Abstract
BACKGROUND:
Six multidisciplinary cancer centers were selected and funded by the Merck Foundation (2017–2021) to collaborate in the Alliance to Advance Patient-Centered Cancer Care (“Alliance”), an initiative to improve patient access, minimize health disparities, and enhance the quality of patient-centered cancer care. These sites share their insights on implementation and expansion of their patient navigation efforts.
METHODS:
Patient navigation represents an evidence-based health care intervention designed to enhance patient-centered care and care coordination. Investigators at 6 National Cancer Institute-designated cancer centers outline their approaches to reducing health care disparities and synthesize their efforts to ensure sustainability and successful transferability in the management of patients with cancer and their families in real-world health care settings.
RESULTS:
Insights are outlined within the context of patient navigation program effectiveness and supported by examples from Alliance cancer center sites: 1) understand the patient populations, particularly underserved and high-risk patients; 2) capitalize on the existing infrastructure and institutional commitment to support and sustain patient navigation; and 3) build capacity by mobilizing community support outside of the cancer center.
CONCLUSIONS:
This process-level article reflects the importance of collaboration and the usefulness of partnering with other cancer centers to share inter-disciplinary insights while undergoing intervention development, implementation, and expansion. These collective insights may be useful to staff at other cancer centers that look to implement, enhance, or evaluate the effectiveness of their patient navigation interventions.
Keywords: cancer control continuum, cancer health disparities, implementation, patient navigation, sustainability
INTRODUCTION
Addressing cancer from a biopsychosocial perspective requires treating the biological disease and addressing the psychosocial impact of cancer on patients and families.1,2 It also requires recognition of the substantial economic burden experienced by patients and society3,4 and the devastating consequences of health disparities.5,6 The American Cancer Society’s landmark publication, Report to the Nation on Cancer in the Poor,7 identified cancer health disparities as an unmet need and contended that cancer cannot be reduced to a “one-size-fits-all” experience. Cancer health disparities are impacted by race, ethnicity, socioeconomic status, geographical location, primary language, culture, and health insurance status.8–10 Patients with cancer who experience social, environmental, and/or economic disadvantages are considered “underserved” because they often endure a greater cancer care burden compared to other groups.5,11 For example, the delivery of cancer care for underserved patients is often fragmented, including coordination challenges and treatment barriers.12,13 Accordingly, efforts to address whole-person cancer care delivery, especially for underserved patients, must be prioritized.
High quality patient-centered cancer care requires coordination between primary and specialty care, effective patient-provider communication, reduction in barriers to care, and engagement of patients in their own treatment decisions. Patient navigation programs reflect the capacities of the cancer center and the needs of their communities. This article outlines 3 shared insights and “lessons learned” from the Alliance to Advance Patient-Centered Cancer Care (“Alliance”), a partnership of sites funded by the Merck Foundation focused on reducing disparities in cancer care: 1) know the patient populations represented within the catchment area, with particular focus on the needs of underserved and high-risk patients; 2) use the existing infrastructure and institutional commitment available to support and sustain the program; and 3) build capacity to mobilize community support outside the cancer center.
Originally developed as a community-focused effort to improve patients’ timeliness to diagnostic resolution and cancer treatment initiation,14 patient navigation programs no longer subscribe to a one-size-fits-all model.15 Some programs focus on a single segment of the cancer care continuum (eg, screening for early detection),16 whereas others address screening, diagnosis, treatment initiation, survivorship, community outreach, and end-of-life-care.17 Programs may be conducted by nurse navigators, community-focused navigators (ie, lay), or some combination or hybrid models,18,19 and the educational and skill levels, methods of training, and tasks assigned to patient navigators vary considerably (Table 1). Programs may also have access to disparate levels of infrastructural support,20 technology assistance,21 and funding,22 lacking standardization in design and function.19
TABLE 1.
Patient Navigation Efforts Throughout the Cancer Care Continuum
| Cancer Care Continuum | Patient Navigation and Tasks |
|---|---|
| Outreach | Navigators use knowledge of the communities in their catchment area to increase awareness of cancer prevention and early detection. Tasks may include:
|
| Screening | Navigators work to increase uptake of cancer screening. Tasks may include:
|
| Diagnosis | Navigators follow-up on suspicious screening results and improve timeliness to diagnostic resolution. Tasks may include:
|
| Treatment | Navigators assist patients as they initiate and adhere to treatment. Tasks may include:
|
| Survivorship | Navigators help individuals adjust to post-treatment cancer survivorship. Tasks may include:
|
| Palliative | Navigators assist individuals who are transitioning to palliative/hospice care. Tasks may include:
|
MATERIALS AND METHODS
The Alliance is committed to improving cancer care access and reducing cancer health disparities. In 2017, grants were awarded to the following 6 National Cancer Institute (NCI)-designated cancer centers: Georgia Cancer Center for Excellence at Grady Health System (GCCE) (Atlanta, GA), the Johns Hopkins University Sidney Kimmel Comprehensive Cancer Center-Center to Reduce Cancer Disparities (SKCCC-CRCD) (Baltimore, MD), Massachusetts General Hospital Cancer Center (MGH) (Boston, MA), Northwestern University Feinberg School of Medicine (NU) (Chicago, IL), the Ohio State University Comprehensive Cancer Center (OSUCCC) (Columbus, OH), and the University of Arizona Cancer Center (UACC) (Tucson, AZ) (Fig. 1). University of Michigan’s School of Nursing (Ann Arbor, MI) serves as the coordinating site (National Program Office [NPO]). This Alliance presents its first collaborative publication on the implementation, expansion, and re-design of their patient navigation programs.
Figure 1.
