Abstract
Purpose
This study aimed to evaluate the level of treatment adherence and identify predictors of adherence in glaucoma patients during the coronavirus disease 2019 (COVID-19) pandemic in Zagreb, Croatia.
Methods
The cross-sectional study was conducted among primary open-angle glaucoma (POAG) patients at the Department of Ophthalmology, University Hospital Centre Zagreb, between 1st April 2020 and 1st April 2021. The sociodemographic data, clinical, and drug information were recorded. The treatment adherence was assessed through a self-administered questionnaire, the Culig Adherence Scale (CAS). Statistical analyses were performed using TIBCO Statistica™ 14.0.0.
Results
113 POAG patients (48M/65F) with a mean age of 65.89 ± 8.53 years were included in this study. According to the CAS, only 39.8% of patients adhered to topical glaucoma treatment. Educational level was positively related to adherence to treatment (p = 0.022). The main predictors for adherence were the patients' positive attitude towards the drug's effect, family support, and good relationship with the healthcare providers (p < 0.05, respectively). The majority of patients stated forgetfulness as the main reason for skipping drug dosing.
Conclusions
Non-adherence to treatment was prevalent among patients with POAG during the COVID-19 pandemic in Zagreb, Croatia. Personal beliefs and attitudes towards treatment, family support, and patient-healthcare provider relationship were significant predictors of adherence. Special consideration should be given to the whole health system-level strategies targeting the adherence to treatment, especially in crises, in order to achieve positive therapeutic outcomes.
The study protocol was registered in the DRKS - German Clinical Trials Register, DRKS-ID: DRKS00022081.
Keywords: Glaucoma, adherence to treatment, COVID-19, predictors, questionnaire
Introduction
Glaucoma is the leading cause of permanent vision impairment worldwide. The entity describes a multifactorial and heterogeneous group of clinical conditions that cause glaucomatous optic neuropathy and consecutive visual field (VF) loss.1 The most common type of glaucoma is primary open-angle glaucoma (POAG).1 Until today, there is no clearly defined cure for glaucoma. However, randomized clinical trials have consistently shown that a reduction of IOP decreases the risk of disease progression.2,3 Current glaucoma guidelines recommend ocular medication in the form of drops as a first-line treatment for patients diagnosed with POAG.1 In addition, the long-term periodical follow-ups to evaluate IOP, VF, and optic nerve head are essential parts of glaucoma care.1 Thus, adherence is considered a crucial component of lifelong glaucoma management due to the chronic course of the disease.1
Adherence is a multidimensional phenomenon, defined as “the extent to which a person's behaviour in taking medication corresponds with agreed recommendations from a healthcare provider in dosage, time, and frequency of drug administration”.4 Evidence indicates that patient adherence to antiglaucoma management is far from optimal, and multiple barriers have been identified so far.5,6 Considering the significant association between poor medication adherence and glaucomatous loss of visual function over time, the persistence in glaucoma self-management is crucial.7 Non-adherence to glaucoma management is directly related to lack of IOP control, inducing POAG-related VF loss, functional disabilities, and consequent decreased vision-related quality of life, as well as increased treatment costs.3,8,9 Therefore, it has been emphasized as a major health and economic problem.5,6
In the light of the public health crisis caused by the rapid spread of the novel coronavirus SARS-CoV-2 (Severe Acute Respiratory Syndrome Coronavirus-2), the World Health Organization (WHO) declared it a pandemic in March 2020.10 The first COVID-19 (coronavirus disease 2019) case in Zagreb, Croatia, was registered on 25th February 2020.11 Three weeks later, to safeguard public health, the Croatian Government had introduced preventative measures which included ‘stay at home’ messages, schools shut-down, travel restrictions, physical distancing requirements and adaptation of health care delivery to the perceived needs of the pandemic. Moreover, in the middle of the crisis caused by the COVID-19 pandemic, Zagreb region was hit by two major earthquakes in the last 140 years, which also raised population concerns.12,13
During the COVID-19 outbreak, unprecedented circumstances had placed a heavy burden on the health care system globally. The particularly vulnerable groups have been the elderly and persons with various chronic illnesses, regarding a higher risk of morbidity and mortality.14 Since efforts of the health care system have been focused on the prevention and management of infection, the continuity of treatment of various chronic diseases has been indirectly compromised.15,16 In particular, challenges have been posed in providing proper and regular ophthalmic care.17,18 In response to COVID-19 at our Clinic, we have implemented all measures according to the current guidelines that allowed us to maintain the integrity of our health systems and take continuous ophthalmic care of the patients while minimizing the threat of SARS-CoV-2 spread.19,20 However, according to the author's observations, the hospital outpatient activity decreased by a third during the first year of the pandemic.
