Abstract
Virtual Integrated Multi-Site Patient Aligned Care Team (V-IMPACT) was a Veterans Health Administration (VHA) initiative created to increase access to primary care for Veterans through Clinical Video Telehealth (CVT) appointments. Between January and August 2019, we conducted 48 semi-structured qualitative interviews with Veterans who had a V-IMPACT appointment. Many participants shared feelings of skepticism before their first appointments but for some, their opinions changed. Veterans talked about how their opinion of video care changed for the better when it made care more convenient or timelier or met their health care needs. For some Veterans, their opinion about video care stayed the same or worsened because they had a poor relationship or rapport with their provider, did not feel like they received needed care, or did not feel like video care was useful. These findings offer an opportunity for telecare providers to better understand and support patients and to deliver effective care in the context of rapidly growing telehealth modalities.
Keywords: telehealth, Veterans, rural healthcare, qualitative content analysis, patient perspectives/narratives
Introduction
In 2014, a Veterans Affairs (VA) community-based outpatient clinic (CBOC) in Mountain Home, Idaho, encountered challenges hiring mental health providers. The nearest VA Medical Center (VAMC) to Mountain Home is in Boise, Idaho, and staff at the VAMC stepped in to begin providing virtual Patient Aligned Care Team (PACT) (the VA's version of the patient-centered medical home) services to Mountain Home Veterans. This was the beginning of what would become the Virtual Integrated Multi-Site Patient Aligned Care Team (V-IMPACT) initiative.
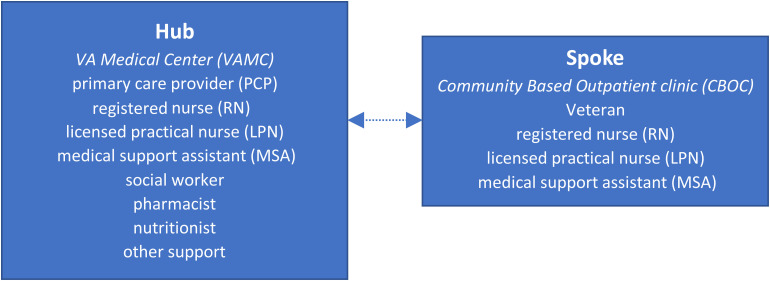
V-IMPACT increased access to primary care for Veterans, many of whom lived in rural areas that faced provider recruitment and retention challenges. Specifically, V-IMPACT used a hub-and-spoke model (1) where primary care providers (PCPs) located at “hub sites” (VAMCs) provided virtual appointments through Clinical Video Telehealth (CVT) to patients at “spoke sites” (CBOCs). Hub sites had more resources than smaller CBOCs and were in larger metropolitan areas with fewer recruitment and retention challenges; thus, the hub sites provided gap coverage for the smaller, often rural spoke sites which frequently experienced medical provider shortages. V-IMPACT used principles from PACT, a patient-centered care model that utilizes a multidisciplinary team including a PCP, registered nurse (RN), licensed practical nurse (LPN), and medical support assistant (MSA). Depending on the needs of patients, within this model additional staff (eg, social worker, pharmacist, nutritionist, etc.) may participate in a patient's care. Trained on-site nurses at spoke sites facilitate synchronous video telehealth appointments for patients, often staying in the appointment to operate a high-definition camera and to act as the “hands” of the provider, if needed, including operating digital stethoscopes (Figure 1).
Figure 1.
Hub-and-Spoke Model.
The goals of V-IMPACT were to increase access to primary care for rural Veterans, closer to where they live, and to allow for better care continuity. Following the 2014 pilot in Boise, Idaho, by 2018 V-IMPACT had expanded to 10 hubs serving 44 spoke clinics. We evaluated the V-IMPACT initiative in a multi-method study that included a quantitative component (reported in Lu et al., 2021 (2)); however, we only report the qualitative findings here. The goals of the qualitative evaluation were to understand Veteran experiences of V-IMPACT, including telehealth acceptability and any barriers or facilitators associated with V-IMPACT appointments.
