Abstract
Background and Aim:
Robotic surgery is an advancing technology and patients may not be fully aware of these advancements. Social media and advertisements may falsely skew patients’ understanding. This study aims to seek awareness, understanding. and attitude toward robotic surgery in Singapore.
Materials and Methods:
A cross-sectional study of 472 patients and/or their relatives (response rate 94.4%) in a specialist outpatient clinic chosen through convenience sampling from May to July 2017 was performed. All healthcare workers or participants <21 years of age were excluded. A 19-point survey questionnaire including patient sociodemographics and awareness and attitudes toward robotic surgery was administered. Univariate and multivariate analysis was performed to assess participants’ preference for robotic surgery.
Results:
Two hundred and sixty (55.1%) of the participants were female and the majority were aged 21–40 years old (55.5%). 250 participants (53.0%) reported having heard of robotic surgery; majority (n=205, 82.0%) were from the media. Two hundred and six (43.6%) participants had the misconception that robotic surgery involved an automated robot. Multivariate analysis showed that perception that robotic surgery yielded better results was independently associated with preference for robotic surgery (prefers robotic surgery: n=56/159 (35.2%), do not prefer robotic surgery: n=81/313 (25.9%), odds ratio (OR) 1.61, 95% confidence interval (CI): 1.06–2.45, P=0.026). Having concerns that wrong surgery may be performed by robotic surgery were also independently associated with disinclination toward robotic surgery (OR 0.51 [95% CI: 0.35–0.76], P=0.001).
Conclusion:
Understanding of robotic surgery was poor with several misconceptions. It is paramount to clarify these misconceptions to advocate for informed decision-making.
Relevance for Patients:
Measures need to be taken to ensure adequacy of pre-operative counseling in patients undergoing robotic surgery. Misconceptions on benefits and risks of robotic surgery should be cleared before decision on the surgical access and approach.
Keywords: Asia, awareness, informed consent, laparoscopy, minimally invasive surgery, patient education, robotic surgery
1. Introduction
Fusion of technological innovation with clinical medicine has given rise to minimally invasive surgery (MIS). Surgery has seen a significant shift from traditional open surgery to MIS with improvements in wound healing time, reduced length of hospitalization stay and perioperative complications, and better cosmesis [1,2]. Conventional laparoscopy remains the most common form of MIS. However, robotic surgery has witnessed a tremendous increase in its use, with a 400-fold growth in adoption from 2000 to 2010 [3]. Unlike conventional laparoscopy, the present systems used in robotic surgery provide improvements in three-dimensional view with depth perception, eliminates hand tremors, and provides a wider degree of movement [4].
However, with these recent improvements in technological innovation and surgical techniques, patients may not be fully aware and up-to-date with these advancements. A preliminary search in PubMed (dated 14 December, 2020) on surveys on public perception of robotic surgery reflected only a small number of relevant studies [5-9]. A recent study by Boys et al. which surveyed 747 participants residing mainly in the United States of America reported that 72% of the participants thought that robotic surgery was safer, faster, and offered better results [7]. A qualitative study by McDermott et al. who conducted semi-structured interviews on 25 participants in the United Kingdom similarly demonstrated a general lack of understanding of robotic surgery among young lay people [10]. The results of the survey revealed the chasm in knowledge gaps and the potential unrealistic myths that the general public may have with regards to robotic surgery. It is the duty of a clinician to provide individualized information and educate his or her patient on the benefits and disadvantages of any procedure. Moreover, the lack of understanding demonstrated in existing studies is alarming given the shift toward robotic surgery. Unmet expectations for post-operative outcomes may lead to patient dissatisfaction and medicolegal litigations [11].
Till date, there is a lack of studies on public perception and misconceptions the general public may have on robotic surgery. Our study aims to add value to existing literature by first, understanding the awareness, perception, knowledge, and attitude toward robotic surgery in attendees of a surgical outpatient clinic.
2. Materials and Methods
This is a descriptive and cross-sectional study of patients and their relatives who visited the general surgical outpatient clinic at a university-affiliated academic teaching hospital over 2.5 months from May to July 2017. Healthcare workers and participants <21 years of age were excluded from the study. Participants who were illiterate in English were also excluded from the study. Participation in the survey was voluntary; no further contact was made with the participant should he or she refuse. This study was approved by a local institutional review board (National Healthcare Group Domain Specific Review Board, Ref: 2017/00343). Definitions in the survey study are in concordant with the American Association for Public Opinion Research reporting guidelines [12].
2.1. Description of survey
This is a 19-point survey questionnaire (Supplementary Material) constructed based on existing surveys of European Commission and Boys et al. [7,13]. The survey was administered in written form using pen and paper and was available only in English language. No translation was required as participants who were illiterate in English were excluded from the study. The survey consisted of two components: (1) Patient demographics such as age, gender, ethnicity, education level (lower education: secondary school and below vs. higher education: diploma and above), employment status, type of housing (lower purchasing power: executive flats and Housing Developmental Board (HDB) flat vs. higher purchasing power: condominium or private properties), interest level in scientific discoveries, and experience with robots and (2) awareness and attitudes toward robots and robotic surgery. We did not exclusively adopt a Likert scale for our survey to improve participation and ease of completion; the use of binary questions has been shown to be an acceptable alternative to the Likert scale to reduce fatigue and length of survey [14]. For the purpose of this study, the term “public” is defined as the patients and/or their relatives who participated in the survey. The modified survey was not validated in our local population as this was the first study conducted in Singapore to assess the perception and knowledge of robotic surgery locally.
