Abstract
PCR detection methods are useful in studies of organisms not amenable to culture. Inhibitors in environmental samples can interfere with such assays. We describe a magnetic bead DNA capture protocol that removes inhibitors from outdoor air samples, maintaining the sensitivity of a 16S Pneumocystis carinii mitochondrial rRNA gene-based PCR.
Pneumocystis carinii pneumonia (PCP) remains the most common opportunistic infection among individuals diagnosed with AIDS in the United States (5). However, basic knowledge of the ecology and epidemiology of the causative agent, P. carinii, is still lacking. The once widely accepted theory of PCP reactivation in severely immunosuppressed persons is currently being questioned in favor of the view that most episodes of PCP result from a de novo acquisition of the organism through inhalation of contaminated air (8, 11–13, 16, 18, 19, 21–24).
There is anecdotal evidence supporting the hypothesis that patients with fulminant PCP are the source of infectious P. carinii, shedding large numbers of organisms into their immediate environment as is the case with tuberculosis (2, 3, 7, 9, 10, 17). Alternatively, some studies suggest the existence of environmental reservoirs (20, 25), a transmission model which more closely resembles that of aspergillosis. Determining the source(s) of infectious P. carinii organisms is key to understanding when and how potential exposure control measures could be instituted.
PCR-based detection methods used in conjunction with environmental sampling are key tools in understanding the ecology and epidemiology of pathogens, such as P. carinii, that are difficult or impossible to culture. However, PCR results may be compromised by the presence of inhibitors in environmental samples. Such inhibitors have been reported in air, soil, and water samples (1, 4, 15). These include humic acid, clays, various organics, and large amounts of nontarget DNA in the collected sample, although additional types of inhibitors are likely to exist (4). Here we describe a methodology that allows for successful amplification of a target P. carinii DNA sequence spiked onto on a membrane filter containing inhibitory materials collected from a suburban outdoor environment.
Air samples were collected from an urban indoor environment and from a suburban outdoor environment during the autumn in the Southeastern United States. Air samples were collected over a 24-h period at approximately 0.4 liters per min using polyvinylidene difluoride filters (pore size, 0.45 μm) for use with PCR analysis and at approximately 0.25 liters per min using polycarbonate filters (pore size, 0.45 μm) for use with microscopic analysis. Indoor air sampling for viable fungi was accomplished using an Andersen impactor containing malt extract agar plates which were incubated at 25°C for approximately 1 week.
Fungal concentrations (in CFU per cubic meter) in the indoor environment were performed to assess the potential for microbial contamination. The rationale for this was that a high indoor fungal concentration would be indicative of conditions that encourage microbial contamination and thus potentially lead to PCR inhibition due to the presence of a large amount of nontarget DNA in the extract. The outdoor air samples were collected in autumn from a suburban location to provide a worst-case scenario for fungal concentrations in the general outdoors, and to permit collection of samples potentially containing other PCR inhibitors, such as partially combusted organic materials.
Polyvinylidene difluoride filters collected from both environments were spiked with various numbers of P. carinii cells (14), and DNA was prepared from the material adhering to each filter. Cell lysis was carried out directly on the filter by incubating the filter in a solution containing 150 mM NaCl, 10 mM Tris-HCl (pH 8.0), 1 mM EDTA, 0.5% sodium dodecyl sulfate and proteinase K (0.4 mg/ml) after incubating for 1 h at 55°C. DNA was extracted with phenol-chloroform followed by ethanol precipitation. The DNA pellet was resuspended in 20 μl of sterile water, and 10 μl was used as a template in the PCR to specifically amplify a fragment of the P. carinii 16S mitochondrial rRNA as described elsewhere (26), with the exception that the annealing temperature was raised from 50 to 55°C.