Methods
Recruitment
We used a purposive sampling approach to identify Veterans with recent V-IMPACT experience. We sent letters describing the study to 342 Veterans who had a video appointment with a V-IMPACT provider within the prior 3 months and followed up by phone to schedule an interview with interested participants.
Data Collection
From January to August 2019, we conducted semi-structured telephone interviews with 48 Veterans from 8 hubs and 20 spoke sites (Table 1), 22% of whom were female and 78% of whom were male. The interview guide (Supplemental material 1) was designed to elicit descriptions of Veteran experiences with virtual appointments, their acceptance of telehealth, and any barriers or facilitators they identified with V-IMPACT. Questions were sequenced from least to most constrained, allowing for participants to share salient concepts, and included follow-up probes grounded in the Veteran's verbatim language (3). The Consolidated Framework for Implementation Research (CFIR) (4) and RE-AIM (Reach, Effectiveness, Adoption, Implementation, Maintenance) (5) guided the overall evaluation and were used to create the interview guide. Interviews lasted between 20 and 45 minutes. Interviews were audio-recorded and transcribed verbatim.
Table 1.
Interview Participants by Hub Site.
| Total | |
|---|---|
| H1 | 6 |
| H2 | 4 |
| H3 | 10 |
| H4 | 6 |
| H5 | 6 |
| H6 | 3 |
| H7 | 5 |
| H8 | 8 |
| Total | 48 |
Analysis
A team of 3 analysts used deductive and inductive content analysis (6) to analyze interview data, using a combination of a priori codes based on interview guide questions and open coding to categorize the data. We performed quality assurance on transcripts before coding and used ATLAS.ti version 8 (7), a qualitative data analysis software, to code transcripts. During the analysis period, we held weekly meetings to refine the codebook, review analytic memos, establish consensus, and refine themes (8).
Results
We found that Veteran satisfaction with their video care was complex and depended on (1) the specific needs of the patient, (2) how much they understood about what was happening, and (3) if they were given information about what video care can do. Perceived quality of care played a significant part in acceptability and whether a Veteran changed their opinion on video care.
“I can tell you that it was very odd to me at first, and I didn't like it but it's really no different. It just feels weird talking to a screen instead of a doctor at first. But like I said, the communication is very clear.”
For some Veterans, their opinion about video care stayed the same or got worse because of a challenging relationship or poor rapport with their provider, and some did not feel like they received needed care or they did not understand why they needed to have a video visit. Some reported that they did not appreciate the video because they perceived that the video visit did not feel as “personal” or “intimate” as in-person care.
Finally, there were some Veterans whose opinions were not as straightforward. While some felt their options were either video or no care, others felt their options were video care or traveling great distances to see a provider. Neither “choice” was perceived a good one by these participants. Some Veterans offered that if faced with not having a doctor or seeing one over the video, they would choose the video; this is with the caveat that those Veterans would prefer seeing a provider in person. Some Veterans had this perception of limited choice either because they lived rurally and far from any facility or their local CBOC had a hard time retaining in-person providers: “I don't know, it would be better than nothing, because there's so many Veterans that need to be seen.”
When assessing Veteran satisfaction and telehealth acceptability, Veterans who accessed V-IMPACT appointments shared mixed opinions, which were influenced by convenience of care, rapport with provider, and whether the appointment met their care needs. Many Veterans shared their experiences of being “skeptical at first,” “leery,” or “unsure at first” but for some, their opinions changed after the first appointment. Most participants who changed their opinion about telehealth from neutral or negative to positive reported the V-IMPACT encounter as their first experience of seeing a provider over video. We found mixed opinions under 3 themes: convenience, rapport, and meeting Veteran needs.
Convenience
Veterans talked about how their opinion of video care changed for the better when it made care more convenient or timely. This included getting appointments faster than they otherwise would have, receiving needed care, appointments being on time, and appointments taking less time because of reduced travel burden on Veterans to get to their local clinic versus the VAMC. For example, 1 participant detailed the lesser travel burden provided by the telehealth option at their CBOC:
“Well, if I drive from my house to the clinic, and do it over the internet deal [telehealth appointment], I’ve only got 2 miles to go to get there… I go in, I have the discussion of whatever we need to talk about and am done anywhere from 30 minutes to an hour. Then I come right straight home. Now, if I had to go to the Veterans [hospital], I’d have to drive for 3 hours to get there to have the discussion. And if I went down on the shuttle, then I’d have to wait until 2:00 in the afternoon, or 5:00, to get a ride back home. And with having problems with my back and arthritis, that is very uncomfortable, long sit in the waiting room just to get a ride home.”
