Abstract
Introduction:
Sexual function is a vital aspect of human health and is recognized as a critical component of cancer survivorship. Understanding and evaluating the impacts of radiotherapy on female sexual function requires precise knowledge of organs involved in sexual function and the relationship between radiotherapy exposure and sexual tissue function. Although substantial evidence exists describing the impact of radiotherapy on male erectile tissues and related clinical sexual outcomes, there is very little research in this area in females. The lack of biomedical data in female patients makes it difficult to design studies aimed at optimizing sexual function post radiotherapy treatment for female pelvic malignancies.
Aims:
This scoping review identifies and categorizes current research on the impacts of radiotherapy on normal female erectile tissues including damage to normal functioning, clinical outcomes of radiation-related female erectile tissue damage, and techniques to spare erectile tissues or therapies to treat such damage.
Methods:
An evaluation of the evidence was performed and a summary of findings was generated per PRISMA-ScR guidelines. Manuscripts were included in the review that involved normal female erectile tissues and radiotherapy side effects.
Results:
Results show that little scientific investigation into the impacts of radiotherapy on female erectile tissues has been performed.
Conclusion:
Collaborative scientific investigations by clinical, basic and behavioral scientists in oncology and radiotherapy are needed to generate radiobiologic and clinical evidence to advance prospective evaluation, prevention and mitigation strategies that may improve sexual outcomes in female patients.
Keywords: radiotherapy, sexual dysfunction, cancer, survivorship, female sexual toxicity
Introduction
Sexual function is a vital aspect of human health and is recognized as a critical component of cancer survivorship1. Sexual dysfunction—including difficulties with interest, comfort, arousal or orgasm—is prevalent among women receiving radiotherapy for pelvic malignancies and can cause significant distress2–14. Maintaining the capacity for pleasurable sexual activity after cancer therapy can be fundamental to quality of life1, yet there are few effective preventative and mitigating strategies for female* patients1, 8, 15, 16.
The female erectile tissues—herein described as the bulboclitoris17 or the organ comprised of the clitoris and vestibular bulbs18, 19—compose the anatomic basis for female sexual arousal and orgasm20, 21. While the impact of radiotherapy on organs such as the vagina or ovaries, vital to sexual and reproductive function in female patients, has been studied in detail, the impact of radiotherapy on erectile tissues is lacking despite the fact that they are often included in the radiotherapy fields for pelvic malignancies and are injured by this treatment2, 3, 7–11, 22. Conversely, the impacts of radiotherapy on male erectile tissues and associated neurovasculature23, methods and biomarkers measuring radiation-related damage to these tissues23, 24, and the related impacts of radiotherapy on sexual function outcomes is well established23–26.
Evaluating the impact of radiotherapy on the function of the female erectile tissues requires synthesizing existing evidence to inform and design studies of this emerging research area. A comprehensive review on this subject has yet to be performed.
To address this deficiency, this scoping review aims to identify and report current evidence on the effect of radiotherapy on female erectile tissues and related sexual toxicities. The goal of this review is to comprehensively address the primary research questions including: what is the impact of radiotherapy on female erectile tissues; what are the toxicities and associated clinical outcomes secondary to radiotherapy effects on female erectile tissues; what techniques, methods, or biomarkers are used to assess the impact of radiotherapy on female erectile tissues; finally, what techniques or therapies are currently used to treat radiation-related damage to female erectile tissues.
Materials and Methods
We performed a scoping review per the PRISMA Extension for Scoping Reviews (PRISMA-ScR)27 and the Joanna Briggs Institute28 to examine the extent, range, and nature of available research and identify research gaps29. A scoping review provides a rigorous comprehensive, systematic approach to synthesize current heterogeneous literature to identify gaps in knowledge and provide an effective summary for practitioners and guide researchers. This review focuses on female patients who received radiotherapy treatment for pelvic malignancies (including external beam radiation therapy, proton therapy and interstitial as well as intracavitary brachytherapy). Primary studies that investigated any effect of radiotherapy on the function normal female erectile tissues were identified.
