Abstract
Background:
Spinopelvic characteristics influence the hip’s biomechanical behavior. However, there is currently little knowledge regarding what “normal” characteristics are. This study aimed to determine how static and dynamic spinopelvic characteristics change with age, sex, and body mass index (BMI) among well-functioning volunteers.
Methods:
This was a cross-sectional cohort study of 112 asymptomatic volunteers (age, 47.4 ± 17.7 years; 50.0% female; BMI, 27.3 ± 4.9 kg/m2). All participants underwent lateral spinopelvic radiography in the standing and deep-seated positions to determine maximum hip and lumbar flexion. Lumbar flexion (change in lumbar lordosis, ∆LL), hip flexion (change in pelvic-femoral angle, ∆PFA), and pelvic movement (change in pelvic tilt, ΔPT) were determined. The hip user index, which quantifies the relative contribution of the hip to overall sagittal movement, was calculated as (∆PFA/[∆PFA + ∆LL]) × 100%.
Results:
There were decreases of 4.5° (9%) per decade of age in lumbar flexion (rho, −0.576; p < 0.001) and 3.6° (4%) per decade in hip flexion (rho, −0.365; p < 0.001). ∆LL could be predicted by younger age, low standing PFA, and high standing LL. Standing spinopelvic characteristics were similar between sexes. There was a trend toward men having less hip flexion (90.3° ± 16.4° versus 96.4° ± 18.1°; p = 0.065) and a lower hip user index (62.9% ± 8.2% versus 66.7% ± 8.3%; p = 0.015). BMI weakly correlated with ∆LL (rho, −0.307; p = 0.011) and ∆PFA (rho, −0.253; p = 0.039).
Conclusions:
Spinopelvic characteristics were found to be age, sex, and BMI-dependent. The changes in the lumbar spine during aging (loss of lumbar lordosis and flexion) were greater than the changes in the hip, and as a result, the hip’s relative contribution to overall sagittal movement increased. Men had a greater change in posterior pelvic tilt when moving from a standing to a deep-seated position in comparison with women, secondary to less hip flexion. The influence of BMI on spinopelvic parameters was low.
The relationship among the hip, pelvis, and spine has recently received great interest, as patients with spinopelvic pathology have been shown to have higher rates of complications, including dislocation, following total hip arthroplasty (THA)1-4. The position of the lumbar spine affects the pelvic position, which in turn influences acetabular orientation5,6, an important determinant of hip biomechanics in native4,7,8 and replaced hips9,10. In patients with hip osteoarthritis, femoroacetabular flexion is reduced, which is associated with an increased posterior pelvic tilt (PT) in the seated position and corresponding compensation in the lumbar spine (reduction in lordosis angle)11. This compensatory mechanism is reversed after THA in individuals without a history of spinal fusion12.
Changes in spinopelvic parameters during aging might be different between asymptomatic and symptomatic individuals, because the latter may have developed altered motion due to the underlying pathology13. In order to better understand the role of the sagittal spinopelvic characteristics in hip mechanics and THA outcomes, it is necessary to determine what “normal” is (i.e., spinopelvic characteristics in asymptomatic volunteers without a history of hip or spinal pathology), and to be able to predict how the characteristics differ with age and between sexes. Most literature has suggested that lumbar lordosis (LL) and hip flexion decrease during aging, and evidence exists for differences between males and females. However, most of these studies have only used clinical examination to evaluate range of motion or have only focused on a single aspect of the kinetic chain13-17.
The aims of this study were (1) to evaluate a cohort of asymptomatic volunteers to define “normal” radiographic static and dynamic spinopelvic parameters: LL, sacral slope (SS), PT, and pelvic-femoral angle (PFA), and their changes between standing and deep-seated positions (lumbar flexion [∆LL], hip flexion [∆PFA], and pelvic movement [ΔPT]), and (2) to determine whether and how these are influenced by age, sex, and body mass index (BMI).
Materials and Methods
This was an institutional review board-approved, single-center, prospective, cross-sectional cohort study. The hospital’s health-care workers and patients presenting to the fracture clinic with upper-limb injuries were invited to participate. Inclusion criteria included an age of ≥18 years, the absence of hip symptoms (Oxford hip score of ≥45, with 0 to 48 being worst to best), no signs of hip osteoarthritis (Tönnis grade of ≤1), and absence of spinal pathology (no history of spinal surgery and an Oswestry Disability Index of <20, with 0 to 100 being no to maximal disability). An a priori sample size calculation was performed using G*Power (version 3.1.9.2; Heinrich Heine University); a sample size of 111 patients was found to be sufficient to detect a change in PT, in moving from the standing to the “deep-seated” position, of ≥10° when 1 − β = 0.95, α = 0.05, and the standard deviation is 15°.
Cohort Description
A total of 117 volunteers were recruited between March 2018 and November 2021 at a tertiary academic center (The Ottawa Hospital) and signed an informed consent form. One volunteer was excluded due to previously undiagnosed scoliosis, and 4 volunteers had radiographs of insufficient quality; the remaining 112 volunteers were analyzed.
There were 56 male and 56 female volunteers (50% each). The mean age (and standard deviation) was 47.4 ± 17.7 years (range, 23.5 to 86.7 years), and the mean BMI was 27.3 ± 4.9 kg/m2 (range, 18.0 to 40.8 kg/m2). There were no significant differences in age (p = 0.119) or BMI (p = 0.719) between males and females (Table I).
TABLE I.
Demographics*
| Whole Cohort (N = 112) | Females (N = 56) | Males (N = 56) | P Value† | |
|---|---|---|---|---|
| Age (yr) | 47.4 ± 17.7 (23.0-86.7) | 50.1 ± 17.3 (23.5-75.8) | 44.7 ± 17.8 (23.0-86.7) | 0.119 |
| BMI (kg/m2) | 27.3 ± 4.9 (18.0-40.8) | 27.1 ± 5.3 (18.0-37.5) | 27.5 ± 4.5 (21.0-40.8) | 0.890 |
The values are given as the mean and standard deviation, with the range in parentheses.
Mann-Whitney U test.
Radiographic Assessments
Volunteers underwent radiographic assessment consisting of a standing and a supine anteroposterior radiograph of the pelvis and lateral radiographs of the lumbar spine, pelvis, and femur in the standing and deep-seated positions. In the deep-seated position, the volunteer sat on a height-adjustable chair with the femora parallel to the floor and the trunk tilted as far forward as possible without discomfort and without abducting or rotating the femora18-20. This position was chosen because it is associated with maximal sagittal flexion of the kinetic chain; it is the position at greatest risk for femoroacetabular impingement21 and has been shown to better identify spinal compensatory mechanisms18,22,23.
