Abstract
Objective
To examine associations between neighborhood built environment (BE) variables, residential property values, and longitudinal 1- and 2-year changes in body mass index (BMI).
Methods
The Seattle Obesity Study III was a prospective cohort study of adults with geocoded residential addresses, conducted in King, Pierce, and Yakima Counties in Washington State. Measured heights and weights were obtained at baseline (n = 879), year 1 (n = 727), and year 2 (n = 679). Tax parcel residential property values served as proxies for individual socioeconomic status. Residential unit and road intersection density were captured using Euclidean-based SmartMaps at 800 m buffers. Counts of supermarket (0 versus. 1+) and fast-food restaurant availability (0, 1–3, 4+) were measured using network based SmartMaps at 1600 m buffers. Density measures and residential property values were categorized into tertiles. Linear mixed-effects models tested whether baseline BE variables and property values were associated with differential changes in BMI at year 1 or year 2, adjusting for age, gender, race/ethnicity, education, home ownership, and county of residence. These associations were then tested for potential disparities by age group, gender, race/ethnicity, and education.
Results
Road intersection density, access to food sources, and residential property values were inversely associated with BMI at baseline. At year 1, participants in the 3rd tertile of density metrics and with 4+ fast-food restaurants nearby showed less BMI gain compared to those in the 1st tertile or with 0 restaurants. At year 2, higher residential property values were predictive of lower BMI gain. There was evidence of differential associations by age group, gender, and education but not race/ethnicity.
Conclusion
Inverse associations between BE metrics and residential property values at baseline demonstrated mixed associations with 1- and 2-year BMI change. More work is needed to understand how individual-level sociodemographic factors moderate associations between the BE, property values, and BMI change.
Highlights
-
•
Strong, inverse cross-sectional relationships between the built environment, residential property values (a proxy for individual socioeconomic status), and measured BMI were observed.
-
•
Measures of the built environment and residential property values showed modest and inconsistent associations with 1- and 2-year BMI change.
-
•
There was suggestive evidence that age may moderate the association between urban density and 1- and 2-year BMI change while education may moderate the association between residential property values and 2-year BMI change.
1. Introduction
Obesity prevalence in small-area studies has long been linked to selected aspects of the neighborhood built environment (BE) (Drewnowski et al., 2020; Garfinkel-Castro, Kim, Hamidi, & Ewing, 2017; Parise, 2020; Wilkins et al., 2019). Those BE features that were associated with walking, green space, active transport, and recreational activities were associated with lower prevalent obesity (Buszkiewicz et al., 2021a, 2021b; Congdon, 2019; Drewnowski et al., 2020; Mooney et al., 2020a; Parise, 2020). By contrast, associations between measures of the local food environment and prevalent obesity were decidedly mixed (Drewnowski et al., 2020; Hobbs et al., 2019a; Wilkins et al., 2019). In general, higher socioeconomic status was more strongly associated with lower prevalent obesity than was physical proximity to food sources, whether supermarkets or fast-food restaurants (Buszkiewicz et al., 2020; Hobbs et al., 2019b).
Observed cross-sectional associations between BE metrics and prevalent obesity may have been influenced by historic patterns of systemic inequity across neighborhoods (Assari, 2018; Lam, Vaartjes, Grobbee, Karssenberg, & Lakerveld, 2021; Wong et al., 2018). Both housing segregation as well as structural (e.g. wealth gap) and individual economic determinants (e.g., education) can determine where people live and work (Drewnowski et al., 2020; Wong et al., 2018). Residential mobility patterns can also vary by age, race/ethnicity, and education; the same options to relocate to healthier neighborhoods are not equally available to everyone (Buszkiewicz et al., 2021a; Drewnowski et al., 2020; Wong et al., 2018). Recognizing these limitations and the potential selection bias in study design (Lam et al., 2021), researchers have increasingly turned to exploring the potential impact of BE variables on the longitudinal trajectories of weight change, and more specifically weight gain (Buszkiewicz et al., 2021a, 2021b; Drewnowski et al., 2019, 2020; Letarte et al., 2020).
Recent longitudinal studies of geo-localized electronic health records for large patient cohorts were able to explore which, if any, aspects of the BE were responsible for weight change (Buszkiewicz et al., 2021a, 2021b). A recent study of 115,260 insured adults in King County, Washington (WA) found that residential and road intersection densities, used as proxies for walkability, were associated with a lower but not clinically meaningful weight gain (<0.5 kg) over five years (Buszkiewicz et al., 2021b). Proximity to fast-food restaurants or supermarkets had little influence on weight change, with any apparent association accounted for by the correlation with urban density (Buszkiewicz et al., 2021b). Similarly, a study of >1.5 million men and women in Sweden found a strong and consistent associations between neighborhood deprivation metrics and higher obesity risk but little influence of fast-food outlets or the availability of facilities for physical activity (Okuyama et al., 2020).
The goal of this study was to determine whether BE measures at baseline had any influence on changes in body mass index (BMI) at year 1 and/or at year 2. We further compared these associations with that of residential property values, a proxy measure of socioeconomic status (SES) associated with individual accumulated wealth, and BMI change (Berrigan et al., 2015; Coffee, Lockwood, Rossini, Niyonsenga, & McGreal, 2020; Drewnowski et al., 2016, 2020; Leonard et al., 2016, 2017; Ware, 2019). We evaluated these associations in a prospective cohort of adult respondents from three urban and rural counties in WA State, which differed in both racial/ethnic composition and in urban form (Buszkiewicz et al., 2020; Gupta et al., 2021; Rose et al., 2020). A secondary question was whether any associations between BE measures, residential property values, and BMI change might be modified by age group, gender, race/ethnicity, or education. The type, duration, and level of BE exposure as well as individual susceptibility to the BE may differ by age (Hobbs et al., 2019a, 2019b; Sarkar, Webster, & Gallacher, 2017; Zhang & Yin, 2019), gender (Bell, Hamer, & Shankar, 2014; Buszkiewicz et al., 2021a; Sarkar et al., 2017), race/ethnicity (Buszkiewicz et al., 2021a; Wong et al., 2018), or education (Parise, 2020; Wong et al., 2018) in important ways. A better understanding of potential modification by demographic variables may have implications for community design and for BE-centered obesity prevention efforts (Buszkiewicz et al., 2021a; Letarte et al., 2020).
2. Methods
2.1. Study population
Details on the Seattle Obesity Study (SOS) III cohort have been published elsewhere (Buszkiewicz et al., 2020; Gupta et al., 2021; Rose et al., 2020). In brief, the SOS III recruited participants from sites in King County (University of Washington), Pierce County (MultiCare Institute for Research and Innovation), and Yakima County (Fred Hutch). All participants were screened prior to entry into the study and were excluded if they: 1) were not the primary food shopper in the household, 2) were less than 21 years of age or older than 59 at baseline, 3) were pregnant or breastfeeding at baseline, 4) had any physical mobility issues, or 5) were not English or Spanish speaking. Each participant's baseline address upon entry into the cohort was geocoded using ArcGIS (ESRI, 2011) with county-level point reference data; geocoded home locations served as the primary means to determine BE exposures.
2.2. BE variables and residential property values
Tax parcel-level residential property value was the primary individual-level SES measure of interest. Residential property values take into account both land and structures and offer an objective, geocoded proxy measure of SES that is linked to prevalent obesity (Berrigan et al., 2015; Coffee et al., 2020; Drewnowski et al., 2016, 2020; Leonard et al., 2016, 2017; Ware, 2019). The tax parcel is the smallest structural unit of geographic disaggregation available (Berrigan et al., 2015). For multiple dwellings at a single address, the value of each tax parcel per residential unit was calculated by dividing the assessed value, obtained from 2016 county tax assessor records, by the number of units at that parcel. In addition, property values can be aggregated to any geographic boundary (Berrigan et al., 2015). Some SOS III participants (n = 52) home addresses were located outside King, Pierce, and Yakima but near the border; therefore, parcel-level residential property value data was not available. For these participants, residential property values were assigned the average values using an 800 m buffer of around nearby border parcels. Residential property values were split into tertiles for analysis.
