Highlights
-
•
We describe a pilot RCT on the feasibility of an intervention for minority stress.
-
•
AWARENESS aims to improve mental health, substance use, and HIV outcomes.
-
•
We examined outcomes for sexual minority men living with HIV who use substances.
-
•
Feasibility was supported by high intervention and procedure completion rates.
-
•
Participants applied the intervention to intersectional identities/characteristics.
Keywords: Substance use, Minority stress, HIV, LGBT, Sexual minority
Abstract
Introduction
The minority stress model is the primary explanatory model for disparities in substance use and other mental health problems among sexual minority men (SMM) compared to heterosexual men. This pilot randomized controlled trial tested the feasibility of AWARENESS, a novel 9-session cognitive-behavioral psychotherapeutic intervention that targets intersectional minority stress and stigma, among sexual minority men living with HIV who use substances.
Methods
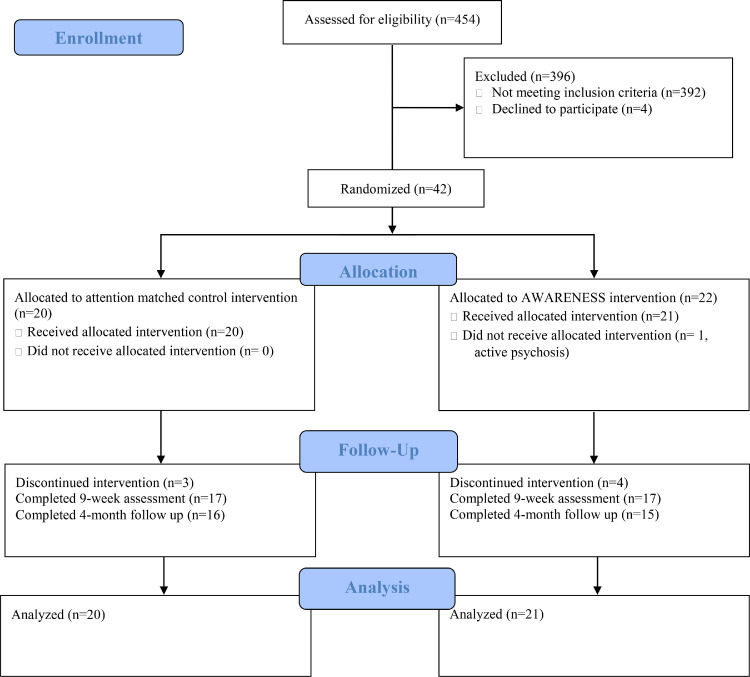
Feasibility was determined by the number of participants screened to obtain the target sample size, the percentage of eligible participants randomized, percentage of study intervention and assessment visits attended, time to complete study procedures, and percentage of data completeness of intervention assessments. Forty-two sexual minority men living with HIV with any illicit substance use or who reported at least one occasion of consuming five or more drinks in one setting in the last three months were randomized to AWARENESS (n = 22) or an attention control condition (n = 20).
Results
Feasibility of the trial was supported, with adequate completion of study procedures and visits (73% completed all intervention sessions, 71% completed all study assessment sessions). This trial also demonstrated the feasibility of using AWARENESS skills and strategies in relation to multiple intersecting identities, with participants discussing an average of 5.7 identities (e.g., sexual orientation) or individual characteristics (e.g., socioeconomic status) in relation to intervention content.
Conclusion
Our results support the feasibility of an AWARENESS trial to reduce intersectional minority stress related to multiple identities and characteristics among sexual minority men living with HIV who use substances.
1. Introduction
Sexual minority men experience higher rates of substance use and other mental health problems than their heterosexual peers, with minority stress (i.e., prejudice events and conditions, anticipation of prejudice, concealment of one's sexual orientation, and internalized stigma) being the primary explanatory model for these disparities (Meyer, 2003). The minority stress model can be extended to account for intersectional minority stress related to one's intersecting identities or characteristics (Bowleg et al., 2003). These intersecting minority identities or characteristics can include race, HIV-status, or socioeconomic status (Bowleg, 2012; Bowleg et al., 2003). Evidence has further suggested that the experience of a minority stressor (i.e.., mistreatment related to one's sexual orientation, Livingston et al., 2017) or stigma related to another stigmatized characteristic (i.e., HIV-related stigma, Rendina et al., 2018) is related to subsequent substance use and changes in mood and anxiety (Livingston et al., 2020), and stigma related to substance use has also been shown to be related to reduced engagement in HIV care (Batchelder et al., 2021). Furthermore, minority stress may lead to poor physical health outcomes among sexual minority people through both direct impacts on physical health (e.g., through alterations in inflammation and immune function) and indirect effects due to coping (e.g., through substance use, Flentje et al., 2020). Among people living with HIV, minority stress, substance use, and poor mental health are important predictors of HIV-related health outcomes (e.g., Carrico et al., 2014; Cole et al., 1996; Leserman, 2008). Taken together, these data underscore the importance of addressing minority stress, substance use, and mental health among sexual minority men living with HIV.
Although minority stress related to intersecting identities is an inevitability in the lives of many sexual minority men living with HIV, it has also been suggested that coping can be an important moderator of the negative health outcomes related to minority stress (Flentje et al., 2019). Previously published cognitive behavioral interventions that integrated coping strategies for stress related to HIV status or discrimination have shown decreased minority stress and improved related health outcomes both among sexual minority men and sexual minority men living with HIV (Antoni et al., 2000a, 2000b; Bogart et al., 2018; Lutgendorf et al., 1998; Pachankis et al., 2015; Ross et al., 2007). Given evidence that supporting coping skills for discrimination or stress related to HIV had shown promise, we developed AWARENESS, a cognitive behavioral psychotherapeutic intervention designed to directly address and develop coping skills for intersectional minority stress.
