Abstract
Objectives
The development of Brain-Computer Interfaces to restore communication (cBCIs) in people with severe motor impairment ideally relies on a close collaboration between end-users and other stakeholders, such as caregivers and researchers. Awareness about potential differences in opinion between these groups is crucial for development of usable cBCIs and access technology (AT) in general. In this study, we compared the opinions of prospective cBCI users, their caregivers and cBCI researchers regarding: 1) what applications would users like to control with a cBCI; 2) what mental strategies would users prefer to use for cBCI control; and 3) at what stage of their clinical trajectory would users like to be informed about AT and cBCIs.
Methods
We collected data from 28 individuals with locked-in syndrome, 29 of their caregivers and 28 cBCI researchers. The questionnaire was supported with animation videos to explain different cBCI concepts, the utility of which was also assessed.
Results
Opinions of the three groups were aligned with respect to the most desired cBCI applications, but diverged regarding mental strategies and timing of being informed about cBCIs. Animation videos were regarded as clear and useful tools to explain cBCIs and mental strategies to end-users and other stakeholders.
Conclusions
Disagreements were clear between stakeholders regarding which mental strategies users prefer to use and when they would like to be informed about cBCIs. To move forward in the development and clinical implementation of cBCIs, it will be necessary to align the research agendas with the needs of the end-users and caregivers.
Keywords: Brain-Computer Interface, Communication, user-centered design, locked-in syndrome, caregivers, researchers
1. Introduction
Assistive technology (AT) has been developed to facilitate and/or enable communication in people with paralysis and communication impairments, serving those with some form of (residual) voluntary movement control 1,2. For individuals with poor volitional control of their muscles or with no movement control (locked-in syndrome; LIS) such technology often falls short. In these cases, Brain-Computer Interfaces (BCIs) may present the only alternative to establish communication 3, as BCIs are intended to be controlled without any residual muscle activity.
The effectiveness of cBCIs in the motor-impaired target population largely depends on the quality of the BCI system but also on its acceptance by the end-user 4-10. There is an increasing awareness about the importance of accommodating the wishes, needs and opinions of end-users in the design of BCIs 4,11. However, the proper incorporation of such ‘User-Centered Design’ requires other stakeholders, such as researchers and caregivers, to be aware of these factors. Earlier studies have focused on the opinion of caregivers 6,12 and rehabilitation professionals 13, in order to evaluate, inform and define design requirements of BCIs. However, a direct comparison between the user’s opinion and the opinion of their caregivers and cBCI researchers has not yet been conducted.
In a previous study we assessed the opinion of prospective cBCI users about which applications users would like to control with a cBCI, which mental strategies users would prefer to use for cBCI control, and when during the clinical trajectory users would like to be informed about cBCIs and AT in general 14. For that, we administered a questionnaire to 28 Dutch individuals with LIS (prospective users) that incorporated animation videos specifically designed to introduce and explain cBCIs. We showed that, despite differences in etiology, individuals with LIS agree with respect to applications, mental strategies and timing of information 14.
In the current report, we extend these results by including caregivers and researchers and compare their opinions on the three above topics with those of the users. Furthermore, given that (most) cBCIs are still in the development stage and the concept of mental strategies for BCI control can be difficult to convey, we assessed the clarity and comprehension of the animation videos as a tool to introduce and explain cBCIs.
2. Material and Methods
A questionnaire was administered to each of the three different target groups: prospective cBCI users; their caregivers; and a group of international cBCI researchers. The questionnaires were implemented on the Qualtrics Survey platform (www.qualtrics.com/). The study was assessed by the local ethics board of the Medical University Center (UMC) Utrecht, who determined it to be exempt from the Dutch Medical Scientific Research Act. Following standard UMC Utrecht policy, all participants (or caregivers on behalf of the users) gave written informed consent to participate in the study at the beginning of the home visit (users) or by completing and submitting the online questionnaire (caregivers and researchers).
2.1. Participants
2.1.1. Prospective users
We included 28 Dutch individuals with LIS and administered the questionnaire in Dutch during a 3-hour home visit. The user population was divided into two groups depending on the etiology underlying their motor impairment: neuromuscular disorder (NMD; e.g., amyotrophic lateral sclerosis; 13 participants) or sudden onset (SO; e.g., trauma or stroke; 15 participants). Detailed information about the home interview, data description, demographics and results regarding the user group can be found in 14.
2.1.2. Caregivers
An online questionnaire (in Dutch) was sent to 41 primary caregivers (professional caretakers and family members) who provide daily care to one of the included prospective users. In total, 29 caregivers completed the questionnaire (71% inclusion rate). Eight users were associated with one caregiver each, 9 were matched with two caregivers and one was matched with three caregivers. The caregiver group was divided into two groups depending on the type of disorder of the user they provided care for: 15 NMD-related caregivers and 14 SO-related caregivers.
2.1.3. Researchers
An online questionnaire (in English) was sent to 70 international BCI researchers whose work was related to both cBCIs and individuals with communication impairment. Email addresses were obtained from BCI research groups, from publications on the topic of cBCI and by referral from other BCI researchers. Approached researchers were spread over 15 countries and 48 different institutions (maximum 4 researchers per institution). To avoid biased responses, the authors of this manuscript and their respective research teams were not included in the study. In total, 29 researchers (41% inclusion rate) completed and submitted the questionnaire.
2.2. Structure of the questionnaire
All three questionnaires consisted of five sections: 1) demographics, 2) introduction to cBCI, 3) cBCI applications, 4) mental strategies and 5) time of information. The users’ and caregivers’ questionnaires were written in Dutch, while the researchers’ questionnaire was written in English. Different sentence forms were used to indicate if respondents were asked to give their own opinion, or to convey their idea about what and end-user would prefer. In total, 9 animation videos (21-110 s in duration) were used for the introduction of the concept of cBCI and for explaining 8 different mental strategies for cBCI control. The animation videos were tailored for this study, narrated in Dutch or English and reviewed by one individual with LIS and the co-authors’ research teams. In order to assess the quality of the animation videos, we asked the BCI researchers for feedback in an additional section (see 2.2.6). In the questionnaire, the order in which the applications, mental strategies and respective ranking questions were presented was randomized and therefore differed between participants.
