Abstract
Background
Throughout the coronavirus disease 2019 (COVID-19) pandemic, not only medical personnel but also paramedics or emergency medical technicians (EMT) have faced multiple physical and psychological challenges while performing their duties. The current study aimed to evaluate the psychological effects of managing patients with COVID-19 on the paramedics and EMT.
Materials and Methods
A survey targeting paramedics and EMT in Korea was conducted in December 2020. An official letter requesting participation and with the link to an online-based survey was sent to the Public Emergency Medical Services. Only one response was accepted from each participant.
Results
A total of 326 paramedics and EMT responded to the survey. Among them, 66.3% (216/326) had experience in managing patients with COVID-19. No differences in the distribution of sex, age, working area, duration of working experience, and underlying comorbidities were observed between those who did (COVID-19 group) and did not (non-COVID-19 group) experience managing patients with COVID-19. The percentage of participants who showed severe posttraumatic stress disorder (PTSD) symptoms was significantly higher in the COVID group than in the non-COVID group (11.1% vs. 3.6%, P = 0.029). The participants in the COVID group had a significantly higher mean Global Assessment of Recent Stress Scale score than those in the non-COVID group (18.7 ± 11.1 vs. 16.1 ± 9.9, P = 0.042). The proportion of paramedics and EMT willing to leave their job if given a chance was higher in the COVID group than the non-COVID group (24.1% vs. 9.1%, P = 0.001). Additionally, paramedics and EMT in the COVID group tended to show concern regarding exposure to COVID-19 infection.
Conclusion
The experience of managing patients with COVID-19 resulted in psychological distress among paramedics and EMT in Korea.
Keywords: COVID-19, Psychological distress, Paramedics, EMT, Korea
Introduction
Since its emergence in China in late December 2019, the coronavirus disease 2019 (COVID-19) has spread rapidly across countries, causing an unprecedented pandemic [1]. In Korea, the first patient confirmed to have COVID-19, who entered from Wuhan, China, was detected in mid-January, 2020, after which a large-scale outbreak occurred in Daegu and surrounding areas, becoming one of the first countries to have been affected by the pandemic [2,3].
In response to the pandemic, professionals from several fields have been engaged in COVID-19-related work. In addition to being a medical professional in the hospital, paramedics or emergency medical technicians (EMT) have been directly engaging with patients with COVID-19 since the beginning of the pandemic. In Korea, paramedics and EMT belong to the Public Emergency Medical Services and are mainly performing jobs that are associated with patient transfer during emergencies. As such, paramedics and EMT have been tasked with the transfer of COVID-19-confirmed patients between the community and hospitals or among hospitals during the pandemic [3].
Given the highly contagious nature of COVID-19, frontline professionals might perceive the threat of COVID-19 contagion during the management of suspected or confirmed cases, resulting in psychological distress [4,5]. With the continuation of the COVID-19 outbreak for about 1 year, not only medical personnel but also paramedics or EMT have faced multiple physical and psychological challenges while carrying out their duties. However, studies regarding psychological effects among paramedics or EMT, who have played a pivotal role in response to the pandemic, have been limited in Korea. The current study, therefore, aimed to evaluate the psychological effects of managing patients with COVID-19 in paramedics and EMT. Furthermore, differences in psychological effects experienced by paramedics and EMT according to their experience of managing patients with COVID-19 were evaluated.
Material and methods
1. Study design
This study was performed as a part of project ‘health impact assessment of health care workers undertaking COVID-19 treatment and management in Korea’. Because 1,000 to 1,500 samples are considered the optimal balance for accuracy and economic feasibility in a public opinion poll, the survey targeted a total of 1,500 health care workers [6]. Of them, 300 samples were allocated for paramedics and EMT, considering the number of COVID-19 response workers in September 2020.
The survey started to conduct on December 4, 2020. An official letter requesting participation that included a link to the online-based survey was sent to the Public Emergency Medical Services, who then distributed the link to the fire departments of each province. The number of respondents was monitored daily and the survey was finished on the day the collected responses exceeded 300. Only one response was accepted from each participant. The respondents were then divided according to whether or not they had experience in managing patients with COVID-19, and the psychological effects were compared.
2. Ethics statement
The study protocol was approved by the Public Institutional Review Board Designated by the Ministry of Health and Welfare (IRB number: P01-202011-23-001). Written informed consent was obtained from each participant via online participation.
3. Survey items
The questionnaire consisted of five sections: (1) baseline characteristics of the respondents, (2) experience in the management of patients with COVID-19, (3) mental health after the COVID-19 pandemic, (4) perception of COVID-19-related work, and (5) job satisfaction and required support. The following scales were used for measuring the emotional and psychological status of the respondents: primary care posttraumatic stress disorder screening for DSM-5, Insomnia severity index, global assessment of recent stress scale (GARS), Oldenburg burnout inventory, patient health questionnaire-9, and generalized anxiety disorder-7. Total scores were utilized for the interpretation of each scale, and cutoff values were defined as described previously [7,8,9,10,11].
Items regarding the perception of COVID-19-related work were developed based on previous questionnaires used for measuring the psychological effects in health care workers during previous outbreaks of severe acute respiratory syndrome and Middle East respiratory syndrome [12,13], and items belonging to concerns regarding COVID-19-related work were measured using a 5-point Likert scale. For the five factors included in “required support,” the respondents determined the priority order according to the importance of each factor. The factors were calculated using a priority weighing method (1st place, 5 points; 2nd, 4 points; 3rd, 3 points; 4th, 2 points; 5th, 1 point) (Supplementary File 1). The continuous variables in the present study were presented as mean ± standard deviation.