Moreover, emerging evidence suggests that the pandemic has indubitably disrupted health behaviour among glaucoma patients worldwide.18,21–25 In particular, the patients' adherence has been adversely influenced, exacerbating already known barriers and manifesting new problems specific for the continuous period.21,24
Concerning the pandemic-related problems, this study was conducted to assess the treatment adherence and identify the predictors of adherence among glaucoma patients treated at Zagreb University Hospital Center during the COVID-19 outbreak. The study's secondary goal was to determine the main reasons for non-adherence to glaucoma treatment.
Materials and methods
This cross-sectional study was approved by the Ethics Committee of the University Hospital Centre Zagreb (class 8.1-20/65, reference number 2/02/21 AG), and it was carried out in line with the Helsinki Declaration. The participants included in the study had been duly informed about the study and signed written informed consent.
The study was conducted between 1st April 2020 and 1st April 2021 at the Department of Ophthalmology, Zagreb University Hospital Center in Zagreb, Croatia, which provides public tertiary health care. Patients were selected consecutively during routine clinical outpatient glaucoma practice.
The target population included patients diagnosed with POAG aged 18 years or older. POAG was based on criteria for diagnosis setting: IOP values from medical history higher than 21 mmHg, presence of an open angle on gonioscopy, typical glaucomatous disc cupping, and compatible VF defects. All patients had been prescribed topical hypotensive therapy for at least one year.
Patients who were not eligible to participate in this study were patients with other glaucoma types or other eye diseases and patients with VF defects caused by other systemic diseases. Patients with more than 10% of unanswered points in questionnaires were excluded.
All patients underwent comprehensive ophthalmologic examinations, including best-corrected visual acuity (BCVA) using the Snellen chart, slit-lamp biomicroscopy, gonioscopy, and dilated fundus examination. IOP was measured using a Goldmann applanation tonometer.
Patients were provided with two self-administered surveys conducted anonymously.
The general data survey assessed sociodemographic data, including gender, age, education level, living conditions, and marital status; clinical information, including duration of POAG, family history of glaucoma, systemic comorbidities, and information about antiglaucoma and systemic medications.
Medication adherence was evaluated using the Culig Adherence Scale (CAS), the valid and reliable self-administered instrument consisting of 68 items divided into nine parts. Each section contains questions related to the possible factors that may influence treatment adherence, including patients' attitudes and beliefs about the therapy, the influence of patient's family and environment, patients' relationships with the doctor and pharmacist regarding treatment, symptoms of depression and anxiety, patient's habits (physical activity and alcohol consumption) and the impact of adverse effects of medication. The information about the reasons for non-adherence was also evaluated. The patient's adherence was defined by detecting the frequency of missed application of the prescribed medications. The possible answers were “I never forget to take my medication,” “I forget to take my medication during the last week, last month, last 1–3 months, and more than the last three months.” According to the answer to this item, patients were divided into two groups. Those who answered with “never forget” were considered adherent, while all other respondents were non-adherent. The psychometric properties of the questionnaires were previously confirmed in the Croatian population (Cronbach's alpha coefficient was 0.94).26
Statistical analysis was performed using TIBCO Statistica™ 14.0.0. The normality of data distribution was tested by the Kolmogorov-Smirnov or Shapiro-Wilk test, and the homogeneity of variance by the Leven test Results of descriptive analyses were expressed as means ± SD for continuous variables and numbers (percentages) for categorical variables. The Kendall's tau correlation test was used to evaluate the direction of associations, and binary logistic regression analysis was used to assess their strength and independence. In all analyses, a p-value < 0.05 was considered statistically significant.
Results
Out of 120 patients recruited on the inclusion visit, 7 (5,8%) were excluded due to more than 10% unanswered points in questionnaires. Therefore, the data from 113 POAG patients (48 male / 65 female), with a mean age of 65.89 ± 8.53 years, who met all study criteria were processed and analysed.
Their sociodemographic data and clinical information are presented in Table 1. Most of the patients graduated high school (48.6%), lived in a family (78.5%), and were married (76%). Most of the patients had glaucoma for more than five years (72.6%), had a negative family history of glaucoma (72.6%), and used only one antiglaucoma medication (74.3%). 75.7% of included patients also had systemic comorbidities and used systemic therapy.