With the guidance of a research librarian, search terms were generated and preliminary searches were used to refine the search strategy. Table 1 shows the PICOS (Population, Intervention, Comparison, Outcome, Study design) framework used to guide the initial inclusion/exclusion of research reports. Our systematic protocol was registered in the Open Science Framework database (https://osf.io/tyfa8/). We then performed a comprehensive search of electronic bibliographic databases, including in PubMed/MEDLINE using MeSH and Title/Abstract terms. We also conducted a hand search of the reference list of included studies.
Table 1.
Population, Intervention, Control, Outcome, Study Design (PICOS) inclusion criteria
| Population: | Female patients with pelvic malignancies |
| Intervention: | Pelvic radiotherapy in the preoperative, postoperative or definitive settings |
| Control: | Comparators were optional |
| Outcomes: | Post-radiotherapy sexual function related to erectile tissues |
| Study design: | All guidelines, reviews, and retrospective, prospective, and basic scientific studies |
The preliminary search strategy included combinations of specific terms for the female erectile tissues [(clitor* or vestibular bulb* or bulbs of the vestibule or bulb of the vestibule) or (female and (corpora spongios* or corpus spongios* or corpus cavernos* or corpora cavernos* or pudendal or orgasm or erectile))], and terms for radiotherapy: radiation or irradiat* or radiotherap* or proton* or brachy*. All full-text studies that were published between 1971 and September 2020, in English, in peer-reviewed journals, and addressed the review question were included.
Two reviewers (D.M. and J.K.) independently screened all titles/abstracts retrieved by the search strategy to identify articles according to the inclusion and exclusion criteria. In case of disagreement, a third independent reviewer was consulted (J.B.). Tiebreak was required in four instances with an inter-rater reliability of 0.90 (95% confidence interval: 0.82, 0.94). Studies were excluded from full-text review when they discussed non-cancer topics or included primary malignancy of the tissues of interest. Studies were also excluded if they exclusively discussed outcomes unrelated to radiotherapy (“non-radiotherapy outcomes”; e.g. surgical outcomes alone without any discussion of radiotherapy outcomes), or reported solely on outcomes unrelated to the function of the erectile tissues (“other morbidities”; e.g. diarrhea).
After initial screening, full text was obtained for further assessment. A standardized data extraction form was used, including authors, year of publication, title, article type, population, aims, methodology, outcomes, and important results. Quality of quantitative publications was assessed using the Quality Assessment Tool for Observational Cohort and Cross-Sectional Studies30 and a numerical analysis regarding the extent, nature and distribution of reports was provided along with a narrative synthesis to describe characteristics of relevant reports. Formal risk of bias assessment was not applicable for this scoping review, consistent with Arksey and O’Malley’s framework29 and Joanna Briggs Institute methodological guidance for Scoping Reviews28.
Results
Of the 55 identified articles (Figure 1), 41 were excluded because they did not meet study inclusion criteria during the initial review process. The reasons they did not meet inclusion criteria were the following: patients with malignancy of the organ (vulva or erectile tissues), n=25; non-radiotherapy outcomes, n=7; non-cancer topics, n=5; and, other morbidities, n=4. Of the 13 remaining articles, 10 were excluded after full-text review. The reasons for exclusion of articles were the following: non-radiotherapy outcomes, n=6; and, other morbidities, n=4.
Figure 1. PRISMA Flow Diagram.
