Abstract
Hydroxyderivatives of vitamin D3, including classical 1,25(OH)2D3 and novel CYP11A1-derived hydroxyderivatives, exert their biological activity by acting as agonists on the vitamin D receptor (VDR) and inverse agonists on retinoid-related orphan receptors (ROR)α and γ. The anti-cancer activities of CYP11A1-derived hydroxyderivatives were tested using cell biology, tumor biology and molecular biology methods in human A431 and SCC13 squamous (SCC)- and murine ASZ001 basal (BCC)-cell carcinomas, in comparison with classical 1,25(OH)2D3. Vitamin D3-hydroxyderivatives with or without a C1α(OH) inhibited cell proliferation in a dose-dependent manner. While all the compounds tested had similar effects on spheroid formation by A431 and SCC13 cells, those with a C1α(OH) group were more potent in inhibiting colony and spheroid formation in the BCC line. Potent anti-tumorigenic activity against the BCC line was exerted by 1,25(OH)2D3, 1,20(OH)2D3, 1,20,23(OH)3D3, 1,20,24(OH)3D3, 1,20,25(OH)3D3 and 1,20,26(OH)3D3, with smaller effects seen for 25(OH)D3, 20(OH)D3 and 20,23(OH)2D3. 1,25(OH)2D3, 1,20(OH)2D3 and 20(OH)D3 inhibited the expression of GLI1 and β-catenin in ASZ001 cells. In A431 cells, these compounds also decreased the expression of GLI1 and stimulated involucrin expression. VDR, RORγ, RORα and CYP27B1 were detected in A431, SCC13 and ASZ001 lines, however, with different expression patterns. Immunohistochemistry performed on human skin with SCC and BCC showed nuclear expression of all three of these receptors, as well as megalin (transmembrane receptor for vitamin D-binding protein), the level of which was dependent on the type of cancer and antigen tested in comparison with normal epidermis. Classical and CYP11A1-derived vitamin D3-derivatives exhibited anticancer-activities on skin cancer cell lines and inhibited GLI1 and β-catenin signaling in a manner that was dependent on the position of hydroxyl groups. The observed expression of VDR, RORγ, RORα and megalin in human SCC and BCC suggested that they might provide targets for endogenously produced or exogenously applied vitamin D hydroxyderivatives and provide excellent candidates for anti-cancer therapy.
Keywords: vitamin D, keratinocytes, vitamin D receptor, retinoidrelated orphan receptor α, retinoid-related orphan receptor γ, squamous cell carcinoma, basal cell carcinoma
Introduction
The ultraviolet spectrum of solar radiation (UVR) that reaches surface of the earth includes both UVA and UVB corresponding to the wavelengths of 320-400 and 290-320 nm, respectively. Both induce various biological effects that are wavelength dependent (1-4). UVR exposure can lead to a range of skin pathologies including skin aging, solar keratosis and melanoma or non-melanoma skin cancers (NMSC). Due to its pleiotropic effects UVR is defined as a full cutaneous carcinogen with UVB being an important etiological factor responsible for basal (BCC) and squamous (SCC) cell carcinomas (4-7). The two chromophore dependent (predominantly UVB) and chromophore independent mechanisms, such as generation of reactive oxygen species (ROS), are involved in epidermal cancerogenesis (2,3,5,8,9), a process further amplified by modification of local homeostasis, including immunosuppression (10). While the mortality for BCC and SCC is low, they are the commonest human cancers with a significant economic burden on the health care system in the USA and worldwide (11). Their incidence increases in immunocompromised patients, including those with organ transplantation, where tumors behave more aggressively. In addition, military personnel are unavoidably exposed in an unprotected manner to high doses of UVR during training or when deployed to locations with high solar radiation. Therefore, occupational overexposure to UVB will be experienced by those who work outdoors or who are exposed intermittently, potentially leading to the development and progression of BCC and SCC. While a number of therapeutic approaches are being tested against these cancers, they are costly and not fully effective, which in part could be secondary to the phenomenon of UVB-induced field of cancerization (12). Therefore, there is an urgent need to establish economical and non-toxic chemopreventive and therapeutic measures against UVB-induced cancer.
UVB also has a beneficial role in biology where transformation of 7-dehydrocholesterol (7DHC) to vitamin D3 (D3) in the skin supplies much of this hormonal precursor for systemic use (13,14). Higher doses of UVB lead to photoisomerization of the previtamin D3 intermediate to lumisterol (L3) and tachysterol (T3) (13). In the classical pathway, D3 is activated by hydroxylation at C25 producing 25(OH)D3 in the liver and subsequently at C1 producing 1,25(OH)2D3 (kidney) with local (skin) production also occurring (13,15,16). 1,25(OH)2D3, in addition to regulating calcium homeostasis, has pleiotropic activities that include anti-cancer effects (13,15-18). In the skin, it regulates formation of the epidermal barrier, hair cycling and attenuates cancerogenesis and inflammatory processes (13,16,19-22). 1,25(OH)2D3 can also protect against UVB-induced cell death and DNA damage (23-26) with topically applied D3 precursor being able to inhibit UVB-induced cancerogenesis in mice (27).
We previously reported an alternative metabolic pathway of D3 activation initiated by the action of CYP11A which converted D3 to 20(OH)D3 and 22(OH)D3 with some further side-chain hydroxylations producing di-hydroxy (such as 20,23(OH)2D3) and tri-hydroxy species. The major product was 20(OH)D3 and this can be further modified by other CYP enzymes including CYP2R1, CYP27A1 and CYP27B1 (28-34). Many of these pathway products and intermediates have been detected in both humans and animals (28,29,31,33,34). 20(OH)D3 has been shown to be present in serum and to accumulate together with its downstream derivatives in human epidermis (28,29,31). Thus, 20(OH)D3 and related metabolites are physiologically relevant endogenous bioregulators that can be defined as natural products (35). They show antiproliferative, prodifferentiation, anti-inflammatory and anti-cancer effects that are comparable to those of 1,25(OH)2D3 (30,36-41). They also protect human keratinocytes against UVB damage (42-45) and topically applied 20(OH)D3 attenuates UVB-induced skin damage in Skh:hr1 mice (46).
While the phenotypic effects of canonical 1,25(OH)2D3 are predominantly mediated through interaction with the vitamin D receptor (VDR) through genomic and non-genomic mechanisms (13,47-50), CYP11A1-derived vitamin D hydroxyderivatives, in addition to acting on VDR (51-53), can also act on retinoid-related orphan receptors (RORs) α and γ (54-56) and the aryl hydrocarbon receptor (AhR) (57). Furthermore, clinico-pathological analyses of human melanoma samples have shown that expression of VDR and RORα and γ changes during tumor progression and correlates with disease outcomes (58-62).
Notably, 20(OH)D3 and 20,23(OH)2D3 are noncalcemic and non-toxic at extremely high doses in rats and mice (37,39,63,64) unlike the majority of low-calcemic derivatives of D3 that have been chemically synthesized (18,65), identifying the former as potential therapeutics.
Therefore, using a wide range of CYP11A1-derived vitamin D hydroxyderivatives, some modified by 1α-hydroxylation by CYP27B1, the present study examined their anticancer potential in human SCC and murine BCC lines. In addition, it analyzed the expression of the VDR, RORα and γ, and megalin/LRP2 which is a transmembrane receptor for vitamin d-binding protein for cellular import of 25(OH)D3 (66-68), in a panel of benign and malignant epidermal lesions.
Materials and methods
Vitamin D derivatives
Vitamin D3 and D2, 1,25(OH)2D3 and 25(OH)D3 were purchased from MilliporeSigma. Hydroxyderivatives of D3 and D2 were synthesized enzymatically or non-enzymatically as described in Fig. S1 and purified as previously described (30,32,63,69-76). The purity of the compounds was >99%. The compounds were dissolved in ethanol and applied to cell cultures as previously described (44,51,57). All vitamin D-derived compounds were dissolved in ethanol. The active compounds were prepared as stock solutions at 10−4 M and then diluted with medium to final concentrations ranging from 10−7 to 10−12 M (as indicated in the figures) and added to cell cultures. In each experiment, the control with vehicle (ethanol) was prepared.
Cell culture
The murine basal cell carcinoma (BCC) cell line ASZ001 and human skin squamous cell carcinoma (SCC) cell lines were used for the experiments. ASZ001 was a gift from Dr Ervin Epstein (University of California, San Francisco, CA) (77,78), A431 was purchased from ATCC (cat. no. CRL-1555) and SCC13 was a gift from Dr. S. K. Katiyar (University of Alabama at Birmingham, Birmingham, AL) (79). The BCC cell line was cultured in 154CF medium (Thermo Fisher Scientific, Inc.) (77,78) and SCC cell lines were cultured in Dulbecco's modified Eagle's medium (DMEM; Corning Inc.), supplemented with 10% fetal bovine serum (FBS; MilliporeSigma), antibiotic-antimycotic solution (Corning Inc.) and maintained in 5% CO2 at 37°C (79). For experimental treatment, charcoal-treated FBS (ctFBS) was used as previously described (44).
Proliferation assays
The MTS, sulforhodamine B (SRB) tests were used to measure proliferation of BCC and SCC cells as described previously (80,81). BCC and SCC cells were seeded on 96-well plates in complete culture medium for 24 h in 5% CO2 at 37°C. The next day the medium was replaced with serum-free medium and the cells starved for the subsequent 24 h. Cells were treated with secosteroids dissolved in ethanol and added to culture medium with 10% charcoal-treated FBS, for 24, 48 and 72 h. To assess the effects of secosteroids on BCC and SCC cells, the metabolic activity was tested using a tetrazolium compound and an electron coupling reagent (MTS; CellTiter 96 AQueous One Solution Cell Proliferation Assay, Promega Corporation), as previously described (80,81): 20 µl of MTS/PMS solution was added to the cells and incubated for 2 h at 37°C then read the absorbance at 490 nm using Cytation 5 (BioTek Instruments, Inc.). SRB was also used to determine cell number and cell viability by colorimetric evaluation of total protein content as the dye binds to cellular proteins. The BCC and SCC cells were assayed as described previously (82). Briefly, after the treatment with secosteroids, BCC and SCC cells were fixed for 1 h with 10% trichloroacetic acid at 4°C and incubated with 0.4% sulforhodamine B in 1% acetic acid for 30 min at room temperature. Next, the protein-bound dye was dissolved in Tris base solution and the absorbance was measured at 565 nm using Cytation 5 (BioTek Instruments, Inc.).
Spheroids and colony formation
To assess the ability of the secosteroids being tested to inhibit anchorage-independent growth of BCC and SCC cells, the spheroid formation test was performed as previously described (81). Briefly, cells were seeded into ultra-low attachment 96-well plates in culture medium supplemented with epidermal growth factor (MilliporeSigma), basic fibroblast growth factor (MilliporeSigma), insulin (Thermo Fisher Scientific, Inc.), bovine serum albumin (MilliporeSigma) and B27 supplement (Thermo Fisher Scientific, Inc.). After seven days the plate was scanned using a Cytation 5 microplate reader and Gene5 software (BioTek Instruments, Inc.).
For colony formation assay, cells were plated in 6-well plates (1,000 cells/well) and incubated with graded concentrations of the secosteroids for 6 days. After methanol (70%) fixation at 4°C and staining with 0.1% crystal violet, the colonies were counted using Cytation 5 (BioTek Instruments, Inc.) and analyzed by Gene 5 software. The large (>0.5 mm), medium (>0.25 mm) and small colonies (>0.1 mm) colonies were counted.
Western blot analysis
RIPA Lysis and Extraction Buffer (Thermo Scientific; cat. no. 89901) was used for whole cell extract and Nuclear Extract kit (Active Motif, Inc.; cat. no. 54001) for nuclear and cytoplasmic fractions as described previously (43,44). Protein concentration was measured with Pierce BCA Protein Assay kit (Thermo Scientific; cat. no. 23225). For protein separation 4-15% Mini-PROTEAN TGX Stain-Free Protein Gels, 10 well, 30 µl (Bio-Rad Laboratories, Inc.; cat. no. 4568083) were used with 20 µg of proteins loaded per lane. The proteins were transferred to Immobilon-P PVDF membranes (MilliporeSigma; cat. no. IPVH00010). Prior incubation with primary antibodies the membranes were incubated with 5% skimmed milk in TBS-T buffer (Tris-buffer saline containing 0.1% (v/v) Tween 20 and 5% (w/v) skim milk) for 1 h at room temperature.
Immunodetection of VDR protein expression was performed using VDR antibody (D-6; cat. no. sc-13133; Santa Cruz Biotechnology, Inc.) at a 1:200 dilution (1 h incubation at room temperature) followed by treatment of secondary antibody, m-IgGκ BP-HRP (cat. no. sc-516102; Santa Cruz Biotechnology, Inc.; 1 h incubation at room temperature at 1:2,000 dilution). RORα Polyclonal Antibody (cat. no. PA1-812; Invitrogen; Thermo Fisher Scientific, Inc.; 1:1,000) and RORg(t) monoclonal Antibody (cat. no. 14-6988-82; Invitrogen; Thermo Fisher Scientific, Inc.; 1:500) were used for RORα and RORγ protein expression, respectively at 1 h at room temperature. Goat Anti-Rabbit IgG (cat. no. ab6721; Abcam; 1:5,000) and Anti-rat IgG, HRP-linked Antibody (cat. no. 7077; Cell Signaling Technology, Inc.; 1:2,000) were used as secondary antibodies for RORα and RORg, respectively. The membranes were reprobed with following antibodies to measure the protein loading. Lamin C: lamin A/C antibody (N-18) (Santa Cruz; cat. no. sc-6215) for primary antibody (1 h incubation at room temperature at 1:200 dilution) with donkey anti-goat IgG-HRP (Santa Cruz; cat. no. sc-2020) for secondary antibody (1 h at room temperature at 1:5,000 dilution). α-Tubulin: alpha Tubulin Antibody (Thermo Fisher Scientific, Inc.; cat. no. 62204) for primary antibody (1 h incubation at room temperature at 1:5,000 dilution) and goat anti-mouse IgG-HRP (Santa Cruz; cat. no. sc-2005) for secondary antibody (1 h incubation at room temperature at 1:5,000 dilution). β-Actin: anti-β-Actin-Peroxidase antibody, mouse monoclonal (MilliporeSigma; cat. no. A3854) with 1hr incubation at room temperature at 1:10,000 dilution. After each incubation with primary antibody membranes were washed three times with TBS-T (Tris-buffer saline containing 0.1% (v/v) Tween 20) for 10 min each prior incubation with secondary antibody. Immuno-reactivity was detected using the SuperSignal West Pico PLUS Chemiluminescent Substrate (Thermo Fisher Scientific, Inc., cat. no. 34580) or Immobilon Crescendo Western HRP substrate (MilliporeSigma; cat. no. WBLUF0500). The integrated optical density of the bands was analyzed by ImageJ software, version 1.53a (National Institutes of Health).