Residential and road intersection density at 800 m, calculated as units per hectare, served as urban form measures of the neighborhood BE. Residential density was selected as this metric has been shown to be highly predictive of walkability (Buszkiewicz et al., 2021b; Huang, Moudon, Cook, & Drewnowski, 2015; Mooney et al., 2020b; Pouliou & Elliott, 2010; Sarkar et al., 2017) while road intersection density has been correlated walking route connectivity (Durand et al., 2016). Both measures have been correlated with prevalent obesity (Buszkiewicz et al., 2021a, 2021b; Durand et al., 2016; Huang et al., 2015; Mooney et al., 2020b). Prior work has found little difference in the strength of the association between walking and the buffer size of neighborhood walkability metrics (Villanueva et al., 2014). The 800 m buffer distance was chosen as is it equivalent to the distance the average adult can walk in about 10 min and has been used in prior work evaluating the relationship between these measures of the BE and body weight (Buszkiewicz et al., 2021a, 2021b). For these measures, the geocoded home locations were estimated using Euclidean-based SmartMaps and focal processing methods in PostgreSQL/PostGIS and R (ESRI, 2011; R Core Team, 2019; The PostGIS Development Group, 2021; The PostgreSQL Global Development Group, 2021). Developed by the University of Washington Urban Form Lab, SmartMaps are continuous rasterized surfaces that provide a grid of neighborhood-level BE values within a given study area (Buszkiewicz et al., 2021a, 2021b; Hurvitz, Moudon, Kang, Saelens, & Duncan, 2014; Moudon, Cook, Ulmer, & Hurvitz, 2011). More details on how Euclidean-based SmartMaps are generated and how they confer greater efficiency over other geoprocessing methods can be found in prior publications (Buszkiewicz et al., 2021a, 2021b; Drewnowski et al., 2019; Hurvitz et al., 2014; Mooney et al., 2020b; Moudon et al., 2011). As with residential property values, residential and road intersection density were stratified using tertiles for ease of interpretation.
Counts of fast-food restaurants and supermarkets at 1600 m served as food environment measures of the neighborhood BE. Counts of proximal supermarkets and food-fast restaurants are commonly used to measure the food environment (Drewnowski et al., 2020; Hobbs et al., 2019a; Wilkins et al., 2019). Fast-food restaurants were defined as restaurants where one pays for meals before eating and consisted of chains that tended to serve less healthy processed food options (not including coffee shops) (Vernez Moudon et al., 2013). Prior work has shown little difference in the strength of association between neighborhood food environment buffer size and BMI particularly when using broad definitions for fast-food restaurants, such as the aforementioned definition (Wilkins et al., 2019). The 1600 m buffer distance was chosen as is it equivalent to the distance the average adult can walk in about 20 min and, as with our chosen urban form metrics, have been used in prior work evaluating the relationship between these measures of the BE and BMI (Buszkiewicz et al., 2021a, 2021b). Geo-localized data on supermarkets and fast-food restaurants were obtained from food permit addresses from county public health agencies (Vernez Moudon et al., 2013). These count measures were operationalized using network-based SmartMaps (Hurvitz et al., 2014). Fast-food restaurant counts were categorized as “0”, “1–3”, or “4+” within the 1600 m buffer. Supermarket counts were categorized into a binary variable: “0” versus “1+.”
2.3. Weight and height measurement
Each study participant had their height, in feet, and weight, in pounds, measured by trained study staff using calibrated scales and stadiometers at baseline. These in-person measurements were then repeated at each follow-up visit 1 and 2 years later. Each height was then converted to meters and each weight was converted to kilograms. Weights (<31.75 kg or >317.52 kg) and baseline heights (<1.22 m or >2.44 m) flagged as biologically implausible were excluded based on prior work (Buszkiewicz et al., 2021a, 2021b). Each participant's BMI at each time point was calculated using the formula . BMI values < 15.0 kg/m2 or >100 kg/m2 were excluded as biologically implausible (Buszkiewicz et al., 2021a, 2021b). Our primary outcome of interest, BMI change, was defined as .
2.4. Covariates
We included several sociodemographic factors known to be associated with the BE exposures and BMI (Buszkiewicz et al., 2021b; Drewnowski et al., 2015a). All sociodemographic data were self-reported at baseline via the computer-assisted SOS health behavior survey and entered in the study database by trained staff. These variables included age (21–39, 40–49, and 50–59 years), gender (male, female), race/ethnicity (non-Hispanic White, Hispanic, Other), educational attainment (high school education or less, some college, and college or more), and home ownership (own, rent or other). Note that, in this study, “Hispanic” was also included as a race category, in addition to being included as an ethnicity category, to be culturally sensitive to the largely Hispanic population of Yakima who self-identified as Hispanic as both a race and ethnicity. Self-reported racial/ethnic identities served as our best available indicator of participants’ exposure to systemic, structural racism and its association with the BE and BMI change. The “Other” racial/ethnic category included non-Hispanic Black, Asian, Native Hawaiian/other Pacific Islander, American Indian/Alaskan Native, and other self-described racial categories, such as multiracial categories. These populations were aggregated due to sample size limitations. Finally, we also included county-level fixed effects to control for differential data collection at each study site and to serve as a proxy measure to account for unobserved county-level factors that may be potential confounders.
2.5. Statistical analysis
Included in the analytic sample were SOS III participants with complete data on measures of the BE, and sociodemographic information. Participants missing weight data for both 1- and 2-year follow-up were excluded. The analytic sample was 819 participants at baseline, and 727 participants at year 1, and 679 participants at year 2. We first conducted descriptive analyses of our analytic population examining sociodemographic and BE characteristics at baseline. We also examined the distribution of BE characteristics by sociodemographic covariates. We then examine bivariate associations between residential property values and our selected measures of the BE as well as correlations among BE variables. We also examined bivariate associations between residential property values, mean BMI at baseline, and mean BMI change.
2.5.1. Baseline residential property values, BE characteristics, and BMI
We regressed each BE measure with baseline BMI to estimate the mean BMI cross-sectionally associated with each residential property values tertile, residential and road intersection density tertile, and category of fast-food restaurant and supermarket availability, adjusting for covariates. The adjusted means reported are those with an average observed adjusted set of sociodemographic characteristics in the study population. Omnibus Wald tests at each time point were conducted to determine whether there were any statistically significant differences in adjusted mean BMIs across tertiles of residential property values or density measures (2nd versus 1st tertile, 3rd versus 1st tertile) and category of fast-food restaurant (1–3 versus 0, 4+ versus 0) and supermarket availability (1+ versus 0). To examine effect measure modification across sociodemographic factors, we conducted the same analyses but interacted each BE measure with age group, gender, race/ethnicity, and education. Note that for analyses examining effect measure modification by race/ethnicity, the category ‘Other’ was excluded due to small sample size limitations; however, this racial/ethnic category was included in all other models where race/ethnicity was used as a covariate.
2.5.2. Baseline residential property values and BE characteristics and change in mean BMI
We then implemented a set of linear mixed-effects models (LMMs) (Laird & Ware, 1982) to estimate the mean change in BMI from baseline to 1- and 2-year follow-up modeled separately with each BE metric adjusting for covariates. LMMs allowed us to account for within respondent repeated measures of BMI and missing BMI data. We report adjusted mean changes using an average observed set of sociodemographic characteristics in the analytic sample. As with the cross-sectional analyses, Wald tests were used to test differences across BE metric categories; however, in longitudinal analyses the estimate being compared is the difference in mean BMI from baseline to 1- or 2-year follow-up. As a secondary analysis we also examined effect measure modification by age, gender group, race/ethnicity, and education using a three-way interaction between residential property values or each BE metric, time, and the sociodemographic factor. All LMM models were fit using a random intercept. All tests were two-sided using an level of .05. Analyses were conducted using Stata version 17 (StataCorp, 2021).
3. Results
The SOS III population sample was mostly women (81.4%) and homeowners (64.1%), with a high representation of non-Hispanic Whites (47.7%), 50-59-year-olds (37.9%), and participants with college and/or graduate degrees (44.3%) (Table 1). Obesity prevalence (BMI>30) was 43.5%. Most participants had at least 1 supermarket within 1600 m of home (65.1%), whereas half (49.1%) lived within 1600 m of 4+ fast-food restaurants.
Table 1.