AWARENESS is a nine session, individually delivered intervention that targets psychoeducation and coping strategies for all components of minority stress: discrimination, anticipation of discrimination, concealment of identity, and internalized stigma (Meyer, 2003). AWARENESS is also designed to identify and address individually relevant outcomes related to minority stress including substance use, mood, anxiety, and other behaviors identified by the individual. In prior publication, we described the structure and investigated the acceptability of AWARENESS in detail (Flentje, 2020). The intervention provides education, empowerment, and coping skills to help sexual minority individuals manage experiences of discrimination, stigma, and concealment. In providing skills to manage experiences of minority stress, AWARENESS is intended to alleviate the negative health outcomes that may be moderated by experiences of discrimination, stigma, and concealment (i.e., substance use, mental health, HIV outcomes). The intervention maps onto the minority stress model, while utilizing concept generalization to create a participant led approach by applying the intervention to the unique experience of identity and individual characteristics of the individual participant. Built upon the idea of identity salience (Yakushko et al., 2009), the intervention follows the participant's lead in terms of which identity or personal characteristics are relevant to the elements of minority stress and related coping skills.
The purpose of this study was to conduct a pilot randomized controlled trial to examine the feasibility of a 9-session cognitive-behavioral intervention (AWARENESS). We examined the number of participants screened to obtain the target sample size, the percentage of eligible participants randomized, the percentage of study intervention and assessment visits attended, the time to complete study procedures, and the percentage of data completeness of intervention assessments. In this pilot randomized controlled trial, we also sought to identify how participants applied the psychoeducation and coping strategies discussed in the intervention to multiple intersecting identities. We further analyzed preliminary data on hypothesized mechanisms (i.e., minority stress) and health outcomes AWARENESS was intended to impact including substance use, depression, anxiety, and symptoms of post-traumatic stress disorder, and HIV viral load and ART medication adherence among sexual minority men living with HIV who were episodic substance users to demonstrate feasibility of analysis. We also analyzed preliminary data and associated outcomes for participants who were high in minority stress at baseline versus those that were low in minority stress.
2. Methods
2.1. Participants
Participants were recruited from community settings and health clinics in the San Francisco Bay Area. To be eligible for the study participants had to: be 18 or older, speak English, be able to consent, be a sexual minority man (defined as sexual activity with a man in the three years prior or identification as gay or bisexual), provide evidence or documentation that they were HIV-positive (e.g., a letter of diagnosis or medication bottles with matched photo ID), and report at least one occasion of drinking five or more drinks in a single setting or of using an illicit substance in the previous three months. Participants were excluded if they were currently enrolled in formal substance use disorder treatment, currently met criteria for a severe substance use disorder (6 or more symptoms aligning with DSM criteria within the past 12 months) or had current symptoms consistent with schizophrenia or psychosis (2 or more current symptoms) or bipolar disorder (6 or more symptoms within the past year) experienced while not using substances.
2.2. Procedure
Flyers were posted in community settings (e.g., coffee shops) and at healthcare clinics and advertisements were posted online (e.g., craigslist). The study team also conducted in-person recruitment at healthcare clinics or in community settings. Study participants were invited to refer additional participants via snowball sampling. Potential participants were screened over the phone via interview or entered eligibility information directly into a tablet when screened in person.
Eligible persons were invited to a first study visit at a community mental health clinic where someone from the study team reviewed the study with participants and participants reviewed and signed the informed consent form, completed assessment measures, and then were randomized to AWARENESS or a matched attention control condition (Fig. B1). Randomization was done in blocks of 4 using random assignment generation in R (R: A Language and Environment for Statistical Computing, 2016) by the primary investigator. The study interventionist opened an envelope with the intervention assignment prior to starting with a new participant. The matched attention 9-session control condition consisted of the completion of assessments and a writing exercise focused on neutral content (similar to Carrico et al., 2019). Participants then returned for eight one-hour intervention sessions spaced approximately one week apart. At the final (ninth) session participants stayed for completion of a post-intervention assessment. Participants were asked to return for a follow-up assessment approximately four months post-randomization. Both study conditions were delivered by an interventionist with a PhD in Clinical Psychology. Blinded staff administered assessment visits. Participants were compensated $50 for completing each assessment visit and $20 for each intervention visit.
Fig. B1.
AWARENESS Pilot Randomized Control Trial Consort Diagram. Consort diagram of enrollment, randomization, intervention, and analysis of AWARENESS and attention control condition.
2.3. Measures
2.3.1. Content
AWARENESS (Flentje, 2020) includes nine individually delivered intervention sessions. The first session included an introduction to and discussion of the participant's experience of sexual minority and intersectional identities and experiences of discrimination. The intervention includes two sessions (respectively, psychoeducation and coping skills) for each of the components of minority stress: discrimination, anticipation of discrimination, concealment, and internalized stigma. The final session covers a summary of intervention content, where the participant and interventionist discuss planned future application of knowledge and skills within the AWARENESS intervention. The study interventionist noted the minority statuses and individual characteristics discussed in relation to intervention content during the intervention.
2.3.2. Mechanisms
Minority stress was measured using the Cultural Assessment of the Risk of Suicide (CARS), sexual minority stress subscale (Chu et al., 2013a). This subscale consists of five items answered on a 6-point scale ranging from “strongly disagree” to “strongly agree”, resulting in a continuous score ranging from 5 to 30. Scores at or above 14 are considered moderate or severe sexual minority stress and have been found to be predictive of depression, hopelessness, and suicide attempts (Chu et al., 2013b) in a validation sample of 950 culturally diverse adults drawn from the general population (Chu et al., 2013a). Internalized stigma and concealment components of minority stress were also measured with the Revised Internalized Homophobia Scale (IHP-R, Herek et al., 2009, a measure of the internalized stigma component of sexual minority stress). The IHP-R consists of 5 items rated on a scale ranging from 1 “strongly disagree” to 5 “strongly agree” and results in a continuous score representing internalized stigma (taken as a mean of the 5 items, range 1–5) with higher scores indicating more stigma. Outness was measured using the “Out to the World” subscale of the Outness Inventory (OI, Mohr and Fassinger, 2000), which measures the degree to which an individual is open about their sexual orientation in social settings (i.e., with new straight friends, work peers, work supervisors, and strangers). Responses on the Outness Inventory range from 1 “person definitely does not know about your sexual orientation status” to 7 “person definitely knows about your sexual orientation status, and it is openly talked about” and results in a continuous score (mean of all items) with higher scores indicating greater outness.
