Dear Editor,
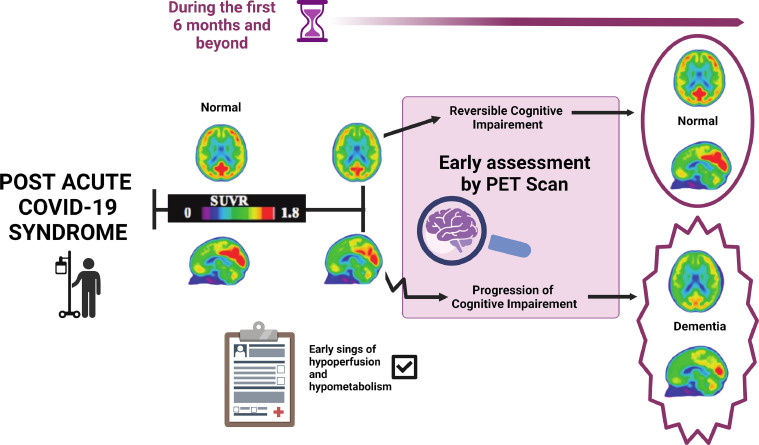
Recent evidence shows that SARS-COV2 infection could become a significant risk factor for dementia, in addition to aging, due to the virus' damage to the brain (Toniolo et al., 2021). Cognitive impairment, brain fog, and dementia are associated with the spectrum of psychiatric disorders in post-acute COVID-19 syndrome (PDPACS) (Paez et al., 2022; Toniolo et al., 2021)). Due to the course of dementia and early reversible cognitive decline in PDPACS, having a differential diagnosis among these disorders within the first six months could be challenging. Therefore through this letter, we want to highlight the importance of follow-up through imaging studies, specifically Proton Emission Tomography (PET). PET could analyze early brain changes after SARS-CoV-2 infection and become part of the standard of care differentiating cognitive impairement from irreversible cognitive impairement, otherwise known as dementia (Fig. 1 ). (Rudroff et al., 2021).
Fig. 1.
Role of PET scan in the early assessment of cognitive impairment or dementia in PDPACS. PET could analyze early metabolic brain changes during the first 6 months after SARS-CoV-2 infection before structural modifications. PET may become part of the standard of care, differentiating cognitive decline from irreversible cognitive decline, otherwise known as dementia. PET uses 18F, a glucose consumption biomarker. Higher incorporation of 18F is shown in the PET images with red). Image created with BioRender.com.
Magnetic Resonance Imaging (MRI) and PET scans are used to identify the effects of SARS-COV-2 infection in the brain. MRI analysis showed that 41 of 57 patients (71%) had perfusion abnormalities and ischemic and hemorrhagic lesions in white matter (Lambrecq et al., 2021). In contrast, PET scans allow the observation of the earliest abnormalities like hypometabolism in amygdala, and hippocampus, and the spread towards the thalamus, pons, medulla, and bilateral cerebellum, correlated with patients abnormalities such as hyposmia/anosmia, memory loss, and cognitive complaints of significant clinical relevance in PDPACS (Rudroff et al., 2021). PET advantages over MRI are due to the use of [18F] fluorodeoxyglucose (18F-FDG) radiotracer as a glucose consumption biomarker, which can help target metabolic changes in the brain before structural abnormalities mainly observed by MRIs (Rudroff et al., 2021).
Alzheimer's Disease (AD), and SARS-COV-2-infection, show early pathogenic similarities in the brain associated with hypometabolic changes before the appearance of structural modifications such as atrophy. Considering this, MRIs are less informative than PETs and will not detect the first signs of cellular metabolic stress that may lead to dementia. (Suzuki et al., 2019). Interestingly, Herholz et al., assessed 395 patients with AD and compared them to normal subjects. By using PET, they observed a reduction in the 18F-FDG uptake in the parietal, temporal, and prefrontal lobes. They found a mild to moderate AD (93% sensitivity and specificity) and very mild AD (i.e., mini-mental status examination (MMSE ≥ 4) (with 84% sensitivity and 93% specificity) (Rudroff et al., 2021). AD and PET scans of post-COVID-19 share similar pathological changes associated with cellular metabolic stress as an early marker of dementia. Monitoring the persistence or advancement of hypometabolism in the brain with PET and the absence of cognitive recovery could indicate the progression towards dementia in comparison to reversible cognitive impairment.