4. Statistical analysis
R software version 4.0.4 (R Foundation for Statistical Computing, Vienna, Austria) was used for statistical analysis. Categorical variables were analyzed using the chi-square test or Fisher’s exact test, as appropriate. Student’s t-test or Welch's t-test was used for continuous variables. A two-tailed P value of <0.05 was considered statistically significant.
Results
1. Basic characteristics of respondents
On December 29, 2020, the number of responses reached the targeted amount. A total of 326 paramedics and EMT responded to the survey. Among them, 66.3% (216/326) had experience in managing patients with COVID-19. The overall characteristics of the respondents are detailed in Table 1. Among the respondents, 32.8% were female, and the majority were under the age of 40 (88.3%). Furthermore, most of the respondents had worked as paramedics and EMT for 15 years or less (94.1%). No differences in the distribution of sex, age, and length of working experience were observed between those who did (COVID-19 group) and did not (non-COVID-19 group) experience managing patients with COVID-19.
Table 1. Baseline characteristics of the respondents.
| Total (n = 326) | Experience in managing COVID-19 patients (n = 216) | No experience in managing COVID-19 patients (n = 110) | P-value | |||
|---|---|---|---|---|---|---|
| Female Sex | 107 (32.8) | 67 (31.0) | 40 (36.4) | 0.331 | ||
| Age | ||||||
| <30 | 92 (28.2) | 62 (28.7) | 30 (27.3) | 0.309 | ||
| 30 - 39 | 196 (60.1) | 132 (61.1) | 64 (58.2) | - | ||
| 40 - 49 | 35 (10.7) | 19 (8.8) | 16 (14.6) | - | ||
| 50 - 59 | 3 (0.9) | 3 (1.4) | 0 (0.0) | - | ||
| ≥60 | 0 (0.0) | 0 (0.0) | 0 (0.0) | - | ||
| Length of working experience, years | ||||||
| <5 | 197 (60.4) | 134 (62.0) | 63 (57.3) | 0.603 | ||
| 6 - 15 | 110 (33.7) | 71 (32.9) | 39 (35.5) | - | ||
| ≥16 | 19 (5.8) | 11 (5.1) | 8 (7.3) | - | ||
| Working area | ||||||
| Metropolitan area | 111 (34.1) | 92 (42.6) | 19 (17.3) | <0.001 | ||
| Gangwon Province | 15 (4.6) | 7 (3.2) | 8 (7.3) | - | ||
| Chungcheong Province | 59 (18.1) | 42 (19.4) | 17 (15.5) | - | ||
| Jeolla Province | 66 (20.3) | 28 (13.0) | 38 (34.6) | - | ||
| Gyeongsang Province | 70 (21.5) | 45 (20.8) | 25 (22.7) | - | ||
| Jeju Province | 5 (1.5) | 2 (0.9) | 3 (2.7) | - | ||
| Residence type, during the COVID-19 outbreaka | ||||||
| Living with family members | 257 (78.8) | 172 (79.6) | 85 (77.3) | 0.622 | ||
| Living with non-family members | 2 (0.6) | 2 (0.9) | 0 (0.0) | 0.552 | ||
| Living alone | 76 (23.3) | 51 (23.6) | 25 (22.7) | 0.858 | ||
| Underlying comorbidities | ||||||
| Existence of physical illnesses | 71 (21.8) | 49 (22.7) | 22 (20.0) | 0.579 | ||
| Hypertension | 7 (2.2) | 4 (1.9) | 3 (2.7) | 0.692 | ||
| Diabetes | 2 (0.6) | 2 (0.9) | 0 (0.0) | 0.551 | ||
| Hyperlipidemia | 3 (0.9) | 2 (0.9) | 1 (0.9) | 1.000 | ||
| Chronic liver disease | 4 (1.2) | 2 (0.9) | 2 (1.8) | 0.606 | ||
| Chronic heart disease | 3 (0.9) | 1 (0.5) | 2 (1.8) | 0.264 | ||
| Chronic pulmonary disease | 1 (0.3) | 1 (0.5) | 0 (0.0) | 1.000 | ||
| Malignancy | 1 (0.3) | 0 (0.0) | 1 (0.9) | 0.337 | ||
| Musculoskeletal disorder | 59 (18.1) | 44 (20.4) | 15 (13.6) | 0.135 | ||
| Existence of mental illnesses | 7 (2.1) | 4 (1.9) | 3 (2.7) | 0.692 | ||
| Depression | 1 (0.3) | 1 (0.5) | 0 (0.0) | 1.000 | ||
| Anxiety | 4 (1.2) | 2 (0.9) | 2 (1.8) | 0.606 | ||
| Insomnia | 3 (0.9) | 2 (0.9) | 1 (0.9) | 1.000 | ||
Values are presented as number (%).
aThis question requested the respondent to select multiple items.
COVID-19, coronavirus disease 2019.
Most of the respondents (78.8%) were living with family members during the COVID-19 outbreak. Approximately 20.0% and 2.0% of the respondents had physical and mental illnesses, respectively. No difference in the underlying comorbidities was observed between the COVID-19 and non-COVID-19 group.
