Summary
Low- and middle-income countries (LMICs) across the Pacific region have been severely impacted by the COVID-19 pandemic, and emergency care (EC) clinicians have been on the frontline of response efforts. Their responsibilities have extended from triage and clinical management of patients with COVID-19 to health system leadership and coordination. This has exposed EC clinicians to a range of ethical and operational challenges.
This paper describes the context and methodology of a rapid, collaborative, qualitative research project that explored the experiences of EC clinicians in Pacific LMICs during the COVID-19 pandemic. The study was conducted in three phases, with data obtained from online regional EC support forums, key informant interviews and focus group discussions. A phenomenological approach was adopted, incorporating a hybrid inductive and deductive thematic analysis. Research findings, reported in other manuscripts in this collection, will inform multi-sectoral efforts to improve health system preparedness for future public health emergencies.
Funding
Epidemic Ethics/World Health Organization (WHO) initiative, supported by Foreign, Commonwealth and Development Office/Wellcome Grant 214711/Z/18/Z (Phases 1 and 2A) and an Australasian College for Emergency Medicine Foundation International Development Fund Grant.
Keywords: COVID-19, Pandemic, Emergency care, Pacific, Ethics, Qualitative research, Lessons learnt
Background
COVID-19 and the pacific region
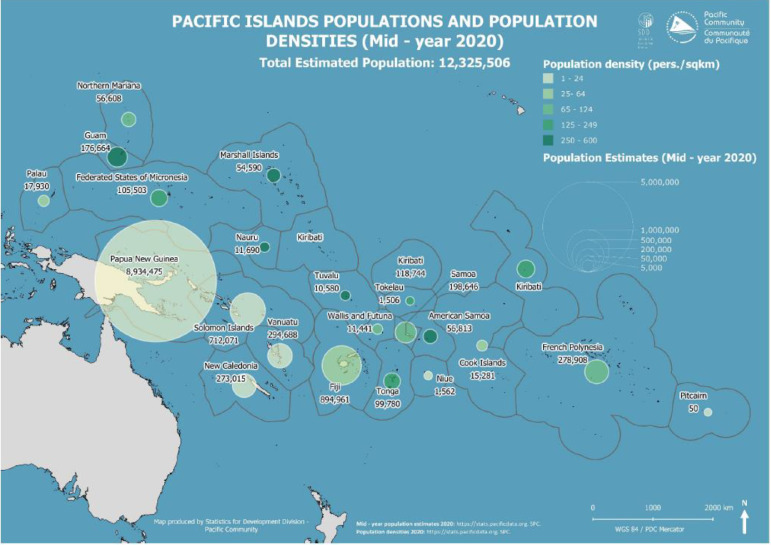
The Pacific is home to over 12 million people, spread across more than 25,000 islands and approximately one third of the Earth's surface area.1,2 The region is predominantly comprised of low- and middle-income countries (LMICs), which vary significantly in population size, demographics and geography (Figure 1).1 A majority of Pacific Island Countries and Territories (PICTs) score below the average preparedness level on the Global Health Security Index, suggesting limited capacity to detect and respond to public health emergencies.3
Figure 1.
Pacific Island country and territory populations and population densities.
Source: pacific community.1
Despite geopolitical diversity, PICTs share common strengths and challenges arising from sociocultural and language links, colonisation experiences and extreme vulnerability to environmental, climate and mass disaster events.4, 5, 6 Increasingly, Pacific stakeholders desire collaboration and resource sharing to aid effective regional responses to global health challenges.2,7, 8, 9, 10
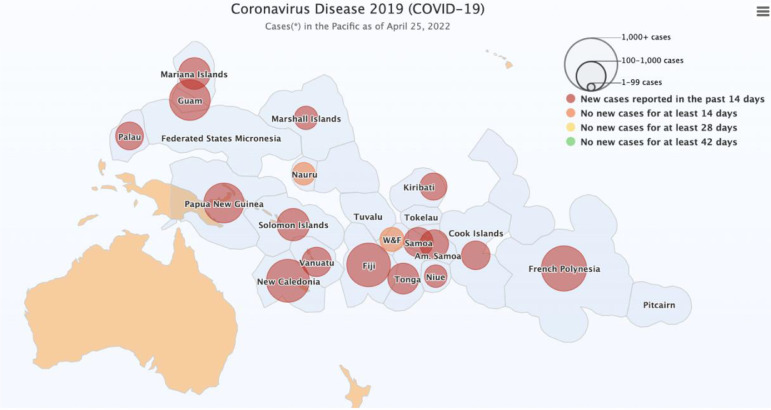
SARS-CoV-2 is a novel form of coronavirus that causes the acute respiratory disease COVID-19. Since the declaration of a global pandemic in March 2020, COVID-19 has spread to the majority of PICTs.11 Figure 2 details the total number of cases reported by the Pacific Community, formerly the Secretariat of the Pacific Community (SPC), as of 25th April 2022. Few PICTs remain case-free or have reported no community transmission, despite the success of many Pacific Small Island States in maintaining a ‘COVID zero-tolerance’ approach for the first 18 months of the pandemic.11 Owing to differences in population demographics, governance systems and health sector capacity between countries,2 the experience of COVID-19 across the Pacific has been highly variable. The unfolding nature of the pandemic means that its full impact is yet to be realised.
Figure 2.
COVID-19 case numbers as of 25th April 2022.
Source: pacific community.11
Despite the significant health, social and economic challenges posed by COVID-19, the global community has much to learn from the responses of Pacific LMICs. Innovative and successful approaches by several countries provide valuable lessons of relevance to both high- and low-resource contexts.12, 13, 14
Emergency care systems and public health emergencies
Emergency care (EC) is an integrated platform for delivering quality, accessible and time-sensitive healthcare services for acute illness and injury. It is an essential component of the broader health system, and an important tool for achieving universal health coverage and the health-related Sustainable Development Goals (SDGs).15, 16, 17, 18 Strong EC systems are also crucial for achieving the targets of the Sendai Framework for Disaster Risk Reduction.19 Like the SDG 2030 agenda, the Sendai Framework informs resilient development strategies, which are highly relevant to the Pacific context.20
In many LMICs, EC systems are underdeveloped, contributing to compromised population health outcomes and excess morbidity and mortality for both communicable and non-communicable diseases.15, 16, 17, 18 Effective EC systems incorporate pre-hospital and facility-based care, and intersect with other components of the health sector.15, 16, 17 Across the Pacific region, significant gaps in EC capacity have been reported, as well as poor integration of EC with public health emergency and disaster response plans.21
COVID-19 has had a major impact on EC systems across the globe.22 It has disrupted usual functioning, and placed significant pressure on ambulance services, emergency departments (EDs) and critical care units. A major challenge has been maintaining ‘business as usual’ while simultaneously meeting infection prevention and control (IPC) requirements and providing effective care for patients with confirmed COVID-19.23, 24, 25, 26 Fluctuating demand for EC, including extreme peaks and troughs, and delays in resource procurement have further compounded these issues.22,25, 26, 27, 28, 29
Crucially, the pandemic has reinforced the intrinsic link between routine EC and disaster preparedness and resilience, and emphasised the importance of effective triage, surveillance and clinical care at the point of entry into healthcare facilities.14,22,23,26,28,30, 31, 32 It has also illustrated how surge events can stress health systems, even those that are more mature and well-resourced.12,14,33 Together, these observations highlight a global need for robust EC systems that are resilient and responsive to public health emergencies.