2.3.3. Substance use and mental health outcomes
The Alcohol Smoking and Substance Involvement Screening Test (ASSIST, Humeniuk et al., 2008, administered in the original format which queried substance use in the three months prior and also in a format adapted to be relevant to a 30-day timeframe to be more responsive within the timeframe of the intervention for measures after the intervention) was used to measure substance use. The ASSIST results in a continuous score for each substance used, with higher scores indicative of greater substance use severity. A cutoff score of 4 or more is considered moderate risk (11 or more for alcohol only), and 27 or more is considered high risk. The Alcohol Use Disorders Identification Test (Saunders et al., 1993) was also used to measure alcohol use. The Patient Health Questionnaire-9 (PHQ-9, Kroenke and Spitzer, 2002) was used to measure depression, the Generalized Anxiety Disorder-7 item (GAD-7, Spitzer et al., 2006) was used to assess anxiety, and the Patient Checklist-Civilian (PCL-C, Weathers and Ford, 1996) was used to measure symptoms of post-traumatic stress disorder. The PCL-C was added after the first 11 participants had been randomized, thus was only administered for a subset of the study visits.
2.3.4. HIV outcomes
HIV viral load was measured via standard laboratory procedures using the Abbott Realtime HIV Viral Load and CLIA certified Roche test provided by two different laboratories due to laboratory changes mid-study. A visual analogue scale (ranging 0–100) was used to measure medication adherence.
2.4. Analysis
Analyses were conducted using Stata 15.1 and SAS Version 9.4. Feasibility was assessed through the number of people required to be screened to obtain a target N = 40; the rate of enrollment per month; the proportion who completed informed consent, were randomized, and started the intervention; the percentage of intervention sessions attended (target 80% of participants to attend 7 or more of designated intervention sessions, corresponding to more than 75% of intervention sessions); time duration of assessment procedures and proportion completed (target 70% to complete all assessments, target completion time less than 1 ½ hours); and data completeness (target 90% complete data among study outcomes including substance use, mental health, and HIV outcomes among assessed participants). We examined whether there were differences in data completeness and intervention sessions attended by whether participants had undetectable viral load at baseline (as a proxy of sub-optimal HIV care engagement) using chi-square analyses to identify if there were systematic differences in trial feasibility among individuals who had detectable HIV viral load and may be less likely to be adequately engaged in care.
Outcomes are reported at baseline, nine weeks (conclusion of intervention), and at four-month follow-up. This pilot was not powered for inferential analysis yet we report inferential analysis here to demonstrate the feasibility of running these analyses. Preliminary analyses of outcomes were conducted using generalized linear mixed models. All outcomes were continuous. Within these models, intervention group (treatment versus control), time, and a group by time interaction effect were modeled as fixed effects. Residual correlations among repeated measures within the same participants were modeled using an unstructured covariance structure. We further examined 3-way interactions between intervention group, time, and minority stress (low versus moderate or high) at baseline. Dependent variables included the mechanism (sexual minority stress, internalized stigma, outness) and outcomes (substance use, mental health, and HIV outcomes). Viral load was log10 transformed prior to analysis. Alpha was set to 0.05 for effects tested in these exploratory analyses.
3. Results
3.1. Participants
See Table A1 for demographic information of participants. All participants reported their sexual orientation as gay, just over half (54%) reported their race as White, 17% as African American or Black, 15% reported multiple races, 5% reported they were Filipino, 5% reported they were Native American, and 2% reported they were Asian. In addition, 15% of the participants reported Hispanic or Latino ethnicity. Most participants (78%) reported moderate or high risk on one or more substances as measured on the ASSIST; 15% of participants were moderate or high risk on one substance, 39% on two substances, 15% on three substances, and 10% on four or more substances. Participants were moderate or high risk on the ASSIST on the following substances: cannabis (66%), tobacco (51%), amphetamine type stimulants (44%), alcohol (24%), sedatives or sleeping pills (22%), cocaine (20%), inhalants (12%), hallucinogens (7%), other drugs (5%), and opioids (2%).
Table A1.
Baseline demographic and clinical information of 41 sexual minority men living with HIV who participated in the AWARENESS pilot RCT.
| AWARENESS condition n = 21 | Attention matched control n = 20 | |
|---|---|---|
| Sexual orientation | ||
| Gay | 21 (100%) | 20 (100%) |
| Age M (SD), Range | 53.0 (8.3) | 53.7 (11.5) |
| Race | ||
| Asian | 1 (5%) | 0 (0%) |
| Black/African American | 3 (14%) | 4 (20%) |
| Filipino | 1 (5%) | 1 (5%) |
| Multiracial | 2 (10%) | 4 (20%) |
| Native American | 1 (5%) | 1 (5%) |
| Prefer not to answer | 1 (5%) | 0(0%) |
| White | 12 (57%) | 10 (50%) |
| Ethnicity | ||
| Hispanic/Latino | 2 (10%) | 4 (20%) |
| Income | ||
| < $10,000 | 4 (19%) | 8 (40%) |
| $10,000-$20,000 | 12 (57%) | 5 (25%) |
| $20,000-$30,000 | 4 (19%) | 1 (5%) |
| $30,000-$40,000 | 0 (0%) | 2 (10%) |
| $40,000-$100,000 | 0 (0%) | 2 (10%) |
| >$100,000 | 1 (5%) | 2 (10%) |
| Education | ||
| High school graduate | 6 (29%) | 1 (5%) |
| Trade/technical school | 2 (10%) | 2 (10%) |
| Some college | 5 (24%) | 4 (20%) |
| 2 -year college degree | 3 (14%) | 3 (15%) |
| 4-year college degree | 4 (19%) | 5 (25%) |
| Graduate or professional degree | 1 (5%) | 5 (25%) |
| ASSIST | ||
| Moderate risk for alcohol or another drug | 14 (67%) | 14 (70%) |
| High risk for alcohol or another drug | 2 (10%) | 2 (10%) |
| AUDIT 8a | 3 (14%) | 5 (25%) |
| PHQ-9 10a | 6 (29%) | 4 (20%) |