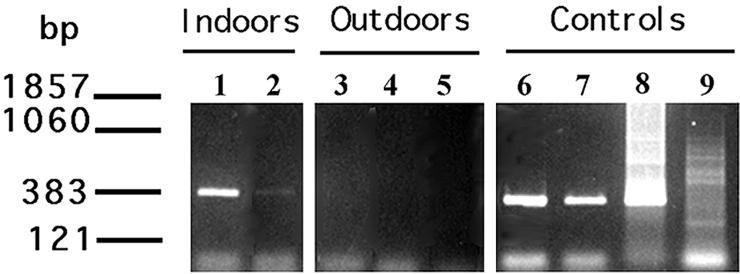
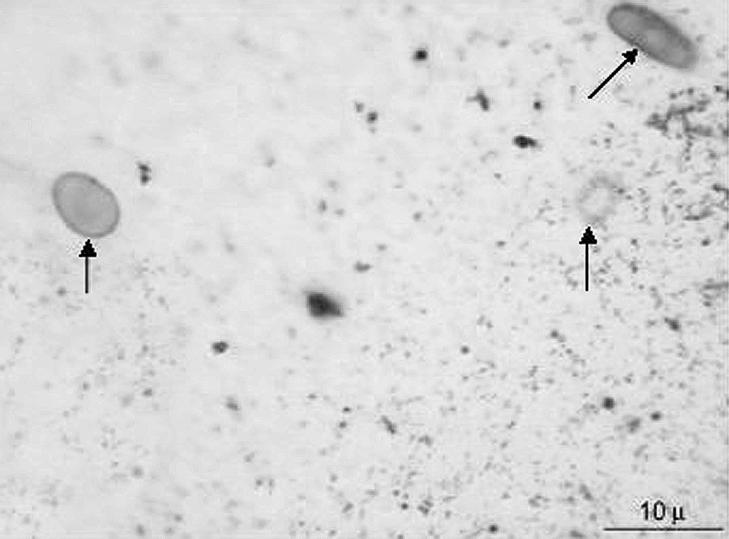
In the absence of any contaminants from the airborne environment, the PCR assay produced a strong signal from DNA prepared from as few as 102 organisms applied to and eluted from a filter (Fig. 1). In contrast, significant inhibition of the PCR was noted with filters used to collect outdoor air samples, while only slight PCR inhibition was noticed with filters used to collect indoor samples. In filters used to collect air samples from an indoor environment, a diminished signal was detected from filters spiked with 102 and 103 organisms (Fig. 1). In contrast, no signals were detected in filters exposed to outdoor air and spiked with up to 104 organisms (Fig. 1). These results suggested that unknown materials present in the outdoor air samples resulted in a PCR sensitivity loss of 1 to 2 logs and a slight loss of PCR sensitivity in the indoor samples. Samples from the indoor environment collected on malt extract agar indicated that there was an average viable fungal airborne concentration of 2.5 × 102 CFU/m3, most of which were fungi normally found in the outdoor environment, such as Aspergillus, Cladosporium, and Penicillium species. Direct microscopic analysis of the polycarbonate filters indicated that the average fungal spore concentration was approximately 103/m3 (which includes both nonviable spores and organisms not capable of growth on the malt extract agar). The outdoor fungal spore concentration was estimated to be 104/m3 from direct microscopic examination of the filters (Fig. 2). It is possible that the 10-fold difference in fungal contamination between the indoor and outdoor environments explains a portion of the PCR inhibition exhibited by the indoor and outdoor samples. Alternatively, the polymorphic, submicrometer particles found in abundance on the outdoor filters (Fig. 2) and not on the filter samples taken indoors might have been responsible for the PCR inhibition.
FIG. 1.
PCR inhibition occurring in the context of air samples. DNA was prepared from the filters and used as a template in the mitochondrial PCR as described in the text. Lane 1, 103 P. carinii organisms spiked onto a filter previously exposed to a contaminated indoor environment; lane 2, 102 P. carinii organisms spiked onto a filter previously exposed to a contaminated indoor environment; lane 3, 104 P. carinii organisms spiked onto a filter previously exposed to the outdoor environment; Lane 4, 103 P. carinii organisms spiked onto a filter exposed to the outdoor environment; lane 5, 102 P. carinii organisms spiked onto a filter previously exposed to the outdoor environment. Lane 6, 103 P. carinii organisms spiked onto an unexposed filter; lane 7, 102 P. carinii organisms spiked onto an unexposed filter; lane 8, positive control; lane 9, negative control.
FIG. 2.
Digital image of polycarbonate filter surface exposed to 360 liters of outdoor air over a 24-h period. Arrows indicate fungal spores. Small polymorphic particles represent the partially combusted organic particles discussed in the text. The number of fungal spores calculated to be on the surface of the entire filter was 10,800. Magnification, ×1,000.