2.2.1. Section 1: Demographics
Participants were asked to answer a list of multiple-choice/short-answer questions on their demographics. When applicable, more than one multiple-choice answer could be selected and a free-text field was available to accommodate other options.
2.2.2. Section 2: Introduction
Communication BCIs were introduced by means of an animation video (Figure 1), which explained the concept of a BCI in general and of cBCIs in particular. Of note, we described a conceptually ideal system that would be 100% accurate and 100% accepted by the users to ensure that participants would focus on evaluating the mental strategy rather than the efficacy of the cBCI.
Figure 1 – Representative screenshots of the animation videos used in the questionnaire.
Three illustrative screenshots of the videos used to explain the concept of BCIs, BCI-based communication and mental strategies that can be used to control the BCI. For simplicity and consistency across mental strategies, we used a spelling matrix as a control application (middle panel) and a button press (and subsequent letter selection) as a control output (upper panel).
2.2.3. Section 3: cBCI applications
We asked the opinion about 6 possible cBCI applications, including private conversation and writing (e.g., email, chat, diary), direct personal communication (e.g., voice synthesis, direct conversation), environmental control (e.g., home appliances, alarm), general computer use (e.g., playing games, internet surfing, social media), artistic expression (e.g., painting, producing music) and emotions and facial expressions (e.g., expressing feelings, emoji’s). As users were currently using AT with specific applications, we considered these applications as the optimal target for a cBCI. Hence, we asked users what applications their current AT device provided and how often they used these applications. Lastly, we asked users to rank all applications from most preferred to least preferred. Caregivers and researchers were asked to consider their knowledge about the user’s opinions and preferences and indicate 1) which applications they thought the users would find essential in a cBCI, 2) how often they thought these would be used by the user and 3) to rank the application from the most preferred by the user to the least preferred.
2.2.4. Section 4: Mental strategies
We identified 8 mental strategies that can be used for cBCI control: hand movement attempt, other body part movement attempt, attempted speech, counting backwards, visual imagery, visual P300, auditory P300 and steady-state visual evoked potentials (SSVEPs). Each mental strategy was presented using a specific animation video (Figure 1). For simplicity and to avoid bias across mental strategies, the control application (spelling matrix with automatic scanning) and the control output (button press and subsequent letter selection) were the same for every mental strategy. After each mental strategy video, the respondent was asked to imagine using that particular mental strategy and rate it on a 5-point Likert scale on difficulty and enjoyability. The clarity of the mental strategies as illustrated by the videos was also rated using the same scale. In this section of the questionnaire we considered the caregivers as a “control group”, in that they were asked to rate each paradigm from their own perspective. As the opinion of the researchers about the paradigms were likely biased by their own research topics, we asked them instead to report what they thought the users would rate. In the end of the fourth section, we asked all participants to rank the top four mental strategies from their own (users and caregivers) or the users’ perspective (researchers).
2.2.5. Section 5: Time of information
In this section we separated the results by type of etiology (NMD and SO) and compared the opinions of the three groups. We asked the users, caregivers and researchers in which phase of their medical history they/the user would like to be informed about AT aids including cBCIs. Namely, ‘as soon as possible’ after diagnosis/incident, ‘before rehabilitation’ (possible period between incident/hospitalization and start of therapy), ‘during rehabilitation’, ‘after rehabilitation’, ‘when no residual movement/speech is available’ or an open field for another timepoint. For simplicity and clarity, in the researchers’ questionnaire we repeated this question and asked the researchers to respond separately for the SO and the NMD situation. For both users and caregivers this separation was not necessary as they were asked to reflect on their own situation and their answers could be linked to only one group.
2.2.6. Section 6: BCI researchers’ feedback
Besides the assessment of the videos’ clarity in section 4 of the questionnaire, we asked the BCI researchers for their opinion about how well the videos in general introduce cBCIs to prospective users and other stakeholders, such as caregivers, family members and rehabilitation centers.
2.3. Data analysis
2.3.1. Descriptive statistics and open answers
Descriptive statistics were used to describe the results of the three questionnaires. Percentages were used for comparison between groups. These were computed relative to the total number of respondents per group (N=28 for users; N=29 for caregivers; and N=29 for researchers) or to a subgroup of participants when applicable. Non-parametric Kruskal-Wallis and post-hoc Mann-Whitney tests were used to compare Likert scale responses between groups.
2.3.2. Ranking questions
As in our previous report 14, we quantified the importance or preference of the participants for specific applications and mental strategies (ranking questions) using a center-of-mass (COM) score. The COM scores vary between 0 and the total number of ranked options (4 or 6), such that the larger COM scores correspond to a higher preference. Meaningful differences in COM values across applications or mental strategies were identified using a Monte Carlo randomization method to estimate the expected variance of the scores when ranking would be performed randomly (see 14 for more details).
