Abstract
This article aims to provide new perspectives for the treatment of low back pain (LBP). A narrative literature review highlights the treatment strategies currently anchored in the guidelines as well as the extensive attempts to identify subgroups within the non-specific low back pain (NSLBP) classification. A variety of multimodal approaches exist for both diagnostic assessments and therapy approaches. Nonetheless, there are often gaps in the classification systems as well as in published treatment concepts with regard to the implementation of musculoskeletal functional disorders. Indeed, a growing body of evidence shows that more holistic and flexible approaches are needed to individually diagnose and target the complexity of LBP. As an example, both a diagnostic and a (independently developed) therapeutic LBP concept will be presented and discussed. Ultimately, guidelines and subgroup classification systems can only reflect the complexity of LBP, if they capture its entire multidimensional and biopsychosocial character in both the diagnostic and therapeutic processes. Furthermore, the expansion of the pain definition to include the nociplastic pain mechanism, as an important driver of LBP, has the potential to provide important impulses for further necessary research. In conclusion, the implementation of a functional musculoskeletal approach along with the emerging nociceptive pain concept in individually targeted holistic approaches seems to be the successful way to deal with the complexity of LBP.
Keywords: biomedical approach, classification, complex treatment of the musculoskeletal system, functional musculoskeletal examination, LBP, multimodal treatment, nociceptive pain concept
Introduction
Low back pain (LBP) is a major challenge for the health system. It is one of the leading diagnoses in terms of costs and sick days for most countries in the Western hemisphere.1–3 In the Global Burden Disease Study 2019, LBP is one of the significant drivers of disability concerning disability-adjusted-life-years. 4 Moreover, various misguided developments have become apparent with regard to the diagnosis and treatment of LBP. These have been discussed many times in recent years. Well-known examples of this are the discussions of excessive spinal operations and radiological imaging as well as over prescription of opioids.5–9 While patients usually do not differentiate LBP, experts distinguish between acute and chronic as well as specific and non-specific LBP. This differentiation aims to facilitate the selection of targeted diagnostic and therapeutic options depending on the causes and course of the disease. First, it is essential to detect serious and dangerous pathologies at an early stage and to exclude non-spinal causes, which must be promptly referred to further special diagnostics, therapy and/or other specialist disciplines. Second, most episodes of LBP improve significantly within 6 weeks. 10 Therefore, it is important to decide when different diagnostic options (i.e. imaging and psychologists) are best utilised to be able to carry out a targeted therapy. A rough algorithm summarising the diagnostic approach and classification is shown in Figure 1.
Figure 1.
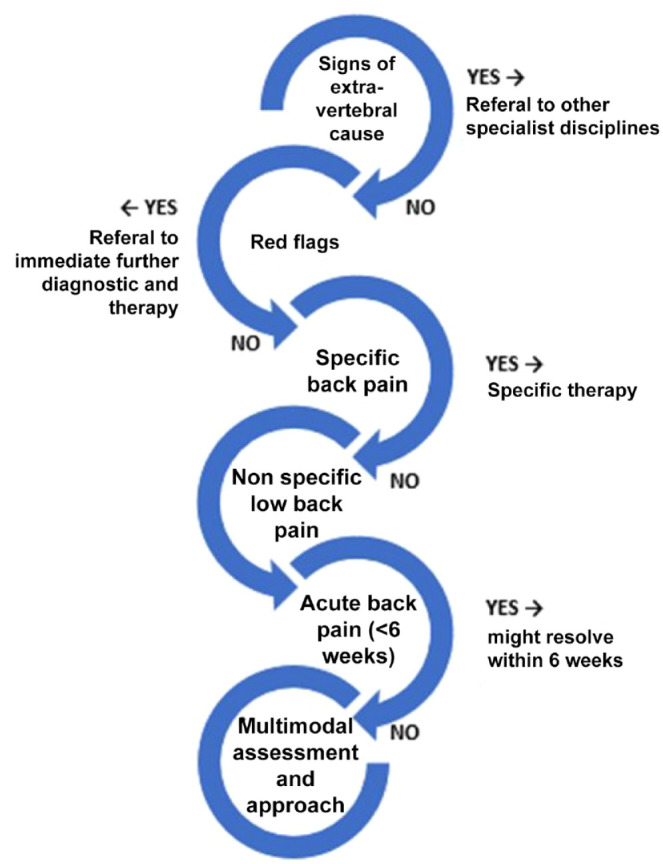
Low back pain classification and diagnostic approach.
Non-specific low back pain (NSLBP) is defined by the absence of a known pathoanatomical cause for the pain. 11 In contrast, specific LBP includes vertebral (spinal stenosis, etc.) as well as extra vertebral causes. Currently, several national guidelines have developed treatment recommendations for LBP.12–17 The current guidelines take into account the multicausal genesis of LBP, especially for NSLBP. The exact pathophysiology of NSLBP is not yet fully understood, although there is a consensus that multiple biophysical, psychosocial, pain processing, and comorbidities interact. 18
The trend in LBP therapy is moving away from spinal operations, injections, opioids, and passive therapy methods towards patient education, activating exercise therapy and behavioural psychotherapy (Table 1 outlines treatment methods). The usual diagnostics for acute and chronic LBP, as laid down in the guidelines, are based on the biopsychosocial model of disease. Diagnostic algorithms derived from this model control further diagnostic measures, such as imaging and psychological assessments on the basis of the information obtained in the medical history and clinical examination. A general consensus has established, that psychological assessments should be used within the first 6 weeks after the onset of symptoms, if the symptoms do not respond to the initial treatment regime. 12 This algorithm differentiates between extra vertebral causes and serious spinal pathologies that require immediate further diagnosis and intervention (‘red flags’, see Table 2). For the remaining LBP population, the exploration of structural, psychological, psychosocial factors as well as comorbidities and pain-processing mechanisms influencing the pain symptomatology is ensured. Hartvigsen et al. 18 have summarised in detail the risk factors and triggers that interact with each other in a spectrum of the biopsychosocial model consisting of biophysical, psychological, social, genetic factors and comorbidities. In addition to other chronic diseases (asthma, headache, diabetes), 19 lifestyle factors, such as smoking, obesity, little physical activity,20–23 or physically as well as psychologically stressful work exposure 24 were found to be relevant in increasing the risk of LBP.
Table 1.