The emergency care workforce and COVID-19
Among the essential building blocks underpinning health systems, human resources are critical.34 EC clinicians are frontline providers for routine care, but are also expected to lead preparation, response and recovery efforts during surge events and public health emergencies. Throughout the pandemic, EC clinicians have played important roles in risk-stratifying patients, providing initial therapy, establishing goals of care, and identifying patients who may benefit from advanced interventions.13,30 In some settings, they have also been called upon to lead hospital-wide emergency operations and coordinate public health response efforts including national and sub-national policy and planning.13,30
In many LMICs, the number of healthcare workers (HCWs) with specific training in EC is extremely limited.35 This is particularly the case in the Pacific region.21 Consequently, EC systems in resource-limited settings often rely on a small workforce that is highly committed but uniquely threatened by employment instability and clinical workload challenges. Commonly, EC leaders in LMICs work in professional isolation with poor access to support networks and ongoing training. Burnout is a risk for all EC clinicians, but the probability of experiencing stress and fatigue is exacerbated when resources are limited.36 A lack of redundancy in the EC workforce, and a reliance on a small number of clinician leaders, is a reality for many PICTs.37
Challenges for emergency care clinicians responding to the pandemic
The pandemic has compounded the challenges faced by EC clinicians, and placed them at significant risk of virus exposure, illness and death.13,33 Stigma associated with COVID-19 contact has also emerged as a major issue for LMIC HCWs.13,30 Although data are limited, there is early evidence of psychological harm and moral injury associated with the delivery of frontline care, especially in settings where resources are limited.25,38 The net result of these effects has been to further impair the EC workforce.30
COVID-19 has also exposed a range of ethical, operational, health and wellbeing issues for EC clinicians.13,30,31,39 These include the tension between a HCW's right to safety – for instance, through an adequate supply of personal protective equipment (PPE) and appropriate occupational health and safety policies – and the responsibility to provide care, particularly in the setting of a surge event. Other issues include challenges in resource allocation, especially where facilities have limited capacity for advanced interventions such as intubation and ventilation; disconnect between donor priorities (including advanced medical technology, such as ventilators) and locally-identified needs (such as PPE and equipment to facilitate basic EC); and barriers to effective care for patient groups that are culturally and socio-economically disenfranchised yet disproportionately affected by public health emergencies. The gendered impact of the pandemic, including the multiple responsibilities of women as HCWs and care providers within their own families, has also impacted the EC workforce.13,30,33,40 These issues have played out in many LMICs, where a focus on essential rather than resource-intensive care has been advocated.28,32
Some of these challenges are consistent with the ethical and operational tensions identified in previous public health emergencies.39,41, 42, 43 While the concepts may not be unique to COVID-19, the extent of the current pandemic is unprecedented.33 A concerted effort is therefore required to address these issues, with the aim of strengthening surge response capacity and minimising moral distress among EC clinicians (among many other important overlapping factors).
Learning from the lived experience of emergency care clinicians
Research is limited on how best to adapt the COVID-19 pandemic response to resource-limited settings and values, particularly for the EC workforce, and especially in the Pacific region. Although guidance has been generated for HCW protection and the allocation of scarce resources during public health emergencies, it is not easily translated to the LMIC context.41, 42, 43, 44, 45, 46, 47, 48, 49, 50 In turn, there may be lessons for all countries from the adaptive, innovative and pragmatic responses to COVID-19 implemented in LMICs, especially in relation to the ethical and operational challenges faced by frontline clinicians.13
In response to these knowledge gaps, we initiated a rapid, prospective, qualitative research project to explore the experiences of EC clinicians and other key stakeholders in Pacific LMICs responding to the pandemic. Our study aimed to capture the rich and diverse voices of EC clinicians in the Pacific region, and to document lessons learned to inform recommendations to improve health system preparedness for future public health emergencies. To the best of our knowledge, our research is the most in-depth qualitative study bringing to light the voice and lived experience of EC clinicians in the Pacific region as they respond to the contemporaneous COVID-19 crisis.
This article summarises the context, research methods and potential implications of the project. Subsequent papers will present study results, and explore key themes identified from analysis of the data.
Methods
Context
The geopolitical and sociocultural context for this research is described above. Many PICTs are remote, island nations, with a small and fluid health workforce, limited health infrastructure and fragile EC systems.21 Although several PICTs have achieved rapid disease control through border closures, geographic isolation has created novel challenges for clinical and public health responses.13
The Australasian College for Emergency Medicine (ACEM), the peak body for emergency medicine in Australia and Aotearoa New Zealand, and SPC, an intergovernmental organisation mandated with providing technical, scientific and development functions for its Pacific member states and territories,9 together identified an urgent need to examine the PICT experience in detail. This research was facilitated by an existing partnership and Memorandum of Understanding between the two organisations.