2.2. Study protocol
Participants of this study were sampled by convenience sampling. Patients and/or their relatives in the general surgical outpatient clinic (which also included technical visits for wound care, or blood tests before a clinic consult a few days later) were approached for the survey and were briefed on the purpose and the components of the survey. These participants were approached either before or after the clinic consultation. Each household who participated in the survey was only provided with one survey form regardless of the number of people per household present. They were also briefed that the survey would take approximately 10 min and to complete the survey to the best of their abilities without referring to any resources. It was also emphasized that the survey results would be anonymized, and participants may withdraw from the survey at any point of the study without any repercussions. No further contact was made with patients and/or their relatives who declined to participate in the survey. Participants who consented to the survey were redirected to a quiet designated room allocated for completion of the survey. One coinvestigator was present to allow participants to clarify any doubts and ensure completion of the survey forms. The investigator did not influence that the understanding participants have on the study. Participants who completed the survey were thanked for their contribution and proceeded on with their original agenda in the clinic.
2.3. Statistical analysis
All statistical analyses were performed with IBM SPSS version 25.0 (SPSS Inc., Chicago, III., USA). For Singapore’s population of 6 million, at 95% confidence interval (CI) and 5% margin for error, a sample size of 385 participants is adequate. We factored for incomplete response rate of about 10% and thus set a goal to recruit at least 425 participants. Categorical values were described as percentages and analyzed by Chi-square test (χ2). Statistical significance was determined by P<0.05. Strength of association was analyzed by Cramer’s V (fc): <0.20 represents weak association, 0.20–0.30 represents moderate association, and >0.30 represents strong association. Multivariate analysis was performed when univariate analysis had p<0.100 using logistic regression to address for potential confounding factors on participants’ preference for robotic surgery: Age, gender, ethnicity, educational level, employment status, type of housing, interest in scientific discoveries, and prior experience with robots.
3. Results
A total of 500 patients and/or relatives were approached during this study duration. Four hundred and seventy-five people participated in the survey. Three surveys were incomplete and were excluded from the final statistical analyses. Four hundred and seventy-two valid surveys were analyzed, with a response rate of 94.4%.
3.1. Patient demographics
Table 1 summarizes the demographics of the study population. Around half of the participants were aged between 21 and 40 years old (n=262, 55.5%). More than half received higher education (Diploma and above) (n=342, 72.5%), and were employed/self-employed (n=290, 61.4%). The majority of the participants had lower purchasing power living in executive or HDB flats (n=375, 79.4%). A minority of patients had no interest in scientific discoveries (n=98, 20.8%). One hundred and ninety-six (41.5%) had no experience with robots. Table 2 summarizes that the awareness, perception, knowledge, and attitude participants have toward robotic surgery.
Table 1. Sociodemographic profile of participants.
| n=472 (%) | |
|---|---|
| Age | |
| 21–40 | 262 (55.5) |
| 41–60 | 158 (33.5) |
| 61–80 | 47 (10.0) |
| >80 | 5 (1.1) |
| Gender | |
| Male | 212 (44.9) |
| Female | 260 (55.1) |
| Ethnicity | |
| Chinese | 409 (86.7) |
| Malay | 29 (6.1) |
| Indian | 26 (5.5) |
| Others | 8 (1.7) |
| Highest educational level | |
| Primary school or lower | 29 (6.1) |
| Secondary school | 101 (21.4) |
| Diploma | 116 (24.6) |
| Degree (Bachelor’s) | 202 (42.8) |
| Postgraduate degree (Master’s degree and above) | 24 (5.1) |
| Employment status | |
| Working/Employed | 246 (52.1) |
| Self-employed | 44 (9.3) |
| Student | 96 (20.3) |
| Retired | 26 (5.5) |
| Homemaker | 24 (5.1) |
| Unemployed | 33 (7.0) |
| Unable to work | 3 (0.6) |
| Type of housing | |
| Housing Development Board flat (1–3 room) | 73 (15.5) |
| Housing Development Board flat (4 room) | 168 (35.6) |
| Housing Development Board flat (5 room) | 102 (21.6) |
| Executive flats and others | 32 (6.8) |
| Condominium and private flats | 64 (13.6) |
| Landed property | 33 (7.0) |
| Interest in scientific discoveries | |
| Very interested | 87 (18.4) |
| Somewhat interested | 287 (60.8) |
| Not interested | 98 (20.8) |
| Experience with robots | |
| At home | 203 (43.0) |
| At work | 46 (9.7) |
| Others | 27 (5.7) |
| No | 196 (41.5) |
Table 2. Awareness, perception, knowledge, and attitude participants have toward robotic surgery.