Baseline sociodemographic factors, built environment characteristics, and weight status of the Seattle Obesity Study III analytic sample (n = 819).
| Characteristic | n | % |
|---|---|---|
| Age (years) | ||
| 21-39 | 269 | 32.8 |
| 40-49 | 240 | 29.3 |
| 50-61 | 310 | 37.9 |
| Gender | ||
| Men | 152 | 18.6 |
| Women | 667 | 81.4 |
| Race/ethnicity | ||
| Non-Hispanic White | 391 | 47.7 |
| Hispanic | 332 | 40.5 |
| Other | 96 | 11.7 |
| Education | ||
| High school or less | 279 | 34.1 |
| Some College | 177 | 21.6 |
| College or more | 363 | 44.3 |
| Home ownership | ||
| Rent or other | 294 | 35.9 |
| Own | 525 | 64.1 |
| Residential property value, parcel level | ||
| Tertile 1: $10,889 to $130,644 | 274 | 33.5 |
| Tertile 2: $133,974 to $295,000 | 272 | 33.2 |
| Tertile 3: $300,300 to $1,492,000 | 273 | 33.3 |
| Residential density, 800 m buffer | ||
| Tertile 1: 0.01 to 3.74 | 273 | 33.3 |
| Tertile 2: 3.74 to 9.01 | 273 | 33.3 |
| Tertile 3: 9.05 to 104.86 | 273 | 33.3 |
| Road intersection density, 800 m buffer | ||
| Tertile 1: 0.00 to 0.35 | 274 | 33.5 |
| Tertile 2: 0.35 to 0.57 | 275 | 33.6 |
| Tertile 3: 0.57 to 1.12 | 270 | 33.0 |
| Fast-food restaurant availability, 1600 m buffer | ||
| 0 | 187 | 22.8 |
| 1-3 | 230 | 28.1 |
| 4+ | 402 | 49.1 |
| Supermarket access, 1600 m buffer | ||
| 0 | 286 | 34.9 |
| 1+ | 533 | 65.1 |
| Body mass index (BMI) category | ||
| Normal weight (BMI <25.0 kg/m2)a | 216 | 26.4 |
| Overweight (BMI ≥25.0 kg/m2 and <30.0 kg/m2) | 247 | 30.2 |
| Obese (BMI ≥30 kg/m2) | 356 | 43.5 |
Included in this group are fewer than 10 participants are underweight.
In this sample, higher residential property values were associated with 50–59-year-olds, those with a college degree or more, and with non-Hispanic Whites (Table 2). Higher residential density was also associated with 50–59-year-olds and at least a college education. Higher residential density was also associated with college education and age. Prevalent obesity was associated with lower residential density, lower property values, and lower counts of supermarkets and fast-food restaurants within a 1600 m radius.
Table 2.
Baseline residential property values and built environment characteristics by sample sociodemographic characteristics (n = 819).
| Characteristic | Residential property values (parcel level) |
Residential density (800 m) |
Road intersection density (800 m) |
Fast-food restaurant availability (1600 m) |
Supermarket availability (1600 m) |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Tertile |
Tertile |
Tertile |
0 |
1 to 3 |
4+ |
0 |
1+ |
|||||||
| 1 |
2 |
3 |
1 |
2 |
3 |
1 |
2 |
3 |
||||||
| % | % | % | % | % | % | % | % | % | % | % | % | % | % | |
| Age (years) | ||||||||||||||
| 21-39 | 44.2 | 34.9 | 20.8 | 37.2 | 30.9 | 32.0 | 35.3 | 34.9 | 29.7 | 20.5 | 27.9 | 59.1 | 35.7 | 64.3 |
| 40-49 | 38.8 | 30.8 | 30.4 | 42.1 | 35.4 | 22.5 | 40.0 | 33.8 | 26.3 | 29.6 | 27.1 | 34.6 | 42.1 | 47.9 |
| 50-61 | 20.0 | 33.6 | 46.5 | 23.2 | 33.9 | 42.9 | 26.8 | 32.3 | 41.0 | 19.7 | 30.2 | 58.3 | 28.7 | 71.3 |
| Gender | ||||||||||||||
| Men | 18.4 | 40.8 | 40.8 | 13.2 | 28.3 | 58.6 | 15.1 | 31.6 | 53.3 | 11.8 | 21.7 | 66.5 | 19.7 | 80.3 |
| Women | 36.9 | 31.5 | 31.6 | 37.9 | 34.5 | 27.6 | 37.6 | 34.0 | 28.3 | 25.3 | 29.5 | 45.1 | 38.4 | 61.6 |
| Race/ethnicity | ||||||||||||||
| Non-Hispanic White | 5.9 | 37.9 | 56.3 | 11.8 | 34.8 | 53.5 | 19.2 | 29.9 | 50.9 | 18.2 | 22.8 | 59.1 | 25.3 | 74.7 |
| Hispanic | 72.0 | 22.3 | 5.7 | 67.2 | 29.8 | 3.0 | 54.8 | 38.0 | 7.2 | 31.6 | 33.7 | 34.6 | 47.3 | 52.7 |
| Other | 12.5 | 52.1 | 35.4 | 4.2 | 39.6 | 56.3 | 17.7 | 33.3 | 49.0 | 11.5 | 30.2 | 58.3 | 31.3 | 68.8 |
| Education | ||||||||||||||
| High school or less | 72.8 | 22.9 | 4.3 | 66.7 | 28.0 | 5.4 | 55.2 | 36.6 | 8.2 | 31.5 | 29.8 | 38.7 | 48.0 | 52.0 |
| Some College | 28.3 | 41.8 | 29.9 | 23.2 | 45.8 | 31.1 | 29.4 | 36.2 | 34.5 | 20.9 | 27.1 | 52.0 | 34.5 | 65.5 |
| College or more | 5.8 | 36.9 | 57.3 | 12.7 | 31.4 | 55.9 | 18.7 | 30.0 | 51.2 | 17.1 | 27.3 | 55.7 | 25.1 | 74.9 |
| Home ownership | ||||||||||||||
| Rent or other | 45.9 | 37.8 | 16.3 | 38.8 | 24.8 | 36.4 | 36.4 | 30.6 | 33.0 | 17.35 | 24.8 | 57.8 | 33.3 | 66.7 |
| Own | 26.5 | 30.7 | 42.9 | 30.3 | 38.1 | 31.6 | 31.8 | 35.2 | 33.0 | 25.9 | 29.9 | 44.2 | 35.8 | 64.2 |
| Body mass index (BMI) category | ||||||||||||||
| Normal weight (BMI <25.0 kg/m2)a | 12.0 | 33.3 | 54.6 | 15.7 | 30.6 | 53.7 | 18.5 | 28.2 | 53.2 | 15.3 | 24.1 | 60.7 | 25.0 | 75.0 |
| Overweight (BMI ≥25.0 kg/m2 and <30.0 kg/m2) | 32.4 | 31.6 | 36.0 | 31.6 | 35.2 | 33.2 | 30.8 | 37.7 | 31.6 | 21.5 | 27.9 | 50.6 | 31.6 | 68.4 |
| Obese (BMI ≥30 kg/m2) | 47.2 | 34.3 | 18.5 | 45.2 | 33.7 | 21.1 | 44.4 | 34.0 | 21.6 | 28.4 | 30.6 | 41.0 | 43.3 | 56.7 |
Note: All densities calculated as units per hectare. Residential property value tertile ranges are: Tertile 1: $10,889 to $130,644; Tertile 2: $133,974 to $295,000; Tertile 3: $300,300 to $1,492,000. Residential density tertile ranges are: Tertile 1: 0.01 to 3.74; Tertile 2: 3.74 to 9.01; Tertile 3: 9.05 to 104.86. Road intersection density tertile ranges are: Tertile 1: 0.00 to 0.35; Tertile 2: 0.35 to 0.57; Tertile 3: 0.57 to 1.12.
Included in this group are fewer than 10 participants are underweight.
Table 3 shows the cross-sectional relation between baseline BMI, residential property values, and BE measures. Mean baseline BMI was 30.0 kg/m2 (95% CI: 29.5, 30.4). The top tertile of residential property values was associated with lower BMI compared lowest tertile (28.4 kg/m2, 95% CI: 27.4, 29.3 vs 30.6 kg/m2, 95% CI: 29.6, 31.7, p = 0.012). There were no differences in BMI across tertiles of residential density. However, the highest tertile of intersection density (800 m buffer) was associated with lower mean BMI compared to the lowest (28.9 kg/m2, 95% CI: 28.0, 29.7 vs 30.7 kg/m2, 95% CI: 29.8, 31.6, p = 0.008). Higher counts (4+) of fast-food restaurants (1600 m buffer) were associated with lower BMI compared to none (29.2 kg/m2, 95% CI: 28.6, 29.9 vs 30.8 kg/m2, 95% CI: 29.8, 31.8, p = 0.012). Higher counts (1+) of supermarkets (1600 m buffer) were associated with lower BMI compared to none (29.5 kg/m2, 95% CI: 28.9, 30.0 vs 30.9 kg/m2, 95% CI: 30.1, 31.8, p = 0.005).