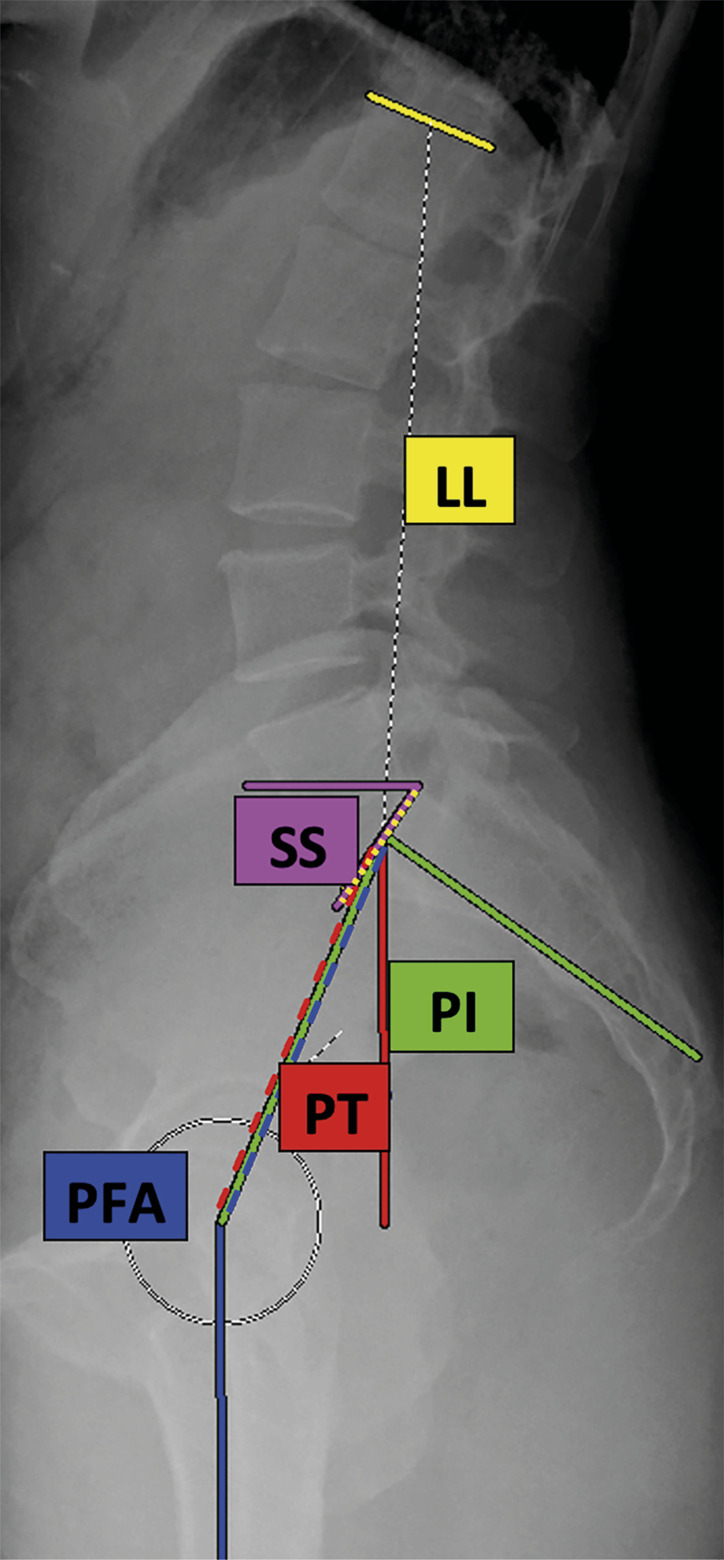
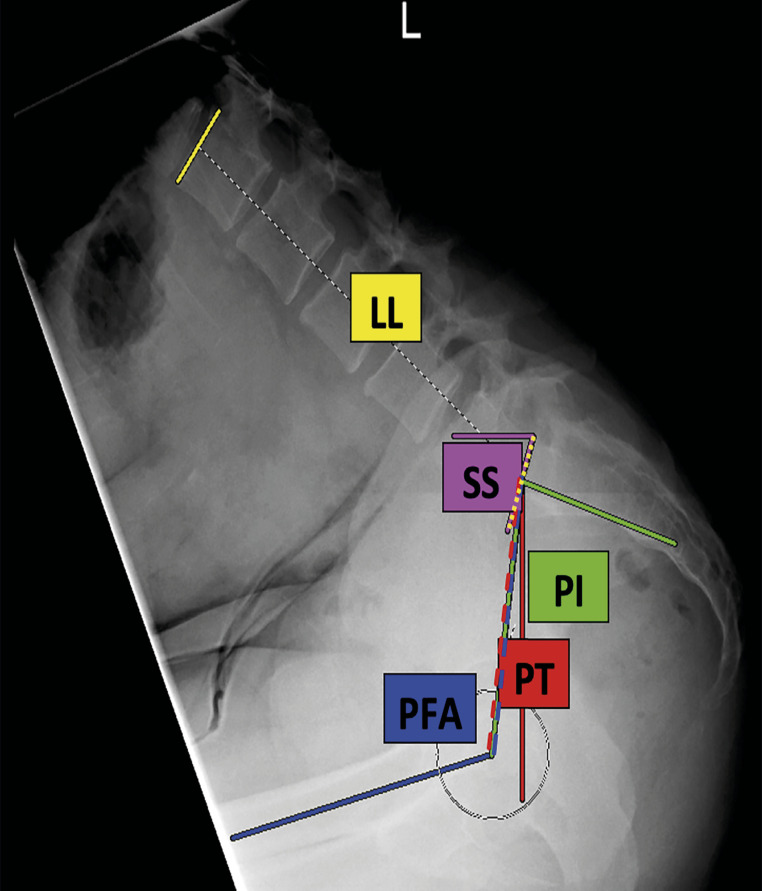
The following parameters were measured using PACS (picture archiving and communication system) software for digital radiography: LL, SS, pelvic incidence (PI), PT, and PFA3,11,18,20,24 (Figs. 1-A and 1-B , Table II). There were no missing values for any of the variables.
Fig. 1-A and Fig. 1-B.
Fig. 1-A and Fig. 1-B Examples of radiographic measurements of lumbar lordosis (LL), sacral slope (SS), pelvic tilt (PT), pelvic incidence (PI), and the pelvic-femoral angle (PFA) in 1 of the volunteers in the standing (Fig. 1-A) and the deep-seated (Fig. 1-B) position.
