Abstract
A 77-year-old-man presents with chorea, parasomnias, dysarthria and dysphagia, and cognitive issues. A broad workup reveals positive anti-IgLON5 antibody. This case report represents a textbook example of anti-IgLON5 syndrome.
Section 1
A 77-year-old man with a history of hypertension, hyperlipidemia, obstructive sleep apnea (diagnosed about 10 years prior), and prior alcohol use disorder presented with multiple progressive neurologic complaints, including dysphagia, frequent falls, sleep changes, worsened cognition, and new, involuntary movements. His symptoms began about 3 years prior with a slow decline in his memory and cognition: he initially forgot items such as passwords, later progressing to difficulty with finances. In the preceding 6 months, his cognition acutely worsened, to the point that he had recently driven in the wrong direction on a familiar road for several hours. Over the same time course, he developed progressive difficulty swallowing, slurred speech, and imbalance, resulting in frequent falls and unintentional 27 kg weight loss. He reported new sleep disturbances, including flailing his arms while sleeping, sleepwalking, and falling asleep at random during the day. In the preceding month, he developed auditory and visual hallucinations. Finally, in the 2 weeks before presentation, he experienced new, recurrent, intermittent, involuntary jerking movements of the axial musculature.
His examination was notable for mildly impaired attention and recall, with preserved concrete reasoning. At one point during the interview, he fell asleep but was quickly arousable. He had prominent dysarthria affecting primarily guttural consonants. When testing horizontal saccades, he had overshoot dysmetria and required 3–4 beats to fixate on an object. Although he had difficulty initiating vertical gaze, he could fully elevate and depress his eyes. He had adventitious and choreatic movements of both the lower face and neck and spontaneous and synchronous myoclonus of the axial and proximal upper limbs bilaterally, occasionally associated with guttural sounds (Video 1). Vibratory sensation was mildly reduced in the bilateral lower extremities. His strolling gait was normal and narrow based, but he turned en bloc and could not walk on his toes or perform tandem. He had postural instability on retropulsion and a positive Romberg. There was no tremor, rigidity, bradykinesia, or increased tone. There were no fasciculations. His reflexes are 2+ throughout (except at the ankles, where they are absent); there was no clonus, and his plantar response was flexor bilaterally. He did not have any appendicular dysmetria. He was not actively responding to internal stimuli suggestive of active hallucinations, and the remainder of his general examination was unremarkable.
Patient movements and sounds.Download Supplementary Video 1 (6MB, mp4) via http://dx.doi.org/10.1212/200705_Video_1
Questions for Consideration:
Where would you localize the lesion(s)?
What are the differential diagnoses?
Section 2
This patient presents with multiple neurologic issues and a likely multifocal localization. His cognitive problems appear to affect memory, suggesting primarily hippocampal involvement. The hyperkinetic movements can be classified into chorea and axial/proximal myoclonus, indicating involvement of the neostriatum and thalamus/cerebellum, or their outflow tracts, respectively. The presence of hallucinations along with the postural instability and falling suggests the involvement of dopaminergic pathways. His bulbar symptoms indicate brainstem involvement, possibly the nucleus ambiguus given the prominent guttural components and dysphagia. The localization of the sleep disorders may include these brainstem structures or extend to the hypothalamus.
The differential diagnosis includes neurodegenerative processes such as primary movement disorders and dementias as well as inflammatory/immune-mediated processes and toxic-metabolic causes. Atypical parkinsonian syndromes are unlikely because of the absence of bradykinesia, tremor, and rigidity, or supranuclear gaze palsy (progressive supranuclear palsy), frank dysautonomia (multiple system atrophy), or striking asymmetric dystonia or apraxia (corticobasal syndrome).1 An atypical presentation of Huntington disease, or other degenerative forms of chorea, is possible, although the patient does not report any family history for similar conditions. Prion disease can present with a combination of cognitive decline, myoclonus, chorea, and gait difficulties, but the clinical course seems to be too slow for this diagnosis. Cognitive impairment, sleep disorders, and bulbar signs of dysarthria and dysphagia can be seen in frontotemporal dementia with motor neuron disease (FTD-MND), although the hyperkinetic movements would be atypical. The history of alcohol abuse raises the specter of nutritional deficiencies, particularly in conjunction with the positive Romberg and reduced vibratory sense on examination, although no deficiency would be likely to cause the patient's current syndrome. Given this, an immune-mediated process remains possible.
Question for Consideration:
What investigations can provide a diagnosis?