| n=472 (%) | |
|---|---|
| Awareness | |
| Heard about robotic surgery | |
| Yes | 250 (53.0) |
| No | 222 (47.0) |
| Source of information# | |
| Media | 205 (82.0) |
| Magazine | 37 (14.8) |
| Doctor | 33 (13.2) |
| Friends and relatives | 30 (12.0) |
| Perception and/or knowledge | |
| Which type of surgery is robotic surgery most similar to?# | |
| Traditional open surgery | 23 (9.2) |
| Laparoscopic surgery | 161 (64.4) |
| Laser surgery | 66 (26.4) |
| Understanding of robotic surgery | |
| Robot performs surgery, trained surgeon stands by | 138 (29.2) |
| Surgeon controls robotic arms and instrument | 266 (56.4) |
| Surgeon tells robot what to do, robot follows each command | 40 (8.5) |
| Surgeon not present in the operating theatre; robot performs according to software | 28 (5.9) |
| Perceptions of robotic surgery compared to non-robotic surgery$ | |
| Faster | 221 (46.8) |
| Safer | 138 (29.2) |
| Better results | 137 (29.0) |
| Less painful | 66 (14.0) |
| Costly | 212 (44.9) |
| None of the above | 73 (15.5) |
| Concerns regarding robotic surgery | |
| Robot malfunctions causing internal damage | 373 (79.0) |
| Robot performs wrong procedure | 260 (55.1) |
| Do you think robotic malfunction has occurred before during surgery? | |
| Never | 15 (3.2) |
| Yes | 115 (24.4) |
| Unsure | 342 (72.5) |
| Attitude | |
| Would you prefer to undergo robotic surgery? | |
| Yes | 159 (33.7) |
| No | 313 (66.3) |
| Perceptions of surgeons trained in robotic surgery | |
| More skilled | 154 (32.6) |
| Similar | 257 (54.4) |
| Less skilled | 61 (12.9) |
| Perceptions of hospitals using robotic surgery | |
| Better | 201 (42.6) |
| Similar | 253 (53.6) |
| Worse | 18 (3.8) |
Expressed as a percentage of participants who have heard of robotic surgery (n=250). Percentages do not add to 100 due to multiple option selection
3.2. Awareness of robotic surgery
About half of the participants (n=250, 53.0%) reported having heard of robotic surgery, of which 205 (82.0%) were from the media. Participants with interest in scientific discoveries were more likely to have heard of robotic surgery although the association was weak (P=0.046, fC =0.114).
3.3. Perceptions and knowledge of robotic surgery (Table 2)
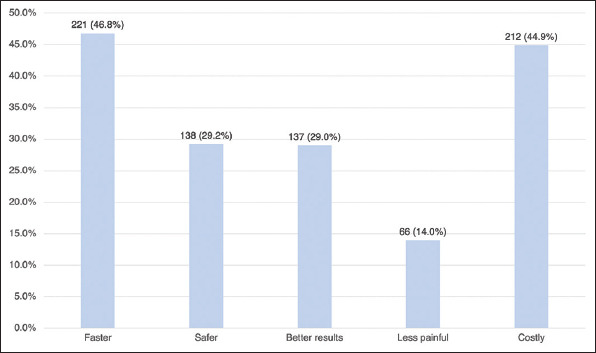
Majority of those who heard of robotic surgery correctly identified it as being most similar to laparoscopic surgery (n=161/250, 64.4%). About half the participants (n=206/472, 43.6%) thought that robotic surgery involved an automated robot rather than manual control of robotic arms by a surgeon. This was not correlated to education level (P=0.162). In comparison with non-robotic surgery, 221 (46.8%) and 212 (44.9%) participants thought that robotic surgery was faster but more expensive, respectively (Table 2). Figure 1 shows participants’ perceptions of robotic surgery compared to non-robotic surgery. A minority of patients thought that robotic surgery was safer (n=138, 29.2%), less painful (n=66, 14.0%), and able to offer better outcomes (n=137, 29%).
Figure 1. Perceptions of robotic surgery compared to non-robotic surgery.
3.4. Attitude toward robotic surgery
One hundred and fifty-nine (33.7%) participants preferred the use of robotic surgery. Table 3 summarizes the differences in sociodemographics, attitudes, and perceptions of participants who preferred robotic surgery compared to those who did not. Preference for use of robotic surgery was significantly correlated with the perception that robotic surgery yielded better results (preferred robotic surgery: n=56 (35.2%) vs. did not prefer: n=81 (25.9%), P=0.035). Multivariate analysis also showed that perception that robotic surgery yielded better results was independently associated with preference for robotic surgery (Odds ratio [OR] 1.61, 95% CI: 1.06–2.45, P=0.026). Having concerns that wrong surgery may be performed by robotic surgery were also independently associated with disinclination toward robotic surgery (OR 0.51 (95% CI: 0.35–0.76), P=0.001). However, preference for robotic surgery was not significantly correlated with the perception that robotic surgery is faster (P=0.095, φC =0.077), safer (P=0.594, φC =0.025), less painful (P=0.057, φC =0.087), and costly (P=0.274, φC =0.050).