Flow cytometry
A431 cells were treated with 100 nM 1,20(OH)2D3, 1,25(OH)2D3, 20(OH)D3, or ethanol (vehicle) for 24 h. To test the stimulation of differentiation by vitamin D3 derivatives, after treatment the cells were fixed in 2% paraformaldehyde (Thermo Fisher Scientific, Inc.) in PBS for 1 h at room temperature. Following washing with PBS, pellets were resuspended in 100 µl of permeabilizing solution containing 0.1% BSA and 0.1% NaN3 in PBS and 0.2 µg primary antibody against involucrin (Novocastra Laboratories Ltd.). Cells stained with isotype control antibody (IgG1; Caltag Medsystems) were used as controls. After overnight incubation at 4°C, cells were washed with PBS and resuspended in 100 µl of permeabilizing solution containing sheep anti-mouse FITC-conjugated secondary antibody (1:50; cat. no. NCL-SAM-FITC; Novocastra Laboratories Ltd.). After 3 h of incubation at 4°C, cells were washed with PBS, centrifuged and resuspended in 500 µl of PBS. Samples were read and analyzed with an Accuri C6 (BD Bioscience) flow cytometer and BD Accuri C6 Plus software 8 (BD Bioscience). The FL-1 signal (collected from 10,000 events inside scatter/forward scatter window after debris exclusion) was recorded. Forward (relative to cell size) and side (relative to cell granularity) scatter were recorded. The number of events (positive cells)-FL-1 signal values are presented as difference between mean fluorescence intensity of sample stained with specific and isotype control antibody (dMFI). Scatter signal values were presented as MSI (mean signal intensity).
Immunofluorescence studies
VDR, RORα and RORγ in BCC and SCC cells were immunostained as previously described (81) (for details see Fig. S2: Scheme for immunohistochemistry and characteristic of reagents used). Briefly, the cells were seeded in a 96-well plate and grown until reaching ~70% confluence then fixed with 4% buffered formalin for 20 min at room temperature. Following permeabilization, the cells were blocked with 0.5% Triton X-100 and 2% bovine serum albumin (BSA) for 1 h at room temperature, followed by overnight incubation with primary antibodies (VDR; clone 9A7; Thermo Fisher Scientific, Inc., cat. no. MA1-710, 1:50) and RORα (1:400) and RORγ (1:400) [both antibodies developed at NIEHS and characterized as reported in (54)] overnight at 4°C and incubation with the secondary antibody (goat anti-rat IgG (H+L) Cross-Adsorbed Secondary Antibody, cat. no. A-11006A, Alexa Fluor 488goat anti-rabbit immunoglobulin G (IgG; H + L) Cross-Adsorbed Secondary Antibody, Alexa Fluor 488, cat. no. A-11008; both Thermo Fisher Scientific, Inc.), diluted 1:1,000 for 1 h at room temperature. After washing the cell nuclei were stained with propidium iodide (PI; MilliporeSigma) and examined with a Cytation 5 microplate reader (BioTek Instruments, Inc.). For changes in GLI1 and β-catenin expression, ASZ001 and A431 lines were treated with 20(OH)D3, 1,20(OH)2D3, 25(OH)D3, 1,25(OH)2D3 or vehicle (ethanol) at 10−7 M at 37°C for 24 h. After washing the cell nuclei were stained with propidium iodide (PI; MilliporeSigma) and examined with a Cytation 5 microplate reader (BioTek Instruments, Inc.).
Immunohistochemistry
For immunohistochemistry, the standard formalin-fixed paraffin-embedded skin samples of normal skin BCC, SCC in situ and invasive SCC were included in this study (Table SI). The authors declare that this investigation was carried out following the rules of the Declaration of Helsinki of 1975 (revised in 2008) and this study was approved by the institutional review board (IRB) of the University of Alabama at Birmingham under IRB-940831016 (OCCC Tissue Procurement CORE Facility) and IRB-00000726 (Title E150427002, Dr. A. Slominski PI). The IRB of the University of Alabama at Birmingham, which gave its permission for conducting the present study, waived the requirement to obtain patients' informed consent for this research. VDR, RORα, RORγ and megalin in tissues samples of normal skin, BCC and SCC were labelled as previously described (83,84) (for details see Fig. S2). Briefly, heat-induced antigen retrieval (96°C, 20 min) in high pH unmasking solution (Vector Laboratories, Inc.) was performed on formalin-fixed paraffin embedded sections, followed by blocking of endogenous peroxidase for 10 min. The sections were incubated 30 min at room temperature with anti-Lrp2/Megalin antibody (cat. no. ab76969; Abcam) or overnight with other antibodies (anti-VDR; clone 9A7; cat. no. MA1-710) or anti-RORγ and anti-RORα [generated as previously described (54)] with subsequent incubation at room temperature with secondary antibodies conjugated with HRP (ready-to-use anti-rabbit (cat. no. MP-7451) and anti-mouse (cat. no. MP-7452) ImmPRESS antibodies, Vector Laboratories, Inc. for RORs and megalin; anti-rat antibody, (1:200; cat. no. ab97057; Abcam) for VDR. The immunolabelling was visualized with peroxidase substrate ImmPACT NovaRED (Vector Laboratories Inc.) and the sections were mounted with permanent mounting (Thermo Fisher Scientific, Inc.) under coverslips. Sections were analyzed under a light microscope (magnification, ×200). The mean staining intensity was assessed by two observers (ATS and AAB).
The analysis of the expression of RORA and RORC mRNA level followed public genomics data repository Gene Expression Omnibus, accession number GSE7553 http://www.ncbi.nlm.nih.gov/geo). For details on data collection, methods and patient's characteristic performed by Riker et al (85) please refer to their original paper.
Reverse transcription-quantitative (RT-q) PCR
Cultures at 70% confluency were used for treatment. After treatment for 24 h with secosteroids, cells were detached using trypsin and centrifuged at 271 × g for 5 min at 4°C. Cell pellets were then collected, and total RNA was isolated using an Absolutely RNA Miniprep kit (1.2 ml per 4×106 cells) (Agilent Technologies, Inc.). The RNA purity and quantification were performed with Cytation 5 (BioTek Instruments, Inc.) and the absorbance 260/280 ratio ~2 checked for the purity. Total RNA (0.5 µg) was used for cDNA synthesis with a High-Capacity cDNA Reverse Transcription kit (Applied Biosystems, Waltham, MA, USA) following the manufacturer's protocol. The cDNA (750 ng) was used for qPCR. β-actin was used as an internal control. qPCR was performed using Kapa SYBR Fast qPCR Master Mix (Kapa Biosystems; Roche Diagnostics) with QuantStudio 6 Flex Real-Time PCR Systems (Applied Biosystems; Thermo Fisher Scientific, Inc.) in quadruplicate, following the manufacturer's protocol and as previously described (43,44). Primer sequences are listed in Table SII. Data were collected with QuantStudio Real-Time PCR Software v1.2 (Applied Biosystems; Thermo Fisher Scientific, Inc.) and the amount of mRNA was normalized by the comparative 2−ΔΔCq method followed by calculating the fold change, using β-actin as a housekeeping gene as described previously (43,44). The experiments were repeated three times.
Statistical analysis
Data exported from Microsoft Excel were analyzed using GraphPad Prism 7 (GraphPad Software, Inc.) statistical software and are presented as means ± SD or SEM as indicated in the figures legend. The data were analyzed by one way ANOVA with Dunnett's multi comparison post-hoc test or the Student's t-test as detailed in figure legends.
Results
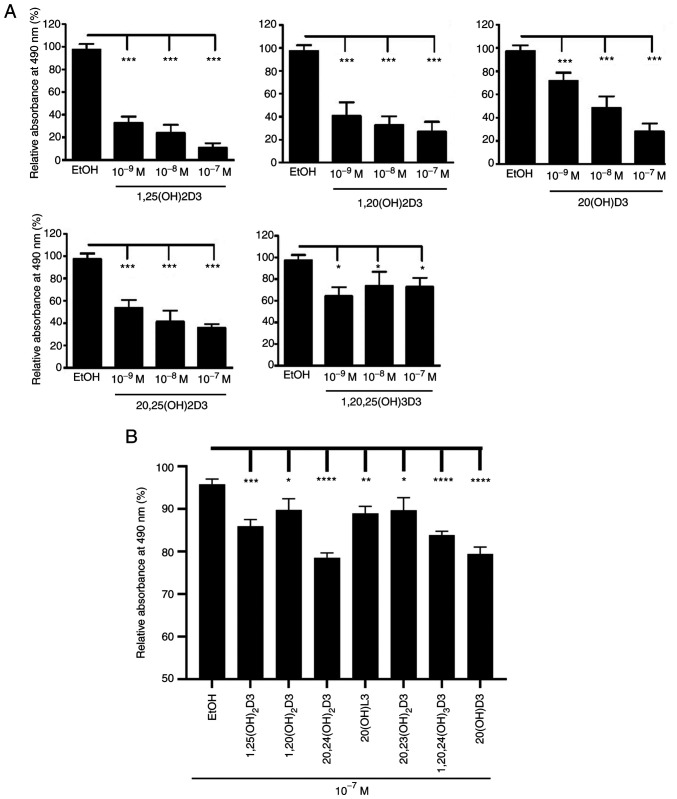
The present study investigated the in vitro antitumor effects of CYP11A1-derived D3-hydroxyderivatives using established lines of human squamous (A431 and SCC-13) and mouse basal cell (ASZ0001) carcinoma. The structures of the secosteroids that were tested are presented in Table I, with stereochemistry shown where known. The MTS tests showed that a range of representative vitamin D3-hydroxyderivatives inhibited proliferation of basal and squamous cell carcinoma cells in a dose-dependent manner (Fig. 1). Similar inhibitory effects were observed using the RBS assay (data not shown).
Table I.
Chemical structures of vitamin D hydroxyderivatives analyzed.