Rapport
For some, their opinion changed for the better because of a good relationship or rapport with their provider and feeling that the provider addressed their concerns. We heard about appointments matching up to Veteran perceptions of what their quality of care “should be,” which for some meant increasing continuity of care and trust:
“Well, if somebody goes out there and the primary doctor is not there, and they have to see a new doctor, then, you know, you’re just starting over again, because they don't know about your history, or anything like that… And then you go to a new doctor, and you’re going to do the same thing over and over again. To be comfortable with them and trust, trust is a lot. It is to me, I don't know. In my opinion, they should have more video like that, that way they could take care of more people.”
Other Veterans perceived that missing the “human” connection element of video care made it harder to build a relationship with their provider:
“Well, to me, it doesn't have the human affect. Like seeing a doctor in person, you’ve got that relationship, you’ve got that satisfaction that he's there and he can see your emotions, he knows exactly what your feelings are at the time, and whatever pain you’re going through, versus over a video conference, which is speaking through a TV monitor… My opinion, it's not normal. I would rather see a doctor in person for my health reasons, than a doctor that's away and doesn't know me personally.”
Other patients perceived their providers as cold, acting like “they didn't even enjoy” what they were doing, not listening, or having “disappeared mentally.” Unsurprisingly, most of these Veterans had negative views of video care after this first visit. Just as feeling “listened to” enabled some Veterans to feel cared for, other Veterans felt dismissed by their video-based providers:
“I could tell [video appointments] was something that was saddled on that doctor that he had to do, I only seen him once, but he had an air of being bored silly, in my opinion. I mean, what kind of relationship can you establish with somebody over television?”
These Veterans felt their providers were disinterested in their care needs:
“I don't know how to explain it, he's just weird. He’d interrupt you and he’d put you on hold, and he wouldn't come back for 15, 20 minutes. Then he’d talk for only 5 minutes and then say, ‘I’ve got another call,’ or something. He constantly did that the whole time, you waited more than he spoke. Just like he wasn't interested.”
Among those who changed their opinion for the better after the first visit, whether they had a good interaction with their specific provider over the video was key to the experience. One Veteran described feeling their provider communicated well:
“I’m very pleased with the whole process, the appointment. He took his time, answered my questions. I was very pleased; I have no complaints about it at all. I think I went in there a little skeptical as to whether or not it would be as effective as it used to be, one on one with a doctor, but I have no complaints.”
This positive experience led to an improved perception of what telehealth can offer.
Some Veterans who had a positive experience with telehealth attributed this to having established an in-person relationship with their provider prior to starting video visits with them and others felt like they would rather meet in-person but had a fine experience with their initial visit: “Meeting [providers] in person would be nice… but other than that, I can't complain about the care I’ve been getting through video.”
Meeting Veteran Needs
Opinions also changed through perceptions that video is “good for some things.” Veterans listed a variety of those options, from “minor things” like sorting out medication to “check[ing] my health and mak[ing] sure things are going the way they should be going.”
Veterans also discussed the importance of getting their care needs met, which increased the acceptability of a telehealth option:
“Getting my needs met. Right now, I’m so comfortable and relaxed with my VA, which, I was really disappointed before. Now I have no problem with it. I’d refer anybody to the VA right now, because of the video. Since they’ve got the video in operation, and the nurses are on their toes with everything now, I feel that everything is just fine. I have no problem with it.”
Some Veterans who expressed surprise at the utility of telehealth also expressed caution about it being the only way they see a provider:
“…one has got to recognize the limitations; if I had a rash, or I was coming down with something like one of these horrible tropical diseases and the doctor actually had to see my skin, I don't know that the fidelity of the video hook up with giving the physician adequate information about the property of my skin; am I pale? Am I sweating? Does the rash have blisters? I think they’d have trouble with that.”