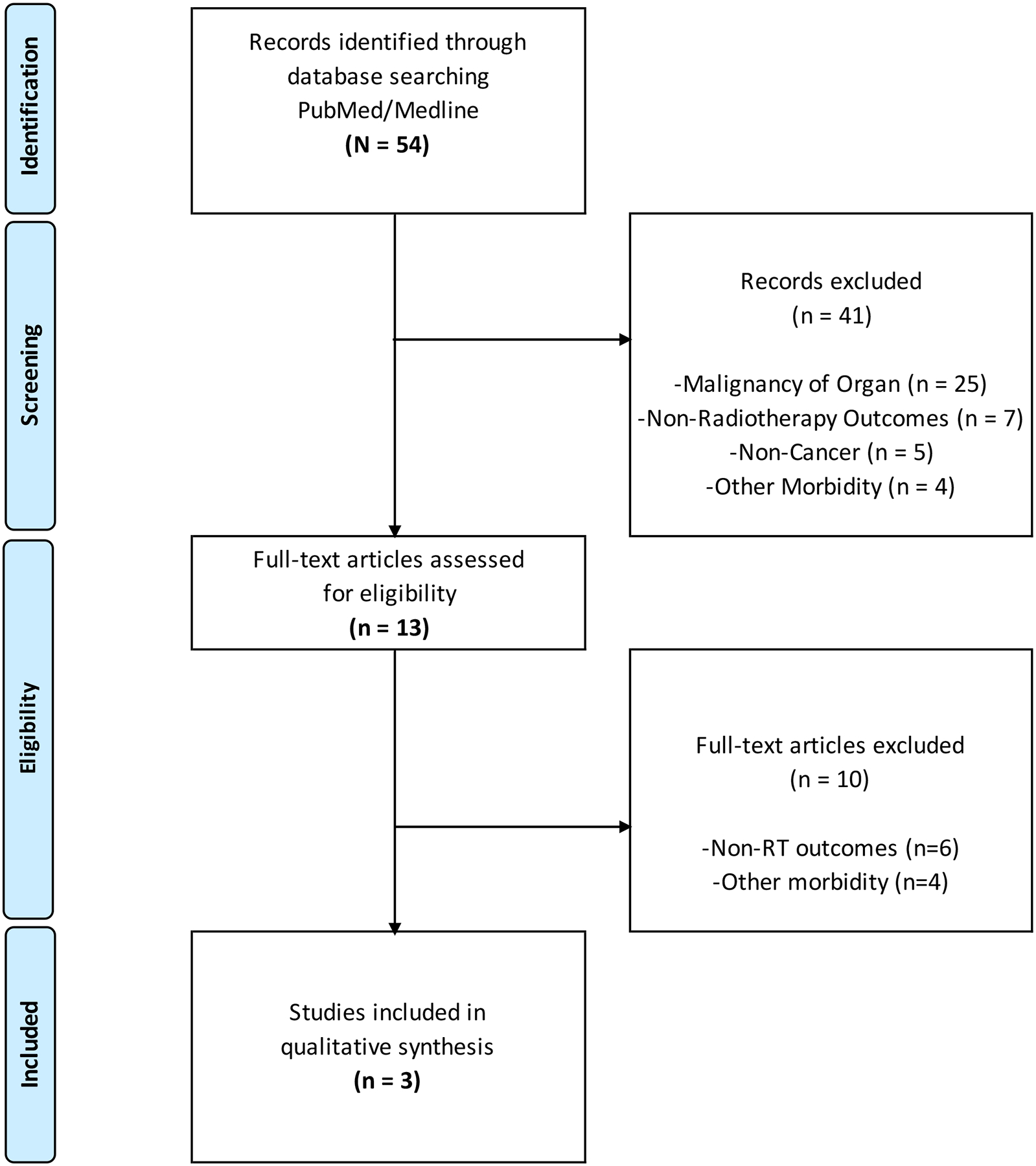
Abbreviations: RT, radiotherapy; PRISMA, Preferred Reporting Items for Systematic Reviews and Meta-Analyses.
Three articles were included in the final review and narrative synthesis (Table 2): one guideline and two non-randomized studies on intervention effects. Articles were published between 2005 and 2015. Both quantitative studies were of good quality but included small sample sizes for pilot data collection and thus had limited scope and generalizability. One study by Pietrangeli et al.31 included a direct assessment of patients receiving surgery and radiotherapy on nerve function of the erectile tissues, however this study included a small number (n=10) of patients who had received chemoradiotherapy and their outcomes were not reported separately for males and females. The quality of this study was poor given the limited pre-post participation rate, small sample size and lack of sample size justification, single post-treatment assessment not completed on all participants, and lack of controlling for confounding variables. The second study by Schroder et al.32 evaluated an intervention to improve sexual outcomes using validated sexual outcome measures and physical exam but was limited to a pilot cohort of 13 female patients.
Table 2.