Table 3. Sociodemographics, attitudes, and perceptions of participants have of robotic surgery in those who preferred robotic surgery and those who did not.
| Total (n=472) | Prefers robotic surgery (n=159) | Does not prefer robotic surgery (n=313) | Univariate analysis | Multivariate analysis* | |||
|---|---|---|---|---|---|---|---|
|
|
|
||||||
| OR (95% CI) | P-value | OR (95% CI) | P-value | ||||
| Age | 0.94 (0.64–1.37) | 0.733 | - | - | |||
| 21–40 | 262 (55.5) | 90 (56.6) | 172 (55.0) | ||||
| >40 | 210 (44.5) | 69 (43.4) | 141 (45.0) | ||||
| Highest educational level | 1.26 (0.82–1.95) | 0.296 | - | - | |||
| Lower education (secondary school or lower) | 130 (27.5) | 39 (24.5) | 91 (29.1) | ||||
| Higher education (diploma or higher) | 342 (72.5) | 120 (75.5) | 222 (70.9) | ||||
| Type of housing | 0.96 (0.60–1.55) | 0.871 | - | - | |||
| Lower purchasing power (Executive or Housing Development Board flats) | 375 (79.4) | 127 (79.9) | 248 (79.2) | ||||
| Higher purchasing power (Condominium and private flats) | 97 (20.6) | 32 (20.1) | 65 (20.8) | ||||
| Perceptions of robotic surgery compared to non-robotic surgery | |||||||
| Faster | 221 (46.8) | 83 (52.2) | 138 (44.1) | 1.39 (0.94–2.03) | 0.095 | 1.32 (0.89–1.96) | 0.163 |
| Safer | 138 (29.2) | 44 (27.7) | 94 (30.0) | 0.89 (0.58–1.36) | 0.594 | - | - |
| Better results | 137 (29.0) | 56 (35.2) | 81 (25.9) | 1.56 (1.03–2.35) | 0.035 | 1.61 (1.06–2.45) | 0.026 |
| Less painful | 66 (14.0) | 29 (18.2) | 37 (11.8) | 1.66 (0.98–2.82) | 0.057 | 1.62 (0.95–2.77) | 0.078 |
| Costly | 212 (44.9) | 77 (48.4) | 135 (43.1) | 1.24 (0.84–1.82) | 0.274 | - | - |
| Concerns regarding robotic surgery | |||||||
| Robot malfunctions causing internal damage | 373 (79.0) | 127 (79.9) | 246 (78.6) | 1.08 (0.67–1.73) | 0.747 | 1.07 (0.66–1.73) | 0.782 |
| Robot performs wrong procedure | 260 (55.1) | 70 (44.0) | 190 (60.7) | 0.51 (0.35–0.75) | 0.001 | 0.51 (0.35–0.76) | 0.001 |
| Perceptions of surgeons trained in robotic surgery | - | 0.899 | - | - | |||
| More skilled | 154 (32.6) | 52 (32.7) | 102 (32.6) | ||||
| Similar | 257 (54.4) | 88 (55.3) | 169 (54.0) | ||||
| Less skilled | 61 (12.9) | 19 (11.9) | 42 (13.4) | ||||
| Perceptions of hospitals using robotic surgery | - | 0.136 | - | - | |||
| Better | 201 (42.6) | 77 (48.4) | 124 (39.6) | ||||
| Similar | 253 (53.6) | 75 (47.2) | 178 (56.9) | ||||
| Worse | 18 (3.8) | 7 (4.4) | 11 (3.5) | ||||
Multivariate analysis was performed using logistic regression to address for potential confounding factors on participants’ preference for robotic surgery: Age, gender, ethnicity, educational level, employment status, type of housing, interest in scientific discoveries, and prior experience with robots, CI: Confidence interval; OR: Odds ratio
4. Discussion
This study demonstrates that the chasm of knowledge gaps people may have with regards to robotic surgery. While these findings are not completely unexpected by the authors, the results provide a clearer understanding on the extent of misconception patients may have and the unmet need in patient education on robotic surgery. Patient education is paramount in the current era of medical practice to provide a patient-centric health-care system and to allow patients to make informed decisions.
Our study demonstrated that the majority of the participants correctly identified laparoscopic surgery to be the most similar to robotic surgery (n=161/250, 64.4%), which is similar to the study by Boys et al. (n=583/747, 78.0%) [7]. However, our study also demonstrated that almost half of the participants had the misconception that robots exercise autonomy in robotic surgery, unlike the study by Boys et al. (43.6% in our study vs. 21% in their study). The difference in our results may be due to the sociogeographical differences in our study populations. Extent of local marketing in Singapore is likely to be less prevalent compared to its Western counterparts, which first saw the introduction of robotic surgery [15]. Unfortunately, there are no existing studies reporting the perception of robotic surgery in the local context, hence, re-emphasising the importance of the study to provide an overview of the current understanding and perception of robotic surgery in the population. In addition, the difference in our results may be due to the exclusion of healthcare workers in our study, unlike the study by Boys et al. [7], where 53.3% of the respondents were healthcare workers. Participants with a background in healthcare are more likely to be aware of the basics of robotic surgery and may skew results. On the contrary, lay participants may lack health literacy and also skew results. Our study included patients and/or their relatives attending the surgical outpatient clinic, who are more likely to be in-tuned with surgical advances, as compared to lay public. The greater proportion of participants expressing misconception on robotic surgery may be due to sociodemographic profile, geographic differences, or the lack of understanding. Another study by Irani et al. demonstrated similar findings: 67.5% of 214 patients did not know that movement of the robotic arms during surgery was performed manually by surgeons [16].