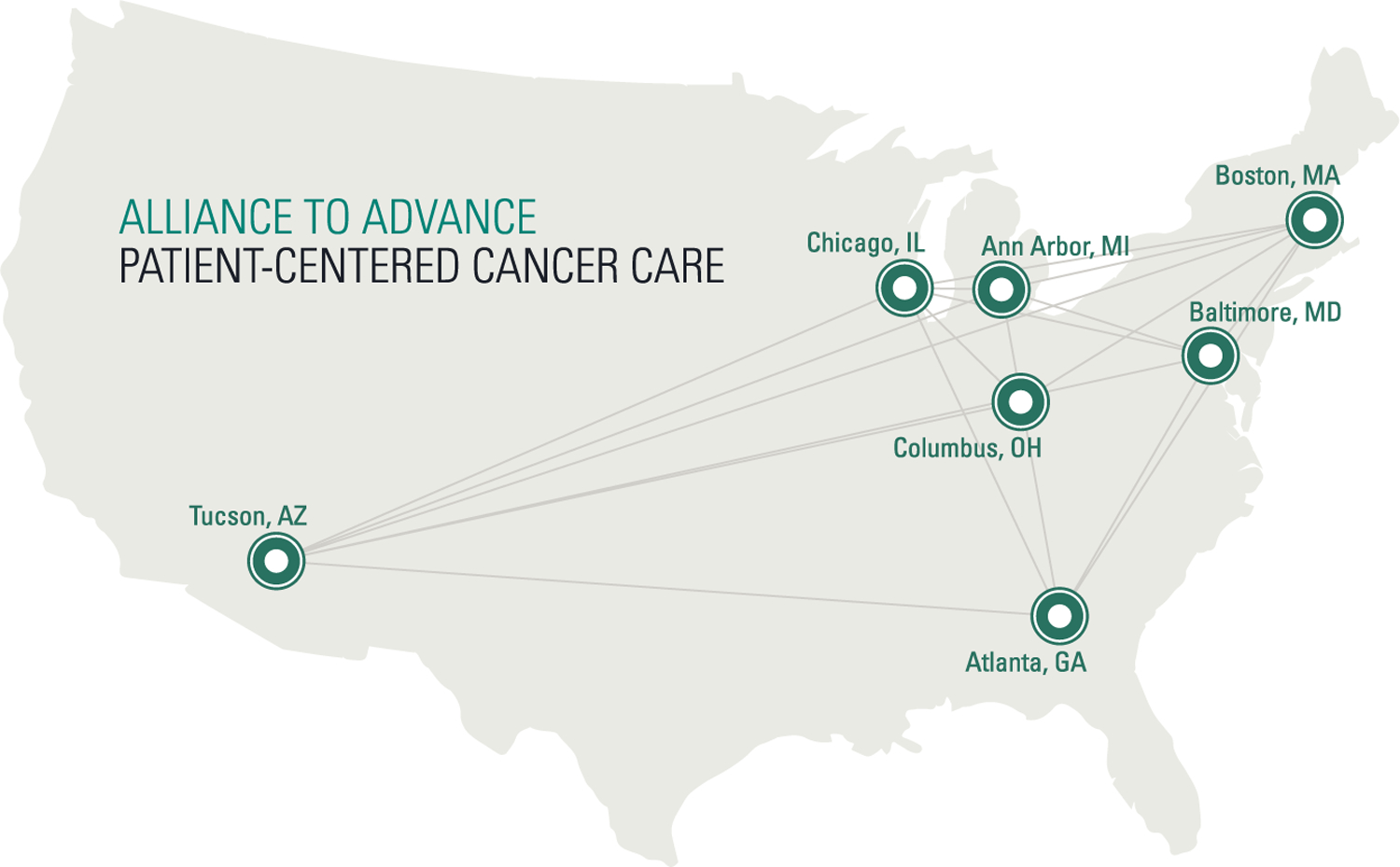
Map of Alliance to Advance Patient-Centered Cancer Care sites.
Throughout the project period, Alliance sites shared common aims of improving high quality cancer care through patient navigation, while applying methods and approaches most suited to each site’s self-identified catchment area. All program sites implemented evidence-based components of patient navigation, although the modality of care and intervention duration differed based on community needs and considerations. Outcome metrics included both shared assessments (eg, patient-reported quality of life; patient use of emergency care) and site-specific outcomes. This framework allowed connections and information-sharing across sites while also respecting the unique aspects of each cancer care and local setting. The Alliance infrastructure, including staff associated with the NPO, provided structure for regular consultation between investigators, their community partners, and other stakeholders. The comprehensive and multimodal process included semi-annual cross-site investigator meetings, regular webinars on effective patient navigation program implementation, and reviews of each site’s patient navigation intervention sustainability as evaluated through bi-annual systematic quantitative and qualitative data collection. Core elements of quantitative data collection included participant numbers and characteristics (including an assessment of representativeness of the target population), along with interim outcomes. Qualitative assessments focused on perceptions of the program among interventionists, clinical staff, community partners, and other involved stakeholders (eg, patients, cancer care administrators, and policy experts). These structured efforts, as well as less formal site collaborations, provided opportunities to enhance the “connective tissue” across sites while allowing local-level responsiveness to community and catchment needs.
The process of program evaluation was guided by the implementation science framework, RE-AIM.23 Specifically, RE-AIM was used in gathering enrollment, retention, and patient-reported outcomes data every 6 months over the past 4 years, allowing the sites to consistently track specific metrics of “Reach”(proportion of underserved patients using the intervention), “Effectiveness” (ability to demonstrate pre- and post-intervention changes in patient-reported outcomes such as quality of life and satisfaction), “Adoption” (referral patterns), “Implementation”(consistent utilization of the intervention included time between referral and first contact with patient navigator), and “Maintenance” (process toward intervention sustainability). The 3 insights were developed over a period of several years in consultation with all site investigators and validated by site members during the process of manuscript construction. Information was gathered by the manuscript’s primary authors (E.S.V.H. and H.A.H.) and further consolidated by staff at the Alliance coordinating site. An iterative and collaborative process further refined the overall themes. Specific examples were produced in collaboration with site-specific personnel, including input from patient navigators and on-site administrators. Although comprehensive assessments of effectiveness using the RE-AIM framework are ongoing, interim analyses, including published work from the sites,24–28 have demonstrated key benefits that support the 3 insights outlined in this article.
The interventions developed by the 6 Alliance NCI-designated cancer centers targeted education and outreach, cancer screening, diagnosis and staging, cancer treatment, survivorship, and end-of-life care (Table 2); sought improvements in the timeliness of treatment initiation for patients with different types of cancer, reductions in barriers to seeking care, psychosocial support, survivorship care, community outreach, and cancer prevention; and encompassed differing populations of underserved patients, levels of infrastructural support, technological assistance, and availability of resources within their communities. Sites enhanced their patient navigation programs in various ways (eg, lay navigator, technology, nurse navigators into other disease teams, community partnerships and referral processes etc.), but all programs used intervention expansion and have been enrolling and systematically tracking patients in their patient navigation interventions at 6-month intervals from 2017 through 2021.
TABLE 2.
