Abstract
BACKGROUND:
With advances in medical care, patients with cystic fibrosis are more commonly living into adulthood, yet there are limited data describing the need for GI surgery and its outcomes in adult cystic fibrosis patients.
OBJECTIVE:
We aim to use a national administrative database to evaluate trends in abdominal GI surgery and associated postoperative outcomes among adult cystic fibrosis patients.
DESIGN:
This was a national retrospective cohort study.
SETTING:
A national all-payor administrative database from 2000 to 2014 was used.
PATIENTS:
Patients included adults (age ≥18 years) with cystic fibrosis undergoing abdominal GI surgery.
MAIN OUTCOME MEASURES:
The primary outcome was trend over time in number of surgical admissions. Secondary outcomes included morbidity and mortality by procedure type.
RESULTS:
We identified 3075 admissions for abdominal surgery, of which 28% were elective. Major GI surgical procedures increased over the study period (p < 0.01), whereas appendectomy and cholecystectomy did not demonstrate a clear trend (p = 0.90). The most common procedure performed was cholecystectomy (n = 1280; 42%). The most common major surgery was segmental colectomy (n = 535; 18%). Obstruction was the most common surgical indication (n = 780; 26%). For major surgery, in-hospital mortality was 6%, morbidity was 37%, and mean length of stay was 15.9 days (SE 1.2).
LIMITATIONS:
The study is limited by a lack of granular physiological and clinical data within the administrative data source.
CONCLUSIONS:
Major surgical admissions for adult patients with cystic fibrosis are increasing, with the majority being nonelective. Major surgery is associated with significant morbidity, mortality, and prolonged length of hospital stay. These findings may inform perioperative risk for adult patients with cystic fibrosis in need of GI surgery. See Video Abstract at http://links.lww.com/DCR/B850.
PROCEDIMIENTOS QUIRÚRGICOS ABDOMINALES EN PACIENTES ADULTOS CON FIBROSIS QUÍSTICA: ¿CUÁLES SON LOS RIESGOS?
ANTECEDENTES:
Con los avances en la medicina, los pacientes con fibrosis quística viven más comúnmente hasta la edad adulta, pero hay datos escasos que describan la necesidad de cirugía gastrointestinal y sus resultados en pacientes adultos con fibrosis quística.
OBJETIVO:
Nuestro objetivo es utilizar una base de datos administrativa nacional para evaluar las tendencias en la cirugía gastrointestinal abdominal y los resultados posoperatorios asociados entre los pacientes adultos con fibrosis quística.
DISEÑO:
Estudio de cohorte retrospectivo nacional.
AJUSTE:
Base de datos administrativa nacional de todas las instituciones pagadoras desde 2000 a 2014.
PACIENTES:
Todos los pacientes adultos (edad> 18) con fibrosis quística sometidos a cirugía gastrointestinal abdominal.
PRINCIPALES MEDIDAS DE RESULTADO:
El resultado primario fue la tendencia a lo largo del tiempo en el número de ingresos quirúrgicos. Los resultados secundarios incluyeron morbilidad y mortalidad por tipo de procedimiento.
RESULTADOS:
Identificamos 3.075 ingresos por cirugía abdominal de los cuales el 28% fueron electivos. Los procedimientos quirúrgicos gastrointestinales mayores aumentaron durante el período de estudio (p <0,01) mientras que la apendicectomía y la colecistectomía no demostraron una tendencia clara (p = 0,90). El procedimiento realizado con mayor frecuencia fue la colecistectomía (n = 1.280; 42%). La cirugía mayor más común fue la colectomía segmentaria (n = 535; 18%). La obstrucción fue la indicación quirúrgica más común (n = 780; 26%). Para la cirugía mayor, la mortalidad hospitalaria fue del 6%, la morbilidad del 37% y la estadía media de 15,9 días (EE 1,2).
LIMITACIONES:
El estudio está limitado por la falta de datos clínicos y fisiológicos granulares dentro de la fuente de datos administrativos.
CONCLUSIONES:
Los ingresos quirúrgicos mayores de pacientes adultos con fibrosis quística están aumentando y la mayoría no son electivos. La cirugía mayor se asocia con una morbilidad y mortalidad significativas y una estancia hospitalaria prolongada. Estos hallazgos pueden informar el riesgo perioperatorio para pacientes adultos con fibrosis quística que necesitan cirugía gastrointestinal. Consulte Video Resumen en http://links.lww.com/DCR/B850. (Traducción—Dr. Felipe Bellolio)
Keywords: Abdominal surgery, Colorectal surgery, Cystic fibrosis
Cystic fibrosis (CF) is an autosomal recessive disease of the cystic fibrosis transmembrane conductance regulator (CFTR) gene, affecting bicarbonate and chloride transport at the cellular level, including along the apical surface of the epithelial lining of the intestinal tract, where it modulates luminal surface liquid.1 Progressive respiratory failure is the most common cause of premature death in CF patients; however, GI dysfunction is a critical cause of morbidity and includes pancreatic insufficiency with malabsorption, distal intestinal obstruction syndrome (DIOS), and meconium ileus, as well as increased risk for colon cancer.2–4 Recent therapeutic advancements, including the development of CFTR modulators, have resulted in improved life expectancy and provide partial correction of the molecular defect, including in the GI tract.5 For a cohort of CF patients born in 2017, the median predicted survival was 46.2 years, compared to 29 years for those born in 1986.6 In addition to their improved life expectancy, the proportion of CF patients older than 18 years exceeded 50% (52.5%) for the first time in 2016, rising from 40% in 2002.6
Cystic fibrosis–associated GI pathologies including meconium ileus, gastroesophageal reflux disease, DIOS, pancreatic exocrine insufficiency, and liver disease present in childhood and persist throughout the lifespan.3,4 As a result of improved life expectancy, common adult surgical problems and emergencies may also arise. Relative to non-CF patients, adult patients with CF have demonstrated an increased risk of biliary pathology as well as colorectal and pancreatic cancer.7,8 It is also known that CF patients may be at an increased risk of perioperative complications attributable to respiratory insufficiency, poorly controlled diabetes, chronic malnutrition or, in the case of patients who have received a lung transplant, chronic immunosuppression.9 Yet, data regarding the frequency and outcomes of GI surgery in the adult CF population are largely limited to small single-institution series.