3. Results
3.1. Demographics
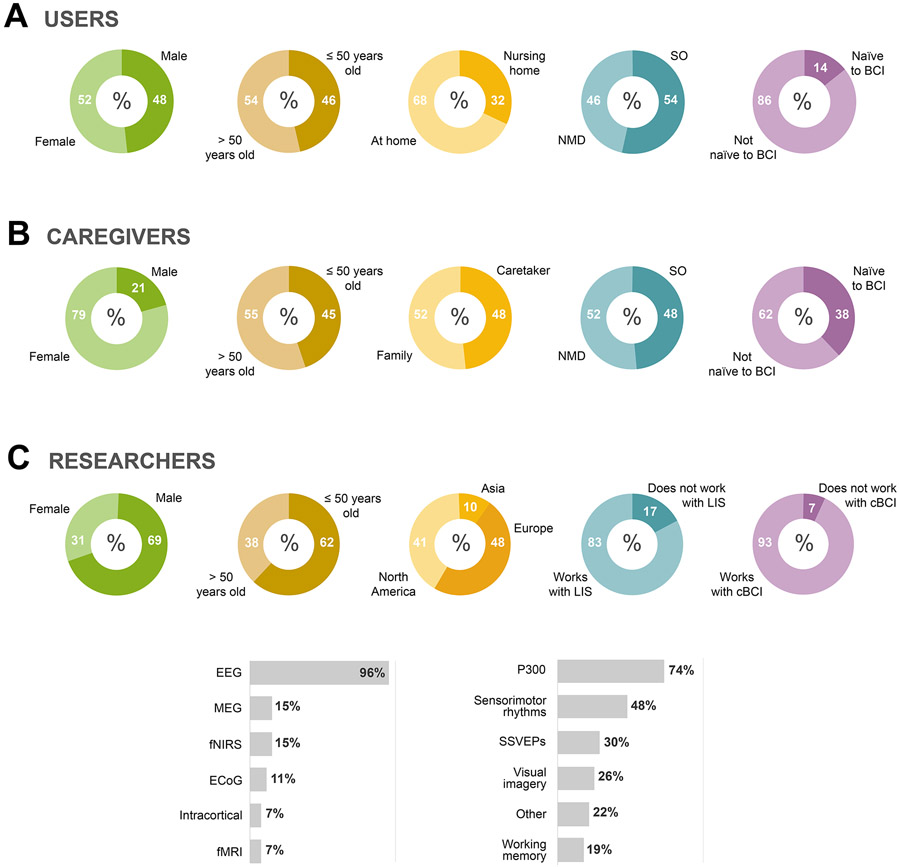
Of the 28 users (52% female), 68% lived at home and 32% in a nursing home; about half were locked-in as a result of NMD (46%) and the other half due to an SO event (54%) (Figure 2A). Of the 29 caregivers (median age 52 years old; range 20-85 years old; 79% female), 52% were family members, 52% cared for users with NMD and 48% for users with SO (Figure 2B). More than half of the caregivers and users were familiar with the BCI concept (62% and 86%, respectively). Of the 28 BCI researchers (median age 48 years old, range 27-73 years old; 69% male), most worked either in North-America (41%) or in Europe (48%) (Figure 2C). As expected, the majority worked with or close to individuals with LIS (83%). In addition, 93% of the researchers worked or had experience with cBCIs. The majority used EEG signals (96%) and worked with P300 (74%) and/or sensorimotor rhythms (48%) as mental strategies for cBCI control (Figure 2C).
Figure 2 – Demographic description of the users, caregivers and researchers.
Demographic information of the users (N=28), caregivers (N=29) and researchers (N=29) included in this study was extracted from Section 1 of the questionnaire. A) Information (in percentage) about the user’s gender (male, female), age group (≤ 50 years old, > 50 years old), living situation (at home or at a nursing home), etiology (neuromuscular disease, NMD; sudden onset, SO) and whether they were naïve to BCI. B) Information (in percentage) about the caregiver’s gender (male, female), age group (≤ 50 years old, > 50 years old), personal/professional relation to the user (family member, professional caregiver), type of LIS of individual the caregiver takes care of (neuromuscular disease, NMD; sudden onset, SO), and whether they were naïve to BCI. C) Information (in percentage) about the researcher’s gender (male, female), age group (≤ 50 years old, > 50 years old), continent of residence (Asia, Europe or North America), and whether they worked with individuals with locked-in syndrome (LIS) and communication Brain-Computer Interfaces (cBCIs). Bar plots indicate most used signal acquisition techniques by researchers in their line of work, as well as the most investigated mental strategies for controlling a BCI.
3.2. cBCI applications
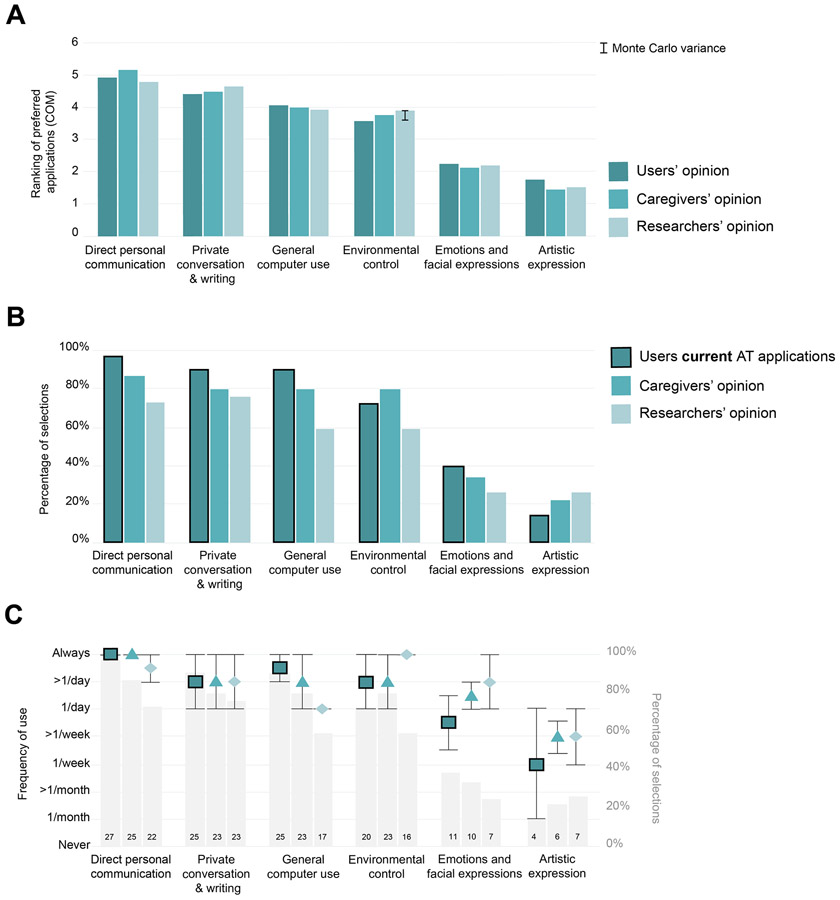
Users, caregivers and researchers showed similar preference rankings for all applications (Figure 3A; differences between groups smaller than the Monte Carlo variance 0.32), with the exception of ‘environmental control’ (difference of 0.33 between users and researchers). ‘Direct personal communication’, ‘private conversation & writing’ and ‘general computer use’ were the top three ranked applications. Comparison of the percentage of users using a certain application to the percentage of caregivers and researchers indicating that application as essential to be provided by a cBCI showed that all applications (except ‘environmental control’ and ‘artistic expression’) were selected less frequently by caregivers and researchers than by users (Figure 3B). When compared with how often the users used the applications, the caregivers’ estimation of frequency of use was more often in line with the one reported by the users than that of researchers; with the exception of the frequency of use of ‘emotions & facial expressions’ and ‘artistic expression’, which was estimated to be higher by caregivers and researchers (Figure 3C).