Table 1.
Sociodemographic data, clinical and drug information of patients with primary open-angle glaucoma included in the study (n = 113).
| Level of education | 10.1% primary school |
48.6% high school |
16.5% collage |
20.2% faculty |
4.6% PhD |
|---|---|---|---|---|---|
| Living conditions | 21.5% alone |
78.5% in a family |
|||
| Marital status | 76% married |
3.8% divorced |
6.7% single |
||
| Duration of glaucoma | 3.5% < 2 years |
23.9% 2–5 years |
72.6% > 5 years |
||
| Family history of glaucoma | 27.4% positive |
72.6% negative |
|||
| Number of antiglaucoma medications | 74.3% one |
21.2% two |
4.4% three |
||
| Systemic comorbidities and therapy |
75.7% yes |
24.3% no |
According to the CAS, only 45 (39.8%) patients were adherent to topical glaucoma. In the non-adherent group (60.2%), 7 (10.3%) patients claimed not to take medication last week, 35 (51.5%) last month, 19 (27.9%) last 1–3 months, and 7 (10.3%) patients did not take it more than last three months.
The adherence to topical glaucoma treatment was significantly positively correlated with the educational level (p = 0.022), while marginally negatively with a positive family history of glaucoma (p = 0.057) and the number of antiglaucoma medications (p = 0.058) (Table 2). No correlation was found between the adherence to the treatment and gender (p = 0.947), age (p = 0.252), living conditions (p = 0.379), marital status (p = 0.695), duration of POAG (p = 0.688), and the prevalence of systemic comorbidities and systemic therapy (p = 0.473) (data not shown).
Table 2.
Correlations between the adherence to topical glaucoma treatment, educational level, and clinical data.
| Adherence to the topical glaucoma treatment | |||
|---|---|---|---|
| Kendall Tau | Z | P | |
| Educational level | 0.148 | 2.2844 | 0.022 |
| Family history of glaucoma | −0.125 | −1.896 | 0.057 |
| Number of antiglaucoma medications | −0.122 | −1.818 | 0.058 |
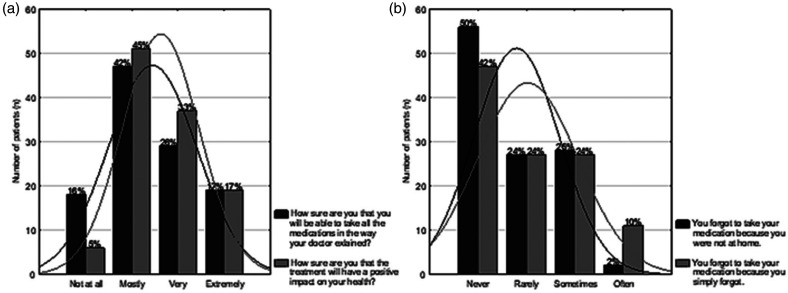
Regarding the attitude towards antiglaucoma treatment, 48 (43%) patients were very sure that they would be able to take medications as agreed with doctor, 47 (41%) were mainly sure, and 18 (16%) of them were not at all sure of taking the prescribed medications properly (Figure 1(A)). 95% of patients were very or mostly certain that the treatment would positively impact their health, while only 5% were not sure of the treatment's positive effect (Figure 1(A)). 32% of patients reported the symptoms of a bad mood, and 23% of them the symptoms of anxiety. Regarding the patient's habits, the results showed a lack of physical activity (only 13% of patients exercised regularly) and alcohol consumption practice (21% of patients drank every day or three to four times a week).
Figure 1.
a. Attitude towards antiglaucoma treatment. b. Main reasons for non-adherence.
The two main reasons for non-adherence were forgetfulness (58%) and not being at home (50%) (Figure 1(B)). 18% of patients sometimes or rarely skipped their treatment because of fear of an adverse effect of medications.
