Abstract
Objective:
To evaluate final posttreatment occlusion in patients with complete unilateral cleft lip and palate (cUCLP) by comparing (1) 3 treatment centers, (2) males and females, (3) cleft and noncleft sides, (4) right- and left-sided clefts, and (5) orthodontic treatment with/without orthognathic surgery (OS).
Design:
Retrospective cohort study.
Patients:
Blinded posttreatment dental casts of 56 patients (19.4 ± 1.4 years) with cUCLP from 3 centers in Switzerland.
Main Outcome Measure:
Occlusal assessment using the modified Huddart/Bodenham (MHB) index.
Results:
Our sample comprised 35 males and 21 females, 46 with left- and 10 with right-sided clefts, of which 32 had undergone OS. The final posttreatment occlusion showed a median MHB score of 0 (interquartile range: −1.0 to 2.0) in the total sample and did not seem to depend on treatment center, sex, or OS. The MHB scores for the anterior buccal and the buccal segments were more negative on the cleft than on the noncleft side (P = .002 and P = .006, respectively). When the cleft was on the left side, the MHB score tended to be more positive in the labial (P = .046) and anterior buccal segments (P = .034).
Conclusions:
This study shows a very satisfactory final posttreatment occlusion in patients with cUCLP. The more constricted buccal occlusion on the cleft side emphasizes the attention that should be given in correcting the more medially positioned lesser maxillary segment. The influence of cleft-sidedness should be analyzed further on a sample including more patients with right-sided clefts.
Keywords: Treatment outcome, final post-treatment, dental occlusion, dental arch relationships, crossbite, cleft lip and palate, multicentre study
Introduction
Cleft lip and palate is a common congenital facial malformation with a prevalence of about 0.7 per 1000 newborns worldwide (IPDTOC Working Group, 2011). Patients with a cleft show a wide range of aesthetic and morphological malformations as well as functional impairments (Vargervik, 1981; Evans, 2004; Mossey et al., 2009). Following initial cleft diagnosis, parents are often concerned about the facial appearance of their child, as well as their potential functional limitations and psychosocial well-being. An interdisciplinary team approach is recommended from birth until adulthood (Evans, 2004). For the parents, the patient, and the multidisciplinary team alike, an optimal final posttreatment outcome is desired.
In this particular population, malocclusions with varying degrees of severity are common, resulting from midface deficiency, maxillary arch constriction, and congenitally missing and malformed teeth (Vargervik, 1981; Evans, 2004; Antonarakis & Fisher, 2015). Several studies have been carried out looking at dental arch relationships in patients with clefts and their development over time in relation to growth and treatment. The final posttreatment occlusion, however, has not received much attention, either because patient samples studied are often too young to have completed growth and their full treatment protocol or because patients who have undergone combined orthodontic/surgical treatment are assessed with regard to the surgical outcome rather than occlusion. Using a cohort design, the Americleft studies investigated patients between 6 and 12 years of age before the start of active orthodontic treatment (Hathaway et al., 2011). The Dutchcleft studies looking at patients with complete unilateral cleft lip and palate (cUCLP) assessed the transverse dental arch relationships from the deciduous dentition until the age of 12 years, with or without a first phase of orthodontic treatment having already been undertaken (Bongaarts et al., 2004; Noverraz et al., 2015). In the United Kingdom, occlusal outcomes were evaluated after the completion of fixed appliance treatment; however, cases that had required orthognathic surgery were excluded (Deacon et al., 2007). In 2 studies, namely the Eurocleft project that looked at patients with cUCLP (Mølsted et al., 2005) and a Dutch study including patients with bilateral CLP (Heidbuchel & Kuijpers-Jagtman, 1997), dental arch relationships were assessed until the age of 17 years. However, in both of these studies, at the time of evaluation, there were several patients still needing maxillary osteotomies, meaning that the overall treatment had not yet been completed and thus final posttreatment occlusion could not be assessed. Few recent studies assessing posttreatment occlusion, including combined orthodontic/surgical cases, are available in the literature (Marcusson & Paulin, 2004; Trimetsuntorn et al., 2020); nevertheless, the latter sample consisted of different cleft types with few participants in each subgroup.
The lack of studies analyzing final posttreatment outcome in patients with clefts highlights the difficulties in obtaining homogeneous cohorts (with regard to cleft type and treatment protocol) with reasonable sample sizes and standardized final records. In order to evaluate the effects of interdisciplinary treatment protocols, along with the effects of different treatment options (eg, Mueller et al., 2012; Peanchitlertkajorn et al., 2018), it is indispensable to critically assess the final posttreatment outcome. This allows one to adequately inform the patient/parents using the best available evidence. This especially applies to complex, time-consuming, and expensive treatments, as is the case with orthodontic treatment, combined with orthognathic surgery if necessary.
The aim of the present study was to evaluate final posttreatment occlusion in patients with cUCLP by comparing the outcome among (1) 3 treatment centers in Switzerland, (2) males and females, (3) the cleft and noncleft sides, (4) right- and left-sided clefts, and (5) orthodontic treatment with or without combined orthognathic surgery.
Methods
Ethical approval was granted for the present study by the cantonal Research Ethics Board of Zurich, Switzerland (N°KEK-StV-Nr. 20/14). For the present retrospective study, data from the medical records and final posttreatment dental casts of patients with cUCLP at adulthood were obtained from 3 centers (Geneva, Lausanne, Zurich). Inclusion criteria were patients of Caucasian descent with a nonsyndromic cUCLP, without the presence of other congenital facial anomalies besides the cleft.