This study sought to characterize trends, risks, and outcomes of GI surgery in a growing adult CF patient population using a national administrative database.
METHODS
Study Design/Data Source
For this retrospective study evaluating trends and outcomes in adult CF patients undergoing GI surgery, we used the Nationwide Inpatient Sample (NIS), the largest US all-payor database, from 2000 to 2014. The NIS is an administrative database compiled as a part of the Healthcare Cost and Utilization Project (HCUP) under the auspices of the Agency for Healthcare Research and Quality (AHRQ). Through the use of hospital billing data, diagnosis codes, and procedural codes, the NIS captures patient demographics, diagnoses, and procedures from a representative 20% sampling of US inpatient hospital discharges. Discharge weights were applied per the NIS sampling algorithm to extrapolate data from the representative 20% sample to the full US population. Further detailed information related to data collection methodology may be found at http://www.hcup-us.ahrq.gov. As this study contained only deidentified data without any protected health information, the study is not considered human subject research and was therefore not subject to institutional review board approval. This study was conducted in accordance with STROBE (STrengthening the Reporting of OBservational studies in Epidemiology) guidelines.
Patients
Using International Classification of Diseases, 9th Revision (ICD-9), diagnosis codes 277.0, 277.00, 277.01, 277.02, 277.03, and 277.09, we identified all admissions for patients with CF during the study period. Of patients admitted with a diagnosis of CF, we selected all admissions for adult patients (age ≥18 years) undergoing common GI surgical procedures, as denoted by the ICD-9 procedure codes listed in Supplemental Table 1 at http://links.lww.com/DCR/B851. In brief, these included cholecystectomy, small bowel resection, appendectomy, colectomy, proctectomy, ostomy creation/revision/reversal, and lysis of adhesions. The utilization of laparoscopy was denoted by a designated procedure code, although no data are available for conversion to open surgery. Indication for surgery was catalogued according to a query for ICD-9 diagnosis codes for common GI pathologies, as outlined in Supplemental Table 1 at http://links.lww.com/DCR/B851. Patients undergoing more than 1 procedure and with more than 1 diagnosis were noted as such. Patient demographics, hospital characteristics, and treatment setting were extracted from the database. Specifically, extracted variables are listed in Table 1, with age stratified by decade. Hospital size is stratified by bed size, with strata varying by urban versus rural location and teaching status (https://www.hcup-us.ahrq.gov/db/vars/hosp_bedsize/nisnote.jsp). To quantify burden of comorbid illness in administrative data, Charlson Comorbidity Index (CCI) was calculated using ICD-9 diagnosis codes.10
TABLE 1.
Demographics and hospital characteristics for all study patientsa
| Demographics and hospital characteristics | Missing | All n = 3075 | Nonelective n = 2004 | Elective n = 781 | p value |
|---|---|---|---|---|---|
| Age, y, n (%) | 0 | <0.01 | |||
| 18–29 | 1658 (54) | 1184 (59) | 331 (42) | ||
| 30–39 | 657 (22) | 383 (19) | 203 (26) | ||
| 40–49 | 386 (13) | 258 (13) | 108 (14) | ||
| 50–59 | 200 (7) | 104 (5) | 80 (10) | ||
| 60+ | 154 (5) | 74 (4) | 59 (8) | ||
| Female, n (%) | 0 | 1692 (55) | 1072 (54) | 442 (57) | 0.50 |
| Race, n (%) | 503 (16) | 0.05 | |||
| White | 2252 (91) | 1518 (91) | 564 (91) | ||
| Black | 48 (2) | 28 (2) | 15 (2) | ||
| Hispanic | 91 (4) | 72 (4) | 15 (2) | ||
| Asian/Pacific Islander | 5 (0) | 5 (0) | 0 (0) | ||
| Native American | 15 (1) | 0 (0) | 15 (2) | ||
| Other | 67 (3) | 54 (3) | 8 (1) | ||
| Payor, n (%) | 571 (19) | 0.32 | |||
| Medicare | 575 (24) | 377 (25) | 154 (26) | ||
| Medicaid | 414 (17) | 250 (16) | 116 (19) | ||
| Private | 1215 (51) | 759 (50) | 299 (50) | ||
| Self-pay | 102 (4) | 83 (5) | 14 (2) | ||
| No charge | 5 (0) | 0 (0) | 5 (0) | ||
| Other | 93 (4) | 64 (4) | 13 (2) | ||
| Charlson Comorbidity Index, n (%) | 0 | 0.20 | |||
| 0 | 1437 (47) | 947 (47) | 347 (45) | ||
| 1 | 1028 (34) | 689 (34) | 238 (31) | ||
| 2+ | 591 (20) | 368 (18) | 195 (25) | ||
| History of lung transplant, n (%) | 0 | 315 (10) | 181 (9) | 109 (14) | 0.08 |
| Malnutrition, n (%) | 0 | 406 (13) | 320 (16) | 71 (9) | 0.03 |
| Hospital size, n (%) | 9 (<1) | 0.14 | |||
| Small | 243 (8) | 162 (8) | 71 (9) | ||
| Medium | 682 (21) | 394 (20) | 209 (27) | ||
| Large | 2113 (70) | 1434 (72) | 496 (64) | ||
| Location/teaching, n (%) | 9 (<1) | 0.12 | |||
| Rural | 204 (7) | 139 (7) | 45 (6) | ||
| Urban nonteaching | 596 (20) | 431 (22) | 113 (15) | ||
| Urban teaching | 2237 (74) | 1420 (71) | 619 (80) |
a Data for elective vs nonelective available for 2002–2014; total n = 2784.