Figure 3 – Comparison between users’ current AT application and expected cBCI applications.
A) Ranking of preferred applications to be supported by a cBCI, using the center-of-mass (COM) metric. Meaningful differences between groups were estimated using the Monte Carlo variance indicated on the top right corner (0.32). In addition, the size of the Monte Carlo variance is indicated on top of the one bar that showed a larger-than-Monte-Carlo-variance difference from users. Rating scales ranged from 1 (least preferred) to 6 (most preferred). B) Percent of users that have a specific AT application currently available at home (dark green, highlighted with black line) compared with the importance of these applications as rated by the caregivers (green) and researchers (light green). C) Median and median absolute deviation (error bars) of how often each application was (estimated to be) used. Of note, the frequency of usage of each application was computed from the number of participants that selected that specific application in B (gray bars; units in the right-side y-axis; copies of the information given in B).
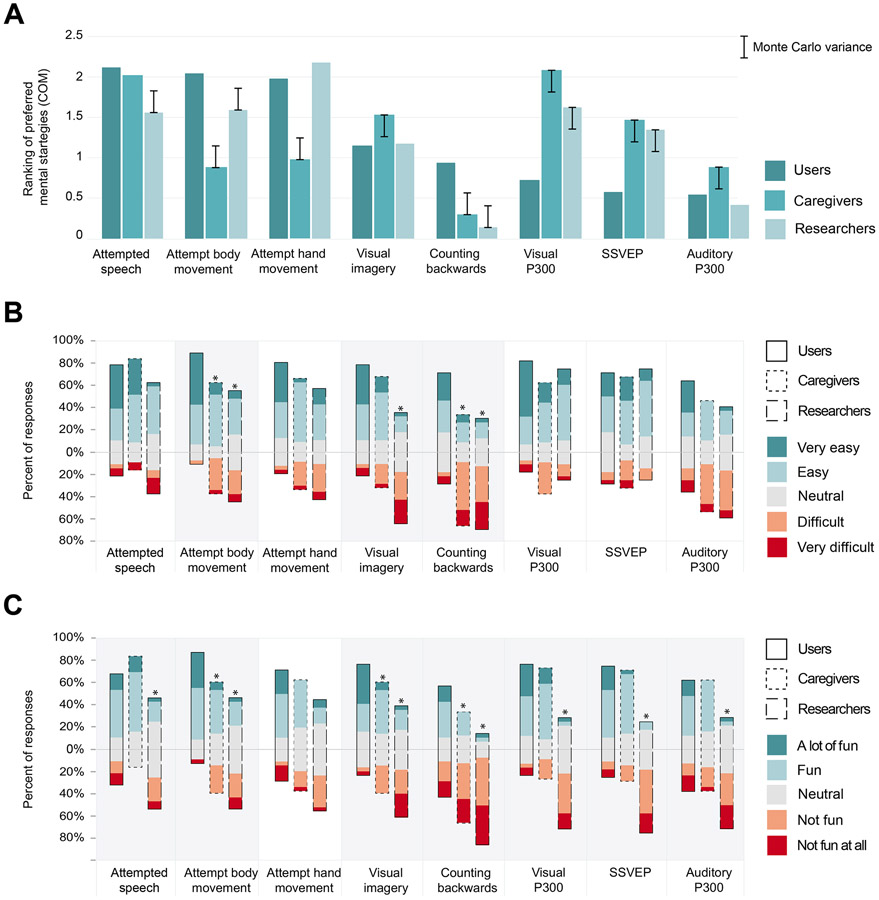
3.3. Mental strategies
Results show that attempted speech was equally favored by caregivers (here considered abled control group) and users. Caregivers (Figure 4A) showed a meaningfully higher preference than users for visual strategies such as P300 and SSVEP and visual imagery (larger than Monte Carlo variance of 0.28), and considerably lower preference for body part action generation (attempted hand or body movement) than users. Similar differences were found between users and researchers (Figure 4A) for the visually induced paradigms (P300 and SSVEP). In contrast to the caregivers, researchers considered attempted speech less favorable than the users, albeit still among the four most favored strategies. The most chosen body parts across the groups were the feet (9 users and 10 researchers) and toes (7 users and 8 caregivers). Overall, users found all strategies very easy to execute (Figure 4B). Furthermore, caregivers and/or researchers rated attempted body movement, visual imagery and counting backwards as significantly more difficult than the users (Kruskal Wallis test for 3 groups and 8 strategies, p<0.05 Bonferroni corrected for N=8; Mann-Whitney test within strategy, p<0.05; Figure 4B). Differences between users and caregivers/researchers were found for the question about the level of enjoyability. For all but one strategy (attempted hand movement), there was a significant difference across groups (Kruskal Wallis test for 3 groups and 8 strategies, p<0.05 Bonferroni corrected for N=8; Figure 4C). Within strategies tests (Mann-Whitney test within strategy, p<0.05; Figure 4C) showed that users found attempted body movement, visual imagery and counting backwards significantly more enjoyable than caregivers and researchers, and that users found attempted speech, visual P300, SSVEP and auditory P300 significantly more enjoyable than researchers.
Figure 4 – Comparison between users’, caregivers’ and researchers’ opinion about mental strategies.
A) Center-of-mass (COM) values computed for the top 4 mental strategies for users, caregivers and researchers. Note that caregivers rank their preference from their own perspective (as an abled control group), whereas researchers ranked from the perspective of the users. Monte Carlo variance is indicated on the top right corner of each panel and at each caregiver/research bar of which the difference with the user bar is larger or smaller than the Monte Carlo variance (0.28). Ranking scales ranged from 1 (least preferred) to 4 (most preferred). B-C) Percent of participants that rated each strategy (in a 5-points Likert scale) according to how easy (B) and how enjoyable (C) it is. The charts position the % of replies vertically such that positive responses are stacked above the horizontal baseline (0%) and negative responses are stacked below the baseline. The ‘neutral’ is centered around 0%. Mental strategies highlighted in gray showed a statistically significant difference between groups (Kruskal Wallis test, p < 0.05, Bonferroni corrected for 8 repetitions). For the strategies with significant difference between groups, pair-wise Mann-Whitney tests were used to test which groups were statistically different between users and researchers or caregivers (* < 0.05).
