Abstract
Thoracic outlet syndrome commonly presents with the neurogenic subtype and can be caused in rare circumstances by an anatomic abnormality such as a cervical rib, for which surgical excision is the mainstay of management. An inadequately excised first or cervical rib can result in recurrent symptoms. We have reported the case of a 30-year-old woman who had presented with symptoms of right recurrent arterial and neurogenic thoracic outlet syndrome. She underwent repeat right-sided first rib and cervical rib resection with brachial plexus neural lysis and right carotid–axillary bypass via a combined supraclavicular and infraclavicular approach. At 12 months of follow-up, improvement in her symptoms was noted.
Keywords: Arterial, Cervical rib, Neurogenic, Recurrent, Thoracic outlet syndrome
Thoracic outlet syndrome (TOS) is a constellation of symptoms that results from compression of the neurovascular bundle passing through three key anatomic sites: the scalene triangle, costoclavicular space, and pectoralis minor space. TOS is classified into three types according to which structures have been compressed: neurogenic (nTOS), arterial (aTOS), and venous TOS. This condition classically affects younger, physically active patients with scalene muscle abnormalities from repetitive movements. Predisposing anatomic abnormalities also increase the risk, such as the presence of a cervical rib. Most patients who develop TOS will develop the neurogenic subtype (95%), with cervical hyperextension injuries the most common etiology.1 In contrast, aTOS is rarer (1%) and can be caused by the presence of a cervical rib or an anomalous first rib.1 Compression of the subclavian artery can lead to aneurysmal changes with subsequent development of thromboembolism; thus, patients with aTOS are strong candidates for surgical intervention. An inadequately excised first rib or cervical rib can result in recurrent arterial and/or neurogenic symptoms. In the present case report, we have detailed the successful treatment of a patient with recurrent arterial and new-onset neurogenic symptoms after an inadequately excised first and cervical rib. The patient provided written informed consent for the report of her case details and imaging studies.
Case report
We have presented the case of a 30-year-old woman with a history of surgically treated aTOS who had presented with symptoms of right nTOS and recurrent aTOS. The patient had previously presented to an outside hospital with a pulseless right upper extremity and found to have an occluded right subclavian artery resulting from compression by a cervical rib. She had undergone open thromboembolectomy via brachial incision of the right upper extremity, excision of the first rib, and partial excision of a cervical rib with an interposition Dacron graft of the subclavian artery. On follow-up, duplex ultrasound showed compression of the Dacron graft from the remnant first rib and cervical rib. The findings from subsequent angiograms resulted in stenting and repeated balloon angioplasty, with inadequate expansion of the stent (Fig 1). The patient presented to our institution 18 months later with pain, numbness, and tingling suggestive of nTOS and duplex ultrasound findings consistent with severe stenosis within the interposition bypass graft in the subclavian artery, likely from extrinsic compression.
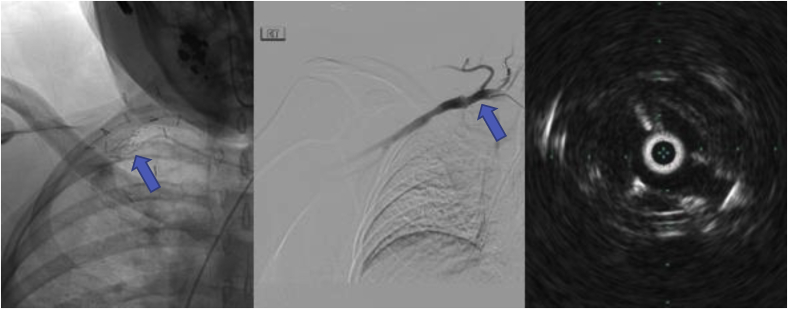
Fig 1.
Right subclavian arteriogram demonstrating mid-segment stenosis (arrow) within the stent and intravascular ultrasound demonstrating stenosis (arrow) with “pancaking” of the stent in the mid-segment from extrinsic compression.
We performed repeat right-sided first rib and cervical rib resection with brachial plexus neural lysis and right carotid–axillary bypass via a combined supraclavicular and infraclavicular approach (Fig 2). Intraoperatively, it was apparent that the area where the cervical rib had fused with the remnant first rib was compressing the previous Dacron graft (Fig 3). The entirety of the remainder of the first rib, which was anterior, and the area where the cervical rib had fused with the first rib were excised. A right upper extremity angiogram was performed at case completion, which showed a patent bypass and a patent brachial and ulnar artery with adequate revascularization of the palmar arch. The radial artery was noted to be chronically occluded from her initial presentation.