Outcomes
Our primary outcome was the utilization of elective and nonelective GI surgical procedures in adult CF patients over the study period. Procedures were classified as elective if the hospital admission was designated elective by the NIS. Due to small numbers for any given year, for certain analyses, the study period was dichotomized into early (2000–2007) and late (2008–2014). Secondary outcomes included indication for surgery, in-hospital death, in-hospital complications, length of hospital stay, and discharge to location other than home. Complications were identified using ICD-9 diagnosis codes as listed in Supplemental Table 1 at http://links.lww.com/DCR/B851, whereas tracheostomy was recorded by ICD-9 procedure code.
Subset Analyses
Separate analyses were conducted for elective and nonelective admissions. Elective versus nonelective admissions were designated in the NIS beginning in 2002; thus, these comparisons were conducted for study years 2002 to 2014. Distinct analyses were also performed according to procedure type. Major procedures included small bowel resection, colectomy, proctectomy, ostomy creation, ostomy closure, ostomy revision, and lysis of adhesions. Minor surgery included appendectomy and cholecystectomy. A comparison of CF versus non-CF patients undergoing segmental colectomy was conducted.
Statistical Analysis
Test for trend over time was assessed using Joinpoint regression analyses on logarithmically transformed data. Specifically, we evaluated for significant change in the average annual percentage change in case numbers, as has been previously described.11 Trend analyses were conducted using Joinpoint Regression Program 4.8.0.1 (National Cancer Institute). Categorical variables were analyzed using the χ2 or Fisher exact test when appropriate. Continuous variables were compared using 2-tailed independent samples t test. Comparisons were made with respect to age, race, insurance status, CCI score, hospital size, and hospital teaching status. Throughout all analyses, statistical significance was determined by a criterion of p < 0.05. All non–trend-related analyses were conducted using IBM SPSS Statistics version 25.0 for Macintosh (IBM Corp., Armonk, NY).
RESULTS
Demographics
We identified 3075 admissions meeting inclusion criteria, of which 28% were elective. Mean age at the time of surgery was 31.9 (SE 0.52) years, with 24% of patients aged 40 years or older. Lung transplant recipients comprised 12% of CF patients receiving major surgery and 9% of CF patients receiving minor surgery. Patient and hospital characteristics are reported in Table 1.
Operative Trends
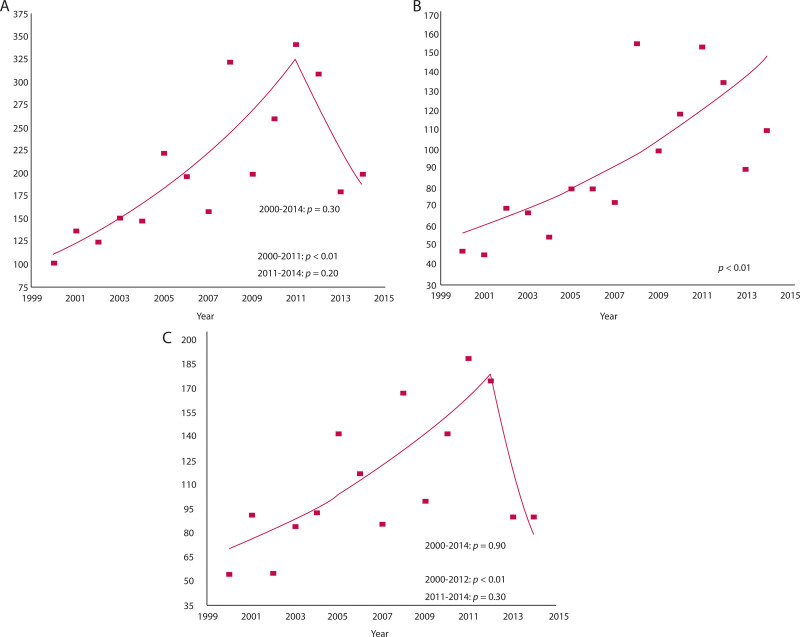
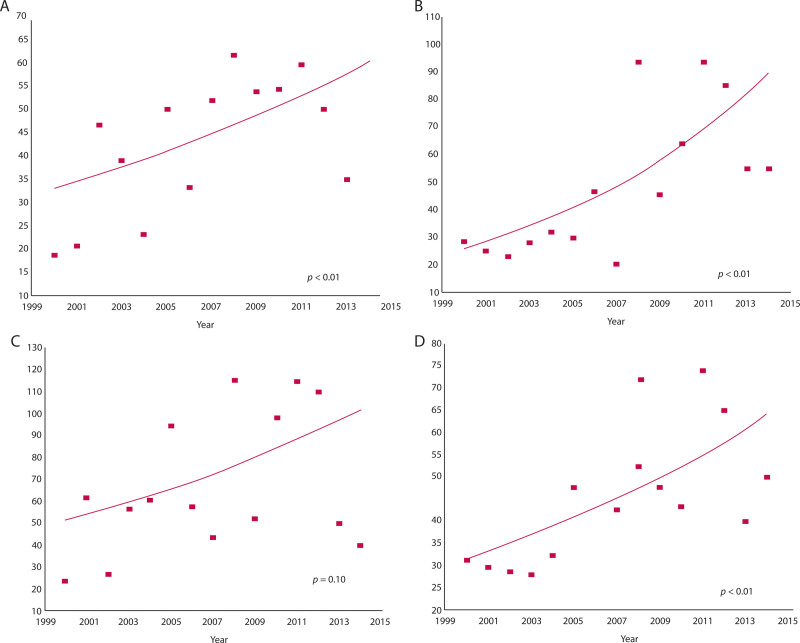
Significant increases in the number of admissions for surgery over the study period were noted in total procedures (2000–2011), major procedures (2000–2014), and minor procedures (2000–2012; Fig. 1). Over the full study period of 2000 to 2014, total and minor procedures did not demonstrate a trend (Fig. 1). Stratifying by age, admissions for major and minor surgery increased significantly over the study period in patients aged 30 years or older (Fig. 2). Major procedures also rose significantly in patients aged 18 to 30 years, while the trend in minor procedures for patients aged 18 to 30 years did not reach significance (Fig. 2).