Patient Navigator Programs at Each of the Centers
| Alliance to Advance Patient-Centered Cancer Care | Outreach | Screening | Diagnosis | Treatment | Survivorship | Palliative |
|---|---|---|---|---|---|---|
Georgia Cancer Center for Excellence at Grady Health System (GCCE)
|
X | X | ||||
Johns Hopkins University Sidney Kimmel Comprehensive Cancer Center-Center to Reduce Cancer Disparities (SKCCC-CRCD)
|
X | X | X | X | X | |
University of Arizona Cancer Center (UACC)
|
X | X | X | X | ||
Massachusetts General Hospital Cancer Center (MGH)
|
X | X | ||||
The Ohio State University Comprehensive Cancer Center (OSUCC)
|
X | X | ||||
Northwestern University Feinberg School of Medicine (NU)
|
X | X | X |
RESULTS
Program Highlights
Improving cancer care coordination as a means of enhancing patient care outcomes represents the primary, unifying aim of the Alliance. This section highlights the designs of our patient navigation programs, with examples to illustrate shared insights (See Table 3).
TABLE 3.
Three Insights for Patient Navigation Intervention Implementation
| Insight | Relevance | Action Steps |
|---|---|---|
| (1) Know patient populations represented within the catchment area | Identifying medically underserved patients allows for more targeted patient navigation efforts and increases likelihood of reducing cancer health disparities |
|
| (2) Use existing infrastructure and institutional commitment | Understanding the existing infrastructure and health care setting characteristics before intervention implementation may lead to greater acceptability and utilization of patient navigation intervention |
|
| (3) Build capacity to mobilize community support | Fostering strong community support within and outside of a cancer center will support long-term program sustainability |
|
University of Arizona Cancer Center (UACC) supports a program with nurse navigators assigned to each disease-oriented team. The program was expanded to include a lay community-focused navigator, housed at the cancer center, to improve care coordination and support patients, particularly underserved patients at cancer diagnosis, treatment, and survivorship. The UACC catchment area includes a 5-county region of Southern Arizona; 29% to 83% of each county’s population identifies as Hispanic/Latino. Southern Arizona consists of low socioeconomic status29 rural and frontier areas with the exception of 1 urban center.30 Accordingly, the underserved patients served at UACC include Hispanic/Latino, low income, rural, and older adult patients.31,32 The navigation program was enhanced with the inclusion of a bilingual, bicultural navigator who became fully integrated into the clinical oncology setting, allowing for utilization of community resources and enhanced coordination among clinical teams. The navigator receives referrals from 1 of the UACC clinical teams, completes a “barriers to cancer care” assessment, and uses community resources and clinical advocacy to work with each patient over a 3-month period to address each barrier. The navigator has successfully reached underserved populations and documented significant decreases in patient-reported barriers to care and increases in community awareness and resource support across UACC and its community partners.24–26
The Ohio State University Comprehensive Cancer Center (OSUCC) expanded their preexisting patient navigation program by introducing a technology-focused symptom and needs monitoring program to connect patients with lay navigators who were already providing language-based and culturally based services to patients through the Center for Cancer Health Equity. The catchment area of OSUCCC is the entire state of Ohio, which contains large metropolitan areas as well as an expansive rural population, including Appalachian counties with high poverty rates. The OSUCCC is centrally located within the state; patients drive between 30 minutes and 3 hours to the medical center. Within the context of OSUCCC and Ohio, underserved patients include predominantly rural and lower socioeconomic status individuals.33 Patients participate in a voluntary, monthly survey via text messages or telephone calls from a study coordinator. Concerns related to symptoms or treatment are forwarded to clinical health care teams, and concerns related to nonclinical needs (eg, transportation, difficulty paying for utilities, or finding supportive services) are addressed by the lay navigator. This use of technology provides an efficient way to address patients’ needs outside of clinic and gives patients “permission” to report symptoms or concerns they were hesitant to mention in clinic.27,34 Needing neither the navigator nor the patient physically in clinic was particularly useful during the Coronavirus disease (COVID-19) pandemic.
The Johns Hopkins University Sidney Kimmel Comprehensive Cancer Center-Center to Reduce Cancer Disparities (SKCCC-CRCD) enhanced their preexisting patient navigation program by developing innovative technology within the electronic medical records system to pro-actively identify recently diagnosed underserved patients and automate their care coordination across specialty and primary care transitions. This frees providers and navigators to provide quality care for the served population. The SKCCC treats patients from every county of Maryland, including the urban region of Baltimore. Within the context of SKCCC-CRCD and the Baltimore area, underserved patients include predominantly lower socioeconomic and African American/Black individuals. The patient navigation team worked to establish a new branch of their Community Advisory Groups aimed at informing patients and families of existing resources, conducting program evaluation of the cancer survivorship clinic, and reviewing and integrating navigation activities across the system. Prior Community Advisory Group activities were expanded to the Eastern Shore of Maryland (Somerset, Wicomico, and Worchester counties) in collaboration with TidalHealth Peninsula Regional Medical Center in 2021. Navigators refer patients to video training resources designed to build communication skills, enhance discussions surrounding treatment options/side effects, identify treatment challenges and obstacles, and support shared decision-making. The Epic electronic health record module designed to support lung cancer survivors’ access to services has been expanded to survivors of breast cancer with plans to include colon and prostate cancers.
Georgia Cancer Center for Excellence at Grady Health System (GCCE) expanded their preexisting patient navigation program by expanding their nurse patient navigation to include navigation support for additional disease sites including breast and lung cancer. The GCCE serves a primarily Black/African American population (approximately 80%), and approximately one-third of the patient population is uninsured. The navigation team bridged the gap between cancer diagnosis and timely initiation of treatment by targeting patients with a new cancer diagnosis, improving treatment start times, eliminating barriers to treatment initiation, promoting adherence, and enhancing patient-provider communication and patient self-efficacy. Outcomes were achieved by developing and implementing a protocol that quickly linked newly diagnosed patients with nurse navigators, who provide timely communication and coordination with patients to reduce time to start of treatment. The team also enhanced transportation resources for patients at high risk of missing appointments and referred eligible patients to needed resources such as a physical activity coach or a registered dietician. Efforts from the GCCE’s nurse navigation team have led to reduction in time from diagnosis to treatment initiation for patients in GCCE’s breast, gynecology (GYN), and lung cancer clinics.35,36 Within the context of GCCE and the Atlanta area, underserved patients include uninsured and underinsured, lower socioeconomic status, and African American/Black individuals.
