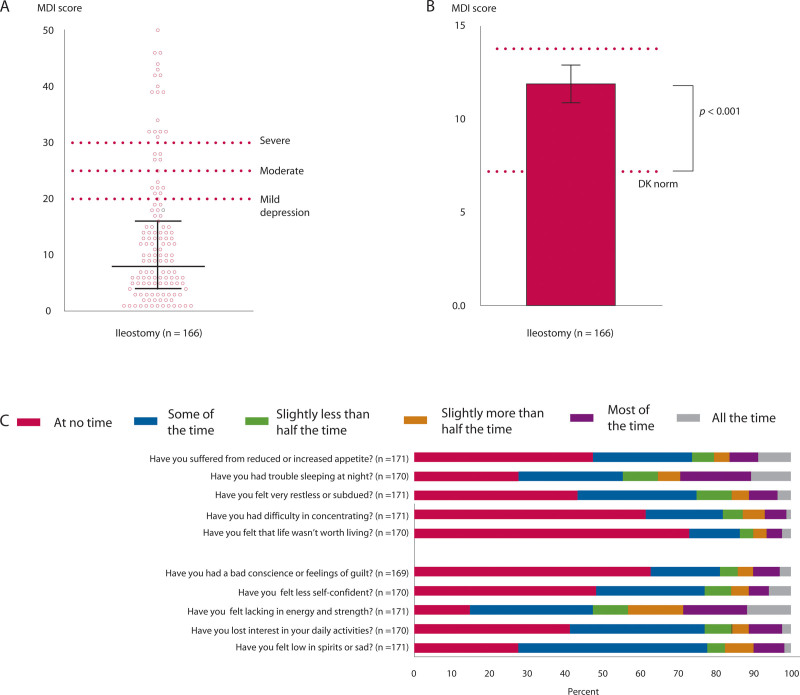
The MDI screening tool indicated that 18% (95% CI 13%–25%) of people living with ileostomies were depressed, which is 2.6 times higher than the general Danish population (7%, 95% CI 6%–9%). The median MDI was 8 (IQR 4–16, range 0–50) points (Fig. 5A). The mean MDI score was 12 points, which is 4.8 points higher than the background population (p < 0.001; Fig. 5B). In the present study, participants with a score indicating mild, moderate, or severe depression were a median 5 years younger than responders with no indication of depression (p = 0.35), their median BMI was 2.4 kg/m2 higher (p = 0.02), and 77% (95% CI 58%–89%) were women compared with 53% (95% CI 45%–61%) in those without depression (p = 0.13). Their mean Stoma-QoL score was 16.9 (± 2 SD) points lower than the scores of participants without depression (p < 0.001). Individual PROs in the MDI questionnaire indicated that lack of energy and trouble sleeping at night were the most common symptoms. Twenty-nine percent (95% CI 22%–36%) lacked energy and 29% (95% CI 23%–37%) had trouble sleeping all/most of the time (Fig. 5C). There were no statistically significant differences in depression scores between different indications for stoma formation (p = 0.26). Patients who had an ileostomy because of cancer tended to have lower median depression scores (5.5, IQR 1–10.5, range 0–39), and patients with miscellaneous stoma indications tended to have a higher median depression score (13, IQR 6–17, range 0–32). Patients with UC had a median score of 8 (IQR 4–15, range 0–50), and patients with CD had a median depression score of 9 (IQR 4–17, range 0–32).
FIGURE 5.
Major Depression Inventory (MDI). A, The overall MDI depression score, with indications of depression severity (median and IQR). B, Comparison of MDI scores with a Danish normative score12 (mean, 95% CI). C, Proportions of individual answers to the MDI questionnaire. DK = Danish; IQR = interquartile range.
Lack of energy affected Stoma-QoL negatively, both when participants with an indication of depression were included (mean difference 13.7, 10–17 points, p < 0.001) and when they were excluded (mean difference 7.7, 3–13 points, p = 0.002). Self-perceived health (EQ-5D-5L VAS) was negatively affected if participants felt tired during the day, regardless of depression score (median difference 18 points, p < 0.001). HRQoL was negatively associated with being unemployed/receiving incapacity benefit (p = 0.02), and drinking <1 unit or >15 units of alcohol per week (p = 0.02). We found no associations between HRQoL and education, income, smoking habits, or marital status.