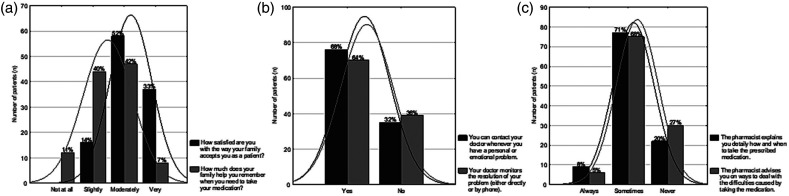
Figure 2 (A, B, and C). present the attitude and affection of patients' families, doctors, and pharmacists towards their disease treatment. 37 (33%) patients were very satisfied with the way their family accepted them as a patient, while 76 (67%) of them were slightly or moderately satisfied with the family acceptance (Figure 2(A)). 89% of family members moderately, or very much helped the patients remember to take their medications. In comparison, 11% of family members did not support the patients in taking the prescribed medication (Figure 2(A)). 77 (68%) of patients could contact their doctors whenever they had a problem, and 72 (64%) of doctors monitored the resolution of patients' problems (Figure 2(B)). 90 (80%) pharmacists explained to the patients detailly how and when to take the prescribed medication, and 82 (73%) of them advised the patients how to deal with the difficulties caused by taking the medication (Figure 2(C)).
Figure 2.
Attitude and affection of the family (a), the doctor (b), and the pharmacist (c) towards the disease treatment.
Table 3. presents the main predictors for adherence to the topical glaucoma treatment using univariate logistic regression analyses. The patient's self-assurance of ability to take the medication as agreed with the doctors, positive attitude towards the therapy, family support, and good relationship with the caregiver are the leading and statistically significant predictors of adherence (p < 0.05).
Table 3.
Predictors for adherence to the topical glaucoma treatment using univariate logistic regression analyses.
| OR (95% CI) | p | |
|---|---|---|
| Self-assurance of ability to take the medication in the way agreed with the doctor | 2.27 (1.44–3.59) | <0.001 |
| Positive attitude to the cure effect of medication | 2.48 (1.47–4.17) | <0.001 |
| Family acceptance of the patient's disease | 3.27 (1.66–6.43) | <0.001 |
| Family help with taking the medication | 2.68 (1.50–4.80) | <0.001 |
| Possibility to contact the doctor whenever is needed | 20.38 (4.48–92.65) | <0.001 |
| Feeling comfortable when asking the doctor about any problem | 4.10 (1.79–9.35) | <0.001 |
| The pharmacist's interest if the patient is taking the medication for the first time | 4.27 (1.85–9.86) | <0.001 |
| The pharmacist's explanation of why it is crucial to take the medication regularly | 2.46 (1.29–4.70) | 0.006 |
| Pharmacist's detailed advice on how and when to take the medication | 3.76 (1.51–9,37) | 0.004 |
| Pharmacist's advice on taking prescribed medication with other over-the-counter medications | 2.80 (1.36–5.79) | 0.005 |
| Pharmacist's advice on resolving the difficulties caused by taking the medication | 2.64 (1.79–5.91) | 0.017 |
Discussion
The present study aimed to evaluate the level of adherence to topical glaucoma treatment and investigate the predictors of adherence among glaucoma patients in Zagreb, Croatia, during the COVID-19 outbreak.
The results demonstrated that 39.8% of patients were adherent to glaucoma treatment. Similar adherence trends were observed worldwide among glaucoma patients recently.21,23,24 On the other hand, the results of an extensive population project that investigated treatment adherence in various chronic diseases in Zagreb, conducted before the COVID-19 pandemic, in which the authors used the same questionnaire, showed adherence of 52% among 25 chronic glaucoma patients.27 However, the results related to glaucoma adherence were estimated on the small sample, with patients having various types of the disease, therefore, not comparable to herein presented results. Therefore, the present study is the first one that investigated adherence in POAG patients in Croatia at all, and there are no other entirely proper data for the comparison in this region.
Ayub et al. investigated the impact of the COVID-19 pandemic on adherence to tertiary centre visits in Brazil and found a significant reduction in the number of clinical visits, VF exams, surgical procedures, and discharges of drugs.18 Raccete et al. reported a worsening of treatment adherence estimated objectively by using Medication Event Monitoring System (MEMS) caps in glaucoma patients in the US, documenting an adverse impact of the COVID-19 outbreak on health behaviour, which places patients at risk of vision loss.25 On the other hand, the study conducted in Enugu, Nigeria, revealed that the pandemic did not reduce adherence to follow-up appointments but revealed the continued low rate of adherence in the system.22
The present study showed that the main patients' sociodemographic factors were not associated with adherence to treatment in the final regression analysis, except the educational level, which was significantly positively correlated to adherence. Similar results have been observed in other studies, showing that more educated patients have greater health literacy and thus better adherence to treatment.28,29 Mylona et al. found in the Greek population that the COVID-19 pandemic disproportionally impacted patients of older age and lower educational levels, disturbing their ability to follow treatment plan.23
According to the WHO, treatment adherence is a multidimensional concept, and its associated factors are classified into five groups: patient-related, disease-related, drug-related, health care system-related, and environmental-related factors.4 Additionally, adherence is described as a dynamic process and is likely to oscillate in response to personal and situational circumstances changes.5 In this study, the univariate logistic regression analyses identified the main predictors for adherence to glaucoma pharmacotherapy. Factors associated with adherence were related to three main categories: patient characteristics, family support, and relationship with healthcare providers (general doctors, ophthalmologists, and pharmacists).