Fig 2.
Intraoperative photograph showing paraclavicular approach with resected rib and right carotid–axillary bypass with polytetrafluoroethylene.
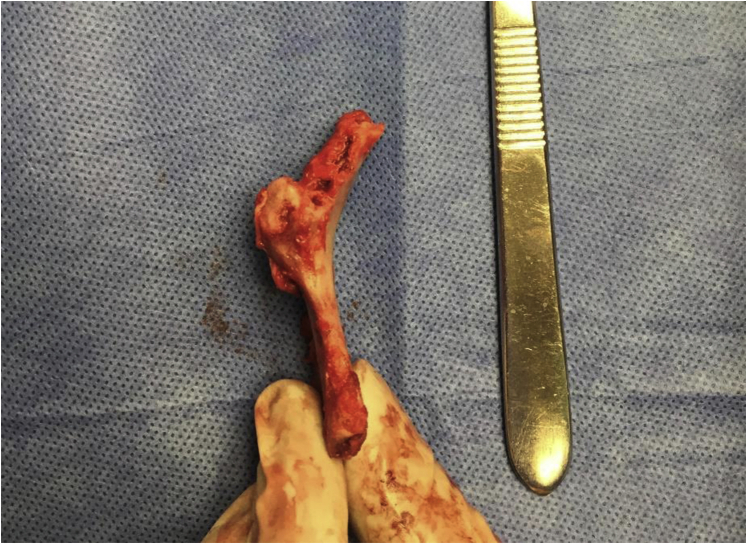
Fig 3.
Remnant first rib with anomalous insertion of the cervical rib.
The patient’s immediate postoperative course was unremarkable. She had developed a small right-sided pneumothorax that resolved with insertion of a pigtail catheter that was subsequently removed on postoperative day 1. The patient’s right upper extremity motor and sensory symptoms gradually improved. At discharge, a palpable ulnar pulse was appreciated with chronic absence of a radial pulse. At 12 months of follow-up in the clinic, the patient noted an improvement in the pain and numbness in the right upper extremity. She had a palpable right ulnar pulse, and duplex ultrasound showed a widely patent carotid–axillary bypass.
Discussion
Recurrent aTOS with nTOS is rare and can develop after an inadequately excised first and/or cervical rib. Our patient had initially presented with aTOS and had subsequently presented with coexisting nTOS and recurrent aTOS after inadequate removal of the first rib and cervical rib. In a retrospective study examining the postoperative outcomes of aTOS patients, 27% of the aTOS patients had presented with nonvascular symptoms, especially neurogenic.2 This directly contrasts with patients who develop nTOS, with the vast majority presenting with symptoms of brachial plexus compression only. A retrospective study performed at Johns Hopkins found that 22 of 423 patients presenting with nTOS had had coexisting subclavian artery compression.3,4 The results from these studies have confirmed the presence of a patient population presenting with mixed aTOS and nTOS.
The surgical approaches to TOS include resection of the first rib with either scalenectomy or scalenotomy for decompression.5 First rib resection is performed with either supraclavicular or transaxillary approaches for nTOS, with similar procedural and postoperative outcomes. However, supraclavicular approaches allow for adjunct procedures and vascular reconstruction and is preferred for aTOS.6 The patient’s initial operation for aTOS involved only a supraclavicular approach for rib excision and arterial reconstruction. Approximately 50% of the first rib was removed, with partial excision of the cervical rib and division of both anterior and middle scalene muscles. However, the present case has demonstrated the need for complete excision of the first rib and the anomalous cervical rib attachment to prevent recurrent symptoms. The repeat nature of the operation required both a supraclavicular and an infraclavicular approach for adequate visualization for rib excision and bypass from the right carotid artery to the axillary artery.