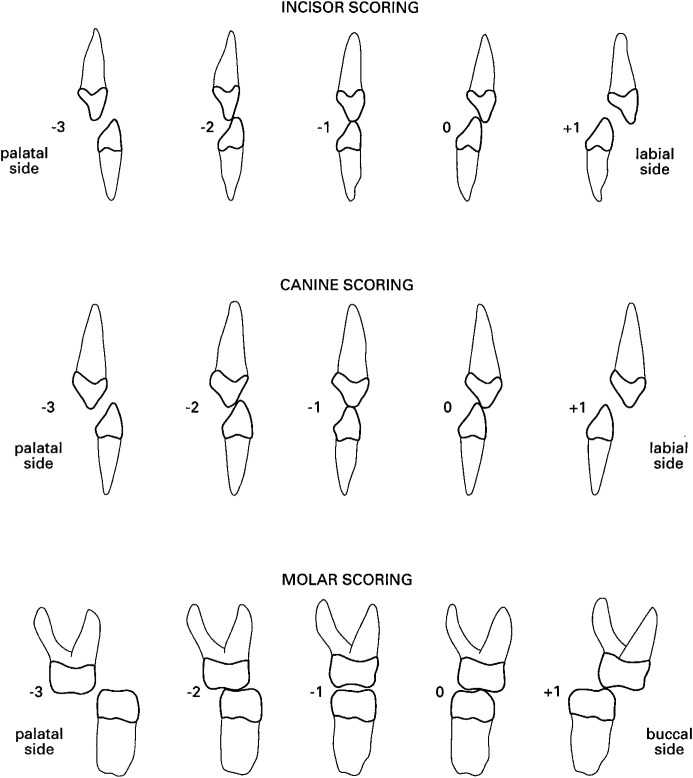
Dental casts were collected, duplicated, trimmed so as to create standardized bases with a predefined size, and coded for blinding purposes. The occlusion was assessed by one examiner (J.B.), using the modified Huddart/Bodenham (MHB) index (Huddart & Bodenham, 1972; Mossey et al., 2003; Bongaarts et al., 2004; Gray & Mossey, 2005; Altalibi et al., 2013). The MHB index was measured for the labial segment (central incisors), the 2 anterior buccal segments (canine and first premolar on the cleft and noncleft sides), and the 2 buccal segments (canine to first permanent molar on the cleft and noncleft sides). The lateral incisors were not assessed as they are often absent in patients with cleft lip and palate. Each of the 10 upper teeth received a score depending on their position relative to the antagonist teeth (normal occlusion: 0; edge-to-edge position: −1; crossbite with contact: −2; crossbite without contact: −3; increased overjet or buccal occlusion: +1; Figure 1). A tooth was considered in crossbite (or in edge-to-edge position) when at least half of its width was in crossbite (or in an edge-to-edge position; Staudt & Kiliaridis, 2009). All 10 assessments per patient were added to obtain a cumulative total score and also divided into labial, anterior buccal, and buccal segments.
Figure 1.
Modified Huddart/Bodenham (MHB) index for incisors, canines, and premolars/molars (Bongaarts et al., 2004, permission for use of figure obtained from The Cleft Palate-Craniofacial Journal).
Overjet and overbite were measured with calipers at the central incisor of the cleft and noncleft sides. The largest value determined the maximum overjet and overbite, respectively. The deviation of the maxillary midline was measured with respect to the mandibular midline. Deviation to the noncleft side was given a positive score and deviation to the cleft side a negative score.
The sagittal canine and molar relationships were scored according to the Angle classification. Class I occlusion was scored as 0, class II scored in positive premolar widths, and class III in negative premolar widths. A quarter premolar width was scored as 1, half as 2, three quarters as 3, and a full premolar width as 4 (Bongaarts et al. 2004).
In order to assess intrarater reliability, the measurements were repeated, by the same examiner, on 16 dental casts of randomly chosen subjects after an interval of at least 2 weeks.
Statistics
Descriptive statistics of outcome variables were calculated as quartiles, including median and interquartile range (IQR), while age was reported as mean and SD.
The effect of each of the independent variables “center,” “sex,” “cleft sidedness,” and “orthognathic surgery” was tentatively tested on each of the outcome variables “MHB score,” “overjet,” “overbite,” “midline deviation,” “canine and molar relationship” using Kruskal-Wallis or Wilcoxon rank sum test, respectively. For theses outcome variables, intrasubject differences between cleft and noncleft sides were also assessed using Wilcoxon signed-rank statistics and all results were tabulated (cf. Tab. 2 with Supplemental Appendix). Additionally, Spearman correlations were computed to estimate the associations between the MHB score and secondary outcome variables such as overjet and overbite.
Intrarater reliability was assessed on the subset of repeated measurements. Linearly weighted Cohen κ was used for ordinal variables, including the MHB score at every tooth site separately as well as for canine and molar relationships. For continuous variables such as overjet, overbite, and midline deviation (mm), the intraclass correlation coefficient (ICC) was used. All calculations were performed with the statistical software R (R Core Team, 2020), including the package “irr” (Gamer et al., 2020), and the significance level α was set at .05.
Results
Sample
The total sample consisted of dental casts from 56 patients (mean age: 19.4 ± 1.4 years), 35 of which were males and 21 females (sex ratio M/F: 1.7). Forty-six patients presented with a left-sided cleft (82%) and 10 patients (18%) with a right-sided cleft. In 24 patients (43%), orthodontic treatment had been carried out without orthognathic surgery. A combined orthodontic/orthognathic surgical treatment had been undertaken in 32 patients (57%: 20 males and 12 females). In 30 of these cases, the cleft was left-sided, while in 2, it was right-sided (Table 1).
Table 1.
Sample Description.
| Number | Age, mean (SD) | Sex | Cleft side | |||
|---|---|---|---|---|---|---|
| Male | Female | Left | Right | |||
| Center 1 | 8 | 18.3 (1.1) | 7 | 1 | 5 | 3 |
| Surgery (yes/no) | (2/6) | (2/5) | (0/1) | (1/4) | (1/2) | |
| Center 2 | 22 | 19.0 (1.8) | 14 | 8 | 15 | 7 |
| Surgery (yes/no) | (7/15) | (6/8) | (1/7) | (6/9) | (1/6) | |
| Center 3 | 26 | 20.0 (0.6) | 14 | 12 | 26 | 0 |
| Surgery (yes/no) | (23/3) | (12/2) | (11/1) | (23/3) | (0/0) | |
| Total | 56 | 19.4 (1.4) | 35 | 21 | 46 | 10 |
| Surgery (yes/no) | (32/24) | (20/15) | (12/9) | (30/16) | (2/8) | |
Group 1 (treatment center 1; University of Geneva)
Treatment center 1 provided dental casts from 8 patients (7 males; 1 female), 5 of which were from left-sided cUCLP and 3 from right-sided cUCLP. The mean age of this subsample was 18.3 ± 1.1 years.
In this center, lip repair was performed according to Tennison at about 3 months of age and palate closure (both hard and soft palate) according to Veau (7 patients) or Widmaier (1 patient) at about 12 months of age. During the early mixed dentition, 6 patients underwent orthodontic palatal expansion. Alveolar bone grafting with cancellous bone from the iliac crest was performed at about 9 years of age, before the eruption of the permanent canine. In the permanent dentition, fixed orthodontic treatment was undertaken for arch alignment. The orthodontic treatment was provided by postgraduate students in orthodontic training, supervised by the cleft lip and palate team orthodontist. Two patients (25%) had orthognathic surgery (LeFort I) at the end of growth.
Group 2 (treatment center 2; Lausanne)
Treatment center 2 provided dental casts from 22 patients (14 males; 8 females), 15 of which were from left-sided cUCLP and 7 from right-sided cUCLP. The mean age of this subsample was 19.0 ± 1.8 years.