Section 3
Given the patient's history of alcohol abuse, initial laboratory studies focused on nutritional deficiencies as well as other toxic-metabolic causes. These included levels of thiamine, B12, folate, and thyroid-stimulating hormone, as well as antitreponemal and HIV antibodies, which were all unremarkable, except for B12, which was low at 245 pg/mL. However, the patient's symptoms did not improve with repletion of B12. To screen for neurodegenerative causes, an MRI of the brain was ordered but was unremarkable. Specifically, there was no atrophy of the caudate or midbrain, cortical ribboning, or T2 hyperintensity of the corticospinal tracts. Given the patient's waxing and waning level of consciousness during initial interview as well as a history of parasomnias, EEG and polysomnography were obtained. Continuous EEG demonstrated mild encephalopathy, without epileptiform discharges or seizures. Polysomnogram demonstrated both obstructive and central sleep apnea, without stridor, REM, or NREM parasomnias. Investigations then turned to inflammatory/autoimmune causes, including paraneoplastic syndromes, given the patient's age. The erythrocyte sedimentation rate and C-reactive protein were elevated (36 mm/hr and 111.6 mg/L, respectively). CT of the chest, abdomen, and pelvis demonstrated no signs of malignancy. As there was now some evidence of inflammation, but no clear etiology, CSF sampling was pursued to evaluate for autoimmune causes, and antibody panels were sent in both the serum and CSF. Lumbar puncture showed 5 white blood cells (96% lymphocytes), 0 red blood cells, glucose of 70 mg/dL, protein of 57 mg/dL, negative real-time quaking-induced conversion (RT-QuIC) and 14.3.3, and a positive anti-IgLON5 antibody at a 1:16 titer (normal <1:2). A serum paraneoplastic antibody panel was initially negative, as the standard panel did not include anti-IgLON5; however, subsequent specific testing of the serum for anti-IgLON5 revealed a positive titer at 1:480 (normal <1:240).
In the case of this patient, a trial of plasma exchange, followed by IV and oral steroids, and then azathioprine, did not result in any meaningful change in his disease progression. After an extensive discussion with family regarding his goals of care, he was transitioned to hospice care and died about 5 months after his diagnosis of anti-IgLON5 disease. An autopsy was not performed.
Discussion
Anti-IgLON5 disease is a newly described neurologic disorder, with features in cognitive, movement, and neuroinflammatory domains. It is characterized by antibodies that target the immunoglobulin-like cell adhesion molecule IgLON5. Anti-IgLON5 antibodies cause an irreversible antibody-mediated internalization of surface IgLON5. The exact pathogenesis of this disorder is still under debate, and it is overall unclear whether this is a primary neurodegenerative tauopathy resulting in a secondary immune response or a primary autoimmune disorder resulting in neurodegeneration. There is a strong association with human leukocyte antigen (HLA) DRB1*10:01 and HLA-DQB1*05:01 alleles, further pointing to the complex interaction between neuroimmunology and neurodegeneration.2,3 Pathologic examination typically reveals neuronal loss and tau accumulation in the tegmental brainstem nuclei and hypothalamus, likely explaining its neurodegenerative features. However, diagnosis of anti-IgLON5 disease without associated brainstem tau deposition has been described.4,5
Symptoms of anti-IgLON5 disease are typically insidious in onset, taking up to 2.5 years for a diagnosis. However, they can occasionally occur rapidly (over less than 4 months) in almost a quarter of patients.3 Clinical manifestations are heterogeneous and include bulbar symptoms (dysphagia, dysarthria, and respiratory failure), sleep disorders (sleep apnea, REM, and non-REM parasomnias), gait instability, movement disorders (chorea, myoclonus, and Parkinsonism), cognitive dysfunction, and dysautonomia.3,6 Some patients have a PSP-like phenotype with gaze palsies (predominantly vertical) and postural instability, although the lack of the former in our patient makes this phenotype less likely in this case.7 Diagnostic evaluation should include a serum test for the anti-IgLON5 antibody. CSF may also show a positive anti-IgLON5 antibody and a nonspecific mild elevation in protein. MRI and EEG are otherwise relatively unremarkable. Anti-IgLON5 disease is not commonly associated with malignancy or other autoimmune disorders.8