Treatment methods low back pain.
| Classification of low back pain | Therapy principle | Methods |
|---|---|---|
| Specific low back pain |
Address the underlying pathology |
- Conservative (e.g. physiotherapy, manual therapy, physical
therapy, exercise therapy) - Interventional treatment (e.g. injections) - Surgery |
| Acute non-specific low back pain |
“Wait and see” (a majority resolves within 6 weeks) plus patient
support |
- Patient education - Pain medication (if necessary) |
| Chronic non-specific low back pain | Multimodal approach, targeting individual contributors within a holistic framework involving an interdisciplinary treatment team | - Multimodal therapy, including physical and psychological approaches individually tailored to the various contributors |
Table 2.
Red flags.
| Red flags | Signs |
|---|---|
| Trauma/fracture |
Severe trauma (e.g. accident), minor trauma (osteoporosis),
systemic steroid therapy |
| Tumour |
Age > 50 years, prior history of tumour, B symptoms: (fever,
night sweats, and weight loss), pain increasing in supine
position, intense pain at night |
| Infection |
B symptoms, intense pain at night, prior history of bacterial
infection, prior infiltration therapy, IV drug abuse, immune
suppression, underlying malignancy, exotic travel |
| Radiculopathy/cauda equina syndrome | Segmental pain, paresthesia in area of pain, loss of strength (grade 3 or less), sudden loss of bladder/bowel function, perianal/perineal hypaesthesia, death of nerve root |
Missing (or unspecific degenerative) structural findings usually lead to the diagnosis of NSLBP and the intensified diagnostic focus on psychological and psychosocial factors. A current guideline recommends collecting patient information about the benign self-limiting course of LBP, addressing possible psychosocial risk factors in combination with supportive drug therapy (non-steroidal anti-inflammatory drugs (NSAIDs)) and accompanying non-drug therapy, if necessary. 12
Although there are difficulties in implementing this recommendation in practice, 25 it is not sufficiently clear which pathological correlate is behind this (often) self-limiting LBP. The recommended administration of NSAIDs suggests that there might be a somatic correlate that is associated with an endogenous inflammatory response and thus reacts to the administration of NSAIDs. The term NSLBP additionally implies that there is no specific cause for LBP, but actually means that there is no described structural cause for the LBP. Regardless of pathoanatomical causes, back pain is usually associated with impairments of movement or other musculoskeletal dysfunction patterns. This has encouraged researchers to identify subgroups characterised by musculoskeletal functional symptoms regarding the biomedical part of a biopsychosocial assessment. Furthermore, in revising the definition of pain, the International Association for the Study of Pain (IASP) has extended its classification to include nociplastic pain, which is considered an important pain mechanism for NSLBP. 26
In the following, an overview of the development of different classification systems and their limitations as well as the new concept of nociplastic pain will be presented. This is followed by a detailed description of a conceptual classification model and a practical multimodal treatment concept, both of which comprehensively and pragmatically address the complexity of back pain.
Subgroup classification systems of NSLBP
Considering the biopsychosocial approach, including the multiple influences, triggers, and risk factors that can contribute to and perpetuate LBP, it becomes clear that the rough division into acute/chronic and specific/nonspecific is obviously insufficient to target and treat the multiple facets of back pain. The heterogeneity of NSLBP has already led to the demand for the identification of suitable subgroups and the development of classification systems for a more specific diagnosis and therapy. 27 This occurred in 1995 at the International Forum on Primary Care Research on LBP. However, there has been no discussion about the inhomogeneous nature of NSLBP patients.28–30 People with LBP vary considerably in terms of degree of chronicity, pain intensity, functional limitations, impairments of activities of daily living (ADLs) and pain impact. In addition, psychosocial factors have a significant impact on prognosis and symptom severity and are therefore important factors in the management of LBP. 31
The literature shows that various approaches can be found to define different subgroups of NSLBP patients via different biomechanical and/or psychosocial pathologies. A cross-country comparative review by Billis et al. identified 39 subgroup classifications in nine different countries (the United Kingdom, France, Switzerland, Sweden, Denmark, Canada, the United States, Australia, and New Zealand). They based on three different paradigms: pathoanatomic and/or clinical features (biomedical); psychological and social/work features (psychosocial); and mixed biomedical and psychosocial features (biopsychosocial). 32 Different ‘cultural trends’ emerged in the comparison of the different classification systems. Furthermore, it became obvious that there is no NSLBP classification system that is internationally established, effective, reliable, and valid. 32 Interestingly, cultural differences were not only reflected in varying diagnostic procedures, but even in different medical, physical, and psychosocial findings.33–35 Consequently, this results in different management of NSLBP patients from different cultural backgrounds. Overall, only four papers describing classification systems with a biopsychosocial approach could be identified,36-39 the others used a solely biomechanical or psychosocial approach. The majority of the classification systems found are based on a biomedical approach and come from a wide variety of therapeutic schools, methods, and health professionals.
Biopsychosocial classification systems
The biopsychosocial classification system INTERMED was developed in Switzerland (1999) and distinguishes between patients at different stages of disability and identifies biopsychosocial aspects of NSLBP. Information from the biological, psychosocial, social, and health care domains is considered in a time context (history, current state, and prognosis). The biological domain processed information on chronicity, diagnostic uncertainty, disease severity, diagnostic profile, and complications; the psychological domain included coping restrictions, psychiatric dysfunction and symptoms, treatment resistance, and mental health threat. In addition, social information (family disruption, social support, residential instability, social integration, and vulnerability) and health care aspects (treatment intensity and experience, organisational complexity, referral appropriateness, and care needs) are included in the classification system to further distinguish patients with chronic, disabling NSLBP and to associate patient profiles with treatment outcomes.36,37
Harper et al.’s 38 taxonomy is based on the former World Health Organization (WHO) Classification of Impairment, Disabilities, and Handicaps (since revised to International Classification of Functioning, Disability, and Health, 2001; ICF) and is based on a total of 14 categories of health problems. These include pain, mobility, work, self-care, sexual behaviour, systems and resources, home management, family dynamics, socialisation, recreation, general health perception, alertness and coping, psychological stress, and depression. From these categories, three levels emerge: an organic impairment level, a personal dysfunction level and deviations from common social behaviour patterns. 38 Among the biopsychosocial models described by Billis et al., O’Sullivan’s 39 classification system is described in the following section on physiotherapy movement-based classifications.