Considering these studies and early evidence, PET could become a standard of care tool to evaluate earlier pathogenic changes in the brain, possibly due to the excess inflammation, which is characteristic of SARS-COV-2 infection. More studies will be needed to validate PET; however, its use could help differentiate the persistence of cognitive impairment from dementia. The use of PET may help diagnose and could be indicated in thousands of patients recovered from COVID-19 with early signs of PDPACS, and alleviate the burden in health systems around the world.
Author contributions
MV, AF, BN, CEV, YLT, and AC wrote the manuscript, reviewed and cured data; KZ and AC revised the manuscript information, clinical data and applications. MV and AF conceptualize the article and provided the idea of using PET as a standard of care tool to evaluate earlier pathogenic changes in the brain, possibly due to the excess inflammation, which is characteristic of SARS-COV-2 infection. AC supervised, mentored and administered the work. MV, AF, BN, CEV, YLT, KZ and AC reviewed and commented on the manuscript to its final form and approval.
Funding
Sistemas Médicos de la Universidad San Francisco de Quito, SIME - USFQ. Escuela de Medicina, Colegio de Ciencias de la Salud COCSA, USFQ, Quito, Ecuador. These funding sources had no role in the design of this study and will not have any role during its execution, analyses, interpretation of the data, or decision to submit results.
Declaration of Competing Interest
Other authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
- Lambrecq V., Hanin A., Munoz-Musat E., Chougar L., Gassama S., Delorme C., Cousyn L., Borden A., Damiano M., Frazzini V., Huberfeld G., Landgraf F., Nguyen-Michel V.-.H., Pichit P., Sangare A., Chavez M., Morélot-Panzini C., Morawiec E., Raux M., Luyt C.-.E., Cohort COVID-19 Neurosciences (CoCo Neurosciences) Study Group Association of clinical, biological, and brain magnetic resonance imaging findings with electroencephalographic findings for patients with COVID-19. JAMA Netw. Open. 2021;4 doi: 10.1001/jamanetworkopen.2021.1489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paez A.F., Nicolalde B., Esquetini-Vernon C., Lara-Taranchenko Y., Velez-Arteaga M., Zambrano K., Ocampo J., Fusaro S., Capa G., Caicedo A. The time to act: early recommendations on patient care for psychiatric disorders in post-acute COVID-19 syndrome (PDPACS); Response to Llach and Ammella´s letter to the editor (Llach and Anmella, 2022) Eur. Neuropsychopharmacol. 2022;60:89–90. doi: 10.1016/j.euroneuro.2022.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rudroff T., Workman C.D., Ponto L.L.B. 18F-FDG-PET imaging for post-COVID-19 brain and skeletal muscle alterations. Viruses. 2021;13 doi: 10.3390/v13112283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Suzuki H., Venkataraman A.V., Bai W., Guitton F., Guo Y., Dehghan A., Matthews P.M., Alzheimer's Disease Neuroimaging Initiative Associations of regional brain structural differences with aging, modifiable risk factors for dementia, and cognitive performance. JAMA Netw. Open. 2019;2 doi: 10.1001/jamanetworkopen.2019.17257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Toniolo S., Scarioni M., Di Lorenzo F., Hort J., Georges J., Tomic S., Nobili F., Frederiksen K.S., Management Group of the EAN Dementia and Cognitive Disorders Scientific Panel Dementia and COVID-19, a bidirectional liaison: risk factors, biomarkers, and optimal health care. J. Alzheimers Dis. 2021;82:883–898. doi: 10.3233/JAD-210335. [DOI] [PubMed] [Google Scholar]