Massachusetts General Hospital Cancer Center (MGH) enhanced their preexisting patient navigation program by expanding its lay navigation program to include more direct connections and coordination between oncology and primary care. The MGH Cancer Center includes a number of community locations, serving a large portion of New England. The navigation team developed a comprehensive and searchable electronic registry of patients seen in primary care at MGH Community Health Centers, clinics that serve many low-income residents, immigrants with limited English proficiency, and refugees. Systematic identification allowed them to support their underserved patients as they transitioned from primary to oncology care. Within the context of MGH and the Boston area, underserved patients include patients with cancer and serious mental illness, lower socioeconomic status individuals, and individuals for whom English is not their primary language.37 Building on strong community health care partnerships, MGH recruited physician champions from each community health center (CHC), allowing the navigation team to identify underserved patients early, improve patient access to timely cancer care, and increase adherence to cancer treatment.28 The MGH Cancer Center also hired bi-cultural and multi-lingual lay navigators to ensure culturally sensitive cancer navigation support. The navigation program uses technology and community partnerships to support improved diagnostic resolution and cancer treatment initiation and adherence for underserved community patients.
Northwestern University Feinberg School of Medicine (NU) enhanced their preexisting patient navigation services by partnering with federally qualified health centers (FQHCs) and using core tenants of patient navigation to promote patient-provider communication and patient referrals and to connect patients with a recent cancer diagnosis with survivorship services and specialist partners. Within the context of NU and the Chicago area, underserved patients include Latino, African American, lesbian, gay, bisexual, transgender, queer, homeless, and immigrant and refugee populations that are receiving primary care services from FQHCs in the greater Chicago area. Patient navigation teams were comprised of Care Coordinators who were already established members of the care team, and had experience assisting patients with scheduling appointments, obtaining cancer screenings, navigating insurance barriers, and accessing other resources. The program leveraged its relationships with health centers to expand on Care Coordinators’ existing duties and establish relationships with patients and clinical teams to address unmet needs of symptom management during cancer treatment. Using established care team members is critical to creating the foundation for sustainability within community-based health centers.
Insights for Effective Patient Navigation Programs
Become informed about the patient populations represented within the cancer center’s catchment area and understand the unique needs of underserved and high-risk patients
A foundational aspect of successful patient navigation is the intention to support medically underserved patients and mitigate cancer health disparities.38 NCI-designated cancer centers must understand the patient populations represented within their catchment areas in terms of demographics (race, ethnicity, primary language, etc), cancer incidence and mortality rates, economic burdens (socioeconomic status, health insurance status, etc), and health inequities (unequal allocation of resources, disability status, immigration status, etc).39,40 Recommended actions include identifying specific needs within the community and shaping the patient navigation program to address these patient populations. Articulating how navigation programs reduce inequities in access to quality care will be critical when requesting sustained resources to keep the programs strong.
Stakeholder feedback represents a critical technique for understanding the needs of a cancer center’s underserved and high-risk patient population. Considered part of best practices,41 stakeholder engagement strengthens intervention development, impact, and sustainability.42 Stakeholders may include medical professionals, patient financial advisors, CHCs, and patients themselves.43 Through structured feedback sessions, patient navigation programs can be evaluated by those most connected to the pressing unmet needs of individuals within that setting. Use of stakeholder and community engagement can positively impact patient and staff uptake of the intervention and increase long-term sustainability of the program.44 In the RE-AIM framework, “Reach” is defined as the proportion of individuals participating in an intervention that actually represent the population the intervention was designed to target.45 Documentation of a strong “Reach” increases the likelihood that an implemented patient navigation program is actually serving those patients most in need of support.
Example: University of Arizona Cancer Center
Researchers at the University of Arizona implemented an action research approach46 with 3 components. First, community health professionals and underserved cancer survivors participated in a process of stakeholder engagement to understand the unmet needs of patients in Southern Arizona. Specifically, a formal needs assessment was conducted before initiation of the community-focused patient navigation program.47 Barriers to cancer care were identified, including gaps in communication between oncology and primary care providers, lack of clarity in recommendations for survivorship care, and gaps in responsiveness to community-based patient referrals. Second, researchers investigated the cultural and linguistic needs within the cancer center’s catchment area, in which 25% of the Hispanic population reports monolingual preference for Spanish.48 Third, researchers met with administrators of the UACC to discuss community-focused patient navigation. This led to an improved electronic communication system between UACC and the regional federally qualified health center, El Rio Health. The community-focused patient navigation program was then developed as 1) bilingual and bicultural, 2) it was predicated on academic-community partnerships, and 3) it was supported by enhanced communication for cancer care patients. Efforts associated with these catchment area factors have enhanced the representativeness of the underserved patient population being served by UACC’s community-focused patient navigation program.24
Example: The Ohio State University Comprehensive Cancer Center
The patient navigation program is imbedded within the Center for Cancer Health Equity (CCHE), with the mandate to reduce barriers to cancer preventive measures, diagnosis, treatment, and healthy survivorship. Recognizing their large catchment area—especially rural areas—it became imperative to know their communities’ demographic characteristics, languages spoken, culture, and percent underserved. Specifically, OSUCCC researchers identified the unmet needs of rural patients and expanded their navigation program to include use of technology (eg, smartphones to communicate with patients in “real time” in English and other languages) to improve access and communication to rural communities. For example, mammography screening efforts use mobile support to save patients from traveling long distances. Specifically, when a woman requests screening, the patient navigator can work with a local community health worker to determine how to pay for the mammogram; where the mammogram will be performed (facility close to woman’s home or a mobile van event hosted by CCHE and OSUCCC); when the mammogram will be done; and how she will get to the appointment. These efforts required understanding the landscape of the catchment area, community and utilization of technology, community health workers, transportation services, and technology-driven communication to improve care access for rural patients.