2. Experience in the management of patients with COVID-19
Table 2 summarizes the COVID-19 group's experience in the management of patients with COVID-19. Among the 216 respondents in the COVID-19 group, 52.8% managed ≤5 patients with COVID-19, whereas 14.8% managed >20 patients. Moreover, 71.7% and 15.3% participated in patient management for <15 days and ≥90 days, respectively. The proportion of respondents who managed patients with psychiatric problems or those on mechanical ventilation or extracorporeal membrane oxygenation was 8.3% for each. Approximately 60.0% of the respondents in the COVID group checked the vital signs and took the history of patients with COVID-19, while approximately 30.0% of them performed a physical examination. Almost all respondents (97.2%) completed training for the use of personal protective equipment (PPE); however, some respondents had experience in not using certain PPE during the management of patients with COVID-19.
Table 2. Experience related to the management of COVID-19 patients.
| Total (n = 216) | Managing COVID-19 patients <15 days (n = 155) | Managing COVID-19 patients ≥5 days (n = 61) | P-value | ||
|---|---|---|---|---|---|
| No. of managed COVID-19 patients | |||||
| 1 - 5 | 114 (52.8) | 102 (65.8) | 12 (19.7) | <0.001 | |
| 6 - 10 | 47 (21.8) | 39 (25.2) | 8 (13.1) | - | |
| 11 - 20 | 23 (10.7) | 7 (4.5) | 16 (26.2) | - | |
| ≥21 | 32 (14.8) | 7 (4.5) | 25 (41.0) | - | |
| Days of participating in the management of COVID-19 patients | |||||
| <15 | 155 (71.7) | - | - | - | |
| 15 - 89 | 28 (13.0) | - | - | - | |
| ≥90 | 33 (15.3) | - | - | - | |
| Patients typea | |||||
| Smoker | 33 (15.3) | 20 (12.9) | 13 (21.3) | 0.122 | |
| Dementia | 23 (10.7) | 15 (9.7) | 8 (13.1) | 0.461 | |
| Having psychiatric problems | 18 (8.3) | 11 (7.1) | 7 (11.5) | 0.295 | |
| Ventilator or ECMO therapy | 18 (8.3) | 10 (6.5) | 8 (13.1) | 0.111 | |
| Range of COVID-19 managementa | |||||
| Checking vital signs | 126 (58.3) | 86 (55.5) | 40 (65.6) | 0.176 | |
| History taking | 130 (60.2) | 86 (55.5) | 44 (72.1) | 0.024 | |
| Physical examination | 60 (27.8) | 39 (25.2) | 21 (34.4) | 0.171 | |
| Positional changes | 13 (6.0) | 7 (4.5) | 6 (9.8) | 0.200 | |
| Establishing vascular access | 3 (1.4) | 2 (1.3) | 0 (0.0) | 1.000 | |
| Disposal of corpse | 1 (0.5) | 1 (0.6) | 0 (0.0) | 1.000 | |
| Experience with managing MERS patients | 29 (13.4) | 17 (11.0) | 12 (19.7) | 0.091 | |
| Completion of training on the use of personal protective equipment for the management of COVID-19 patients | 210 (97.2) | 149 (96.1) | 61 (100.0) | 0.188 | |
| Experience with not using personal protective equipment during the management of COVID-19 patients | |||||
| Gloves | 0 (0.0) | 0 (0.0) | 0 (0.0) | - | |
| Disposable gown | 5 (2.3) | 3 (1.9) | 2 (3.3) | 0.371 | |
| Goggles or other eye protection | 7 (3.2) | 5 (3.2) | 2 (3.3) | 1.000 | |
| N95 respirator | 3 (1.4) | 3 (1.9) | 0 (0.0) | 0.483 | |
| Cover all | 2 (0.9) | 1 (0.6) | 1 (1.6) | 0.096 | |
| Experience with COVID-19-associated symptoms | 62 (28.7) | 42 (27.1) | 20 (32.8) | 0.405 | |
| Experience with isolation due to contact with COVID-19 patients | 53 (24.6) | 37 (23.9) | 16 (26.2) | 0.717 | |
| Difficulties with COVID-19-related work | |||||
| Fear for the possibility of COVID-19 infection | 182 (84.3) | 126 (81.3) | 56 (91.8) | 0.056 | |
| The stigma of being a healthcare worker and the feeling of sorry for the family | 157 (72.7) | 106 (68.4) | 51 (83.6) | 0.024 | |
| Work-related conflicts among colleagues | 107 (49.5) | 74 (47.7) | 33 (54.1) | 0.400 | |
| Responsibility for patient care | 117 (54.2) | 75 (48.4) | 42 (68.9) | 0.007 | |
Values are presented as number (%).
aThis question requested the respondent to select multiple items.
COVID-19, coronavirus disease 2019; ECMO, extracorporeal membrane oxygenation; MERS, Middle-East respiratory syndrome.
A total of 62 (28.7%) and 53 (24.6%) respondents had experience with COVID-19-associated symptoms and with isolation due to contact with patients with COVID-19, respectively. The proportion of respondents with each experience was significantly higher in the COVID-19 than in the non-COVID-19 group (COVID-19 associated symptom, 28.7% vs. 16.4%, P = 0.014; isolation due to contact with patients with COVID-19, 24.5% vs. 12.7%, P = 0.013). Two respondents were contracted COVID-19 but it was unclear whether the transmission is related to occupational exposure.
Regarding difficulties with COVID-19-related work, 84.3% of the respondents feared the possibility of COVID-19 infection, whereas 72.7% of them experienced stigma related to being a health care worker and felt apologetic toward their family. Paramedics and EMT who managed COVID-19 patients for 15 days or more showed a higher rate of experiencing fear of the possibility of COVID-19 infection, the stigma of being a healthcare worker, and feeling of sorry for the family, and responsibility for patient care than those who managed COVID-19 patients for lesser than 15 days.