Table 3.
Baseline cross-sectional associations between BMI (kg/m2) residential property values, and built environment characteristics (n = 819).
| Characteristic | Mean | (95% CI) | P-value |
|---|---|---|---|
| Overall | 30.0 | (29.5, 30.4) | – |
| Socioeconomic status | |||
| Residential property value, parcel level | |||
| Tertile 1: $10,889 to $130,644 | 30.6 | (29.5, 31.7) | – |
| Tertile 2: $133,974 to $295,000 | 31.0 | (30.1, 31.8) | 0.652 |
| Tertile 3: $300,300 to $1,492,000 | 28.4 | (27.4, 29.3) | 0.012 |
| Built environment | |||
| Residential density, 800 m buffer | |||
| Tertile 1: 0.01 to 3.74 | 30.6 | (29.5, 31.6) | – |
| Tertile 2: 3.74 to 9.01 | 30.3 | (29.5, 31.1) | 0.712 |
| Tertile 3: 9.05 to 104.86 | 29.0 | (28.1, 30.0) | 0.072 |
| Road intersection density, 800 m buffer | |||
| Tertile 1: 0.00 to 0.35 | 30.7 | (29.8, 31.6) | – |
| Tertile 2: 0.35 to 0.57 | 30.3 | (29.5, 31.1) | 0.512 |
| Tertile 3: 0.57 to 1.12 | 28.9 | (28.0, 29.7) | 0.008 |
| Fast-food restaurant availability, 1600 m buffer | |||
| 0 | 30.8 | (29.8, 31.8) | – |
| 1-3 | 30.6 | (29.7, 31.5) | 0.770 |
| 4+ | 29.2 | (28.6, 29.9) | 0.012 |
| Supermarket availability, 1600 m buffer | |||
| 0 | 30.9 | (30.1, 31.8) | – |
| 1+ | 29.5 | (28.9, 30.0) | 0.005 |
BMI = body mass index; CI = confidence interval.
Note: All densities calculated as units per hectare. Residential unit and road intersection densities based on Euclidean distance. Fast-food restaurant and supermarket counts based on network-based buffer. Buffers of 800 m correspond, approximately, to 10-min walkable distance while buffers of 1600 m correspond to a 20-min walkable distance. Models adjust age, gender, race/ethnicity, education, home ownership, and county of residence.
P-values test for differences between the 2nd or 3rd tertile compared to the 1st for density measures, 1–3 or 4+ fast-food restaurants versus 0 for fast-food restaurant availability, and 1+ versus 0 for supermarket availability.
It should be noted that residential property values were moderately correlated with residential density (r = 0.46) and road intersection density (r = 0.34) (Supplemental Table 1). However, residential property values were weakly correlated with counts of supermarkets (r = 0.13) and fast-food restaurants (r = 0.06). Bivariate associations between residential property values and BE variables along with data on changes in BMI are provided in Supplemental Figs. 1 and 2.
Table 4 shows the associations between residential property values, BE measures, and adjusted mean BMI change from baseline to 1-year and 2-year follow-up. Overall, BMI increased by 0.10 units (95% CI: -0.01, 0.20) from baseline to 1-year. At 1-year follow-up, there was no evidence of a difference in mean BMI by residential property values or supermarket availability. However, there was evidence of a 1-year difference across measures of urban form and fast-food restaurant availability. Compared with participants in the lowest tertile, participants residing in areas with the highest tertile of residential density (mean BMI change: -0.01 kg/m2, 95% CI: -0.18, 0.15 vs 0.26 kg/m2, 95% CI: 0.06, 0.45, p = 0.038) and road intersection density (mean BMI change: -0.07 kg/m2, 95% CI: 0.23, 0.09 vs 0.37 kg/m2, 95% CI: 0.18, 0.56, p < 0.001) experienced less change in their BMI. There was also evidence of less change in BMI between the 2nd and 1st tertile of road intersection density (p = 0.004). Compared to those participants with 0 fast-food restaurants within a 1600 m buffer from their home, those with 4+ experience less change in their BMI (mean BMI change: -0.03 kg/m2, 95% CI: 1–17, 0.10 vs 0.26 kg/m2, 95% CI: 0.02, 0.50, p = 0.037).
Table 4.
Association between baseline residential property values and built environment characteristics with BMI (kg/m2) at 1 and 2 years from baseline (n = 819).
| Characteristic | 1 year |
2 years |
||||
|---|---|---|---|---|---|---|
| Mean | (95% CI) | P-value | Mean | (95% CI) | P-value | |
| Overall | 0.10 | (-0.01, 0.20) | – | 0.29 | (0.16, 0.43) | – |
| Socioeconomic status | ||||||
| Residential property value, parcel level | ||||||
| Tertile 1: $10,889 to $130,644 | 0.19 | (0.00, 0.37) | – | 0.43 | (0.17, 0.70) | – |
| Tertile 2: $133,974 to $295,000 | 0.06 | (-0.12, 0.24) | 0.342 | 0.38 | (0.13, 0.62) | 0.747 |
| Tertile 3: $300,300 to $1,492,000 | 0.05 | (-0.11, 0.20) | 0.264 | 0.08 | (-0.11, 0.26) | 0.031 |
| Built environment | ||||||
| Residential density, 800 m buffer | ||||||
| Tertile 1: 0.01 to 3.74 | 0.26 | (0.06, 0.45) | – | 0.48 | (0.23, 0.73) | – |
| Tertile 2: 3.74 to 9.01 | 0.05 | (-0.12, 0.21) | 0.099 | 0.17 | (-0.06, 0.39) | 0.068 |
| Tertile 3: 9.05 to 104.86 | −0.01 | (-0.18, 0.15) | 0.038 | 0.23 | (0.02, 0.45) | 0.141 |
| Road intersection density, 800 m buffer | ||||||
| Tertile 1: 0.00 to 0.35 | 0.37 | (0.18, 0.56) | – | 0.46 | (0.22, 0.71) | – |
| Tertile 2: 0.35 to 0.57 | −0.01 | (-0.18, 0.16) | 0.004 | 0.25 | (0.02, 0.48) | 0.217 |
| Tertile 3: 0.57 to 1.12 | −0.07 | (0.23, 0.09) | <0.001 | 0.17 | (-0.05, 0.38) | 0.076 |
| Fast-food restaurant availability, 1600 m buffer | ||||||
| 0 | 0.26 | (0.02, 0.50) | – | 0.43 | (0.14, 0.72) | – |
| 1-3 | 0.19 | (0.00, 0.38) | 0.651 | 0.50 | (0.25, 0.75) | 0.704 |
| 4+ | −0.03 | (-0.17, 0.10) | 0.037 | 0.11 | (-0.08, 0.29) | 0.070 |
| Supermarket availability, 1600 m buffer | ||||||
| 0 | 0.21 | (0.01, 0.40) | – | 0.44 | (0.19, 0.70) | – |
| 1+ | 0.04 | (-0.08, 0.16) | 0.146 | 0.22 | (0.06, 0.37) | 0.135 |
BMI = body mass index; CI = confidence interval.
Note: All estimates represent the change in weight or BMI comparing 1-year or 2-year follow-up to baseline. All densities calculated as units per hectare. Residential unit and road intersection densities based on Euclidean distance. Fast-food restaurant and supermarket counts based on network-based buffer. Buffers of 800 m correspond, approximately, to 10-min walkable distance while buffers of 1600 m correspond to a 20-min walkable distance. Separate linear mixed models with the outcome percent weight change at 1 and 2 years from baseline for each built environment characteristic adjusting for age, gender, race/ethnicity, home ownership, and county of residence.
P-values test for differences between the 2nd or 3rd tertile compared to the 1st for density measures, 1–3 or 4+ fast-food restaurants versus 0 for fast-food restaurant availability, and 1+ versus 0 for supermarket availability.
At year 2, overall BMI gain was 0.29 kg/m2 (95% CI: 0.16, 0.43). There was no difference in mean BMI change by residential or road intersection density tertiles nor fast-food restaurant or supermarket availability; however, there was evidence of a 2-year difference for residential property values. Compared with participants in the lowest tertile of residential property values, participants in the highest tertile experienced less BMI change (mean BMI change: 0.08 kg/m2, 95% CI: -0.11, 0.26 vs. 0.43 kg/m2, 95% CI: 0.17, 0.70, p = 0.031).