Physiotherapy movement-based and biomedical-based subgroup classifications
Biomedical-based subgroup systems focus on impairments of body function and/or body structures. They are often developed by physiotherapists as they involve a detailed musculoskeletal examination and they prioritise the evaluation of back function, such as altered movement or loading strategies. An interesting summary and analysis of the different classification strategies comes from Karayannis et al. 40 Nonetheless, various subgroup systems could be identified that included both psychological and psychosocial aspects. Within this systematic review, 28 physiotherapeutic-derived subgroup methods were identified and differentiated into the following paradigms or strategies: mechanical diagnosis and treatment (MDT), treatment-based classification (TBC), pathoanatomic-based classification (PBC), movement system impairment (MSI) classification and the O’Sullivan classification system (OCS). 40
MDT explore if the NSLBP can be reinforced or reduced by direction-specific, repeated lumbar spine movements or postures. A well-known method that is based on this principle would be McKenzie. 41 TBC, for example, described by Delitto et al., 42 distinguishes LBP symptoms at different levels, such as the necessary treatment setting (requires physical therapy only, multidisciplinary setting or referral to another discipline) as well as the severity (acute, subacute phase, and deconditioning). In addition, one of four treatment assignments is defined, for example, ‘manipulation’, ‘stabilisation’, ‘specific exercise’, or ‘traction’. The examination procedures involve some typical orthopaedic tests and a neurological examination. PBC is represented by Petersen et al. 43 and focus on orthopaedic tests addressing all structures which can potentially cause LBP. The diagnostic approach follows a hierarchy approach based on the frequency of known pathologies. MSI described by Sahrmann 44 postulates that prolonged postures and repeated movements cause tissue damage altering joint movement precision, which is tested with specific alignment tests. O’Sullivan 39 introduced a classification system based on the identification of maladaptive spinal postures, movement patterns and motor control patterns causing pain. Impairments of musculoskeletal function are according to O’Sullivan are to be considered in three subgroups: the first and second in the context of underlying pathological or psychological/psychosocial factors to which they are secondary or the third as the primary driver of the pain disorder. When musculoskeletal impairments are primary, associated psychological, social, or neurophysiological factors contribute to the disease but are not dominant or leading. Therefore, the exploration of cognitive and behavioural aspects is an important part of the system apart from the physical examination.
Even if the biomechanical approach dominates, all classification strategies acknowledge psychological and psychosocial influencing factors, such as cognitive or behavioural aspects in the OCS. 39 Nevertheless, they diverge essentially in their emphasis on psychosocial factors. 40 Despite this, detailed examination procedures of back and movement function have not yet found their way into the guidelines for non-specific LBP. Furthermore, these subclassification systems lack a broad biopsychosocial approach that includes a neurophysiological pain approach, psychological, and psychosocial factors.
Limitations of the subgroup classification approach
Much has been published and discussed on the topic of subgroup classification and interestingly, although they lack evidence for their effectiveness, only a few are based on a biopsychosocial approach. Nevertheless, no classification system has been established to further specify the NSLBP into subgroups, at least not with expert consensus.
However, profound data are available, which show that therapy concepts that address unidimensional subgroups (psychological, movement, and pain sensitivity) are not superior to unmatched comparative interventions.45–47 In an attempt to generate different classification patterns from a variety of multidimensional data, Rabey et al. 48 summarised typical clusters from three different subgroups (pain sensitivity, psychological scores, and pain response to movement), allowing for a total of 27 different classification patterns. The result shows that 26 of the possible 27 classification patterns occurred analysing 294 participants with LBP. This result impressively shows that NSLBP strongly varies individually in the extent of potential influencing factors present and is thus characterised by a pronounced complexity. Nonetheless, no conclusions can be drawn as to the extent to which all factors in a pattern have an equal influence on the disease or whether leading and secondary factors exist, which should influence treatment strategy and design. For the therapeutic approach, it can be concluded that the basis of an individualised therapy must be a multidimensional diagnosis, which ideally covers the entire spectrum of contributors to LBP. However, it also appears essential that the contributing factors are evaluated in terms of their relevance and significance as well as their treatability to generate a targeted and diagnosis-adapted therapy concept.
Nociplastic pain concept
The IASP has recently added the term nociplastic pain to the pain classification system. The previous classification into nociceptive pain caused by stimulation of nociceptors and neuropathic pain based on dysfunction or damage to the nervous system failed to capture the phenomenon of pain centralisation or central sensitisation. It also failed to cover patients with non-specific pain, characterised by the absence of a nociceptive or neuropathic cause, for example, NSLBP. Nociplastic pain is defined as ‘pain that arises from altered nociception despite no clear evidence of actual or threatened tissue damage causing the activation of peripheral nociceptors or evidence for disease or lesion of the somatosensory system causing the pain’ (IASP website: https://www.iasp-pain.org/resources/terminology/?ItemNumber = 1698). In a recent review on nociplastic pain affecting the musculoskeletal system, however, Kosek et al. 27 emphasise that the term should not be considered synonymous with central sensitisation, as additional contributing influences of peripheral sensitisation cannot be excluded. Rather, the concept would correspond very well with the perception that primary subgroups of pain (e.g. fibromyalgia, complex regional pain syndrome) are characterised by nociplastic conditions. 26 Nevertheless, the simultaneous presence of different pain mechanisms is possible and persistent nociceptive pain is considered a risk factor for nociplastic pain.49,50 Therefore, clinical criteria as well as a grading system for nociplastic pain in the musculoskeletal system were developed.
These criteria are based on chronic pain longer than 3 months in duration with regional distribution and no evidence that nociceptive or neuropathic pain is either present or entirely responsible for the pain and:
- clinical pain hypersensitivity phenomena (e.g. static or dynamic mechanical allodynia, heat or cold allodynia)
- a history of pain hypersensitivity in the region (sensitivity to touch, pressure, movement, or temperature)
- comorbidities (e.g. increased sensitivity to sound/light/odours, sleep disturbance, fatigue, and cognitive problems).
If clinical signs of pain hypersensitivity are present in addition to the chronic pain, a possible neruroplastic pain is present. If all the criteria listed are given, a probable neuroplastic pain is to be assumed. 26 However, it must be considered that these currently developed criteria are still based on expert experience and further studies to establish them are yet to be carried out.
Nonetheless, the introduction of the pain mechanism ‘nociplastic pain’ may help to describe and explain the underlying pathology of NSLBP.
In regard to tailored pain management and treatment, Nijs et al. 51 summarise that ‘injury and pathology-oriented approaches’ should be used for patients with nociceptive pain, while a multimodal approach is required for nociplastic pain.