An important cause of recurrent TOS is the presence of a residual or an inadequately excised rib.7 Likes et al3,4 examined a patient subset with recurrent nTOS and found that complete excision of the first rib resulted in beneficial outcomes without significant morbidity. This suggests that complete excision of a first rib will be adequate surgical treatment for patients with recurrent TOS. Our patient differed because she had experienced new-onset nTOS with recurrent aTOS. However, removal of the first rib had resulted in reduced neurologic symptoms at 12 months postoperatively, supporting the results of Likes et al.3,4
aTOS is the rarest form of TOS and presents with symptoms of pain, a diminished pulse, claudication, and associated neurologic deficits in the upper extremities.8 The surgical approach for aTOS depends on the degree of subclavian artery pathology and type of bony abnormality. A 2017 retrospective study by Vemuri et al2 demonstrated excellent postoperative outcomes for 40 patients with aTOS. All the patients had undergone thoracic outlet decompression with complete anterior and middle scalenectomies through the supraclavicular (62.5%) or paraclavicular (37.5%) approach. During the operation, the respective bony abnormalities and subclavian pathologies were corrected, with a 92% rate of subclavian graft patency at 4.5 years with equally excellent functional outcomes.2
However, 7% of these patients had presented with recurrent aTOS due to an occluded subclavian artery graft. Additionally, all the patients who had experienced recurrent aTOS had had a more complicated vascular presentation on referral, including previous brachial artery thromboembolism and a history of strokes. Thus, prior vascular complications might increase the risk of recurrent aTOS. Our patient had presented with a patent graft at 12 months of follow-up, confirming the need for repeat surgery to adequately decompress the thoracic outlet and remove any extrinsic compression on the new bypass graft. The patient’s multiple previous endovascular approaches to maintain graft patency, including stent placement and balloon angioplasty, had proved unsuccessful.
Most patients who developed recurrent nTOS will exhibit an osseous or musculotendinous abnormality, which can be resolved via a subsequent reoperation.3 The literature supports the full resection of a rib in patients who have experienced recurrent nTOS secondary to an inadequately excised rib. Regarding venous TOS, limited infraclavicular exposure with removal of the medial first rib will usually be adequate to treat the underlying pathology and adequately decompress the vein. However, given the risk of recurrence with both nTOS and aTOS, as evidenced by our case report, we would advocate for complete excision of the cervical rib and first rib, which can be achieved via a supraclavicular approach.
Conclusions
Recurrent aTOS with nTOS is an extremely rare presentation with the respective surgical management having sparse representation in the literature. In the present case report, we have described the successful management of recurrent right-sided aTOS with new-onset nTOS via repeat rib resection, brachial plexus neural lysis, and carotid–axillary bypass.
Footnotes
Author conflict of interest: none.
The editors and reviewers of this article have no relevant financial relationships to disclose per the Journal policy that requires reviewers to decline review of any manuscript for which they may have a conflict of interest.
References
- 1.Osgood M.J., Lum Y.W. In: Rutherford’s vascular surgery and endovascular therapy. 9th ed. Sidawy A., Perler B.A., editors. Elsevier; 2019. Thoracic outlet syndrome: pathophysiology and diagnostic evaluation. [Google Scholar]
- 2.Vemuri C., McLaughlin L.N., Abuirqeba A.A., Thompson R.W. Clinical presentation and management of arterial thoracic outlet syndrome. J Vasc Surg. 2017;65:1429–1439. doi: 10.1016/j.jvs.2016.11.039. [DOI] [PubMed] [Google Scholar]
- 3.Likes K., Dapash T., Rochlin D.H., Freischlag J.A. Remaining or residual first ribs are the cause of recurrent thoracic outlet syndrome. Ann Vasc Surg. 2014;28:939–945. doi: 10.1016/j.avsg.2013.12.010. [DOI] [PubMed] [Google Scholar]
- 4.Likes K., Rochlin D.H., Call D., Freischlag J.A. Coexistence of arterial compression in patients with neurogenic thoracic outlet syndrome. JAMA Surg. 2014;149:1240–1243. doi: 10.1001/jamasurg.2014.280. [DOI] [PubMed] [Google Scholar]
- 5.Lee F., Burt B.M. In: Adult chest surgery. 3rd ed. Sugarbaker D.J., Bueno R., Burt B.M., Groth S.S., Loor G., Wolf A.S., et al., editors. McGraw Hill; 2020. Thoracic outlet syndrome. [Google Scholar]
- 6.Aboul Hosn M., Goffredo P., Man J., Nicholson R., Kresowik T., Sharafuddin M., et al. Supraclavicular versus transaxillary first rib resection for thoracic outlet syndrome. J Laparoendosc Adv Surg Tech A. 2020;30:737–741. doi: 10.1089/lap.2019.0722. [DOI] [PubMed] [Google Scholar]
- 7.Ambrad-Chalela E., Thomas G.I., Johansen K.H. Recurrent neurogenic thoracic outlet syndrome. Am J Surg. 2004;187:505–510. doi: 10.1016/j.amjsurg.2003.12.050. [DOI] [PubMed] [Google Scholar]
- 8.Brooke B.S., Freischlag J.A. Contemporary management of thoracic outlet syndrome. Curr Opin Cardiol. 2010;25:535–540. doi: 10.1097/HCO.0b013e32833f028e. [DOI] [PubMed] [Google Scholar]