Capitalize on existing infrastructure to support and sustain a patient navigation program
A common tenet across effective intervention development, implementation and sustainability is the concept of “not reinventing the wheel.” This requires in-depth understanding of the health care setting where an intervention is intended to occur before development and implementation.49 Awareness of opportunities can support acceptability of an intervention because resources can then be used more appropriately.49 Within the context of RE-AIM, effective intervention implementation is influenced by the degree to which the intervention is effectively “Adopted” into the target setting. Understanding of the target settings’ resources (personnel, technology, training capacity, etc) supports effective intervention implementation by capitalizing on key features of the target setting that are already working well.50 Likewise, understanding structural characteristics, available resources, social and electronic networks, culture and climate for change, compatibility, priorities, incentives and setting readiness for implementation are key factors associated with effective intervention implementation.51 Awareness of “slack resources” within a health care setting may also allow for greater acceptability as financial support allows staff to engage in new interventions.52
Researchers identified the following existing infrastructure and available resources that could support their patient navigation intervention effectiveness: physical space (eg, spot for navigator to sit at cancer center), electronic medical communication and database systems (eg, use of advanced reports within Epic), existing staff (eg, clinical research managers), recruitment pathways (eg, booths at the cancer center or study announcements through care team flyers), and job titles (eg, identifying if the job title, “lay navigator” exists within the health care system).53 Capitalizing on existing infrastructure can increase the feasibility of intervention implementation and support the acceptability of the patient navigation program.
Example: Johns Hopkins University Sidney Kimmel Comprehensive Cancer Center-Center to Reduce Cancer Disparities
Building on decades-long engagement with their Community Advisory Groups (first founded in 2009) and advisors within the Johns Hopkins Clinical Research Network, researchers developed a set of strategies and tools to address disparities in access to care. They incorporated a database expert who was previously tasked with screening patients with a new cancer diagnosis referred from zip codes representing underserved communities. They then used the electronic health record to integrate previously identified underserved patients and design care coordination plans for those “high-risk” patients. High-risk patients were defined within “high-risk zip codes” developed by mapping the East Baltimore community that lies adjacent to and around the SKCCC. Researchers worked with SKCCC’s Tumor Registry to identify all cancer cases, collaborated with Baltimore City Health Department to examine “State of Maryland” mortality data for these 9 zip codes, and worked with the Epic staff to build an electronic system that identified callers from these key zip codes who were seeking a “cancer appointment” at the SKCCC. Ultimately, this researcher-designed tool merged an extensive data mapping system with a clinical guideline translation, promoting use of local community resources and tailoring a follow-up process to preventative measures to improve patient outcomes. This “new patient call center database” led to quicker initiation of cancer treatment and more effective transition to survivorship care. Patients received a MyChart “Transition to Primary Care” checklist following active cancer therapy. Another set of web-based communication empowerment training tools, Time to Talk, supported navigators and provided resources for patients and families by decreasing time to first appointments, supporting appointment adherence, MyChart registration and utilization among minority patients, and increasing satisfaction with cancer care. Tools and navigation also flow to a new model: Primary Care for Cancer Survivors, where patients who receive survivorship care report increased confidence in the cancer-informed, holistic care received since the program was established in August 2015. The Hopkins team also worked with Epic to produce daily reports of telephone calls (from high-risk zip codes) to the Oncology Call Center requesting a “first appointment” for a new cancer diagnosis with the goal of more efficiently connecting patient navigators with underserved patients and providing earlier supportive interventions. This approach capitalizes on existing infrastructure as it relates to cancer care coordination efforts, especially for underserved patients.
Example: Georgia Cancer Center for Excellence
Georgia Cancer Center for Excellence at Grady Health System recognized that their lay patient navigation program was producing improvements in outcomes including reduced no-show rates and treatment compliance, so they expanded the program to include nurse navigation. With support from administration, they transitioned an existing nurse into a nurse navigator role for the GI/GU tumor sites; they observed that the nurse navigator gained a high level of acceptability within and across cancer teams. They then expanded the nurse navigation program into other disease sites including breast, GYN, and lung. By identifying nurses with clinical expertise, having the initial navigator train and mentor them, and transitioning them into nurse navigators, GCCE researchers gained a high level of acceptability for expansion among their clinical and administrative teams. The nurse navigation intervention was also able to leverage additional existing technology infrastructure to improve navigation effectiveness. For example, nurse navigators worked with the information technology (IT) department to customize an internal dashboard that tracked nurse navigation metrics. This partnership allowed nurse navigators to more accurately and consistently track and address patients’ barriers to care. For example, the cancer center’s annual Community Health Needs Assessment had identified transportation as a consistent barrier to timely treatment. Using the IT tracking system, researchers instituted an electronic National Comprehensive Cancer Network distress screening with automatic referral triggers for high scoring patients, making it easier for navigators to address barriers. Nurse navigators found that patients who were not on a public transit line or in Grady’s nonemergency transport service area were the ones who experienced more clinic no-shows. This transportation barrier was amplified and prioritized among nurse navigators, and identification of this barrier was a result of existing infrastructure expansion.
Recognize the capacity for mobilizing community support outside the cancer center
Designing an effective patient navigation program requires clarification of the sufficiency of external community resources and organizational support outside the care setting.43 The process of barrier reduction relies heavily on consistent community resource support. For example, a common barrier experienced by underserved patients involves the financial toxicity of cancer treatment.54 In a recent study, patient navigators estimated that 75% of their patients were experiencing financial toxicity,55 and 50% of those navigators also reported that insufficient community resources led to their inability to help these patients.55 Thus, the degree of community support often has strong implications for the sustainability of certain programs and initiatives.
Community health clinics are community resources that serve as primary care settings for many underrepresented patients. When patients present with concerning symptoms consistent with a diagnosis of cancer, connections between community health clinics and patient navigators within a cancer center strengthen the likelihood that the patient will be referred for top-quality cancer care. Community support serves as a beneficial resource for patient navigators, enhances the referral process, helps build mutual trust, and enhances the reputations of both organizations. Within the RE-AIM framework, “Maintenance” of an effective intervention relies heavily on organizational partnerships to sustain an intervention, especially after grant funding has ended.56 With an eye toward sustainability and intervention maintenance, strong community support and acceptability are critical for the long-term sustainability of a patient navigation programs, especially those that rely on community resources and outside health care facilities such as community primary care clinics.
Example: Massachusetts General Hospital Cancer Center
Researchers at MGH recognized the importance of mobilizing community support outside the cancer center by analyzing data on cancer care outcomes. They identified significant disparities between patients receiving care at MGH CHCs as compared with other MGH primary care practices. Mass General Hospital CHCs serve underserved patients in Northeastern Massachusetts where cancer mortality is significantly higher than the US average. These patients are often poor, ethnic and racial minorities, and/or immigrants or refugees who do not speak English and/or are not educated. The MGH patient navigation program hired diverse bi-cultural navigators who spoke several languages and partnered with CHCs to accelerate underserved patients’ access to care. In collaboration with their IT department, they developed an algorithm to create a “TopCare” patient registry that identified patients with a new cancer diagnoses at CHCs. An MGH oncologist, CHC primary care physician, and navigator work together to review the TopCare CHC list on a daily basis. Navigators identify and contact underserved patients and expediently enroll them in the MGH navigation program. One example of this community partnership has been through the North Suffolk Mental Health Association, where MGH enhanced navigation and coordinated cancer care for patients living with serious mental illness. Mobilizing community support has ensured that underserved, newly diagnosed patients receive improved timeliness in their cancer treatments.