Acceptance of robotic surgery was poor in our study (33.7%). However, this is not surprising and is concordant with other surveys conducted on robotic surgery: A study by Chu et al. on pelvic organ prolapse surgery found that only 6.4% of patients preferred robotic surgery [5]. Our study found that 212 participants (44.9%) felt that robotic surgery was costly, and of which 135 (63.7%) did not prefer robotic surgery. This result suggests that preference for robotic surgery may be correlated to the participants’ perception of its benefits. This is concordant with the study by Makar et al. [8], which demonstrated that the risk of post-operative complications and length of post-operative recovery were important factors in patient’s decision for robotic surgery. However, value-driven outcomes are more important than cost and a patient-centric health system should measure and report such outcomes which are independent of health-care costs. Other factors affecting their preference for robotic surgery included the misconceptions that (1) robots were autonomous in robotic surgery (43.6%), (2) possibility of performing the wrong procedure (55.1%), and (3) inability for robots to react to changes in situations and make judgments as a surgeon would. Possibility of performing the wrong procedure is a valid concern and is definitely possible with any kind of surgery; however, this responsibility lies with the operating team rather than the use of robots. These misconceptions should be addressed to allow patients to make informed decisions on their choice of surgical approach in any surgery.
In addition, only a minority of patients perceived robotic surgery to be safer (n=138, 29.2%), less painful (n=66, 14.0%), and able to offer better outcomes (n=137, 29.0%). This is unlike the study conducted by Boys et al. [7], which demonstrated that the majority of participants (72.0%) thought that robotic surgery was safer, less painful, and/or offered superior results. This is interesting as Boys et al. included healthcare workers in their survey and one would expect them to be better informed about the technical abilities of the robotic system compared to lay participants included in our study [7]. Unfortunately, there is currently a lack of strong evidence demonstrating the superiority of the robotic approach for most procedures [17]. The majority of the studies demonstrated similar perioperative and oncological outcomes when comparing robotic with laparoscopic surgery [18,19]. As our questionnaire was focused on the understanding of robotic surgery in general, these results may not be reflective of the participants’ understanding of robotic surgery for specific types of surgeries, such as the use of robotic surgery in prostatectomy, which has shown superior outcomes in 12-month urinary continence recovery compared to the laparoscopic approach [20]. This draws attention on the importance of public education to bridge the existing knowledge gaps and misconceptions the public may have on robotic surgery. This also reiterates the need for surgeons and/or other health-care professionals to convey individualized information that is patient-centric to allow informed decision-making on their preference on the type of surgery, which has been found to be inadequate in the local context [21].
Interestingly, the majority of the participants were concerned about the risk of internal damage during robotic surgery due to robotic malfunction (n=373, 79.0%) and the risk of wrong procedure being performed (n=260, 55.1%). This is in stark contrast with the study by Boys et al. [7], where 67.0% and 15.0% of the participants were concerned about the risk of malfunction and wrong procedure being performed, respectively. These differences may reflect the contrasting patient demographics and sociocultural background between the study populations [22]. In addition, their study included participants with health-care background are likely to be more aware of robotic surgery which could have contributed to the differences in results.
About half of the participants (n=221/472, 46.8%) thought that robotic surgery was faster than non-robotic surgery. Although there are studies comparing the speed of robotic surgery versus non-robotic surgery, the majority of the evidence suggest that robotic surgery is slower due to a steep learning curve and time needed for docking of the robot arms [23,24]. These perceptions may be due to the advertisement of robotic surgery, which portrays robotic surgery to be “superior” to conventional laparoscopy or open surgery. Robotic surgery is more precise due to intuitive instrument handling, tremor elimination, and motion scaling [25]. However, these advantages may be easily misunderstood as clear superiority of robotic surgery over its traditional counterparts.
Advancement in medicine in the 21st century has shifted its focus from doctor-centric to patient-centric care with emphasis on patient autonomy and informed decision-making [26]. However, studies have demonstrated that adequacy of informed consent was generally inadequate [21,27]. In addition, there are presently no established guidelines depicting the information required for consent to be valid [28]. This is especially challenging in consent taking for robotic surgery due to the higher technical complexity which may hinder the patient’s ability to comprehend the procedure [11]. The 2015 Montgomery ruling refined the standards of informed consent and emphasized the need of a more patient-centered approach during the informed taking consent [29,30]. This is of greater importance in the context of advances in surgical techniques, where patients need to be educated on the benefits and risks compared to traditional management options. Inadequate consent taking may lead to patient dissatisfaction and compromise the doctor-patient relationship. Furthermore, a local study by Chia et al. in 2019 described the lack of informed consent [21], where less than half of participants were unable to recall serious complications of either hernia repair or laparoscopic cholecystectomy. Multiple clinic consult sessions may be required to ensure adequate understanding of the surgical procedure. Schroeck et al. proposed that this is more pronounced in robotic surgery where patients have higher preconceived expectations and resultingly increased dissatisfaction from their unmet expectations [31]. Our study results demonstrate that doctors need to elevate the health literacy of the patient to eliminate misconceptions about robotic surgery.