In this center, a passive orthopedic plate (without extension into the soft palate) was used in the neonatal period. Primary surgery was performed according to Malek, with soft palate closure at about 3 months of age and lip, alveolus, and hard palate closure at about 6 months of age. During the early mixed dentition, orthodontic palatal expansion was performed in 18 patients. Alveolar bone grafting with cancellous bone from the iliac crest was performed at about 9 years of age, before the eruption of the permanent canine. In the permanent dentition, fixed orthodontic treatment was undertaken for arch alignment by the same cleft lip and palate team orthodontist in all patients. Surgically assisted rapid maxillary expansion was carried out in 2 patients. Orthognathic surgery was performed at the end of growth in 7 patients (32%), with LeFort I having been undertaken in 6 patients and bimaxillary surgery in 1.
Group 3 (treatment center 3; University of Zurich)
Treatment center 3 provided dental casts from 26 patients (14 males; 12 females), all of which were from left-sided cUCLP. The mean age of this subsample was 20.0 ± 0.6 years.
The treatment in this center involved the placement of a passive orthopedic plate with extension into the soft palate after birth. Primary surgery with lip repair according to Millard-Perko was performed at about 6 months of age, soft palate closure according to Widmaier-Perko at about 18 months of age, and hard palate closure with a mucoperiosteal flap at about 4.5 years of age. No orthodontic appliances were used during the mixed dentition. Alveolar bone grafting, mainly with cancellous bone from the iliac crest, was performed before (11 patients) or after (10 patients) the eruption of the permanent canine. In 5 patients, grafting was performed both before and after the eruption of the permanent canine. It was only in the permanent dentition that fixed orthodontic treatment was started, performed by the cleft lip and palate team orthodontist or by different collaborating orthodontists in private practices. Two patients underwent surgically assisted rapid maxillary expansion. Twenty-three patients (88%) underwent orthognathic surgery after the cessation of growth, with a Le Fort I osteotomy being performed in 7 patients and bimaxillary surgery in 16 patients.
Measurements
Intrarater reliability was very good for the performed measurements (κ = 1.00, ICC = 1.00). Descriptive statistics are shown for the total sample, comprising the MHB score for all teeth (median: 0.0; lower quartile: −1.0; upper quartile: 2.0), as well as for the different segments respectively (Tab. 2 with Supplemental Appendix). This is similarly shown for the various subgroups, namely comparing different centers, sex, orthodontics with or without orthognathic surgery, cleft to noncleft side, and cleft-sidedness.
Center 1 versus 2 versus 3
The treatment center did not seem to influence the final posttreatment occlusion assessed by the MHB index (total arch P = .495; labial segment P = .402; cleft-sided and noncleft-sided buccal segment P = .803 and P = .788, respectively). Concerning the sagittal occlusion, in center 3, the molars on both sides tended to occlude more often in a class II relationship than in centers 1 and 2 where a class I relationship was most frequent (cleft side: P < .001; noncleft side: P = .002; Tab. 2 with Supplemental Appendix).
Sex
No significant difference was observed comparing males to females (eg, total arch MHB score: median 0 and 0, respectively, P = .440).
Orthognathic Surgery
No significant differences in the occlusion were found based on the decision to perform orthognathic surgery or not, as long as the cleft and noncleft sides were looked at together (eg, total arch MHB score: median 0.5 and 0, respectively, P = .470; Table 2). Differences between the cleft side and noncleft side in this respect are detailed below.
Table 2.
Descriptive Statistics.
| Minimum | Lower quartile | Median | Upper quartile | Maximum |
IQR |
P value | |||
|---|---|---|---|---|---|---|---|---|---|
| q.0% | q.25% | q.50% | q.75% | q.100% | |||||
| Total sample | CS + NCS | ||||||||
| MHB all (teeth 1 + 3 + 4 + 5 + 6) | CS + NCS | −5.00 | −1.00 | 0.00 | 2.00 | 4.00 | 3.00 | ||
| MHB labial (tooth 1) | CS + NCS | −2.00 | 0.00 | 1.00 | 2.00 | 2.00 | 2.00 | ||
| MHB anterior buccal (teeth 3 + 4) | CS + NCS | −5.00 | 0.00 | 0.00 | 0.00 | 2.00 | 0.00 | ||
| MHB buccal (teeth 3 + 4 + 5 + 6) | CS + NCS | −5.00 | −1.00 | 0.00 | 0.00 | 2.00 | 1.00 | ||
| Overjet maximum (mm) | CS + NCS | 0.00 | 1.00 | 1.50 | 2.00 | 3.50 | 1.00 | ||
| Overbite maximum (mm) | CS + NCS | −0.50 | 1.00 | 2.00 | 2.50 | 5.00 | 1.50 | ||
| Midline deviation (mm) | CS + NCS | −4.50 | −0.13 | 0.00 | 1.00 | 2.50 | 1.13 | ||
| Cleft side versus noncleft side | CS/NCS | ||||||||
| MHB all (teeth 1 + 3 + 4 + 5 + 6) | CS | −5.00 | −1.00 | 0.00 | 1.00 | 2.00 | 2.00 | .006 | |
| NCS | −4.00 | 0.00 | 0.00 | 1.00 | 3.00 | 1.00 | |||
| MHB labial (tooth 1) | CS | −1.00 | 0.00 | 0.00 | 1.00 | 1.00 | 1.00 | .043 | |
| NCS | −3.00 | 0.00 | 0.50 | 1.00 | 1.00 | 1.00 | |||
| MHB anterior buccal (teeth 3 + 4) | CS | −4.00 | 0.00 | 0.00 | 0.00 | 1.00 | 0.00 | .002 | |
| NCS | −1.00 | 0.00 | 0.00 | 0.75 | 2.00 | 0.75 | |||
| MHB buccal (teeth 3 + 4 + 5 + 6) | CS | −5.00 | −1.00 | 0.00 | 0.00 | 1.00 | 1.00 | .006 | |
| NCS | −2.00 | 0.00 | 0.00 | 0.00 | 2.00 | 0.00 | |||
| Overjet (mm) | CS | 0.00 | 0.50 | 1.00 | 1.50 | 3.50 | 1.00 | <.001 | |
| NCS | −3.00 | 1.00 | 1.50 | 2.00 | 3.50 | 1.00 | |||
| Overbite (mm) | CS | 0.00 | 1.00 | 1.50 | 2.50 | 5.00 | 1.50 | .848 | |
| NCS | −1.00 | 0.88 | 1.50 | 2.50 | 5.00 | 1.62 | |||
| Canine relationship | CS | −1.00 | 3.00 | 4.00 | 4.00 | 8.00 | 1.00 | <.001 | |
| NCS | 0.00 | 0.00 | 0.00 | 2.00 | 6.00 | 2.00 | |||
| Molar relationship | CS | −5.00 | 0.00 | 4.00 | 5.00 | 10.00 | 5.00 | <.001 | |
| NCS | −4.00 | 0.00 | 0.00 | 4.00 | 9.00 | 4.00 | |||
| Cleft sidedness: left versus right | Left/right | CS + NCS | |||||||
| MHB all (teeth 1 + 3 + 4 + 5 + 6) | Left | CS + NCS | −5.00 | −0.75 | 0.50 | 2.00 | 4.00 | 2.75 | .056 |
| Right | −2.00 | −2.00 | 0.00 | 0.00 | 2.00 | 2.00 | |||
| MHB labial (tooth 1) | Left | CS + NCS | −2.00 | 0.00 | 1.00 | 2.00 | 2.00 | 2.00 | .046 |
| Right | −2.00 | 0.00 | 0.00 | 0.00 | 2.00 | 0.00 | |||
| MHB anterior buccal (teeth 3 + 4) | Left | CS + NCS | −3.00 | 0.00 | 0.00 | 1.00 | 2.00 | 1.00 | .034 |
| Right | −5.00 | −1.75 | 0.00 | 0.00 | 0.00 | 1.75 | |||
| MHB buccal (teeth 3 + 4 + 5 + 6) | Left | CS + NCS | −5.00 | −1.00 | 0.00 | 0.50 | 2.00 | 1.50 | .164 |
| Right | −5.00 | −2.00 | 0.00 | 0.00 | 0.00 | 2.00 | |||
| Overjet maximum (mm) | Left | CS + NCS | 0.00 | 1.00 | 1.50 | 2.00 | 3.50 | 1.00 | .008 |
| Right | 0.00 | 0.50 | 1.00 | 1.00 | 2.00 | 0.50 | |||
| Overbite maximum (mm) | Left | CS + NCS | 0.00 | 1.50 | 2.00 | 2.50 | 5.00 | 1.00 | .330 |
| Right | −0.50 | 0.50 | 1.50 | 2.50 | 3.00 | 2.00 | |||
| Midline deviation (mm) | Left | CS + NCS | −4.50 | −0.50 | 0.00 | 1.00 | 2.50 | 1.50 | .973 |
| Right | −3.50 | 0.00 | 0.00 | 0.75 | 1.00 | 0.75 |
Abbreviations: CS, cleft side; IQR, interquartile range; MHB, modified Huddart/Bodenham; NCS, noncleft side.