The pain and disability driver management (PDDM) model
The following model is based on the ICF model (WHO’s International Classification of Functioning, Disability, and Health), which provides the biopsychosocial framework, which is essential for the exploration and classification of LBP. 52 The authors of the following model explain that they do not want to create a new classification system, but to apply and systematise the ICF system to NSLBP.
Tousignant-Laflamme et al. present a model that derives from known factors driving pain and disability. The ICF-based model considers different drivers of pain and disability from the categories of deficits in body functions and structures as well as personal and environmental factors, which are divided into a total of five domains. Although this system is intended for the rehabilitation setting, its pragmatic approach can complement and enrich reflection on the best approach to address NSLBP. The assessment within the different domains aims to find out which domains play a role in the clinical presentation of the patient and to derive and apply targeted therapy elements accordingly. Each symptom or disease aspect is assigned to one of two categories. One category consists of components that are common and easy to influence and the other category consists of components that are more complex and difficult to influence and require a more aggressive or interdisciplinary approach. Domain I describes nociceptive pain drivers, so that, a first step of exploration is to distinguish between nociceptive and neuropathic pain. The modifiable category consists of various functional musculoskeletal factors, such as movement control, mobility, or specific mechanical pain patterns. Complex situations that require intensified and multidisciplinary approaches include post-surgical conditions, structural stability deficits and highly deconditioned patients. Domain II is characterised by nervous system dysfunction (NSD) drivers. Peripheral or central origins of NSD are considered influenceable and nervous system hypersensitivity (e.g. hyperalgesia, allodynia, central sensitisation) is considered a complex manifestation. Comorbidity drivers belong to domain III, in which the physical (e.g. musculoskeletal comorbidities) are described as modifiable and the mental health comorbidities are grouped as complex. Domain IV covers cognitive–emotional drivers, which are closely associated with increased pain perception and can be a predictor of long-term disability. They are divided into the potential modifiable maladaptive cognitions and the complex maladaptive behaviours. Domain V, the last domain, is made up of contextual drivers, that is, environmental factors, which in turn can be divided into occupation-related contextual drivers and complex social environment contextual drivers.
Compared with the classification systems presented so far, the ICF-based system offers the strongest biopsychosocial orientation in combination with a pragmatic approach to the diagnosis and treatment of NSLBP. On the basis of the findings collected within the presented domains, a therapy specifically oriented towards these domains is carried out.
At present, the model has not yet been transferred into clinical practice, recently, results of a Delphi survey to validate the model were published. 53 In addition there are data from a feasibility study that shows preliminary evidence that this model might have potential to improve NSLBP management, although the application was carried out by physiotherapists alone rather than an interdisciplinary team. 54
Although a comprehensive classifications system has not yet been established, a detailed characterisation of the individually relevant contributors to LBP seems to be a precondition to further develop clinical guidelines addressing this disease. This model seems promising to provide a valid basis for a subclassification system based on a broad biopsychosocial approach to disclose the secrets of the black box NSLBP. Moreover, within the German catalogue of operation and procedure codes (OPCs), a comparable approach has been established over the last 20 years.
Multimodal non-surgical complex treatment of the musculoskeletal system OPC (8-977)
In the context of multimodal pain therapy, which in Germany largely takes place in a hospital setting rather than in rehabilitation, the inclusion of psychosocial and workplace-related risk factors in diagnosis and therapy has long been established. However, the explicit analysis and inclusion of musculoskeletal function deficits is missing from the diagnostic algorithms of multimodal pain therapy and the national (and international) guidelines. The additional assessment of musculoskeletal function pathologies as a further diagnostic level could considerably expand the diagnostic spectrum and identify different subgroups to be addressed with targeted treatment strategies. Therefore, the procedure ‘Multimodal non-surgical complex treatment of the musculoskeletal system’ (OPC 8-977) was added to the OPC catalogue in Germany. This includes a multimodal interdisciplinary treatment of multifactorial diseases of the musculoskeletal system, which is based on the biopsychosocial disease model. It also provides an interdisciplinary diagnostic procedure reflecting different categories (i.e. functional and structural, psychological, psychosocial). This diagnostic process seems comparable with the diagnostic approach that explores the different domain levels of the ICF model (i.e. the pain and disability driver management (PDDM)). Accordingly, the detection of musculoskeletal function deficits is included as well. Both physicians and physiotherapists who use this model have been trained in manual medicine. The desired target of the diagnostic process is to administer a tailored treatment concept, which is based on the obtained dysfunctions and deficits focus on individual needs of the patient. In the following, the underlying diagnostic and therapeutic principle and philosophy is briefly summarised. 55
The standardised diagnostic procedure leads to the identification of distinct subgroups (i.e. functional musculoskeletal, psychological, or pain intervention pathway), that require different treatment priorities. These are individually adapted to the personal needs of the patients. Diagnosis and therapy are conducted by an interdisciplinary team consisting of medical specialists with additional qualifications in functional musculoskeletal medicine (manual medicine) and special pain therapy, psychotherapists, various groups of therapists (physiotherapists, occupational therapists and sports therapists) and care professionals. The multimodal interdisciplinary diagnostic process includes the differentiated assessment of symptoms and signs at different biopsychosocial factors. Based on the biopsychosocial model, the diagnostic process is carried out at five different assessment levels:
- Pathomorphological structural changes.
- Neuromusculoskeletal functional disorders.
- Psychological dimensions.
- Social aspects.
- Neurophysiological pain and pain chronicity mechanisms.
After the findings of the different biopsychosocial assessment levels have been compiled, the classification and evaluation with regard to the development of the disease and the current symptoms of the disease are carried out. This assessment is made jointly in an interdisciplinary team meeting. At the end of this interdisciplinary diagnostic evaluation, a pathogenetic actuality diagnosis is made, which identifies the currently prevailing influencing factors. On this basis, the main therapeutic goal and the corresponding treatment pathway with the individual therapy priorities is determined. The therapy goals and the composition of the resulting clinical pathway are discussed with the patient in a therapy agreement conversation.