Our institution is 1700 bedded hospital and is one of the largest tertiary hospitals in Singapore, with approximately 100 thoracic robotic surgeries, 80–90 urological robotic surgeries, 20–25 gastrointestinal robotic surgeries annually at the point of the study. Our study demonstrated several misconceptions patients had toward robotic surgery; of which may be attributed to the relatively lower volume of robotic surgeries performed annually compared to other high-volume centers worldwide. Hence, our study places emphasis on the knowledge gaps patients may have and the need for adequate explanation before making a decision. This is of greater significance in this digital age where the majority of the people obtain their information through the media (n=205/250, 82.0%) in our study). Collaboration with healthcare workers, industry partners, and media is essential to ensure accurate portrayal of information, clarify misconceptions, and enhance patients’ understanding. For instance, health-care campaigns with online contests may be conducted to promote interest and raise awareness on updates in the surgical field [32]. In addition, videos on robotic surgery in the relevant specialties may be screened in clinics to improve understanding on a particular type of surgery. Use of videos has been shown to improve patients’ understanding in clinical settings and should be considered in both the local and global context [33].
One of the limitations of our study is the possibility of Berkson’s bias due to convenience sampling in a hospital setting and in particular, in a general surgery specialist outpatient clinic, which may not be representative of the general population. Our study also did not collect data on participants who have had robotic surgery previously which may improve their understanding on the topic; however, this is likely to be, at most, only a small number of participants. This study still provides an understanding of the current knowledge gaps people may have and it is likely that these misconceptions may be more pronounced in the community setting due to the lack of exposure to health education. Our survey is also not validated in local population; however, this survey is adopted from existing surveys on knowledge of robotic surgery in a large population. As this is the first study on the perception and knowledge of robotic surgery in Singapore, we are unable to validate any existing surveys. In addition, the study was conducted in English and we did not collect data on the level of literacy in the English language in the participants. This may introduce selection bias toward English-speaking individuals which may not be representative of the general population in Singapore. However, we did collect data on the educational qualifications of participants which provide insight on the demographics of the population and the impact on their level of understanding of robotic surgery. Finally, this is a single-institution study conducted in Singapore which may not be generalizable to other countries. Nevertheless, this reflects the prevalence of a low level of understanding patients have toward robotic surgery in Singapore and it is noteworthy to compare with studies conducted in other countries to compare and contrast the differences to come up with solutions to solve this knowledge gap.
5. Conclusion
Knowledge gaps with regards to robotic surgery in general are apparent, although the extent of knowledge gap is uncertain as it is multifactorial. There is an unmet need to bridge the knowledge gap to improve patients’ understanding of robotic surgery. Collaboration with healthcare workers, industry partners, and media can be made to ensure accurate portrayal of information, clarify misconceptions, and enhance patients’ understanding.
Acknowledgments
We would like to thank Ms Klaryce Lim for her assistance in the administration of the survey and transcription of written data.
Appendix
Survey administered to participants
-
What is your age range? Circle the appropriate option
- 21–40 years
- 41–60 years
- 61–80 years
- >80 years
-
What is your gender? Circle the appropriate option.
- Male
- Female
- Prefer not to comment or disclose
-
What is your education level? Circle the appropriate option.
- Primary school – PSLE or less
- Secondary school
- Diploma
- Degree graduate
- Degree Postgraduate
-
What is your employment status? Circle the appropriate option.
- Unemployed
- Self-employed
- Employee
- Student
- Retired
- Homemaker
- Unable to work
-
What is your ethnicity? Circle the appropriate option.
- Chinese
- Malay
- Indian
- Others
-
What is your type of dwelling? Circle the appropriate option.
-
HDB flat
- 1–3 room
- 4 room
- 5 room
- Executive flats and others
- Condominium and private flats
- Landed property
- Others
-
-
What is your interest level in scientific discoveries (e.g., robots)? Circle the appropriate option
- Very interested
- Somewhat interested
- Not interested
-
Have you ever used or are currently using such robots at home or at work (e.g., vacuum cleaner)? Circle the appropriate option
- Yes, at home
- Yes, at work
- Yes, somewhere else
- No
-
Have you ever had a surgical procedure performed on yourself or a family member? Circle the appropriate option
- Yes
- No
-
Have you heard of robotic surgery? Circle the appropriate option
- Yes
- No (skip to question 13)
-
How or where did you hear of robotic surgery? Circle all that apply
- Friends/relatives
- Your doctor
- Magazine
- Media
- Unsure
- Other (please specify)
-
Which type of surgery is robotic surgery most similar to? Circle the appropriate option.
- Traditional open surgery (big cut over skin)
- Laparoscopic surgery (keyhole surgery, small cuts over skin)
- Laser surgery
-
Which answer best fits with your understanding of robotic surgery? Circle the appropriate option.
