Abstract
Objective
Pasteurization kills harmful microorganisms found in milk. While consumption of unpasteurized milk and its products is discouraged due to increased risk of infections, some individuals prefer unpasteurized dairy products. Our objective was to estimate the burden of illness from outbreaks arising from consumption of unpasteurized and pasteurized dairy products in Canada and the United States.
Methods
We conducted a systematic review of dairy-associated outbreaks in Canada and the USA from 2007 onward. We searched MEDLINE, Embase, Cochrane Library, TRIP Database for guidelines, and North American government agency websites up to October 2020. We included outbreak reports where the pathogenic microbe was confirmed in both the patient and the dairy product through laboratory testing.
Synthesis
Thirty-two disease outbreaks were linked to dairy consumption. Twenty outbreaks involving unpasteurized products resulted in 449 confirmed cases of illness, 124 hospitalizations, and five deaths. Twelve outbreaks involving pasteurized products resulted in 174 confirmed cases of illness, 134 hospitalizations, 17 deaths, and seven fetal losses. Listeria accounted for 10 out of 12 outbreaks from pasteurized products from 2007 through 2020.
Conclusion
Public warnings about the risk of unpasteurized dairy consumption need to continue and pregnant women and immunocompromised hosts need to be made aware of foods at high risk of contamination with Listeria.
Supplementary Information
The online version contains supplementary material available at 10.17269/s41997-022-00614-y.
Keywords: Dairy products, Raw foods, Pasteurization, Disease outbreak, Listeria
Résumé
Objectif
La pasteurisation tue les micro-organismes dangereux contenus dans le lait. Même si la consommation du lait non pasteurisé et ses produits fût déconseillée en raison d’un risque accru d’infection, certaines personnes préfèrent des produits laitiers non pasteurisés. Notre objectif était d’évaluer le fardeau de maladie des éclosions résultant de la consommation des produits laitiers non pasteurisés et pasteurisés au Canada et aux États-Unis.
Méthode
Nous avons mené une revue systématique des éclosions liées aux produits laitiers au Canada et aux États-Unis depuis 2007. Nous avons cherché dans MEDLINE, Embase, Cochrane Library, TRIP Database et les sites web des agences gouvernementales Nord-Américaines pour la période 2007 jusqu’au mois d’octobre 2020. Nous avons inclus des rapports d’éclosion lorsque les essais en laboratoire ont confirmé la présence du microbe pathogène dans le patient ainsi que dans le produit laitier.
Résultats
Trente-deux éclosions étaient liées à la consommation des produits laitiers. Les produits non pasteurisés étaient impliqués dans 20 éclosions, avec 449 cas de maladie confirmés, 124 hospitalisations et 5 morts. Les produits pasteurisés étaient impliqués dans 12 éclosions, avec 174 cas de maladie confirmés, 134 hospitalisations, 17 morts et sept morts fœtales. Listeria comptait pour 10 des 12 éclosions des produits pasteurisés de 2007 à 2020.
Conclusion
Les avis publics au sujet du risque de la consommation des produits laitiers non pasteurisés devraient continuer et les femmes enceintes et les hôtes immunodéprimés devraient être informés de la nourriture à haut risque de la contamination avec Listeria.
Mots-clés: Produits laitiers, aliments crus, pasteurisation, éclosion de maladie, Listeria
Introduction
Prior to the advent of pasteurization in the late nineteenth century, animal milk was a major cause of foodborne illness (Steele 2000). During pasteurization, milk is heated and then rapidly cooled; the length of time required to kill pathogens is inversely correlated with the temperature that is achieved (Lejeune and Rajala-Schultz 2009). Upon recognition of its importance as a public health measure, pasteurization was mandated in parts of Canada and the United States (USA) in the early 1900s, and legislated federally in Canada since 1991 (Steele 2000; Health Canada 2013). However, regulatory practices regarding the pasteurization of dairy products differ across jurisdictions. In Canada, the sale of unpasteurized milk is illegal, but farm families can consume unpasteurized milk from their own cows (Health Canada 2013). In the USA, interstate sale of unpasteurized milk has been prohibited since 1987 but some jurisdictions permit sales within the state (U.S. Food and Drug Administration 1987). Persons interested in procuring unpasteurized milk in both Canada and the USA can participate in “cow shares” whereby groups of people buy or lease a cow and its milk. Cheese made from unpasteurized milk is permitted for sale in Canada and the USA, provided it has been aged for minimum 60 days (Health Canada 2013; U.S. Food and Drug Administration 2020; Centers for Disease Control and Prevention, 2017a).