| GAD-7 10a | 3 (14%) | 2 (10%) |
| Viral load undetectable (<50 copies/mL) | 17 (81%) | 18 (90%) |
| ART medication adherence 95% | 14 (67%) | 12 (60%) |
| IHP-R M (SD), range | 1.46 (0.65), 1–3 | 1.54 (0.76), 1–3.75 |
| CARS M (SD), range | 13.81 (3.63), 9–21 | 11.2 (5.19), 5–20 |
3.2. Feasibility
Screening for eligibility began in October 2016 and continued through November 2018 (approximately 25 months of screening in duration). In total, 454 participants were screened, of these, four declined to participate and 63 were eligible, though one of these participants was later deemed ineligible as they had participated in an open pilot of the intervention. First randomization occurred in May 2017 and the last participant was randomized in November 2018 (18 months of active study enrollment and randomization); participants screened in the first seven months were maintained on an eligible list prior to study launch and were screened as a continuation of screening from a prior study with identical recruitment criteria. Of note, this study did not have full-time staff, thus the rate of recruitment was based on ∼40% research assistant support. Of the 62 eligible participants, 42 participants completed informed consent, were randomized, and started the intervention (70%; target N was 40 men enrolled, but 2 additional men had screened eligible and wished to complete study visits), 1 of these participants was removed after the first study visit and randomization due to active psychosis, resulting in 41 people who participated in the trial. In total, 30 participants (73%) completed all intervention sessions with 34 participants (83%) completing 7 or more intervention sessions (85% in control and 81% in AWARENESS arm, considered intervention completers). In total, 29 of the 41 individuals (71%) completed all assessment visits and an additional 7 participants completed 2 of the 3 assessment visits (n = 5 baseline and final session assessment, n = 2 baseline and 4-month follow-up). Assessment measures were completed in less than 1 ½ hours (mean 68 min, range 29:177 min). Primary study outcomes had more than 90% complete data across data points among participants who were assessed for all outcomes (ASSIST: 99%; AUDIT: 95%; PHQ-9: 98%; GAD-7: 97%; PCL-C: 94%; 98% reported whether or not they were on ART; of those on ART 100% reported on their adherence). The exception was for HIV viral load data, which were obtained for 85% of the assessment visits. The lower percentage of available data on HIV viral load was due to multiple issues related to blood sampling and processing (e.g., lab failures (2 lost samples), blood draw refusals (2 participants), sample deemed unacceptable by lab (1 sample), and insufficient blood drawn (1 sample)). There was no difference in the percentage of complete data between participants who had undetectable viral load at baseline versus those that did not (p > .05 for all) for all outcomes except for viral load. Analysis of viral load data revealed that participants who had detectable viral load at baseline were more likely to have missing viral load data at a subsequent visit (χ2 = 5.8, p = .02). Further examination of time points where someone with detectable viral load had a study visit but did not have associated viral load data revealed that one participant preemptively indicated he did not want to have his blood drawn at subsequent visits (two missing viral load values) and the other missing values were from participants who had provided blood samples during a time when the clinical laboratory used by the study altered their operations and results were not returned. Thus, this difference in missingness of viral load data does not appear to be attributable to participant characteristics or engagement in HIV care.
3.3. Content
Participants related an average of 5.7 minority statuses or individual characteristics (range 3–10) to the minority stress concepts and coping skills discussed in the intervention sessions. See Table A2 for minority statuses discussed in relation to content. The most frequently endorsed minority statuses or individual characteristics were sexual orientation, endorsed by all participants, HIV-status, endorsed by 95% of participants, and socioeconomic status, endorsed by 76% of participants.
Table A2.
Identity statuses and individual characteristics discussed among 21 sexual minority men living with HIV who participated in the AWARENESS condition.
| n (%) | |
|---|---|
| Sexual orientation | 21 (100%) |
| HIV status | 20 (95%) |
| Socioeconomic status | 16 (76%) |
| Age | 8 (38%) |
| Spirituality or religion | 8 (38%) |
| Race | 7 (33%) |
| Ethnicity | 6 (29%) |
| Weight | 4 (19%) |
| Disability status | 3 (14%) |
| Substance use | 3 (14%) |
| Immigration status | 2 (10%) |
| Mental health status | 2 (10%) |
| Poor health | 2 (10%) |
| Rural versus urban | 2 (10%) |
| Size | 2 (10%) |
| Beliefs in twelve-step program | 1 (5%) |
| Employment status | 1 (5%) |
| Failure to achieve potential | 1 (5%) |
| Gender | 1 (5%) |
| Gender presentation | 1 (5%) |
| Hepatitis C status | 1 (5%) |
| Homelessness | 1 (5%) |
| Obsessive compulsive disorder | 1 (5%) |
| Parent status | 1 (5%) |
| Polyamory | 1 (5%) |
| Role as top versus bottom | 1 (5%) |
| Single (unpartnered) status | 1 (5%) |
| Social anxiety | 1 (5%) |
3.4. Preliminary analysis of outcomes
3.4.1. Mechanism outcomes
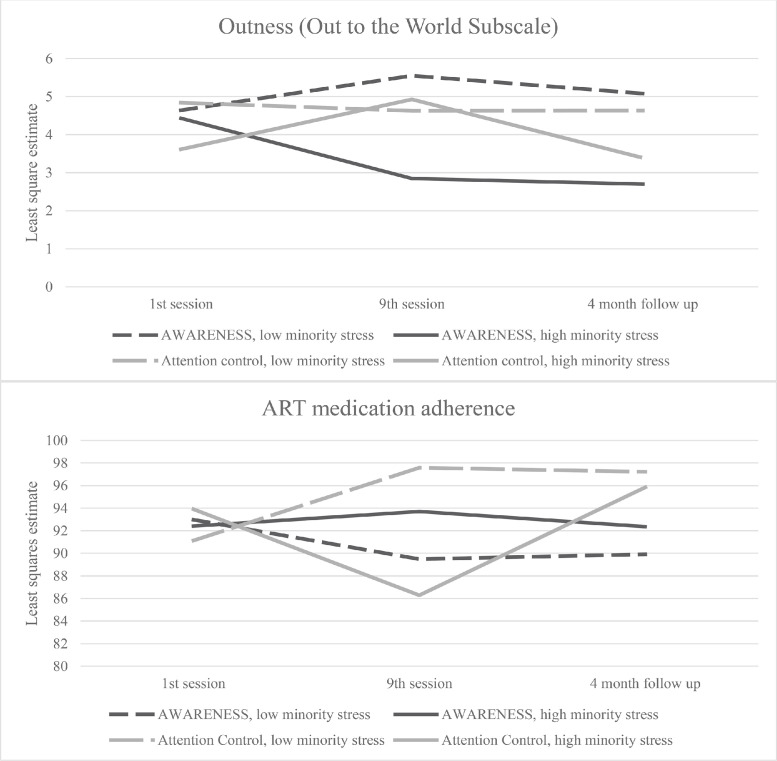
There were no statistically significant differences in the interaction of time by intervention condition in CARS Total Scores, IHP-R scores, or Out to the World subscale scores. There was an interaction between time, intervention condition, and minority stress level at baseline on Out to the World subscale scores (F [2,39] = 3.48, p = .04) with those within the intervention condition who had high minority stress at baseline evidencing reductions in outness scores at the second time point (representing less outness) and those who were in the intervention condition with low minority stress at baseline evidencing increases in outness at the second time point (Fig. B2). There was no interaction between time, intervention condition, and minority stress level at baseline on CARS total scores or IHP-R scores.