Cleft side versus noncleft side
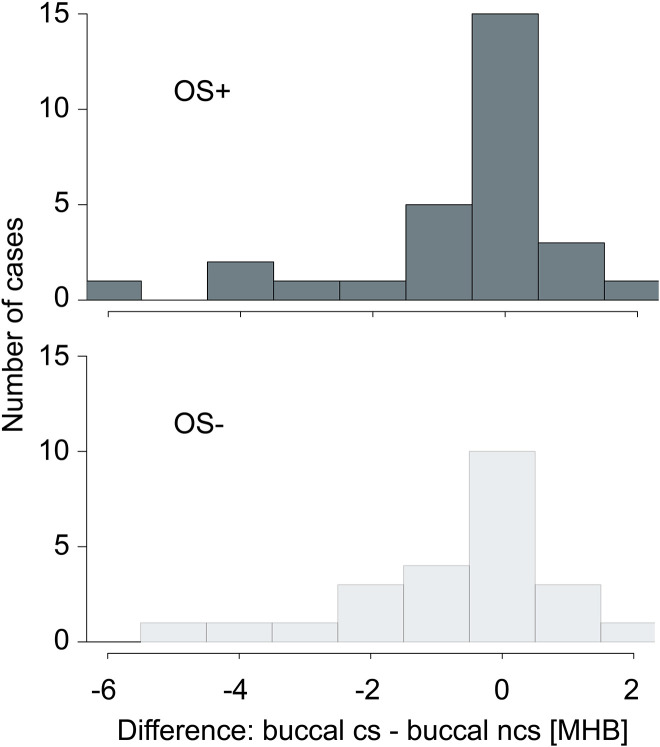
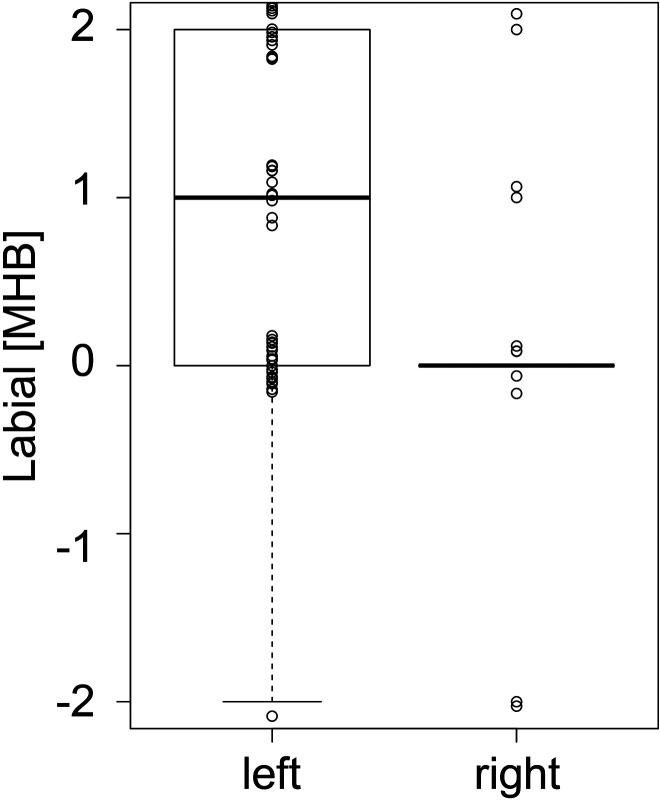
When comparing the cleft side to the noncleft side, the MHB score on the cleft side tended to be more negative overall (P = .006), in the anterior buccal (P = .002), and the buccal segme nts (P = .006; Table 2). In most cases, there seemed to be no difference between the cleft side and the noncleft side, but when a difference was observed, the value on the cleft side was more frequently smaller than the one on the noncleft side (Figure 2). When looking at the patients with orthodontic treatment without orthognathic surgery (n = 24) and those with orthodontic treatment combined with orthognathic surgery (n = 32) separately, the 2 histograms were similar in shape (Figure 3).
Figure 2.
Cleft side versus noncleft side: difference between the buccal segment (teeth 3 + 4 + 5 + 6) on the cleft side (CS) and on the noncleft side (NCS) (modified Huddart/Bodenham index = MHB).
Figure 3.
Cleft side versus noncleft side: difference between the buccal segment (teeth 3 + 4 + 5 + 6) on the cleft side (CS) and on the noncleft side (NCS) (modified Huddart/Bodenham index = MHB) for patients who underwent orthognathic surgery (OS+; top graph) and patients who did not undergo orthognathic surgery (OS−; bottom graph).
The median MHB score of the labial segment was 0 on the cleft side and 0.5 on the noncleft side (P = .043; Table 2). On the noncleft side, the MHB labial score for the subgroup with orthognathic surgery was 1.0 points higher than in patients without orthognathic surgery (P = .016; Table 2).