FIGURE 1.
Number of procedures per year: A, total procedures; B, major procedures; C, minor procedures.
FIGURE 2.
Number of procedures per year: A, major procedures, ages 18–30 years; A, major procedures, age ≥30 years; C, minor procedures, ages 18–30 years; D, and minor procedures, age ≥30 years.
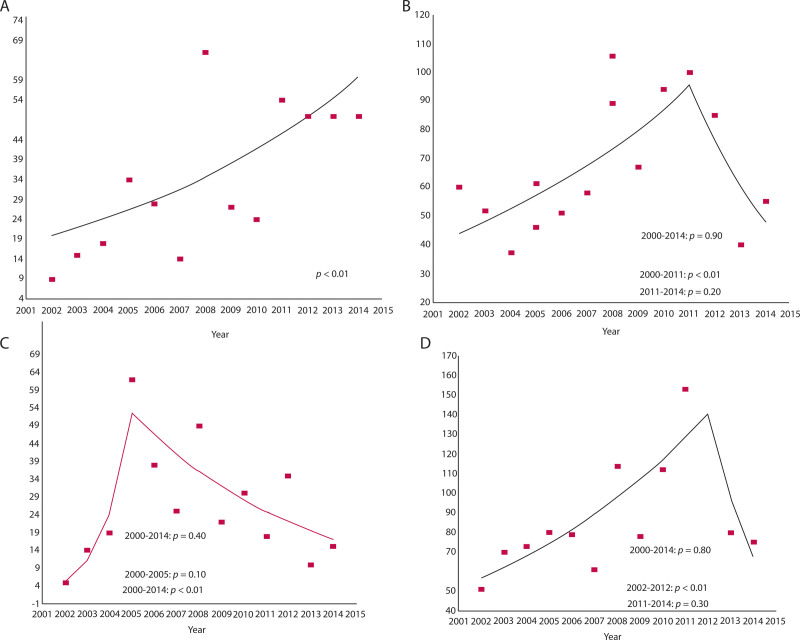
Major elective surgical admissions rose significantly over the study period, whereas nonelective major admissions increased from 2000 to 2011 and did not demonstrate a trend from 2011 to 2014 (Fig. 3). When stratified by elective status, minor elective surgical admissions decreased from 2005 to 2014, whereas minor nonelective admissions increased from 2002 to 2012 (Fig. 3).
FIGURE 3.
Number of procedures per year: A, major elective; B, major nonelective; C, minor elective; and D, minor nonelective.
Surgical Indications and Operations Performed
The most common indication for surgery was bowel obstruction (n = 780; 26%; Table 2). Of the 122 CF patients operated for colorectal cancer, 53% were younger than 50 years. For major operations, the most common operation was segmental colectomy (n = 535; 18%; Table 2). The overall use of laparoscopy for major cases increased during the study (early vs late: 9% vs 21%; p = 0.01). A minimally invasive approach was used in the majority of minor procedures regardless of admission type (nonelective vs elective: 89% vs 86%; p = 0.53).
TABLE 2.
Operative details
| Operative details | All n = 3075 | Nonelective n = 2004 | Elective n = 781 | p value |
|---|---|---|---|---|
| Indication, n (%) | ||||
| Appendicitis | 432 (14) | 377 (9) | 34 (2) | <0.01 |
| Polyp | 43 (1) | 29 (1) | 19 (1) | 0.38 |
| Diverticulitis | 36 (1) | 22 (1) | 9 (1) | 0.86 |
| Colorectal cancer | 122 (2) | 41 (1) | 72 (5) | <0.01 |
| Obstruction | 780 (26) | 756 (18) | 232 (15) | 0.18 |
| Cholecystitis | 241 (8) | 170 (4) | 56 (4) | 0.72 |
| Fistula | 543 (18) | 497 (12) | 124 (8) | 0.05 |
| Sepsis/perforation | 344 (11) | 635 (15) | 122 (8) | <0.01 |
| Procedure, n (%) | ||||
| Small bowel resection | 298 (10) | 212 (5) | 56 (4) | 0.29 |
| Segmental colectomy | 535 (18) | 342 (8) | 172 (11) | 0.13 |
| Total colectomy | 71 (2) | 56 (1) | 10 (1) | 0.29 |
| Appendectomy | 623 (20) | 551 (13) | 53 (3) | <0.01 |
| Proctectomy | 68 (2) | 14 (0) | 55 (4) | <0.01 |
| Stoma creation | 266 (9) | 198 (5) | 34 (2) | 0.04 |
| Stoma revision | 68 (2) | 40 (1) | 19 (1) | 0.67 |
| Stoma closure | 142 (5) | 24 (1) | 104 (7) | <0.01 |
| Lysis of adhesions | 292 (10) | 170 (4) | 102 (7) | 0.08 |
| Cholecystectomy | 1280 (42) | 800 (19) | 359 (23) | 0.14 |
| Multiple procedures | 558 (18) | 388 (9) | 167 (11) | 0.46 |
| Minimally invasive operation, n (%) | 1696 (56) | 1214 (29) | 361 (23) | 0.04 |
In-Hospital Outcomes
Among major operations, patients undergoing nonelective procedures were more likely to have malnutrition (nonelective vs elective: 27% vs 10%; p < 0.01), although CCI score was similar (p = 0.61; Table 3). Overall morbidity was high in patients undergoing major surgery (37%) and differed by admission type (nonelective vs elective: 42% vs 28%; p = 0.03). Outcomes were generally similar for nonelective compared to elective minor procedures (Table 4).