TABLE II.
Definitions of Spinopelvic Parameters
| Parameter | Definition |
|---|---|
| Lumbar lordosis (LL)26 | Lumbar lordosis was calculated as the Cobb angle between a line drawn along the superior end plate of L1 and another line drawn along the superior end plate of S1 |
| Sacral slope (SS)21 | Sacral slope was calculated as the angle between a line drawn along the superior end plate of S1 and the horizontal axis |
| Pelvic incidence (PI)21 | Pelvic incidence was calculated as the angle between the line from the center of the femoral heads to the middle of the superior end plate of S1, and the line perpendicular to the superior end plate of S1 from its midpoint |
| Pelvic tilt (PT)21 | Pelvic tilt was calculated as the angle formed between the line from the center of the femoral head to the middle of the superior end plate of S1 and the vertical axis |
| Pelvic-femoral angle (PFA)27 | The pelvic-femoral angle was calculated as the angle between the line from the center of the femoral heads to the middle of the superior end plate of S1 and the femoral axis |
The radiographic measurements were made by 2 reviewers, 1 fellowship-trained hip arthroplasty surgeon (J.C.F.V.) and 1 fellowship-trained spine surgeon (N.A.B.). Measurements were repeated for a randomly selected 20% of the data set in a blinded fashion. Interobserver reliability was calculated using the correlation coefficient with a 2-way mixed model, and showed excellent agreement of between 0.841 and 0.991 (see Appendix Supplementary Table 1).
Spinopelvic movements were calculated as the difference between the standing and deep-seated positions (∆X = ∆Xdeep-seated − ∆Xstanding) for each of the measured spinopelvic parameters (LL, SS, PI, PT, PFA)19. The sagittal flexion arc (SFA), which is the movement performed by the whole kinetic chain, was calculated as the sum of ∆LL and ∆PFA19.
The hip user index is a percentage that quantifies sagittal femoroacetabular flexion (∆PFA) relative to overall SFA when moving from the standing to the deep-seated position:
A high hip user index means that the hip contributes more to sagittal movement, whereas in a low hip user index, the movement takes place primarily in the lumbar spine19,23.
Patients were categorized into <40, 40 to 60.0, and >60-year age groups. Patients with a hip user index of ≥80% were categorized as hip users23. Spinopelvic balance was calculated as the difference between PI and LL in the standing position and was categorized as flatback (PI − LL: >10°), normal (PI − LL: −10° to 10°), or hyperlordotic (PI − LL: <−10°)6,25-27. Lumbar spinal stiffness was defined as a difference in LL between standing and deep-seated seated positions of ≤20°28.
Statistical Analysis
Statistical analyses were performed using SPSS (version 27; IBM). Continuous variables and categorical variables with 2 categories were compared with an independent-samples t test if they were normally distributed, or a Mann-Whitney U test if they were not. Categorical variables with >2 categories were compared with 1-way analysis of variance (ANOVA) or a Kruskal-Wallis test, respectively. The Spearman correlation coefficient and linear regression analysis were used to assess the correlation between age (as a continuous variable) and spinopelvic measurements. Correlation was graded as weak (rho, ≤0.3), moderate (rho, >0.3 to 0.5), strong (rho, >0.5 to 0.6), or very strong (rho, >0.6)8. Predictors of changes in spinopelvic measurements between standing and deep-seated positions were determined using a multiple regression analysis with a stepwise data entry method. A tolerance level of >0.20 was required in order to exclude collinearity. A p value of <0.05 was considered significant.
Source of Funding
This study was funded by a Physicians of Ontario (Physicians’ Services Incorporated Foundation) resident research grant.
Results
Cohort Characteristics
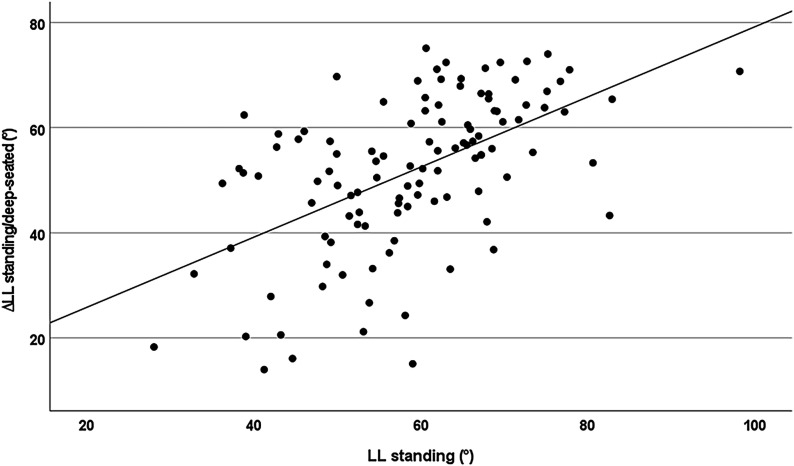
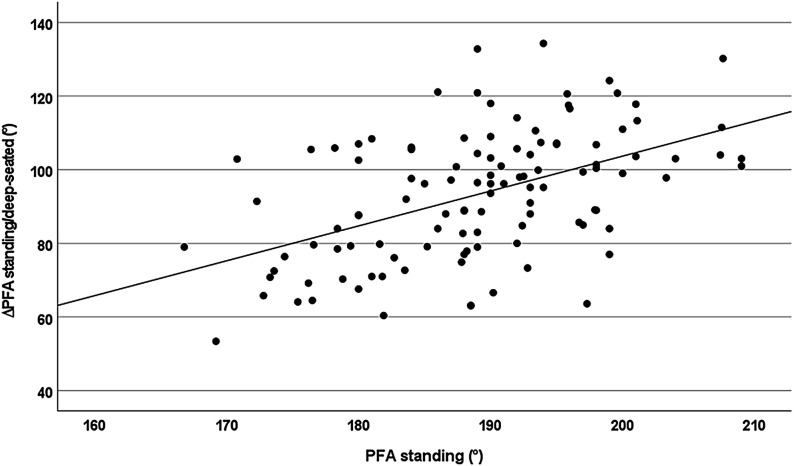
In this group of asymptomatic volunteers, the pelvis tilted an average of 8.4° ± 15.6° anteriorly during movement from the standing to the deep-seated position, while the hip and the lumbar spine flexed by 93.4° ± 17.5° and 51.6° ± 14.6°, respectively. There was a linear correlation between ∆LL and LLstanding (rho, 0.565; p < 0.001) and between ∆PFA and PFAstanding (rho, 0.491; p < 0.001) (Figs. 2 and 3), with an increase in ∆LL of 0.67° per degree of LLstanding and an increase in ∆PFA of 0.95° per degree of PFAstandin. The correlation between ∆LL and ∆PFA did not reach significance (rho, 0.173; p = 0.068).