A moderate correlation was found between the labial MHB score and the maximum overjet (r = 0.51, P < .001). This was also the case when looking at the cleft and noncleft sides individually (cleft side: r = 0.62, P < .001; noncleft side r = 0.59, P < .001). The median overjet tended to be larger on the noncleft compared to the cleft side (1.5 vs 1.0 mm, P < .001; Table 2), as well as on the noncleft side in those having undergone orthognathic surgery (1.5 vs 1.0 mm in those without orthognathic surgery, P = .024; Table 2).
A deviation of the maxillary midline with respect to the mandibular midline was found in 59% of cases. In only 18% of cases, however, the deviation was greater than 1.5 mm. A tendency of midline deviation toward one side (ie, toward the noncleft side vs the cleft side) was not observed (median: 0 mm; IQR: 1.13 mm). Moreover, midline deviation did not seem to depend on whether the patient had undergone orthognathic surgery (P = .119; Table 2).
On the cleft side, the median canine and molar relationship was full class II, whereas on the noncleft side, this was in a class I (P < .001, respectively; Table 2). In the subsample with orthognathic surgery, the occlusion seemed to be similar (cleft side: class II; noncleft side: more class I) but significantly different from the occlusion in the group without orthognathic surgery (cleft side: class II canines, class I molars; noncleft side: class I; for P values cf. Table 2 with Supplemental Appendix).
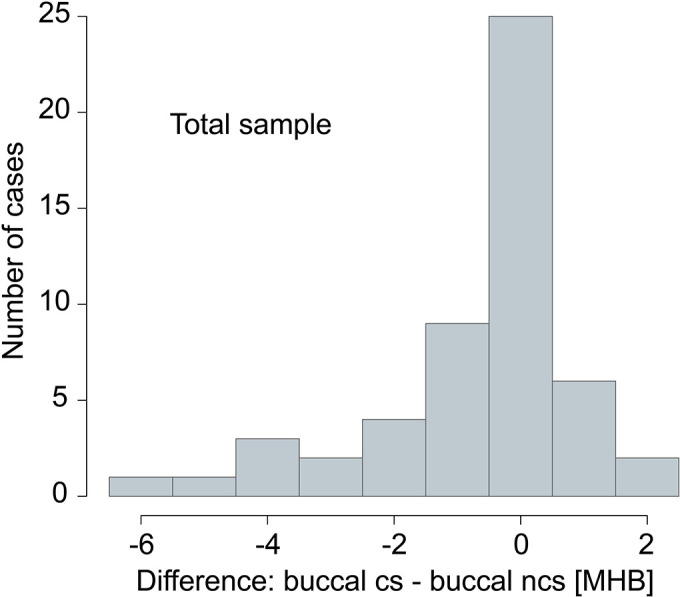
Cleft-sidedness
When left-sided clefts were compared to right-sided clefts, our results suggest that the total MHB score was more positive in left-sided clefts, with borderline significance (P = .056). Looking only at the labial segment, however, there was a statistically significant difference (median MHB score difference of 1.0, P = .046), with a more positive score seen for left-sided clefts (Table 2, Figure 4). When looking at each of the central incisors separately, the median MHB score for the central incisor on the noncleft side tended to be higher (+1) in left-sided compared to right-sided clefts (P = .016; Table 2). Similarly, our results suggest that for the anterior buccal segment, left-sided clefts tended to have more positive MHB scores, whereas right-sided clefts tended to have more negative MHB scores (P = .034; Table 2).
Figure 4.
Cleft sidedness: labial segment (teeth 1 + 1) in patients with left-sided cleft (left) versus patients with right-sided clefts (right) (modified Huddart/Bodenham index = MHB). Higher MHB scores in left-sided clefts compared to right-sided clefts (P = .046). (In this figure, the values have been dragged apart from each other for better visualization.)
In addition, the maximum overjet tended to be 0.5 mm larger when the cleft was on the left side (P = .008). This was also apparent when looking at the overjet on the cleft-sided incisor (median difference of 0.5 mm; P = .017) and noncleft-sided incisor (median difference of 1.0 mm; P = .002) separately.
Discussion
This Swiss intercenter study reveals a very satisfactory final posttreatment occlusion in patients with cUCLP. When comparing our results to MHB scores obtained from other investigations in younger patients (mean total MHB score at 12 years from −3.6 to −4.1, Noverraz et al., 2015; mean total MHB score at 8 years from −7.1 to −10.1, Karsten et al., 2020), it seems that orthodontic treatment with or without orthognathic surgery in the permanent dentition, as performed in our centers, was of benefit for the final occlusion. In addition, the difference between the cleft side and noncleft side seems to be reduced compared to the above-mentioned studies (mean MHB score at 12 years: cleft side: −3.0, noncleft side: −0.6, Noverraz et al., 2015; mean total MHB score at 8 years: cleft side from −4.3 to −5.2, noncleft side from −0.9 to −2.4, Karsten et al., 2020). Our results are also encouraging compared to patients of the same age (total MHB score ≤ −4 in 44%), keeping in mind different weighting of negative MHB scores (Marcusson & Paulin, 2004).
No significant difference in MHB score could be found among the treatment results from the 3 centers under investigation. However, due to the fact that the initial cleft severity was unknown to us and might have differed between the centers, our results do not necessarily imply similar treatment quality among the centers. Each center decided according to its own criteria which patient required combined surgical and orthodontic treatment and which did not. In centers 1 (Geneva) and 2 (Lausanne), 25% and 32% of cases underwent orthognathic surgery, respectively, while in center 3 (Zurich), 88% underwent orthognathic surgery. Thus, the frequency of orthognathic surgery varied significantly between centers, and this may have been due to differences in factors such as the initial cleft severity, maxillary growth among the patients, or relative indications and recommendations for orthognathic surgery.
The more frequent undertaking of orthognathic surgery in center 3 may also be related to a different extraction protocol, reflected by more frequent final class II molar relationships on both sides compared to mostly class I relationships in centers 1 and 2. In the total sample as well as the orthognathic surgery subsample, canine and molar relationships were most often in a class I on the noncleft side and in a full class II on the cleft side (Deacon et al., 2007), the latter reflecting space closure of the frequently missing (Dewinter et al., 2003) or extracted lateral incisors. In contrast, in the subsample without orthognathic surgery, class II canine and class I molar relationships were found most often on the cleft side, probably also related to a distinct extraction pattern. Thus, these sagittal differences must be assessed in the context of the general treatment plan and objectives, as well as the possibility of tooth agenesis, as opposed to differences in treatment quality.