Fig. B2.
Graphs of the significant interactions between outcome variables with time, minority stress, and intervention condition. Above, there was a significant interaction at baseline on outness, as measured by the out to the world subscale of the Outness Inventory. Those in the intervention condition with high minority stress at baseline showed reduced outness scores in the second time point. Outness increased for those in the intervention condition at the second time point for those low in minority stress. The graph below shows the significant interaction on ART medication adherence. There was a reduction in medication adherence at the second time point for those in the attention control condition who were high in minority stress at baseline. Those in the attention control condition who were low in minority stress at baseline showed an increase in adherence in the second time point.
3.4.2. Substance use and mental health
There were no statistically significant differences in the interaction of time by intervention condition, nor the 3-way interaction between time, intervention condition, or minority stress level at baseline in PHQ-9 scores, ASSIST scores, GAD-7 scores, AUDIT, or PCL-C scores. Of note, the interaction of time, intervention condition, and minority stress at baseline on AUDIT scores was near to the established cutoff for alpha (F [2, 39] = 3.02, p = 0.06).
3.4.3. HIV outcomes
There were no interactions between time and intervention condition in adherence or viral load, or in the interaction of time by intervention condition by minority stress level on adherence. There was an interaction between time, intervention condition, and minority stress level at baseline on adherence (F [2, 37] = 5.51, p = .008), with the largest differences noted to be a reduction in adherence at the second time point among individuals in the attention control condition who were high in minority stress at baseline, and an increase in adherence in individuals in the attention control condition who were low in minority stress at baseline (Fig. B2).
4. Discussion
This study demonstrated the feasibility of a trial of AWARENESS. We demonstrated acceptable rates of study and assessment completion, with 73% of participants completing all intervention sessions, and 83% attending 7 or more of the 9 intervention sessions, and 71% of participants completing all assessment visits. Assessments were relatively complete with over 90% complete data on assessment instruments. Taken together this suggests that the procedures related to the implementation of an AWARENESS trial are feasible. Prior work including in-depth interviews with participants demonstrated that the AWARENESS intervention was acceptable to participants (Flentje, 2020).
We found that participants discussed and applied coping skills related to multiple intersecting identities and individual characteristics during the intervention, with participants discussing an average of approximately six different minority statuses or individual characteristics across the sessions (Table A2). This suggests that intervention content can be flexibly applied to the most salient individual characteristics. The most discussed characteristics were sexual minority status, HIV status, and socioeconomic status, likely because all the participants were sexual minority men living with HIV, and most participants had income below $30,000 per year in an expensive urban area. Participants also identified intersecting identities and characteristics that were not the focus of the materials within the AWARENESS manual but for which they identified that the intervention was applicable including: age, spirituality or religion, race, ethnicity, weight, disability status, substance use, mental health, homelessness, and polyamory among others.
Our preliminary data did not detect significant differences in minority stress, mental health, substance use, or HIV outcomes due to the intervention (Table A3). However, as a pilot study, this study was not powered or designed to detect such changes. We did demonstrate the feasibility of running trial analyses. We further note that mean outcomes showed reductions on mental health, substance use, and HIV outcomes, suggesting that larger samples may observe improved health outcomes related to AWARENESS. A full-scale randomized controlled trial would be required to demonstrate the potential of AWARENESS to improve outcomes that we know are impacted by minority stress including substance use, anxiety, depression, and HIV-related outcomes (e.g., ART adherence and HIV viral load).
Table A3.
Comparisons between AWARENESS and the attention matched control condition on study outcomes.