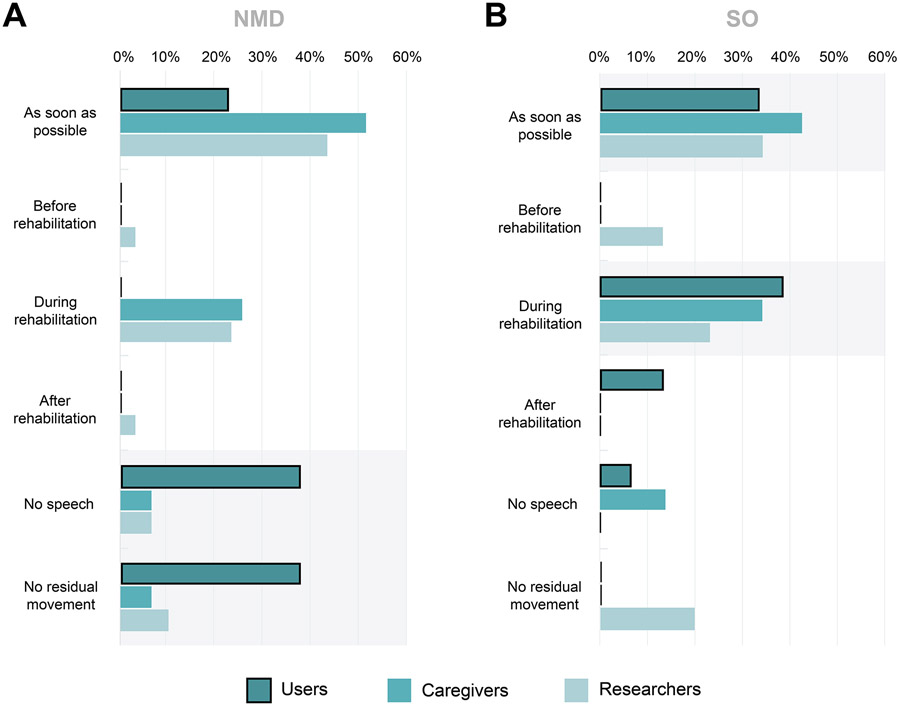
3.4. Time of information
Caregivers and researchers agreed that information about ATs and cBCIs should be provided to users ‘as soon as possible’ after the diagnose of LIS, irrespective of the etiology (Figure 5A-B). However, users of the NMD group (Figure 5A) indicated they would only like to be informed when they have lost the ability to speak or press a button.
Figure 5 – Results of time of AT information ratings.
Opinion of participants (in percentage) per group (users, caregivers and researchers) about the timing of information delivery on AT and cBCIs for people with LIS due to neuromuscular disorder (A: NMD) or sudden onset (B: SO).
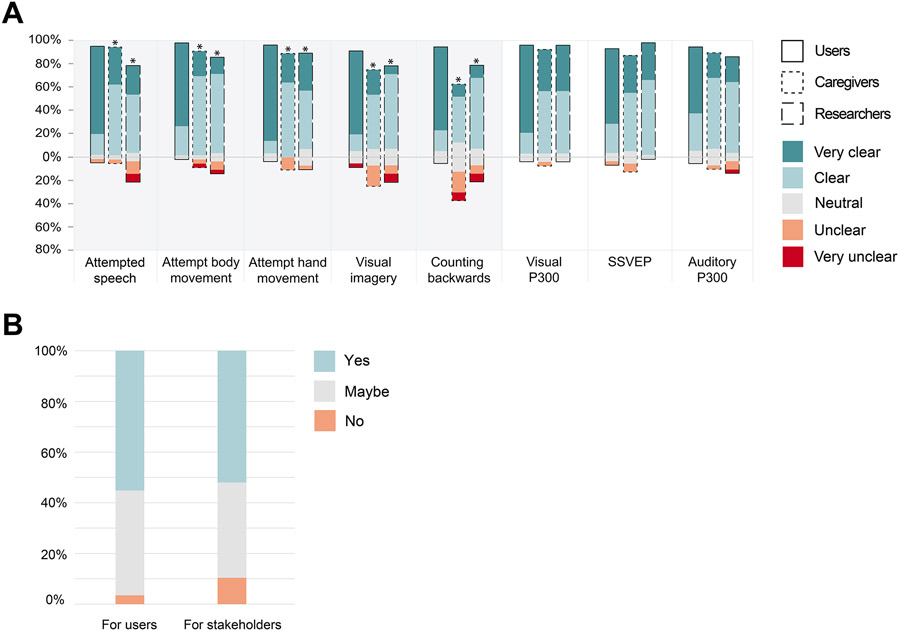
3.5. Animation videos
Overall, users rated the animation videos explaining each strategy as very clear (Figure 6A). Both caregivers and researchers found the videos explaining attempted speech, attempted body and hand movement, visual imagery and counting backwards significantly less clear than the users (Kruskal Wallis test for 3 groups and 8 strategies, p<0.05 Bonferroni corrected for N=8; Mann-Whitney test within strategy, p<0.05). Furthermore, researchers assessed the overall clarity of all 9 videos (Figure 6B). The majority of the researchers indicated that these provided a ‘clear’ introduction and explanation of cBCIs and mental strategies for end-users (55%) and other stakeholders (52%). Most of the participants who replied with ‘maybe’ to this question indicated that the videos were sometimes too simple and could contain more detailed information.
Figure 6 – Animation videos feedback from users, caregivers and researchers.
A) The three respondent groups (users, caregiver and researchers) rated the animation videos introducing each mental strategy according to how clear it was, using a 5-points Likert scale. Videos on mental strategies highlighted in gray showed a statistically significant difference between groups (Kruskal Wallis test, p<0.05, Bonferroni corrected for 8 repetitions). For the strategies with a significant difference between groups, pair-wise Mann-Whitney tests were used to test which groups (caregivers/researchers) were statistically different from the users (* < 0.05). B) Percent of researchers that reported that the animation videos were a clear (or not) means to introduce cBCIs and mental strategies to user and other stakeholders (Yes = clear; No = not clear).