A previous study demonstrated that hybridization of crude nucleic acid preparations with biotinylated pathogen-specific oligonucleotides followed by capture employing streptavidin-coated magnetic beads was useful in eliminating PCR inhibitors (6). To determine if this approach might be successful in restoring the sensitivity of the P. carinii PCR, filters exposed to outdoor air as described above were again spiked with P. carinii organisms. DNA was extracted and precipitated as before. The crude DNA preparations were adjusted to a total volume of 100 μl with DNA binding buffer (100 mM Tris-HCl [pH 7.5], 100 mM NaCl) containing a 25 nM concentration of a biotinylated primer derived from the P. carinii 16S rRNA sequence (5′ biotin-GATGGCTGTTTCCAAGCCCA 3′) . The mixture was heated to 95°C for 3 min and cooled to 35°C, and 100 μg of streptavidin-coated magnetic beads (Dynabeads M-280 Streptavidin) equilibrated in DNA binding buffer was added to each sample. The mixture was incubated at room temperature overnight. The beads were washed four times with 1 ml of DNA binding buffer per wash, and the bound DNA was eluted from the beads by resuspension of the beads in 10 μl of distilled water, followed by heating at 80°C for 2 min. Five microliters of eluted DNA was then used directly as a substrate in the 16S rRNA PCR assay as described above.
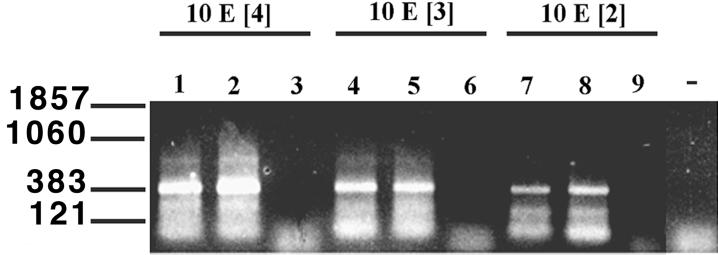
Dynabead purification of the crude nucleic acid preparations prepared from the spiked filters exposed to outdoor air restored the sensitivity of the assay to levels comparable to those seen in filters not exposed to the ambient environment (e.g., Fig. 3). In contrast, nucleic acid prepared from identical filters but not subjected to the Dynabead purification remained unable to support DNA amplification (Fig. 3). To determine if these results reflected a significant improvement in the sensitivity of the assay, a total of 46 replicate filters were analyzed. These replicates concentrated on outdoor air samples, as these were found to be most inhibitory to the PCR, as described above. In the group of samples spiked with P. carinii but in which the DNA was not subjected to magnetic bead purification, 0 of 12 samples produced positive results in the P. carinii PCR. In contrast, 28 of 30 samples subjected to magnetic bead purification were positive in the PCR. As expected, zero of four control filters not spiked with P. carinii were negative, confirming the specificity of the assay. These results demonstrated that magnetic bead capture significantly improved the sensitivity of the PCR assay for the detection of P. carinii in the presence of outdoor air samples (P < 0.0001; Fisher's exact test).
FIG. 3.
PCR signal recovery from air samples following magnetic bead purification. Magnetic bead purification and PCR amplification of the templates were carried out as described in the text. Lanes 1 and 2, 104 P. carinii organisms spiked onto filters previously exposed to the outdoor environment and purified by magnetic bead capture; lane 3, 104 P. carinii organisms spiked onto filters exposed to the outdoor environment without the capture assay; lanes 4 and 5, 103 P. carinii organisms spiked onto filters exposed to the outdoor environment after use of the capture assay; lane 6, 103 P. carinii organisms spiked onto filters exposed to the outdoor environment without capture assay; Lanes 7 and 8, 102 P. carinii organisms spiked onto filters exposed to the outdoor environment after use of the capture assay; lane 9, 102 P. carinii organisms spiked onto filters exposed to the outdoor environment without capture assay; lane 10, negative control.
These results demonstrate that substances collected during normal air sampling protocols may contain inhibitors that can drastically affect the sensitivity and accuracy of PCR-based detection assays. Although simple techniques such as a 10- to 20-fold dilution of the DNA extract have proven useful in preventing PCR inhibition (1), purification of the crude nucleic acids employing biotinylated pathogen-specific oligonucleotides and magnetic capture allow for successful DNA amplification without a loss in sensitivity. This method of DNA purification will be applicable to most indoor and outdoor environments, including clinical and outpatient settings where P. carinii is most likely to be present. This method will therefore be useful in testing the hypothesis that individuals with patent PCP are capable of seeding their environments with large numbers of organisms and in determining the persistence of these organisms in airborne samples.