3. Mental health after COVID-19 pandemic
The mental health status of the respondents after the COVID-19 pandemic is described in Table 3. Psychiatric symptoms, such as depression, anxiety, and insomnia, had developed or aggravated in 5 - 20% of the respondents. However, no significant difference was observed between the COVID-19 and non-COVID-19 groups. In comparison, the proportion of paramedics and EMT who showed severe posttraumatic stress disorder symptoms was significantly higher in the COVID-19 group than in the non-COVID-19 group (11.1% vs. 3.6%, P = 0.029). Furthermore, the participants in the COVID-19 group had significantly higher mean scores for GARS than those in the non-COVID-19 group (18.7 ± 11.1 vs. 16.1 ± 9.9, P = 0.042). A total of 241 (73.9%) respondents experienced exhaustion, with no difference between the COVID-19 and non-COVID-19 groups (76.9% vs. 68.2%, P = 0.092).
Table 3. Mental health after the COVID-19 pandemic.
| Total (n = 326) | Experience in managing COVID-19 patients (n = 216) | No experience in managing COVID-19 patients (n = 110) | P-value | ||
|---|---|---|---|---|---|
| Development or aggravation of psychiatric symptoms | |||||
| Depression | 46 (14.1) | 33 (15.3) | 13 (11.8) | 0.396 | |
| Anxiety | 64 (19.6) | 49 (22.7) | 15 (13.6) | 0.052 | |
| Insomnia | 52 (16.0) | 36 (16.7) | 16 (14.6) | 0.621 | |
| Decreased concentration, memory | 45 (13.8) | 33 (15.3) | 12 (10.9) | 0.280 | |
| Anger | 51 (15.6) | 36 (16.7) | 15 (13.6) | 0.476 | |
| Excessive drinking | 17 (5.2) | 10 (4.6) | 7 (6.4) | 0.506 | |
| Exhaustion | 46 (14.1) | 32 (14.8) | 14 (12.7) | 0.609 | |
| Guilty feeling | 17 (5.2) | 14 (6.5) | 3 (2.7) | 0.149 | |
| PC-PTSD-5 | |||||
| Normal, 0 - 1 point | 279 (85.6) | 177 (81.9) | 102 (92.7) | 0.029 | |
| Mild to moderate, 2 points | 19 (5.8) | 15 (6.9) | 4 (3.6) | - | |
| Severe, ≥3 points | 28 (8.6) | 24 (11.1) | 4 (3.6) | - | |
| ISI | |||||
| Normal, <8 points | 140 (42.9) | 82 (38.0) | 58 (52.7) | 0.063 | |
| Mild, 8 - 14 points | 130 (40.0) | 91 (42.1) | 39 (35.5) | - | |
| Moderate, 15 - 21 points | 48 (14.7) | 37 (17.1) | 11 (10.0) | - | |
| Severe, 22 - 28 points | 8 (2.5) | 6 (2.8) | 2 (1.8) | - | |
| GARS | 17.8 ± 10.8 | 18.7 ± 11.1 | 16.1 ± 9.9 | 0.042 | |
| OLBI | |||||
| Disengagement, ≥16.8 points | 273 (83.7) | 181 (83.8) | 92 (83.6) | 0.970 | |
| Exhaustion, ≥18 points | 241 (73.9) | 166 (76.9) | 75 (68.2) | 0.092 | |
Values are presented as number (%) or mean ± standard deviation.
COVID-19, coronavirus disease 2019; PC-PTSD-5, primary care PTSD screening for DSM-5; ISI, insomnia severity index; GARS, global assessment of recent stress scale; OLBI, Oldenburg burnout inventory.
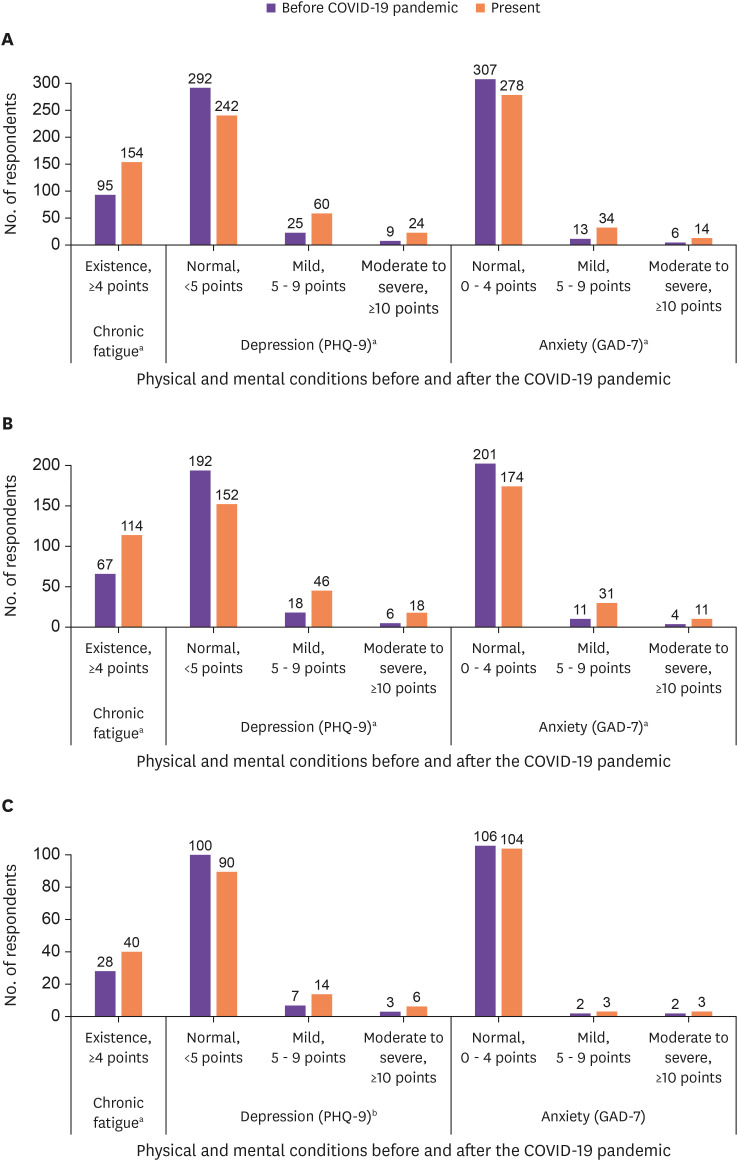
On comparing the physical and mental conditions before and after the COVID-19 pandemic, respondents tended to have chronic fatigue, depression, and anxiety after the COVID-19 pandemic. Such tendencies were observed in both the COVID-19 and non-COVID-19 groups (Fig. 1).