Study characteristics of articles related to pelvic radiotherapy damage to female erectile tissues
| Authors | Year | Title | Article Type | Population | Aims | Methodology | Outcome Measures | Important Results | Quality |
|---|---|---|---|---|---|---|---|---|---|
| Brooks C, Hansen VN, Riddell A, Harris VA, Tait DM. | 2015 | Proposed genitalia contouring guidelines in anal cancer intensity-modulated radiotherapy. | Guideline | N/A | Description of a genitalia contouring atlas for anal canal carcinoma radiotherapy | Image review, institutional multi-disciplinary team consensus, and literature review | N/A | Contouring guidance for genitalia; genitalia constraints and dose received -- Model dose constraints: V20Gy<50%; V30Gy<35%; V40Gy<5%; Max<48–50Gy. Median Mean Dose: 23.7Gy (22.1– 29.1Gy) | N/A |
| Pietrangeli A, Pugliese P, Perrone M, Sperduti I, Cosimelli M, Jandolo B. | 2009 | Sexual dysfunction following surgery for rectal cancer - a clinical and neurophysiological study. | Non-Randomized Study on Intervention Effects | Total N=57 patients with rectal cancer. N=24 females and N=10 patients also treated with chemoradiation. Males and females in this subgroup were not analyzed independently. Includes a subset analysis of those receiving chemo-radiotherapy. | To evaluate the effect of total mesorectal excision with nerve-sparing on sexual function including innervation of erectile tissues | Structured interview and neuro-psychological tests | Sexual function, sacral reflex, evoked potentials and sympathetic skin responses | 59.6% reported sexual impotence overall. increased sacral reflex and sympathetic skin responses and 10% reporting sexual function abnormality in 3 year time frame. | Poor |
| Schroder M, Mell LK, Hurteau JA, Collins YC, Rotmensch J, Waggoner SE, Yamada SD, Small W Jr, Mundt AJ. | 2005 | Clitoral therapy device for treatment of sexual dysfunction in irradiated cervical cancer patients. | Non-Randomized Study on Intervention Effects | 13 female patients with cervical cancer treated with radiotherapy | Evaluation of the efficacy of a clitoral therapy device in reducing radiation-related sexual dysfunction | Pilot cohort study | Difference from baseline to 3 months on the Female Sexual Function Index, Derogatis Interview for Sexual Functioning, Dyadic Adjustment Scalè | At 3 months, the median Female Sexual Function Index total score increased from 17 to 29.4 (p <0.001); the median Derogatis Interview for Sexual Functioning total raw score increased from 46 to 95 (p <0.001); and, gynecologic examinations revealed improved mucosal color and moisture, vaginal elasticity and decreased bleeding and ulceration. | Good |
Discussion
This systematic scoping review of the radiation oncology literature revealed that consideration of the role of the erectile tissues in female sexual function related to radiotherapy has been limited to three manuscripts31–33. Only the important guideline by Brooks et al.33 for contouring male and female genital structures includes portions of the bulboclitoris (only the glans and body of the clitoris) in the external genitalia contours. However, even here the erectile tissues are combined with cutaneous/subcutaneous tissue and fat, which serve a distinct function from erectile tissue. Given that tissue tolerance for radiation is organ-specific, the erectile tissues likely have a different tolerance for radiation based on unique organ structure and function, requiring high level evidence to test this hypothesis. Further, the female genital structures delineated in external genitalia contours are protected to reduce dermatologic toxicity, rather than to protect the sexual function of the bulboclitoris.
In an important and unique departure from other radiation toxicity papers, Schroder et al.32 discuss a clitoral therapy device to improve sexual pleasure outcomes in female patients treated for cervical cancer, though again focus primarily on the clitoral glans and body in their anatomic approach. Finally, Pietrangeli et al.31 discuss nerve stimulation of the sexual organs, including the bulboclitoris, in a cohort that included 24 female surgical patients with rectal cancer, although attention to female patients in the subset receiving chemoradiotherapy (n=10) was not provided. Outside this review, the general toxicity literature on sexual outcomes after pelvic radiotherapy rarely discusses arousal and orgasm except for in the realm of vaginal sex34–38.