Acknowledgments
We thank Marilyn Bartlett, Mark Lansbury, and Pam Durant for providing P. carinii-infected rat lungs for use in this study. This work was supported by a grant from the National Institutes of Health to S.H.V. (project 1 R01 AI54586-01).
REFERENCES
- 1.Alvarez A J, Buttner M P, Stezenbach L D. PCR for bioaerosol monitoring: sensitivity and environmental interference. Appl Environ Microbiol. 1995;61:3639–3644. doi: 10.1128/aem.61.10.3639-3644.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bartlett M S, Lu J-J, Lee C-H, Durant P J, Queener S F, Smith J W. Types of Pneumocystis carinii detected in air samples. J Euk Microbiol. 1996;43:44S. doi: 10.1111/j.1550-7408.1996.tb04980.x. [DOI] [PubMed] [Google Scholar]
- 3.Bartlett M S, Vermund S H, Jacobs R R, Durant P, Shaw M M, Smith J W, Tang X, Lu J-J, Li B-H, Jin S, Lee C-H. Detection of Pneumocystis carinii DNA in air samples: likely environmental risk to susceptible persons. J Clin Microbiol. 1997;35:2511–2513. doi: 10.1128/jcm.35.10.2511-2513.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bej A K, Mahububani M H. Application of the polymerase chain reaction in environmental microbiology. In: Griffen A G H, editor. PCR technology: current innovations. San Diego, Calif: Academic Press; 1994. pp. 327–339. [Google Scholar]
- 5.Centers for Disease Control and Prevention. HIV/AIDS surveillance report 9 (2). Atlanta, Ga: Centers for Disease Control and Prevention; 1997. [Google Scholar]
- 6.Chang G J, Trent D W, Vorndam A V, Vergne E, Kinney R M, Mitchell C J. An integrated target sequence and signal amplification assay, reverse transcriptase-PCR-enzyme-linked immunosorbent assay, to detect and characterize flaviviruses. J Clin Microbiol. 1994;32:477–483. doi: 10.1128/jcm.32.2.477-483.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chave J P, Wauters J P, Van Melle G, Francioli P. Transmission of Pneumocystis carinii from AIDS patients to other immunosuppressed patients: a cluster of Pneumocystis carinii pneumonia in renal transplant recipients. AIDS. 1991;5:927–932. doi: 10.1097/00002030-199108000-00002. [DOI] [PubMed] [Google Scholar]
- 8.Chen W, Gigliotti F, Harmsen A G. Latency is not an inevitable outcome of infection with Pneumocystis carinii. Infect Immun. 1993;61:237–242. doi: 10.1128/iai.61.12.5406-5409.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Goesch T R, Gotz G, Stellbrunk K H, Albrecht H, Weh H J, Hossfield D K. Possible transfer of Pneumocystis carinii between immunodeficient patients. Lancet. 1990;336:627. doi: 10.1016/0140-6736(90)93420-t. [DOI] [PubMed] [Google Scholar]
- 10.Hennequin C, Page B, Roux P, Legendre C, Kreis H. Outbreak of Pneumocystis carinii pneumonia in a renal transplant unit. Eur J Clin Microbiol Infect Dis. 1995;14:122–126. doi: 10.1007/BF02111870. [DOI] [PubMed] [Google Scholar]
- 11.Hughes W T. Natural mode of acquistion for de novo infection with Pneumocystis carinii. J Infect Dis. 1982;145:842–848. doi: 10.1093/infdis/145.6.842. [DOI] [PubMed] [Google Scholar]
- 12.Keely S P, Stringer J R. Sequences of Pneumocystis carinii f. sp. hominis strains associated with recurrent pneumonia vary at multiple loci. J Clin Microbiol. 1997;35:2745–2747. doi: 10.1128/jcm.35.11.2745-2747.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Keely S P, Stringer J R, Baughman R P, Linke M J, Walzer P D, Smulian A G. Genetic variation among Pneumocystis carinii hominis isolates in recurrent Pneumocystis. J Infect Dis. 1995;172:595–598. doi: 10.1093/infdis/172.2.595. [DOI] [PubMed] [Google Scholar]