| Chemical name | Chemical structure | Chemical name | Chemical structure |
|---|---|---|---|
| 1,25(OH)2D3 1α,25-dihydroxyvitamin D3 (1R,3S,Z)-5-(2-((1R,7aR,E)-1-((R)-6-hydroxy-6-methylheptan-2-yl)-7a-methyloctahydro-4H-inden-4-ylidene)ethylidene)-4-methylenecyclohexane-1,3-diol |
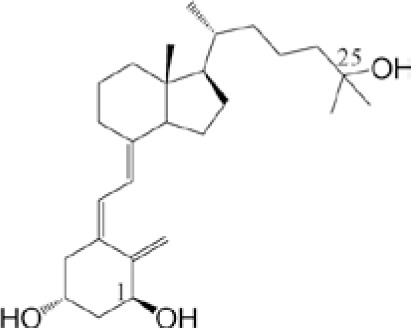
|
20,23(OH)2D3 20S,23S-dihydroxyvitamin D3 (2S,4S)-2-((1S,7aS,E)-4-((Z)-2-((S)-5-hydroxy-2-methylenecyclohexylidene) ethylidene)-7a-methyloctahydro-1H-inden-1-yl)-6-methylheptane-2,4-diol |
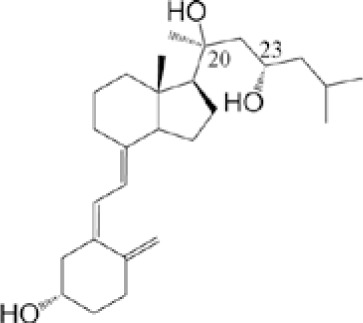
|
| 1,20(OH)2D3 1α,20S-dihydroxyvitamin D3 (1R,3S,Z)-5-(2-((1S,7aS,E)-1-(2-hydroxy-6-methylheptan-2-yl)-7a-methyloctahydro-4H-inden-4-ylidene)ethylidene)-4-methylenecyclohexane-1,3-diol |
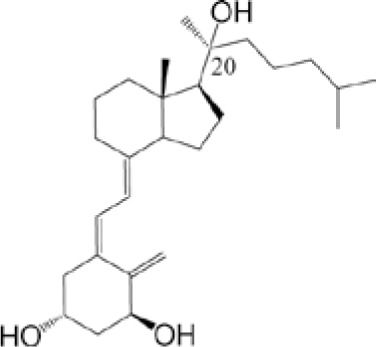
|
20,24(OH)2D3 20S,24R-dihydroxyvitamin D3 (2S,5R)-2-((1S,7aS,E)-4-((Z)-2-((S)-5-hydroxy-2-methylenecyclohexylidene) ethylidene)-7a-methyloctahydro-1H-inden-1-yl)-6-methylheptane-2,5-diol |
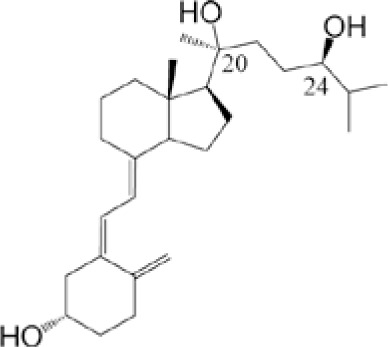
|
| 1,20,23(OH)3D3 1α,20S,23S-trihydroxyvitamin D3 (1R,3S,Z)-5-(2-((1S,7aS,E)-1-((4S)-2,4-dihydroxy-6-methylheptan-2-yl)-7a-methyloctahydro-4H-inden-4-ylidene)ethylidene)-4-methylenecyclohexane-1,3-diol |
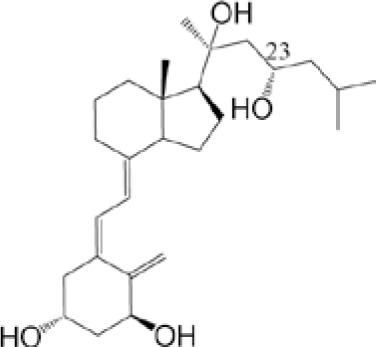
|
20,25(OH)2D3 20S,25-dihydroxyvitamin D3 2-((1S,7aS,E)-4-((Z)-2-((S)-5-hydroxy-2-methylenecyclohexylidene) ethylidene)-7a-methyloctahydro-1H-inden-1-yl)-6-methylheptane-2,6-diol |
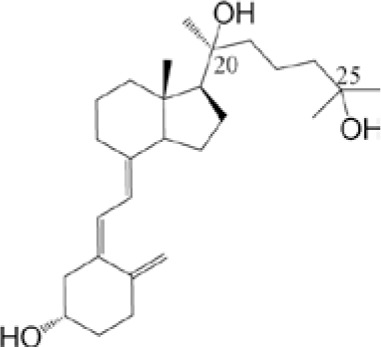
|
| 1,20,24(OH)3D3 1α,20S,24R-trihydroxyvitamin D3 (1R,3S,Z)-5-(2-((1S,7aS,E)-1-((5R)-2,5-dihydroxy-6-methylheptan-2-yl)-7a-methyloctahydro-4H-inden-4-ylidene)ethylidene)-4-methylenecyclohexane-1,3-diol |
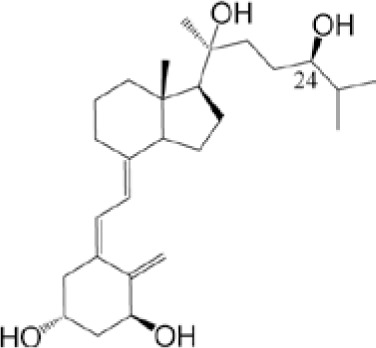
|
17,20(OH)2D2 17R,20S-dihydroxyvitamin D2 (1R,7aS,E)-4-((Z)-2-((S)-5-hydroxy-2-methylenecyclo-hexylidene)ethylidene)-1-((2S,5R,E)-2-hydroxy-5,6-dimethylhept-3-en-2-yl)-7a-methyloctahydro-1H-inden-1-ol |
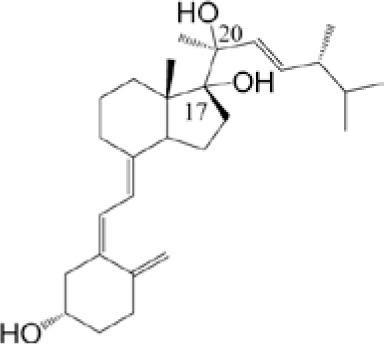
|
| 1,20,25(OH)3D3 1α,20S,25-trihydroxyvitamin D3 (1R,3S,Z)-5-(2-((1S,7aS,E)-1-(2,6-dihydroxy-6-methylheptan-2-yl)-7a-methyloctahydro-4H-inden-4-ylidene)ethylidene)-4-methylenecyclohexane-1,3-diol |
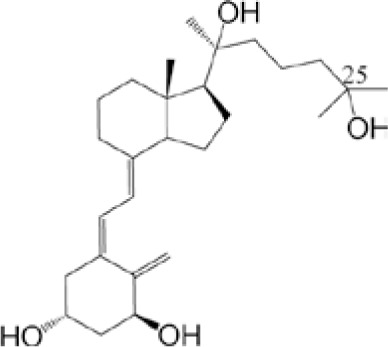
|
20(OH)D2 20-hydroxyvitamin D2 (1S,Z)-3-(2-((1S,7aS,E)-1-((2S,5R,E)-2-hydroxy-5,6-dimethylhept-3-en-2-yl)-7a-methyloctahydro-4H-inden-4-ylidene)ethylidene)-4-methylenecyclohexan-1-ol |
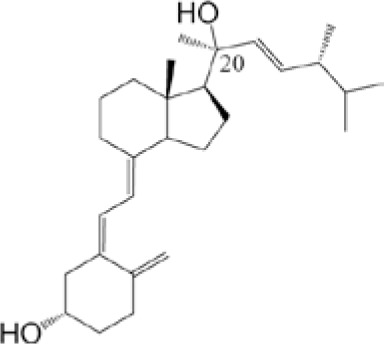
|
| 1,20,26(OH)3D3 1α,20S,26-trihydroxyvitamin D3 (1R,3S,Z)-5-(2-((1S,7aS,E)-1-((2S)-2,7-dihydroxy-6-methylheptan-2-yl)-7a-methyloctahydro-4H-inden-4-ylidene)ethylidene)-4-methylenecyclohexane-1,3-diol |
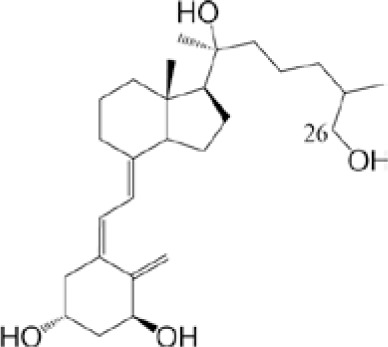
|
22(OH)D3 22-hydroxyvitamin D3 (1S,Z)-3-(2-((1R,7aR,E)-1-((2S)-3-hydroxy-6-methylheptan-2-yl)-7a-methyloctahydro-4H-inden-4-ylidene)ethylidene)-4-methylenecyclohexan-1-ol |
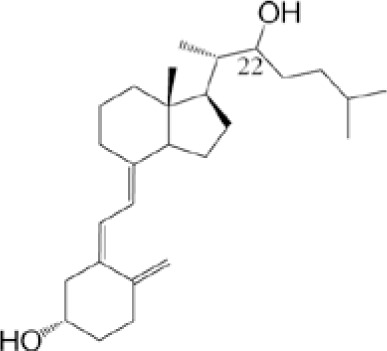
|
| 20(OH)D3 20S-hydroxyvitamin D3 (1S,Z)-3-(2-((1S,7aS,E)-1-((S)-2-hydroxy-6-methylheptan-2-yl)-7a-methyloctahydro-4H-inden-4-ylidene)ethylidene)-4-methylenecyclohexan-1-ol |
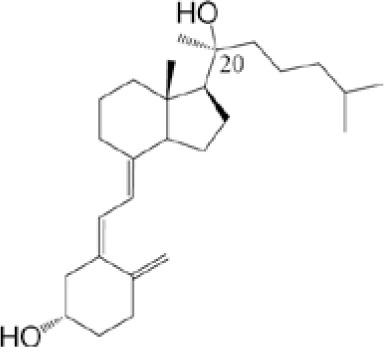
|
25(OH)D3 25-dihydroxyvitamin D3 (1S,Z)-3-(2-((1R,7aR,E)-1-((R)-6-hydroxy-6-methylheptan-2-yl)-7a-methyloctahydro-4H-inden-4-ylidene)ethylidene)-4-methylenecyclohexan-1-ol |
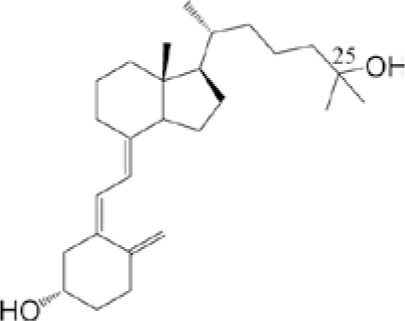
|
Figure 1.
Inhibition of cell proliferation of (A) human A431 cells and (B) murine ASZ001 cells by hydroxy-derivatives of vitamin D3 in comparison with 1,25(OH)2D3 (positive) and ethanol (negative) controls. Cells were seeded in 96-well plates and treated with the listed secosteroids for 24 h and cell proliferation assessed using the MTS assay. Data are shown as means ± SEM (n=6) with ****P<0.0001; ***P<0.001; **P<0.001; *P<0.05 by (A) one way ANOVA with Dunnett's multi comparison post-hoc test or (B) Student's t-test. The concentrations of the secosteroids used are shown on the x axis.
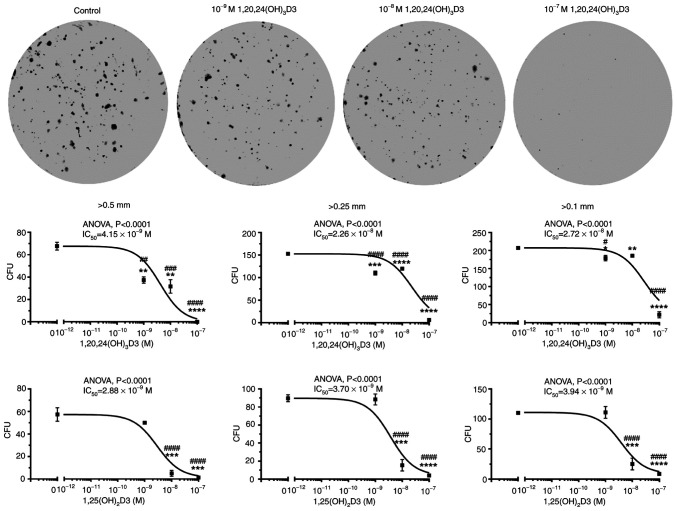
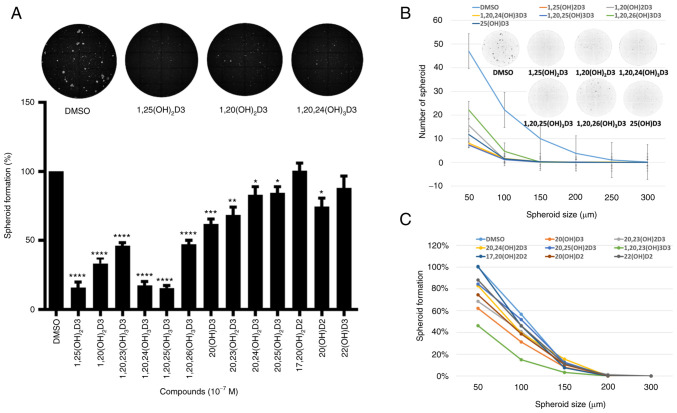
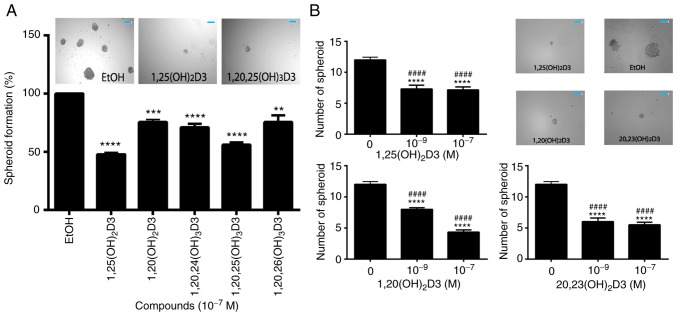
1,20,24(OH)3D3 and 1,25(OH)2D3 were selected to test the effect of secosteroids on colony formation by the murine basal cell carcinoma line, ASZ001 (Fig. 2). The two secosteroids caused a dose-dependent inhibition of the formation of large (>0.5 mm), medium (>0.25 mm) and small colonies (>0.1 mm). Using spheroid formation assays the antitumor activities of all the CYP11A1-derived hydroxyderivatives of vitamin D3 under study (Table I) were tested against the ASZ001 cell line (Fig. 3). The inhibition of spheroid formation by different secosteroids, with or without hydroxyl group at C1α and in comparison with canonical 1,25(OH)2D3, is shown in Fig. 3A. Only 22(OH D3 and 17,20(OH)2D2 failed to significantly inhibit spheroid formation at the dose (10−7 M) tested. Secosteroids having a C1α hydroxyl group generally showed greater inhibition than those lacking this functional group. Fig. 3B and C show the effect of secosteroids on spheroid formation depending on their size. Similar inhibitory effects on spheroid formation by representative secosteroids containing a 1α-hydroxyl group, in comparison with 1,25(OH)2D3, (control) were observed in A431 cell carcinoma cells (Fig. 4A). The dose dependency of selected secosteroids on spheroid formation by SCC13 squamous cells is shown in Fig. 4B with significant inhibition being observed already at 10−9 M.
Figure 2.
1,20,24(OH)3D3 and 1,25(OH)2D3 inhibit colony formation by murine ASZ001 cells. Cells were plated in 6 well-plates (1,000 cells/well) and incubated with graded concentrations of the secosteroids for six days. After methanol fixation and staining with 0.1% crystal violet, the colonies sized >0.5, >0.25, >0.1 mm were counted using Cytation 5 and analyzed by Gene 5 software (BioTek Instruments, Inc.). Representative images for 1,20,24(OH)3D3 treatment are shown at the top of the Figure. Data points for the dose responses (lower panels) are shown as means ± SEM (n=3) *P<0.05, **P<0.01, ***P<0.001, ****P<0.0001 by Student's t-test; #P<0.05, ##P<0.01, ###P<0.001, ####P<0.0001 at one-way AVOVA with Dunnett's multi comparison post-hoc test. IC50 values were calculated from the non-fitted dose-response curves.