TABLE 3.
Demographics and outcomes for major surgery
| Demographics, outcomes | All n = 1275 | Nonelective n = 836 | Elective n = 439 | p value |
|---|---|---|---|---|
| Age, y, n (%) | <0.01 | |||
| 18–29 | 608 (48) | 466 (56) | 142 (32) | |
| 30–39 | 277 (22) | 151 (18) | 126 (29) | |
| 40–49 | 203 (16) | 136 (16) | 67 (15) | |
| 50–59 | 108 (9) | 47 (6) | 61 (14) | |
| 60+ | 79 (6) | 35 (4) | 44 (10) | |
| Female, n (%) | 626 (49) | 403 (48) | 224 (51) | 0.68 |
| Charlson Comorbidity Index, n (%) | 0.61 | |||
| 0 | 465 (36) | 313 (38) | 151 (34) | |
| 1 | 420 (33) | 284 (34) | 136 (31) | |
| 2+ | 391 (31) | 239 (29) | 152 (35) | |
| History of lung transplant, n (%) | 148 (12) | 72 (9) | 76 (17) | 0.04 |
| Malnutrition, n (%) | 269 (21) | 227 (27) | 42 (10) | <0.01 |
| Length of stay, d, mean (SE) | 15.9 (1.2) | 17.5 (1.7) | 12.8 (1.6) | <0.01 |
| Nonhome disposition, n (%) | 422 (33) | 320 (38) | 102 (23) | 0.01 |
| Any complication, n (%) | 470 (37) | 348 (42) | 122 (28) | 0.03 |
| Respiratory complication, n (%) | 143 (3) | 105 (13) | 38 (9) | 0.33 |
| Tracheostomy, n (%) | 109 (9) | 85 (10) | 24 (6) | 0.20 |
| Mortality, n (%) | 72 (6) | 62 (7) | 10 (2) | 0.08 |
TABLE 4.
Demographics and outcomes for minor surgery
| Demographics, outcomes | All n = 1509 | Nonelective n = 1168 | Elective n = 342 | p value |
|---|---|---|---|---|
| Age, y, n (%) | 0.92 | |||
| 18–29 | 907 (60) | 718 (62) | 189 (55) | |
| 30–39 | 308 (20) | 231 (20) | 77 (23) | |
| 40–49 | 164 (11) | 122 (11) | 41 (12) | |
| 50–59 | 76 (5) | 57 (5) | 19 (6) | |
| 60+ | 54 (4) | 39 (3) | 15 (4) | |
| Female, n (%) | 887 (59) | 669 (57) | 218 (64) | 0.32 |
| Charlson Comorbidity Index, n (%) | 0.75 | |||
| 0 | 829 (55) | 633 (54) | 196 (57) | |
| 1 | 507 (34) | 405 (35) | 102 (30) | |
| 2+ | 172 (11) | 129 (11) | 43 (13) | |
| History of lung transplant, n (%) | 142 (9) | 109 (9) | 33 (10) | 0.95 |
| Malnutrition, n (%) | 122 (8) | 93 (8) | 29 (8) | 0.91 |
| Length of stay, d, mean (SE) | 8.1 (0.6) | 7.8 (0.6) | 9.0 (1.3) | <0.01 |
| Nonhome disposition, n (%) | 159 (11) | 106 (9) | 53 (16) | 0.12 |
| Any complication, n (%) | 164 (11) | 121 (10) | 43 (13) | 0.59 |
| Respiratory complication, n (%) | 59 (4) | 39 (3) | 19 (6) | 0.39 |
| Tracheostomy, n (%) | 10 (1) | 5 (0) | 5 (1) | 0.39 |
| Mortality, n (%) | 5 (0) | 5 (0) | 0 (0) | 0.59 |
Segmental Colectomy: CF vs non-CF Patients
Cystic fibrosis patients undergoing segmental colectomy were, on average, more than 2 decades younger than non-CF patients, with differences noted in operative indication (Table 5). Operative details and postoperative outcomes for CF and non-CF patients stratified by admission status are shown in Table 5.
TABLE 5.
Demographics, indications, and outcomes for segmental colectomy: CF patients vs non-CF patients
| Demographics, indications, outcomes | CF elective n = 172 | Non-CF elective n = 1,813,446 | p value elective: CF vs non-CF | CF nonelective n = 342 | Non-CF nonelective n = 1,461,305 | p value nonelective: CF vs non-CF |
|---|---|---|---|---|---|---|
| Age, y, n (%) | <0.01 | <0.01 | ||||
| 18–29 | 38 (22) | 32,335 (2) | 167 (49) | 56,843 (4) | ||
| 30–39 | 39 (23) | 78,906 (4) | 48 (14) | 79,915 (6) | ||
| 40–49 | 28 (17) | 196,528 (11) | 84 (25) | 155,651 (11) | ||
| 50–59 | 43 (25) | 383,516 (21) | 23 (7) | 247,563 (17) | ||
| 60+ | 24 (14) | 1,122,159 (62) | 20 (6) | 921,331 (63) | ||
| Age, y, mean (SE) | 42.4 (2.3) | 63.3 (0.1) | <0.01 | 34.7 (1.8) | 64.0 (0.1) | <0.01 |
| Female, n (%) | 71 (41) | 979,551 (54) | 0.13 | 131 (38) | 782,013 (54) | 0.01 |
| Charlson Comorbidity Index, n (%) | 0.24 | <0.01 | ||||
| 0 | 57 (33) | 671,603 (37) | 119 (35) | 500,691 (34) | ||
| 1 | 39 (23) | 237,172 (13) | 113 (33) | 240,289 (16) | ||
| 2+ | 76 (44) | 904,671 (50) | 110 (32) | 720,323 (49) | ||
| History of lung transplant, n (%) | 24 (14) | 299 (0) | <0.01 | 47 (14) | 0 (0) | <0.01 |
| Malnutrition, n (%) | 14 (8) | 64,958 (4) | 0.14 | 52 (15) | 195,700 (13) | 0.63 |
| Obstruction, n (%) | 63 (37) | 395,697 (22) | 0.03 | 196 (57) | 539,133 (37) | <0.01 |
| Diverticulitis, n (%) | 9 (6) | 408,642 (23) | 0.01 | 12 (4) | 365,688 (25) | <0.01 |
| Cancer, n (%) | 43 (25) | 695,500 (38) | 0.10 | 36 (10) | 405,150 (28) | <0.01 |
| Polyp, n (%) | 9 (6) | 331,970 (18) | 0.05 | 19 (6) | 103,967 (7) | 0.60 |
| Fistula, n (%) | 33 (19) | 189,173 (10) | 0.08 | 121 (35) | 292,237 (20) | <0.01 |
| Sepsis/perforation, n (%) | 24 (14) | 112,640 (6) | 0.05 | 96 (28) | 488,363 (33) | 0.35 |
| Stoma creation, n (%) | 10 (6) | 141,492 (8) | 0.64 | 80 (23) | 511,827 (35) | 0.04 |
| Laparoscopy, n (%) | 39 (23) | 425,051 (23) | 0.89 | 49 (14) | 116,829 (8) | 0.05 |
| Length of stay, d, mean (SE) | 14.1 (3.0) | 7.3 (0.1) | <0.01 | 13.9 (1.5) | 13.8 (0.1) | <0.01 |
| Nonhome disposition, n (%) | 49 (28) | 415,411 (23) | 0.45 | 121 (36) | 808,185 (55) | <0.01 |