Figure 1. Comparison of the physical and mental conditions before and after the COVID-19 pandemic.
(A) Total (n = 326), (B) Experience in managing the COVID-19 patients (n = 216), (C) No experience in managing the COVID-19 patients (n = 110).
aP value <0.001, bP value <0.05.
COVID-19, coronavirus disease 2019; PHQ-9, patient health questionnaire-9; GAD-7, generalized anxiety disorder-7.
4. Perception of COVID-19-related work
Table 4 shows the respondents’ perception of COVID-19-related work. Overall, paramedics and EMT in the COVID-19 group tended to show more concern regarding COVID-19-related work compared to those in the non-COVID-19 group. Notably, they felt more stress at work (3.1 ± 1.1 vs. 2.8 ± 1.0, P = 0.006), they were more afraid they would contract COVID-19 (3.2 ± 1.2 vs. 3.0 ± 1.1, P = 0.042), they were more afraid of infecting others with COVID-19 (3.3 ± 1.3 vs. 3.0 ± 1.2, P = 0.014), and they were more concerned that their family and friends were worried about getting infected by them (3.1 ± 1.3 vs. 2.7 ± 1.3, P = 0.009).
Table 4. Perception of COVID-19 related work.
| Total (n = 326) | Experience in managing COVID-19 patients (n = 216) | No experience in managing COVID-19 patients (n = 110) | P-value | ||
|---|---|---|---|---|---|
| Concerns regarding COVID-19-related worka | |||||
| My job put me in danger | 3.3 ± 1.1 | 3.3 ± 1.1 | 3.2 ± 1.0 | 0.231 | |
| I feel more stress at work | 3.0 ± 1.1 | 3.1 ± 1.1 | 2.8 ± 1.0 | 0.006 | |
| I accept the risks of taking care of COVID-19 patients | 2.3 ± 0.9 | 2.4 ± 0.9 | 2.2 ± 0.7 | 0.091 | |
| I’m afraid I’ll get sick from COVID-19 | 3.1 ± 1.2 | 3.2 ± 1.2 | 3.0 ± 1.1 | 0.042 | |
| I have little control over the problem of getting myself infected or not | 2.4 ± 1.0 | 2.4 ± 1.0 | 2.3 ± 0.8 | 0.083 | |
| If I were infected with COVID-19, survival chances would be low | 1.7 ± 0.8 | 1.7 ± 0.8 | 1.8 ± 0.8 | 0.765 | |
| I think about my resignation because of COVID-19 | 1.5 ± 0.7 | 1.6 ± 0.7 | 1.4 ± 0.6 | 0.070 | |
| I’m afraid I’ll infect others with COVID-19 | 3.2 ± 1.3 | 3.3 ± 1.3 | 3.0 ± 1.2 | 0.014 | |
| My family and friends are worried about getting infected by me | 3.0 ± 1.3 | 3.1 ± 1.3 | 2.7 ± 1.3 | 0.009 | |
| People avoid my family because of my job | 1.9 ± 0.9 | 1.9 ± 1.0 | 1.8 ± 0.8 | 0.192 | |
| Rights and obligations about COVID-19-related work | |||||
| Health care workers are obligated to take care of patients during public health crises by emerging infectious diseases | 311 (95.4) | 208 (96.3) | 103 (93.6) | 0.278 | |
| Health care workers’ care obligation may be suspended or reduced depending on conditions | 262 (80.4) | 176 (81.5) | 86 (78.2) | 0.043 | |
| Health care workers have the right to control their working conditions during a public health crisis by emerging infectious diseases | 250 (76.7) | 170 (78.7) | 80 (72.7) | 0.228 | |
| Having experienced conflicts between the obligation to care for patients and health risks or family sacrifices | 156 (47.9) | 112 (51.9) | 44 (40.0) | ||
Values are presented as number (%) or mean ± standard deviation.
aEach item was measured using a 5-point Likert scale (1 = strongly disagree, 2 = disagree, 3 = neither disagree nor agree, 4 = agree, 5 = strongly agree).
COVID-19, coronavirus disease 2019.
Almost all respondents thought that health care workers were obligated to take care of patients during a public health crisis caused by emerging infectious diseases (95.4%) and that health care workers’ care obligation may be suspended or reduced depending on conditions (80.4%).