Fig. 2.
The relationship between standing lumbar lordosis (LL) and the difference in LL between the standing and deep-seated positions (R2 = 0.299; rho, 0.565; p < 0.001).
Fig. 3.
The relationship between standing pelvic-femoral angle (PFA) and the difference in PFA (hip flexion) between the standing and deep-seated positions (R2 = 0.245; rho, 0.491; p < 0.001).
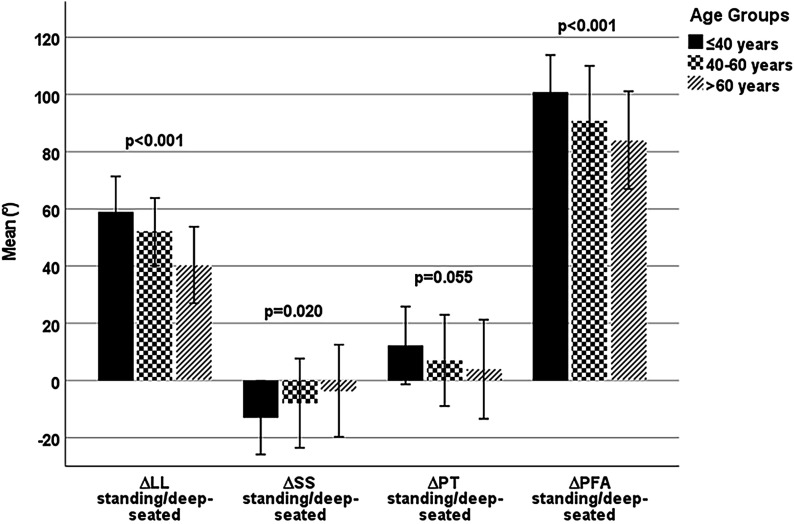
Age and Spinopelvic Characteristics
For all spinopelvic parameters, aging had a larger effect on the dynamic than on the static values in the standing and deep-seated positions (Fig. 4). There were linear decreases of 4.5° (9%) per decade of age in ∆LL (rho, −0.576; p < 0.001) and 3.6° (4%) per decade in ∆PFA (rho, −0.365; p < 0.001). Age did not affect standing SS (rho, 0.020; p = 0.834), standing PT (rho, 0.044; p = 0.645), or standing PI (rho, 0.049; p = 0.610) (Table III).
Fig. 4.
Mean decreases in spinopelvic parameters with age. The whiskers indicate the standard deviation. One-way ANOVA tests with post-hoc Bonferroni tests showed significant differences in the change in lumbar lordosis, ΔLL, in >60-year-olds versus <40-year-olds (p < 0.001) and 40 to 60-year-olds (p < 0.001); in the change in sacral slope, ΔSS, in >60-year-olds versus <40-year-olds (p = 0.018); and in the change in pelvic-femoral angle (ΔPFA) in >60-year-olds versus <40-year-olds (p < 0.001) and in 40 to 60-year-olds versus <40-year-olds (p = 0.022). PT = pelvic tilt.
TABLE III.
Spearman Correlation of Spinopelvic Parameters with Age and BMI
| Age | BMI | |||
|---|---|---|---|---|
| Rho | P Value | Rho | P Value | |
| LLstanding in degrees | −0.270 | 0.004* | −0.344 | 0.004* |
| LLdeep-seated in degrees | 0.408 | <0.001* | 0.016 | 0.895 |
| ∆LLstanding/deep-seated in degrees | −0.576 | <0.001* | −0.307 | 0.011* |
| SSstanding in degrees | 0.020 | 0.834 | −0.065 | 0.603 |
| SSdeep-seated in degrees | −0.212 | 0.025* | −0.194 | 0.115 |
| ∆SSstanding/deep-seated in degrees | 0.236 | 0.012* | 0.186 | 0.132 |
| PTstanding in degrees | 0.044 | 0.645 | 0.033 | 0.789 |
| PTdeep-seated in degrees | 0.227 | 0.016* | 0.194 | 0.116 |
| ∆PTstanding/deep-seated in degrees | −0.194 | 0.031* | −0.177 | 0.152 |
| PFAstanding in degrees | −0.275 | 0.003* | −0.093 | 0.455 |
| PFAdeep-seated in degrees | 0.250 | 0.008* | 0.288 | 0.018* |
| ∆PFAstanding/deep-seated in degrees | −0.365 | <0.001* | −0.253 | 0.039* |
| SFA in degrees | −0.587 | <0,001* | −0.359 | 0.003* |
| PIstanding in degrees | 0.049 | 0.610 | −0.058 | 0.641 |
| PI-LL mismatch in degrees | 0.275 | 0.003* | 0.318 | 0.009* |
| Hip user index in % | 0.173 | 0.068 | 0.083 | 0.505 |
Significant (p < 0.05).
There was a weak correlation between increasing PI-LL mismatch and age, by 2.0° per decade (p = 0.003) (rho, 0.275; p = 0.003). A flatback deformity (PI − LL: >10°) was found in 2 volunteers (4.1%) in the <40-year age group, 4 (12.5%) in the 40 to 60-year age group, and 5 (16.1%) in the >60-year age group (p = 0.111) (Table IV).
TABLE IV.