| Time |
Generalized linear mixed model: session by study condition |
|||||
|---|---|---|---|---|---|---|
| Outcome | Group | Baseline M (SE) | 9 weeks (conclusion) M (SE) | 4-month follow-up M (SE) | F (DF) | p |
| CARS | AWARENESS | 13.33 (0.46) | 12.77 (0.59) | 13.77 (0.62) | 1.41 (2, 39) | 0.26 |
| Control | 11.65 (0.46) | 11.52 (0.63) | 11.67 (0.63) | |||
| IHP-R | AWARENESS | 1.44 (0.15) | 1.53 (0.14) | 1.45 (0.17) | 1.19 (2, 39) | 0.31 |
| Control | 1.57 (0.15) | 1.20 (0.15) | 1.27 (0.17) | |||
| Outness | AWARENESS | 4.54 (0.38) | 4.20 (0.39) | 3.89(0.41) | 0.06 (2, 39) | 0.94 |
| Control | 4.23 (0.41) | 4.78 (0.41) | 4.01 (0.42) | |||
| ASSIST-past 30 days | AWARENESS | 33.81 (5.34) | 31.09 (5.48) | 26.92 (5.76) | 0.39 (2, 39) | 0.68 |
| Control | 36.54 (5.46) | 31.23 (5.63) | 33.31 (5.92) | |||
| AUDIT | AWARENESS | 4.30 (1.05) | 3.66 (1.13) | 2.71 (0.96) | 0.36 (2, 39) | 0.70 |
| Control | 4.56 (1.08) | 4.72 (1.15) | 4.12 (0.99) | |||
| PHQ-9 | AWARENESS | 7.13 (1.07) | 6.83 (1.15) | 8.31 (1.32) | 1.7 (2, 39) | 0.19 |
| Control | 7.11 (1.09) | 8.08 (1.19) | 6.97 (1.34) | |||
| GAD-7 | AWARENESS | 6.42 (0.97) | 5.01 (1.19) | 5.26 (1.45) | 0.66 (2, 39) | 0.52 |
| Control | 5.06 (0.99) | 4.85 (1.23) | 6.25 (1.47) | |||
| PCL-C | AWARENESS | 39.92 (3.21) | 32.74 (3.54) | 36.81 (4.08) | 0.86 (2, 32) | 0.43 |
| Control | 34.82 (3.42) | 36.06 (3.91) | 36.63 (4.53) | |||
| Adhere | AWARENESS | 92.70 (3.49) | 91.59 (3.25) | 91.14 (2.71) | 2.38 (2, 37) | 0.11 |
| Control | 92.52 (4.04) | 91.94 (3.45) | 96.53 (2.94) | |||
| Log10 Viral load | AWARENESS | 0.77 (0.31) | 1.09 (0.31) | 1.12 (0.38) | 1.50 (2, 39) | 0.24 |
| Control | 0.77 (0.32) | 0.52 (0.31) | 0.84 (0.35) | |||
With this study we have demonstrated that our trial procedures were feasible and that AWARENESS was able to be used to additionally address intersectional minority stress in study sessions. However, in this trial, we did not recruit people based on diagnosis or mental health symptoms. This resulted in a sample that, unlike other psychotherapy trials, was not necessarily experiencing clinically significant distress related to specific symptoms. One problem in psychotherapy research is that individuals are clustered in trials by diagnosis, something that is not typically representative of patients appearing for care (Shean, 2014). Minority stress exerts deleterious impacts on multiple biological and health outcomes (Flentje et al., 2020), thus altering the biological and psychological impacts of minority stress may be expected to improve subsequent health outcomes. In our subsequent work, we will examine whether AWARENESS is related to changes in biological outcomes, changes that may occur even in the absence of clinically significant distress.
We further did not recruit based on ART adherence or viral load, and within this study that meant that there was little room for clinical improvement on these outcomes (i.e., the participants within this pilot reported average adherence on ART of more than 90% at baseline and 85% had undetectable viral load, leaving little room for substantial improvement on these outcomes). Our trial inclusion procedures meant that within this trial we had potentially less opportunity for the vast clinical changes related to HIV health outcomes that may be observed in a trial with a more extreme baseline level of a clinical outcome. However, interventions to support sexual minority men living with HIV, including men who are virally suppressed, are important to mitigate the risks of viral rebound among this population. Behavioral interventions have been shown to reduce the risk of viral rebound among sexual minority men with comparable rates of viral suppression (Carrico et al., 2019). We would expect, however, that a reduction in the impact of minority stress would have a transdiagnostic impact, and trials in process for sexual minority men take this transdiagnostic approach to treatment (Pachankis et al., 2019). What we have not yet established is how to measure smaller changes on multiple outcomes—the types of changes that may be meaningful to an individual or even at a population health level but are less detectable by current research methods. In future trials of AWARENESS or for other interventions taking a transdiagnostic approach, there may be a need to recruit based on clinically significant distress. For AWARENESS, this may mean focusing on a specific clinical area impacted by minority stress (e.g., substance use or HIV adherence or viral load at baseline).
We did not detect differences in feasibility of trial procedures between participants who had undetectable viral load at baseline and those that did not, with the exception of obtaining viral load data from subsequent visits, where we obtained less viral load data from participants with a detectable HIV viral load at baseline, though this appeared to be due to clinical lab procedures and not participant characteristics. This suggests that, in general, the trial procedures are feasible with participants with detectable viral load who may be sub-optimally engaged in HIV care, though larger sample sizes of individuals who are sub-optimally engaged in HIV care would be required to confirm this. The missing data related to viral load in this trial was higher than other outcomes and suggests that a future trial may benefit from alternative procedures for assessing viral load, in particular backup procedures when relying on a clinical laboratory or venous blood draw (e.g., alternatives such as dried blood spot procedures that evidence comparability in viral load results, Arredondo et al., 2012).
In this trial, we recruited based on episodic substance use, but did not have specific recruitment criteria requiring clinically significant substance use, and in fact excluded participants who endorsed criteria consistent with a severe substance use disorder who may be better served by substance use disorder treatment. Despite this recruitment strategy, of randomized participants 78% were designated as moderate or high risk based on their use of alcohol or another substance using the ASSIST, with nearly two-thirds of participants designated moderate or high risk on two or more substances. This suggests that among sexual minority men living with HIV, even a modest substance use criterion such as episodic substance use is likely to recruit a sample with polysubstance use.
4.1. Limitations
The results are limited to the population recruited for this study; future studies would need to examine the acceptability and feasibility of AWARENESS in other sexual and gender minority populations. Further, an additional limitation of this study was our sample size. As this was a pilot RCT, we were not adequately powered to examine clinically significant change. Additionally, the inclusion criteria did not include criteria related to minority stress, HIV viral load, ART adherence, or mental health symptoms which limits our ability to draw conclusions about clinically significant change measured here. Further, it may limit the results of our study to individuals who are not in need of improved HIV outcomes. As substance use stigma among people living with HIV who use substances has been found to be associated with missed appointments (Batchelder et al., 2021) and ART adherence (Stringer et al., 2019), future research may need to more directly assess this form of stigma. In this study, participants were not prompted to report substance use stigma but were given the opportunity to discuss this type of stigma in the AWARENESS intervention sessions. An additional limitation was the time period for follow up assessment. Future research will require more than four months to see changes in viral load outcomes. Future trials will remedy these shortcomings.