Example: Northwestern University Feinberg School of Medicine
Northwestern partners with 2 multi-site nonprofit FQHCs to serve disadvantaged and vulnerable patients in Chicago. This community-based approach leverages existing care coordination staff instead of requiring additional hiring (eg, patient navigators). This is a critical step in ensuring sustainability beyond grant funding. Team members were already familiar with their patient populations, integrated into the clinical care team, familiar with community resources, had physical space within health centers, and had access to electronic medical records thereby not disrupting clinical workflows, adding significant costs, or requiring substantial training. Northwestern and FQHC staff review cancer care coordination materials, codevelop workflows for patient identification and outreach, and conduct staff training. They hold bi-weekly meetings to assess progress, patient needs, barriers to outreach, and potential solutions. This ongoing, iterative and active engagement involves key stakeholders and meets the needs of all patients. Northwestern’s project team also includes AllianceChicago, whose health information technology capacity and data infrastructure creates reports that allow FQHCs to identify patients for outreach. Northwestern uses personalized patient care plans based on the 4R model of care—the Right Information and Right Care for the Right Patient at the Right Time. This model provides patients with a clear plan for treatment, regardless of facility or stage of treatment. Plans can be modified to suit each patient’s needs. A Sequence of Care form outlines the patient’s cancer treatment plan, optimizes coordination and quality of care between Northwestern and community partners, and enhances communication among care team, patients, and family members.
DISCUSSION
This article represents a collaborative effort to address regional disparities in cancer care. For the past 4 years, 6 Alliance partners have implemented or expanded their patient navigation programs. They have also witnessed the successes and challenges faced by partner sites during implementation. Alliance sites focused on various components and stages of cancer care and employed navigators with varying levels of education, experience, and skills. Aside from a shared goal of improving health care quality for all and addressing regional disparities, each program focus was quite different. Yet, through extensive literature review and joint reflections at annual meetings and collaborations, investigators have agreed on 3 critical insights for effective patient navigation programs: 1) understanding patient populations and needs of underserved and high-risk patients, 2) using existing infrastructure, and 3) mobilizing community support. These insights are outlined within the context of patient navigation program effectiveness, and recommendations are accompanied with concrete examples.
The novelty of this article is that 6 NCI-designated cancer sites worked together to review the extensive patient navigation literature and identified that, although some prior attempts at cross-site evaluation have been made,57 the majority of literature is based on single-site data. Furthermore, the literature has primarily focused on establishing the efficacy (ie, targeted outcomes) of patient navigation22,58 as opposed to conducting higher process integration on the effective strategies associated with implementing or expanding patient navigation programs. This article synthesizes and distills effective patient navigation implementation into 3 key insights with the hope that future studies will benefit from greater up-front consideration of the catchment area, the infrastructure, and the community support. The sites’ collective experiences speak to the versatility of navigation programs to be individualized to institutions’ objectives while still managing to achieve common goals. Other researchers have created a comprehensive set of needs assessments, resources, program evaluation metrics, and training standards for assessing patient navigation program effectiveness.43 These tools, together with our recommendations distilled from our 6 Alliance sites will be useful for any cancer center looking to implement an effective patient navigation program.
In conclusion, this process-level article reflects the benefits of collaboration and partnering, and serves as a model for patient navigation intervention development, implementation, and expansion. Presented insights may be useful as cancer settings seek to implement, enhance, or evaluate the effectiveness of patient navigation interventions.
FUNDING SUPPORT
This work was supported by grants from the Merck Foundation Alliance to Advance Patient-Centered Cancer Care. This work was also supported by the National Cancer Institute (R01CA163830, U54CA202995, U54CA202997, U54CA203000, and P20CA233304).
CONFLICT OF INTEREST DISCLOSURES
Darrell M. Gray received consulting fees from Guardant Health Inc and was an unpaid board member for the Association of Black Gastroenterologists and Hepatologists. Ahmed Hassoon reports funding from Merck Foundation, the Agency for Healthcare Research and Quality, the National Heart, Lung, and Blood Institute, the American Heart Association, and the Moor Foundation and a graphic processing unit from NVidia. Electra D. Paskett reports a grant (paid to her institution) from Pfizer. Marita G. Titler received 15% to 25% effort/salary support from Merck Foundation for acting as a Co-Investigator for the National Program Office for the Alliance to Advance Patient-centered Cancer Care. Jennifer A. Wenzel, Electra D. Paskett, Michelle J. Naughton, and Heidi A. Hamann report funding from Merck Foundation. The other authors made no disclosures.