| Any complication, n (%) | 48 (28) | 449,417 (25) | 0.67 | 129 (38) | 679,175 (47) | 0.14 |
| Respiratory complication, n (%) | 14 (8) | 80,172 (4) | 0.26 | 42 (12) | 213,828 (15) | 0.55 |
| Tracheostomy, n (%) | 9 (6) | 8371 (1) | <0.01 | 9 (3) | 36,479 (3) | 0.88 |
| Mortality, n (%) | 0 (0) | 25,830 (1) | 0.47 | 33 (10) | 117,940 (8) | 0.63 |
CF = cystic fibrosis.
DISCUSSION
In this first national assessment of trends in GI surgery for adult patients with CF, the number of admissions for major surgery increased during the study period (2000–2014), though there has been a recent downward inflection of nonelective major cases. Although patients aged 18 to 30 years constituted the largest age group for all procedure types, the number of operative admissions for patients aged 30 or older increased by nearly 2-fold for all procedure types. This likely reflects the improvements in survival for patients with CF by birth cohort. Although differences in outcome were seen between elective and nonelective admissions for major surgery, complications were high in both admission types, including respiratory complications and need for tracheostomy. Although CF patients undergoing segmental colectomy were younger and had a lower CCI score compared to non-CF patients, CF patients had a complication profile after segmental colectomy that was largely similar to non-CF patients, suggesting that traditional administrative risk adjustment measures may underestimate morbidity and mortality in this population. However, minor surgery did not show a clear frequency trend over the study period and was associated with relatively few postoperative complications. These data may provide a basis for counseling adult patients with CF and their families on expectations surrounding common GI surgical procedures.
Data regarding outcomes for adult CF patients undergoing GI surgery have been limited to a small number of single-institution studies. A 2012 UK study reported on 377 patients in an effort to characterize outcomes for adult CF patients undergoing GI surgery.12 Sharma et al identified DIOS, biliary disease, and gastroesophageal reflux as the most common indications for surgery. Of patients operated on for DIOS (n = 11), there was no mortality, although 3 had prolonged hospitalization due to respiratory complications. Cogliandolo et al published a retrospective review on postoperative outcomes and quality of life in 9 CF patients undergoing laparoscopic cholecystectomy.13 No major postoperative complications were noted, and patients reported improvement in abdominal pain and postprandial vomiting.
The reports above are similar to our study with regard to outcomes for adult CF patients undergoing appendectomy and cholecystectomy. In our cohort, the majority of appendectomy and cholecystectomy procedures were performed minimally invasively (88%). Similar to Cogliandolo’s study of patients undergoing laparoscopic cholecystectomy, we found a low rate of mortality (n = 5; <1%) for both elective and nonelective appendectomy and cholecystectomy.13 Previous studies of the NIS evaluating outcomes after cholecystectomy and appendectomy aligned with our findings of an in-hospital mortality rate of 0.52% for laparoscopic cholecystectomy and a mortality rate of 0.05% and 0.16% for appendectomy in the setting of nonperforated and perforated appendicitis, respectively.14,15 Our data showed an 11% rate of both nonhome disposition and overall complication, with 4% of patients developing respiratory complications and 1% requiring tracheostomy. Dolan et al reported an 8% nonhome disposition after laparoscopic cholecystectomy for a cohort of patients, of whom 36% were older than 60 years.14 In an NIS study of patients undergoing appendectomy from 2004 to 2011, overall complications were 5% for laparoscopic appendectomy and 11% for open appendectomy when performed for nonperforated appendicitis.15 Although direct risk-adjusted comparisons of CF and non-CF patients are challenging, we conclude that laparoscopic appendectomy and cholecystectomy appear safe in selected CF patients.
Although the CF Foundation Patient Registry has shown an increase in CF prevalence in the United States,6 the performance of appendectomy and cholecystectomy in CF patients did not demonstrate a consistent trend over the study period. The reasons for this are not forthcoming from these administrative data. However, given the comorbidity burden of patients with CF, it is feasible that patients with CF were more commonly considered for nonoperative management of appendicitis or biliary colic. It is certainly the case that evidence to support the nonoperative management of appendicitis evolved over the study period16–19 and may have been applied more zealously to marginal operative candidates. Further dedicated studies are required to better define clinical decision-making for CF patients with appendicitis and biliary colic/cholecystitis.