3.1. Effect measure modification by sociodemographic factors
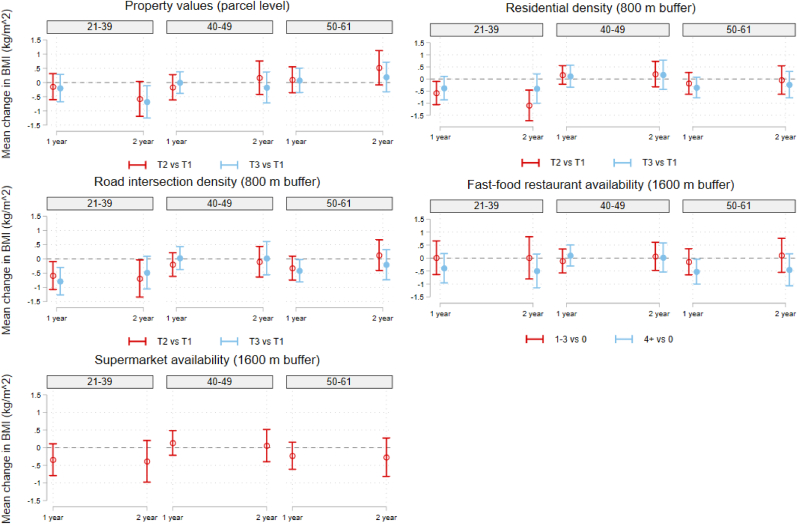
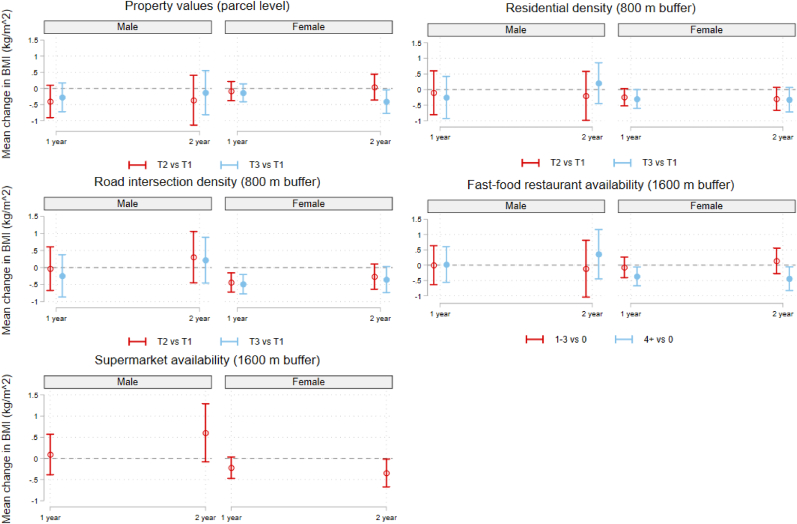
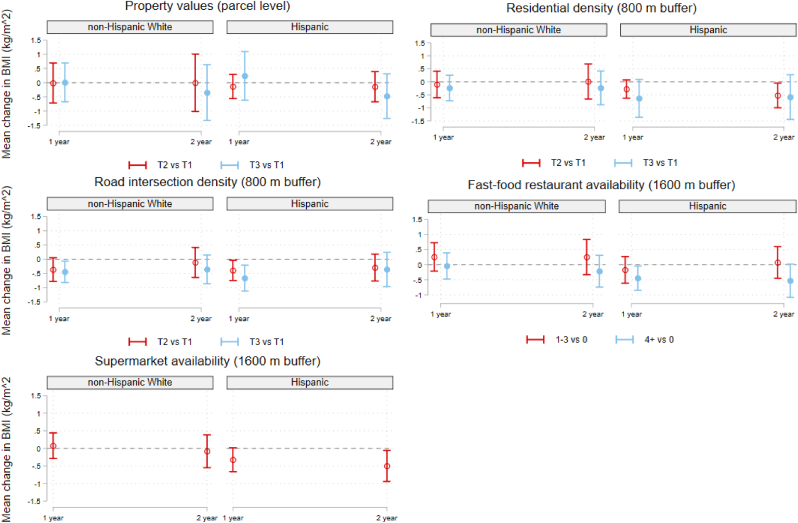
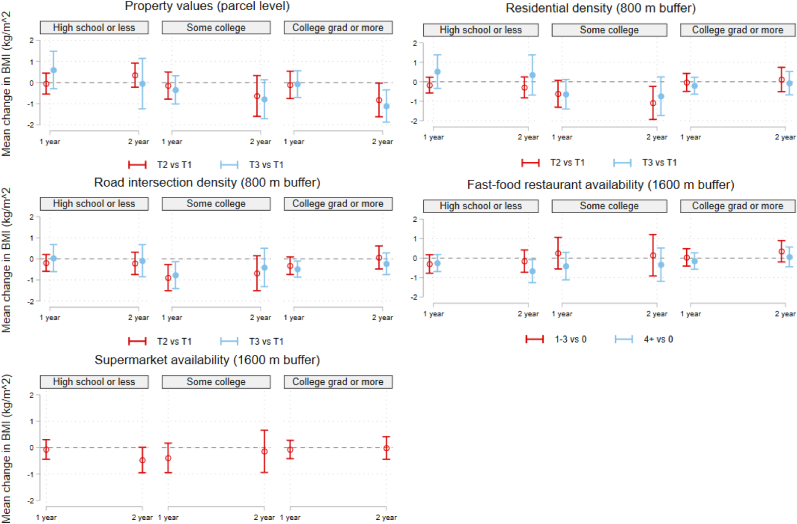
Fig. 1, Fig. 2, Fig. 3, Fig. 4 display the association between residential property values, BE variables, and mean BMI change at 1- and 2-years from baseline across sociodemographic factors. Broadly there was evidence of differential associations by age, gender, and education but not race/ethnicity. A full set of cross-sectional analyses across these sociodemographic factors can be found in Supplemental Figs. 3–6.
Fig. 1.
Change in mean BMI (kg/m2) from baseline to 1- and 2-year follow-up associated with the interaction between categorical age, property values, and built environment characteristics (n = 819).
BMI = body mass index.
Note: All densities calculated as units per hectare. Residential property value tertile ranges are: T1: $10,889 to $130,644; T2: $133,974 to $295,000; T3: $300,300 to $1,492,000. Residential density tertile ranges are: T1: 0.01 to 3.74; T2: 3.74 to 9.01; T3: 9.05 to 104.86. Road intersection density tertile ranges are: T1: 0.00 to 0.35; T2: 0.35 to 0.57; T3: 0.57 to 1.12. Models adjust for age, gender, race/ethnicity, education, home ownership, and county of residence.
Fig. 2.
Change in mean BMI (kg/m2) from baseline to 1- and 2-year follow-up associated with the interaction between gender, property values, and built environment characteristics (n = 819).
BMI = body mass index.
Note: All densities calculated as units per hectare. Residential property value tertile ranges are: T1: $10,889 to $130,644; T2: $133,974 to $295,000; T3: $300,300 to $1,492,000. Residential density tertile ranges are: T1: 0.01 to 3.74; T2: 3.74 to 9.01; T3: 9.05 to 104.86. Road intersection density tertile ranges are: T1: 0.00 to 0.35; T2: 0.35 to 0.57; T3: 0.57 to 1.12. Models adjust for age, gender, race/ethnicity, education, home ownership, and county of residence.
Fig. 3.
Change in mean BMI (kg/m2) from baseline to 1- and 2-year follow-up associated with the interaction between race/ethnicity, property values, and built environment characteristics (n = 723).
BMI = body mass index.
Note: Race/ethnicity category ‘Other’ excluded from models (n = 96) due to small sample size limitations. All densities calculated as units per hectare. Residential property value tertile ranges are: T1: $10,889 to $130,644; T2: $133,974 to $295,000; T3: $300,300 to $1,492,000. Residential density tertile ranges are: T1: 0.01 to 3.74; T2: 3.74 to 9.01; T3: 9.05 to 104.86. Road intersection density tertile ranges are: T1: 0.00 to 0.35; T2: 0.35 to 0.57; T3: 0.57 to 1.12. Models adjust for age, gender, race/ethnicity, education, home ownership, and county of residence.
Fig. 4.