Spinopelvic Parameters by Age Group*
| <40 Yr (N = 49) | 40-60.0 Yr (N = 32) | >60 Yr (N = 31) | P Value | |
|---|---|---|---|---|
| LLstanding (deg) | 61.2 ± 11.3 | 60.3 ± 13.8 | 54.0 ± 9.7 | 0.022† |
| LLdeep-seated (deg) | 2.3 ± 10.7 | 8.3 ± 13.3 | 13.9 ± 12.6 | <0.001† |
| ∆LLstanding/deep-seated (deg) | 58.9 ± 12.5 | 52.0 ± 11.8 | 40.4 ± 13.4 | <0.001† |
| SSstanding (deg) | 38.8 ± 7.1 | 42.2 ± 9.9 | 39.0 ± 7.1 | 0.138 |
| SSdeep-seated (deg) | 51.8 ± 12.6 | 50.2 ± 20.3 | 42.5 ± 17.5 | 0.046† |
| ∆SSstanding/deep-seated (deg) | −13.0 ± 12.9 | −7.9 ± 15.6 | −3.6 ± 16.1 | 0.020† |
| PTstanding (deg) | 13.1 ± 8.2 | 15.1 ± 6.8 | 14.1 ± 8.6 | 0.540 |
| PTdeep-seated (deg) | 0.9 ± 14.4 | 8.1 ± 14.8 | 10.3 ± 18.2 | 0.021† |
| ∆PTstanding/deep-seated (deg) | 12.2 ± 13.6 | 7.0 ± 16.0 | 3.9 ± 17.3 | 0.055 |
| PFAstanding (deg) | 192.1 ± 7.2 | 188.9 ± 10.0 | 184.5 ± 9.3 | 0.001† |
| PFAdeep-seated (deg) | 91.2 ± 13.6 | 98.1 ± 15.1 | 100.7 ± 15.7 | 0.013† |
| ∆PFAstanding/deep-seated (deg) | 100.9 ± 12.9 | 90.9 ± 19.2 | 84.1 ± 17.1 | <0.001† |
| SFA (deg) | 159.8 ± 17.0 | 142.8 ± 21.0 | 124.4 ± 18.9 | <0.001† |
| PIstanding (deg) | 52.0 ± 10.7 | 57.4 ± 12.1 | 53.3 ± 11.4 | 0.106 |
| PI-LL mismatch (deg) | −9.1 ± 11.4 | −3.0 ± 10.7 | −0.7 ± 12.9 | 0.004† |
| Spinopelvic balance (no. [%]) | 0.111‡ | |||
| Hyperlordotic | 24 (49.0%) | 11 (34.4%) | 7 (22.6%) | |
| Normal | 23 (46.9%) | 17 (53.1%) | 19 (61.3%) | |
| Flatback | 2 (4.1%) | 4 (12.5%) | 5 (16.1%) | |
| Hip user index (%) | 63.9 ± 6.8 | 63.2 ± 8.5 | 68.0 ± 10.0 | 0.046† |
All parameters are given as the mean and standard deviation. P values for standing PT, standing PI, and spinopelvic balance were determined with a chi-square test, and the remaining p values were determined with 1-way ANOVA.
Significant (p < 0.05).
Chi-square test.
The hip user index was higher in the >60-year age group (68.0% ± 10.0%) than in the younger age groups (p = 0.046) (Table IV).
Volunteers who had a stiff spine (4 of 122; 3.3%) were on average older than those who did not (62.7 ± 21.3 versus 46.8 ± 17.4 years; p = 0.090).
Sex and Spinopelvic Characteristics
There were no differences in the standing spinopelvic parameters between males and females (Table V). There was no difference in lumbar flexion between sexes. However, there was a trend toward men having less hip flexion (90.3° ± 16.4° versus 96.4° ± 18.1°; p = 0.065) and a lower hip user index (62.9% ± 8.2% versus 66.7% ± 8.3%; p = 0.015).
TABLE V.
Spinopelvic Parameters by Sex
| Whole Cohort (N = 112) | Females (N = 56) | Males (N = 56) | P Value* | |
|---|---|---|---|---|
| LLstanding (deg) | 58.9 ± 12.0 | 58.7 ± 11.9 | 59.1 ± 12.2 | 0.874 |
| LLdeep-seated (deg) | 7.2 ± 12.9 | 8.4 ± 13.1 | 6.0 ± 12.7 | 0.331 |
| ∆LLstanding/deep-seated (deg) | 51.8 ± 14.6 | 50.5 ± 15.7 | 53.1 ± 13.4 | 0.356 |
| SSstanding (deg) | 39.8 ± 8.1 | 40.1 ± 7.7 | 39.6 ± 8.5 | 0.756 |
| SSdeep-seated (deg) | 48.7 ± 16.8 | 54.1 ± 16.2 | 43.4 ± 15.7 | <0.001† |
| ∆SSstanding/deep-seated (deg) | −8.9 ± 15.0 | −14.1 ± 14.6 | −3.7 ± 13.6 | <0.001† |
| PTstanding (deg) | 14.0 ± 7.9 | 13.7 ± 8.5 | 14.3 ± 7.3 | 0.690 |
| PTdeep-seated (deg) | 5.5 ± 16.1 | 0.6 ± 17.3 | 10.5 ± 13.2 | <0.001† |
| ∆PTstanding/deep-seated (deg) | 8.4 ± 15.6 | 13.2 ± 16.0 | 3.7 ± 13.9 | 0.001† |
| PFAstanding (deg) | 189.1 ± 9.1 | 188.3 ± 9.5 | 189.6 ± 8.7 | 0.374 |
| PFAdeep-seated (deg) | 95.8 ± 15.1 | 92.0 ± 16.7 | 99.6 ± 12.4 | 0.008† |
| ∆PFAstanding/deep-seated (deg) | 93.4 ± 17.5 | 96.4 ± 18.1 | 90.3 ± 16.4 | 0.065 |
| SFA (deg) | 145.2 ± 23.6 | 143.4 ± 22.6 | 146.9 ± 24.8 | 0.442 |
| PIstanding (deg) | 53.9 ± 11.4 | 53.9 ± 12.5 | 53.9 ± 10.4 | 0.999 |
| PI-LL mismatch (deg) | −5.0 ± 12.1 | −4.7 ± 13.4 | −5.3 ± 10.9 | 0.802 |
| Hip user index (%) | 64.8 ± 8.4 | 66.7 ± 8.3 | 62.9 ± 8.2 | 0.015† |
Independent-samples t test.
Significant (p < 0.05).
BMI and Spinopelvic Characteristics
BMI was moderately correlated with LLstanding (rho, −0.344; p = 0.004), ∆LL (rho, −0.307; p = 0.011), and PFAdeep-seated (rho, 0.288; p = 0.018), and weakly correlated with ∆PFA (rho −0.253; p = 0.039) (Table III).
Multivariate Regression Analysis
Multiple regression analysis adjusted for age and PI, LL, and PFA in the standing position (Table VI) could explain 56% of the variation (R2 = 0.559) in ∆LL and 39% of the variation (R2 = 0.385) in ∆PFA. This analysis demonstrated that a high ∆LL could be predicted by younger age, low standing PFA, and high standing LL; a high ∆PFA could be predicted by high standing PFA, high standing LL, and low standing PI.
TABLE VI.