5. Job satisfaction and required support
The proportion of respondents who were unsatisfied with their job was 11.3%, with no difference between the COVID-19 and non-COVID-19 groups. The proportion of paramedics and EMT willing to leave their job if given a chance was higher in the COVID-19 group than the non-COVID-19 group (24.1% vs. 9.1%, P = 0.001).
The most required support was a reinforcement of rewards, followed by priority support for health care and establishing a peer support system (Table 5).
Table 5. Job satisfaction and required support.
| Total (n = 326) | Experience in managing COVID-19 patients (n = 216) | No experience in managing COVID-19 patients (n = 110) | P-value | ||
|---|---|---|---|---|---|
| Job satisfaction | |||||
| Unsatisfied | 37 (11.3) | 28 (13.0) | 9 (8.2) | 0.327 | |
| Moderate | 127 (39.0) | 84 (38.9) | 43 (39.1) | - | |
| Satisfied | 162 (49.7) | 104 (48.1) | 58 (52.7) | - | |
| Turnover intention | |||||
| I want to quit my current job | 24 (7.4) | 19 (8.8) | 5 (4.6) | 0.165 | |
| If I have a chance to change jobs, I’ll leave | 62 (19.0) | 52 (24.1) | 10 (9.1) | 0.001 | |
| Actively looking for another job | 8 (2.5) | 7 (3.2) | 1 (0.9) | 0.275 | |
| Required supporta | |||||
| Reinforcement of rewards | 3.6 ± 1.3 | 3.7 ± 1.3 | 3.4 ± 1.5 | 0.085 | |
| Priority support for healthcare | 3.5 ± 1.5 | 3.5 ± 1.5 | 3.4 ± 1.5 | 0.625 | |
| Establishing a peer support system | 2.8 ± 1.4 | 2.6 ± 1.4 | 3.1 ± 1.3 | 0.004 | |
| Regular education about COVID-19 related issues | 2.7 ± 1.2 | 2.7 ± 1.2 | 2.7 ± 1.3 | 0.830 | |
| Establishment and operation of the mental health support team in the institution | 2.5 ± 1.2 | 2.5 ± 1.2 | 2.4 ± 1.3 | 0.687 | |
Values are presented as number (%) or mean ± standard deviation.
aThe factors were calculated using a priority weighing method (1st place, 5 points; 2nd, 4 points; 3rd, 3 points; 4th, 2 points; 5th, 1 point).
COVID-19, coronavirus disease 2019.
Discussion
The current study found that psychological distress among paramedics and EMT in Korea had aggravated during the COVID-19 pandemic and that those who had experience in managing patients with COVID-19 had more severe psychological distress than those who did not. Surprisingly, more than 70.0% of the respondents felt exhaustion. The results of our study highlighted that the COVID-19 pandemic negatively impacted the mental health of paramedics and EMT throughout Korea.
The psychological impact of the COVID-19 pandemic on health care professionals has been well evaluated in several studies. Accordingly, the common finding was that the COVID-19 pandemic had a destructive impact on health care workers’ mental well-being [5,14,15]. According to a study in the United States, health care workers that contracted COVID-19 demonstrated higher levels of depression, anxiety, and burnout [14]. Like other countries, Korean health care workers in the hospital, including physicians, nurses, and administrative workers, have been experiencing high levels of emotional stress during the pandemic [16]. Interestingly, nurses and auxiliary staff who participated in the COVID-19 patient care had more distress from the pandemic situation than physicians in the Korean hospital environment [16]. Moreover, a study revealed that emergency workers in Korea, including paramedics and EMT, were suffering from psychological problems, such as depression and sleep disorders [17]. This study revealed that there were emotional distresses among paramedics and EMT in Korea during the COVID-19 pandemic, similar to other health care professionals.
We found that majority of the paramedics and EMT who were involved in the management of patients with COVID-19 had difficulty in dealing with the fear associated with contracting COVID-19 infection. In fact, previous studies have indicated that the potential factors affecting the mental health of health care workers during the pandemic might include high workload, lack of experience, and fear of contracting COVID-19 infection. A cross-sectional study in Singapore reported that prolonged shifts (≥8 h) and being redeployed were significantly associated with burnout [18]. Another study conducted in Vietnam found that <1 of year experience in the medical field, inadequate PPE in the workplace, working in the department directly in contact with the COVID-19 patient, etc., were the significant factors associated with psychological problems [19]. According to a qualitative study in Korea, the emotional stress experienced by health care workers during the pandemic was attributable to not only increased workloads but also fear of contracting infection and lifestyle changes [20].
Interestingly, the stigma of being a health care worker and feeling apologetic for the family were major difficulties experienced by paramedics and EMT in Korea engaged in COVID-19-related work. Unfortunately, there was excessive fear of COVID-19 transmission among the general population in Korea, especially in the early phase of the COVID-19 outbreak, and several people avoided crowded places or personal meetings due to the possibility of contact with patients with COVID-19. As such, some irrational people had stigmatized even health care workers or their families and kept away from them. To prevent such irrationality from repeating, it will be necessary to provide accurate information regarding the disease to the public and promote social campaigns to prevent stigmatization of certain groups during the pandemic.