Study design
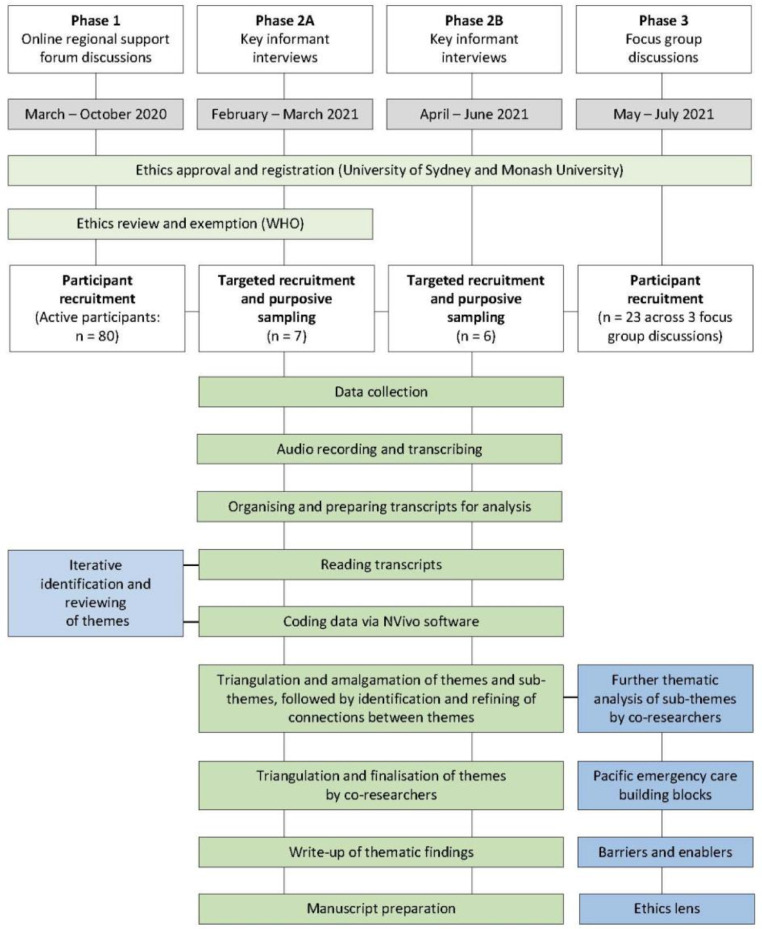
The study was conducted as a collaboration between Australian and PICT researchers affiliated with ACEM and SPC, and employed rapid, prospective, qualitative research methods. Data were gathered from EC clinicians and other relevant stakeholders across Pacific LMICs in three phases: via online regional EC support forums (Phase 1), in-depth interviews with key informants (Phase 2) and focus group discussions (Phase 3).
The research utilised a phenomenological methodological approach, aiming to explore the lived experience of participants from their perspective.51,52 We deliberately used strengths-based, appreciative inquiry53 as a fundamental underpinning of our qualitative data collection, in order to counter the ubiquitous deficit narrative that commonly accompanies research about LMICs.54 As data collection occurred over a seventeen-month period, we incorporated components of participatory action-research,55 with the dual aim of catalysing change (primarily actions to improve and enhance local COVID-19 responses), and increasing understanding in researchers and participants about the nature and effects of the pandemic response in their own contexts. In keeping with our methodological approach, PICT participant researchers elevated their leadership role as data collectors, analysers and regional collaborators during the research project, aiming for ‘Pacific teaching Pacific’ on all COVID-19 response matters. Additionally, through forum, interview and focus group discussions, regional participants strengthened their strategic insights and local pandemic responses, stimulated by the co-learning and research process that enabled sharing of PICT experiences. These techniques were implemented to ensure a strong clinician voice in the research findings and ensure coverage of the full spectrum of ethical and operational issues encountered by EC clinicians.
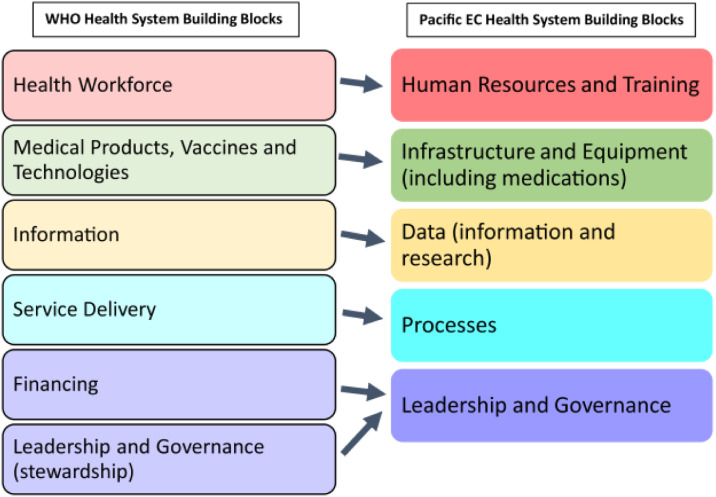
Data collection and analysis methods (described below) were informed by the World Health Organization (WHO) health system building blocks, as adapted for the Pacific EC context (Figure 3).21 These building blocks reflect the importance of human resources (such as trained clinicians), infrastructure (such as IPC-compliant resuscitation areas) and processes (such as triage) to effective EC, and have been endorsed through regional consensus involving clinicians across multiple PICTs.21
Figure 3.
WHO health system building blocks, adapted for the Pacific context.
Source: Phillips et al 2020.21
Researcher characteristics and reflexivity
The research was led by ACEM in collaboration with SPC and key regional stakeholders. ACEM is the not-for-profit organisation responsible for training emergency physicians and advancing professional standards in emergency medicine across Australia and Aotearoa New Zealand. ACEM's Global Emergency Care Committee (GECCo), Global Emergency Care (GEC) Desk and GEC Network aim to improve the capacity of LMICs to deliver safe and effective EC, with a focus on the Pacific region. As the COVID-19 crisis surged in 2020, ACEM pivoted its GEC activities towards technical assistance and support for EC clinicians responding to the pandemic.56 This included the development of COVID-19 EC response guidance specifically tailored to the Pacific context.31,57
SPC is the principal scientific, technical and development organisation in the Pacific region, owned and governed by 26 country and territory members.9 Within SPC's Public Health Division, a Clinical Services Program aims to work collaboratively across the region and with global partners to improve clinical care and service delivery through health workforce strengthening, Pacific-focused research and enhanced regional health governance.
The research team for this study comprised EC clinicians from Australia and PICTs, along with qualitative researchers and development practitioners with experience in Pacific health systems. Team members were actively engaged in all aspects and phases of the research, including data collection through online support forums, interviews and focus groups. In facilitating these sessions, researchers drew on their Pacific context expertise, professional collegial networks, and personal experience as clinicians and care providers during the COVID-19 pandemic. To ensure research rigour and reflexivity, researchers articulated and documented assumptions and biases at the project development stage, throughout data collection, analysis and interpretation, and during research team meetings and discussion.
The presence of strong Pacific regional representation in the research team, as well as involvement in the collection, analysis and interpretation of data, increased the validity, credibility and acceptability of our project for participants. It also addressed issues of respect, reciprocity and research collaboration in the region.58 Funders had no role in study design, results analysis or manuscript preparation.
Sampling, recruitment and participants
Phase one
As the COVID-19 situation escalated across the globe in early 2020, ACEM rapidly convened online support forums for EC clinicians.56 These were facilitated using the video communication platform Zoom,59 and held fortnightly from March to July 2020 and monthly thereafter. Invitations to participate were widely disseminated to EC clinicians and stakeholders in the Pacific region via ACEM, SPC and Pacific regional WHO contacts and networks. Participants were informed verbally and in writing that the forum was being recorded and that data, including comments in the chat function, would be anonymously used in research. They were also advised of their right to contact the researchers if they did not want their data to be used.