Figure 3.
Inhibition of spheroid formation of murine ASZ001 cells by secosteroids. Cells suspended in tumerosphere medium (154CF phenol red free, 0.4% BSA, 20 ng/ml EGF, 10 ng/ml FGF, 5 µg/ml insulin) were treated with the listed secosteroids and seeded into low adhesion 24 well plates (500 cells/well) and incubated for 7 days at 37°C. (A) Spheroids ≥50 µm in size were counted using Cytation 5 (BioTek Instruments, Inc.). Representative images were taken by Cytation 5 at microscopic magnification 4× Data are shown as means ± SEM (n=6) with *P<0.05, **P<0.01, ***P<0.001, ****P<0.0001 by Student's t-test. Inhibition of spheroids formation in relation to (B) their size (means ± SD; n=6) or (C) means where SD ≤15% of the mean; n=6.
Figure 4.
Inhibition of (A) human A431 and (B) human SCC13 cell spheroids formation by secosteroids. Cells suspended in tumerosphere medium (DMEM, 0.4% BSA, 20 ng/ml EGF, 10 ng/ml FGF, 5 ug/ml insulin) were treated with the selected secosteroids and seeded into low adhesion 96 well plates (1,000 cells/well) then incubated for 7 days at 37°C. Spheroids ≥50 um in size were counted using Cytation 5 (BioTek Instruments, Inc.). Scale bar=200 µm. Data represent means ± SEM (n=6) with **P<0.01, ***P<0.001, ****P<0.0001 by the Student's t-test in A or ####P<0.0001 at one-way AVOVA with Dunnett's multi comparison post-hoc test.
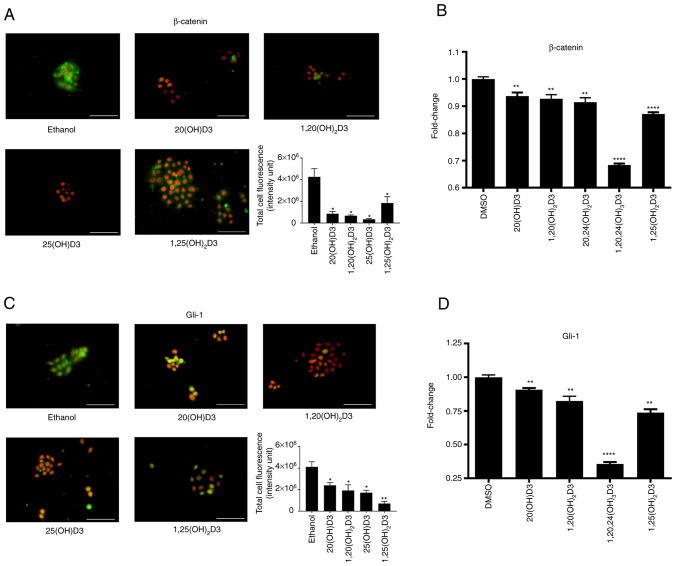
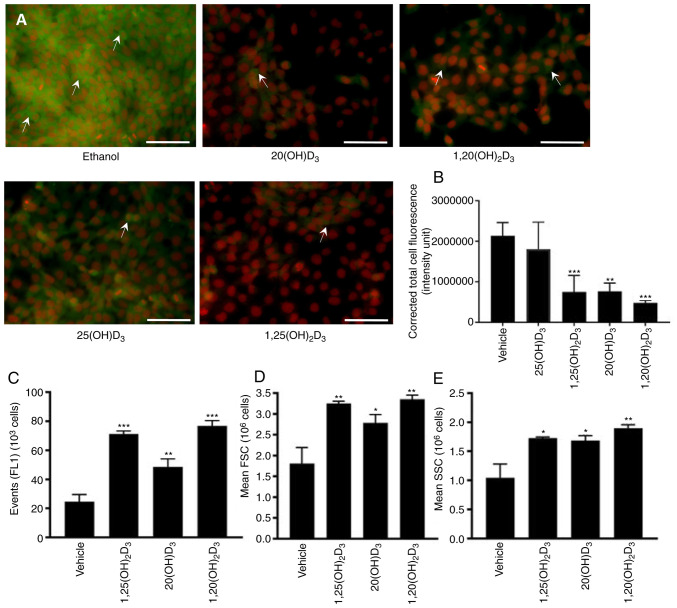
As the authors have previously shown that the antitumor effects against oral squamous cell carcinoma are associated with inhibition of β-catenin and glioma-associated oncogene 1 (Gli1) (80), the effect of vitamin D-hydroxyderivatives on the expression of β-catenin and Gli1 were tested in the murine ASZ001 carcinoma line. The selected secosteroids, including 25(OH)D3 and 1,25(OH)2D3 as well as CYP11A1-derived 20(OH)D3 and 1,20(OH)2D3, significantly inhibited intracellular expression of these proteins (Fig. 5A-D). These effects were further substantiated by inhibition of the expression of Gli1 and Ctnnb1 genes, by a panel of vitamin D derivatives (Fig. 5A-D). A similar inhibitory effect on Gli1 expression by 20(OH)D3, 1,20(OH)2D3 and 1,25(OH)2D3, but not by 25(OH D3 was observed in the A431 line (Fig. 6A and B). The expression of β-catenin was not evaluated as it was below the level of detection by the procedure employed. The effects of 20(OH)D3 and 1,20(OH)2D3 on involucrin expression was also tested in comparison with 1,25(OH)2D3 in the A431 cells. Stimulation by all three secosteroids was observed (Fig. 6C-D).
Figure 5.
Inhibition of β-catenin and GLI1 signaling in the ASZ001 murine basal cell carcinoma cell line by vitamin D hydroxyderivatives. Cells were treated with 10−7 M of representative secosteroids in comparison with vehicle control (ethanol), for 24 h. The cells were stained with (A) murine antibodies against β-catenin (green) or (C) rabbit antibodies against GLI1 (green), or RNA was isolated for qPCR assay of (B) Ctnnb1 (gene coding β-catenin) or (D) Gli1 (gene coding Gli1) gene expression. Cell nuclei are red (counterstained with propidium iodide). Scale bar=100 µm. For protein expression the images were analyzed to calculate the corrected total cell fluorescence [CTCF=integrated density-(area of selected cell x mean fluorescence of background readings)] using ImageJ. For gene expression, data were normalized by the comparative 2−ΔΔCq method followed by calculating the fold change, using β-actin as a housekeeping gene. Data are presented as means ± SEM (n=4) with *P<0.05, **P<0.01, ****P<0.0001 by the Student's t-test.
Figure 6.
Inhibition of GLI1 and stimulation of involucrin expression by vitamin D3 hydroxyderivatives in the A431 human carcinoma cell line. (A) Immunohistochemistry panel showing inhibition of GLI1 (green, marked by arrows) in cells treated with 10−7 M of selected secosteroids in comparison with the vehicle (ethanol) control, for 24 h. Cell nuclei are red (counterstained with propidium iodide). Scale bar=100 µm. (B) Quantification was performed as described in the legend to Fig. 5 and relative values are presented in as means ± SD (n=5) with **P<0.01, ***P<0.001 by Student's t-test. Stimulation of involucrin expression by 10−7 M of the secosteroids in comparison with the vehicle (ethanol) control. After 24 h of incubation cells were harvested, fixed in 2% PFA, stained with anti-involucrin antibody and read with a flow cytometer. Data are presented as (C) the number of positive events (FL-1 or green cells), (D) forward scatter (relative to cell size), or (E) side scatter (relative to cell granularity). Data are presented as means ± SD (n=3) with *P<0.05, **P<0.01, ***P<0.001 by the Student's t-test. Histograms (representative flow chart for each treatment) supporting evidence for the reported quantification is presented in Fig. S3.
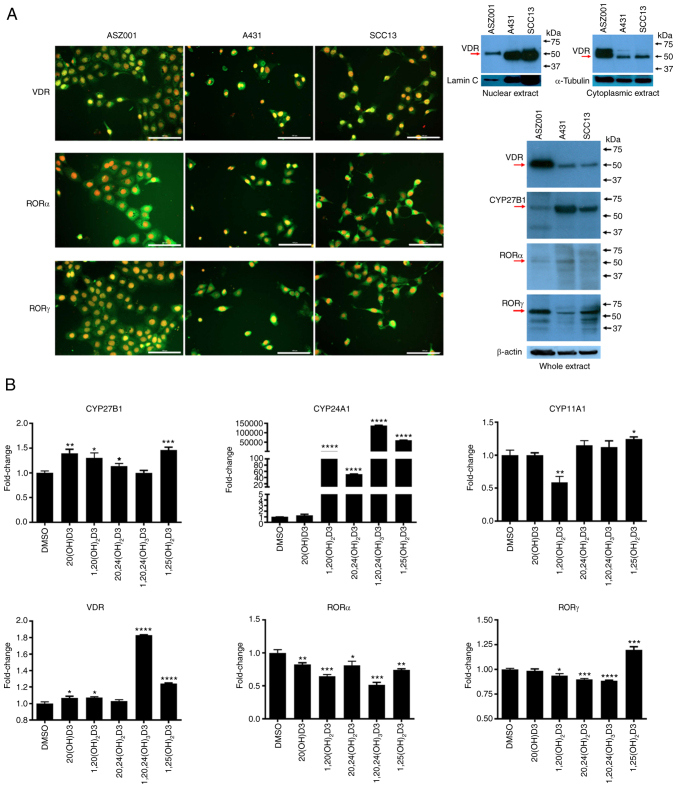
SCC and BCC lines expressed VDR and RORα and γ, which are receptors for vitamin D3 hydroxyderivatives, as well as is the C1α hydroxylase CYP27B1 (Fig. 7A and B). The relative expression of VDR and RORγ in cell extracts was the highest in the ASZ0001 line with RORα being similar in the three lines. CYP27B1 expression was highest in the A431 cells and lowest in the ASZ001 cell extracts (Fig. 7A). The nuclear receptors showed both a cytoplasmic and nuclear staining pattern, while western blotting showed predominant location of the VDR in the cytoplasm of the ASZ001 line (Fig. 7A). The effects of representative vitamin D3 hydroxyderivatives on the gene expression of vitamin D inactivating (Cyp24A1) and activating enzymes (Cyp11a1 and CYP27b1) and nuclear receptors (Vdr, Rora and Rorc) were also tested (Fig. 7B). As expected, the secosteroids with a C1α(OH) showed the strongest stimulation of the expression of Cyp24a1. A smaller stimulation of Cyp27b1 expression (up to 1.5-fold) was seen with all the secosteroids tested except 1,20,24(OH)3D3 which showed no effect. Only a marginal effect was observed for Cyp11a1 expression with 1,20(OH)2D3 decreasing it and 1,25(OH)2D3 increasing it. The majority of the vitamin D3 hydroxyderivatives tested stimulated Vdr gene expression to some degree, with 1,20,24(OH)3D3 showing the strongest effect (1.8 fold). All the secosteroids had an inhibitory effect on Rora. The effects on Rorc were small and variable, mainly inhibiting expression but stimulating it in the case of 1,25(OH)2D3 (Fig. 7B).
Figure 7.
Expression of nuclear receptors for vitamin D3 hydroxyderivatives and CYP enzymes involved in vitamin D metabolism in murine ASZ001, human A431 and human SCC13 carcinoma lines. (A) Immunofluorescence detection (left panel) was performed using antibodies against VDR (MA1-710) and RORα and RORγ (54). The antigen is in green, while cell nuclei are red-counterstained with propidium iodide; scale bar=100 µm. Right panel shows detection of VDR and RORα and RORγ by western blotting (arrows) using specific anti-receptor antibodies (see Materials and methods) for isolated cytoplasmic or nuclear fractions (VDR) from the cells or whole extracts (CYP27B1, RORα and RORγ). Human hepatoma and human melanoma SKMEL-188 cells were used as positive controls for RORα and RORγ. Loading was evaluated using antibodies against lamin C and α-tubulin for nuclear or cytoplasmic fractions, respectively, while with anti-β-actin for whole extracts. (B) shows expression at the mRNA level of Cyp27b1, Cyp24a1, Cyp11a1, Vdr, Rora and Rorc, respectively in ASZ001 murine carcinoma line treated with 10−7 M of the secosteroids listed on the x-axis. Data represent fold change, using β-actin as a housekeeping gene and are shown as means ± SEM (n=4) with *P<0.05, **P<0.01, ***P<0.001, ****P<0.0001 by Student's t-test. ROR, retinoid-related orphan receptor; VDR, vitamin D receptor.
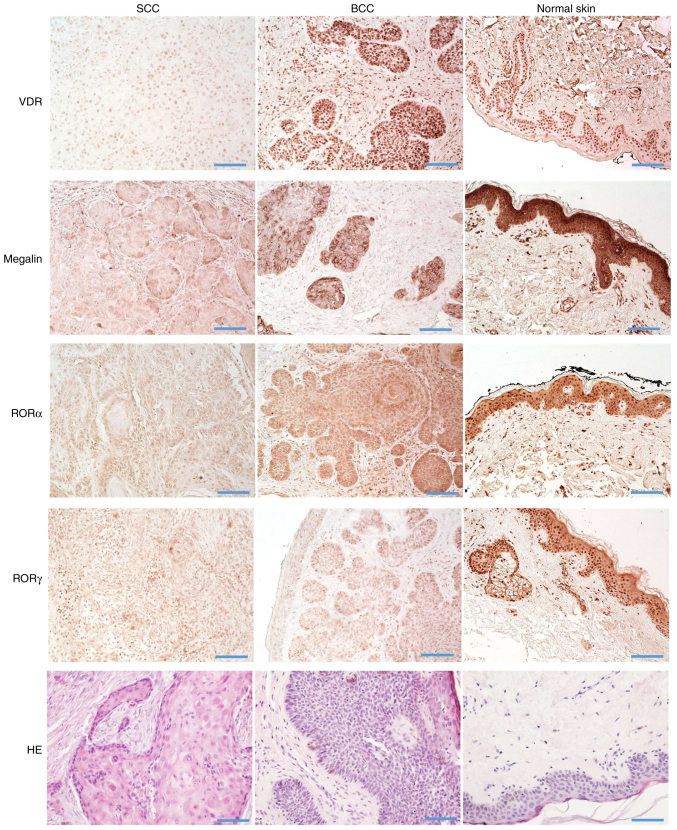
The relative expression of the above nuclear receptors and megalin/LRP2 in normal skin (n=35), BCC (n=12), SSC in situ (n=22) and SCC (n=14) were analyzed by immunohistochemical staining. The characteristics of samples analyzed in this study are presented in Table SI. VDR, RORα and RORγ showed mostly nuclear staining, with very faint cytoplasmic staining in normal, peritumoral and cancerous tissues (Fig. 8). Megalin/LRP2 was localized mostly in the cytoplasm with less expression on cell membranes. Megalin/LRP2 was also found in normal, peritumoral and cancerous tissues (Fig. 8).