In addition to our limited findings, the minimal evidence base for understanding the impacts of radiotherapy on female erectile tissues is exemplified by the lack of systematic or scoping reviews on this topic. Previous articles have discussed sexual dysfunction caused by cancer care, but not the direct effects of radiotherapy. This is in sharp contrast to the broad evidence base for the impacts of pelvic radiotherapy on male erectile tissues. In this patient population, erectile tissue complications after radiotherapy such as erectile function and ejaculation have been studied in detail23, 24, 39, included as endpoints in clinical trials23–25, and have been used to determine who will benefit from advanced techonologies40. Importantly, these anatomic complications are included as fundamental discussion points in shared decision making with patients – especially since some patients are willing to forgo longevity to avoid sexual dysfunction41. Our findings demonstrate that the function of and damage to female erectile tissues in pelvic cancer patients receiving radiotherapy remains an under-represented scientific domain. Addressing this scarcity of data has a broad and invaluable potential impact as the experience of sexual pleasure is essential to human sexuality across the lifespan, including for cancer survivors, and should receive equitable consideration for females as in males1, 26. Collaborative scientific investigations by clinical, basic and behavioral scientists in oncology and radiotherapy are needed to generate radiobiologic and clinical evidence to advance prospective evaluation, prevention and mitigation strategies that may improve sexual outcomes in female patients. We provide a summary of our recommendations for future research and the potential impact and significance of these investigations in Table 3.
Table 3.
Recommendations for Future Research
| Research Priorities | Research Impact and Significance |
|---|---|
| BASIC, RADIOBIOLOGIC and TRANSLATIONAL RESEARCH | |
Elucidate the impacts of radiation on female erectile tissues and their neurovasculature
|
Will enable the development of precision interventions to prevent or mitigate radiation damage to female erectile tissues, modify individual susceptibility, and manage toxicity progression. |
| Identify erectile-tissue specific dosimetric predictors of organ damage and subsequent dysfunction | Precise dose-volume indices can be identified for use in treatment planning below which the risk of clinically-relevant radiation damage to the erectile tissues and resulting difficulty with orgasm and arousal remains low. Build evidence base for advanced technologies such as proton therapy or MRI-guided radiotherapy. |
| Identify objective quantitative imaging biomarker indices of radiation damage | Objective biomarkers are needed to address multidimensional sexual outcomes, and may improve performance of toxicity probability models. Developing reliable biomarkers of radiation effects in erectile tissues can also be used to improve treatment optimization and inform early interventions. |
| Improve anatomic knowledge of the structure and function of the bulboclitoris organ | Accelerate development of anatomy-directed interventions (e.g. suction devices or topical therapies) by incorporating a detailed understanding of anatomic structure, location and function. |
| CLINICAL RESEARCH | |
| Reclassify sexual quality of life measures using precise understanding of the underlying organ dysfunction that incorporates erectile tissues | Ensure radiation damage and organ dysfunction are aligned, recognizing the impacts of damage to female erectile tissues on sexual quality of life. |
| Revise toxicity criteria and diagnosis codes to include erectile tissue organ dysfunction as a genital or anatomic basis of toxicity. | Allow systematic measurement of arousal/orgasm outcomes related to organ damage to be measured in clinical trials and other studies. |
| Develop reproducible standardized anatomic contours of erectile tissues for females. | Harmonize data across studies and institutions to advance research objectives. Inclusion of the bulboclitoris in radiotherapy planning will reveal the role that bulboclitoris damage plays in altering orgasm and arousal functions after radiotherapy. |