Change in mean BMI (kg/m2) from baseline to 1- and 2-year follow-up associated with the interaction between education, property values, and built environment characteristics (n = 819).
BMI = body mass index.
Note: All densities calculated as units per hectare. Residential property value tertile ranges are: T1: $10,889 to $130,644; T2: $133,974 to $295,000; T3: $300,300 to $1,492,000. Residential density tertile ranges are: T1: 0.01 to 3.74; T2: 3.74 to 9.01; T3: 9.05 to 104.86. Road intersection density tertile ranges are: T1: 0.00 to 0.35; T2: 0.35 to 0.57; T3: 0.57 to 1.12. Models adjust for age, gender, race/ethnicity, education, home ownership, and county of residence.
Across age, there was significant evidence that residential property values led to less BMI change at 2 years in 21–39-year-olds compared to 50-61-year-olds when comparing the 2nd and 1st tertile (p = 0.013) and the 3rd to the 1st tertile (p = 0.027) (Fig. 1). There was also evidence of difference BMI change by residential density at 1 year when comparing the 2nd and 1st tertiles between 21 and 39-year-olds compared to 40-49-year-olds (p = 0.018) and at 2 years comparing the 2nd and 1st tertiles between 21 and 39-year-olds compared to 40-49-year-olds (p = 0.002) and 50-61-year-olds (p = 0.017). Although there was suggestive evidence of a differential association by age for road intersection density, we were unable to detect differences between age groups. By gender, when comparing supermarket availability among women and men, there was evidence of a significant difference in mean BMI change from baseline to 2-year follow-up (p = 0.015) (Fig. 2). There was suggestive evidence that education may modify the association between residential property values and 2-year BMI change with a greater association observed among respondents with a college education or more (Fig. 4). However, we were only able to detect a significant difference at 2 years comparing the 2nd and 1st tertile of residential property values between those respondents with a college degree or higher to those with a high school degree or less (p = 0.019).
4. Discussion
Consistent with early cross-sectional work, the present study found that road intersection density and greater proximity to both supermarkets and fast-food restaurants were associated with lower BMI at baseline (Buszkiewicz et al., 2021a, 2021b; Drewnowski et al., 2020). That higher residential property values were also cross-sectionally associated with lower BMI builds upon prior work which showed a relationship between higher values and lower prevalent obesity (Drewnowski et al., 2015b, 2020). However, these strong, inverse, cross-sectional associations between residential property values, BE measures, and BMI did not always translate to changes in BMI at 1- and 2-year follow-up. At year 1, residential density, road intersection density, and fast-food restaurant availability were associated with 1-year BMI change. At year 2, associations with BE measures were no longer observed with only residential property values associated 2-year BMI change in the SOS III cohort. Importantly, we also observed that associations between the BE, residential property values, and 1- and 2-year BMI change varied by age, gender, and education but not by race/ethnicity.
Although overall associations between measures of the BE, property values, and BMI change were small, there were some notable findings. First, we did not observe a relationship between residential property values and 1-year BMI change but we did observe an association with 2-year weight change (Drewnowski et al., 2015a). Similar work using property appraisal data as a proxy for neighborhood condition found an inverse relation between change in neighborhood condition and weight change at 7-year follow-up, which was more pronounced among those residents who did not move (Leonard et al., 2017). Other work using hedonistic price models to define neighborhood deprivation found that individuals who lived in or moved to more disadvantaged neighborhoods tended to gain more weight over a period of 7 years (Powell-Wiley et al., 2015). Second, the finding that denser urban form was linked to lower mean BMI at baseline and was associated with BMI change at 1-year follow-up is consistent with the hypothesis that BE features that are more conducive to walking and active transport help to lower obesity risk (Drewnowski et al., 2020; Lake et al., 2017; Lam et al., 2021; McCormack et al., 2018; Mooney et al., 2020a; Salvo, Lashewicz, Doyle-Baker, & McCormack, 2018). Similar findings from the much larger Moving to Health cohort were reported recently (Buszkiewicz et al., 2021a, 2021b). Third, recent studies of the association between the local food environment and prevalent obesity have come to the growing conclusion that no such association may exist (Cobb et al., 2015; Drewnowski et al., 2020; Lam et al., 2021; Wilkins et al., 2019). This may be due, in part, to the types of metrics that are frequently used. Density counts of supermarkets, grocery stores, fast-food restaurants, and convenience stores within close to one's home were among the most frequent measures of putative exposure to the food environment. However, these measures tend to be highly correlated with urban density. Our limited findings with respect to the relation between fast-food restaurants, supermarkets, and weight in cross-sectional analyses and fast-food restaurants and BMI change in longitudinal analyses may be entirely explained by their close correlation with measures of urban form as exhibited in prior work (Buszkiewicz et al., 2021b).
Although there have been several studies that have evaluated the association between the BE and BMI change in specific sociodemographic subpopulations, few studies have directly examined differences across sociodemographic strata. With respect to age, our suggestive findings of a greater association between the BE and BMI change at younger ages stands in contrast with the mixed body of evidence which has found stronger associations in older adults (Hobbs et al., 2019a), younger adults (Hobbs et al., 2019c; Sarkar et al., 2017), or no association at all (Buszkiewicz et al., 2021a). Prior work has found men and women may be sensitive to different aspects of the BE related to walkability and active transport, which may, in turn, influence long-term obesity risk (Bell et al., 2014; Buszkiewicz et al., 2021a; Sarkar et al., 2017). However, our finding of a differential association between supermarket availability and BMI change may be related to our study inclusion criteria which stipulated that participants must be the primary food shoppers in their household, a role which disproportionally falls to women. Our lack of finding a differential relationship between BE and BMI by race/ethnicity change stands in contrast with prior work suggesting that the BE may disproportionately benefit non-Hispanic Whites (Wong et al., 2018). One study found that measures of the BE were associated with less weight gain in non-Hispanic Whites and non-Hispanic Blacks but found no such association in Hispanics or non-Hispanic Asians (Buszkiewicz et al., 2021a). More work is needed to understand the underlying structural factors underpinning these health inequities. Finally, to our knowledge, our finding that the association between residential property values and BMI change may be stronger in those with higher education is novel and warrants further study.
This study had several notable strengths. First, this study extends the prior work of SOS I (cross-sectional) and SOS II (1-year follow-up) by 1) examining 2-year change in BMI, 2) directly comparing the association between measures of the BE and BMI change to the association between residential property values and BMI change, and 3) evaluating these associations in both an urban (King County, Pierce County) and rural (Yakima County) settings (Office of Financial Management, 2019). Second, we extend the broad BE-obesity literature by examining the association between the BE, residential property values, and 1- and 2-year BMI change across age, gender, race/ethnicity, and education. To our knowledge, few studies have directly evaluated the BE-BMI change relationship across these sociodemographic subpopulations with most prior work focusing on restricting their analyses to specific populations (Buszkiewicz et al., 2021a; Drewnowski et al., 2020; Letarte et al., 2020). Moreover, this study represents the first study to evaluate the residential property value-BMI change relation in this manner.
This study also had limitations. First, duration of exposure to baseline BE measures could not be determined. The observed BE and social gradient in obesity prevalence could be the result of an accumulated influence of the BE on weight over a prolonged period. Second, reasons for living in a particular neighborhood were not explored. There are many economic and sociodemographic determinants which influence health, where individuals can live, and whether individuals are able to relocate that undergird observed neighborhood BE exposures (Drewnowski et al., 2020). Historic patterns of residential segregation, driven by systemic, structural racism, has profoundly impacted the human geography of the US and other cities (Popescu, Duffy, Mendelsohn, & Escarce, 2018). Moreover, longstanding inequities in educational opportunities, work opportunities, and intergenerational accumulation of wealth not only influence where individuals live, but how they interact with their neighborhood BE and subsequent health outcomes (Tung, Cagney, Peek, & Chin, 2017). Indeed these systemic, structural factors highlight the limitations of cross-sectional studies of the BE, weight, and BE and the need for more longitudinal work. Third, the study did not measure usage of neighborhood resources. Residing in a given neighborhood does not necessarily mean residents will utilize those resources since others factors, such as preference or economic barriers may be at play (Sharp, Macrorie, & Turner, 2015). Fourth, restricting analyses of BE and health to the residential environment may overestimate the possible influence of that BE since people's exposure includes BE beyond that of their place of residence (Chaix et al., 2017). Fifth, although our use of flexible SmartMap-based BE measures and residential property values at the parcel level did not restrict our measures to administrative boundaries, future work should also consider the role of spatial interrelatedness (Coman, Steinbach, & Cao, 2021). This may be particularly important in much larger cohorts where the likelihood of having participants adjacent in space may be higher. Sixth, the SOS III cohort was small and therefore lacked power to detect many differences across sociodemographic subpopulations. Nevertheless, we believe it is critical to health equity research to examine differential BE-BMI associations across sociodemographic factors and that it remains a fruitful area for future research (Buszkiewicz et al., 2021a; Letarte et al., 2020; Wong et al., 2018; Zhang & Yin, 2019).