4. Discussion
In this study we compared the opinions of individuals with LIS with those of caregivers and of researchers working in the field of cBCI. Overall, caregivers and researchers ranked the importance of different cBCI applications similar to users, but disagreed with the users regarding preferred mental strategies and timing of being informed with respect to etiology.
4.1. Preferred applications
The self-evident strong preference for direct and private communication by the users has been previously reported in 4. Here we show that priorities of cBCI applications are consistent between users, the ones who provide daily care and the ones who develop the technology, demonstrating that caregivers and researchers are able to estimate these priorities well. We found that ‘emotions and facial expressions’ and ‘artistic expression’ were the least preferred applications, and that the frequency of use of these applications was overestimated by the caregivers and researchers. This result contrasts that of previous studies that suggested that artistic expression is an important BCI tool for individuals with severe paralysis (e.g., 15-19). One could argue that such application is not provided by all current communication aids, whereas communication is a universally used concept. We also show that while the top applications were currently used by more than 90% of the users at home, a smaller number of caregivers and researchers selected these as essential to be provided by a cBCI. This discrepancy could be the result of a comparison between current (users) and future (caregivers, researchers) situations.
4.2. Preferred mental strategies
To our knowledge this is the first study to compare the preference of multiple mental strategies for BCI control between potential end-users, an able-bodied control group (caregivers) and researchers developing BCIs based on these strategies. We show that preferences of users for certain mental strategies are often not aligned with the opinion of caregivers and the expectations of researchers. In fact, caregivers and researchers were unable to estimate or predict the users’ opinion about attempted body and hand movement, visual imagery and evoked stimuli. Interestingly, discrepancies between individuals with LIS and other stakeholders have been reported before, regarding for example the quality-of-life rating of individuals with LIS. Whereas healthy individuals, medical professionals and caregivers sometimes assume that the quality of life of an individual with LIS is low and not worth living for 20, the quality of life as rated by individuals with LIS is often reported to be comparable to that of healthy groups 20-23. With respect to the current study, it should be noted that the overestimation of the visual P300 strategy by the researchers could be explained by the fact that 74% of the researchers participating in this study investigate and develop visual P300 paradigms 19,24-29.
4.3. Time of information
Users, irrespective of their etiology, expressed a preference to be informed about AT and BCIS when they reach the locked-in state 14. This moment is especially relevant for users diagnosed with NMD, where the locked-in state is typically reached in later stages of the disease progression. This choice contrasts with that of caregivers and researchers, who estimated that users with NMD would like to be informed as soon as possible after being diagnosed. The discrepancy between groups is in line with findings regarding timing of information related to prognostics and end-of-life communication for individuals with advanced late-stage illnesses, such as metastatic diseases and ALS 30-32. Factors such as the patients’ acceptance of their medical diagnosis, can play an important role in the readiness of the patient to receive information. Indeed, several studies with patients with metastatic diseases showed that patients rather not discuss end-of-life or palliative care at the time of diagnosis and that, as the illness progresses, caregivers seemed to want more information about clinical treatment options than patients 30. Similarly, it has been reported that individuals with ALS experience difficulties in coming to terms with the diagnosis and adjust to disease progression, and that clinicians and patients diverge with respect to how patients perceive and comprehend their condition 32. Discrepancies between patients and health professionals have been further systematically described in 31, where the authors report that health professionals tend to overestimate the awareness of the patients regarding their prognosis and that patients should be given the option to defer the discussion of prognosis and end-of-life decisions to later time points in the clinical trajectory, although these results may depend on the country and culture. Yet, some participants also preferred to be informed as soon as possible. A similar dichotomous finding was recently also reported in a study with individuals with ALS 33, illustrating that ideal timing of information is highly subject specific. Indeed, while researchers, caregivers and clinicians should be sensitive to the opinion of end-users, there are some arguments for not waiting too long with providing information. These arguments include sufficient time for learning how to use the technology (training time) and avoiding last-minute (urgent) decisions for one or another AT solution.
4.4. Animation videos
The videos used in this study to introduce and explain the concept of cBCI and mental strategies were positively rated by the three groups, and in particular by the users. Indeed, the added value of animations to explain complex health information has been reported before (e.g., 34), supporting the notion that animations are an effective tool for providing information to individuals, independent of their level of health literacy. Although some researchers indicated that the animations should provide more detailed information about the technology, we wanted to use the same questions and videos for all three groups, specifically accommodating users and caregivers who we reasoned may be confused by more complex or detailed videos.
4.5. Limitations and future directions
The researchers group comprised individuals from several research institutes in multiple countries, whereas the samples of users and caregivers were limited to the Dutch population. These differences in location may be associated with cultural differences that yield differences in opinion. Based on the current results, we believe a larger replication study with users and caregivers from multiple countries could provide insight in the effect of cultural factors. Furthermore, a previous study has suggested that the decision about AT implementation needs to be shared between the user and health care professional 35. However, the opinion (and acceptance) of health care providers regarding cBCIs is still largely unknown.
5. Conclusion
The opinion of prospective users regarding BCIs for communication was compared with the one of their respective caregivers and cBCI researchers. We showed that, even though users, caregivers and researchers agree on which communication outputs have the highest priority for cBCI, they disagree on which mental strategies are preferred for cBCI control and on the time point at which AT and cBCIs should be introduced to users with NMD. The misalignment in opinions of groups strengthens the argument for a user-centered design approach in the BCI field.
Supplementary Material
Implications for rehabilitation:
Brain-Computer Interfaces may offer people with severe motor impairment a brain-based and muscle-independent approach to control communication-technology. The successful development of communication BCIs (cBCIs) relies on a close collaboration between end-users and other stakeholders, such as caregivers and researchers.
Our work reveals that people with locked-in syndrome (end-users), their caregivers and researchers developing cBCIs agree that direct and private forms of communication are the most desired cBCI applications, but disagree regarding the preferred mental strategies for cBCI control and when to be informed about cBCIs.
Animation videos are an effective tool for providing information to individuals, independent of their level of health literacy, regarding the concept of cBCIs and mental strategies for control.