One other worry that was expressed by Veterans who had a negative experience with video was concern that telehealth meant that they were not cared for by VA: “It makes me feel… like they don't care enough about our care to even give us a live doctor. They put you in front of a television. And that's about the way that we all see it.”
Veterans suggested a possible solution—to be clear with patients, up front and throughout the telecare process, about what can and cannot be done over video: “I think you’re going to have to make a super effort to educate these people, and inform them that, first of all, that it's not dangerous, and not overly intrusive” and others asking for more general information, “probably just a better description in the beginning of, ‘this is going to be a video visit, this is what you can expect,’ walking into it, I think it would’ve helped me.”
Discussion
Much of the literature about patient experience with telehealth outlines what works and what does not work, but most do not explicitly address how patient opinions may change about video care after use. There are several studies focused on the utility of telehealth for improving patient outcomes (9–11). For example, Donelan et al. (12) note that through the increasing use of telehealth, there is much that patients appreciate about virtual health care: “Patients appear to value the face-to-face interactive nature… because they maintain a real-time personal connection” (p. 43). Gordon et al.'s 2020 (13) discussion of patient perspectives of telehealth found mixed perceptions for Veterans using CVT visits. Our study found some of those same Veteran perceptions of what they liked (less wait time, less travel time, perception that providers pay more attention) and did not like (cannot have an in-person exam with the PCP, perception that providers pay less attention). While our findings align with Gordon et al. in terms of mixed perceptions, our data adds to this literature a discussion of how interactions with V-IMPACT providers may have influenced Veteran perceptions about telehealth after an initial appointment.
Many of our findings highlight the importance of clear communication between the Veterans and their providers, including about the utility of video care. One theme was the perception of not getting needed care over video because video care is not the same experience as in-person: providers cannot physically palpate a patient's body (although high-tech equipment is used at the CBOC to examine a person's body over video), and interactions and building rapport may be different online. The apprehensions expressed by our Veteran participants about technology issues and the inability of video providers to palpate their patients directly should be addressed explicitly with patients to allay the concerns of those who are unfamiliar with how video care can work. Those who changed their opinions to appreciate video care noted an understanding of how they could get what they need over video.
The COVID-19 pandemic ushered in a rapid increase in telehealth modalities (14,15). Given that large numbers of patients are now forced to utilize some telemedicine for their routine care (16,17), refining how telecare is delivered is highly relevant to improving the patient experience in our “new normal” (18). This is especially important given findings that despite this new normal, patients may still prefer in-person visits (19). Our data represents experiences from a pre-pandemic context, wherein many patients were often not yet routinely using telemedicine for primary care visits, facing a less pressured environment to try virtual care. While utilizers of telehealth before COVID-19 may have had different reasons for trying virtual visits (20), what makes a virtual visit both effective and patient-centered before the pandemic remains salient to enable better patient experience (21). Gordon et al. (13) argue that video visits provide an opportunity for providers to “facilitate patient engagement and accommodate patient concerns and requests” (p1757), which some patients experienced in our study, and others did not. Providers and administrators should consider special attention to both relationship building and clear communication about virtual care to increase patient buy-in and better patient experience (22), especially to ensure the longer-term sustainability of telemedicine modalities (16).
There are a few limitations of our study. Our findings are specific to VA, representing some Veteran experiences and VA-specific processes. Some of our findings may be more clinic context-specific or geographically specific (eg, timeliness and travel convenience). While there is relevance to other populations who use telehealth modalities, some findings may not be applicable to other health care systems. We did not collect demographic information on the Veterans we interviewed beyond sex, therefore cannot provide any insights related to age or race/ethnicity characteristics. We did not find sex or gender-specific insights in this study.
Conclusion
Because of the COVID-19 pandemic, health care workers have been further pushed to deliver care in ways that work for patients who may be uninterested or unfamiliar with video care. We present concrete examples of patient perceptions and how those did or did not change. These findings offer an opportunity for VA, and for health care centers who provide telecare, to better understand and support patients and to deliver effective care in the context of more routine telehealth modalities from a time when virtual care was less of a norm. COVID-19 necessitated speedily introducing and shifting patients to telehealth (23–25). Increasing our understanding of how to make telehealth a better experience for patients is crucial to continuing care and offers an opportunity to keep reimagining how to educate and support patients who receive telehealth.