Figure 8.
Immunohistochemical detection of VDR, RORα, RORγ, megalin and hematoxylin and eosin stained sections of human SCC (left column), BCC (middle column) and normal skin (right column) on archival formalin-fixed paraffin-embedded sections. Scale bar=100 µm. Immunohistochemistry was performed on the on archival formalin-fixed paraffin-embedded sections. The methodology for IHC is described in the Materials and methods and with flow chart in Fig. S2. SCC, squamous cell carcinomas; BCC, basal cell carcinomas.
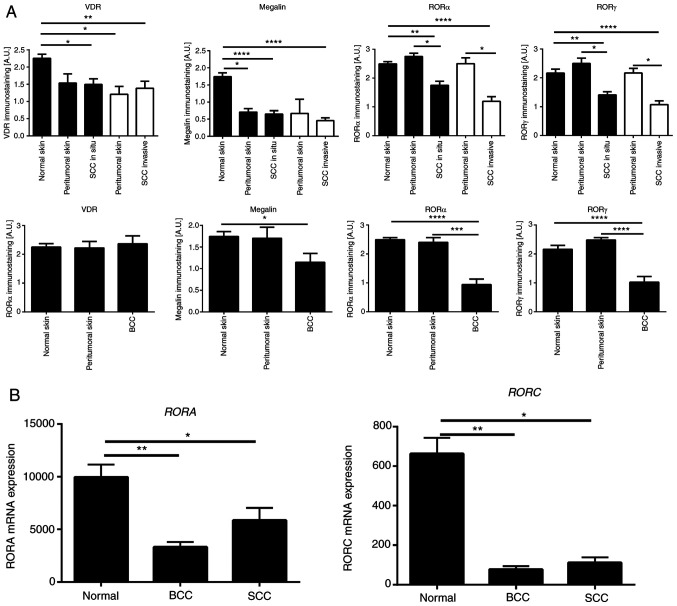
Semiquantitative analysis of the VDR and megalin/LRP2 expression showed similar levels of immunostaining in SCC in situ and invasive and unaffected peritumoral skin; however, their expression was significantly lower in comparison with normal control skin samples (Fig. 9A). Compared to BCC, the VDR expression level was similar in normal and peritumoral skin and BCC samples (Fig. 9). On the other hand, megalin/LRP2 showed significantly lower expression levels in BCC in comparison with normal and peritumoral skin (Fig. 9A). RORα and RORγ expression in peritumoral skin was similar to normal skin, while their expression was significantly reduced in SCC (in situ and invasive) and BCC (Fig. 9A). This trend was also found for the mRNA expression of RORA and RORC (Fig. 9B) using the genomic data from the public repository (Gene Expression Omnibus, accession number GSE7553).
Figure 9.
Quantitative analysis of nuclear receptor expression in SCC and BCC. (A) Quantitative comparison of immunostaining of VDR, RORα, RORγ and megalin in SCC (n=14), SCC in situ (n=22), BCC (n=12), normal (n=35) and peritumoral skin samples. Data are presented as mean values ± SD. Statistically significant differences were determined with ANOVA followed by Dunn's multiple comparisons test with *P<0.05, **P<0.01, with ***P<0.001, ****P<0.0001. The immunohistochemical stained archival formalin-fixed paraffin-embedded sections were used for quantifications as described in the Materials and methods. (B) Quantitative comparison of mRNA expression of RORA (probe 226682_at) and RORC (probe 228806_at) in SCC (n=11), BCC (n=15) and normal skin (n=4) was performed using data from the genomic repository (Gene Expression Omnibus, accession number GSE7553 http://www.ncbi.nlm.nih.gov/geo). Data are shown as means ± SD. Statistically significant differences were determined with the ANOVA followed by Dunn's multiple comparisons test with *P<0.05, **P<0.01. SCC, squamous cell carcinomas; BCC, basal cell carcinomas; ROR, retinoid-related orphan receptor; VDR, vitamin D receptor.
Discussion
The present study demonstrated that active forms of vitamin D3, including classical 1,25(OH)2D3 and novel CYP11A1-derived hydroxyderivatives, show in vitro anticancer activities against human A431- and SCC13- and murine ASZ001-carcinoma cell lines as measured by cell proliferation assays and colony- and spheroid-formation assays. While the anti-tumor effects against NMSC of 1,25(OH)2D3 were expected (27,77,86-92), the above data are the first reports on the inhibitory effects of CYP11A1-derived D3-hydroxyderivates on cutaneous lines of SCC and BCC. These data are also consistent with the ability of CYP11A1-derived vitamin D hydroxyderivatives to inhibit proliferation of primary and immortalized non-tumorigenic epidermal keratinocytes (51,55,93) and their anti-cancer properties in oral squamous cell carcinoma (80) and melanoma (94-96). The significance of these findings is emphasized by the lack or low calcemic activities of the best characterized of CYP11A1-derived hydroxyderivatives, namely 20(OH)D3, 20,23(OH)2D3 and 1,20(OH)2D3, and their lack of measurable toxicity at pharmacological doses (39). Furthermore, they have been identified in the human body (29,31,34,45,97,98) and are considered as natural products (35). Thus, CYP11A1-derived hydroxyderivatives of vitamin D are excellent candidates for principal or adjuvant therapeutics in the treatment of cutaneous SCC and BCC.
Some differences in the efficacies of the vitamin D3 hydroxyderivatives were observed depending on the cell line and the positions of the hydroxyl groups on the secosteroids, particularly the presence of the C1α-hydroxyl group. While the anti-proliferative and anti-tumor effects of D3 hydroxyderivatives were similar in both SCC lines, compounds with a C1α(OH) showed higher efficacy in the BCC line for spheroid formation. These differences can be rationalized by significantly higher expression of the VDR and lower expression of CYP27B1 in the ASZ001 line in comparison with A431 and SCC13 lines. Specifically, the VDR shows high selectivity for 1,25(OH)2D3 (48,99) and other C1α-hydroxyderivatives of D3 (52,53,55). Thus, higher levels of VDR and its greater level in the cytoplasmic fraction of ASZ001 cells indicated its relatively high availability in this BCC line for binding of C1α-hydroxyderivatives, necessary for its translocation to the nucleus and induction of transcriptional activity. Furthermore, the relatively low expression of CYP27B1 in these cells pointed to less efficient hydroxylation of CYP11-derived hydroxyderivatives that lack a C1α(OH), thus potentiating the difference between secosteroids with and without the C1α (OH).
D3-hydroxyderivatives can also activate other nuclear and non-nuclear receptors besides the VDR (42,100). Specifically, CYP11A1-derived D hydroxyderivatives act as inverse agonists on ROR α and γ (54,55), which are expressed in these lines, providing additional regulatory targets. This is further substantiated by our study in which knocking out RORγ in murine fibroblasts reverses the antiproliferative and anti-fibrotic effects of D3 hydroxyderivatives on these phenotypic traits (56). In other tumor models, the expression of these receptors decrease during melanoma progression (59) and there is a positive correlation between the expression of RORs and the expression of HIF-1α (hypoxia-inducible factor 1α) (60). Notably, D3-hydroxyderivatives can affect gene expression of enzymes involved in activation or inactivation of active forms of D3, as well as their receptors (Fig. 7B). Specifically, they caused a small stimulation of CYP27B1 expression in a manner unrelated to the absence or presence of a C1α(OH). They significantly stimulated CYP24A1 [an inactivating enzyme (101,102)] expression with selectivity for compounds containing a C1α(OH). This further substantiated the selectivity of the derivatives containing a C1α(OH) for the VDR, since CYP24A1 is a well-established downstream target of the VDR (16,103). There was little effect on CYP11A1 expression and small but variable stimulation of VDR expression by the various secosteroids. This is consistent with previous reports showing that VDR expression can be stimulated by active forms of vitamin D (30,104). All compounds inhibited RORA expression and the majority also inhibited RORC expression with the exception of 1,25(OH)2D3, which stimulated the expression of this gene. In summary, the actions of hydroxyderivatives of D3 are complex involving both VDR-dependent and independent (RORs) mechanisms. Their actions may also be influenced by their in vivo metabolism by vitamin D-activating and inactivating enzymes and by their abilities to regulate these enzymes, as well as their abilities to regulate expression of their target receptors. This opens exciting possibilities for future studies.
Application of vitamin D and of 1,25(OH)2D3 can inhibit BCC development and growth through inhibition Hh signaling (27,77,87,88). Similarly, the authors have shown that D3 hydroxyderivatives can inhibit Hh signaling and β-catenin expression in oral SCC (80), while another study has shown that 1,25(OH)2D3 inhibits β-catenin signaling in epidermal keratinocytes (105). In agreement with these studies the present study showed that classical and CYP11A1-derived D3 hydroxyderivatives can inhibit GLI1 and β-catenin expression in the murine ASZ001 cell line and Gli1 in the human A431 line, identifying these pathways as realistic targets for bioregulation.
Immunocytochemistry performed on human biopsies of SCC in situ, invasive SCC and BCC showed nuclear expression of all three receptors. This finding is consistent with previous reports on the VDR expression in NMSCs biopsies (90,106). However, some differences in the level of immunoreactivity require explanation. Studies by Reichrath et al (90,106) report an increase in VDR immunoreactivity in SCC and BCC compared with normal skin. The present study showed a slight but significant decrease in VDR expression in SCC in comparison with normal skin and no difference in VDR expression between BCC and control skin. These quantitative differences could be secondary to differences in the patient population, fixation protocols, tissue processing or different antibodies used. However, in agreement with Reichrath et al (90,106), the present study did not observe any marked differences between different types of SCC and BCC and observed an inhibition of SCC growth in vitro by D3-hydroxyderivatives. With respect to RORα and γ, these receptors have a similar expression in peritumoral and normal skin and show comparatively lower expression in SCC and BCC. This pattern is consistent with decreased expression of the receptors observed during the progression of melanocytic lesions to a more malignant phenotype (59) or with decreased expression of corresponding genes in SCC and BCC as evaluated from the public genomics data repository (GSE7553). RORs are targets for CYP11A1-derived hydroxyderivatives (54,55). Therefore, a decrease in their expression may reduce the anti-tumor effects of the hydroxyderivatives via their inverse agonist activity on RORs. Finally, the present study observed decreased expression in the SCC and BCC samples of transmembrane glycoprotein-LRP2/megalin, which is implicated in vitamin D3 transport into the cell (66-68). The decrease in expression of RORs, VDR and LRP2/megalin was recently reported in hyperproliferative/inflammatory diseases, such as psoriasis (84). Thus, disturbed expression of LRP2/megalin, VDR, RORα and RORγ in skin cancerous lesions suggests defects in the vitamin D endocrine system in cancerous tissue that could facilitate tumor growth. Their detection in all SCC and BCC samples indicated that they can serve as realistic targets for therapeutic activity of novel vitamin D hydroxyderivatives. However, it should be noted that not only cancerous keratinocytes express the receptors for vitamin D and are targets for CYP11A1-derived hydroxymetabolites of vitamin D but they also regulate a differentiation program in normal epidermal keratinocytes. Specifically, hydroxymetabolites of vitamin can induce differentiation, inhibit proliferation, act as photoprotectants and as anti-aging and anti-inflammatory factors in normal epidermal keratinocytes (51,53,93,107,108).
In conclusion, the present study identified several CYP11A1-derived vitamin D analogs which are endogenously produced (29,31,33,34,45,98), as potential cutaneous anti-cancer therapeutics. Their anti-cancer activity can be mediated via different mechanisms. It is well known that 1,25(OH)2D3 promotes the differentiation of keratinocytes (93,109). The present study demonstrated that 20(OH D3, 1,20(OH)2D3 and 1,25(OH)2D3 also stimulated involucrin expression in skin cancer cells. The other mechanisms relate to effects on Hh/GLI1 and β-catenin signaling pathways uncontrolled activities of which promote cancer development and progression (107,110). The present study showed that GLI1 and β-catenin are downregulated following treatment with CYP11A1-derived D3 hydroxyderivatives. Expression of nuclear receptors for these hydroxyderivatives were further observed in all samples of SCC and BCC, which potentially can be targeted in vivo for anti-tumor activity. This is the first time, to the best of the authors' knowledge, that a range of CYP11A1-derived vitamin D hydroxyderivatives have been tested against cutaneous SCC and BCC. The finding that RORs are expressed in skin cancer cells is also new. It has previously been shown that 1,25(OH)2D3 inhibits the growth of BCC in mice through the activation of the VDR and inhibition of Hh signaling, in a VDR-independent manner, with the effects being stronger than those of the cyclopamine (88). It was also reported that D3 inhibits Hh signaling and growth of murine BCC cells to a similar degree as cyclopamine with an effect independent of the VDR (77). Notably, topical application of the D3 prohormone can inhibit UVB-induced BCC with orally delivered D3 having no effect (27). In addition, calcipotriol (analog of 1,25(OH)2D3) inhibits cutaneous cancerogenesis in mice (86) and in clinical studies shows a synergistic effect with other therapeutic modalities against actinic keratosis (86,111). While calcemic and other toxic effects place limits on the therapeutic use of 1,25(OH)2D3 or its synthetic derivatives at pharmacological doses, major CYP11A1-derived vitamin D derivatives are noncalcemic and non-toxic or show low calcemic effects at supra-pharmacological doses (37,39,63,64). They have also been detected in natural products (35) and show potent protective properties against UVB-induced damage (43,44). Besides the VDR they can act on other nuclear receptors (42,57,112), including RORs (54), extending the therapeutic possibilities for their use. The present study provided exciting challenges for medicinal chemistry to develop more receptor-specific ligands based on the lead structures of the CYP11A1-derived hydroxyderivatives.