REFERENCES
- 1.Caruso R, Nanni MG, Riba MB, Sabato S, Grassi L. The burden of psychosocial morbidity related to cancer: patient and family issues. Int Rev Psychiatry. 2017;29:389–402. doi: 10.1080/09540261.2017.1288090 [DOI] [PubMed] [Google Scholar]
- 2.Raleigh ZT. A biopsychosocial perspective on the experience of lung cancer. J Psychosoc Oncol. 2010;28:116–125. doi: 10.1080/07347330903438990 [DOI] [PubMed] [Google Scholar]
- 3.PDQ Adult Treatment Editorial Board. Financial toxicity (financial distress) and cancer treatment (PDQ): patient version. In: PDQ Cancer Information Summaries. National Cancer Institute; 2019. [PubMed] [Google Scholar]
- 4.Pisu M, Henrikson NB, Banegas MP, Yabroff KR. Costs of cancer along the care continuum: what we can expect based on recent literature. Cancer. 2018;124:4181–4191. doi: 10.1002/cncr.31643 [DOI] [PubMed] [Google Scholar]
- 5.Zavala VA, Bracci PM, Carethers JM, et al. Cancer health disparities in racial/ethnic minorities in the United States. Br J Cancer. 2021;124:315–332. doi: 10.1038/s41416-020-01038-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bailey ZD, Feldman JM, Bassett MT. How structural racism works—racist policies as a root cause of U.S. racial health inequities. N Engl J Med. 2021;384:768–773. doi: 10.1056/NEJMms2025396 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.A summary of the American Cancer Society Report to the Nation: cancer in the poor. CA Cancer J Clin. 1989;39:263–265. doi: 10.3322/canjclin.39.5.263 [DOI] [PubMed] [Google Scholar]
- 8.Aslam Khan M, Kumar Patel G, Kumar Srivastava S, et al. Looking at cancer health disparities without the colored lenses. Cancer Health Disparities. 2019;3:e1–e9. doi: 10.9777/chd.2019.1004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ko NY, Hong S, Winn RA, Calip GS. Association of insurance status and racial disparities with the detection of early-stage breast cancer. JAMA Oncol. 2020;6:385–392. doi: 10.1001/jamaoncol.2019.5672 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Olazagasti C, Duma N. Cancer care for all? Tales of caring for undocumented patients with cancer. Oncologist. 2020;25:552–554. doi: 10.1634/theoncologist.2020-0113 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.National Cancer Institute. Cancer disparities. Published 2021. Accessed August 24, 2021. https://www.cancer.gov/about-cancer/understanding/disparities
- 12.Molina G, Qadan M. Addressing fragmentation of care requires strengthening of health systems and cross-institutional collaboration. Cancer. 2019;125:3296–3298. doi: 10.1002/cncr.32337 [DOI] [PubMed] [Google Scholar]
- 13.Weaver SJ, Jacobsen PB. Cancer care coordination: opportunities for healthcare delivery research. Transl Behav Med. 2018;8:503–508. doi: 10.1093/tbm/ibx079 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Oluwole SF, Ali AO, Adu A, et al. Impact of a cancer screening program on breast cancer stage at diagnosis in a medically underserved urban community. J Am Coll Surg. 2003;196:180–188. doi: 10.1016/S1072-7515(02)01765-9 [DOI] [PubMed] [Google Scholar]
- 15.Hedlund N, Risendal BC, Pauls H, et al. Dissemination of patient navigation programs across the United States. J Public Health Manag Pract. 2014;20:e15–e24. doi: 10.1097/PHH.0b013e3182a505ec [DOI] [PubMed] [Google Scholar]
- 16.Battaglia TA, Burhansstipanov L, Murrell SS, Dwyer AJ, Caron ASE. Assessing the impact of patient navigation: prevention and early detection metrics. Cancer. 2011;117(suppl 15):3553–3564. doi: 10.1002/cncr.26267 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Braun KL, Kagawa-Singer M, Holden AEC, et al. Cancer patient navigator tasks across the cancer care continuum. J Health Care Poor Underserved. 2012;23:398–413. doi: 10.1353/hpu.2012.0029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wells KJ, Valverde P, Ustjanauskas AE, Calhoun EA, Risendal BC. What are patient navigators doing, for whom, and where? A national survey evaluating the types of services provided by patient navigators. Patient Educ Couns. 2018;101:285–294. doi: 10.1016/j.pec.2017.08.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ustjanauskas AE, Bredice M, Nuhaily S, Kath L, Wells KJ. Training in patient navigation. Health Promot Pract. 2016;17:373–381. doi: 10.1177/1524839915616362 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Valverde PA, Calhoun E, Esparza A, Wells KJ, Risendal BC. The early dissemination of patient navigation interventions: results of a respondent-driven sample survey. Transl Behav Med. 2018;8:456. doi: 10.1093/TBM/IBX080 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Haque S, Ebron S, Bailey B, Blumenfeld B. Use of health information technology among patient navigators in community health interventions. Perspect Heal Inf Manag. 2019;16:1a. [PMC free article] [PubMed] [Google Scholar]
- 22.Bernardo BM, Zhang X, Beverly Hery CM, Meadows RJ, Paskett ED. The efficacy and cost-effectiveness of patient navigation programs across the cancer continuum: a systematic review. Cancer. 2019;125:2747–2761. doi: 10.1002/cncr.32147 [DOI] [PubMed] [Google Scholar]
- 23.Glasgow RE, Harden SM, Gaglio B, et al. RE-AIM planning and evaluation framework: adapting to new science and practice with a 20-year review. Front Public Health. 2019;7:64. doi: 10.3389/fpubh.2019.00064 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ver Hoeve ES, High B, Hernandez M, Armin J, Ali-Akbarian L, Hamann HA, Calhoun E. Implementation and Preliminary Evaluation of a Community-Focused Patient Navigation Program to Address Barriers to Care for Underserved Cancer Patients. In: Presented Virtually: American Society of Preventative Oncology; 2020. https://bit.ly/2U9RMbN [Google Scholar]
- 25.Ver Hoeve ES, High B, Hernandez M, et al. Characterizing Pre- and Post-Intervention Barriers to Care Among Underserved Cancer Patients. In: Poster presented virtually at the Society of Behavioral Medicine Annual Conference. 2021. [Google Scholar]
- 26.Ver Hoeve ES, Ali-Akbarian L, Lothfi NM, et al. Expanding community-focused patient navigation to address barriers to care for underserved cancer patients. In: Poster presented at the Society of Behavioral Medicine Annual Conference. Washington, D.C.: Society of Behavioral Medicine; 2019. [Google Scholar]
- 27.Naughton MJ, Salani R, Lustberg MB, et al. PROMIS-10 scores at six months post-baseline among breast and gynecologic oncology patients participating in a text-based symptom monitoring program with patient navigation. J Clin Oncol. 2020;38(suppl 15):e19173. doi: 10.1200/JCO.2020.38.15_SUPPL.E19173 [DOI] [Google Scholar]