Supplemental Material
Supplemental material, sj-docx-1-jpx-10.1177_23743735221107237 for “I was Unsure at First”: A Qualitative Evaluation of Patient Perceptions of VA Clinical Video Telehealth Visits in the V-IMPACT Program by Ashley C Mog, Megan Moldestad, Rachael Kenney, Lauren Stevenson, Marcie Lee, P Michael Ho and George G Sayre in Journal of Patient Experience
Footnotes
Declaration of Conflicting Interests: The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: Declaration of Conflicts of Interest: PMH is supported by grants from NHLBI, VA HSR&D, and University of Colorado School of Medicine. He has a research agreement with Bristol-Myers Squibb through the University of Colorado. He serves as the Deputy Editor for Circulation: Cardiovascular Quality and Outcomes. Authors ACM, MM, RK, LS, ML, and GGS declare no conflicts of interest. The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of the Department of Veterans Affairs or the United States Government.
Ethical Approval: This work was conducted as a health care operations quality improvement evaluation (VHA Handbooks 1605.1 and 1605.2) and did not require Institutional Review Board review.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was funded by the Veterans Health Administration Office of Rural Health (grant number n/a) and part of a partnership sponsored by the Veterans Health Administration Office of Primary Care Operations.
ORCID iD: Rachael Kenney https://orcid.org/0000-0002-6498-3005
Statement of Human and Animal Rights: All procedures in this study were conducted in accordance with the VHA Office of Rural Health approved protocols. The activities were undertaken in support of a VHA operational project and did not constitute research, in whole or in part, in compliance with VHA Handbook 1058.05. Therefore, institutional review board approval was not required.
Statement of Informed Consent: Written informed consent was obtained from patients for their anonymized information to be published.
Supplemental Material: Supplemental material for this article is available online.
References
- 1.Elrod JK, Fortenberry JL. The hub-and-spoke organization design: an avenue for serving patients well. BMC Health Serv Res. 2017;17(1):25-33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lu AD, Gunzburger E, Glorioso TJ, Smith WB, Kenney RR, Wooley MA, et al. Impact of longitudinal virtual primary care on diabetes quality of care. J Gen Intern Med. 2021;36(9):1-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sayre G, Young J. Beyond Open-Ended Questions: Purposeful Interview Guide Development to Elicit Rich, Trustworthy Data. Veteran Health Administration Primary Care Analytics Team: VA Health Services Research & Development. https://www.hsrd.research.va.gov/for_researchers/cyber_seminars/archives/video_archive.cfm?SessionID=2439 (2018, Accessed December 12, 2021).
- 4.Damschroder L, Hall C, Gillon L, Reardon C, Kelley C, Sparks J, et al. The Consolidated Famework for Implementation Research (CFIR): progress to date, tools and resources, and plans for the future. Implement Sci. 2015;10(Suppl 1):A12. [Google Scholar]
- 5.Holtrop JS, Rabin BA, Glasgow RE. Qualitative approaches to use of the RE-AIM framework: rationale and methods. BMC Health Serv Res. 2018;18(1):1-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Elo S, Kyngäs H. The qualitative content analysis process. J Adv Nurs. 2008;62(1):107-15. [DOI] [PubMed] [Google Scholar]
- 7.ATLAS.ti Scientific Software Development GmbH. Qualitative Data Analysis. 2018; Retrieved July 2, 2018 from: http://atlasti.com/.
- 8.Mog A, Moldestad M. Behind the scenes: Qualitative analysis and dissemination tools. Veteran Health Administration Primary Care Analytics Team: VA Health Services Research & Development. https://www.hsrd.research.va.gov/for_researchers/cyber_seminars/archives/video_archive.cfm?SessionID=3803 (2020, Accessed December 12, 2021).