We noted an overall increase in major GI surgery over time, though there was a recent tapering off of this trend for nonelective major cases (Figs. 1 and 3). As the most common indication for major surgery was obstruction, it is possible that the recent change in trajectory for nonelective major surgery may be associated with prevention of distal intestinal obstruction syndrome; however, Cochrane systematic reviews report a paucity of evidence on preventive measures or the utilization of pancreatic enzyme supplementation.20,21
When comparing CF and non-CF patients undergoing colectomy, no differences in mortality or overall complications were identified in either the elective or nonelective groups. Yet, length of stay for CF patients undergoing elective surgery is twice as long as the non-CF group (CF vs non-CF: 14.1 vs 7.3 days; p < 0.01), with an increase in postoperative tracheostomy (CF vs non-CF: 6% vs 1%; p < 0.01). Nonelective CF patients showed no clinically significant differences in length of stay compared to non-CF patients and had a decreased risk of ostomy creation (Table 5). Similar overall morbidity and mortality for CF patients compared to non-CF patients appear to challenge traditional risk adjustment measures. Increasing age and burden of comorbid illness have been associated with increased morbidity and mortality in large data colectomy risk adjustment models.22,23 Thus, it is striking that the CF group has similar morbidity and mortality despite being decades younger and, in the case of nonelective colectomy, having a lower CCI score. Perhaps due to differences in operative indication or other unmeasured patient or case complexity, it is reasonable to hypothesize that unmeasured confounders account for what may be excess morbidity for CF patients undergoing segmental colectomy. Considering a broader cross-selection of major GI surgery, tracheostomy rate was 10% in nonelective cases and 6% in elective cases. In-hospital mortality was 7% in nonelective major GI cases and 2% in elective major GI cases. Major GI surgery for adult CF patients carries significant morbidity and mortality, possibly in excess of non-CF patients. These data may provide caution to providers when counseling CF patients on preoperative risk.
The findings of this study are limited by the retrospective design, which utilized an administrative data source. Accordingly, these data are susceptible to coding errors and a lack of clinical granularity, such as surgical complexity and physiological status, including pulmonary function. Regarding coding practices, secular trends have been observed, with increased attention to coding comorbid conditions to capture admission complexity.24,25 However, our findings of increasing major surgical utilization in CF patients are in line with the known increasing prevalence of CF in the United States,6 and the concurrent absence of a clear trend in minor cases suggests that the increase in major cases is a real phenomenon. Operative status categorization as elective versus nonelective procedures was extrapolated from admission type, as degree of urgency of procedure, per se, is not available in the NIS. Additionally, the data are limited to the index hospitalization without capability to identify subsequent admissions or other longitudinal parameters such as neoadjuvant cancer treatment. Last, the design of this study prevents the ability to provide a direct comparator such as a group of CF patients forgoing surgery with similar pathology or non-CF patients undergoing surgery other than segmental colectomy. This limits our ability to draw precise conclusions regarding the relative incidence of adverse events.
Yet, this largest study of adult CF patients undergoing GI surgery provides a novel approach to the assessment of outcomes of a large population of adult CF patients over an extended period of time. These data suggest that appendectomy and cholecystectomy may be performed with a safety profile relatively comparable to the general population, albeit with high rates of pulmonary complications. However, when looking at major abdominal surgeries, morbidity and mortality appear increased relative to traditional risk adjustment, such as age and CCI score. As CF patients are living longer and undergoing GI operations associated with advancing age, this study provides critical insight into the risks of surgery for this unique population. This is all the more important, as the risk of colorectal cancer in adult patients with CF is 5 to10 × greater compared to the general population, with an age at presentation 20 to 30 years younger than the general population.26–28 In our cohort, more than half of CF patients operated for colorectal cancer were younger than 50 years. Consensus recommendations from the Cystic Fibrosis Colorectal Cancer Screening Task Force reflect these risks, with CF patients advised to initiate screening colonoscopy earlier and more frequently than average risk individuals.8
CONCLUSIONS
Patients with CF are living longer, and their need for GI surgery is increasing, as evident by our study showing an increase in major GI operations over time. Although minor surgeries such as cholecystectomy and appendectomy show a safety profile relatively similar to the general population, patients undergoing major GI surgery have a high risk of postoperative complications, nonhome disposition, and mortality. These data have implications for discussion of treatment options and surgical consent for adult CF patients and their families. Future directions to expand on these data may include a multicenter surgical registry of adult CF patients, with granular clinical data aimed at enriching our understanding of the clinical course after surgery, including posthospital adverse events.
Supplementary Material
Footnotes
Supplemental digital content is available for this article. Direct URL citations appear in the printed text, and links to the digital files are provided in the HTML and PDF versions of this article on the journal’s website (www.dcrjournal.com).
Funding/Support: None reported.
Financial Disclosures: Dr Gaertner is an advisory board member for Coloplast and was provided travel expenses for course attendance (Intuitive Surgical). Dr Curran was provided travel expenses for course attendance (Intuitive Surgical).
ePoster presented at the virtual meeting of the American Society of Colon and Rectal Surgeons, June 2020.
REFERENCES
- 1.Centers for Disease Control. Facts About Cystic Fibrosis. Available at: https://www.cdc.gov/scienceambassador/documents/cystic-fibrosis-fact-sheet.pdf November 1995. Accessed August 8, 2020.