Since our evaluation of BE characteristics is based within the context of WA State, the extent to which these findings are readily generalizable to other US states or internationally is uncertain. Tax assessor data may be harder to obtain for some areas, may not be practical for use in areas without open markets, or where home sales or rent renewals are sporadic. Moreover, residential property values may not be predictive of health in all communities or countries. Finally, we lacked the power to distinguish more precise differences in mean percentage weight change for many BE metrics. Relatedly, we were unable to explore interactions between measures of urban form, the food environment, and residential property values.
5. Conclusions
Observed, clear differences in BMI across residential property values and BE metrics at baseline were consistent with early, cross-sectional work pointing to strong, inverse associations with prevalent obesity. However, much like newer analyses of large, longitudinal cohorts, we observed modest and inconsistent associations between the BE, property values, and 1- and 2-year BMI change. We also found suggestive evidence that age may moderate the association between urban density and BMI change while education may moderate the association between residential property values and BMI change. Larger longitudinal cohorts are needed to explore whether and to what extent measures of BE disadvantage are associated with trajectories of weight gain across population subgroups over extended periods of time. A question of particular interest is what structural or social forces act to promote or concentrate obesity in so called ‘obesogenic’ neighborhoods.
Ethical statement
I certify that all study procedures were approved by the institutional review boards at each site (UW Human Subjects Division/Fred Hutch HSD# 50269, MultiCare IRB protocol #16.07). Further documentation to this effect is available upon request.
Author statement
AD developed the initial study concepts. AD, CMR, LKK, and JM lead study site recruitment. AVM and PMH developed the SmartMaps exposure assessment tool. AC, AD, CMR, and JHB developed the study design and analytic plan with consultation from all other co-authors and JHB conducted analyses. JHB wrote the manuscript with the assistance of AD. All authors provided critical feedback and helped shape the research, analysis, interpretation of findings, and the manuscript. AD provided project supervision.
Declaration of competing interest
Adam Drewnowski has received grants, honoraria, and consulting fees from numerous food, beverage, and ingredient companies and from other commercial and nonprofit entities with an interest in diet quality and nutrient density of foods. All other authors have no conflicts of interest to declare.
Acknowledgements:
This manuscript was supported by a grant from the National Institutes of Health: 5 R01 DK076608-10.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ssmph.2022.101158.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- Assari S. Unequal gain of equal resources across racial groups. International Journal of Health Policy and Management. 2018;7:1–9. doi: 10.15171/ijhpm.2017.90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bell J.A., Hamer M., Shankar A. Gender-specific associations of objective and perceived neighborhood characteristics with body mass index and waist circumference among older adults in the English Longitudinal Study of Ageing. American Journal of Public Health. 2014;104:1279–1286. doi: 10.2105/AJPH.2014.301947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berrigan D., Hipp J.A., Hurvitz P.M., et al. Geospatial and contextual approaches to energy balance and health. Annals of GIS. 2015;21:157–168. doi: 10.1080/19475683.2015.1019925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buszkiewicz J.H., Bobb J.F., Hurvitz P.M., et al. Does the built environment have independent obesogenic power? Urban form and trajectories of weight gain. International Journal of Obesity. 2021;45:1914–1924. doi: 10.1038/s41366-021-00836-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buszkiewicz J.H., Bobb J.F., Kapos F., et al. Differential associations of the built environment on weight gain by sex and race/ethnicity but not age. International Journal of Obesity. 2021;45:2648–2656. doi: 10.1038/s41366-021-00937-9. 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buszkiewicz J., Rose C., Gupta S., Ko L.K., Mou J., Moudon A.V., et al. A cross-sectional analysis of physical activity and weight misreporting in diverse populations: The Seattle Obesity Study III. Obesity Science Practical. 2020;6:615–627. doi: 10.1002/osp4.449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chaix B., Duncan D., Vallée J., Vernez-Moudon A., Benmarhnia T., Kestens Y. The “Residential” effect fallacy in neighborhood and health studies: Formal definition, empirical identification, and correction. Epidemiology. 2017;28:789–797. doi: 10.1097/EDE.0000000000000726. [DOI] [PubMed] [Google Scholar]
- Cobb L.K., Appel L.J., Franco M., et al. The relationship of the local food environment with obesity: A systematic review of methods. Study Quality, and Results. 2015;23:1331–1344. doi: 10.1002/oby.21118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coffee N.T., Lockwood T., Rossini P., Niyonsenga T., McGreal S. Composition and context drivers of residential property location value as a socioeconomic status measure. Environ Plan B Urban Anal City Sci. 2020;47:790–807. [Google Scholar]
- Coman E.N., Steinbach S., Cao G. Spatial perspectives in family health research. Family Practice. 2021:1–7. doi: 10.1093/fampra/cmab165. [DOI] [PubMed] [Google Scholar]
- Congdon P. Obesity and urban environments. International Journal of Environmental Research and Public Health. 2019;16:464. doi: 10.3390/ijerph16030464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Drewnowski A., Aggarwal A., Cook A., Stewart O., Moudon A.V. Geographic disparities in healthy eating index scores (HEI-2005 and 2010) by residential property values: Findings from Seattle obesity study (SOS) Preventive Medicine. 2016;83:46–55. doi: 10.1016/j.ypmed.2015.11.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Drewnowski A., Aggarwal A., Tang W., Moudon A.A.V. Residential property values predict prevalent obesity but do not predict 1-year weight change. Obesity. 2015;23:671–676. doi: 10.1002/oby.20989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Drewnowski A., Aggarwal A., Tang W., Moudon A. Residential property values predict prevalent obesity but do not predict 1-year weight change. Obesity. 2015;23:671–676. doi: 10.1002/oby.20989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Drewnowski A., Arterburn D., Zane J., et al. The moving to health (M2H) approach to natural experiment research: A paradigm shift for studies on built environment and health. SSM - Population of Health. 2019;7 doi: 10.1016/j.ssmph.2018.100345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Drewnowski A., Buszkiewicz J., Aggarwal A., Rose C., Gupta S., Bradshaw A. Obesity and the built environment: A reappraisal. Obesity. 2020;28:22–30. doi: 10.1002/oby.22672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Durand C.P., Oluyomi A.O., Gabriel K.P., et al. The effect of light rail transit on physical activity: Design and methods of the travel-related activity in neighborhoods study. Frontiers in Public Health. 2016;4:103. doi: 10.3389/fpubh.2016.00103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- ESRI . Vol. 10. 2011. (ArcGIS desktop: Release). [Google Scholar]
- Garfinkel-Castro A., Kim K., Hamidi S., Ewing R. Obesity and the built environment at different urban scales: Examining the literature. Nutrition Reviews. 2017;75:51–61. doi: 10.1093/nutrit/nuw037. [DOI] [PubMed] [Google Scholar]
- Gupta S., Rose C.M., Buszkiewicz J., Otten J., Spiker M.L., Drewnowski A. Inedible food waste linked to diet quality and food spending in the Seattle Obesity Study SOS III. Nutrients. 2021;13:479. doi: 10.3390/nu13020479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hobbs M., Green M., Roberts K., Griffiths C., Mckenna J. Reconsidering the relationship between fast-food outlets, area-level deprivation, diet quality and body mass index: An exploratory structural equation modelling approach. Journal of Epidemiology & Community Health. 2019;73:861–866. doi: 10.1136/jech-2018-211798. [DOI] [PubMed] [Google Scholar]
- Hobbs M., Griffiths C., Green M.A., Christensen A., McKenna J. Examining longitudinal associations between the recreational physical activity environment, change in body mass index, and obesity by age in 8864 Yorkshire Health Study participants. Social Science & Medicine. 2019;227:76–83. doi: 10.1016/j.socscimed.2018.06.027. [DOI] [PubMed] [Google Scholar]