The misalignment in opinions of different groups of stakeholders about cBCIs strengthens the argument for a user-centered design approach in the development of cBCIs and access technology designed for daily life usage.
Acknowledgements
The authors thank the participants for their time and motivation to answer the questionnaire, Merel Horsmeier for designing and producing the animation videos, Wesley Sewnundun for implementing the questionnaire in Qualtrics, and Ruben Sars for his help during the home-visits and in distributing the questionnaire to the caregivers. This research was funded by the ERC-Advanced ‘iConnect’ project (grant ADV 320708) (NFR), Dutch Technology Foundation STW NeuroCIMT project (grant 14906) (NFR) and the National Institute On Deafness And Other Communication Disorders of the National Institutes of Health (U01DC016686) (NFR).
Footnotes
Conflicts of interest: We have no Conflict of Interest
Data Availability
The animation videos used in the questionnaires (Video 1 – Video 9; translated to English) are available at https://doi.org/10.5281/zenodo.3271440. The BCI researchers’ questionnaire (in English) is available in Supplementary Materials. The Users’ and Caregivers’ questionnaires (Dutch only) and data that support the findings can be made available upon reasonable request to the authors.
References
- 1.Tai K, Blain S, Chau T. A Review of Emerging Access Technologies for Individuals With Severe Motor Impairments. Assist Technol. 2008;20(4):204–221. doi: 10.1080/10400435.2008.10131947 [DOI] [PubMed] [Google Scholar]
- 2.Bernat JL. Medical Decision Making by Patients in the Locked-in Syndrome. Neuroethics. Published online March 14, 2018:1–10. doi: 10.1007/s12152-018-9358-7 [DOI] [Google Scholar]
- 3.Brunner C, Birbaumer N, Blankertz B, et al. BNCI Horizon 2020: towards a roadmap for the BCI community. Brain-Comput Interfaces. 2015;2(1):1–10. doi: 10.1080/2326263X.2015.1008956 [DOI] [Google Scholar]
- 4.Huggins JE, Wren PA, Gruis KL. What would brain-computer interface users want? Opinions and priorities of potential users with amyotrophic lateral sclerosis. Amyotroph Lateral Scler. 2011;12(5):318–324. doi: 10.3109/17482968.2011.572978 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Basha D, Dostrovsky JO, Lopez Rios AL, Hodaie M, Lozano AM, Hutchison WD. Beta oscillatory neurons in the motor thalamus of movement disorder and pain patients. Exp Neurol. 2014;261:782–790. doi: 10.1016/j.expneurol.2014.08.024 [DOI] [PubMed] [Google Scholar]
- 6.Blain-Moraes S, Schaff R, Gruis KL, Huggins JE, Wren PA. Barriers to and mediators of brain–computer interface user acceptance: focus group findings. Ergonomics. 2012;55(5):516–525. doi: 10.1080/00140139.2012.661082 [DOI] [PubMed] [Google Scholar]
- 7.Schicktanz S, Amelung T, Rieger JW. Qualitative assessment of patients’ attitudes and expectations toward BCIs and implications for future technology development. Front Syst Neurosci. 2015;9. doi: 10.3389/fnsys.2015.00064 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lahr J, Schwartz C, Heimbach B, Aertsen A, Rickert J, Ball T. Invasive brain–machine interfaces: a survey of paralyzed patients’ attitudes, knowledge and methods of information retrieval. J Neural Eng. 2015;12(4):043001. doi: 10.1088/1741-2560/12/4/043001 [DOI] [PubMed] [Google Scholar]
- 9.Blabe CH, Gilja V, Chestek CA, Shenoy KV, Anderson KD, Henderson JM. Assessment of brain–machine interfaces from the perspective of people with paralysis. J Neural Eng. 2015;12(4):043002. doi: 10.1088/1741-2560/12/4/043002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Huggins JE, Moinuddin AA, Chiodo AE, Wren PA. What Would Brain-Computer Interface Users Want: Opinions and Priorities of Potential Users With Spinal Cord Injury. Arch Phys Med Rehabil. 2015;96(3, Supplement):S38–S45.e5. doi: 10.1016/j.apmr.2014.05.028 [DOI] [PubMed] [Google Scholar]
- 11.Fager SK, Fried-Oken M, Jakobs T, Beukelman DR. New and emerging access technologies for adults with complex communication needs and severe motor impairments: State of the science. Augment Altern Commun. 2019;0(0):1–13. doi: 10.1080/07434618.2018.1556730 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Andresen EM, Fried-Oken M, Peters B, Patrick DL. Initial constructs for patient-centered outcome measures to evaluate brain–computer interfaces. Disabil Rehabil Assist Technol. 2016;11(7):548–557. doi: 10.3109/17483107.2015.1027298 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Nijboer F, Bos DP-O, Blokland Y, van Wijk R, Farquhar J. Design requirements and potential target users for brain-computer interfaces – recommendations from rehabilitation professionals. Brain-Comput Interfaces. 2014;1(1):50–61. doi: 10.1080/2326263X.2013.877210 [DOI] [Google Scholar]
- 14.Branco MP, Pels EGM, Sars RH, et al. Brain-Computer Interfaces for Communication: Preferences of Individuals With Locked-in Syndrome. Neurorehabil Neural Repair. Published online February 3, 2021:1545968321989331. doi: 10.1177/1545968321989331 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Muenssinger JI, Halder S, Kleih SC, et al. Brain Painting: First Evaluation of a New Brain–Computer Interface Application with ALS-Patients and Healthy Volunteers. Front Neurosci. 2010;4. doi: 10.3389/fnins.2010.00182 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Zickler C, Halder S, Kleih SC, Herbert C, Kübler A. Brain Painting: Usability testing according to the user-centered design in end users with severe motor paralysis. Artif Intell Med. 2013;59(2):99–110. doi: 10.1016/j.artmed.2013.08.003 [DOI] [PubMed] [Google Scholar]