Related to patients' characteristics, most of the patients were sure that they would take all the medications in the way agreed with the doctor, which showed a statistically significant positive correlation with adherence. In addition, almost all patients believed that the treatment would positively impact their health. As glaucoma is asymptomatic in its early stages, and the disease management is preventative rather than curative, patients' positive expectations and motivation are important for good adherence. Subathra et al. recently reported non-adherence among glaucoma patients in India since they haven't experienced subjective improvements in quality of vision, related to insufficient knowledge about glaucoma's natural course.24 However, despite having positive beliefs about the therapy, patients in the present study showed low overall adherence to treatment. Authors suggested that the ongoing pandemic supported the beliefs in the benefits of therapy since the circumstances related to the health crisis have raised awareness about health and well-being in general. On the other hand, it decreased the motivation for medication self-management due to the psychological affections, such as fear, uncertainty, stress related to the virus and disease it causes, social isolation, loneliness, and financial concerns, since it is already known that psychological factors adversely influence patients' motivation to adhere to treatment recommendations.30,31 In that line, mental health is vital for self-efficacy and proper adherence, as psychological reactions to novel situations characterize the pandemic.
Related to family support, one-third of our patients were content with how their family accepted them as a patient, while the rest reported some degree of dissatisfaction. Most patients in the present study reported that family members provided them with therapy assistance, and the results are consistent with Assem et al., who showed that participants who had family support were 1.7 times more adherent to their medication than those who had no family support.32 However, in the current circumstances of COVID-19 pandemics, some patients lost close contact with family members due to preventative measures (social distancing and self-isolation), which resulted in reduced help with therapy. It is already known that medication self-management may feel burdensome for some patients with glaucoma due to impaired vision or physical disabilities, indicating that the lack of family support might be an indicator of poor adherence to treatment.6,29 Moreover, in the context of the COVID-19 pandemic, deficient and inadequate family relationships and support have been found as risk factors for depression and anxiety, resulting in poor adherence motivation.31,33 Considering that DiMatteo in a meta-analysis concluded that support from friends and family promotes adherence by encouraging optimism and self-esteem.34
Related to the healthcare providers, in the present study adherence was significantly higher among patients who reported that a doctor was available whenever they had a health problem. In response to pandemics and limited access to health care facilities in Croatia, SMS and e-mail communication was reinforced, thus partially filling the gap in patients' health care provision. However, in the recent period, doctors in Croatia have been facing unique and aggravated challenges, in addition to the many pressures already associated with the strained health care system. Buller et al. found that poor communication between patients and healthcare providers resulted in the wrong treatment regimen in nearly one in five patients.35 Glaucoma Adherence and Persistency Study results implied the importance of doctor-patient relationship, communication, and health-related beliefs about adherent behaviour.36 However, according to recent evidence, the global health crisis has posed strains in providing thorough and timely glaucoma care for patients who missed their scheduled appointments.17,18,24 The long-term effect of the gap in regular follow-ups on the visual outcome is yet to be investigated. Pre-COVID-19 studies proposed advancing technologies like teleglaucoma to improve the capabilities of the clinician in managing glaucoma.37 That is of particular importance in the actual situation of abrupt interruption of healthcare delivery which poses threats to adequate adherence and risk of vision loss.