- The robot performs the surgery while a trained surgeon stands by and makes sure the robot does things correctly
- The surgeon controls the robotic arms and instruments and does all of the operating
- The surgeon tells the robot what to do and the robot then follows each command
- The surgeon is not present in the operation theatre and robot performs the surgery according to the software program installed
-
Compared to non-robotic surgery, use of the robot is associated with which of the following? Circle all that apply
- The procedure is safer
- The procedure is less painful
- The procedure has better results
- The procedure is faster
- The procedure is costly
- None of the above
-
Robotic malfunction during a surgery: Circle the appropriate option
- Has never occurred
- Has occurred
- Unsure
-
If you needed surgery and it could be done with a robot, would you prefer that the robot be used? Circle the appropriate option
- Yes
- No
-
Do you have any of the following concerns about surgery by a robot? Circle all that apply
- The robot malfunctions causing internal damage during the surgery
- The robot does the wrong operation on you
- Other (please specify):
-
Do you think surgeons that use the robot are: Circle the appropriate option
- More skilled than surgeons that do not use the robot
- Similar in skill to surgeons that do not use the robot
- Less skilled than surgeons that do not use the robot
-
Do you think that hospitals that have a robot are: Circle the appropriate option
- Better hospitals than those that do not have robot
- Similar to hospitals that do not have a robot
- Worse hospitals than those that do not have a robot.
Conflict of Interest
All of the authors declare no conflicts of interest.
Ethics Approval
Consent to participate
Written consent was obtained from all participants. All results which are described deidentified data.
Consent for publication
All participants are aware that the study is conducted for the purpose of research and this is also described in the written consent.
Availability of data and material
Data will not be publicly available; however, requests may be made to the corresponding author.
References
- [1].Nilsson G, Larsson S, Johnsson F. Randomized Clinical Trial of Laparoscopic Versus Open Fundoplication:Blind Evaluation of Recovery and Discharge Period. Br J Surg. 2000;87:873–8. doi: 10.1046/j.1365-2168.2000.01471.x. [DOI] [PubMed] [Google Scholar]
- [2].Mori KM, Neubauer NL. Minimally Invasive Surgery in Gynecologic Oncology. ISRN Obstet Gynecol. 2013;2013:312982. doi: 10.1155/2013/312982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Intuitive Surgery Inc. The Da Vinci Surgery Experience. California: Intuitive Surgery Inc; 2013. pp. 10–1. [Google Scholar]
- [4].Agha R, Muir G. Does Laparoscopic Surgery Spell the End of the Open Surgeon? J R Soc Med. 2003;96:544–6. doi: 10.1258/jrsm.96.11.544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Chu CM, Agrawal A, Mazloomdoost D, Barenberg B, Dune TJ, Pilkinton ML, et al. Patients'Knowledge of and Attitude Toward Robotic Surgery for Pelvic Organ Prolapse. Female Pelvic Med Reconstruct Surg. 2019;25:279–83. doi: 10.1097/SPV.0000000000000556. [DOI] [PubMed] [Google Scholar]
- [6].Ahmad A, Ahmad ZF, Carleton JD, Agarwala A. Robotic Surgery:Current Perceptions and the Clinical Evidence. Surg Endosc. 2017;31:255–63. doi: 10.1007/s00464-016-4966-y. [DOI] [PubMed] [Google Scholar]
- [7].Boys JA, Alicuben ET, DeMeester MJ, Worrell SG, Oh DS, Hagen JA, et al. Public Perceptions on Robotic Surgery, Hospitals with Robots, and Surgeons that Use Them. Surg Endosc. 2016;30:1310–6. doi: 10.1007/s00464-015-4368-6. [DOI] [PubMed] [Google Scholar]
- [8].Markar SR, Kolic I, Karthikesalingam AP, Wagner O, Hagen ME. International Survey Study of Attitudes Towards Robotic Surgery. J Robotic Surg. 2012;6:231–5. doi: 10.1007/s11701-011-0301-8. [DOI] [PubMed] [Google Scholar]
- [9].Jassim SS, Benjamin-Laing H, Douglas SL, Haddad FS. Robotic and Navigation Systems in Orthopaedic Surgery:How Much do Our Patients Understand? Clin Orthop Surg. 2014;6:462–7. doi: 10.4055/cios.2014.6.4.462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].McDermott H, Choudhury N, Lewin-Runacres M, Aemn I, Moss E. Gender Differences in Understanding and Acceptance of Robot-assisted Surgery. J Robotic Surg. 2020;14:227–32. doi: 10.1007/s11701-019-00960-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Ferrarese A, Pozzi G, Borghi F, Pellegrino L, Di Lorenzo P, Amato B, et al. Informed Consent in Robotic Surgery:Quality of Information and Patient Perception. Open Med (Warsaw, Poland) 2016;11:279–85. doi: 10.1515/med-2016-0054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].American Association for Public Opinion Research. Standard Definitions:Final Dispositions of Case Codes and Outcome Rates for Surveys. United States: American Association for Public Opinion Research; 2011. [Google Scholar]