The therapy methods required in the OPC catalogue are individually adapted and coordinated targeting the individual situation and needs of the patient. Passive therapies, such as, for example, heat, massage and hydrotherapy are used as adjuvant pain therapy or for muscle relaxation and preparation for physiotherapy. Spinal injections (e.g. epidural steroid injections, facet joint injections) can often reduce the acute immobilising pain to such an extent that physiotherapeutic treatments in the corresponding spinal region with its musculature and the associated connective tissue structures become possible. Frequently, exercise therapy can only be carried out after adequate pain relief has been achieved. Important therapy elements, which are used to varying degrees in almost all patients, are both coordinative training and a stabilising exercise programme addressing segmental spinal stabilisation. Since chronic pain is usually associated with disorders of the autonomic nervous system (especially the sympathetic nervous system), appropriate forms of treatment, such as, for example, foot reflexology or hydrotherapy (affusions and wet packings) as well as cardiovascular endurance training can be used as supportive therapy. Above all, therapy techniques should be selected that the patients can also continue independently at home. Overall, therapy planning has to be structured in such a way, that the elements used change from passive to predominantly active methods in the treatment course. The psychoeducational and psychotherapeutic therapy elements are also adapted to individual needs and symptoms. In addition to comprehensive information on the development of pain disorders in the musculoskeletal system, cognitive, emotional and behavioural aspects of pain and pain management are explained. Topics, such as self-care, are also addressed and relaxation techniques are taught in group settings. Individual psychological influencing factors are also covered in individual sessions, often with the result that readiness for further outpatient psychotherapeutic treatment can be worked out. 55
The OPC code specifies the duration and intensity of treatment as well as treatment components of this inpatient programme. A total of at minimum 30 therapy sessions are required for a treatment duration of at least 12 days. Nonetheless, the therapy elements are put up individually on the basis of the multimodal assessment. The overall treatment goal of all clinical pathways is to restore outpatient treatment capability or a rehabilitation ability. The resulting length of stay is also individual and determined in team meetings depending on the course of treatment during the stay.
Scientific data on the effectiveness of the described therapy concept are available. In 2003, a study by Pioch and Seidel 56 was able to show the effectiveness of a manual medicine-based inpatient treatment concept with regard to the reduction of pain intensity and pain-related impairment. The functional musculoskeletal therapy pathway of the ‘non-surgical multimodal complex treatment of the musculoskeletal system’ presented here (OPC 8-977) was evaluated within the framework of a multicentre, single-arm study with eight orthopaedic clinics having specialised in the treatment of chronic pain disorders of the musculoskeletal system. The study focussed on the improvement of pain intensity and back-specific function. Pain intensity was reduced at all measurement points (postinterventional, 6 and 12 months after treatment) with high effect sizes. Back-specific function measured with the Oswestry Disability Index also significantly improved over the entire observation period. 57 Nevertheless, in a single-arm study, it must be considered that the study effects cannot be attributed to the intervention alone; therefore, further studies including control groups are necessary to substantiate the study outcomes.
Synthesis and critical appraisal
At present, LBP therapy still faces various questions and challenges. The literature demonstrates extensive attempts to understand LBP mechanisms and to optimise therapy strategies. The number of randomized controlled trials (RCTs) has nearly doubled since 2010. 17 Nevertheless, the situation has not substantially changed. Unfortunately, it was not possible to push back the enormous disability burden caused by LBP. Despite numerous international guidelines, the majority of LBP is considered non-specific and often takes a chronic progression. Although guidelines have realised the necessity to implement the biopsychosocial approach, this was not enough to change course. The ambiguous label NSLBP might play a leading part within this story.
Defined as LBP without a specific cause, 11 this description focusses on (the lack of) structural (anatomical) causes. Thus, guidelines lack a sufficient biomedical approach, including functional musculoskeletal signs and symptoms, rather than exclusively structural changes that are not sufficient to target the underlying biomedical courses of LBP. This is one of the several reasons that explain undesirable developments, including the increase in unnecessary imaging and rising numbers of spinal surgery. Accordingly, specific LBP due to structural changes is considered specifically treatable (e.g. with surgery). This conviction still persists even though the literature has repeatedly shown that structural findings correlate little with symptoms.58,59 Neglecting the exploration of functional musculoskeletal causes of LBP negates an efficient treatment option. Various studies have shown that complex musculoskeletal dysfunctions play a role in chronic LBP.39,60–63 Both, the ambiguous denotation and the lack of a complete biomedical approach have led to numerous attempts to identify subgroups. But in spite of this, it has not been possible to describe any uniform subgroups so far. Perhaps, an expansion of the concept of (often unidimensional) subgroups into holistic and flexible conceptual frameworks, developing screening tools to predict prognosis and outcome is the solution to overcome the term NSLBP, to optimise therapeutic options and to address the complexity of LBP. Therefore, a broad diagnostic process, which includes all elements of the biopsychosocial model must be the baseline to adequately address LBP and prevent the development of chronic progression. A promising example for this purpose might be the PDDM, even though it is still in the validation process.
Nonetheless, it seems essential to turn the focus more towards treatment. Clinical recommendations, as well, have remained substantially unchanged over the past few years. There is a fundamental agreement that psychosocial interventions must be part of the therapy regime. 17 However, the treatment of functional musculoskeletal symptoms is not part of the recommendations. This is not surprising, taking into account, that the overview of clinical practice guidelines by Oliveira et al. 17 shows, that only three guidelines included functional musculoskeletal tests such as palpation, posture assessment and spinal rage of movement testing within their physical examination routine. An explanation contributing to this development might be that manual therapy is not considered as an unequivocal positive recommendation in LBP treatment. Within the context of evidenced based medicine treatments methods are mainly investigated within unimodal trials, testing one technique against another and/or placebo, if possible. All therapeutic methods, such as heat, massage, manual therapy, exercise therapy and so on, have been typically tested in unimodal trials for their effectiveness.
This approach fails when applied in a complex and multidimensional disease as LBP, where guidelines and experts call for a multimodal strategy. Furthermore, this fundamentally contradicts the multimodal therapy approach, hindering the development of an appropriate guideline recommendation does not seem to be developable at all on this scientific basis. Therefore, it should be considered how the components of multimodal therapies can be better evaluated in their multimodal context and interactions. Nevertheless, both Rabey’s 48 and Tousignant’s 52 findings show that biomechanical aspects of back pain should not be disregarded but rather implemented with structural and psychosocial factors in diagnostic and therapeutic procedures.