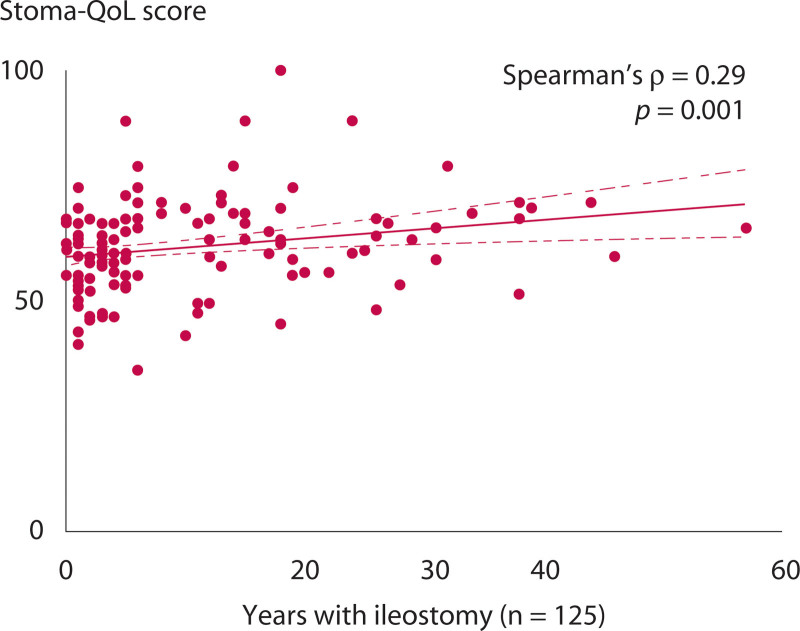
The Stoma-QoL score was positively associated with how long the patients had had their ileostomy (Spearman ρ = 0.24, p = 0.004, n = 153). Furthermore, the correlation was stronger if participants with an indication of depression were excluded (Spearman ρ = 0.29, p = 0.001, n = 125; Fig. 6).
FIGURE 6.
Relationship between years living with an ileostomy and Stoma-QoL score in patients without depression. Stoma-QoL = stoma-specific quality of life.
The sensitivity analyses elicited no differences in overall scores of EQ-5D-5L or MDI when using simple imputations for the missing data. Mean Stoma-QoL decreased 0.1 point if assigning the best HRQoL choice for missing values and decreased 0.3 if assigning a mean value for missing values. Neither strategy changed main proportions or comparisons.
DISCUSSION
The present study demonstrates that PROs are useful to investigate issues that may affect HRQoL in patients with specific diseases or conditions. We found that people living with an ileostomy frequently experience fatigue reflected in tiredness, lack of energy, poor sleep, and the need to rest during the day. They also report a need to know the immediate location of the nearest toilet and fear of leakages. Having an ileostomy may lead to feeling less sexually attractive. A fifth of the patients feel depressed. A third experience pain and have trouble performing their usual activities. People living with an ileostomy may have low HRQoL, which almost a fourth of them attribute directly to their ileostomy.
Fatigue is frequent in patients with IBD, both during active disease and in patients without a flare.15 Our data indicate that having an ileostomy in itself may be associated with fatigue. Generic questionnaires that do not investigate fatigue, sleep, and stoma-related issues possibly generate falsely elevated HRQoL scores, which can complicate the comparison of HRQoL scores in patients who have a stoma with scores in the background population. Visual analog scale scores of self-perceived HRQoL may improve the comparison, but VAS scores do not offer possible explanations of low HRQoL or inform the effort to identify treatment opportunities. In the present study, HRQoL was assessed with a generic questionnaire (EQ-5D-5L). Even though EQ-5D-5L is not sensitive to stoma-specific burdens, it still indicated that people living with ileostomies have a lower HRQoL than the background Danish population. Although statistically significant, a 0.124 difference in the index score is not necessarily clinically important. The individual PROs show that, in particular, pain and the ability to perform normal activity can be affected. Moreover, they support the overall MDI score, indicating that almost one-fifth of the patients are depressed. Looking into the individual questions of the MDI questionnaire, lack of energy and poor sleep are the main explanations for the high depression score. This underscores the significance of selecting appropriate PROs for investigation and of the cautious interpretation of the overall scores.