5. Conclusion
In sum, this study found that a trial of AWARENESS, a 9-session cognitive behavioral intervention to help individuals cope with intersectional minority stress is feasible, able to be applied to multiple intersecting minority statuses, and that changes observed in the outcome variables, while not statistically significant, were in the anticipated direction. A larger trial will provide more definitive information about the efficacy of this intervention.
Institutional review board
This project was reviewed and approved through the Institutional Review Board of the University of California, San Francisco.
Clinical trial registration
NCT03143205 https://clinicaltrials.gov/ct2/show/NCT03143205?term=NCT03143205&draw=2&rank=1.
Contributors
All authors have reviewed the final article. Primary Investigator: Annesa Flentje, PhDa,b. Research design, implementation, and article preparation: Gowri Sundera. Research design and article preparation: James W. Dilley, MDc,b. Research design and article preparation: Torsten B. Neilands, PhDd. Data analyses, and article preparation: Nadra E. Lisha, PhDe. Research implementation and article preparation: Katie E. Katuzny, PhDb. Research design and article preparation: Adam Carrico, PhDg.
Declaration of Competing Interest
No conflict declared.
Funding
This project was supported through funding from the National Institute on Drug Abuse, through K23DA039800 awarded to Dr. Flentje. Dr. Neilands was supported in part by R01DA052016. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.dadr.2022.100059.
Appendix. Supplementary materials
References
- Antoni M.H., Cruess D.G., Cruess S., Lutgendorf S., Kumar M., Ironson G., Klimas N., Fletcher M.A., Schneiderman N. Cognitive–behavioral stress management intervention effects on anxiety, 24-hr urinary norepinephrine output, and T-cytotoxic/suppressor cells over time among symptomatic HIV-infected gay men. J. Consult. Clin. Psychol. 2000;68(1):31–45. doi: 10.1037//0022-006x.68.1.31. http://dx.doi.org/10.1037/0022-006X.68.1.31. [DOI] [PubMed] [Google Scholar]
- Antoni M.H., Cruess S., Cruess D.G., Kumar M., Lutgendorf S., Ironson G., Dettmer E., Williams J., Klimas N., Fletcher M.A., Schneiderman N. Cognitive-behavioral stress management reduces distress and 24-hour urinary free cortisol output among symptomatic HIV-infected gay men. Ann. Behav. Med. 2000;22(1):29–37. doi: 10.1007/BF02895165. [DOI] [PubMed] [Google Scholar]
- Arredondo M., Garrido C., Parkin N., Zahonero N., Bertagnolio S., Soriano V., de Mendoza C. Comparison of HIV-1 RNA Measurements Obtained by Using Plasma and Dried Blood Spots in the Automated Abbott Real-Time Viral Load Assay. J. Clin. Microbiol. 2012;50(3):569–572. doi: 10.1128/JCM.00418-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Batchelder A.W., Foley J.D., Wirtz M.R., Mayer K., O’Cleirigh C. Substance Use Stigma, Avoidance Coping, and Missed HIV Appointments Among MSM Who Use Substances. AIDS Behav. 2021;25(5):1454–1463. doi: 10.1007/s10461-020-02982-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bogart L.M., Dale S.K., Daffin G.K., Patel K.N., Klein D.J., Mayer K.H., Pantalone D.W. Pilot intervention for discrimination-related coping among HIV-positive Black sexual minority men. Cult. Divers. Ethn. Minor. Psychol. 2018;24(4):541–551. doi: 10.1037/cdp0000205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bowleg L. The problem with the phrase women and minorities: intersectionality—an important theoretical framework for public health. Am. J. Public Health. 2012;102(7):1267–1273. doi: 10.2105/AJPH.2012.300750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bowleg L., Huang J., Brooks K., Black A., Burkholder G. Triple Jeopardy and Beyond: multiple Minority Stress and Resilience Among Black Lesbians. J. Lesbian Stud. 2003;7(4):87–108. doi: 10.1300/J155v07n04_06. [DOI] [PubMed] [Google Scholar]
- Carrico A.W., Neilands T.B., Dilworth S.E., Evans J.L., Gόmez W., Jain J.P., Gandhi M., Shoptaw S., Horvath K.J., Coffin L., Discepola M.V., Andrews R., Woods W.J., Feaster D.J., Moskowitz J.T. Randomized controlled trial of a positive affect intervention to reduce HIV viral load among sexual minority men who use methamphetamine. J. Int. AIDS Soc. 2019;22(12):e25436. doi: 10.1002/jia2.25436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carrico A.W., Shoptaw S., Cox C., Stall R., Li X., Ostrow D.G., Vlahov D., Plankey M.W. Stimulant use and progression to AIDS or mortality after the initiation of highly active antiretroviral therapy. JAIDS and J. Acquired Immune Deficiency Syndr. 2014;67(5):508–513. doi: 10.1097/QAI.0000000000000364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chu J., Floyd R., Diep H., Pardo S., Goldblum P., Bongar B. A tool for the culturally competent assessment of suicide: the Cultural Assessment of Risk for Suicide (CARS) Measure. Psychol. Assess. 2013;25(2):424. doi: 10.1037/a0031264. [DOI] [PubMed] [Google Scholar]
- Chu, J., Floyd, R., Diep, H., Pardo, S., Goldblum, P., & Bongar, B. (2013b). A tool for the culturally competent assessment of suicide: the Cultural Assessment of Risk for Suicide (CARS) Measure Manual.http://psycnet.apa.org/journals/pas/25/2/424/. [DOI] [PubMed]
- Cole S.W., Kemeny M.E., Taylor S.E., Visscher B.R., Fahey J.L. Accelerated course of human immunodeficiency virus infection in gay men who conceal their homosexual identity. Psychosom. Med. 1996;58(3):219–231. doi: 10.1097/00006842-199605000-00005. [DOI] [PubMed] [Google Scholar]