In the subgroup with orthognathic surgery, slightly higher labial MHB scores and overjet were observed on the noncleft side than in subjects not having undergone orthognathic surgery. Similarly, these values seemed to be higher in patients with left-sided than right-sided clefts. These results may be correlated, given the high rate of orthognathic surgery in left-sided clefts. The difference, although statistically significant, is small and perhaps clinically irrelevant (1 entity in MHB score and 0.5-1.0 mm in overjet), and it has to be highlighted that the labial MHB score and overjet were normal in the group without orthognathic surgery, while these were only slightly increased in the orthognathic surgery group. Along with this finding, the sagittal canine and molar relationships on the noncleft side tended to be slightly class II compared to the class I relationships found in the group without orthognathic surgery. Both findings may indicate a slight surgical overcorrection on the noncleft side, possibly resulting from the effort to render the cleft-sided overjet positive. This presumption is corroborated by the outcome of the total sample, where the labial MHB score and overjet on the noncleft side seemed to slightly exceed the rather normal values on the cleft side. A follow-up evaluation regarding the development of this region over time would be revealing indeed.
Besides the situation described labially, final posttreatment occlusion in our sample as expressed by MHB score did not seem to depend on the decision to perform orthognathic surgery. Additionally, midline discrepancy, which was found in almost 60% of patients (comparable to Deacon et al., 2007), did not seem to be influenced by orthognathic surgery. Thus, it can be assumed that the decision to perform orthognathic surgery or not was valid as far as occlusion is concerned and that the more severe cases underwent surgery more often than the less severe ones, who would not have benefited from it.
On the cleft side compared to the noncleft side, the more constricted buccal occlusion (Marcusson & Paulin, 2004; Noverraz et al., 2015) reflects the difficulty in correcting the more medially positioned lesser maxillary segment. Even if treatment could achieve a mesial movement of the lesser segment in terms of space closure for a missing lateral incisor, the often-required simultaneous buccal expansion remains challenging, especially in the region of the cleft. In fact, the cleft-sided canine and first premolar area tended to be constricted in our sample, despite orthodontic palatal expansion in the mixed dentition in 43% of patients (n = 24). In the absence of a midpalatal suture posterior to the incisive foramen in patients with cUCLP, expansion prior to bone grafting only enhances the distance from the lesser segment to the nasal septum. Stability becomes an issue (Marcusson & Paulin, 2004; Li & Lin, 2007; Trimetsuntorn et al., 2020), and inversion of the conventional treatment protocol with palatal expansion after bone grafting has been proposed, showing opening of the intermaxillary suture in the premaxilla in 43% of cases (Da Silva Filho et al., 2009, Garib et al., 2017).
We had over 4 times more patients with left-sided than with right-sided clefts. Over 65% of the patients with left-sided clefts underwent orthognathic surgery, compared to only 20% of the ones with right-sided clefts. This might be one reason why, in contrast to the literature (Noverraz et al., 2015), the labial and anterior buccal MHB score in our sample tended to be higher in patients with left-sided clefts. Furthermore, it cannot be excluded that the initial cleft morphology and severity may have been different between patients with left- and right-sided clefts. The influence of cleft-sidedness on the occlusal outcome may also be explained by the handedness of the orthodontist and/or the surgeon. The small number of patients with right-sided clefts in our sample however, especially those who had undergone orthognathic surgery, does not allow for more than extrapolations on the influence of cleft-sidedness on final posttreatment occlusion.
We are aware that one of the limitations of our study is the relatively small sample size and that a larger sample would have led to more reliable results. However, our sample of 56 patients with cUCLP is not to be underestimated, especially given the fact that these were patients followed from birth to adulthood and the challenges of collecting these patients, as reflected in the literature.
The ongoing Scandcleft randomized trials are exemplary in this point, with over 400 cases prospectively determined based on a power analysis (Semb et al., 2017). However, as stated by the authors themselves, including patient collection from 10 centers, 27 years will pass by to obtain records of the 18-year-old patients. The occlusion in 411 eight-year-olds was presented recently (Heliövaara et al., 2020; Karsten et al., 2020). This time interval is challenging in itself, demanding excellent collaboration of the patients until the final records are taken and a rigorous adhesion to the protocol including standardized documentation by the different centers. Furthermore, progress in treatment procedures may occur over this time span but cannot be incorporated into the predetermined protocol of the trial, so that ethical questions may arise. Similarly, when the use of a new, arising scoring system may be advantageous, it should be considered with caution if the power analysis was based on the traditional one (Heliövaara et al., 2017; Heliövaara et al., 2020 vs Karsten et al., 2017; Karsten et al., 2020).
From this point of view, the Eurocleft project has advantages, being set up as a longitudinal cohort study starting at 9 years of age only. Initially (Shaw et al., 1992), it included approximately 150 patients from 6 centers, after random exclusion of cases in order not to exceed 30 cases per center. To our knowledge, a power analysis was not performed. In the run of time, one center stopped participation (Semb et al, 2005) and at the dental arch evaluation at 17 years of age (Mølsted et al., 2005); slightly over 120 subjects were investigated, several however still needing orthognathic surgery. This is not astonishing, since patients not having completed growth have been included.
In contrast to the above-mentioned investigations, our study is retrospective with the focus on collecting adult patients who have fully completed their cleft follow-up and treatment. Our sample comprised the records of 56 adult patients. Especially with a retrospective study design, it is extremely difficult to obtain a sufficient sample of patients with cleft lip and palate having completed growth. Recent publications on the improvement of the Peer Assessment Rating index after orthodontic treatment disposed of slightly higher sample sizes (80 and 71 patients with UCLP, Tintodana et al., 2020; Stonehouse-Smith et al., 2021, respectively), without however mentioning the age of the patients at the moment when the postorthodontic records were taken, thus leaving the possibility of having included postorthodontic but still growing patients.
The struggle of collecting records of patients having completed growth is reflected in the rather small sample size in studies investigating true final posttreatment occlusion as we did and follow-up (39 patients in Marcusson & Paulin, 2004; and 18 patients in Trimetsuntorn et al., 2020). The recent study of Trimetsuntorn et al. (2020) went so far as to include patients with different cleft types in order to reach a sample size of 18 patients.
In the present study, we made the effort to enlarge our sample by collaborating with other centers treating patients from a similar geographical and ethnic background. This gave us the opportunity to grasp an actual picture of the final occlusal situation in these patients in our region. As mentioned in the Introduction, we could not find any study investigating the final occlusal outcome in adult patients with cleft reaching our sample size. However, we are well aware that our results depict only tendencies, a fact that we tried to emphasize in the article, using terms such as “tended to,” “seemed to,” “could not be found,” and so on. Even if the reliability of our results is limited by the sample size, the results are of value showing tendencies and serving as basis for “a priori” power analyses of subsequent studies.
In the future, it would be interesting to relate the initial cleft severity as well as the occlusal status at the moment of the decision-making process for or against orthognathic surgery to the present findings. Furthermore, the investigation should be expanded toward a more holistic view of final outcomes, including skeletal parameters, extraoral appearance, and patient satisfaction.