| Determine variability of radiation dose delivered to the bulboclitoris and feasibility of avoidance without compromising tumor control or other important toxicity outcomes. | Bulboclitoris normal tissue complication modeling will generate the first radiation planning indices that can be employed clinically to maintain of a low rate of bulboclitoris-related complications without compromising cancer outcomes. Such modeling is necessary to identify the benefit of advanced technologies or to allow for shared decision making–especially since some patients are willing to trade longevity to avoid sexual dysfunction. Will enable prospective trials such as cooperative group anatomy-sparing phase II trials and/or integration into other therapeutic trials. |
| Elucidate the precise relationship of radiation dose, erectile tissue toxicity, and sexual outcomes such as arousal, orgasm, and dyspareunia. | Provide an evidence base for clinical discussions about late effects of radiotherapy that can be expanded to include female sexual pleasure. |
| Elucidate the relationship between erectile tissue function and multimodality cancer care (surgery, endocrine therapies, ovarian failure), biopsychosocial aspects of sexuality, and social determinants of health | Improve the performance of toxicity models using multidimensional predictors sexual outcomes. Identify needs for multidisciplinary team-based approaches to managing sexual outcomes in cancer survivorship. |
| Evaluate equitable distribution of radiotherapy resources related to sexual outcomes. | Improve equity in the investment of research and development funding and generate evidence to support equitable distribution of advanced technologies. |
| EDUCATION | |
| Develop education interventions for radiation oncology clinicians about the structure, function and importance of bulboclitoris anatomy to female sexual outcomes. | Empower clinicians to incorporate female sexual pleasure and relevant anatomy into clinical decision-making. |
| Develop patient-provider educational interventions on incorporating erectile tissue toxicity into discussions about treatment-related toxicity and exploration of shared decision-making. | Normalize female sexual pleasure as an important aspect of sexuality in cancer survivorship and re-orient discussions about sexual outcomes to prioritize maintenance of sexual pleasure in addition to vaginal health. |
Limitations of this review include the inclusion of articles written only in English. In addition, our search criteria included only full-text articles and does not include research that may have been presented at conferences and is yet to be published in a peer-reviewed journal. In addition, since our review only focused on female erectile tissues, sexual dysfunction in female cancers as a whole is not addressed.
Our next steps are guided by our primary finding of the omission of female erectile tissues from investigations of radiation toxicities, which precludes the development of robust interventions to prevent, mitigate and treat sexual toxicities related to cancer treatment. The evidence synthesized by this review and the knowledge gap revealed, justifies and informs future foundational studies necessary to understand the effect of radiotherapy on normal female erectile tissues and the resultant impact on clinical outcomes.
Conclusion
The lack of research on the impact of radiotherapy on female erectile tissues is a problem that needs to be addressed to provide comprehensive evidence-based survivorship care in sexual health for female patients. Further investigation is essential to develop effective interventions to prevent and mitigate treatment-related toxicity due to radiotherapy damage to the female erectile tissues.
Acknowledgements:
We gratefully acknowledge and thank Rachel Pinotti, MLIS, Director or Library Education & Research Services at the Icahn School of Medicine at Mount Sinai, for her assistance in designing a comprehensive search strategy for this project. We also gratefully acknowledge the feedback of Dr. Gwendolyn Quinn, Professor at the NYU School of Medicine for her contributions to the manuscript.
Funding Statement:
Research reported in this publication was supported by the National Cancer Institute of the National Institutes of Health [T32CA225617; UG1CA189867 (NRG Oncology Foundation, Inc.)] and the Office of the Director, National Institutes of Health (DP5OD031876). Role of the Funder/Sponsor: The funders had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication. Any opinions, findings, and conclusions expressed in this material are those of the author(s) and do not necessarily reflect those of the National Institutes of Health.