- 9.Chumbler NR, Haggstrom D, Saleem JJ. Implementation of health information technology in Veterans health administration to support transformational change: telehealth and personal health records. Med Care. 2011;49(12):S36-42. [DOI] [PubMed] [Google Scholar]
- 10.Kruse CS, Krowski N, Rodriguez B, Tran L, Vela J, Brooks M. Telehealth and patient satisfaction: a systematic review and narrative analysis. BMJ Open. 2017;7(8):e016242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Polinski JM, Barker T, Gagliano N, Sussman A, Brennan TA, Shrank WH. Patients’ satisfaction with and preference for telehealth visits. J Gen Intern Med. 2016;31(3):269-75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Donelan K, Barreto EA, Sossong S, Michael C, Estrada JJ, Cohen AB, et al. Patient and clinician experiences with telehealth for patient follow-up care. Am J Manag Care. 2019;25(1):40-4. [PubMed] [Google Scholar]
- 13.Gordon HS, Solanki P, Bokhour BG, Gopal RK. “I’m not feeling like I’m part of the conversation” patients’ perspectives on communicating in clinical video telehealth visits. J Gen Intern Med. 2020;35:1751-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Garfan S, Alamoodi AH, Zaidan BB, Al-Zobbi M, Hamid RA, Alwan JK, et al. Telehealth utilization during the COVID-19 pandemic: a systematic review. Comput Biol Med. 2021;138:104878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Latifi R, Doarn CR, Merrell RC. (eds) Telemedicine, telehealth and telepresence: Principles, strategies, applications, and new directions. Cham, Switzerland: Springer Nature Switzerland AG; 2021. [Google Scholar]
- 16.Thomas EE, Taylor ML, Ward EC, Hwang R, Cook R, Ross J, et al. Beyond forced telehealth adoption: a framework to sustain telehealth among allied health services. J Telemed Telecare. 2022;0(0):1-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Volcy J, Smith W, Mills K, Peterson A, Kene-Ewulu I, McNair M, et al. Assessment of patient and provider satisfaction with the change to telehealth from in-person visits at an academic safety net institution during the COVID-19 pandemic. J Am Board Fam Med. 2021;34(Supplement):S71-6. [DOI] [PubMed] [Google Scholar]
- 18.Emanuel EJ, Osterholm M, Gounder CR. A national strategy for the “new normal” of life with COVID. JAMA Netw Open. 2022;327(3):211-12. [DOI] [PubMed] [Google Scholar]
- 19.Ahmad F, Wysocki RW, Fernandez JJ, Cohen MS, Simcock XC. Patient perspectives on telemedicine during the COVID-19 pandemic. Hand (N Y). 2021;00(0):1-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Holtz BE. Patients perceptions of telemedicine visits before and after the coronavirus disease 2019 pandemic. Telemed J E Health. 2021;27(1):107-12. [DOI] [PubMed] [Google Scholar]
- 21.Nitiema P. Telehealth before and during the COVID-19 pandemic: analysis of health care workers’ opinions. J Med Internet Res. 2022;24(2):e29519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Keenan AJ, Tsourtos G, Tieman J. Promise and peril-defining ethical telehealth practice from the clinician and patient perspective: a qualitative study. Digit Health. 2022;8:1-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Pfender E. Mental health and COVID-19: implications for the future of telehealth. J Patient Exp. 2020;7(4):433-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wosik J, Fudim M, Cameron B, Gellad ZF, Cho A, Phinney D, et al. Telehealth transformation: COVID-19 and the rise of virtual care. J Am Med Inform Assoc. 2020;27(6):957-62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Zhou X, Snoswell CL, Harding LE, Bambling M, Edirippulige S, Bai X, et al. The role of telehealth in reducing the mental health burden from COVID-19. Telemed J E Health. 2020;26(4):377-9. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-docx-1-jpx-10.1177_23743735221107237 for “I was Unsure at First”: A Qualitative Evaluation of Patient Perceptions of VA Clinical Video Telehealth Visits in the V-IMPACT Program by Ashley C Mog, Megan Moldestad, Rachael Kenney, Lauren Stevenson, Marcie Lee, P Michael Ho and George G Sayre in Journal of Patient Experience