Forum participants included key EC clinicians, other HCWs, EC program managers/coordinators and policymakers, as well as representatives from the WHO Representative Office of the South Pacific and ACEM Fellows with Pacific experience and professional connections with EC colleagues in the region. Participation was open to all interested stakeholders with no exclusion criteria. In total, there were 437 attendances across 13 forums between March and October, with more than 80 individuals from 15 different PICTs actively contributing (providing comments and perspectives) in one or more sessions. This constitutes the sample for phase one of this project.
Phase two
The second phase of data collection used semi-structured, in-depth interviews with 13 informants across the Pacific region, conducted and recorded using Zoom between February and June 2021. Sampling was purposive and opportunistic, using personal ACEM and SPC networks. There was no minimum sample size as the aim was to have representation across disciplines (particularly a combination of emergency medicine physicians and nurse leaders), PICTs and genders.
Interviewees were invited because of their experience leading and/or coordinating EC in a Pacific LMIC during the COVID-19 pandemic. Informants were from Fiji, Kiribati, Palau, Papua New Guinea (PNG), Samoa, Solomon Islands, Timor Leste, Tonga and Vanuatu. All interviewees provided with a detailed participant information sheet and provided written consent prior to interview. To meet WHO ethics requirements, informants for Phase 2A (Figure 4) were asked to respond as an official representative of their employing health service/organisation.
Figure 4.
Data collection, processing and analysis flowchart.
Phase three
Phase three of the study occurred between May and July 2021 and involved data collection via focus group discussions with EC stakeholders from recognised geographical regions of the Pacific: Micronesia (encompassing the Federated States of Micronesia, Kiribati, Marshall Islands, Nauru, Palau and the northern Pacific states), Polynesia (Cook Islands, Samoa, Tokelau, Tonga, Tuvalu and other small island states) and Melanesia (Fiji, PNG, Solomon Islands and Vanuatu, as well as Timor Leste).60 Participants were recruited opportunistically and purposively through ACEM online support forums and ACEM, SPC and regional networks, with a particular focus on engaging women participants, nurses, non-physician HCWs and other clinical and non-clinical stakeholders. Focus group participation was open to all interested stakeholders, without exclusion criteria. Dates and times of scheduled sessions were widely circulated and participants invited to attend sessions focussing on their country or sub-region, but not excluded from other sessions. Participants provided informed consent in verbal (recorded) format. These sessions also were conducted and recorded on the Zoom video conferencing platform. Collected data were de-identified to protect participants’ anonymity.
Data collection, processing and analysis
Data tools and collection
To encourage wide participation in discussion and limit complexity, we adopted a simplified version of the Pacific EC System building block framework to gather data during the Phase 1 online support forums. Following a clinical update, discussion was framed using the four EC components (staff, supplies, systems and space) referenced in ACEM COVID-19 guidance,31 with an emphasis on one component in each session (Appendix 1). Research team members facilitated and encouraged open discussion among participants. High meeting frequency enabled rapid adaptation of each forum theme and regional emphasis, depending on participant needs, new issues arising, or changed pandemic events within countries.
For the Phase 2 interviews, researchers used an interview guide purposefully developed by the research team (Appendix 2). This guide more explicitly adopted the five Pacific EC System building blocks to structure questioning, and also incorporated elements of feminist,61 safety science,61, 62, 63 and medical ethics theoretical frameworks44,49,50 within an ‘enablers and barriers’ structure. As interviews progressed, topic questions were iteratively adapted and refined according to participant responses and feedback, and to improve clarity and understanding. Interviews were conducted by a research assistant and at least one other research team member using a modified conversational technique specific for the Pacific context.64 Informants were offered the opportunity to review the interview transcript and to request removal or amendment of content if there were misunderstandings or they did not agree with the transcription.
A discussion guide was developed for the Phase 3 focus group sessions, incorporating core elements of the Phase 2 interview tool, but with particular emphasis on gender and feminist theoretical framing (Appendix 3). Again, questions were iteratively refined for clarity and understanding during and after focus group sessions. Focus group discussions were facilitated by at least two members of the research team. Because of wide and anonymous participation, participants were not able to review transcripts of discussions, but were advised they could withdraw from the study or request removal of specific comments if required.
Data processing and analysis
Recordings of 13 online support forums (containing over 18 hours of discussion), 12 in-depth interviews (with a duration of approximately 45-90 minutes each) and three focus group discussions were transcribed verbatim by research assistants (LH and OM), and subsequently de-identified. Data were entered into the QSR NVivo data management program.65 Preliminary coding was performed using this platform by one research assistant (LH) and subsequently (independently) by multiple researchers across all components of the data.
A hybrid inductive (data driven)66 and deductive67 thematic analysis approach was used to interpret the collated data and identify themes relevant to the description of the phenomenon.68,69 Deductive codes were determined by the research objectives and analytical frameworks, including the WHO health system building blocks adapted to the Pacific EC context (Figure 3).21 Inductive codes expanded an a priori code or described a new theme.
Codes were integrated and categorised, with preliminary themes identified and agreed upon by the researchers. Due to the volume of data related to each of the five building blocks, and to enhance inter-rater reliability, paired members of the multidisciplinary research team were assigned coded data for a building block and tasked with reviewing key enablers and barriers, identifying sub-themes and highlighting key ethical and operational issues. Each pair presented findings, with exemplifying quotes from the data, to a workshop of the broader research team. Themes were reviewed and verified through discussion, data triangulation and reference to the pre-specified research questions (Figure 4).
Theoretical framing
Given the gendered impact of the pandemic,40 we used feminist theory in our data collection and analysis to ensure our research represented the experience and voices of women at the frontline, and identified gender specific dimensions of the COVID-19 EC response.61 Safety science theoretical approaches also informed the interpretation of HCW, patient and health system safety and risk management issues.62,63 Findings also were developed in relation to the four tenets of ethical decision-making (autonomy, beneficence, non-maleficence and justice), with reference to other ethics frameworks and guidance documents related to the COVID-19 response.44,49,50
All research team members contributed to the development and presentation of findings that will be a focus of subsequent papers. Reporting of study data will adhere to Enhancing the Quality and Transparency of Health Research (EQUATOR)70 and Standards for Reporting Qualitative Research (SRQR) guidelines.71
Ethical issues and approval
Ethics approval was provided by The University of Sydney Human Research Ethics Committee (Reference 2020/480) and registered with Monash University Human Research Ethics Committee (Reference 28325). Research protocols related to Phase 1 and 2A of the research were also reviewed by the World Health Organization's AdHoc COVID-19 Research Ethics Review Committee (Protocol ID CERC.0077) and declared exempt.