Only a few previous studies have investigated stoma-specific HRQoL in people living with ileostomies. The participants in the present study had a mean Stoma-QoL score of 58.8 points. For comparison, a Danish population of patients with an ileostomy or colostomy had a mean score of 62.6 points,7 and Swedish patients with a sigmoidostomy scored 64.7 points.16 This indicates that the type of stoma may affect the overall HRQoL. Our results are similar to those of previous studies in the sense that we found low overall HRQoL, fatigue, and increasing HRQoL with increasing time since ileostomy formation.1,17 The higher scores can reflect response shifts, where a gradual adaptation to new life circumstances can change self-assessment of HRQoL.18 Studies have found that, although people living with ileostomies often cope well, subgroups can have considerable problems.2,3,19 A low HRQoL may not necessarily be caused by having a stoma per se. In a study comparing patients with CD with or without a stoma, HRQoL was not decreased in the group living with a stoma.20 In patients treated for rectal cancer, HRQoL might even be higher in those with a stoma, due to fewer GI problems.21
In the present study, we invited all people with ileostomies available from the general population in the Central Denmark Region, which enhances the external validity of the study. Differences in patient education may affect HRQoL,22 as may differences in surgical techniques,23 so the external validity of the overall scores may be limited to patients receiving comparable health care. The response rate was fair, but this does not rule out selection bias, and those experiencing problems could be more likely to accept the invitation to participate than those who experienced no problems. It is also conceivable that fatigued patients with the lowest HRQoL would decline the invitation, balancing any bias. Most responders were women and older than nonresponders, which may reduce the external validity. Stratification for comorbidity and treatment was not possible in this study, but most people living with ileostomies are not receiving any treatment relating to their stoma, and the highlighted PROs may affect their HRQoL regardless. Not all patients answered all questions, and we may have introduced bias by omitting overall scores if a single question was missing. The sensitivity analysis did not indicate that missing values affected the overall conclusions, and the bias was toward estimating better HRQoL, which strengthens our findings. We have included answers from both electronic and paper versions of the questionnaires, which could introduce differences in responses; but, in general, the 2 methods generate comparable results.24 Evaluation of symptoms before and after stoma creation and comparison of similar groups with and without ileostomy could have elaborated our analyses. We did not have information on current disease state or treatment. Active disease in patients with CD or ongoing cancer treatment may adversely affect fatigue or HRQoL. The present data did not allow evaluation of possible surgical alternatives to stoma formation, whether the patient actively chose the surgery or whether the stoma was permanent, which are all factors that may affect HRQoL. Future studies could include these parameters.
Treatment strategies for this patient group are limited. Supplements of high-dose vitamin B1 may reduce fatigue in patients with IBD,25 and because most patients with ileostomies have or have had IBD, this treatment could potentially benefit some patients. Deficiencies from iron, zinc, vitamin D, and vitamin B12 are associated with impaired HRQoL in patients with an ileostomy,1 which implies that increased attention to their nutritional status could improve quality of care. Our data indicate that a few simple questions may help discover patients who could benefit from additional assessments, although this should be tested further in prospective intervention studies.
Our study underpins that fatigue is frequent in people living with ileostomies and that this may influence their daily lives and HRQoL. The high occurrence of tiredness and lack of energy emphasizes the importance of recognizing fatigue as a clinical manifestation that should be addressed in the clinical management of the patients. Depression, pain, problems performing usual activities, fear of leakages, and sexual problems are also common. Reducing fatigue and stoma-specific challenges ought to be a primary aim in future clinical trials because it potentially may improve HRQoL in people living with ileostomies.
Footnotes
Financial Disclosures: None reported.
Funding/Support: This study was supported by the Colitis-Crohn Patient Association, Denmark, and the Ostomy Patient Association (COPA) Denmark.
Poster presentation at the virtual conference of the European Society for Clinical Nutrition and Metabolism (ESPEN), September 19 to 21, 2020.