Furthermore, the impact of the community pharmacists' role on medication adherence among glaucoma patients during the pandemic presented as substantial. Present study results demonstrated that 80% of pharmacists explained to the patients about their pharmacotherapy, which significantly correlates with treatment adherence. This result is consistent with the study conducted in Ethiopia, which showed that glaucoma patients who got information on medication from a pharmacist were 1.8 times more adherent to treatment.32 Community pharmacists play a vital role in a public health crisis for patients with chronic diseases who require regular visits and repeated medical prescriptions.38 Therefore, the pharmacists' public-health interventions, like educating, advising, and promoting continued adherence, are requisite when access to health facilities is limited, like in the recent era. Previously, several strategies have been proposed that could be implemented to ensure continued access to medication, including expanding the capacity for mail-order and home delivery, which could be crucial for adequate adherence in a time of crisis.39
The secondary endpoint of this study was to determine the main reasons for non-adherent behaviour. The most common responses were forgetfulness and not being at home. Possible explanations are changes in patients' everyday habits caused by unique circumstances related to COVID-19, as a daily routine is shown to be an important factor for adequate adherence to treatment.4,7 Moreover, psychological affections and stress exacerbated through the global crisis might also contribute to forgetfulness during the pandemics. According to the above-mentioned, the patient's adherence behaviour could be facilitated by identifying how the person can integrate medication-taking into their daily routine.7 On the other hand, the studies conducted recently in other parts of the world showed that situational factors, such as financial issues, transportation difficulties, and nonavailability of medicines, are the most commonly cited obstacles against adherence among glaucoma patients during the pandemic.21,24 In the end, there are potentially some unknown factors pronounced at the time of the public health crisis that played an important role in patients’ health behaviour, which has yet to be identified.
Various strategies to bridge the barriers to adherence and promote adherent behaviour are described in the literature.40,41 In light of pandemics, digital medicine platforms, mobile health applications, and electronic reminders may produce favourable results. However, it should be noted that new technologies are less likely to be used by less educated, older, and lower-income patients, which present the most vulnerable social group.
Limitations
The authors addressed some limitations of the present study. The patients were collected from a single health centre. Additionally, despite the small number, some of them were excluded because more than 10% of unanswered items in the questionnaire might cause selection bias. Furthermore, the evidence of the impact of the COVID-19 pandemic was based on convenience samples and a relatively small number of patients, without comparable pre-pandemic data of our cohort. The data regarding the rate of adherence may be misjudged for two reasons. First, the study was based on a self-report questionnaire, so the validity of the responses was challenging to control due to the patients' tendency to overestimate treatment adherence. The data would be more reliable if the level of adherence were estimated using more objective measures, such as electronic MEMS devices or electronic pharmacy data (i.e. medication possession ratio, MPR). Second, the proper level of adherence is likely to be underestimated as patients who did not attend the Clinic during the pandemic did not participate in the study. Finally, our research is not powered to assess the direct impact of the COVID-19 by using specific pandemic-related questions. Therefore, to strengthen the value of our study, there is a need for more extended clinical investigations.
Conclusions
The present study is the first to attempt treatment adherence among glaucoma patients in Croatia. The results showed a poor level of adherence among glaucoma patients during the COVID-19 pandemic.
A significant correlation between adherence and individual facilitators like positive health-related beliefs and attitudes towards disease treatment was found. The essential impact of the family support and close patient-healthcare provider relationship in the management of glaucoma was also detected. The authors suggest that by enhancing the patients' motivation and self-efficacy and ameliorating their relationship with family and healthcare providers, adherence to glaucoma treatment may increase, positively impacting the therapeutic regimen's effectiveness.
Further investigations are warranted to investigate the long-term influence of pandemic-related adherence on the functional and structural visual outcome of POAG patients.
Finally, the findings of this study provided general practitioners, ophthalmic care professionals, pharmacists, and public health organizations insight into health behaviour in terms of adequate treatment of glaucoma patients during the COVID-19 to better prepare for a potential sudden interruption of glaucoma management in the future. Hence, the whole system-level approach is required to contribute to glaucoma management in order to ameliorate adherence and achieve positive treatment outcomes.