- 28.Percac-Lima S, Ivan S, Ashburner J, et al. Implementing a patient navigation program for community health center patients newly diagnosed with cancer. J Clin Oncol. 2021;39(suppl 28):103. doi: 10.1200/JCO.2020.39.28_suppl.10333052753 [DOI] [Google Scholar]
- 29.Making Action Possible for Southern Arizona. Median household income. Accessed September 12, 2021. https://mapazdashboard.arizona.edu/economy/median-household-income
- 30.Making Action Possible for Southern Arizona. Geography primer for Southern Arizona. Accessed August 24, 2021. https://mapazdashboard.arizona.edu/article/geography-primer-southern-arizona
- 31.Batai K, Gachupin FC, Estrada AL, Garcia DO, Gomez J, Kittles RA. Patterns of cancer related health disparities in Arizona. Cancer Health Disparities. 2019;3:e1–e20. [PMC free article] [PubMed] [Google Scholar]
- 32.Making Action Possible for Southern Arizona. Population profile. Accessed September 12, 2021. https://mapazdashboard.arizona.edu/workforce-demographics/population-profile
- 33.Paskett ED, Young GS, Bernardo BM, et al. The CITIES Project: understanding the health of under-represented populations in Ohio. Cancer Epidemiol Biomarkers Prev. 2019;28:442. doi: 10.1158/1055-9965.EPI-18-0793 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Naughton MJ, Salani R, Peng J, et al. Feasibility of implementing a text-based symptom-monitoring program of endometrial, ovarian, and breast cancer patients during treatment. Qual Life Res. 2021;30:3241–3254. doi: 10.1007/s11136-020-02660-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Rehr S, Coples S, Garret R, et al. The impact of nurse navigation on adherence to care for patients treated with breast cancer in a safety net hospital. Cancer Res. 2021:81(suppl 4):PS7–58. [Google Scholar]
- 36.Rehr C, Carter T, Flenaugh E, et al. Improving timeliness of care for breast, GYN, and aerodigestive cancer patients with nurse navigators in a safety net hospital. J Clin Oncol. 2020;38(suppl 29):183.31794325 [Google Scholar]
- 37.Neal CD, Weaver DT, Raphel TJ, et al. Patient navigation to improve cancer screening in underserved populations: reported experiences, opportunities, and challenges. J Am Coll Radiol. 2018;15:1565–1572. doi: 10.1016/j.jacr.2018.03.001 [DOI] [PubMed] [Google Scholar]
- 38.Freeman HP. Patient navigation: a community based strategy to reduce cancer disparities. J Urban Health. 2006;83:139–141. doi: 10.1007/s11524-006-9030-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Blake KD, Ciolino HP, Croyle RT. Population health assessment in NCI-designated cancer center catchment areas. Cancer Epidemiol Biomarkers Prev. 2019;28:428–430. doi: 10.1158/1055-9965.EPI-18-0811 [DOI] [PubMed] [Google Scholar]
- 40.Paskett ED, Hiatt RA. Catchment areas and community out-reach and engagement: the new mandate for NCI-designated cancer centers. Cancer Epidemiol Biomarkers Prev. 2018;27:517–519. doi: 10.1158/1055-9965.EPI-17-1050 [DOI] [PubMed] [Google Scholar]
- 41.Shelef DQ, Rand C, Streisand R, et al. Using stakeholder engagement to develop a patient-centered pediatric asthma intervention. J Allergy Clin Immunol. 2016;138:1512–1517. doi: 10.1016/j.jaci.2016.10.001 [DOI] [PubMed] [Google Scholar]
- 42.Silberberg M, Martinez-Bianchi V. Community and stakeholder engagement. Prim Care. 2019;46:587–594. doi: 10.1016/j.pop.2019.07.014 [DOI] [PubMed] [Google Scholar]
- 43.National Academies of Sciences, Engineering, and Medicine. Establishing Effective Patient Navigation Programs in Oncology: Proceedings of a Workshop. National Academies Press; 2018. doi: 10.17226/25073 [DOI] [PubMed] [Google Scholar]
- 44.Concannon TW, Fuster M, Saunders T, et al. A systematic review of stakeholder engagement in comparative effectiveness and patient-centered outcomes research. J Gen Intern Med. 2014;29:1692–1701. doi: 10.1007/s11606-014-2878-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.RE-AIM. Improving reach. Accessed August 25, 2021. https://www.re-aim.org/about/what-is-re-aim/reach/improving-reach/
- 46.Brydon-Miller M, Greenwood D, Maguire P. Why action research? Action Res. 2003;1:9–28. doi: 10.1177/14767503030011002 [DOI] [Google Scholar]
- 47.Vann R, Armin J, Bueno Y, et al. Formative qualitative research with cancer survivors to inform a cancer survivorship program. In: Poster presented at El Rio-Wright Center for Graduate Medical Education Community Health Improvement and Research Fair, Tucson, AZ. [Google Scholar]
- 48.Pew Research Center. Demographic and economic profiles of Hispanics by state and county, 2014. Pew Research Center: Hispanic Trends. Accessed January 21, 2021. https://www.pewresearch.org/hispanic/states/state/az/county/04027 [Google Scholar]
- 49.Croot L, O’Cathain A, Sworn K, et al. Developing interventions to improve health: a systematic mapping review of international practice between 2015 and 2016. Pilot Feasibility Stud. 2019;5:127. doi: 10.1186/s40814-019-0512-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.RE-AIM. Adoption–key questions. Accessed August 25, 2021. https://www.re-aim.org/resources-and-tools/adoption-key-questions/
- 51.Consolidated Framework for Implementation Research. Constructs. Accessed August 12, 2020. https://cfirguide.org/constructs/
- 52.Damanpour F. Organizational innovation: a meta-analysis of effects of determinants and moderators. Acad Manag J. 1991;34:555–590. doi: 10.2307/256406 [DOI] [Google Scholar]
- 53.Greenhalgh T, Robert G, Macfarlane F, Bate P, Kyriakidou O. Diffusion of innovations in service organizations: systematic review and recommendations. Milbank Q. 2004;82:581–629. doi: 10.1111/j.0887-378X.2004.00325.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Zafar SY. Financial toxicity of cancer care: it’s time to intervene. J Natl Cancer Inst. 2016;108:djv370. doi: 10.1093/jnci/djv370 [DOI] [PubMed] [Google Scholar]
- 55.Spencer JC, Samuel CA, Rosenstein DL, et al. Oncology navigators’ perceptions of cancer-related financial burden and financial assistance resources. Support Care Cancer. 2018;26:1315–1321. doi: 10.1007/s00520-017-3958-3 [DOI] [PubMed] [Google Scholar]
- 56.RE-AIM. Reach effectiveness adoption implementation maintenance. Accessed April 14, 2021. https://www.re-aim.org/
- 57.Freund KM, Battaglia TA, Calhoun E, et al. National Cancer Institute Patient Navigation Research Program: methods, protocol, and measures. Cancer. 2008;113:3391–3399. doi: 10.1002/CNCR.23960 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Paskett ED, Harrop JP, Wells KJ. Patient navigation: an update on the state of the science. CA Cancer J Clin. 2011;61:237–249. doi: 10.3322/caac.20111 [DOI] [PMC free article] [PubMed] [Google Scholar]