Footnotes
Conflicts of Interest: None
REFERENCES
- 1.Lindau ST, Abramsohn EM, Matthews AC. A manifesto on the preservation of sexual function in women and girls with cancer. Am J Obstet Gynecol. 2015;213:166–174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bruner DW, Lanciano R, Keegan M, Corn B, Martin E, Hanks GE. Vaginal stenosis and sexual function following intracavitary radiation for the treatment of cervical and endometrial carcinoma. Int J Radiat Oncol Biol Phys. 1993;27:825–830. [DOI] [PubMed] [Google Scholar]
- 3.Grigsby PW, Russell A, Bruner D, et al. Late injury of cancer therapy on the female reproductive tract. Int J Radiat Oncol Biol Phys. 1995;31:1281–1299. [DOI] [PubMed] [Google Scholar]
- 4.Canty J, Stabile C, Milli L, Seidel B, Goldfrank D, Carter J. Sexual Function in Women with Colorectal/Anal Cancer. Sex Med Rev. 2019;7:202–222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Seguin L, Touzani R, Bouhnik AD, et al. Deterioration of Sexual Health in Cancer Survivors Five Years after Diagnosis: Data from the French National Prospective VICAN Survey. Cancers (Basel). 2020;12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Abbott-Anderson K, Kwekkeboom KL. A systematic review of sexual concerns reported by gynecological cancer survivors. Gynecol Oncol. 2012;124:477–489. [DOI] [PubMed] [Google Scholar]
- 7.Lammerink EA, de Bock GH, Pras E, Reyners AK, Mourits MJ. Sexual functioning of cervical cancer survivors: a review with a female perspective. Maturitas. 2012;72:296–304. [DOI] [PubMed] [Google Scholar]
- 8.Jensen PT, Froeding LP. Pelvic radiotherapy and sexual function in women. Transl Androl Urol. 2015;4:186–205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Jensen PT, Groenvold M, Klee MC, Thranov I, Petersen MA, Machin D. Longitudinal study of sexual function and vaginal changes after radiotherapy for cervical cancer. Int J Radiat Oncol Biol Phys. 2003;56:937–949. [DOI] [PubMed] [Google Scholar]
- 10.Bergmark K, Avall-Lundqvist E, Dickman PW, Henningsohn L, Steineck G. Vaginal changes and sexuality in women with a history of cervical cancer. N Engl J Med. 1999;340:1383–1389. [DOI] [PubMed] [Google Scholar]
- 11.Flay LD, Matthews JH. The effects of radiotherapy and surgery on the sexual function of women treated for cervical cancer. Int J Radiat Oncol Biol Phys. 1995;31:399–404. [DOI] [PubMed] [Google Scholar]
- 12.Wallington DG, Holliday EB. Preparing Patients for Sexual Dysfunction After Radiation for Anorectal Cancers: A Systematic Review. Pract Radiat Oncol. 2021;11:193–201. [DOI] [PubMed] [Google Scholar]
- 13.Cherven B, Sampson A, Bober SL, et al. Sexual health among adolescent and young adult cancer survivors: A scoping review from the Children’s Oncology Group Adolescent and Young Adult Oncology Discipline Committee. CA Cancer J Clin. 2021;71:250–263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Yerramilli D, Drapek L, Nipp RD, et al. Sexual Function, Quality of Life, and Mood After Radiation Therapy in Patients with Anal Cancer. J Gastrointest Cancer. 2020;51:204–210. [DOI] [PubMed] [Google Scholar]
- 15.Incrocci L, Jensen PT. Pelvic radiotherapy and sexual function in men and women. J Sex Med. 2013;10 Suppl 1:53–64. [DOI] [PubMed] [Google Scholar]
- 16.Candy B, Jones L, Vickerstaff V, Tookman A, King M. Interventions for sexual dysfunction following treatments for cancer in women. Cochrane Database Syst Rev. 2016;2:CD005540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Marshall DC, Ghiassi-Nejad Z, Powers A, et al. A first radiotherapy application of functional bulboclitoris anatomy, a novel female sexual organ-at-risk, and organ-sparing feasibility study. Br J Radiol. 2021;94:20201139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.O’Connell HE, Sanjeevan KV, Hutson JM. Anatomy of the clitoris. J Urol. 2005;174:1189–1195. [DOI] [PubMed] [Google Scholar]
- 19.Di Marino V, Lepidi H. Anatomic Study of the Clitoris and the Bulbo-Clitoral Organ. 1st ed. Cham: Springer International Publishing : Imprint: Springer,; 2014:1 online resource (XV, 152 pages 109 illustrations, 103 illustrations in color. [Google Scholar]
- 20.Hite S The New Hite Report. 2nd ed. ed. London: Hamlyn; 2000. [Google Scholar]