Footnotes
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Data availability statement: The authors confirm that the data supporting the findings of this study are available within the article and its supplementary materials. The authors state that this manuscript has not been published previously and is not considered for publication elsewhere. Its publication is approved by all authors and tacitly or explicitly by the responsible authorities where the work was carried out. If accepted, it will not be published elsewhere in the same form, in English or any other language, including electronically, without the written consent of the copyright holder.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Dina Lešin Gaćina https://orcid.org/0000-0002-2468-2195
References
- 1.European Glaucoma society terminology and guidelines for glaucoma, 5th edition. Br J Ophthalmol 2021; 105: 1–169. [DOI] [PubMed] [Google Scholar]
- 2.Kass MA, Heuer DK, Higginbotham EJ, et al. The ocular hypertension treatment study: a randomized trial determines that topical ocular hypotensive medication delays or prevents the onset of primary open-angle glaucoma. Arch Ophthalmol Chic Ill 1960 2002; 120: 701–713; discussion 829–830. [DOI] [PubMed] [Google Scholar]
- 3.Musch DC, Gillespie BW, Lichter PR, et al. Visual field progression in the collaborative initial glaucoma treatment study the impact of treatment and other baseline factors. Ophthalmology 2009; 116: 200–207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sabaté E. Adherence to long-term therapies: evidence for action. Geneva: World Health Organization, 2003. [Google Scholar]
- 5.Newman-Casey PA, Robin AL, Blachley T, et al. The most common barriers to glaucoma medication adherence: a cross-sectional survey. Ophthalmology 2015; 122: 1308–1316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Robin AL, Muir KW. Medication adherence in patients with ocular hypertension or glaucoma. Expert Rev Ophthalmol 2019; 14: 199–210. [Google Scholar]
- 7.Newman-Casey PA, Niziol LM, Gillespie BW, et al. The association between medication adherence and visual field progression in the collaborative initial glaucoma treatment study. Ophthalmology 2020; 127: 477–483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Haymes SA, Johnston AW, Heyes AD. Relationship between vision impairment and ability to perform activities of daily living. Ophthalmic Physiol Opt J Br Coll Ophthalmic Opt Optom 2002; 22: 79–91. [DOI] [PubMed] [Google Scholar]
- 9.Loon SC, Jin J, Jin Goh M. The relationship between quality of life and adherence to medication in glaucoma patients in Singapore. J Glaucoma 2015; 24: e36–e42. [DOI] [PubMed] [Google Scholar]
- 10.Cucinotta D, Vanelli M. WHO Declares COVID-19 a pandemic. Acta Bio-Medica Atenei Parm 2020; 91: 157–160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Čivljak R, Markotić A, Kuzman I. The third coronavirus epidemic in the third millennium: what’s next? Croat Med J 2020; 61: 1–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Čivljak R, Markotić A, Capak K. Earthquake in the time of COVID-19: the story from Croatia (CroVID-20). J Glob Health 2020; 10: 010349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Svetina L, Kosec A, Curkovic M, et al. A case study of complex disasters within the resilience framework in Zagreb, Croatia: two earthquakes in one pandemic. Environ Res 2022; 204: 112079. [DOI] [PubMed] [Google Scholar]
- 14.Lancet T. Redefining vulnerability in the era of COVID-19. The Lancet 2020; 395: 1089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Esposti LD, Buda S, Nappi C, et al. Implications of COVID-19 infection on medication adherence with chronic therapies in Italy: a proposed observational investigation by the fail-to-refill project. Risk Manag Healthc Policy 2020; 13: 3179–3185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Chudasama YV, Gillies CL, Zaccardi F, et al. Impact of COVID-19 on routine care for chronic diseases: a global survey of views from healthcare professionals. Diabetes Metab Syndr Clin Res Rev 2020; 14: 965–967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Nair AG, Gandhi RA, Natarajan S. Effect of COVID-19 related lockdown on ophthalmic practice and patient care in India: results of a survey. Indian J Ophthalmol 2020; 68: 725–730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ayub G, de Vasconcelos JPC, Costa VP. The impact of COVID-19 in the follow-up of glaucoma patients in a tertiary center: a comparison between Pre-pandemic and pandemic periods. Clin Ophthalmol Auckl NZ 2021; 15: 4381–4387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Nguyen AX, Gervasio KA, Wu AY. Differences in SARS-CoV-2 recommendations from major ophthalmology societies worldwide. BMJ Open Ophthalmol 2020; 5. DOI: 10.1136/bmjophth-2020-000525. Epub ahead of print 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lešin Gaćina D, Ivkić PK, Škegro I, et al. Ophthalmological aspects of COVID-19: literature review and our experience. Infektološki Glas 2020; 40: 64–67. [Google Scholar]