Multiple Regression Analysis of Differences in Spinopelvic Characteristics Between the Standing and Deep-Seated Positions*
| Spinopelvic Motion and Significant Predictors | Unstandardized β Coefficient (95% CI) | Standardized β Coefficient | P Value | Collinearity Tolerance† |
|---|---|---|---|---|
| ∆LLstanding/deep-seated | ||||
| Age | −0.435 (−0.547 to −0.323) | −0.526 | <0.001 | 0.871 |
| LLstanding | 0.549 (0.390 to 0.708) | 0.450 | <0.001 | 0.946 |
| PFAstanding | −0.455 (−0.668 to −0.243) | −0.284 | <0.001 | 0.913 |
| ∆SSstanding/deep-seated | ||||
| PFAstanding | −0.562 (−0.855 to −0.270) | −0.342 | <0.001 | 1.000 |
| ∆PTstanding/deep-seated | ||||
| PFAstanding | 0.584 (0.280 to 0.88) | 0.341 | <0.001 | 1.000 |
| ∆PFAstanding/deep-seated | ||||
| PFAstanding | 1.387 (1.040 to 1.734) | 0.724 | <0.001 | 0.683 |
| PIstanding | −0.739 (−1.050 to −0.428) | −0.484 | <0.001 | 0.540 |
| LLstanding | 0.465 (0.213 to 0.717) | 0.319 | <0.001 | 0.750 |
Adjusted for age and PI, LL, and PFA in the standing position. The listed factors explained 55.9% of the variability in ∆LL (R2 = 0.559), 11.7% of the variability in ∆SS (R2 = 0.117), 11.6% of the variability in ∆PT (R2 = 0.116), and 38.5% of the variability in ∆PFA (R2 = 0.385) between the standing and deep-seated positions. CI = confidence interval.
Collinearity was considered to exist if the tolerance was <0.20.
Multiple regression analysis adjusted for age and PI, LL, and PFA in the standing position could explain 38% of the variation (R2 = 0.379) in the hip user index. A high hip user index could be predicted by older age, high standing PFA, and low standing LL.
Discussion
In this prospective, cross-sectional study, we aimed to define “normal” spinopelvic parameters in a cohort of asymptomatic, well-functioning volunteers, and to assess the influence of age, sex, and BMI. This is of relevance as surgeons aim to understand the hip-spine pathomechanics across the spectrum of hip pathology ranging from the young adult patient with hip impingement and/or dysplasia to the elderly patient with hip-spine syndrome requiring both spinal and hip surgery. Both static (LLstanding, PFAstanding, PI-LL mismatch) and dynamic (∆LL, ∆SS, ∆PT, ∆PFA) parameters changed with age, but only for ∆LL and ∆PFA was the impact of age large enough to predict “natural” evolution. Lumbar flexion (∆LL) decreased by 4.5°, equivalent to 9%, per decade of age. Hip flexion also decreased, but only by 3.6°, equivalent to 4%, per decade. This difference is likely to lead to a relatively greater hip user index with age, as was seen in the >60-year-old volunteers. Standing spinopelvic characteristics were similar between sexes. However, men exhibited stiffer hips, as evidenced by their lower hip user index. This is likely due to morphological differences between male and female hips, and highlights a potential difference in the required arc of movement between sexes during activities of daily living. BMI exhibited a weak to moderate correlation with the measured parameters; the higher the BMI, the smaller the amount of hip and lumbar flexion, and the smaller the standing LL. A higher BMI is associated with greater abdominal and thigh girths. This likely leads to soft-tissue impingement29, which in turn restricts flexion and prevents the hip from going to a position that is at risk for femoroacetabular impingement in a native hip or dislocation after THA.
Both static and dynamic parameters were found to change with age, even among well-functioning volunteers. It is of interest that the only static parameters that remained unchanged were PI, PT, and SS, which are all algebraically interlinked24. PT reflects sagittal balance, and it is thus unsurprising that in this well-functioning cohort, PT was the same among all age groups (approximately 14°), indicating appropriate sagittal balance and transfer of load. However, other static sagittal characteristics changed with age. There was a trend toward an increase in the PI-LL mismatch with age. A severe sagittal spinal deformity (PI-LL mismatch of >20°26), which has been associated with a higher risk of dislocation after THA27, was only present in some >60-year-old volunteers. Similarly, PFAstanding decreased with age, and the magnitude of that change between age groups was similar to the change in LLstanding (approximately 7°). This indicates that the reduction in LL is accompanied by an upright posture in which relatively greater hip flexion is needed to achieve a balanced position with acceptable PT (i.e., the greater hip flexion is a compensation mechanism).
The decrease in lumbar flexion (∆LL) with age can be explained by intervertebral disc and facet joint degeneration, which is associated with a reduction in lumbar curvature and range of motion13,30. Overall, ∆LL decreased by 4.5° per decade of age, which equates to approximately a 9% relative decrease in lumbar flexion per decade. Hip flexion likewise decreased with age, but only by 3.6° per decade, which equates to a relative reduction of only 4% per decade. This difference can lead to greater relative hip use with aging and might render the hip at risk for dislocation and adverse biomechanics. Increasing lumbar spinal stiffness during aging is a concern in patients treated with THA, as it can increase the risk of dislocation (for the same reason that patients with lumbar fusion have a higher risk of dislocation)1,2,30.
There was a weak correlation between hip flexion (∆PFA) and lumbar flexion (∆LL) (rho, 0.079). These findings indicate that flexion of the hip and flexion of the lumbar spine are, for the most part, independently regulated on the basis of the local anatomy and characteristics. Further study is required to identify the factors that primarily govern these movements. Because of the physiological loss of lordosis during aging, the relationship between LL and PI also appears to be dependent on age13. Results from the multiple regression analysis showed that 56% of the variation in ∆LL was explained by aging, LLstanding, and PFAstanding. Based on our results, although spinopelvic balance as measured by the PI-LL mismatch was significantly correlated with ∆LL, PI alone was not sufficient to explain the variation in ∆LL.
There were no differences in static standing spinal characteristics between sexes, which is in contrast to previous studies based on clinical or only static radiographic assessments13,14,17. We identified a lower hip user index in men, indicating that the hip contributes relatively less to sagittal movement in males than in females. Men tend to have a smaller femoral head-neck offset and smaller combined (acetabular and femoral) version31-33, which can lead to femoroacetabular impingement in the deep-seated position. To compensate for this, men tilt their pelvs more posteriorly in the deep-seated position (as reflected by lower SS and higher PT), and thereby effectively increased their acetabular version to allow for greater impingement-free hip flexion4.
BMI exhibited a weak to moderate correlation with the measured parameters. Higher BMI was associated with reduced hip and lumbar flexion, but that is most likely the secondary consequence of soft-tissue impingement between the thigh and abdomen29 and is unlikely to result in intra-articular impingement or directly contribute to instability after hip arthroplasty.