Conclusion
This Swiss intercenter study suggests that it is possible to achieve a very satisfactory final posttreatment occlusion in patients with cUCLP using a combined orthodontic and surgical approach when necessary. The more constricted buccal occlusion on the cleft side reflects the difficulty in correcting the more medially positioned lesser maxillary segment. The influence of cleft-sidedness on the occlusal outcome, provided that it can be corroborated in a larger sample, may be explained by differences in initial cleft severity or in criteria used for recommending orthognathic surgery or possibly by the handedness of the orthodontist and/or surgeon.
Supplementary Materials
Supplemental Material, sj-docx-1-cpc-10.1177_10556656211028506 for Final Posttreatment Occlusion in Patients With Unilateral Cleft Lip and Palate by Christine B. Staudt, Julia Bollhalder, Martina Eichenberger, Giorgio La Scala, Georges Herzog, Daniel B. Wiedemeier and Gregory S. Antonarakis in The Cleft Palate-Craniofacial Journal
Supplemental Material, sj-xlsx-1-cpc-10.1177_10556656211028506 for Final Posttreatment Occlusion in Patients With Unilateral Cleft Lip and Palate by Christine B. Staudt, Julia Bollhalder, Martina Eichenberger, Giorgio La Scala, Georges Herzog, Daniel B. Wiedemeier and Gregory S. Antonarakis in The Cleft Palate-Craniofacial Journal
Acknowledgments
The authors wish to thank Mr G. Pedroli, chief dental technician, for duplicating, trimming, and recoding the dental casts; all patients and their parents for having completed the proposed treatment and follow-up; all multidisciplinary health care teams, including Dr. W. Gnoinski and Prof. C. Le Coultre, for the treatment, documentation, and classification of the records; and the department chairs Prof. T. Eliades (Zurich) and Prof. S. Kiliaridis (Geneva).
Author’s Note: This study was presented orally at the annual meeting of the Swiss Society for Cleft Lip and Palate and Craniofacial Anomalies (SGLKG), Bern, Switzerland, on November 30, 2018, and at the European Cleft Palate Craniofacial Association (ECPCA) Congress, Utrecht, the Netherlands, on June 14, 2019.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iDs: Christine B. Staudt https://orcid.org/0000-0002-7141-6500
Giorgio La Scala https://orcid.org/0000-0003-1572-598X
Gregory S. Antonarakis https://orcid.org/0000-0001-6741-6922
Supplementary Materials: Supplemental material for this article is available online.
References
- Altalibi M, Saltaji H, Edwards R, Major PW, Flores-Mir C. Indices to assess malocclusions in patients with cleft lip and palate. Eur J Orthod. 2013;35(6):772–782. [DOI] [PubMed] [Google Scholar]
- Antonarakis GS, Fisher DM. Permanent tooth agenesis and maxillary hypoplasia in patients with unilateral cleft lip and palate. Plast Reconstr Surg. 2015;136(5):648e–656e. [DOI] [PubMed] [Google Scholar]
- Bongaarts CA, Kuijpers-Jagtman AM, van t Hof MA, Prahl-Andersen B. The effect of infant orthopedics on the occlusion of the deciduous dentition in children with complete unilateral cleft lip and palate (Dutchcleft). Cleft Palate Craniofac J. 2004;41(6):633–641. [DOI] [PubMed] [Google Scholar]
- Da Silva Filho OG, Boiani E, Cavassan AD, Santamaria M. Rapid maxillary expansion after secondary alveolar bone grafting in patients with alveolar cleft. Cleft Palate Craniofac J. 2009;46(3):331–338. [DOI] [PubMed] [Google Scholar]
- Deacon S, Bessant P, Russell JI, Hathorn I. What are the occlusal outcomes for unilateral cleft lip and palate patients? a national project in the UK. Brit Dent J. 2007;203(8):E18. [DOI] [PubMed] [Google Scholar]
- Dewinter G, Quirynen M, Heidbüchel K, Verdonck A, Willems G, Carels C. Dental abnormalities, bone graft quality, and periodontal conditions in patients with unilateral cleft lip and palate at different phases of orthodontic treatment. Cleft Palate Craniofac J. 2003;40(4):343–350. [DOI] [PubMed] [Google Scholar]
- Evans CA. Orthodontic treatment for patients with clefts. Clin Plast Surg. 2004;31(2):271–290. [DOI] [PubMed] [Google Scholar]
- Gamer M, Lemon J, Fellows I, Singh P. irr: various coefficients of interrater reliability and agreement. Published 2019. Accessed July 14, 2020. https://CRAN.R-project.org/package=irr
- Garib D, Miranda F, Sathler R, Kuijpers-Jagtman AM, Aiello CA. Rapid maxillary expansion after alveolar bone grafting with rhBMP-2 in UCLP evaluated by means of CBCT. Cleft Palate Craniofac J. 2017;54(4):474–480. [DOI] [PubMed] [Google Scholar]
- Gray D, Mossey P. Evaluation of a modified Huddart/Bodenham scoring system for assessment of maxillary arch constriction in unilateral cleft lip and palate subjects. Eur J Orthod. 2005;27(5):507–511. [DOI] [PubMed] [Google Scholar]
- Hathaway R, Daskalogiannakis J, Mercado A, Russell K, Long RE, Jr, Cohen M, Semb G, Shaw W. The Americleft study: an inter-center study of treatment outcomes for patients with unilateral cleft lip and palate: part 2. Dental arch relationships. Cleft Palate Craniofac J. 2011;48(3):244–251. [DOI] [PubMed] [Google Scholar]
- Heidbuchel KL, Kuijpers-Jagtman AM. Maxillary and mandibular dental-arch dimensions and occlusion in bilateral cleft lip and palate patients form 3 to 17 years of age. Cleft Palate Craniofac J. 1997;34(1):21–26. [DOI] [PubMed] [Google Scholar]
- Heliövaara A, Küseler A, Skaare P, Shaw W, Mølsted K, Karsten A, Brinck E, Rizell S, Marcusson A, Sæle P, et al. Scandcleft randomised trials of primary surgery for unilateral cleft lip and palate: 6. Dental arch relationships in 5 year-olds. J Plast Surg Hand Surg. 2017;51(1):52–57. [DOI] [PubMed] [Google Scholar]
- Heliövaara A, Skaare P, Küseler A, Shaw W, Mølsted K, Karsten A, Marcusson A, Brinck E, Rizell S, Sæle P, et al. Scandcleft randomized trials of primary surgery for unilateral cleft lip and palate. Dental arch relationships in 8 year-olds. Eur J Orthod. 2020;42(1):1–7. [DOI] [PubMed] [Google Scholar]