Beyond this, due to the complexity of LBP, all different dimensions of the biopsychosocial model must be integrated into the therapy accordingly. This means that the corresponding therapy elements must be implemented into a comprehensive therapy plan simultaneously, with an individually adapted focus and intensity. In the literature, multimodal treatment concepts for LBP are mainly found in the rehabilitative context. 64 This also explains the predominant focus on function restoration, back school, or cognitive behavioural programmes with the aim of improving functional capacity, pain management, or ADLs. These approaches are not surprising, considering that the rehabilitative model has different objectives than the curative model in an acute care setting. Rehabilitation aims primarily at improving activities or participation limitations, rather than curing deficits in bodily functions and structures. This also means that certain pain therapy options, for example, injection techniques, are not usually realisable in the rehabilitation clinic settings. This also raises the question of which setting offers the best conditions for successful LBP therapy. Presumably, chronic LBP with a considerable chance of recovery or LBP with predictors of poor prognosis should be treated early on in an inpatient setting with access to the complete facilities of a hospital or pain clinic. In Germany, the OPC catalogue provides three multimodal pain therapy possibilities. The ‘Multimodal Pain Therapy (OPC 8-918)’ was developed first and mainly focuses on pain management as well as a cognitive and behavioural approach concentrating on active therapy elements. The second and third, the ‘Multimodal non-surgical complex Treatment of the Musculoskeletal System’ (OPC 8-977) and the ‘Multimodal rheumatological complex treatment’ (OPC 8-983) have been developed to address complex, multifactorial and multicausal diseases of the musculoskeletal system and rheumatological diseases. These three OPC procedures have been implemented within a comprehensive concept targeting complex and multicausal diseases of the musculoskeletal system, chronic pain and rheumatological diseases. The fundamental idea of this concept is based on a complete evaluation of all dimensions contributing to, for example, LBP, including an advanced physical examination targeting functional musculoskeletal symptoms. The complex individual constellation of all biopsychosocial factors is evaluated within an interdisciplinary diagnostic procedure. In the same way, all biopsychosocial dimensions and symptoms are concurrently addressed in therapy. Passive therapy tools are included and act as supportive elements for managing pain or enhance the effectiveness of other therapies, such as manual or exercise therapy. Nevertheless, there is a certain hierarchy of methods application, progressing from passive to more and more active therapy tools within the duration of treatment. Taking into account the multidimensional character of LBP, this seems to be a promising practical treatment approach addressing the complexity of LBP.
A recent paper by Hush has highlighted the need to develop interventions which appreciate the complexity of NSLBP and even proposed the reconceptualisation of LBP within a ‘complexity science framework’. 65 Therefore, multimodal and individualised interventions addressing that complexity should be developed. Hush also claimed to change methods evaluating interventions concerning LBP, as RCTs would only address a fraction of its complex characteristics. 66
However, the WHO and IASP have now differentiated chronic pain syndromes into primary and secondary forms in the latest, 11th edition of the International Classification of Diseases (ICD), which came into effect in January 2022. Back pain (low back, cervical and thoracic pain) is now listed under primary musculoskeletal pain and described as multifactorial, depending on biological, psychological and social factors (ICD-11 for Mortality and Morbidity Statistics (who.int)). This classification is linked to the concept that the entities labelled ‘primary pain’ are considered to be nociplastic pain. 26
Overall, a change in perspective seems necessary for the management of NSLBP, shifting on one hand from unimodal subgroups to a holistic and flexible conceptual framework that includes both the new pain mechanism of nociplastic pain and integrates musculoskeletal functional pathologies into individual and targeted treatment concepts.
Conclusion
In conclusion, due to the complexity of NSLBP, the current treatment management for NSLBP is not sufficient or adequate to successfully reduce the global burden of disability. However, from the author’s point of view, both the ICF-based diagnostic approach and the presented inpatient multimodal treatment concept are promising concepts that should be further evaluated and developed.
Key points
Current diagnostic and therapy approaches for LBP lack a comprehensive physical assessment of functional musculoskeletal signs and symptoms.
People with NSLBP require individualised, holistic treatment approaches that comprehensively assess all biopsychosocial dimensions (including nociplastic pain mechanisms) and symptoms.
Advanced evaluation methods are necessary to adequately investigate multimodal LBP approaches.
Acknowledgments
I wish to thank Sean Wiebersch for his help in language editing and proofreading.
Footnotes
Ethics approval and consent to participate: No investigations involving human subjects were undertaken writing this paper.
Consent for publication: Not applicable.
Author contribution(s): Anke Steinmetz: Conceptualisation; Visualisation; Writing – original draft; Writing – review & editing.
ORCID iD: Anke Steinmetz  https://orcid.org/0000-0002-7118-3372
https://orcid.org/0000-0002-7118-3372
Funding: The author received no financial support for the research, authorship and/or publication of this article.
Conflict of interest statement: The author declared no potential conflicts of interest with respect to the research, authorship and/or publication of this article
Availability of data and materials: Not applicable.
References
- 1. Maniadakis N, Gray A. The economic burden of back pain in the UK. Pain 2000; 84: 95–103. [DOI] [PubMed] [Google Scholar]
- 2. Geurts JW, Willems PC, Kallewaard JW, et al. The impact of chronic discogenic low back pain: costs and patients’ burden. Pain Res Manag 2018; 2018: 4696180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Dutmer AL, Schiphorst Preuper HR, Soer R, et al. Personal and societal impact of low back pain: the Groningen Spine Cohort. Spine 2019; 44: E1443–E1451. [DOI] [PubMed] [Google Scholar]