As outlined above, the study was specifically designed to explore ethical issues and tensions through the lens of Pacific EC clinicians. For this reason, safeguards were put in place to address the risk that participation in the study exacerbated psychological distress. Our collaborative, reflexive approach to the research offered an effective means of screening for potential harm and providing collegial support. Providing a safe space for experience sharing, reflection and mentorship was one of the original aims of the online forums.56
Discussion
This novel, qualitative study explores the lived experience of EC clinicians in Pacific LMICs responding to the pandemic. It has intentionally emphasised the unique circumstances of PICTs, and used appreciative inquiry, reflexive and action research approaches to present clinician and other important stakeholder voices. In addition to illuminating Pacific experiences and extrapolating key lessons and recommendations for future health surge events, the research process has deliberately empowered PICT participant researchers through the action research methodology to increase their clinical and collaborative regional leadership over time.
Our study findings fill an important knowledge gap, regarding the best means to adapt COVID-19 pandemic response to resource-limited environments, particularly in relation to EC systems. Although a significant amount of technical guidance has been generated during the pandemic, much of it has focussed on high-income settings with advanced public health and clinical care capacity. Given the wide variation in health system responses to COVID-19 across the globe, all countries stand to benefit from structured analysis of the innovative and pragmatic solutions implemented in LMICs.33 Importantly, our study used qualitative inquiry to give voice to frontline clinicians across the Pacific, and learn from their lived experience of responding to the COVID-19 pandemic.
Although there is emerging data regarding the personal and professional implications for HCWs engaged in COVID-19 response,33,38 little has been published regarding the specific experiences of EC clinicians – let alone in the Pacific regional context. EC providers are unique in that they are exposed to a range of ethical and operational challenges that are not experienced in other aspects of the health system. This reflects that EC clinicians are often confronted by undifferentiated patients with acute illness and injury, and are frequently required to make important clinical decisions in the face of incomplete information and limited resources.
Limitations of this study include an underrepresentation of some PICTs, exclusion of the French-speaking Pacific, and a predominance of Australian clinicians among the research team. All data was collected in English, which although the common language of health education and practice in the participating PICTs, may have limited nuance and cultural depth to communication. In order to address potential gender, role and cultural barriers to open participation in group settings, we sought to ensure researchers were matched for gender and Pacific representation (for example; ensuring women researchers led focus groups with largely female nurse participants), and enshrine flexibility and responsiveness when structuring group events. PICT researchers within our team led some data collection, and provided essential guidance on interview / focus group conduct and data interpretation. Over time, the research team established credibility and trustworthiness with PICT participants, potentially mitigating risks of under-participation in data-collection activities. Despite our efforts, these factors may bias the findings and limit the generalisability to certain Pacific LMICs. Additionally, the political, cultural and health system structures in each Pacific country are unique, and there is heterogeneity even within PICTs. Solutions that have been successfully employed in one context may not be applicable in another.
As a result of pandemic travel restrictions, we only collected data using online video formats. Although potentially limiting capture of nuance or culturally distinct communication through participant discomfort or practical connectivity challenges, this method has been found feasible and acceptable for interview data collection.72,73 As with telehealth and telemonitoring,74 video conferencing technology is increasingly familiar to EC clinicians across the globe, and has been widely employed throughout the pandemic to facilitate global emergency care education and research.75
None of our bespoke data collection tools were piloted prior to implementation, primarily due to the real-life constraints of Pacific regional research, where individual stakeholders have multiple competing responsibilities and limited available time. Because our research explored a contemporaneous or unfolding public health emergency event, combined with our team being multidisciplinary and including PICT clinicians, we iteratively developed and refined our research tools internally to reach a standard of acceptability, content validity and relevance satisfying all regional research team members.
A further limitation is the study period, which was concentrated on the initial 17 months of the pandemic. The COVID-19 public health emergency continues to evolve, with new challenges, evidence and technical guidance emerging on a regular basis, now especially including the delivery of COVID-19 vaccination. Despite the dynamic nature of the pandemic, the principles of effective EC and disaster response are relatively static, and the key themes, findings and recommendations are likely to remain relevant to this and future public health emergencies, as well as contribute to lessons and learnings for the sustainable achievement of the Sendai Framework for Disaster Risk Reduction and SDG 2030 agenda in the Pacific regional context.
Notwithstanding these limitations, the research findings and recommendations will help scientifically inform and improve health system preparedness for future public health emergencies. Importantly, the study has also identified factors that will strengthen the capacity of Pacific EC systems to provide quality and sustainable care during routine operations as well as surge events. This knowledge will enhance resilience, reduce preventable morbidity and mortality attributable to inadequate EC access, and improve overall patient and population health outcomes.
Conclusion
LMICs across the Pacific region have been severely impacted by the COVID-19 pandemic, and EC clinicians are on the frontline of the response. EC clinicians’ responsibilities include triage and care of patients with COVID-19, as well as health system leadership and coordination. As a consequence, they are exposed to a range of ethical and operational challenges, amplifying the risk of psychological distress and moral injury.
This rapid, collaborative, qualitative research project has used novel methods to document the experiences of EC clinicians in Pacific LMICs during the COVID-19 pandemic. Study results, published in other papers in this issue [CITATIONS], will inform efforts to improve health system preparedness for future public health emergencies. Importantly, the findings will strengthen EC system capacity to provide timely, quality and accessible care during routine operations as well as surge events.
Appendix 1. Example of invitation and 4S structure used to guide online support forums
Contributors
MC, GP, RM, CEB, GOR and SK were primarily responsible for study design. DS, MK, PP and BK provided regional perspectives and contextual advice throughout all aspects of the project. All authors participated in data collection through online support forums, interviews or focus group discussions. LH, OM and SK were responsible for transcription, with LH undertaking preliminary coding and presentation of data to the broader research team. MC, GP, RM, GOR, CEB, SK, DS and LH contributed to thematic analysis, secondary coding and synthesis, including data triangulation, amalgamation and integration. MC, GP, RM and LH developed the first draft of this manuscript. The final version was reviewed and approved by all authors.
Data sharing statement
Study protocols and de-identified data that underpin these findings may be available (between 9 and 24 months after publication) to investigators whose proposed use of these data has been approved by an independent review committee, and subject to any restrictions imposed by relevant ethics committees, funders, the Australasian College for Emergency Medicine or the Pacific Community. Proposals to use the data may be submitted, and data made available, without investigator support.
Editor note
The Lancet Group takes a neutral position with respect to territorial claims in published maps and institutional affiliations.