Professionals working at the frontline of the pandemic might be at a higher vulnerability to mental health problems than other professionals given that they are directly engaged with treating infected patients despite the risk of contracting COVID-19 [21]. Indeed, health care workers who come in contact with patients at the frontline, before the infection is confirmed, are more vulnerable to contract COVID-19 and show more psychological distress compared to other health care professionals [14,22]. A previous study in Korea found that approximately 90.0% of infectious diseases physicians, another profession working at the frontlines, showed burnout, and only 40.0% of them were satisfied with their job [5]. The situation seems to be similar for paramedics and EMT, with 76.9% of the COVID-19 group feeling exhausted and 24.1% of them wanting to leave their job if given the chance. Considering that the loss of workforce would amplify the burden on the remaining workers, prompting them to quit their job and therefore creating a vicious cycle, the Korean society should pay attention to the results of our study and should endeavor to address the exhaustion perceived by the workforce essential to combat against the pandemic and ensure the continuity of their function. As shown in the present study, reinforcement of rewards might be the most urgent improvement that would help paramedics and EMT directly cope with the COVID-19 pandemic. In fact, a cross-sectional study in Israel found that inappropriate compensation for hard work and lack of opportunities for promotion were crucial factors in the decision to leave among paramedics and EMT [23]. Prioritizing support for health care workers, especially mental health aid, is another aspect that should be considered. Given that the current pandemic has lasted longer than initially expected and that health care workers have been experiencing a wide range of emotional stress, such support might be crucial for sustaining workers and aiding their ability to cope throughout the duration of the pandemic [24].
This study has some potential limitations worth noting. First, selection bias could not be avoided given that the survey was conducted based on a first-come, first-served approach and the respondents might have had more interest in the study than those who did not respond. Moreover, there is the possibility that respondents included those who are familiar with computers or smartphones, given that the responses were collected using an online-based platform. Second, the survey period might have affected the results of the survey. In fact, December 2020 was in the middle of the third wave of the COVID-19 pandemic in Korea and paramedics and EMT might have had higher workloads and more stress compared to other periods [25]. Finally, stressful conditions other than the COVID-19 pandemic were not considered in this study and there is the possibility that some variables were affected not by the pandemic, but by other conditions. However, given the fact that the whole society was focused on the countermeasure to the COVID-19 pandemic, there was a low possibility of existing other stressful tasks comparable to the pandemic during the study period.
In conclusion, the experience of managing patients with COVID-19 resulted in psychological distress for paramedics and EMT in Korea. The Korean society should consider the results of our study and should endeavor to establish appropriate support for the paramedics and EMT managing patients with COVID-19.
ACKNOWLEDGMENTS
We appreciate Boyoung Shim, Eunbi Park, and Juhwan Jeong for their devoted work for this research.
Footnotes
Funding: This research was supported by a grant of the Korea Health Technology R&D Project through the Korea Health Industry Development Institute (KHIDI), funded by the Ministry of Health & Welfare, Korea (grant number: HC20C0003). The funder of the study had no role in conducting the study, data analysis, or writing of this manuscript.
Conflict of Interest: No conflict of interest.
- Conceptulization: KTK.
- Data curation: BK, KTK.
- Formal analysis: BK, KTK.
- Funding acquisition: KTK.
- Investigation: All authors.
- Methodology: All authors.
- Project administration: KTK.
- Resources: All authors.
- Software: BK, KTK.
- Supervision: KTK.
- Validation: All authors.
- Visualization: BK.
- Writing – original draft: BK.
- Writing – review & editing: BK, KTK.
SUPPLEMENTARY MATERIAL
A questionnaire for healthcare workers responding to the COVID-19 outbreak
References
- 1.Chen N, Zhou M, Dong X, Qu J, Gong F, Han Y, Qiu Y, Wang J, Liu Y, Wei Y, Xia J, Yu T, Zhang X, Zhang L. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet. 2020;395:507–513. doi: 10.1016/S0140-6736(20)30211-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kim JY, Choe PG, Oh Y, Oh KJ, Kim J, Park SJ, Park JH, Na HK, Oh MD. The first case of 2019 novel coronavirus pneumonia imported into Korea from Wuhan, China: Implication for infection prevention and control measures. J Korean Med Sci. 2020;35:e61. doi: 10.3346/jkms.2020.35.e61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Choi WS, Kim HS, Kim B, Nam S, Sohn JW. Community treatment centers for isolation of asymptomatic and mildly symptomatic patients with coronavirus disease, South Korea. Emerg Infect Dis. 2020;26:2338–2345. doi: 10.3201/eid2610.201539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Shahzad F, Du J, Khan I, Fateh A, Shahbaz M, Abbas A, Wattoo MU. Perceived threat of COVID-19 contagion and frontline paramedics’ agonistic behaviour: Employing a stressor-strain-outcome perspective. Int J Environ Res Public Health. 2020;17:5102. doi: 10.3390/ijerph17145102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Park SY, Kim B, Jung DS, Jung SI, Oh WS, Kim SW, Peck KR, Chang HH Korean Society of Infectious Diseases. Psychological distress among infectious disease physicians during the response to the COVID-19 outbreak in the Republic of Korea. BMC Public Health. 2020;20:1811. doi: 10.1186/s12889-020-09886-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Scheaffer RL, Mendenhall W, 3rd, Ott RL, Gerow KG. Elementary survey sampling. 7th ed. Boston, MA: Brooks/Cole; 2012. [Google Scholar]