- 4. Vos T, Lim SS, Abbafati C, et al. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet 2020; 396: 1204–1222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Downie A, Hancock M, Jenkins H, et al. How common is imaging for low back pain in primary and emergency care? Systematic review and meta-analysis of over 4 million imaging requests across 21 years. Br J Sports Med 2020; 54: 642–651. [DOI] [PubMed] [Google Scholar]
- 6. Martin BI, Mirza SK, Spina N, et al. Trends in lumbar fusion procedure rates and associated hospital costs for degenerative spinal diseases in the United States 2004 to 2015. Spine 2019; 44: 369–376. [DOI] [PubMed] [Google Scholar]
- 7. Volkow ND, McLellan AT. Opioid abuse in chronic pain – misconceptions and mitigation strategies. N Eng J Med 2016; 374: 1253–1263. [DOI] [PubMed] [Google Scholar]
- 8. Lee SS, Choi Y, Pransky GS. Extent and impact of opioid prescribing for acute occupational low back pain in the emergency department. J Emerg Med 2016; 50: 376–384. [DOI] [PubMed] [Google Scholar]
- 9. Fritz JM, King JB, McAdams-Marx C. Associations between early care decisions and the risk for long-term opioid use for patients with low back pain with a new physician consultation and initiation of opioid therapy. Clin J Pain 2018; 34: 552–558. [DOI] [PubMed] [Google Scholar]
- 10. Da C, Menezes Costa L, Maher CG, et al. The prognosis of acute and persistent low-back pain: a meta-analysis. CMAJ 2012; 184: E613–E624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Maher C, Underwood M, Buchbinder R. Non-specific low back pain. The Lancet 2017; 389: 736–747. [DOI] [PubMed] [Google Scholar]
- 12. Chenot J-F, Greitemann B, Kladny B, et al. Non-specific low back pain. Dtsch Arztebl Int 2017; 114: 883–890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Stochkendahl MJ, Kjaer P, Hartvigsen J, et al. National Clinical Guidelines for non-surgical treatment of patients with recent onset low back pain or lumbar radiculopathy. Eur Spine J 2018; 27: 60–75. [DOI] [PubMed] [Google Scholar]
- 14. Qaseem A, Wilt TJ, McLean RM, et al. Noninvasive treatments for acute, subacute, and chronic low back pain: a clinical practice guideline from the American College of Physicians. Annals of Internal Medicine 2017; 166: 514–530. [DOI] [PubMed] [Google Scholar]
- 15. National Institute for Health Care Excellence. Low back pain and sciatica: management of non-specific low back pain and sciatica. London: National Institute for Health Care Excellence. [Google Scholar]
- 16. Koes BW, van Tulder M, Lin C-WC. An updated overview of clinical guidelines for the management of non-specific low back pain in primary care. Eur Spine J 2010; 19: 2075–2094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Oliveira CB, Maher CG, Pinto RZ, et al. Clinical practice guidelines for the management of non-specific low back pain in primary care: an updated overview. Eur Spine J 2018; 27: 2791–2803. [DOI] [PubMed] [Google Scholar]
- 18. Hartvigsen J, Hancock MJ, Kongsted A, et al. What low back pain is and why we need to pay attention. The Lancet 2018; 391: 2356–2367. [DOI] [PubMed] [Google Scholar]
- 19. Ferreira PH, Beckenkamp P, Maher CG, et al. Nature or nurture in low back pain? Results of a systematic review of studies based on twin samples. Eur J Pain 2013; 17: 957–971. [DOI] [PubMed] [Google Scholar]
- 20. Shiri R, Falah-Hassani K. Does leisure time physical activity protect against low back pain? Systematic review and meta-analysis of 36 prospective cohort studies. Br J Sports Med 2017; 51: 1410–1418. [DOI] [PubMed] [Google Scholar]
- 21. Shiri R, Karppinen J, Leino-Arjas P, et al. The association between obesity and low back pain: a meta-analysis. Am J Epidemiol 2010; 171: 135–154. [DOI] [PubMed] [Google Scholar]
- 22. Shiri R, Karppinen J, Leino-Arjas P, et al. The association between smoking and low back pain: a meta-analysis. Am J Med 2010; 123: 87.e7–87.e35. [DOI] [PubMed] [Google Scholar]
- 23. Zhang TT, Liu Z, Liu YL, et al. Obesity as a risk factor for low back pain: a meta-analysis. Clin Spine Surg 2018; 31: 22–27. [DOI] [PubMed] [Google Scholar]
- 24. Steffens D, Ferreira ML, Latimer J, et al. What triggers an episode of acute low back pain? A case-crossover study. Arthritis Care Res (Hoboken) 2015; 67: 403–410. [DOI] [PubMed] [Google Scholar]
- 25. Chenot J-F, Scherer M, Becker A, et al. Acceptance and perceived barriers of implementing a guideline for managing low back in general practice. Implement Sci 2008; 3: 7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Kosek E, Clauw D, Nijs J, et al. Chronic nociplastic pain affecting the musculoskeletal system: clinical criteria and grading system. Pain 2021; 162: 2629–2634. [DOI] [PubMed] [Google Scholar]
- 27. Borkan JM, Koes B, Reis S, et al. A report from the second international forum for primary care research on low back pain. Reexamining priorities. Spine 1998; 23: 1992–1996. [DOI] [PubMed] [Google Scholar]
- 28. Bouter LM, van Tulder MW, Koes BW. Methodologic issues in low back pain research in primary care. Spine 1998; 23: 2014–2020. [DOI] [PubMed] [Google Scholar]
- 29. Kent P, Keating J. Do primary-care clinicians think that nonspecific low back pain is one condition? Spine 2004; 29: 1022–1031. [DOI] [PubMed] [Google Scholar]
- 30. Leboeuf-Yde C, Lauritsen JM, Lauritzen T. Why has the search for causes of low back pain largely been nonconclusive? Spine 1997; 22: 877–881. [DOI] [PubMed] [Google Scholar]
- 31. Melloh M, Elfering A, Egli Presland C, et al. Identification of prognostic factors for chronicity in patients with low back pain: a review of screening instruments. Int Orthop 2009; 33: 301–313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Billis EV, McCarthy CJ, Oldham JA. Subclassification of low back pain: a cross-country comparison. Eur Spine J 2007; 16: 865–879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Brena SF, Sanders SH, Motoyama H. American and Japanese chronic low back pain patients: cross-cultural similarities and differences. Clin J Pain 1990; 6: 118–124. [DOI] [PubMed] [Google Scholar]
- 34. Sanders SH, Brena SF, Spier CJ, et al. Chronic low back pain patients around the world: cross-cultural similarities and differences. Clin J Pain 1992; 8: 317–323. [DOI] [PubMed] [Google Scholar]
- 35. Skovron ML, Szpalski M, Nordin M, et al. Sociocultural factors and back pain. A population-based study in Belgian adults. Spine 1994; 19: 129–137. [DOI] [PubMed] [Google Scholar]
- 36. Stiefel FC, Jonge P, de Huyse FJ, et al. INTERMED – an assessment and classification system for case complexity. Results in patients with low back pain. Spine 1999; 24: 378–384; discussion 385. [DOI] [PubMed] [Google Scholar]