Declaration of interests
MC, GP, RM and GOR declare they are recipients of International Development Fund Grants from the Australasian College for Emergency Medicine Foundation. GP reports past research funding from the Pacific Community (SPC) and visiting Faculty status at the University of Papua New Guinea and Fiji National University. Additionally, RM reports grants from the Australian Government Department of Foreign Affairs and Trade as well as scholarships from the National Health and Medical Research Council (NHMRC) and Monash University. GOR reports that he is the recipient of a NHMRC Early Career Research Fellowship. CEB reports past research consultancy funding from SPC.
Acknowledgments
Acknowledgements
The authors would like to acknowledge all EC clinicians and stakeholders across the Pacific who are involved with the COVID-19 pandemic response, especially those who participated in this study. Thanks also to the staff of the Australasian College for Emergency Medicine and the Pacific Community for their support of this project and the emergency care community more broadly. The authors also acknowledge other healthcare workers and public health personnel who have made significant contributions to pandemic responses.
Funding
Phases 1 and 2A of this study were part of an Epidemic Ethics/World Health Organization (WHO) initiative, supported by Foreign, Commonwealth and Development Office/Wellcome Grant 214711/Z/18/Z. Copyright of the original work on which this publication is based belongs to WHO. The authors have been given permission to publish this manuscript. The authors alone are responsible for the views expressed in this publication and they do not necessarily represent the views, decisions or policies of WHO.
Co-funding for this research was received from the Australasian College for Emergency Medicine Foundation via an International Development Fund Grant to Principal Investigator MC. RM is supported by a National Health and Medical Research Council (NHMRC) Postgraduate Scholarship and a Monash Graduate Excellence Scholarship. GOR is supported by a NHMRC Early Career Research Fellowship. CEB is supported by a University of Queensland Development Research Fellowship. None of these funders played any role in study design, results analysis or manuscript preparation.
Footnotes
Supplementary material associated with this article can be found in the online version at doi:10.1016/j.lanwpc.2022.100517.
Appendix. Supplementary materials
Appendix 2. Key informant interview guide
Appendix 3. Focus group discussion guide
References
- 1.Pacific Community. Population estimates and projections. https://sdd.spc.int/topic/population-estimates-and-projections. Accessed 4 June 2021.
- 2.World Health Organization Western Pacific Regional Office . WHO; Geneva, Switzerland, Manila: 2017. Pacific Island Countries and Areas – WHO Cooperation Strategy 2018–2022. [Google Scholar]
- 3.Nuclear Threat Initiative and Johns Hopkins School of Public Health Centre for Health Security . Johns Hopkins Center for Health Security 621 E. Pratt Street Suite 210 Baltimore; MD 21202, Washington DC: 2019. Global Health Security Index: Building Collective Action and Accountability. [Google Scholar]
- 4.McIver L, Woodward A, Hales S, et al. Health impacts of climate change in pacific island countries: a regional assessment of vulnerabilities and adaptation priorities. Environ Health Perspect. 2016;124(11):1707–1714. doi: 10.1289/ehp.1509756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Fritsch K, Zang Y. The Asia pacific emergency and disaster nursing network: promoting the safety and resilience of communities. SE Asia J of Trop Med Pub Health. 2009;40(suppl 1):71–78. [Google Scholar]
- 6.Lee D, Zhang H, Nguyen C. The economic impact of natural disasters in pacific island countries: adaptation and preparedness. IMF Working Papers. 2018;18(108):1. doi: 10.5089/9781484353288.001. [DOI] [Google Scholar]
- 7.Brolan CE, McEwan CA, Hill PS. Australia's overseas development aid commitment to health through the sustainable development goals: a multi-stakeholder perspective. Globalization Health. 2019;15(1):1–19. doi: 10.1186/s12992-019-0507-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Pacific Islands Forum Secretariat; Suva, Fiji: 2014. Pacific Islands Forum Secretariat, Framework for Pacific Regionalism. [Google Scholar]
- 9.Pacific Community. Pacific community. https://www.spc.int/about-us. Accessed 23 October 2020.
- 10.Australian Government Department of Foreign Affairs and Trade. Indo-pacific centre for health security. https://indopacifichealthsecurity.dfat.gov.au. Accessed 17 June 2021.
- 11.Pacific Community. COVID-19: pacific community updates. https://www.spc.int/updates/blog/2021/06/covid-19-pacific-community-updates. Accessed 27 April 2022
- 12.Dalglish SL. COVID-19 gives the lie to global health expertise. Lancet. 2020;395(10231):1189. doi: 10.1016/S0140-6736(20)30739-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Woodruff IG, Mitchell RD, Phillips G, et al. COVID-19 and the Indo–Pacific: implications for resource-limited emergency departments. Med J Aust. 2020;213(8):345–349. doi: 10.5694/mja2.50750. [DOI] [PubMed] [Google Scholar]
- 14.Phillips G, Cox M COVID-19 and emergency care in the pacific. DevPolicy Blog. https://devpolicy.org/covid-19-and-emergency-care-in-the-pacific-20200428/. Published 2020. Accessed 28 April 2020.
- 15.Mitchell R, Phillips G, O'Reilly G, Creaton A, Cameron P. World health assembly resolution 72.16: what are the implications for the Australasian College for Emergency Medicine and emergency care development in the Indo-Pacific? Emerg Med Australas. 2019;31(5):696–699. doi: 10.1111/1742-6723.13373. [DOI] [PubMed] [Google Scholar]
- 16.Reynolds TA, Sawe H, Rubiano AM, et al. In: Disease Control Priorities. Volume 9: Improving Health and Reducing Poverty. 3rd ed. Jamison DT, Gelband H, Horton S, et al., editors. World Bank Group; Washington DC: 2018. Strengthening health systems to provide emergency care. [DOI] [Google Scholar]
- 17.Thind A, Hsia R, Mabweijano J, Hicks ER, Zakariah A, Mock CN. In: Disease Control Priorities. Volume 1: Essential Surgery. 3rd Ed. Debas H, Donkor P, Gawande A, Jamison D, Kruk M, Mock C, editors. The World Bank; Washington DC: 2015. Prehospital and emergency care. [DOI] [Google Scholar]
- 18.Shanahan T, Risko N, Razzak J, Bhutta Z. Aligning emergency care with global health priorities. Int J Emerg Med. 2018;11(1):52. doi: 10.1186/s12245-018-0213-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.United Nations Office for Disaster Risk Reduction . United Nations Office for Disaster Risk Reduction; Geneva, Switzerland: 2015. Sendai Framework for Disaster Risk Reduction 2015 - 2030. [Google Scholar]
- 20.Pacific Community. Framework for Resilient Development in the Pacific: An Integrated Approach to Address Climate Change and Disaster Risk Management [FRDP] 2017–2030. Suva. Pacific Communityhttps://www.resilientpacific.org/en/framework-resilient-development-pacific.