- 17.Botrel L, Holz EM, Kübler A. Brain Painting V2: evaluation of P300-based brain-computer interface for creative expression by an end-user following the user-centered design. Brain-Comput Interfaces. 2015;2(2-3):135–149. doi: 10.1080/2326263X.2015.1100038 [DOI] [Google Scholar]
- 18.Holz EM, Botrel L, Kübler A. Independent home use of Brain Painting improves quality of life of two artists in the locked-in state diagnosed with amyotrophic lateral sclerosis. Brain-Comput Interfaces. 2015;2(2-3):117–134. doi: 10.1080/2326263X.2015.1100048 [DOI] [Google Scholar]
- 19.Botrel L, Holz EM, Kübler A. Using Brain Painting at Home for 5 Years: Stability of the P300 During Prolonged BCI Usage by Two End-Users with ALS. In: Schmorrow DD, Fidopiastis CM, eds. Augmented Cognition. Enhancing Cognition and Behavior in Complex Human Environments. Lecture Notes in Computer Science. Springer International Publishing; 2017:282–292. [Google Scholar]
- 20.Laureys S, Pellas F, Van Eeckhout P, et al. The locked-in syndrome : what is it like to be conscious but paralyzed and voiceless? In: Laureys S, ed. Progress in Brain Research. Vol 150. The Boundaries of Consciousness: Neurobiology and Neuropathology. Elsevier; 2005:495–611. doi: 10.1016/S0079-6123(05)50034-7 [DOI] [PubMed] [Google Scholar]
- 21.Kübler A, Nijboer F, Mellinger J, et al. Patients with ALS can use sensorimotor rhythms to operate a brain-computer interface. Neurology. 2005;64(10):1775–1777. doi: 10.1212/01.WNL.0000158616.43002.6D [DOI] [PubMed] [Google Scholar]
- 22.Bruno M-A, Bernheim JL, Ledoux D, Pellas F, Demertzi A, Laureys S. A survey on self-assessed well-being in a cohort of chronic locked-in syndrome patients: happy majority, miserable minority. BMJ Open. 2011;1(1):e000039. doi: 10.1136/bmjopen-2010-000039 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Rousseau M-C, Baumstarck K, Alessandrini M, Blandin V, Billette de Villemeur T, Auquier P. Quality of life in patients with locked-in syndrome: Evolution over a 6-year period. Orphanet J Rare Dis. 2015;10:88. doi: 10.1186/s13023-015-0304-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Sellers EW, Donchin E. A P300-based brain–computer interface: Initial tests by ALS patients. Clin Neurophysiol. 2006;117(3):538–548. doi: 10.1016/j.clinph.2005.06.027 [DOI] [PubMed] [Google Scholar]
- 25.Kübler, Furdea A, Halder S, Hammer EM, Nijboer F, Kotchoubey BA Brain–Computer Interface Controlled Auditory Event-Related Potential (P300) Spelling System for Locked-In Patients. Ann N Y Acad Sci. 2009;1157(1):90–100. doi: 10.1111/j.1749-6632.2008.04122.x [DOI] [PubMed] [Google Scholar]
- 26.Pires G, Nunes U, Castelo-Branco M. Statistical spatial filtering for a P300-based BCI: Tests in able-bodied, and patients with cerebral palsy and amyotrophic lateral sclerosis. J Neurosci Methods. 2011;195(2):270–281. doi: 10.1016/j.jneumeth.2010.11.016 [DOI] [PubMed] [Google Scholar]
- 27.Brunner P, Ritaccio AL, Emrich JF, Bischof H, Schalk G. Rapid Communication with a “P300” Matrix Speller Using Electrocorticographic Signals (ECoG). Front Neurosci. 2011;5. doi: 10.3389/fnins.2011.00005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Vansteensel MJ, Kristo G, Aarnoutse EJ, Ramsey NF. The brain-computer interface researcher’s questionnaire: from research to application. Brain-Comput Interfaces. 2017;4(4):236–247. doi: 10.1080/2326263X.2017.1366237 [DOI] [Google Scholar]
- 29.Wolpaw JR, Bedlack RS, Reda DJ, et al. Independent home use of a brain-computer interface by people with amyotrophic lateral sclerosis. Neurology. 2018;91(3):e258–e267. doi: 10.1212/WNL.0000000000005812 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Parker SM, Clayton JM, Hancock K, et al. A Systematic Review of Prognostic/End-of-Life Communication with Adults in the Advanced Stages of a Life-Limiting Illness: Patient/Caregiver Preferences for the Content, Style, and Timing of Information. J Pain Symptom Manage. 2007;34(1):81–93. doi: 10.1016/j.jpainsymman.2006.09.035 [DOI] [PubMed] [Google Scholar]
- 31.Hancock K, Clayton JM, Parker SM, et al. Discrepant Perceptions About End-of-Life Communication: A Systematic Review. J Pain Symptom Manage. 2007;34(2):190–200. doi: 10.1016/j.jpainsymman.2006.11.009 [DOI] [PubMed] [Google Scholar]
- 32.Hogden A, Greenfield D, Nugus P, Kiernan MC. Engaging in patient decision-making in multidisciplinary care for amyotrophic lateral sclerosis: the views of health professionals. Patient Prefer Adherence. 2012;6:691–701. doi: 10.2147/PPA.S36759 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Versalovic E, Diamond M, Klein E. “Re-identifying yourself”: a qualitative study of veteran views on implantable BCI for mobility and communication in ALS. Disabil Rehabil Assist Technol. Published online September 17, 2020:1–8. doi: 10.1080/17483107.2020.1817991 [DOI] [PubMed] [Google Scholar]
- 34.Ahmed E, Alike Q, Keselman A. The Process of Creating Online Animated Videos to Overcome Literacy Barriers in Health Information Outreach. J Consum Health Internet. 2015;19(3-4):184–199. doi: 10.1080/15398285.2015.1089395 [DOI] [Google Scholar]
- 35.Johnston P, Currie LM, Drynan D, Stainton T, Jongbloed L. Getting it “right”: how collaborative relationships between people with disabilities and professionals can lead to the acquisition of needed assistive technology. Disabil Rehabil Assist Technol. 2014;9(5):421–431. doi: 10.3109/17483107.2014.900574 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The animation videos used in the questionnaires (Video 1 – Video 9; translated to English) are available at https://doi.org/10.5281/zenodo.3271440. The BCI researchers’ questionnaire (in English) is available in Supplementary Materials. The Users’ and Caregivers’ questionnaires (Dutch only) and data that support the findings can be made available upon reasonable request to the authors.