- Hobbs M., Griffiths C., Green M.A., Jordan H., Saunders J., Christensen A., et al. Fast-food outlet availability and obesity: Considering variation by age and methodological diversity in 22,889 Yorkshire Health Study participants. Spat Spatiotemporal Epidemiol. 2019;28:43–53. doi: 10.1016/j.sste.2018.11.001. [DOI] [PubMed] [Google Scholar]
- Huang R., Moudon A.V.A., Cook A.J., Drewnowski A. Vol. 28. 2015. pp. 604–612. (The spatial clustering of obesity: Does the built environment matter?). [DOI] [PubMed] [Google Scholar]
- Hurvitz P.M., Moudon A.V., Kang B., Saelens B.E., Duncan G.E. Emerging technologies for assessing physical activity behaviors in space and time. Frontiers in Public Health. 2014;2:2. doi: 10.3389/fpubh.2014.00002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laird N.M., Ware J.H. Random-effects models for longitudinal data. Biometrics. 1982;38:963–973. [PubMed] [Google Scholar]
- Lake A., Townshend T., Burgoine T., Buttriss J., Welch A., Kearney J., et al. In: Public heal. Nutr. Nutr. Soc. Textb. Ser. 2nd ed. Buttriss J., Welch A., JM K., SA L.-N., editors. 2017. Obesogenic neighbourhood food environments; pp. 327–338. [Google Scholar]
- Lam T.M., Vaartjes I., Grobbee D.E., Karssenberg D., Lakerveld J. Associations between the built environment and obesity: An umbrella review. International Journal of Health Geographics. 2021;20:1–24. doi: 10.1186/s12942-021-00260-6. 2021 201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leonard T., Ayers C., Das S.R., Neeland I.J., Powell-Wiley T.M. Do neighborhoods matter differently for movers and non-movers? Analysis of weight gain in the longitudinal dallas heart study. Health & Place. 2017;44:52–60. doi: 10.1016/j.healthplace.2017.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leonard T., Powell-Wiley T.M., Ayers C., Murdoch J.C., Yin W., Pruitt S.L. Property values as a measure of neighborhoods: An application of hedonic price theory. Epidemiology. 2016;27:518–524. doi: 10.1097/EDE.0000000000000470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Letarte L., Pomerleau S., Tchernof A., Biertho L., Owen E., Waygood D., et al. Neighbourhood effects on obesity: Scoping review of time-varying outcomes and exposures in longitudinal designs. BMJ Open. 2020;10:e034690. doi: 10.1136/bmjopen-2019-034690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCormack G., Blackstaffe A., Nettel-Aguirre A., Csizmadi I., Sandalack B., Uribe F., et al. The independent associations between walk Score® and neighborhood socioeconomic status, waist circumference, waist-to-hip ratio and body mass index among urban adults. International Journal of Environmental Research and Public Health. 2018;15:1226. doi: 10.3390/ijerph15061226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mooney S.J., Bobb J.F., Hurvitz P.M., et al. Impact of built environments on body weight (the moving to health study): Protocol for a retrospective longitudinal observational study. JMIR Research Protocol. 2020;9 doi: 10.2196/16787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mooney S.J., Hurvitz P.M., Moudon A.V., Zhou C., Dalmat R., Saelens B.E. 2020. Residential neighborhood features associated with objectively measured walking near home: Revisiting walkability using the Automatic Context Measurement Tool (ACMT). Heal Place. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moudon A.V.A., Cook A., Ulmer J., Hurvitz P. A neighborhood wealth metric for use in health studies. American Journal of Preventive Medicine. 2011;41:88–97. doi: 10.1016/j.amepre.2011.03.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Office of Financial Management . 2019. Population density and land area criteria used for rural area assistance and other programs.https://ofm.wa.gov/washington-data-research/population-demographics/population-estimates/population-density/population-density-and-land-area-criteria-used-rural-area-assistance-and-other-programs [Google Scholar]
- Okuyama Kenta, Li Xinjin, Abe Takafumi, Hamano Tsuyoshi, Franks Paul, Nabika Toru, Sundquist Kristina. Fast food outlets, physical activity facilities, and obesity among adults: a nationwide longitudinal study from Sweden. International Journal of Obesity. 2020;44:1703–1711. doi: 10.1038/s41366-020-0588-5. [DOI] [PubMed] [Google Scholar]
- Parise I. The built environment and obesity: You are where you live. Australian Jouranl of Genetical Practice. 2020;49:226–230. doi: 10.31128/AJGP-10-19-5102. [DOI] [PubMed] [Google Scholar]
- Popescu I., Duffy E., Mendelsohn J., Escarce J.J. Racial residential segregation, socioeconomic disparities, and the White-Black survival gap. PLoS One. 2018;13 doi: 10.1371/journal.pone.0193222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pouliou T., Elliott S.J. Individual and socio-environmental determinants of overweight and obesity in Urban Canada. Health & Place. 2010;16:389–398. doi: 10.1016/j.healthplace.2009.11.011. [DOI] [PubMed] [Google Scholar]
- Powell-Wiley T.M., Cooper-McCann R., Ayers C., Berrigan D., Lian M., McClurkin M., et al. Change in neighborhood socioeconomic status and weight gain: Dallas heart study. American Journal of Preventive Medicine. 2015;49:72–79. doi: 10.1016/j.amepre.2015.01.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- R Core Team . 2019. R: A language and environment for statistical computing. [Google Scholar]
- Rose C.M., Gupta S., Buszkiewicz J., Ko L.K., Mou J., Cook A., et al. Small increments in diet cost can improve compliance with the Dietary Guidelines for Americans. Social Science & Medicine. 2020;266 doi: 10.1016/j.socscimed.2020.113359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salvo G., Lashewicz B., Doyle-Baker P., McCormack G. Neighbourhood built environment influences on physical activity among adults: A systematized review of qualitative evidence. International Journal of Environmental Research and Public Health. 2018;15:897. doi: 10.3390/ijerph15050897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sarkar C., Webster C., Gallacher J. Association between adiposity outcomes and residential density: A full-data, cross-sectional analysis of 419 562 UK biobank adult participants. The Lancet Planetary Health. 2017;1 doi: 10.1016/S2542-5196(17)30119-5. e277–e288. [DOI] [PubMed] [Google Scholar]
- Sharp L., Macrorie R., Turner A. Resource efficiency and the imagined public: Insights from cultural theory. Global Environmental Change. 2015;34:196–206. [Google Scholar]
- StataCorp (2021) Stata statistical software: Release Vol. 17.
- The PostGIS Development Group . 2021. PostGIS. [Google Scholar]
- The PostgreSQL Global Development Group . 2021. The PostgreSQL. [Google Scholar]
- Tung E.L., Cagney K.A., Peek M.E., Chin M.H. Spatial context and health inequity: Reconfiguring race, place, and poverty. Journal of Urban Health. 2017;94:757–763. doi: 10.1007/s11524-017-0210-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vernez Moudon A., Drewnowski A., Duncan G.E., Hurvitz P.M., Saelens B.E., Scharnhorst E. Characterizing the food environment: Pitfalls and future directions. Public Health Nutrition. 2013;16:1238–1243. doi: 10.1017/S1368980013000773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Villanueva K., Knuiman M., Nathan A., Giles-Corti B., Christian H., Foster S., et al. The impact of neighborhood walkability on walking: Does it differ across adult life stage and does neighborhood buffer size matter? Health & Place. 2014;25:43–46. doi: 10.1016/j.healthplace.2013.10.005. [DOI] [PubMed] [Google Scholar]
- Ware J.K. Property value as a proxy of socioeconomic status in education. Education and Urban Society. 2019;51:99–119. [Google Scholar]
- Wilkins E., Radley D., Morris M., Hobbs M., Christensen A., Marwa W.L., et al. A systematic review employing the GeoFERN framework to examine methods, reporting quality and associations between the retail food environment and obesity. Health & Place. 2019;57:186–199. doi: 10.1016/j.healthplace.2019.02.007. [DOI] [PubMed] [Google Scholar]
- Wong M.S., Chan K.S., Jones-Smith J.C., Colantuoni E., Thorpe R.J., Bleich S.N. The neighborhood environment and obesity: Understanding variation by race/ethnicity. Preventive Medicine. 2018;111:371–377. doi: 10.1016/j.ypmed.2017.11.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang H., Yin L. A meta-analysis of the literature on the association of the social and built environment with obesity: Identifying factors in need of more in-depth research. American Journal of Health Promotion. 2019;33:792–805. doi: 10.1177/0890117118817713. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.