- Huddart AG, Bodenham RS. The evaluation of arch form and occlusion in unilateral cleft palate subjects. Cleft Palate J. 1972;9(3):194–209. [PubMed] [Google Scholar]
- IPDTOC Working Group. Prevalence at birth of cleft lip with or without cleft palate: data from the international perinatal database of typical oral clefts (IPDTOC). Cleft Palate Craniofac J. 2011;48(1):66–81. [DOI] [PubMed] [Google Scholar]
- Karsten A, Marcusson A, Hurmerinta K, Heliövaara A, Küseler A, Skaare P, Bellardie H, Rønning E, Shaw W, Mølsted K, et al. Scandcleft randomised trials of primary surgery for unilateral cleft lip and palate: 7. occlusion in 5 year-olds according to the Huddart and Bodenham index. J Plast Surg Hand Surg. 2017;51(1):58–63. [DOI] [PubMed] [Google Scholar]
- Karsten A, Marcusson A, Rizell S, Chalien MN, Heliövaara A, Küseler A, Skaare P, Brinck E, Shaw W, Bellardie H, et al. Scandcleft randomized trials of primary surgery for unilateral cleft lip and palate: occlusion in 8-year-olds according to the Modified Huddart and Bodenham index. Eur J Orthod. 2020;42(1):15–23. [DOI] [PubMed] [Google Scholar]
- Li W, Lin J. Dental arch width stability after quadhelix and edgewise treatment in complete unilateral cleft lip and palate. Angle Orthod. 2007;77(6):1067–1072. [DOI] [PubMed] [Google Scholar]
- Marcusson A, Paulin G. Changes in occlusion and maxillary dental arch dimensions in adults with treated unilateral complete cleft lip and palate: a follow-up study. Eur J Orthod. 2004;26(4):385–390. [DOI] [PubMed] [Google Scholar]
- Mølsted K, Brattstrom V, Prahl-Andersen B, Shaw WC, Semb G. The Eurocleft study: intercenter study of treatment outcome in patients with complete cleft lip and palate. Part 3: dental arch relationships. Cleft Palate Craniofac J. 2005;42(1):78–82. [DOI] [PubMed] [Google Scholar]
- Mossey PA, Clark JD, Gray D. Preliminary investigation of a modified Huddart/Bodenham scoring system for assessment of maxillary arch constriction in unilateral cleft lip and palate subjects. Eur J Orthod. 2003;25(3):251–257. [DOI] [PubMed] [Google Scholar]
- Mossey PA, Little J, Munger RG, Dixon MJ, Shaw WC. Cleft lip and palate. Lancet. 2009;374(9703):1773–1785. [DOI] [PubMed] [Google Scholar]
- Mueller AA, Zschokke I, Brand S, Hockenjos C, Zeilhofer HF, Schwenzer-Zimmerer K. One-stage cleft repair outcome at age 6- to 18-years—a comparison to the Eurocleft study data. Br J Oral Maxillofac Surg. 2012;50(8):762–768. [DOI] [PubMed] [Google Scholar]
- Noverraz RL, Disse MA, Ongkosuwito EM, Kuijpers-Jagtman AM, Prahl C. Transverse dental arch relationship at 9 and 12 years in children with unilateral cleft lip and palate treated with infant orthopedics: a randomized clinical trial (Dutchcleft). Clin Oral Investig. 2015;19(9):2255–2265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peanchitlertkajorn S, Mercado A, Daskalogiannakis J, Hathaway R, Russell K, Semb G, Shaw W, Lamichane M, Fessler J, Long RE, Jr. An intercenter comparison of dental arch relationships and craniofacial form including a center using nasoalveolar molding. Cleft Palate Craniofac J. 2018;55(6):821–829. [DOI] [PubMed] [Google Scholar]
- R Core Team. R: a language and environment for statistical computing. Accessed July 14, 2020. www.R-project.org/
- Semb G, Brattström V, Mølsted K, Prahl-Andersen B, Shaw WC. The Eurocleft study: intercenter study of treatment outcome in patients with complete cleft lip and palate. part 1: introduction and treatment experience. Cleft Palate Craniofac J. 2005;42(1):64–68. [DOI] [PubMed] [Google Scholar]
- Semb G, Enemark H, Friede H, Paulin G, Lilja J, Rautio J, Andersen M, Åbyholm F, Lohmander A, Shaw W, et al. A Scandcleft randomised trials of primary surgery for unilateral cleft lip and palate: 1. Planning and management. J Plast Surg Hand Surg. 2017;51(1):2–13. [DOI] [PubMed] [Google Scholar]
- Shaw WC, Asher-McDade C, Brattström V, Dahl E, McWilliam J, Mølsted K, Plint DA, Prahl-Andersen B, Semb G, The RP. A six-center international study of treatment outcome in patients with clefts of the lip and palate: part 1. Principles and study design. Cleft Palate Craniofac J. 1992;29(5):393–397. [DOI] [PubMed] [Google Scholar]
- Staudt CB, Kiliaridis S. Divergence in prevalence of mesiocclusion caused by different diagnostic criteria. Am J Orthod Dentofacial Orthop. 2009;135(3):323–327. [DOI] [PubMed] [Google Scholar]
- Stonehouse-Smith D, Rahman ANAA, Mooney J, Bellardie H. Occlusal outcome of orthodontic treatment for patients with complete cleft lip and palate. Cleft Palate Craniofac J. March 2021. doi:10.1177/1055665621996116 [DOI] [PubMed] [Google Scholar]
- Tintodana K, Verma S, Singh SP, Kumar V, Verma RK, Bhupali NR. Assessment of orthodontic treatment outcome using Peer Assessment Rating (PAR) index among patients with non-syndromic unilateral cleft lip and palate. J Orthod Sci. 2020;9(1):17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trimetsuntorn K, Manosudprasit A, Manosudprasit A, Phaoseree N, Pisek A, Pisek P. Evaluation of postorthodontic changes in the treatment of cleft lip and palate patients using the PAR index. Cleft Palate Craniofac J. 2020;57(1):29–34. [DOI] [PubMed] [Google Scholar]
- Vargervik K. Orthodontic management of unilateral cleft lip and palate. Cleft Palate Craniofac J. 1981;18(4):256–270. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Material, sj-docx-1-cpc-10.1177_10556656211028506 for Final Posttreatment Occlusion in Patients With Unilateral Cleft Lip and Palate by Christine B. Staudt, Julia Bollhalder, Martina Eichenberger, Giorgio La Scala, Georges Herzog, Daniel B. Wiedemeier and Gregory S. Antonarakis in The Cleft Palate-Craniofacial Journal
Supplemental Material, sj-xlsx-1-cpc-10.1177_10556656211028506 for Final Posttreatment Occlusion in Patients With Unilateral Cleft Lip and Palate by Christine B. Staudt, Julia Bollhalder, Martina Eichenberger, Giorgio La Scala, Georges Herzog, Daniel B. Wiedemeier and Gregory S. Antonarakis in The Cleft Palate-Craniofacial Journal