This study has some limitations. First, we selected patients based on the absence of hip and back pain. However, the absence of symptoms, including a history of pain, does not necessarily indicate that the volunteers had a “normal” spine and hips. The study volunteers might have had features of joint degeneration or pathology (of the hip or spine) without the presence of symptoms. Second, some patients might have had radiographic signs of hip instability or impingement, possibly altering spinopelvic motion to compensate for this instability or impingement4,7. However, the cross-sectional nature of the study would minimize this effect, as the scope of the study was to describe how spinopelvic measurements change with age, sex, and BMI in the overall (asymptomatic) population. Whether and how spinopelvic characteristics are influenced by hip morphology is a matter for future study. Third, the only detailed imaging that was available was the radiographs, which did not include the whole spine. Abnormalities higher in the spine might have existed and influenced lumbar and spinopelvic characteristics, and some patients might have had early degenerative changes of the cartilage or intervertebral discs. Fourth, we examined a wide range of ages (23 to 87 years) to study the natural evolution of the skeleton without hip or spinal pathology. This study does not provide sufficient data to determine what changes might take place in the symptomatic aging spine and hip, particularly among patients >60 years old, who may have a faster rate of degenerative change and should be a cohort for further study. Longitudinal follow-up of the same cohort would allow us to determine which volunteers become symptomatic in time. Finally, it is conceivable that the observed change in LL could be generational, although we consider the possibility that such anatomical changes have taken place across the span of 60 years to be very small.
Conclusions
Spinopelvic characteristics were found to be age, sex, and BMI-dependent. Changes in LL between standing and deep-seated positions were influenced by age, standing LL, and standing PFA. During aging, the lumbar spine lost its flexion to a greater extent than the hip, and consequently, the relative contribution of the hip to overall sagittal movement increased. No differences in standing spinal characteristics were found between sexes. However, men had less hip flexion and thus required greater tilting of the pelvis to accommodate a deeply flexed position. BMI had a weak to moderate correlation with spinopelvic characteristics; higher BMI was associated with less hip and lumbar flexion.
Appendix
Supporting material provided by the authors is posted with the online version of this article as a data supplement at jbjs.org (http://links.lww.com/JBJSOA/A399).
Footnotes
Investigation performed at The Ottawa Hospital, Ottawa, Ontario, Canada
Disclosure: The Disclosure of Potential Conflicts of Interest forms are provided with the online version of the article (http://links.lww.com/JBJSOA/A401).
References
- 1.Esposito CI, Carroll KM, Sculco PK, Padgett DE, Jerabek SA, Mayman DJ. Total Hip Arthroplasty Patients With Fixed Spinopelvic Alignment Are at Higher Risk of Hip Dislocation. J Arthroplasty. 2018. May;33(5):1449-54. [DOI] [PubMed] [Google Scholar]
- 2.Grammatopoulos G, Gofton W, Jibri Z, Coyle M, Dobransky J, Kreviazuk C, Kim PR, Beaulé PE. 2018 Frank Stinchfield Award: Spinopelvic Hypermobility Is Associated With an Inferior Outcome After THA: Examining the Effect of Spinal Arthrodesis. Clin Orthop Relat Res. 2019. Feb;477(2):310-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Heckmann N, McKnight B, Stefl M, Trasolini NA, Ike H, Dorr LD. Late Dislocation Following Total Hip Arthroplasty: Spinopelvic Imbalance as a Causative Factor. J Bone Joint Surg Am. 2018. Nov 7;100(21):1845-53. [DOI] [PubMed] [Google Scholar]
- 4.Grammatopoulos G, Speirs AD, Ng KCG, Riviere C, Rakhra KS, Lamontagne M, Beaule PE. Acetabular and spino-pelvic morphologies are different in subjects with symptomatic cam femoro-acetabular impingement. J Orthop Res. 2018. Jul;36(7):1840-8. [DOI] [PubMed] [Google Scholar]
- 5.Ranawat CS, Ranawat AS, Lipman JD, White PB, Meftah M. Effect of Spinal Deformity on Pelvic Orientation from Standing to Sitting Position. J Arthroplasty. 2016. Jun;31(6):1222-7. [DOI] [PubMed] [Google Scholar]
- 6.Rivière C, Lazennec JY, Van Der Straeten C, Auvinet E, Cobb J, Muirhead-Allwood S. The influence of spine-hip relations on total hip replacement: A systematic review. Orthop Traumatol Surg Res. 2017. Jun;103(4):559-68. [DOI] [PubMed] [Google Scholar]
- 7.Okuzu Y, Goto K, Okutani Y, Kuroda Y, Kawai T, Matsuda S. Hip-Spine Syndrome: Acetabular Anteversion Angle Is Associated with Anterior Pelvic Tilt and Lumbar Hyperlordosis in Patients with Acetabular Dysplasia: A Retrospective Study. JB JS Open Access. 2019. Jan 29;4(1):e0025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Grammatopoulos G, Salih S, Beaulé PE, Witt J. Spinopelvic Characteristics in Acetabular Retroversion: Does Pelvic Tilt Change After Periacetabular Osteotomy? Am J Sports Med. 2020. Jan;48(1):181-7. [DOI] [PubMed] [Google Scholar]
- 9.Sadhu A, Nam D, Coobs BR, Barrack TN, Nunley RM, Barrack RL. Acetabular Component Position and the Risk of Dislocation Following Primary and Revision Total Hip Arthroplasty: A Matched Cohort Analysis. J Arthroplasty. 2017. Mar;32(3):987-91. [DOI] [PubMed] [Google Scholar]
- 10.Grammatopoulos G, Thomas GE, Pandit H, Beard DJ, Gill HS, Murray DW. The effect of orientation of the acetabular component on outcome following total hip arthroplasty with small diameter hard-on-soft bearings. Bone Joint J. 2015. Feb;97-B(2):164-72. [DOI] [PubMed] [Google Scholar]