Although there are no prospective treatment trials in this disease, several immunomodulatory therapies have been used in case reports, including steroids, IV immune globulin, plasmapheresis, rituximab, cyclophosphamide, azathioprine, mycophenolate, and the CD52 monoclonal antibody alemtuzumab.9
In one systematic review, 43.4% of patients with anti-IgLON5 disease responded to immunotherapy, with the highest rates of response seen in those treated with azathioprine, mycophenolate, alemtuzumab, and plasmapheresis.9 Additional factors associated with an improved response rate include combination therapy as well as specific clinical phenotypes, including those with predominantly cognitive impairment and those with sleep disorders.10 Movement disorders seen in anti-IgLON5 patients have a poorer response to immunotherapy, with only 13% of patients experiencing significant and sustained improvement.7
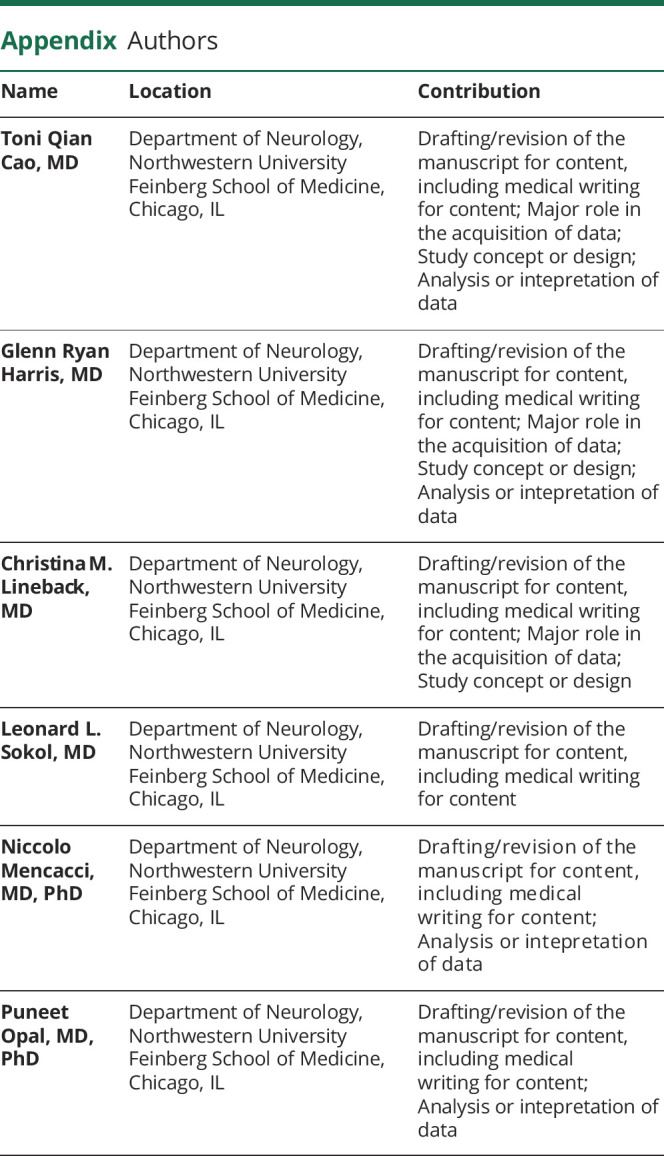
Appendix. Authors
Study Funding
No targeted funding reported.
Disclosure
T. Cao, G. Harris, and C. Lineback report no relevant disclosures. L. Sokol is an ad hoc consultant for Tikvah for Parkinson and ad hoc consultant for the American Film Institute on end-of-life care/palliative care and receives financial support from the Northwestern PSTP Program in Neurology, the MSK R25 NCI 2R25CA190169, and the Huntington's Disease Society of America Center of Excellence (Grant ID: SP0070054). N. Mencacci reports no relevant disclosures. P. Opal receives support from the NIH (1R01NS082351). He has also received funding from the following sources for clinical trials: Biohaven Pharmaceuticals, NIH U01NS104326 (site PI), and the National Ataxia Foundation (CRC-SCA natural history study), as well as royalties from UpToDate. Go to Neurology.org/N for full disclosures.
References
- 1.Postuma RB, Berg D, Stern M, et al. . MDS clinical diagnostic criteria for Parkinson's disease. Mov Disord. 2015;30(12):1591-1601. [DOI] [PubMed] [Google Scholar]
- 2.Dale RC, Ramanathan S. Cell surface antibody-associated neurodegeneration: the case of anti-IgLON5 antibodies. Neurology. 2017;88(18):1688-1690. [DOI] [PubMed] [Google Scholar]
- 3.Gaig C, Graus F, Compta Y, et al. . Clinical manifestations of the anti-IgLON5 disease. Neurology. 2017;88(18):1736-1743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gelpi E, Höftberger R, Graus F, et al. . Neuropathological criteria of anti-IgLON5-related tauopathy. Acta Neuropathol. 2016;132(4):531-543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Erro ME, Sabater L, Martínez L, et al. . Anti-IGLON5 disease: a new case without neuropathologic evidence of brainstem tauopathy. Neurol Neuroimmunol Neuroinflamm. 2020;7(2):e651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Honorat JA, Komorowski L, Josephs KA, et al. . IgLON5 antibody: neurological accompaniments and outcomes in 20 patients. Neurol Neuroimmunol Neuroinflamm. 2017;4(5):e385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gaig C, Compta Y, Heidbreder A, et al. . Frequency and characterization of movement disorders in anti-IgLON5 disease. Neurology. 2021;97(14):e1367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gaig C, Compta Y. Neurological profiles beyond the sleep disorder in patients with anti-IgLON5 disease. Curr Opin Neurol. 2019;32(3):493-499. [DOI] [PubMed] [Google Scholar]
- 9.Cabezudo-García P, Mena-Vázquez N, Estivill Torrús G, Serrano-Castro P. Response to immunotherapy in anti-IgLON5 disease: a systematic review. Acta Neurol Scand. 2020;141(4):263-270. [DOI] [PubMed] [Google Scholar]
- 10.Brunetti V, Della Marca G, Spagni G, Iorio R. Immunotherapy improves sleep and cognitive impairment in anti-IgLON5 encephalopathy. Neurol Neuroimmunol Neuroinflamm. 2019;6(4):e577. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Patient movements and sounds.Download Supplementary Video 1 (6MB, mp4) via http://dx.doi.org/10.1212/200705_Video_1