- [13].European Commission. Special Eurobarometer 382:Public Attitudes Towards Robots. United States: European Commission; 2012. [Google Scholar]
- [14].Dolnicar S, Grün B, Leisch F. Quick, Simple and Reliable:Forced Binary Survey Questions. Int J Market Res. 2011;53:231–52. [Google Scholar]
- [15].Yip SK, Sim HG. Robotic Radical Prostatectomy in East Asia:Development, Surgical Results and Challenges. Curr Opin Urol. 2010;20:80–5. doi: 10.1097/MOU.0b013e3283337bf0. [DOI] [PubMed] [Google Scholar]
- [16].Irani M, Prabakar C, Nematian S, Julka N, Bhatt D, Bral P. Patient Perceptions of Open, Laparoscopic, and Robotic Gynecological Surgeries. BioMed Res int. 2016;2016:4284093. doi: 10.1155/2016/4284093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Ghezzi TL, Corleta OC. 30 Years of Robotic Surgery. World J Surg. 2016;40:2550–7. doi: 10.1007/s00268-016-3543-9. [DOI] [PubMed] [Google Scholar]
- [18].Prete FP, Pezzolla A, Prete F, Testini M, Marzaioli R, Patriti A, et al. Robotic Versus Laparoscopic Minimally Invasive Surgery for Rectal Cancer:A Systematic Review and Meta-analysis of Randomized Controlled Trials. Ann Surg. 2018;267:1034–46. doi: 10.1097/SLA.0000000000002523. [DOI] [PubMed] [Google Scholar]
- [19].Mäenpää MM, Nieminen K, Tomás EI, Laurila M, Luukkaala TH, Mäenpää JU. Robotic-assisted vs Traditional Laparoscopic Surgery for Endometrial Cancer:A Randomized Controlled Trial. Am J Obstet Gynecol. 2016;215:588. e581–7. doi: 10.1016/j.ajog.2016.06.005. [DOI] [PubMed] [Google Scholar]
- [20].Chan KS, Wang ZK, Syn N, Goh BK. Learning Curve of Laparoscopic and Robotic Pancreas Resections:A Systematic Review. Surgery. 2021;170:194–206. doi: 10.1016/j.surg.2020.11.046. [DOI] [PubMed] [Google Scholar]
- [21].Chia CL, Chan KS, Ng MJ, Rao AD, Singaporewalla R. Assessing Adequacy of Informed Consent for Elective Surgery by Student-administered Interview. ANZ J Surg. 2019;89:677–82. doi: 10.1111/ans.15214. [DOI] [PubMed] [Google Scholar]
- [22].Lin CC, Lai YL, Ward SE. Effect of Cancer Pain on Performance Status, Mood States, and Level of Hope Among Taiwanese Cancer Patients. J Pain Symptom Manage. 2003;25:29–37. doi: 10.1016/s0885-3924(02)00542-0. [DOI] [PubMed] [Google Scholar]
- [23].Chan KS, Wang ZK, Syn N, Goh BK. Learning Curve of Laparoscopic and Robotic Pancreas Resections:A Systematic Review. Surgery. 2021;170:194–206. doi: 10.1016/j.surg.2020.11.046. [DOI] [PubMed] [Google Scholar]
- [24].Rocco B, Matei DV, Melegari S, Ospina JC, Mazzoleni F, Errico G, et al. Robotic vs Open Prostatectomy in a Laparoscopically Naive Centre:A Matched?pair Analysis. BJU Int. 2009;104:991–5. doi: 10.1111/j.1464-410X.2009.08532.x. [DOI] [PubMed] [Google Scholar]
- [25].Randell R, Alvarado N, Honey S, Greenhalgh J, Gardner P, Gill A, et al. Impact of Robotic Surgery on Decision Making:Perspectives of Surgical Teams. AMIA Annu Symp Proc. 2015;2015:1057–66. [PMC free article] [PubMed] [Google Scholar]
- [26].Deber RB, Kraetschmer N, Irvine J. What Role do Patients Wish to Play in Treatment Decision Making? Arch Intern Med. 1996;156:1414–20. [PubMed] [Google Scholar]
- [27].Falagas ME, Korbila IP, Giannopoulou KP, Kondilis BK, Peppas G. Informed Consent:How Much and what do Patients Understand? Am J Surg. 2009;198:420–35. doi: 10.1016/j.amjsurg.2009.02.010. [DOI] [PubMed] [Google Scholar]
- [28].Mallardi V. The Origin of Informed Consent. Acta Otorhinolaryngol Ital. 2005;25:312–327. [PubMed] [Google Scholar]
- [29].Coulter A, Hopkins A, Moulton B. Montgomery v Lanarkshire Health Board:Transforming Informed Consent. Bull R Coll Surg Engl. 2017;99:36–8. [Google Scholar]
- [30].Chan SW, Tulloch E, Cooper ES, Smith A, Wojcik W, Norman JE. Montgomery and Informed Consent:Where Are we Now? BMJ. 2017;357:2224. doi: 10.1136/bmj.j2224. [DOI] [PubMed] [Google Scholar]
- [31].Schroeck FR, Krupski TL, Sun L, Albala DM, Price MM, Polascik TJ, et al. Satisfaction and Regret after Open Retropubic or Robot-assisted Laparoscopic Radical Prostatectomy. Eur Urol. 2008;54:785–93. doi: 10.1016/j.eururo.2008.06.063. [DOI] [PubMed] [Google Scholar]
- [32].Steele SR, Arshad S, Bush R, Dasani S, Cologne K, Bleier JI, et al. Social Media is a Necessary Component of Surgery Practice. Surgery. 2015;158:857–62. doi: 10.1016/j.surg.2015.06.002. [DOI] [PubMed] [Google Scholar]
- [33].Brock TP, Smith SR. Using Digital Videos Displayed on Personal Digital Assistants (pdas) to Enhance Patient Education in Clinical Settings. Int J Med Inform. 2007;76:829–35. doi: 10.1016/j.ijmedinf.2006.09.024. [DOI] [PubMed] [Google Scholar]