- 11.Innmann MM, Merle C, Gotterbarm T, Ewerbeck V, Beaulé PE, Grammatopoulos G. Can spinopelvic mobility be predicted in patients awaiting total hip arthroplasty? A prospective, diagnostic study of patients with end-stage hip osteoarthritis. Bone Joint J. 2019. Aug;101-B(8):902-9. [DOI] [PubMed] [Google Scholar]
- 12.Innmann MM, Reichel F, Schaper B, Merle C, Beaulé PE, Grammatopoulos G. How Does Spinopelvic Mobility and Sagittal Functional Cup Orientation Affect Patient-Reported Outcome 1 Year after THA?-A Prospective Diagnostic Cohort Study. J Arthroplasty. 2021. Jul;36(7):2335-42. [DOI] [PubMed] [Google Scholar]
- 13.Dreischarf M, Albiol L, Rohlmann A, Pries E, Bashkuev M, Zander T, Duda G, Druschel C, Strube P, Putzier M, Schmidt H. Age-related loss of lumbar spinal lordosis and mobility—a study of 323 asymptomatic volunteers. PLoS One. 2014. Dec 30;9(12):e116186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Arshad R, Pan F, Reitmaier S, Schmidt H. Effect of age and sex on lumbar lordosis and the range of motion. A systematic review and meta-analysis. J Biomech. 2019. Jan 3;82:1-19. [DOI] [PubMed] [Google Scholar]
- 15.Stathokostas L, McDonald MW, Little RM, Paterson DH. Flexibility of older adults aged 55-86 years and the influence of physical activity. J Aging Res. 2013;2013:743843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Svenningsen S, Terjesen T, Auflem M, Berg V. Hip motion related to age and sex. Acta Orthop Scand. 1989. Feb;60(1):97-100. [DOI] [PubMed] [Google Scholar]
- 17.Medeiros HB, de Araújo DS, de Araújo CG. Age-related mobility loss is joint-specific: an analysis from 6,000 Flexitest results. Age (Dordr). 2013. Dec;35(6):2399-407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Esposito CI, Miller TT, Kim HJ, Barlow BT, Wright TM, Padgett DE, Jerabek SA, Mayman DJ. Does Degenerative Lumbar Spine Disease Influence Femoroacetabular Flexion in Patients Undergoing Total Hip Arthroplasty? Clin Orthop Relat Res. 2016. Aug;474(8):1788-97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Innmann MM, Merle C, Phan P, Beaulé PE, Grammatopoulos G. Differences in Spinopelvic Characteristics Between Hip Osteoarthritis Patients and Controls. J Arthroplasty. 2021. Aug;36(8):2808-16. [DOI] [PubMed] [Google Scholar]
- 20.Stefl M, Lundergan W, Heckmann N, McKnight B, Ike H, Murgai R, Dorr LD. Spinopelvic mobility and acetabular component position for total hip arthroplasty. Bone Joint J. 2017. Jan;99-B(1)(Supple A):37-45. [DOI] [PubMed] [Google Scholar]
- 21.Ganz R, Leunig M, Leunig-Ganz K, Harris WH. The etiology of osteoarthritis of the hip: an integrated mechanical concept. Clin Orthop Relat Res. 2008. Feb;466(2):264-72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Pierrepont J, Hawdon G, Miles BP, Connor BO, Baré J, Walter LR, Marel E, Solomon M, McMahon S, Shimmin AJ. Variation in functional pelvic tilt in patients undergoing total hip arthroplasty. Bone Joint J. 2017. Feb;99-B(2):184-91. [DOI] [PubMed] [Google Scholar]
- 23.Innmann MM, Merle C, Phan P, Beaulé PE, Grammatopoulos G. How Can Patients With Mobile Hips and Stiff Lumbar Spines Be Identified Prior to Total Hip Arthroplasty? A Prospective, Diagnostic Cohort Study. J Arthroplasty. 2020. Jun;35(6S):S255-61. [DOI] [PubMed] [Google Scholar]
- 24.Legaye J, Duval-Beaupère G, Hecquet J, Marty C. Pelvic incidence: a fundamental pelvic parameter for three-dimensional regulation of spinal sagittal curves. Eur Spine J. 1998;7(2):99-103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Schwab FJ, Blondel B, Bess S, Hostin R, Shaffrey CI, Smith JS, Boachie-Adjei O, Burton DC, Akbarnia BA, Mundis GM, Ames CP, Kebaish K, Hart RA, Farcy JP, Lafage V; International Spine Study Group (ISSG). Radiographical spinopelvic parameters and disability in the setting of adult spinal deformity: a prospective multicenter analysis. Spine (Phila Pa 1976). 2013. Jun 1;38(13):E803-12. [DOI] [PubMed] [Google Scholar]
- 26.Vigdorchik JM, Sharma AK, Buckland AJ, Elbuluk AM, Eftekhary N, Mayman DJ, Carroll KM, Jerabek SA. 2021 Otto Aufranc Award: A simple Hip-Spine Classification for total hip arthroplasty : validation and a large multicentre series. Bone Joint J. 2021. Jul;103-B(7)(Supple B):17-24. [DOI] [PubMed] [Google Scholar]
- 27.DelSole EM, Vigdorchik JM, Schwarzkopf R, Errico TJ, Buckland AJ. Total Hip Arthroplasty in the Spinal Deformity Population: Does Degree of Sagittal Deformity Affect Rates of Safe Zone Placement, Instability, or Revision? J Arthroplasty. 2017. Jun;32(6):1910-7. [DOI] [PubMed] [Google Scholar]
- 28.Langston J, Pierrepont J, Gu Y, Shimmin A. Risk factors for increased sagittal pelvic motion causing unfavourable orientation of the acetabular component in patients undergoing total hip arthroplasty. Bone Joint J. 2018. Jul;100-B(7):845-52. [DOI] [PubMed] [Google Scholar]
- 29.Yeung E, Jackson M, Sexton S, Walter W, Zicat B, Walter W. The effect of obesity on the outcome of hip and knee arthroplasty. Int Orthop. 2011. Jun;35(6):929-34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Wiznia DH, Buchalter DB, Kirby DJ, Buckland AJ, Long WJ, Schwarzkopf R. Applying the hip-spine relationship in total hip arthroplasty. Hip Int. 2021. Mar;31(2):144-53. [DOI] [PubMed] [Google Scholar]
- 31.Gosvig KK, Jacobsen S, Sonne-Holm S, Gebuhr P. The prevalence of cam-type deformity of the hip joint: a survey of 4151 subjects of the Copenhagen Osteoarthritis Study. Acta Radiol. 2008. May;49(4):436-41. [DOI] [PubMed] [Google Scholar]
- 32.Hack K, Di Primio G, Rakhra K, Beaulé PE. Prevalence of cam-type femoroacetabular impingement morphology in asymptomatic volunteers. J Bone Joint Surg Am. 2010. Oct 20;92(14):2436-44. [DOI] [PubMed] [Google Scholar]
- 33.Leunig M, Jüni P, Werlen S, Limacher A, Nüesch E, Pfirrmann CW, Trelle S, Odermatt A, Hofstetter W, Ganz R, Reichenbach S. Prevalence of cam and pincer-type deformities on hip MRI in an asymptomatic young Swiss female population: a cross-sectional study. Osteoarthritis Cartilage. 2013. Apr;21(4):544-50. [DOI] [PubMed] [Google Scholar]