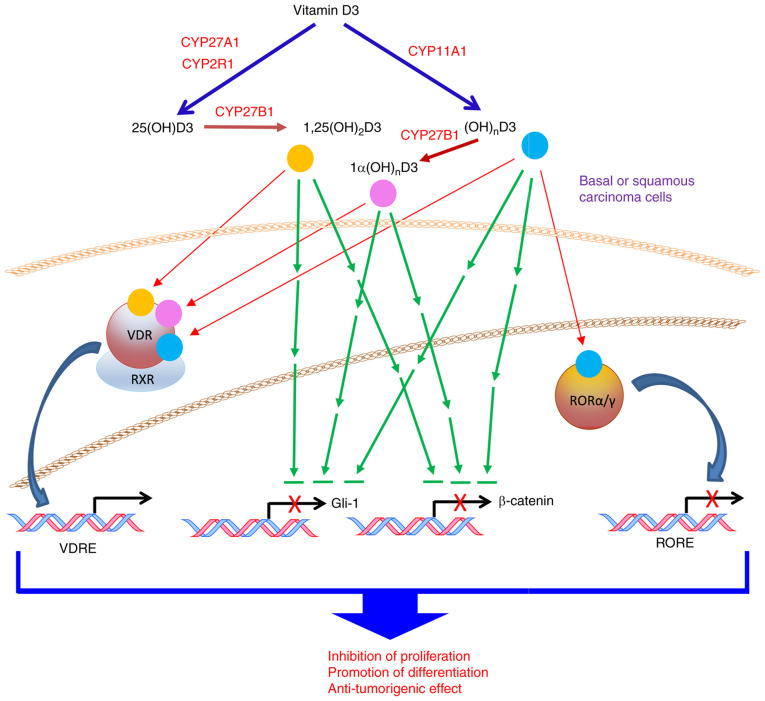
In summary, the present study identified CYP11A1-derived vitamin D hydroxyderivatives as excellent candidates for therapy or prevention of NMSCs, which can act on distinct nuclear receptors and inhibit GLI1 and β-catenin signaling pathways as a part of their anti-cancer activity with a proposed mechanism of action shown in Fig. 10.
Figure 10.
Proposed mechanism of action of novel vitamin D3 hydroxyderivatives. ROR, retinoid-related orphan receptor; VDR, vitamin D receptor.
Supplementary Data
Acknowledgments
Not applicable.
Funding Statement
The present study was in part supported by the NIH (grant nos. 1R01AR073004, R01AR071189 and R21AI149267-01A1) and VA merit (grant no. 1I01BX004293-01A1) to ATS, NIH/NCI grant nos. R21ES034595, R01CA193885 and P01CA210946 to CAE, NIH/NCI grant nos. R01CA193609 and R01CA240447 to WL, the O'Neal Comprehensive Cancer Center Core grant (grant no. P30CA13148) and by the Intramural Research Program of the NIEHS, (grant no. NIH Z01-ES-101585) to AMJ). The contents of the article are solely the responsibility of the authors and do not necessarily represent the official views of the NIH.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Authors' contributions
ATS conceived and supervised the study, analyzed the data and wrote, revised and edited the manuscript. AAB performed the experiments, analyzed the data and wrote, revised and edited the manuscript. TKK performed the experiments, analyzed the data and drafted the manuscript. MME performed the experiments and analyzed the data. ZJ performed the experiments, analyzed the data and drafted the manuscript. SQ performed the experiments and analyzed the data. RMS performed the experiments, analyzed the data and drafted the manuscript. ASWO performed the experiments, analyzed the data and drafted the manuscript. CL performed the experiments, analyzed the data and drafted the manuscript. EP performed the experiments and analyzed the data. WL synthesized vitamin D derivatives, drafted the manuscript and revised and edited the manuscript. AMJ provided anti-RORs antibodies, analyzed the data and drafted, revised and edited the manuscript. RCT synthesized vitamin D derivatives and drafted, revised and edited the manuscript. EKYT synthesized vitamin D derivatives. CE analyzed the data and drafted, revised and edited the manuscript. MA analyzed data, provided cell lines and drafted, revised and edited the manuscript. ATS and AAB confirm the authenticity of all the raw data. All authors read and approved the final version of the manuscript.
Ethics approval and consent to participate
The authors declare that this investigation was carried out following the rules of the Declaration of Helsinki of 1975 (revised in 2008) and this study was approved by the Institutional Review Board of the University of Alabama at Birmingham under IRB-940831016 (OCCC Tissue Procurement CORE Facility) and IRB-00000726 (Title E150427002; Dr. A. Slominski PI).
Patient consent for publication
The IRB of the University of Alabama at Birmingham, which gave its permission for conducting this study, waived the requirement to obtain patients' informed consent for this research.
Competing interests
The authors declare that they have no competing interests.
References
- 1.Slominski AT, Zmijewski MA, Plonka PM, Szaflarski JP, Paus R. How UV light touches the brain and endocrine system through skin, and why. Endocrinology. 2018;159:1992–2007. doi: 10.1210/en.2017-03230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Brash DE. UV signature mutations. Photochem Photobiol. 2015;91:15–26. doi: 10.1111/php.12377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wondrak GT. Let the sun shine in: Mechanisms and potential for therapeutics in skin photodamage. Curr Opin Investig Drugs. 2007;8:390–400. [PubMed] [Google Scholar]
- 4.D'Orazio J, Jarrett S, Amaro-Ortiz A, Scott T. UV radiation and the skin. Int J Mol Sci. 2013;14:12222–12248. doi: 10.3390/ijms140612222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bickers DR, Athar M. Oxidative stress in the pathogenesis of skin disease. J Invest Dermatol. 2006;126:2565–2575. doi: 10.1038/sj.jid.5700340. [DOI] [PubMed] [Google Scholar]
- 6.Slominski AT, Zmijewski MA, Semak I, Zbytek B, Pisarchik A, Li W, Zjawiony J, Tuckey RC. Cytochromes p450 and skin cancer: Role of local endocrine pathways. Anticancer Agents Med Chem. 2014;14:77–96. doi: 10.2174/18715206113139990308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Athar M, Walsh SB, Kopelovich L, Elmets CA. Pathogenesis of nonmelanoma skin cancers in organ transplant recipients. Arch Biochem Biophys. 2011;508:159–163. doi: 10.1016/j.abb.2011.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lo HL, Nakajima S, Ma L, Walter B, Yasui A, Ethell DW, Owen LB. Differential biologic effects of CPD and 6-4PP UV-induced DNA damage on the induction of apoptosis and cell-cycle arrest. BMC Cancer. 2005;5:135. doi: 10.1186/1471-2407-5-135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wondrak GT, Roberts MJ, Jacobson MK, Jacobson EL. 3-hydroxypyridine chromophores are endogenous sensitizers of photooxidative stress in human skin cells. J Biol Chem. 2004;279:30009–30020. doi: 10.1074/jbc.M404379200. [DOI] [PubMed] [Google Scholar]
- 10.Slominski AT, Zmijewski MA, Skobowiat C, Zbytek B, Slominski RM, Steketee JD. Sensing the environment: Regulation of local and global homeostasis by the skin's neuroendocrine system. Adv Anat Embryol Cell Biol. 2012;212:v–vii. 1–115. doi: 10.1007/978-3-642-19683-6_1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lim HW, Collins SAB, Resneck JS, Jr, Bolognia JL, Hodge JA, Rohrer TA, Van Beek MJ, Margolis DJ, Sober AJ, Weinstock MA, et al. The burden of skin disease in the United States. J Am Acad Dermatol. 2017;76:958–972.e2. doi: 10.1016/j.jaad.2016.12.043. [DOI] [PubMed] [Google Scholar]
- 12.Carlson JA, Slominski A, Murphy MJ, Wilson V. Evidence of skin field cancerization. In: Dakubo G, editor. Field Cancerization: Basic Science and Clical Applications. Nova Science Publishers Inc; 2011. pp. 317–369. [Google Scholar]
- 13.Holick MF. Vitamin D: A millenium perspective. J Cell Biochem. 2003;88:296–307. doi: 10.1002/jcb.10338. [DOI] [PubMed] [Google Scholar]
- 14.Holick MF, Tian XQ, Allen M. Evolutionary importance for the membrane enhancement of the production of vitamin D3 in the skin of poikilothermic animals. Proc Natl Acad Sci USA. 1995;92:3124–3126. doi: 10.1073/pnas.92.8.3124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bikle DD. Vitamin D and the skin. J Bone Miner Metab. 2010;28:117–130. doi: 10.1007/s00774-009-0153-8. [DOI] [PubMed] [Google Scholar]
- 16.Holick MF. Vitamin D deficiency. N Engl J Med. 2007;357:266–281. doi: 10.1056/NEJMra070553. [DOI] [PubMed] [Google Scholar]
- 17.Bikle DD. Vitamin D metabolism and function in the skin. Mol Cell Endocrinol. 2011;347:80–89. doi: 10.1016/j.mce.2011.05.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Plum LA, DeLuca HF. Vitamin D, disease and therapeutic opportunities. Nat Rev Drug Discov. 2010;9:941–955. doi: 10.1038/nrd3318. [DOI] [PubMed] [Google Scholar]
- 19.Bikle DD. Vitamin D receptor, UVR, and skin cancer: A potential protective mechanism. J Invest Dermatol. 2008;128:2357–2361. doi: 10.1038/jid.2008.249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Elias PM. Structure and function of the stratum corneum extracellular matrix. J Invest Dermatol. 2012;132:2131–2133. doi: 10.1038/jid.2012.246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bikle DD. Vitamin D: Newly discovered actions require reconsideration of physiologic requirements. Trends Endocrinol Metab. 2010;21:375–384. doi: 10.1016/j.tem.2010.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Indra AK, Castaneda E, Antal MC, Jiang M, Messaddeq N, Meng X, Loehr CV, Gariglio P, Kato S, Wahli W, et al. Malignant transformation of DMBA/TPA-induced papillomas and nevi in the skin of mice selectively lacking retinoid-X-receptor alpha in epidermal keratinocytes. J Invest Dermatol. 2007;127:1250–1260. doi: 10.1038/sj.jid.5700672. [DOI] [PubMed] [Google Scholar]
- 23.Dixon KM, Tongkao-On W, Sequeira VB, Carter SE, Song EJ, Rybchyn MS, Gordon-Thomson C, Mason RS. Vitamin D and death by sunshine. Int J Mol Sci. 2013;14:1964–1977. doi: 10.3390/ijms14011964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Song EJ, Gordon-Thomson C, Cole L, Stern H, Halliday GM, Damian DL, Reeve VE, Mason RS. 1α,25-Dihydroxyvitamin D3 reduces several types of UV-induced DNA damage and contributes to photoprotection. J Steroid Biochem Mol Biol. 2013;136:131–138. doi: 10.1016/j.jsbmb.2012.11.003. [DOI] [PubMed] [Google Scholar]
- 25.Bikle DD, Elalieh H, Welsh J, Oh D, Cleaver J, Teichert A. Protective role of vitamin D signaling in skin cancer formation. J Steroid Biochem Mol Biol. 2013;136:271–279. doi: 10.1016/j.jsbmb.2012.09.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Demetriou SK, Ona-Vu K, Teichert AE, Cleaver JE, Bikle DD, Oh DH. Vitamin D receptor mediates DNA repair and is UV inducible in intact epidermis but not in cultured keratinocytes. J Invest Dermatol. 2012;132:2097–2100. doi: 10.1038/jid.2012.107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Makarova A, Wang G, Dolorito JA, Kc S, Libove E, Epstein EH., Jr Vitamin D3 produced by skin exposure to UVR inhibits murine basal cell carcinoma carcinogenesis. J Invest Dermatol. 2017;137:2613–2619. doi: 10.1016/j.jid.2017.05.037. [DOI] [PubMed] [Google Scholar]
- 28.Slominski AT, Li W, Kim TK, Semak I, Wang J, Zjawiony JK, Tuckey RC. Novel activities of CYP11A1 and their potential physiological significance. J Steroid Biochem Mol Biol. 2015;151:25–37. doi: 10.1016/j.jsbmb.2014.11.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Slominski AT, Kim TK, Li W, Postlethwaite A, Tieu EW, Tang EKY, Tuckey RC. Detection of novel CYP11A1-derived secosteroids in the human epidermis and serum and pig adrenal gland. Sci Rep. 2015;5:14875. doi: 10.1038/srep14875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Tuckey RC, Li W, Shehabi HZ, Janjetovic Z, Nguyen MN, Kim TK, Chen J, Howell DE, Benson HA, Sweatman T, et al. Production of 22-hydroxy metabolites of vitamin d3 by cytochrome p450scc (CYP11A1) and analysis of their biological activities on skin cells. Drug Metab Dispos. 2011;39:1577–1588. doi: 10.1124/dmd.111.040071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Slominski AT, Kim TK, Shehabi HZ, Semak I, Tang EK, Nguyen MN, Benson HA, Korik E, Janjetovic Z, Chen J, et al. In vivo evidence for a novel pathway of vitamin D3 metabolism initiated by P450scc and modified by CYP27B1. FASEB J. 2012;26:3901–3915. doi: 10.1096/fj.12-208975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Tang EK, Chen J, Janjetovic Z, Tieu EW, Slominski AT, Li W, Tuckey RC. Hydroxylation of CYP11A1-derived products of vitamin D3 metabolism by human and mouse CYP27B1. Drug Metab Dispos. 2013;41:1112–1124. doi: 10.1124/dmd.113.050955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Slominski AT, Kim TK, Shehabi HZ, Tang EK, Benson HA, Semak I, Lin Z, Yates CR, Wang J, Li W, Tuckey RC. In vivo production of novel vitamin D2 hydroxy-derivatives by human placentas, epidermal keratinocytes, Caco-2 colon cells and the adrenal gland. Mol Cell Endocrinol. 2014;383:181–192. doi: 10.1016/j.mce.2013.12.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Slominski AT, Kim TK, Li W, Tuckey RC. Classical and non-classical metabolic transformation of vitamin D in dermal fibroblasts. Exp Dermatol. 2016;25:231–232. doi: 10.1111/exd.12872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kim TK, Atigadda V, Brzeminski P, Fabisiak A, Tang EKY, Tuckey RC, Slominski AT. Detection of 7-dehydrocholesterol and vitamin D3 derivatives in honey. Molecules. 2020;25:2583. doi: 10.3390/molecules25112583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Slominski AT, Janjetovic Z, Kim TK, Wright AC, Grese LN, Riney SJ, Nguyen MN, Tuckey RC. Novel vitamin D hydroxyderivatives inhibit melanoma growth and show differential effects on normal melanocytes. Anticancer Res. 2012;32:3733–3742. [PMC free article] [PubMed] [Google Scholar]