- 21.Awwad MA, Masoud M. Influence of COVID-19 on the prognosis and medication compliance of glaucoma patients in the Nile Delta region. Clin Ophthalmol 2021; 15: 4565–4572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kizor-Akaraiwe N, Uche N, Shiweobi J, et al. Glaucoma follow-up care in the face of COVID-19 pandemic in enugu, Nigeria. Niger J Ophthalmol 2021; 29: 22–27. [Google Scholar]
- 23.Mylona I, Dermenoudi M, Glynatsis NM, et al. Patient adherence to glaucoma treatment during the COVID-19 pandemic. Cureus 13. DOI: 10.7759/cureus.15545. Epub ahead of print 9 June 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Subathra GN, Rajendrababu SR, Senthilkumar VA, et al. Impact of COVID-19 on follow-up and medication adherence in patients with glaucoma in a tertiary eye care centre in south India. Indian J Ophthalmol 2021; 69: 1264–1270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Racette L, Abu SL, Poleon S, et al. The impact of the coronavirus disease 2019 pandemic on adherence to ocular hypotensive medication in patients with primary open-angle glaucoma. Ophthalmology 2022; 129: 258–266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Momirovic A, Ganza M, Culig B, et al. Psychometric properties of the Culig’s questionnaire. Psychiatr Danub 2016; 28: 234–241. [PubMed] [Google Scholar]
- 27.Bošković J. Patients medication adherence in chronic diseases in City of Zagreb. PhD Thesis, Faculty of pharmacy and medical biochemistry, 2021. [Google Scholar]
- 28.Muir KW, Santiago-Turla C, Stinnett SS, et al. Health literacy and adherence to glaucoma therapy. Am J Ophthalmol 2006; 142: 223–226. [DOI] [PubMed] [Google Scholar]
- 29.Tsai JC. A comprehensive perspective on patient adherence to topical glaucoma therapy. Ophthalmology 2009; 116: S30–S36. [DOI] [PubMed] [Google Scholar]
- 30.Zhang X, Olson DJ, Le P, et al. The association between glaucoma, anxiety, and depression in a large population. Am J Ophthalmol 2017; 183: 37–41. [DOI] [PubMed] [Google Scholar]
- 31.Sleath BL, Blalock SJ, Muir KW, et al. Determinants of self-reported barriers to glaucoma medicine administration and adherence: a multisite study. Ann Pharmacother 2014; 48: 856–862. [DOI] [PubMed] [Google Scholar]
- 32.Assem AS, Fekadu SA, Yigzaw AA, et al. Level of glaucoma drug adherence and its associated factors among adult glaucoma patients attending felege hiwot specialized hospital, bahir dar city, northwest Ethiopia. Clin Optom 2020; 12: 189–197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Mariani R, Renzi A, Di Trani M, et al. The impact of coping strategies and perceived family support on depressive and anxious symptomatology during the coronavirus pandemic (COVID-19) lockdown. Front Psychiatry 2020; 11: 587724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.DiMatteo MR.Social support and patient adherence to medical treatment: a meta-analysis. Health Psychol Off J Div Health Psychol Am Psychol Assoc 2004; 23: 207–218. [DOI] [PubMed] [Google Scholar]
- 35.Buller AJ, Connell B, Spencer AF. Compliance: clear communication’s critical. Br J Ophthalmol 2005; 89: 1370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Friedman DS, Hahn SR, Gelb L, et al. Doctor-patient communication, health-related beliefs, and adherence in glaucoma results from the glaucoma adherence and persistency study. Ophthalmology 2008; 115: 1320–1327. 1327.e1–3. [DOI] [PubMed] [Google Scholar]
- 37.Kassam F, Yogesan K, Sogbesan E, et al. Teleglaucoma: improving access and efficiency for glaucoma care. Middle East Afr J Ophthalmol 2013; 20: 142–149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Cadogan CA, Hughes CM. On the frontline against COVID-19: community pharmacists’ contribution during a public health crisis. Res Soc Adm Pharm RSAP 2021; 17: 2032–2035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Newman-Casey PA, Blachley T, Lee PP, et al. Patterns of glaucoma medication adherence over four years of follow-up. Ophthalmology 2015; 122: 2010–2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Tapply I, Broadway DC. Improving adherence to topical medication in patients with glaucoma. Patient Prefer Adherence 2021; 15: 1477–1489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Cate H, Bhattacharya D, Clark A, et al. Improving adherence to glaucoma medication: a randomised controlled trial of a patient-centred intervention (the norwich adherence glaucoma study). BMC Ophthalmol 2014; 14: 32. [DOI] [PMC free article] [PubMed] [Google Scholar]