- 2.Singh VK, Schwarzenberg SJ. Pancreatic insufficiency in cystic fibrosis. J Cyst Fibros. 2017;16(Suppl 2):S70–S78. [DOI] [PubMed] [Google Scholar]
- 3.Sathe M, Houwen R. Meconium ileus in cystic fibrosis. J Cyst Fibros. 2017;16 Suppl 2:S32–S39. [DOI] [PubMed] [Google Scholar]
- 4.Abraham JM, Taylor CJ. Cystic fibrosis & disorders of the large intestine: DIOS, constipation, and colorectal cancer. J Cyst Fibros. 2017;16 Suppl 2:S40–S49. [DOI] [PubMed] [Google Scholar]
- 5.Lopes-Pacheco M. CFTR modulators: the changing face of cystic fibrosis in the era of precision medicine. Front Pharmacol. 2019;10:1662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Foundation CF. (2018) Annual Data Report: 2017 Patient Registry. Available at: https://www.cff.org/Research/Researcher-Resources/Patient-Registry/2017-Patient-Registry-Annual-Data-Report.pdf. Accessed August 8, 2020.
- 7.Sabharwal S. Gastrointestinal manifestations of cystic fibrosis. Gastroenterol Hepatol (N Y). 2016;12:43–47. [PMC free article] [PubMed] [Google Scholar]
- 8.Hadjiliadis D, Khoruts A, Zauber AG, Hempstead SE, Maisonneuve P, Lowenfels AB; Cystic Fibrosis Colorectal Cancer Screening Task Force. Cystic fibrosis colorectal cancer screening consensus recommendations. Gastroenterology. 2018;154:736–745.e14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Alattar Z, Thornley C, Behbahaninia M, Sisley A. Proximal small bowel obstruction in a patient with cystic fibrosis: a case report. Surg Case Rep. 2019;5:143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40:373–383. [DOI] [PubMed] [Google Scholar]
- 11.Vuik FE, Nieuwenburg SA, Bardou M, et al. Increasing incidence of colorectal cancer in young adults in Europe over the last 25 years. Gut. 2019;68:1820–1826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sharma A, Morton A, Peckham D, Jayne D. Gastrointestinal surgery in adult patients with cystic fibrosis. Frontline Gastroenterol. 2012;3:242–247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cogliandolo A, Patania M, Currò G, Chillè G, Magazzù G, Navarra G. Postoperative outcomes and quality of life in patients with cystic fibrosis undergoing laparoscopic cholecystectomy: a retrospective study. Surg Laparosc Endosc Percutan Tech. 2011;21:179–183. [DOI] [PubMed] [Google Scholar]
- 14.Dolan JP, Diggs BS, Sheppard BC, Hunter JG. The national mortality burden and significant factors associated with open and laparoscopic cholecystectomy: 1997-2006. J Gastrointest Surg. 2009;13:2292–2301. [DOI] [PubMed] [Google Scholar]
- 15.Masoomi H, Nguyen NT, Dolich MO, Mills S, Carmichael JC, Stamos MJ. Laparoscopic appendectomy trends and outcomes in the United States: data from the Nationwide Inpatient Sample (NIS), 2004-2011. Am Surg. 2014;80:1074–1077. [PubMed] [Google Scholar]
- 16.Vons C, Barry C, Maitre S, et al. Amoxicillin plus clavulanic acid versus appendicectomy for treatment of acute uncomplicated appendicitis: an open-label, non-inferiority, randomised controlled trial. Lancet. 2011;377:1573–1579. [DOI] [PubMed] [Google Scholar]
- 17.Hansson J, Körner U, Khorram-Manesh A, Solberg A, Lundholm K. Randomized clinical trial of antibiotic therapy versus appendicectomy as primary treatment of acute appendicitis in unselected patients. Br J Surg. 2009;96:473–481. [DOI] [PubMed] [Google Scholar]
- 18.Eriksson S, Granström L. Randomized controlled trial of appendicectomy versus antibiotic therapy for acute appendicitis. Br J Surg. 1995;82:166–169. [DOI] [PubMed] [Google Scholar]
- 19.Styrud J, Eriksson S, Nilsson I, et al. Appendectomy versus antibiotic treatment in acute appendicitis. a prospective multicenter randomized controlled trial. World J Surg. 2006;30:1033–1037. [DOI] [PubMed] [Google Scholar]
- 20.Green J, Gilchrist FJ, Carroll W. Interventions for preventing distal intestinal obstruction syndrome (DIOS) in cystic fibrosis. Cochrane Database Syst Rev. 2018;6:CD012619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Somaraju URR, Solis-Moya A. Pancreatic enzyme replacement therapy for people with cystic fibrosis. Cochrane Database Syst Rev. 2020;8:CD008227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Cohen ME, Bilimoria KY, Ko CY, Hall BL. Development of an American College of Surgeons National Surgery Quality Improvement Program: morbidity and mortality risk calculator for colorectal surgery. J Am Coll Surg. 2009;208:1009–1016. [DOI] [PubMed] [Google Scholar]
- 23.Peterson CY, Palazzi K, Parsons JK, Chang DC, Ramamoorthy SL. The prevalence of laparoscopy and patient safety outcomes: an analysis of colorectal resections. Surg Endosc. 2014;28:608–616. [DOI] [PubMed] [Google Scholar]
- 24.Gohil SK, Cao C, Phelan M, et al. Impact of policies on the rise in sepsis incidence, 2000-2010. Clin Infect Dis. 2016;62:695–703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Nimptsch U. Disease-specific trends of comorbidity coding and implications for risk adjustment in hospital administrative data. Health Serv Res. 2016;51:981–1001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Nast D, Paniagua C, Anderson P. Cystic fibrosis: a clinician’s tool for management of care advancing into the adult population. J Am Acad Nurse Pract. 2012;24:625–632. [DOI] [PubMed] [Google Scholar]
- 27.Maisonneuve P, Marshall BC, Knapp EA, Lowenfels AB. Cancer risk in cystic fibrosis: a 20-year nationwide study from the United States. J Natl Cancer Inst. 2013;105:122–129. [DOI] [PubMed] [Google Scholar]
- 28.Maisonneuve P, FitzSimmons SC, Neglia JP, Campbell PW, III, Lowenfels AB. Cancer risk in nontransplanted and transplanted cystic fibrosis patients: a 10-year study. J Natl Cancer Inst. 2003;95:381–387. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.