- 37.Wang J, Slominski A, Tuckey RC, Janjetovic Z, Kulkarni A, Chen J, Postlethwaite AE, Miller D, Li W. 20-Hydroxyvitamin D3 inhibits proliferation of cancer cells with high efficacy while being non-toxic. Anticancer Res. 2012;32:739–746. [PMC free article] [PubMed] [Google Scholar]
- 38.Janjetovic Z, Brozyna AA, Tuckey RC, Kim TK, Nguyen MN, Jozwicki W, Pfeffer SR, Pfeffer LM, Slominski AT. High basal NF-κB activity in nonpigmented melanoma cells is associated with an enhanced sensitivity to vitamin D3 derivatives. Br J Cancer. 2011;105:1874–1884. doi: 10.1038/bjc.2011.458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Slominski AT, Janjetovic Z, Fuller BE, Zmijewski MA, Tuckey RC, Nguyen MN, Sweatman T, Li W, Zjawiony J, Miller D, et al. Products of vitamin D3 or 7-dehydrocholesterol metabolism by cytochrome P450scc show anti-leukemia effects, having low or absent calcemic activity. PLoS One. 2010;5:e9907. doi: 10.1371/journal.pone.0009907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Slominski A, Kim TK, Zmijewski MA, Janjetovic Z, Li W, Chen J, Kusniatsova EI, Semak I, Postlethwaite A, Miller DD, et al. Novel vitamin D photoproducts and their precursors in the skin. Dermatoendocrinol. 2013;5:7–19. doi: 10.4161/derm.23938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Wasiewicz T, Szyszka P, Cichorek M, Janjetovic Z, Tuckey RC, Slominski AT, Zmijewski MA. Antitumor effects of vitamin D analogs on hamster and mouse melanoma cell lines in relation to melanin pigmentation. Int J Mol Sci. 2015;16:6645–6667. doi: 10.3390/ijms16046645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Slominski AT, Chaiprasongsuk A, Janjetovic Z, Kim TK, Stefan J, Slominski RM, Hanumanthu VS, Raman C, Qayyum S, Song Y, et al. Photoprotective properties of vitamin D and lumisterol hydroxyderivatives. Cell Biochem Biophys. 2020;78:165–180. doi: 10.1007/s12013-020-00913-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Chaiprasongsuk A, Janjetovic Z, Kim TK, Tuckey RC, Li W, Raman C, Panich U, Slominski AT. CYP11A1-derived vitamin D3 products protect against UVB-induced inflammation and promote keratinocytes differentiation. Free Radic Biol Med. 2020;155:87–98. doi: 10.1016/j.freeradbiomed.2020.05.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Chaiprasongsuk A, Janjetovic Z, Kim TK, Jarrett SG, D'Orazio JA, Holick MF, Tang EKY, Tuckey RC, Panich U, Li W, Slominski AT. Protective effects of novel derivatives of vitamin D3 and lumisterol against UVB-induced damage in human keratinocytes involve activation of Nrf2 and p53 defense mechanisms. Redox Biol. 2019;24:101206. doi: 10.1016/j.redox.2019.101206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Slominski AT, Janjetovic Z, Kim TK, Wasilewski P, Rosas S, Hanna S, Sayre RM, Dowdy JC, Li W, Tuckey RC. Novel non-calcemic secosteroids that are produced by human epidermal keratinocytes protect against solar radiation. J Steroid Biochem Mol Biol. 2015;148:52–63. doi: 10.1016/j.jsbmb.2015.01.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Tongkao-on W, Carter S, Reeve VE, Dixon KM, Gordon-Thomson C, Halliday GM, Tuckey RC, Mason RS. CYP11A1 in skin: An alternative route to photoprotection by vitamin D compounds. J Steroid Biochem Mol Biol. 2015;148:72–78. doi: 10.1016/j.jsbmb.2014.11.015. [DOI] [PubMed] [Google Scholar]
- 47.Bikle D, Christakos S. New aspects of vitamin D metabolism and action-addressing the skin as source and target. Nat Rev Endocrinol. 2020;16:234–252. doi: 10.1038/s41574-019-0312-5. [DOI] [PubMed] [Google Scholar]
- 48.Bikle DD. Vitamin D: Newer concepts of its metabolism and function at the basic and clinical level. J Endocr Soc. 2020;4:bvz038. doi: 10.1210/jendso/bvz038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Reichrath J, Zouboulis CC, Vogt T, Holick MF. Targeting the vitamin D endocrine system (VDES) for the management of inflammatory and malignant skin diseases: An historical view and outlook. Rev Endocr Metab Disord. 2016;17:405–417. doi: 10.1007/s11154-016-9353-4. [DOI] [PubMed] [Google Scholar]
- 50.Carlberg C. Vitamin D genomics: From in vitro to in vivo. Front Endocrinol (Lausanne) 2018;9:250. doi: 10.3389/fendo.2018.00250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Slominski AT, Kim TK, Janjetovic Z, Tuckey RC, Bieniek R, Yue J, Li W, Chen J, Nguyen MN, Tang EK, et al. 20-Hydroxyvitamin D2 is a noncalcemic analog of vitamin D with potent antiproliferative and prodifferentiation activities in normal and malignant cells. Am J Physiol Cell Physiol. 2011;300:C526–C541. doi: 10.1152/ajpcell.00203.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Kim TK, Wang J, Janjetovic Z, Chen J, Tuckey RC, Nguyen MN, Tang EK, Miller D, Li W, Slominski AT. Correlation between secosteroid-induced vitamin D receptor activity in melanoma cells and computer-modeled receptor binding strength. Mol Cell Endocrinol. 2012;361:143–152. doi: 10.1016/j.mce.2012.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Lin Z, Marepally SR, Goh ESY, Cheng CYS, Janjetovic Z, Kim TK, Miller DD, Postlethwaite AE, Slominski AT, Tuckey RC, et al. Investigation of 20S-hydroxyvitamin D analogs and their 1α-OH derivatives as potent vitamin D3 receptor agonists with anti-inflammatory activities. Sci Rep. 2018;8:1478. doi: 10.1038/s41598-018-19183-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Slominski AT, Kim TK, Takeda Y, Janjetovic Z, Brozyna AA, Skobowiat C, Wang J, Postlethwaite A, Li W, Tuckey RC, Jetten AM. RORα and ROR γ are expressed in human skin and serve as receptors for endogenously produced noncalcemic 20-hydroxy- and 20,23-dihydroxyvitamin D. FASEB J. 2014;28:2775–2789. doi: 10.1096/fj.13-242040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Slominski AT, Kim TK, Hobrath JV, Oak ASW, Tang EKY, Tieu EW, Li W, Tuckey RC, Jetten AM. Endogenously produced nonclassical vitamin D hydroxy-metabolites act as 'biased' agonists on VDR and inverse agonists on RORα and RORγ. J Steroid Biochem Mol Biol. 2017;173:42–56. doi: 10.1016/j.jsbmb.2016.09.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Janjetovic Z, Postlethwaite A, Kang HS, Kim TK, Tuckey RC, Crossman DK, Qayyum S, Jetten AM, Slominski AT. Antifibrogenic activities of CYP11A1-derived vitamin D3-hydroxyderivatives are dependent on RORγ. Endocrinology. 2021;162:bqaa198. doi: 10.1210/endocr/bqaa198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Slominski AT, Kim TK, Janjetovic Z, Brożyna AA, Żmijewski MA, Xu H, Sutter TR, Tuckey RC, Jetten AM, Crossman DK. Differential and overlapping effects of 20,23(OH)2 D3 and 1,25(OH)2 D3 on gene expression in human epidermal keratinocytes: Identification of AhR as an alternative receptor for 20,23(OH)2 D3. Int J Mol Sci. 2018;19:3072. doi: 10.3390/ijms19103072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Markiewicz A, Brożyna AA, Podgórska E, Elas M, Urbańska K, Jetten AM, Slominski AT, Jóźwicki W, Orłowska-Heitzman J, Dyduch G, Romanowska-Dixon B. Vitamin D receptors (VDR), hydroxylases CYP27B1 and CYP24A1 and retinoid-related orphan receptors (ROR) level in human uveal tract and ocular melanoma with different melanization levels. Sci Rep. 2019;9:9142. doi: 10.1038/s41598-019-45161-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Brożyna AA, Jóźwicki W, Skobowiat C, Jetten A, Slominski AT. RORα and RORγ expression inversely correlates with human melanoma progression. Oncotarget. 2016;7:63261–63282. doi: 10.18632/oncotarget.11211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Brożyna AA, Jóźwicki W, Jetten AM, Slominski AT. On the relationship between VDR, RORα and RORγ receptors expression and HIF1-α levels in human melanomas. Exp Dermatol. 2019;28:1036–1043. doi: 10.1111/exd.14002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Brożyna AA, Hoffman RM, Slominski AT. Relevance of vitamin D in melanoma development, progression and therapy. Anticancer Res. 2020;40:473–489. doi: 10.21873/anticanres.13976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Slominski AT, Brożyna AA, Zmijewski MA, Jóźwicki W, Jetten AM, Mason RS, Tuckey RC, Elmets CA. Vitamin D signaling and melanoma: Role of vitamin D and its receptors in melanoma progression and management. Lab Invest. 2017;97:706–724. doi: 10.1038/labinvest.2017.3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Chen J, Wang J, Kim TK, Tieu EW, Tang EK, Lin Z, Kovacic D, Miller DD, Postlethwaite A, Tuckey RC, et al. Novel vitamin D analogs as potential therapeutics: Metabolism, toxicity profiling, and antiproliferative activity. Anticancer Res. 2014;34:2153–2163. [PMC free article] [PubMed] [Google Scholar]
- 64.Slominski A, Janjetovic Z, Tuckey RC, Nguyen MN, Bhattacharya KG, Wang J, Li W, Jiao Y, Gu W, Brown M, Postlethwaite AE. 20S-Hydroxyvitamin D3, noncalcemic product of CYP11A1 action on vitamin D3, exhibits potent antifibrogenic activity in vivo. J Clin Endocrinol Metab. 2013;98:E298–E303. doi: 10.1210/jc.2012-3074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Carlberg C, Molnar F. Current status of vitamin D signaling and its therapeutic applications. Curr Top Med Chem. 2012;12:528–547. doi: 10.2174/156802612799436623. [DOI] [PubMed] [Google Scholar]
- 66.Gao Y, Zhou S, Luu S, Glowacki J. Megalin mediates 25-hydroxyvitamin D3 actions in human mesenchymal stem cells. FASEB J. 2019;33:7684–7693. doi: 10.1096/fj.201802578R. [DOI] [PubMed] [Google Scholar]
- 67.Nykjaer A, Dragun D, Walther D, Vorum H, Jacobsen C, Herz J, Melsen F, Christensen EI, Willnow TE. An endocytic pathway essential for renal uptake and activation of the steroid 25-(OH) vitamin D3. Cell. 1999;96:507–515. doi: 10.1016/S0092-8674(00)80655-8. [DOI] [PubMed] [Google Scholar]
- 68.Kaseda R, Hosojima M, Sato H, Saito A. Role of megalin and cubilin in the metabolism of vitamin D(3) Ther Apher Dial. 2011;15(Suppl 1):S14–S17. doi: 10.1111/j.1744-9987.2011.00920.x. [DOI] [PubMed] [Google Scholar]