- 7.Jung YE, Kim D, Kim WH, Roh D, Chae JH, Park JE. A Brief screening tool for PTSD: Validation of the Korean version of the primary care PTSD screen for DSM-5 (K-PC-PTSD-5) J Korean Med Sci. 2018;33:e338. doi: 10.3346/jkms.2018.33.e338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bastien CH, Vallières A, Morin CM. Validation of the Insomnia Severity Index as an outcome measure for insomnia research. Sleep Med. 2001;2:297–307. doi: 10.1016/s1389-9457(00)00065-4. [DOI] [PubMed] [Google Scholar]
- 9.Peterson U, Demerouti E, Bergström G, Åsberg M, Nygren Å. Work characteristics and sickness absence in burnout and nonburnout groups: A study of Swedish health care workers. Int J Stress Manag. 2008;15:153–172. [Google Scholar]
- 10.Chung K, Park JY, Joung D, Jhung K. Response time as an implicit self-schema indicator for depression among undergraduate students: Preliminary findings from a mobile app-based depression assessment. JMIR Mhealth Uhealth. 2019;7:e14657. doi: 10.2196/14657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Spitzer RL, Kroenke K, Williams JB, Löwe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. 2006;166:1092–1097. doi: 10.1001/archinte.166.10.1092. [DOI] [PubMed] [Google Scholar]
- 12.Chong MY, Wang WC, Hsieh WC, Lee CY, Chiu NM, Yeh WC, Huang OL, Wen JK, Chen CL. Psychological impact of severe acute respiratory syndrome on health workers in a tertiary hospital. Br J Psychiatry. 2004;185:127–133. doi: 10.1192/bjp.185.2.127. [DOI] [PubMed] [Google Scholar]
- 13.Um DH, Kim JS, Lee HW, Lee SH. Psychological effects on medical doctors from the Middle East respiratory syndrome (MERS) outbreak: A comparison of whether they worked at the MERS occurred hospital or not, and whether they participated in MERS diagnosis and treatment. J Korean Neuropsychiatr Assoc. 2017;56:28–34. [Google Scholar]
- 14.Firew T, Sano ED, Lee JW, Flores S, Lang K, Salman K, Greene MC, Chang BP. Protecting the front line: a cross-sectional survey analysis of the occupational factors contributing to healthcare workers’ infection and psychological distress during the COVID-19 pandemic in the USA. BMJ Open. 2020;10:e042752. doi: 10.1136/bmjopen-2020-042752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Vanhaecht K, Seys D, Bruyneel L, Cox B, Kaesemans G, Cloet M, Van Den Broeck K, Cools O, De Witte A, Lowet K, Hellings J, Bilsen J, Lemmens G, Claes S. COVID-19 is having a destructive impact on health-care workers’ mental well-being. Int J Qual Health Care. 2021;33:mzaa158. doi: 10.1093/intqhc/mzaa158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Jo SH, Koo BH, Seo WS, Yun SH, Kim HG. The psychological impact of the coronavirus disease pandemic on hospital workers in Daegu, South Korea. Compr Psychiatry. 2020;103:152213. doi: 10.1016/j.comppsych.2020.152213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Choi MY. Mental and physical factors influencing wellbeing among South Korean emergency workers. Int J Environ Res Public Health. 2020;18:70. doi: 10.3390/ijerph18010070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Tan BYQ, Kanneganti A, Lim LJH, Tan M, Chua YX, Tan L, Sia CH, Denning M, Goh ET, Purkayastha S, Kinross J, Sim K, Chan YH, Ooi SBS. Burnout and associated factors among health care workers in Singapore during the COVID-19 pandemic. J Am Med Dir Assoc. 2020;21:1751–8.e5. doi: 10.1016/j.jamda.2020.09.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Tuan NQ, Phuong ND, Co DX, Son DN, Chinh LQ, Dung NH, Thach PT, Thai NQ, Thu TA, Tuan NA, San BV, Tung VS, An NV, Khanh DN, Long VH, Tai N, Muoi T, Vinh ND, Thien NT, Nhan LD, Tuan NV. Prevalence and factors associated with psychological problems of healthcare workforce in Vietnam: Findings from COVID-19 hotspots in the national second wave. Healthcare (Basel) 2021;9:718. doi: 10.3390/healthcare9060718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lee JY, Lee JY, Lee SH, Kim J, Park HY, Kim Y, Kwon KT. The experiences of health care workers during the COVID-19 pandemic in Korea: a qualitative study. J Korean Med Sci. 2021;36:e170. doi: 10.3346/jkms.2021.36.e170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Awais SB, Martins RS, Khan MS. Paramedics in pandemics: protecting the mental wellness of those behind enemy lines. Br J Psychiatry. 2021;218:75–76. doi: 10.1192/bjp.2020.193. [DOI] [PubMed] [Google Scholar]
- 22.Wang W, Song W, Xia Z, He Y, Tang L, Hou J, Lei S. Sleep disturbance and psychological profiles of medical staff and non-medical staff during the early outbreak of COVID-19 in Hubei Province, China. Front Psychiatry. 2020;11:733. doi: 10.3389/fpsyt.2020.00733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Dopelt K, Wacht O, Strugo R, Miller R, Kushnir T. Factors that affect Israeli paramedics’ decision to quit the profession: a mixed methods study. Isr J Health Policy Res. 2019;8:78. doi: 10.1186/s13584-019-0346-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Eftekhar Ardebili M, Naserbakht M, Bernstein C, Alazmani-Noodeh F, Hakimi H, Ranjbar H. Healthcare providers experience of working during the COVID-19 pandemic: A qualitative study. Am J Infect Control. 2021;49:547–554. doi: 10.1016/j.ajic.2020.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Seong H, Hyun HJ, Yun JG, Noh JY, Cheong HJ, Kim WJ, Song JY. Comparison of the second and third waves of the COVID-19 pandemic in South Korea: Importance of early public health intervention. Int J Infect Dis. 2021;104:742–745. doi: 10.1016/j.ijid.2021.02.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
A questionnaire for healthcare workers responding to the COVID-19 outbreak