- 21.Phillips G, Creaton A, Airdhill-Enosa P, et al. Emergency care status, priorities and standards for the Pacific region: a multiphase survey and consensus process across 17 different Pacific Island countries and territories. Lancet Reg Health - West Pacific. 2020;1(1) doi: 10.1016/j.lanwpc.2020.100002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Mazurik L, Javidan A, Higginson I, et al. Early lessons from COVID-19 that may reduce future emergency department crowding. Emerg Med Australas. 2020;32(6):1077–1079. doi: 10.1111/1742-6723.13612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Govindasamy LS, Hsiao KH, Foong LH, Judkins S. Planning for the next pandemic: reflections on the early phase of the Australian-COVID-19 public health response from the emergency department. Emerg Med Australas. 2021;33(4):759–761. doi: 10.1111/1742-6723.13799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Staib A, Small N. Emergency medicine’s COVID future: facing the triple challenge after flattening the curve. Emerg Med Australas. 2020;32(5):880–882. doi: 10.1111/1742-6723.13566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Conlon C, McDonnell T, Barrett M, et al. The impact of the COVID-19 pandemic on child health and the provision of care in paediatric emergency departments: a qualitative study of frontline emergency care staff. BMC Health Serv Res. 2021;21(1):279. doi: 10.1186/s12913-021-06284-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Mitchell R, Nou G. A ‘new normal’: harnessing the experience of COVID-19 for sustained improvements in global emergency care. Lancet Reg Health - West Pacific. 2020;1 doi: 10.1016/j.lanwpc.2020.100012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Wyatt S, Mohammed MA, Fisher E, McConkey R, Spilsbury P. Impact of the SARS-CoV-2 pandemic and associated lockdown measures on attendances at emergency departments in English hospitals: a retrospective database study. Lancet Reg Health - Europe. 2021;2 doi: 10.1016/j.lanepe.2021.100034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hopman J, Allegranzi B, Mehtar S. Managing COVID-19 in low- and middle-income countries. JAMA. 2020;323(16):1549–1550. doi: 10.1001/jama.2020.4169. [DOI] [PubMed] [Google Scholar]
- 29.Mitchell RD, O'Reilly GM, Mitra B, Smit DV, Miller J, Cameron PA. Impact of COVID-19 State of Emergency restrictions on presentations to two Victorian emergency departments. Emerg Med Australas. 2020;32(6):1027–1033. doi: 10.1111/1742-6723.13606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Bornstein SL, Elton LG, Kennedy F, et al. Rising to the challenge: the emergency nursing response to COVID-19 in the Pacific. Austr Emergency Care. 2021;24(1):1–3. doi: 10.1016/j.auec.2020.09.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Mitchell R, Banks C. Emergency departments and the COVID-19 pandemic: making the most of limited resources. Emerg Med J. 2020;37(5):258–259. doi: 10.1136/emermed-2020-209660. emermed-2020-209660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Baker T, Schell CO, Petersen DB, et al. Essential care of critical illness must not be forgotten in the COVID-19 pandemic. Lancet. 2020;395(10232):1253–1254. doi: 10.1016/S0140-6736(20)30793-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Independent Panel for Pandemic Preparedness and Response . WHO; Geneva, Switzerland: 2021. COVID-19: Make It the Last Pandemic. [Google Scholar]
- 34.Chen L, Evans T, Anand S, et al. Human resources for health: overcoming the crisis. Lancet. 2004;364(9449):1984–1990. doi: 10.1016/S0140-6736(04)17482-5. [DOI] [PubMed] [Google Scholar]
- 35.Obermeyer Z, Abujaber S, Makar M, et al. Emergency care in 59 low- and middle-income countries: a systematic review. Bull World Health Organ. 2015;93(8):577–586. doi: 10.2471/BLT.14.148338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Sawe HR, Murray B, Jamieson J. Compassion fatigue in emergency providers: experiences from Sub-Saharan Africa. Emerg Med Australas. 2016;28(1):109–111. doi: 10.1111/1742-6723.12536. [DOI] [PubMed] [Google Scholar]
- 37.Phillips G, Lee D, Shailin S, O'Reilly G, Cameron P. The pacific emergency medicine mentoring program: a model for medical mentoring in the Pacific region. Emerg Med Australas. 2019;31(6):1092–1100. doi: 10.1111/1742-6723.13366. [DOI] [PubMed] [Google Scholar]
- 38.Bennett P, Noble S, Johnston S, Jones D, Hunter R. COVID-19 confessions: a qualitative exploration of healthcare workers experiences of working with COVID-19. BMJ Open. 2020;10(12) doi: 10.1136/bmjopen-2020-043949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Markwell A, Mitchell R, Wright A, Brown AF. Clinical and ethical challenges for emergency departments during communicable disease outbreaks: can lessons from Ebola virus disease be applied to the COVID-19 pandemic? Emerg Med Australas. 2020;32(3):520–524. doi: 10.1111/1742-6723.13514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Wenham C, Smith J, Morgan R. COVID-19: the gendered impacts of the outbreak. Lancet. 2020;395(10227):846–848. doi: 10.1016/S0140-6736(20)30526-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Venkat A, Asher SL, Wolf L, et al. Ethical issues in the response to Ebola Virus disease in United States emergency departments: a position paper of the American college of emergency physicians, the emergency nurses association, and the society for academic emergency medicine. Acad Emerg Med. 2015;22(5):605–615. doi: 10.1111/acem.12642. Cone DC, ed. [DOI] [PubMed] [Google Scholar]
- 42.Solano T, Gilbert GL, Kerridge IH, Nayyar V, Berry A. Ethical considerations in the management of Ebola virus disease. Med J Aust. 2015;203(4):193–195. doi: 10.5694/mja15.00168. [DOI] [PubMed] [Google Scholar]
- 43.Blais CM, White JL. Ebola and medical ethics - ethical challenges in the management of contagious infectious diseases. Ochsner J. 2015;15(1):5–7. [PMC free article] [PubMed] [Google Scholar]
- 44.Peterson A, Largent EA, Karlawish J. Ethics of reallocating ventilators in the covid-19 pandemic. BMJ. 2020;369(May):10–13. doi: 10.1136/bmj.m1828. [DOI] [PubMed] [Google Scholar]