- 69.Slominski A, Semak I, Zjawiony J, Wortsman J, Li W, Szczesniewski A, Tuckey RC. The cytochrome P450scc system opens an alternate pathway of vitamin D3 metabolism. FEBS J. 2005;272:4080–4090. doi: 10.1111/j.1742-4658.2005.04819.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Tieu EW, Tang EK, Chen J, Li W, Nguyen MN, Janjetovic Z, Slominski A, Tuckey RC. Rat CYP24A1 acts on 20-hydroxyvitamin D(3) producing hydroxylated products with increased biological activity. Biochem Pharmacol. 2012;84:1696–1704. doi: 10.1016/j.bcp.2012.09.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Tang EK, Li W, Janjetovic Z, Nguyen MN, Wang Z, Slominski A, Tuckey RC. Purified mouse CYP27B1 can hydroxylate 20,23-dihydroxyvitamin D3, producing 1alpha,20,23-trihydroxyvitamin D3, which has altered biological activity. Drug Metab Dispos. 2010;38:1553–1559. doi: 10.1124/dmd.110.034389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Tuckey RC, Li W, Zjawiony JK, Zmijewski MA, Nguyen MN, Sweatman T, Miller D, Slominski A. Pathways and products for the metabolism of vitamin D3 by cytochrome P450scc. FEBS J. 2008;275:2585–2596. doi: 10.1111/j.1742-4658.2008.06406.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Tieu EW, Li W, Chen J, Baldisseri DM, Slominski AT, Tuckey RC. Metabolism of cholesterol, vitamin D3 and 20-hydroxyvitamin D3 incorporated into phospholipid vesicles by human CYP27A1. J Steroid Biochem Mol Biol. 2012;129:163–171. doi: 10.1016/j.jsbmb.2011.11.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Li W, Chen J, Janjetovic Z, Kim TK, Sweatman T, Lu Y, Zjawiony J, Tuckey RC, Miller D, Slominski A. Chemical synthesis of 20S-hydroxyvitamin D3, which shows antiproliferative activity. Steroids. 2010;75:926–935. doi: 10.1016/j.steroids.2010.05.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Lin Z, Marepally SR, Ma D, Kim TK, Oak AS, Myers LK, Tuckey RC, Slominski AT, Miller DD, Li W. Synthesis and biological evaluation of vitamin D3 metabolite 20S,23S-dihydroxyvitamin D3 and Its 23R epimer. J Med Chem. 2016;59:5102–5108. doi: 10.1021/acs.jmedchem.6b00182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Slominski A, Semak I, Wortsman J, Zjawiony J, Li W, Zbytek B, Tuckey RC. An alternative pathway of vitamin D metabolism. Cytochrome P450scc (CYP11A1)-mediated conversion to 20-hydroxyvitamin D2 and 17,20-dihydroxyvitamin D2. FEBS J. 2006;273:2891–2901. doi: 10.1111/j.1742-4658.2006.05302.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Tang JY, Xiao TZ, Oda Y, Chang KS, Shpall E, Wu A, So PL, Hebert J, Bikle D, Epstein EH., Jr Vitamin D3 inhibits hedgehog signaling and proliferation in murine basal cell carcinomas. Cancer Prev Res (Phila) 2011;4:744–751. doi: 10.1158/1940-6207.CAPR-10-0285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.So PL, Langston AW, Daniallinia N, Hebert JL, Fujimoto MA, Khaimskiy Y, Aszterbaum M, Epstein EH., Jr Long-term establishment, characterization and manipulation of cell lines from mouse basal cell carcinoma tumors. Exp Dermatol. 2006;15:742–750. doi: 10.1111/j.1600-0625.2006.00465.x. [DOI] [PubMed] [Google Scholar]
- 79.Chaudhary SC, Singh T, Talwelkar SS, Srivastava RK, Arumugam A, Weng Z, Elmets CA, Afaq F, Kopelovich L, Athar M. Erb-041, an estrogen receptor-β agonist, inhibits skin photocarcinogenesis in SKH-1 hairless mice by downregulating the WNT signaling pathway. Cancer Prev Res (Phila) 2014;7:186–198. doi: 10.1158/1940-6207.CAPR-13-0276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Oak ASW, Bocheva G, Kim TK, Brożyna AA, Janjetovic Z, Athar M, Tuckey RC, Slominski AT. Noncalcemic vitamin D hydroxyderivatives inhibit human oral squamous cell carcinoma and down-regulate hedgehog and WNT/β-catenin pathways. Anticancer Res. 2020;40:2467–2474. doi: 10.21873/anticanres.14216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Brożyna AA, Kim TK, Zabłocka M, Jóźwicki W, Yue J, Tuckey RC, Jetten AM, Slominski AT. Association among vitamin D, retinoic acid-related orphan receptors, and vitamin D hydroxyderivatives in ovarian cancer. Nutrients. 2020;12:3541. doi: 10.3390/nu12113541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Brozyna AA, VanMiddlesworth L, Slominski AT. Inhibition of melanogenesis as a radiation sensitizer for melanoma therapy. Int J Cancer. 2008;123:1448–1456. doi: 10.1002/ijc.23664. [DOI] [PubMed] [Google Scholar]
- 83.Slominski AT, Brożyna AA, Zmijewski MA, Janjetovic Z, Kim TK, Slominski RM, Tuckey RC, Mason RS, Jetten AM, Guroji P, et al. The role of classical and novel forms of vitamin D in the pathogenesis and progression of nonmelanoma skin cancers. Adv Exp Med Biol. 2020;1268:257–283. doi: 10.1007/978-3-030-46227-7_13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Brożyna AA, Żmijewski MA, Linowiecka K, Kim TK, Slominski RM, Slominski AT. Disturbed expression of vitamin D and retinoic acid-related orphan receptors α and γ and of megalin in inflammatory skin diseases. Exp Dermatol. 2022;31:781–788. doi: 10.1111/exd.14521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Riker AI, Enkemann SA, Fodstad O, Liu S, Ren S, Morris C, Xi Y, Howell P, Metge B, Samant RS, et al. The gene expression profiles of primary and metastatic melanoma yields a transition point of tumor progression and metastasis. BMC Med Genomics. 2008;1:13. doi: 10.1186/1755-8794-1-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Cunningham TJ, Tabacchi M, Eliane JP, Tuchayi SM, Manivasagam S, Mirzaalian H, Turkoz A, Kopan R, Schaffer A, Saavedra AP, et al. Randomized trial of calcipotriol combined with 5-fluorouracil for skin cancer precursor immunotherapy. J Clin Invest. 2017;127:106–116. doi: 10.1172/JCI89820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Hadden MK. Hedgehog and vitamin D signaling pathways in development and disease. Vitam Horm. 2016;100:231–253. doi: 10.1016/bs.vh.2015.10.006. [DOI] [PubMed] [Google Scholar]
- 88.Uhmann A, Niemann H, Lammering B, Henkel C, Hess I, Nitzki F, Fritsch A, Prüfer N, Rosenberger A, Dullin C, et al. Antitumoral effects of calcitriol in basal cell carcinomas involve inhibition of hedgehog signaling and induction of vitamin D receptor signaling and differentiation. Mol Cancer Ther. 2011;10:2179–2188. doi: 10.1158/1535-7163.MCT-11-0422. [DOI] [PubMed] [Google Scholar]
- 89.Dixon KM, Norman AW, Sequeira VB, Mohan R, Rybchyn MS, Reeve VE, Halliday GM, Mason RS. 1α,25(OH)2-vitamin D and a nongenomic vitamin D analogue inhibit ultraviolet radiation-induced skin carcinogenesis. Cancer Prev Res (Phila) 2011;4:1485–1494. doi: 10.1158/1940-6207.CAPR-11-0165. [DOI] [PubMed] [Google Scholar]
- 90.Reichrath J, Rafi L, Rech M, Mitschele T, Meineke V, Gartner BC, Tilgen W, Holick MF. Analysis of the vitamin D system in cutaneous squamous cell carcinomas. J Cutan Pathol. 2004;31:224–231. doi: 10.1111/j.0303-6987.2003.00183.x. [DOI] [PubMed] [Google Scholar]
- 91.Bikle DD. Vitamin D and the skin: Physiology and pathophysiology. Rev Endocr Metab Disord. 2012;13:3–19. doi: 10.1007/s11154-011-9194-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Dixon KM, Sequeira VB, Deo SS, Mohan R, Posner GH, Mason RS. Differential photoprotective effects of 1,25-dihydroxyvitamin D3 and a low calcaemic deltanoid. Photochem Photobiol Sci. 2012;11:1825–1830. doi: 10.1039/c2pp25208b. [DOI] [PubMed] [Google Scholar]
- 93.Zbytek B, Janjetovic Z, Tuckey RC, Zmijewski MA, Sweatman TW, Jones E, Nguyen MN, Slominski AT. 20-Hydroxyvitamin D3, a product of vitamin D3 hydroxylation by cytochrome P450scc, stimulates keratinocyte differentiation. J Invest Dermatol. 2008;128:2271–2280. doi: 10.1038/jid.2008.62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Podgorska E, Kim TK, Janjetovic Z, Urbanska K, Tuckey RC, Bae S, Slominski AT. Knocking out the vitamin D receptor enhances malignancy and decreases responsiveness to vitamin D3 hydroxyderivatives in human melanoma cells. Cancers (Basel) 2021;13:3111. doi: 10.3390/cancers13133111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Slominski AT, Brożyna AA, Skobowiat C, Zmijewski MA, Kim TK, Janjetovic Z, Oak AS, Jozwicki W, Jetten AM, Mason RS, et al. On the role of classical and novel forms of vitamin D in melanoma progression and management. J Steroid Biochem Mol Biol. 2018;177:159–170. doi: 10.1016/j.jsbmb.2017.06.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Skobowiat C, Oak AS, Kim TK, Yang CH, Pfeffer LM, Tuckey RC, Slominski AT. Noncalcemic 20-hydroxyvitamin D3 inhibits human melanoma growth in in vitro and in vivo models. Oncotarget. 2017;8:9823–9834. doi: 10.18632/oncotarget.14193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Jenkinson C. The vitamin D metabolome: An update on analysis and function. Cell Biochem Funct. 2019;37:408–423. doi: 10.1002/cbf.3421. [DOI] [PubMed] [Google Scholar]
- 98.Jenkinson C, Desai R, Slominski AT, Tuckey RC, Hewison M, Handelsman DJ. Simultaneous measurement of 13 circulating vitamin D3 and D2 mono and dihydroxy metabolites using liquid chromatography mass spectrometry. Clin Chem Lab Med. 2021;59:1642–1652. doi: 10.1515/cclm-2021-0441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Carlberg C, Muñoz A. An update on vitamin D signaling and cancer. Semin Cancer Biol. 2022;79:217–230. doi: 10.1016/j.semcancer.2020.05.018. [DOI] [PubMed] [Google Scholar]
- 100.Zmijewski MA, Carlberg C. Vitamin D receptor(s): In the nucleus but also at membranes? Exp Dermatol. 2020;29:876–884. doi: 10.1111/exd.14147. [DOI] [PubMed] [Google Scholar]
- 101.Tuckey RC, Cheng CYS, Slominski AT. The serum vitamin D metabolome: What we know and what is still to discover. J Steroid Biochem Mol Biol. 2019;186:4–21. doi: 10.1016/j.jsbmb.2018.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Christakos S, Li S, De La Cruz J, Bikle DD. New developments in our understanding of vitamin metabolism, action and treatment. Metabolism. 2019;98:112–120. doi: 10.1016/j.metabol.2019.06.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Christakos S, Dhawan P, Verstuyf A, Verlinden L, Carmeliet G. Vitamin D: Metabolism, molecular mechanism of action, and pleiotropic effects. Physiol Rev. 2016;96:365–408. doi: 10.1152/physrev.00014.2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Medeiros JFP, de Oliveira Borges MV, Soares AA, dos Santos JC, de Oliveira ABB, da Costa CHB, Cruz MS, Bortolin RH, de Freitas RCC, Dantas PMS, et al. The impact of vitamin D supplementation on VDR gene expression and body composition in monozygotic twins: Randomized controlled trial. Sci Rep. 2020;10:11943. doi: 10.1038/s41598-020-69128-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Hu L, Bikle DD, Oda Y. Reciprocal role of vitamin D receptor on β-catenin regulated keratinocyte proliferation and differentiation. J Steroid Biochem Mol Biol. 2014;144(Pt A):237–241. doi: 10.1016/j.jsbmb.2013.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Reichrath J, Kamradt J, Zhu XH, Kong XF, Tilgen W, Holick MF. Analysis of 1,25-dihydroxyvitamin D(3) receptors (VDR) in basal cell carcinomas. Am J Pathol. 1999;155:583–589. doi: 10.1016/S0002-9440(10)65153-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Bikle DD, Ng D, Oda Y, Hanley K, Feingold K, Xie Z. The vitamin D response element of the involucrin gene mediates its regulation by 1,25-dihydroxyvitamin D3. J Invest Dermatol. 2002;119:1109–1113. doi: 10.1046/j.1523-1747.2002.19508.x. [DOI] [PubMed] [Google Scholar]
- 108.Janjetovic Z, Tuckey RC, Nguyen MN, Thorpe EM, Jr, Slominski AT. 20,23-dihydroxyvitamin D3, novel P450scc product, stimulates differentiation and inhibits proliferation and NF-kappaB activity in human keratinocytes. J Cell Physiol. 2010;223:36–48. doi: 10.1002/jcp.21992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Grund-Gröschke S, Stockmaier G, Aberger F. Hedgehog/GLI signaling in tumor immunity-new therapeutic opportunities and clinical implications. Cell Commun Signal. 2019;17:172. doi: 10.1186/s12964-019-0459-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Shang S, Hua F, Hu ZW. The regulation of β-catenin activity and function in cancer: Therapeutic opportunities. Oncotarget. 2017;8:33972–33989. doi: 10.18632/oncotarget.15687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Torezan L, Grinblat B, Haedersdal M, Valente N, Festa-Neto C, Szeimies RM. A randomized split-scalp study comparing calcipotriol-assisted methyl aminolaevulinate photodynamic therapy (MAL-PDT) with conventional MAL-PDT for the treatment of actinic keratosis. Br J Dermatol. 2018;179:829–835. doi: 10.1111/bjd.16473. [DOI] [PubMed] [Google Scholar]
- 112.Slominski AT, Kim TK, Qayyum S, Song Y, Janjetovic Z, Oak ASW, Slominski R M, Raman C, Stefan J, Mier-Aguilar CA, et al. Vitamin D and lumisterol derivatives can act on liver X receptors (LXRs) Sci Rep. 2021;11:8002. doi: 10.1038/s41598-021-87061-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.