- 37. Huyse FJ, Lyons JS, Stiefel FC, et al. ‘INTERMED’: a method to assess health service needs. Gen Hosp Psych 1999; 21: 39–48. [DOI] [PubMed] [Google Scholar]
- 38. Harper AC, Harper DA, Lambert LJ, et al. Symptoms of impairment, disability and handicap in low back pain: a taxonomy. Pain 1992; 50: 189–195. [DOI] [PubMed] [Google Scholar]
- 39. O’Sullivan P. Diagnosis and classification of chronic low back pain disorders: maladaptive movement and motor control impairments as underlying mechanism. Man Ther 2005; 10: 242–255. [DOI] [PubMed] [Google Scholar]
- 40. Karayannis NV, Jull GA, Hodges PW. Physiotherapy movement based classification approaches to low back pain: comparison of subgroups through review and developer/expert survey. BMC Musculoskelet Disord 2012; 13: 24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Hefford C. McKenzie classification of mechanical spinal pain: profile of syndromes and directions of preference. Man Ther 2008; 13: 75–81. [DOI] [PubMed] [Google Scholar]
- 42. Delitto A, Erhard RE, Bowling RW. A treatment-based classification approach to low back syndrome: identifying and staging patients for conservative treatment. Phys Ther 1995; 75: 470–485. [DOI] [PubMed] [Google Scholar]
- 43. Petersen T, Laslett M, Thorsen H, et al. Diagnostic classification of non-specific low back pain. A new system integrating patho-anatomic and clinical categories. Physiotherapy Theory Prac 2003; 19: 213–237. [Google Scholar]
- 44. Sahrmann S, Azevedo DC, Dillen LV. Diagnosis and treatment of movement system impairment syndromes. Braz J Phys Ther 2017; 21: 391–399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Henry SM, van Dillen LR, Ouellette-Morton RH, et al. Outcomes are not different for patient-matched versus nonmatched treatment in subjects with chronic recurrent low back pain: a randomized clinical trial. Spine J 2014; 14: 2799–2810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Bergbom S, Flink IK, Boersma K, et al. Early psychologically informed interventions for workers at risk for pain-related disability: does matching treatment to profile improve outcome. J Occup Rehabil 2014; 24: 446–457. [DOI] [PubMed] [Google Scholar]
- 47. Apeldoorn AT, Ostelo RW, van Helvoirt H, et al. A randomized controlled trial on the effectiveness of a classification-based system for subacute and chronic low back pain. Spine 2012; 37: 1347–1356. [DOI] [PubMed] [Google Scholar]
- 48. Rabey M, Smith A, Kent P, et al. Chronic low back pain is highly individualised: patterns of classification across three unidimensional subgrouping analyses. Scand J Pain 2019; 19: 743–753. [DOI] [PubMed] [Google Scholar]
- 49. Leffler AS, Kosek E, Lerndal T, et al. Somatosensory perception and function of diffuse noxious inhibitory controls (DNIC) in patients suffering from rheumatoid arthritis. Eur J Pain 2002; 6: 161–176. [DOI] [PubMed] [Google Scholar]
- 50. Pollard LC, Ibrahim F, Choy EH, et al. Pain thresholds in rheumatoid arthritis: the effect of tender point counts and disease duration. J Rheumatol 2012; 39: 28–31. [DOI] [PubMed] [Google Scholar]
- 51. Nijs J, Lahousse A, Kapreli E, et al. Nociplastic pain criteria or recognition of central sensitization? Pain phenotyping in the past, present and future. J Clin Med 2021; 10: 3203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Tousignant-Laflamme Y, Martel MO, Joshi AB, et al. Rehabilitation management of low back pain – it’s time to pull it all together! J Pain Res 2017; 10: 2373–2385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Tousignant-Laflamme Y, Cook CE, Mathieu A, et al. Operationalization of the new pain and disability drivers management model: a modified Delphi survey of multidisciplinary pain management experts. J Eval Clin Pract 2020; 26: 316–325. [DOI] [PubMed] [Google Scholar]
- 54. Longtin C, Décary S, Cook CE, et al. Optimizing management of low back pain through the pain and disability drivers management model: a feasibility trial. Plos One 2021; 16: e0245689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Niemier K, Seidel W, Psczolla M, et al. (eds) Schmerzerkrankungen des Bewegungssystems: multimodale Interdisziplinäre Komplexbehandlung. Berlin; Boston, MA: De Gruyter, 2018. [Google Scholar]
- 56. Pioch E, Seidel W. Manuelle Medizin bei chronischen Schmerzen. Evaluation Eines Stationären Behandlungskonzeptes. Schmerz 2003; 17: 34–43. [DOI] [PubMed] [Google Scholar]
- 57. Steinmetz A, Psczolla M, Seidel W, et al. Effect of subgroup-specific multimodal therapy on chronic spinal back pain and function-a prospective inpatient multicentre clinical trial in Germany. Medicine (Baltimore) 2019; 98: e13825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Boden SD, Davis DO, Dina TS, et al. Abnormal magnetic-resonance scans of the lumbar spine in asymptomatic subjects. J Bone Joint Surg Am 1990; 72: 403–408. [PubMed] [Google Scholar]
- 59. Jarvik JJ, Hollingworth W, Heagerty P, et al. The longitudinal assessment of imaging and disability of the back (LAIDBack) study: baseline data. Spine 2001; 26: 1158–1166. [DOI] [PubMed] [Google Scholar]
- 60. Brennan GP, Fritz JM, Hunter SJ, et al. Identifying subgroups of patients with acute/subacute ‘nonspecific’ low back pain: results of a randomized clinical trial. Spine 2006; 31: 623–631. [DOI] [PubMed] [Google Scholar]
- 61. Fritz JM, Cleland JA, Childs JD. Subgrouping patients with low back pain: evolution of a classification approach to physical therapy. J Orthop Sports Phys Ther 2007; 37: 290–302. [DOI] [PubMed] [Google Scholar]
- 62. Niemier K, Ritz W, Seidel W. Der Einfluss muskuloskelettaler Funktionsstörung auf chronische Schmerzsyndrome des Bewegungssystems. Schmerz 2007; 21: 139–145. [DOI] [PubMed] [Google Scholar]
- 63. Radebold A, Cholewicki J, Polzhofer GK, et al. Impaired postural control of the lumbar spine is associated with delayed muscle response times in patients with chronic idiopathic low back pain. Spine 2001; 26: 724–730. [DOI] [PubMed] [Google Scholar]
- 64. Kamper SJ, Apeldoorn AT, Chiarotto A, et al. Multidisciplinary biopsychosocial rehabilitation for chronic low back pain: cochrane systematic review and meta-analysis. BMJ 2015; 350: h444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Hush JM. Low back pain: it is time to embrace complexity. Pain 2020; 161: 2248–2251. [DOI] [PubMed] [Google Scholar]
- 66. Greenhalgh T, Papoutsi C. Studying complexity in health services research: desperately seeking an overdue paradigm shift. BMC Med 2018; 16: 95. [DOI] [PMC free article] [PubMed] [Google Scholar]