REFERENCES
- 1.Schiergens TS, Hoffmann V, Schobel TN, et al. Long-term quality of life of patients with permanent end ileostomy: results of a nationwide cross-sectional survey. Dis Colon Rectum. 2017;60:51–60. [DOI] [PubMed] [Google Scholar]
- 2.Nugent KP, Daniels P, Stewart B, Patankar R, Johnson CD. Quality of life in stoma patients. Dis Colon Rectum. 1999;42:1569–1574. [DOI] [PubMed] [Google Scholar]
- 3.Martinsson ES, Josefsson M, Ek AC. Working capacity and quality of life after undergoing an ileostomy. J Adv Nurs. 1991;16:1035–1041. [DOI] [PubMed] [Google Scholar]
- 4.Gooszen AW, Geelkerken RH, Hermans J, Lagaay MB, Gooszen HG. Quality of life with a temporary stoma: ileostomy vs. colostomy. Dis Colon Rectum. 2000;43:650–655. [DOI] [PubMed] [Google Scholar]
- 5.Brown H, Randle J. Living with a stoma: a review of the literature. J Clin Nurs. 2005;14:74–81. [DOI] [PubMed] [Google Scholar]
- 6.U.S. Department of Health and Human Services FDA Center for Drug Evaluation and Research; U.S. Department of Health and Human Services FDA Center for Biologics Evaluation and Research; U.S. Department of Health and Human Services FDA Center for Devices and Radiological Health. Guidance for industry: patient-reported outcome measures: use in medical product development to support labeling claims: draft guidance. Health Qual Life Outcomes. 2006;4:79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Prieto L, Thorsen H, Juul K. Development and validation of a quality of life questionnaire for patients with colostomy or ileostomy. Health Qual Life Outcomes. 2005;3:62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Devlin NJ, Brooks R. EQ-5D and the EuroQol Group: past, present and future. Appl Health Econ Health Policy. 2017;15:127–137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sørensen J, Davidsen M, Gudex C, Pedersen KM, Brønnum-Hansen H. Danish EQ-5D population norms. Scand J Public Health. 2009;37:467–474. [DOI] [PubMed] [Google Scholar]
- 10.van Hout B, Janssen MF, Feng YS, et al. Interim scoring for the EQ-5D-5L: mapping the EQ-5D-5L to EQ-5D-3L value sets. Value Health. 2012;15:708–715. [DOI] [PubMed] [Google Scholar]
- 11.Olsen LR, Jensen DV, Noerholm V, Martiny K, Bech P. The internal and external validity of the Major Depression Inventory in measuring severity of depressive states. Psychol Med. 2003;33:351–356. [DOI] [PubMed] [Google Scholar]
- 12.Olsen LR, Mortensen EL, Bech P. Prevalence of major depression and stress indicators in the Danish general population. Acta Psychiatr Scand. 2004;109:96–103. [DOI] [PubMed] [Google Scholar]
- 13.Harris PA, Taylor R, Minor BL, et al. ; REDCap Consortium. The REDCap consortium: building an international community of software platform partners. J Biomed Inform. 2019;95:103208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)–a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42:377–381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Farrell D, McCarthy G, Savage E. Self-reported symptom burden in individuals with inflammatory bowel disease. J Crohn’s Colitis. 2016;10:315–322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kald A, Juul KN, Hjortsvang H, Sjödahl RI. Quality of life is impaired in patients with peristomal bulging of a sigmoid colostomy. Scand J Gastroenterol. 2008;43:627–633. [DOI] [PubMed] [Google Scholar]
- 17.El-Tawil A, Nightingale P. Living with stoma: long-term effects on patients’ quality of life. J Clin Cell Immunol. 2013;4:145. [Google Scholar]
- 18.Sprangers MAG, Schwartz CE. Integrating response shift into health-related quality of life research: a theoretical model. Soc Sci Med. 1999;48:1507–1515. [DOI] [PubMed] [Google Scholar]
- 19.Kennedy HJ, Lee ECG, Claridge G, Truelove SC. The health of subjects living with a permanent ileostomy. Q J Med. 1982;51:341–357. [PubMed] [Google Scholar]
- 20.Abdalla MI, Sandler RS, Kappelman MD, et al. The impact of ostomy on quality of life and functional status of Crohn’s disease patients. Inflamm Bowel Dis. 2016;22:2658–2664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bloemen JG, Visschers RG, Truin W, Beets GL, Konsten JL. Long-term quality of life in patients with rectal cancer: association with severe postoperative complications and presence of a stoma. Dis Colon Rectum. 2009;52:1251–1258. [DOI] [PubMed] [Google Scholar]
- 22.Danielsen AK, Burcharth J, Rosenberg J. Patient education has a positive effect in patients with a stoma: a systematic review. Colorectal Dis. 2013;15:e276–e283. [DOI] [PubMed] [Google Scholar]
- 23.Bekkers MJTM, van Knippenberg FCE, van den Borne HW, Poen H, Bergsma J, vanBergeHenegouwen GP. Psychosocial adaptation to stoma surgery: a review. J Behav Med. 1995;18:1–31. [DOI] [PubMed] [Google Scholar]
- 24.Muehlhausen W, Doll H, Quadri N, et al. Equivalence of electronic and paper administration of patient-reported outcome measures: a systematic review and meta-analysis of studies conducted between 2007 and 2013. Health Qual Life Outcomes. 2015;13:167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bager P, Hvas CL, Rud CL, Dahlerup JF. Randomised clinical trial: high-dose oral thiamine versus placebo for chronic fatigue in patients with quiescent inflammatory bowel disease. Aliment Pharmacol Ther. 2021;53:79–86. [DOI] [PubMed] [Google Scholar]