- 45.Persad G, Wertheimer A, Emanuel EJ. Principles for allocation of scarce medical interventions. Lancet. 2009;373(9661):423–431. doi: 10.1016/S0140-6736(09)60137-9. [DOI] [PubMed] [Google Scholar]
- 46.Rosenbaum L. Facing Covid-19 in Italy — ethics, logistics, and therapeutics on the epidemic's front line. N Engl J Med. 2020;382(20):1873–1875. doi: 10.1056/NEJMp2005492. [DOI] [PubMed] [Google Scholar]
- 47.Daugherty Biddison EL, Faden R, Gwon HS, et al. Too many patients…a framework to guide statewide allocation of scarce mechanical ventilation during disasters. Chest. 2019;155(4):848–854. doi: 10.1016/j.chest.2018.09.025. [DOI] [PubMed] [Google Scholar]
- 48.Daugherty Biddison L, Berkowitz KA, Courtney B, et al. Ethical considerations: care of the critically ill and injured during pandemics and disasters: CHEST consensus statement. Chest. 2014;146(4):e145S–e155S. doi: 10.1378/chest.14-0742. [DOI] [PubMed] [Google Scholar]
- 49.British Medical Association . British Medical Association; London, United Kingdom: 2020. COVID-19 – Ethical Issues. A Guidance Note. [Google Scholar]
- 50.Emanuel EJ, Persad G, Upshur R, et al. Fair allocation of scarce medical resources in the time of covid-19. N Engl J Med. 2020;382(21):2049–2055. doi: 10.1056/NEJMsb2005114. [DOI] [PubMed] [Google Scholar]
- 51.van Manen M. But is it phenomenology? Qual Health Res. 2017;27(6):775–779. doi: 10.1177/1049732317699570. [DOI] [PubMed] [Google Scholar]
- 52.Neubauer BE, Witkop CT, Varpio L. How phenomenology can help us learn from the experiences of others. Perspect Med Educ. 2019;8(2):90–97. doi: 10.1007/s40037-019-0509-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Bushe G. In: The Routledge Companion to Organizational Change. Boje D, Burnes B, Hassard J, editors. Routledge; London: 2012. Appreciative Inquiry. Theory and critique. [DOI] [Google Scholar]
- 54.Lawrence DS, Hirsch LA. Decolonising global health: transnational research partnerships under the spotlight. International Health. 2020;12(6):518–523. doi: 10.1093/inthealth/ihaa073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Koshy E, Koshy V, Waterman H. Sage; London: 2010. Action Research in Healthcare. [Google Scholar]
- 56.Cox M Zooming with our indo-pacific EM colleagues. Your ED. Winter. Australia: ACEM Melbourne; 2020:37. https://acem.org.au/getmedia/e1de22ee-3820-4dbf-95c7-7e824f3d0259/ACE_Your-Ed-Winter_online. Accessed 22 June 2021
- 57.Gittus A, Griffiths B, de Salis D, Phillips G. Development and implementation of a Pacific Island centred COVID-19 Healthcare Worker Safety Guide. Emerg Med Australas. 2021;33(3):547–551. doi: 10.1111/1742-6723.13771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Ekeroma A. Collaboration as a tool for building research capacity in the Pacific Islands. Ann Hum Biol. 2018;45(3):295. doi: 10.1080/03014460.2018.1454510. [DOI] [PubMed] [Google Scholar]
- 59.Barbu CM. 2014. zoom: A spatial data visualization tool. (Version 2.0.6)https://github.com/cbarbu/R-package-zoom [Google Scholar]
- 60.D'Arcy P. Cultural divisions and island environments since the time of dumont d'Urville. J Pacific History. 2003;38(2):217–235. [Google Scholar]
- 61.McHugh MC. In: The Oxford Handbook of Qualitative Research. Leavy P, editor. Oxford University Press; 2014. Feminist qualitative research; pp. 136–164. [DOI] [Google Scholar]
- 62.Aven T. What is safety science? Saf Sci. 2014;67:15–20. doi: 10.1016/j.ssci.2013.07.026. [DOI] [Google Scholar]
- 63.Wears RL, Hunte GS. Seeing patient safety ‘like a state. Saf Sci. 2014;67:50–57. doi: 10.1016/j.ssci.2014.02.007. [DOI] [Google Scholar]
- 64.Vaioleti TM. Talanoa research methodology: a developing position on pacific research. Waikato J Educ. 2016;12(1):21. doi: 10.15663/wje.v12i1.296. [DOI] [Google Scholar]
- 65.QSR International Pty Ltd. (2020) NVivo (released in March 2020), https://www.qsrinternational.com/nvivo-qualitative-dataanalysis-software/home. Accessed 4 June 2021.
- 66.Boyatzis RE. SAGE Publications; Thousand Oaks, California: 1998. Transforming Qualitative Information: Thematic Analysis and Code Development. [Google Scholar]
- 67.Crabtree B, Miller W. In: Doing Qualitative Research. 2nd ed. Crabtree B, Miller W, Crabtree Benjamin F, Miller William L., editors. SAGE Publications; 1999. A template approach to text analysis: developing and using codebooks; pp. 163–177. [Google Scholar]
- 68.Fereday J, Muir-Cochrane E. Demonstrating rigor using thematic analysis: a hybrid approach of inductive and deductive coding and theme development. Int J Qual Methods. 2006;5(1):80–92. doi: 10.1177/160940690600500107. [DOI] [Google Scholar]
- 69.Daly J, Kellehear A, Gliksman M. Oxford University Press; Melbourne: 1997. The Public Health Researcher: A Methodological Guide. [Google Scholar]
- 70.Enhancing the quality and transparency of health research.https://www.equator-network.org/.Centre for Statistics in Medicine (CSM), NDORMS, University of Oxford Equator Network. Accessed 4 June 2021.
- 71.O’Brien BC, Harris IB, Beckman TJ, Reed DA, Cook DA. Standards for reporting qualitative research. Acad Med. 2014;89(9):1245–1251. doi: 10.1097/ACM.0000000000000388. [DOI] [PubMed] [Google Scholar]
- 72.Archibald MM, Ambagtsheer RC, Casey MG, Lawless M. Using zoom videoconferencing for qualitative data collection: perceptions and experiences of researchers and participants. Int J Qual Methods. 2019;18:1–8. doi: 10.1177/1609406919874596. [DOI] [Google Scholar]
- 73.Lupton D, Willis K. Routledge; Abingdon: 2021. The COVID-19 Crisis. Social Perspectives. [Google Scholar]
- 74.Smith AC, Thomas E, Snoswell CL, et al. Telehealth for global emergencies: implications for coronavirus disease 2019 (COVID-19) J Telemed Telecare. 2020;26(5):309–313. doi: 10.1177/1357633X20916567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Karim N, Rybarczyk MM, Jacquet GA, et al. COVID-19 pandemic prompts a paradigm shift in global emergency medicine: multidirectional education and remote collaboration. AEM Educ Train. 2021;5(1):79–90. doi: 10.1002/aet2.10551. Coates WC, ed. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix 2. Key informant interview guide
Appendix 3. Focus group discussion guide