- Flentje A. AWARENESS: development of a cognitive-behavioral intervention to address intersectional minority stress for sexual minority men living with HIV who use substances. Psychotherapy (Chic) 2020;57(1):35–49. doi: 10.1037/pst0000243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flentje A., Heck N.C., Brennan J.M., Meyer I.H. The relationship between minority stress and biological outcomes: a systematic review. J. Behav. Med. 2020;43(5):673–694. doi: 10.1007/s10865-019-00120-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Herek G.M., Gillis J.R., Cogan J.C. Internalized stigma among sexual minority adults: insights from a social psychological perspective. J. Couns. Psychol. 2009;56(1):32. [Google Scholar]
- Humeniuk R., Ali R., Babor T.F., Farrell M., Formigoni M.L., Jittiwutikarn J., De Lacerda R.B., Ling W., Marsden J., Monteiro M. Validation of the alcohol, smoking and substance involvement screening test (ASSIST) Addiction. 2008;103(6):1039–1047. doi: 10.1111/j.1360-0443.2007.02114.x. [DOI] [PubMed] [Google Scholar]
- Kroenke K., Spitzer R.L. The PHQ-9: a new depression diagnostic and severity measure. Psychiatr. Ann. 2002;32(9):509–515. [Google Scholar]
- Leserman J. Role of Depression, Stress, and Trauma in HIV Disease Progression: Psychosom Med. 2008;70(5):539–545. doi: 10.1097/PSY.0b013e3181777a5f. [DOI] [PubMed] [Google Scholar]
- Livingston N., Flentje A., Brennan J., Mereish E., Reed O., Cochran B. Real-time associations between discrimination and anxious and depressed mood among sexual and gender minorities: the moderating effects of lifetime victimization and identity concealment—ProQuest. Psychol. Sex Orientat. Gend. Divers. 2020 doi: 10.1037/sgd0000371. https://search.proquest.com/docview/2338973980?accountid=14525 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Livingston N., Flentje A., Heck N.C., Szalda-Petree A., Cochran B.N. Ecological momentary assessment of daily prejudice experiences and nicotine, alcohol, and drug use among sexual and gender minority individuals. J. Consult. Clin. Psychol. 2017;85(12):1131–1143. doi: 10.1037/ccp0000252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lutgendorf S.K., Antoni M.H., Ironson G., Starr K., Costello N., Zuckerman M., Klimas N., Fletcher M.A., Schneiderman N. Changes in cognitive coping skills and social support during cognitive behavioral stress management intervention and distress outcomes in symptomatic human immunodeficiency virus (HIV)-seropositive gay men. Psychosom. Med. 1998;60(2):204–214. doi: 10.1097/00006842-199803000-00017. [DOI] [PubMed] [Google Scholar]
- Meyer I.H. Prejudice, social stress, and mental health in lesbian, gay, and bisexual populations: conceptual issues and research evidence. Psychol. Bull. 2003;129(5):674–697. doi: 10.1037/0033-2909.129.5.674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mohr J., Fassinger R. Measuring dimensions of lesbian and gay male experience. Measur. Eval. Counseling Dev. 2000 http://psycnet.apa.org/psycinfo/2000-05649-001 [Google Scholar]
- Pachankis J.E., Hatzenbuehler M.L., Rendina H.J., Safren S.A., Parsons J.T. LGB-affirmative cognitive-behavioral therapy for young adult gay and bisexual men: a randomized controlled trial of a transdiagnostic minority stress approach. J. Cons. Clin. Psychol. 2015;83(5):575–889. doi: 10.1037/ccp0000037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pachankis J.E., McConocha E.M., Reynolds J.S., Winston R., Adeyinka O., Harkness A., Burton C.L., Behari K., Sullivan T.J., Eldahan A.I., Esserman D.A., Hatzenbuehler M.L., Safren S.A. Project ESTEEM protocol: a randomized controlled trial of an LGBTQ-affirmative treatment for young adult sexual minority men’s mental and sexual health. BMC Public Health. 2019;19(1):1086. doi: 10.1186/s12889-019-7346-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- R: A Language and Environment for Statistical Computing. (2016). R Core Team. https://www.R-project.org/.
- Rendina H.J., Millar B.M., Parsons J.T. Situational HIV stigma and stimulant use: a day-level autoregressive cross-lagged path model among HIV-positive gay and bisexual men. Addict Behav. 2018;83:109–115. doi: 10.1016/j.addbeh.2018.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ross L.E., Doctor F., Dimito A., Kuehl D., Armstrong M.S. Can talking about oppression reduce depression? Modified CBT group treatment for LGBT people with depression. J. Gay Lesbian Soc. Serv. 2007;19(1):1–15. doi: 10.1300/J041v19n01_01. [DOI] [Google Scholar]
- Saunders J.B., Aasland O.G., Babor T.F., De la Fuente J.R., Grant M. Development of the alcohol use disorders identification test (AUDIT): WHO collaborative project on early detection of persons with harmful alcohol consumption-II. Addiction. 1993;88(6):791–804. doi: 10.1111/j.1360-0443.1993.tb02093.x. [DOI] [PubMed] [Google Scholar]
- Shean G. Limitations of randomized control designs in psychotherapy research. Adv Psychiatry. 2014;2014 [Google Scholar]
- Spitzer R.L., Kroenke K., Williams J.B., Löwe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch. Intern. Med. 2006;166(10):1092–1097. doi: 10.1001/archinte.166.10.1092. [DOI] [PubMed] [Google Scholar]
- Stringer K.L., Marotta P., Baker E., Turan B., Kempf M.-.C., Drentea P., Stepanikova I., Turan J.M. Substance Use Stigma and Antiretroviral Therapy Adherence Among a Drug-Using Population Living with HIV. AIDS Patient Care STDS. 2019;33(6):282–293. doi: 10.1089/apc.2018.0311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weathers F., Ford J. Psychometric review of PTSD Checklist (PCL-C, PCL-S, PCL-M, PCL-PR) Measur Stress Trauma Adapt. 1996:250–251. [Google Scholar]
- Yakushko O., Davidson M.M., Williams E.N. Identity salience model: a paradigm for integrating multiple identities in clinical practice. Psychotherapy. 2009;46(2):180–192. doi: 10.1037/a0016080. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.