- 21.Masters WH, Johnson VE. Human sexual response. London: Churchill; 1966. [Google Scholar]
- 22.Stabile C, Goldfarb S, Baser RE, et al. Sexual health needs and educational intervention preferences for women with cancer. Breast Cancer Res Treat. 2017;165:77–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lee JY, Spratt DE, Liss AL, McLaughlin PW. Vessel-sparing radiation and functional anatomy-based preservation for erectile function after prostate radiotherapy. Lancet Oncol. 2016;17:e198–208. [DOI] [PubMed] [Google Scholar]
- 24.Roach M 3rd, Nam J, Gagliardi G, El Naqa I, Deasy JO, Marks LB. Radiation dose-volume effects and the penile bulb. Int J Radiat Oncol Biol Phys. 2010;76:S130–134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Donovan JL, Hamdy FC, Lane JA, et al. Patient-Reported Outcomes after Monitoring, Surgery, or Radiotherapy for Prostate Cancer. N Engl J Med. 2016;375:1425–1437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Heiman JR, Guess MK, Connell K, et al. Standards for clinical trials in sexual dysfunctions of women: research designs and outcomes assessment. J Sex Med. 2004;1:92–97. [DOI] [PubMed] [Google Scholar]
- 27.Tricco AC, Lillie E, Zarin W, et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation. Ann Intern Med. 2018;169:467–473. [DOI] [PubMed] [Google Scholar]
- 28.Peters MDJ, Marnie C, Tricco AC, et al. Updated methodological guidance for the conduct of scoping reviews. JBI Evid Synth. 2020;18:2119–2126. [DOI] [PubMed] [Google Scholar]
- 29.Arksey H, O’Malley L. Scoping Studies: Towards a Methodological Framework. International Journal of Social Research Methodology: Theory & Practice. 2005;8:19–32. [Google Scholar]
- 30.National Institutes of Health. Quality Assessment Tool for Observational Cohort and Cross-Sectional Studies. Bethesda, MD. 2014. Available at: https://www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools. Accessed: August 2021. Last Updated: July 2021. [Google Scholar]
- 31.Pietrangeli A, Pugliese P, Perrone M, Sperduti I, Cosimelli M, Jandolo B. Sexual dysfunction following surgery for rectal cancer - a clinical and neurophysiological study. J Exp Clin Cancer Res. 2009;28:128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Schroder M, Mell LK, Hurteau JA, et al. Clitoral therapy device for treatment of sexual dysfunction in irradiated cervical cancer patients. Int J Radiat Oncol Biol Phys. 2005;61:1078–1086. [DOI] [PubMed] [Google Scholar]
- 33.Brooks C, Hansen VN, Riddell A, Harris VA, Tait DM. Proposed genitalia contouring guidelines in anal cancer intensity-modulated radiotherapy. Br J Radiol. 2015;88:20150032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Berkey FJ. Managing the adverse effects of radiation therapy. Am Fam Physician. 2010;82:381–388, 394. [PubMed] [Google Scholar]
- 35.Koontz BF. Radiation therapy treatment effects: an evidence-based guide to managing toxicity. New York: Demos; 2018. [Google Scholar]
- 36.Halperin E, Wazer D, Perez C, (eds). Perez & Brady’s Principles and Practice of Radiation Oncology. 7th ed. Philadelphia: Wolters Kluwer; 2018. [Google Scholar]
- 37.Tepper J, Foote R, Michalski J, (eds). Gunderson & Tepper’sClinical Radiation Oncology. 5th ed. Philadelphia: Elsevier Inc.; 2015. [Google Scholar]
- 38.Hansen E, Roach M 3rd, (eds). Handbook of Evidence-Based Radiation Oncology. 3rd ed. Cham, Switzerland: Springer International Publishing AG, part of Springer Nature; 2018. [Google Scholar]
- 39.Gay HA, Barthold HJ, O’Meara E, et al. Pelvic normal tissue contouring guidelines for radiation therapy: a Radiation Therapy Oncology Group consensus panel atlas. Int J Radiat Oncol Biol Phys. 2012;83:e353–362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Story MD, Wang J. Developing Predictive or Prognostic Biomarkers for Charged Particle Radiotherapy. Int J Part Ther. 2018;5:94–102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Masya LM, Young JM, Solomon MJ, Harrison JD, Dennis RJ, Salkeld GP. Preferences for outcomes of treatment for rectal cancer: patient and clinician utilities and their application in an interactive computer-based decision aid. Dis Colon Rectum. 2009;52:1994–2002. [DOI] [PubMed] [Google Scholar]