- 14.Lee C-H, Bauer N L, Shaw M M, Durkin M M, Bartlett M S, Queener S F, Smith J W. Proliferation of rat Pneumocystis carinii on cells sheeted on microcarrier beads in spinner flasks. J Clin Microbiol. 1993;31:1659–1662. doi: 10.1128/jcm.31.6.1659-1662.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mahbubani M H, Schaefer F W I, Jones D D, Bej A K. Detection of Giardia in environmental waters by immuno-PCR amplification methods. Curr Microbiol. 1998;36:107–113. doi: 10.1007/s002849900288. [DOI] [PubMed] [Google Scholar]
- 16.Millard P R, Heryet A R. Observation favouring Pneumocystis carinii as a primary infection: a monoclonal antibody study on paraffin sections. J Pathol. 1988;154:365–368. doi: 10.1002/path.1711540413. [DOI] [PubMed] [Google Scholar]
- 17.Olsson M, Lidman C, LaTouche S, Bjorkman A, Roux P, Linder E, Wahlgreen M. Identification of Pneumocystis carinii f. sp. hominis gene sequences in filtered air in hospital environments. J Clin Microbiol. 1998;36:1737–1740. doi: 10.1128/jcm.36.6.1737-1740.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ongibene F P, Masur J, Rogers P, Travis A F, Suffredini L, Feuerstein I, Gill V J, Baird B F, Carrasquillo J S, Parrillo J E, Lane H C, Shelmamer J H. Nonspecific interstitial pneumonitis without evidence of Pneumocystis carinii in asymptomatic patients infected with human immunodeficiency virus (HIV) Ann Intern Med. 1988;109:874–878. doi: 10.7326/0003-4819-109-11-874. [DOI] [PubMed] [Google Scholar]
- 19.Peters S E, Wakefield A E, Sinclair K, Millard P R, Hopkins J L. A search for Pneumocystis carinii in post mortem lungs by DNA amplification. J Pathol. 1992;166:195–198. doi: 10.1002/path.1711660217. [DOI] [PubMed] [Google Scholar]
- 20.Pifer L L, Hughes W T, Stagno S, Woods D. Pneumocystis carinii infection: evidence for high prevalence in normal and immunosuppressed children. Pediatrics. 1978;61:35–41. [PubMed] [Google Scholar]
- 21.Sepkowitz K, Schulager N, Godwin T, Armstrong C, Bucula R. DNA amplification in experimental Pneumocystosis: characterization of serum Pneumocystis carinii DNA and potential P. carinii carrier states. J Infect Dis. 1993;168:421–426. doi: 10.1093/infdis/168.2.421. [DOI] [PubMed] [Google Scholar]
- 22.Tsolaki A G, Miller R F, Underwood A P, Bajeri S, Wakefield A E. Genetic diversity at the internal transcribed spacer regions of the rRNA operon among isolates of Pneumocystis carinii from AIDS patients with recurrent pneumonia. J Infect Dis. 1996;174:141–156. doi: 10.1093/infdis/174.1.141. [DOI] [PubMed] [Google Scholar]
- 23.Vargas S L, Hughes W T, Wakefield A E, Oz H S. Limited persistence and subsequent elimination of Pneumocystis carinii from the lungs after P. carinii pneumonia. J Infect Dis. 1995;172:506–510. doi: 10.1093/infdis/172.2.506. [DOI] [PubMed] [Google Scholar]
- 24.Vogel P, Miller C J, Lowenstine L L, Lackner A A. Evidence of horizontal transmission of Pneumocystis carinii pneumonia in simian immunodeficiency virus-infected rhesus monkeys. J Infect Dis. 1993;168:836–843. doi: 10.1093/infdis/168.4.836. [DOI] [PubMed] [Google Scholar]
- 25.Wakefield A E. DNA Sequences identical to Pneumocystis carinii f. sp. carinii and Pneumocystis carinii f. sp. hominis in samples of air spora. J Clin Microbiol. 1996;34:1754–1759. doi: 10.1128/jcm.34.7.1754-1759.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wakefield A E, Pixley F J, Banerji S, Sinclair K, Miller R F, Moxon E R, Hopkin J M. Amplification of mitochondrial ribosomal RNA sequences from Pneumocystis carinii DNA of rat and human origin. Mol Biochem Parasitol. 1990;43:69–76. doi: 10.1016/0166-6851(90)90131-5. [DOI] [PubMed] [Google Scholar]