Contamination of unpasteurized dairy products can occur by a variety of mechanisms: direct contact with bovine feces, transmission of the organisms from bovine skin/hide, bovine mastitis, primary bovine diseases (i.e., tuberculosis), and environmental contamination from insects, other animals, or humans (Centers for Disease Control and Prevention, 2017a). Multiple microbial etiologies have been linked to unpasteurized dairy outbreaks, including Campylobacter spp., Listeria monocytogenes, bovine tuberculosis, Streptococcus spp., Escherichia coli, brucellosis, salmonellosis, and other enteric pathogens (Centers for Disease Control and Prevention, 2017a). The ubiquity of pasteurization has reduced the proportion of foodborne illness attributable to unpasteurized dairy products from approximately 25% pre-pasteurization to approximately 2% in the twenty-first century (Christidis et al. 2016; Lejeune and Rajala-Schultz 2009). Although the risk is far lower with pasteurized dairy products, they are also a source of illness due to inadequate pasteurization or contamination between pasteurization and consumption (Heiman et al. 2015; Gaulin et al. 2012; Centers for Disease Control and Prevention, 2017a). Process contamination can occur at the production, processing, distribution, or preparation steps.
Both Health Canada and the Centers for Disease Control (CDC) in the USA advise the public that consumption of unpasteurized milk is associated with an increased risk of serious illness, particularly for children, pregnant women, the elderly, and those with compromised immune systems (Centers for Disease Control and Prevention, 2017a; Health Canada 2013). The American Academy of Pediatrics also released a statement in 2014 advising against consumption of unpasteurized milk by children (Committee on Infectious Diseases, Committee on Nutrition for the American Academy of Pediatrics 2014). Despite widespread public health messaging around the dangers of unpasteurized milk, the 2004 Canadian Community Health Survey, which uses in-person and telephone interviews, revealed that 3.6% of participants consumed unpasteurized milk in the seven days prior to the interview (Public Health Agency of Canada 2012). A similar prevalence was reported in Ontario in 2011 (1.84%; 95% CI 0.75–3.74) (Public Health Ontario, Raw Milk Working Group, 2013). In a survey of American adults, the prevalence of unpasteurized milk consumption was 2.1% and 2.4% in females and males respectively in 2006 (Shiferaw et al. 2012), while 3.0% of Americans reported consuming unpasteurized milk in the past seven days in a different 2006–2007 survey (Centers for Disease Control and Prevention, 2007). Consumer reasons for unpasteurized milk preference included consuming food in its “purest” form, purported nutritional benefits, better taste, and supporting farmers (Leamy et al. 2014). While difficult to compare subjective differences such as the taste of the product, numerous studies have demonstrated that pasteurized milk contains equivalent nutrients to unpasteurized milk (Jay-Russell 2010; Lejeune and Rajala-Schultz 2009).
Foodborne outbreaks reported to the CDC are available through The National Outbreak Reporting System (NORS) which defines a foodborne outbreak as “two or more persons experience a similar illness resulting from the ingestion of a common food” (Centers for Disease Control and Prevention 2015). Outbreaks linked to the consumption of unpasteurized dairy products from 1973 through 2012 were previously compiled in multiple reviews to estimate the magnitude of the problem and examine the association between state laws and the number and type of outbreaks. All the reviews found that more outbreaks occurred in states with legal unpasteurized milk sales (Headrick et al. 1998; Langer et al. 2012; Mungai et al. 2015), although dairy legal status is not the only determinant of an outbreak (Whitehead and Lake 2018). From 2009 to 2015, dairy was the second most common food category after fish associated with foodborne outbreaks in the USA (fish: 222 outbreaks (17%); dairy: 136 outbreaks (11%)) (Dewey-Mattia et al. 2018). The majority of the dairy outbreaks (80%, n=109) were from unpasteurized products, while 15% (n=20) were from pasteurized dairy products and the remaining 5% (n=7) had unknown pasteurization status (Dewey-Mattia et al. 2018). Despite legislation, widespread pasteurization, and advice from multiple health organizations, clearly outbreaks of illness linked to consumption of unpasteurized milk and cheese made from unpasteurized milk continue to occur.
The purpose of this systematic review was to determine the burden of illness linked to the consumption of unpasteurized versus pasteurized dairy in Canada and the USA from 2007 onward to characterize differences in the populations infected, the pathogens, and outcomes.
Methods
The methodology for this review was established a priori and the protocol registered with PROSPERO: the International Prospective Register of Systematic Reviews (CRD42017076479). The original protocol included outbreak reports from Canada pre-2007, but this was modified in order to analyze Canadian and American data from the same timeframe. Pre-2007 outbreak data in the USA had previously been analyzed.
Search
We searched electronic databases: Ovid MEDLINE (1946-), Ovid EMBASE (1974-), and the Wiley Cochrane Library (inception-) up to May 24, 2017. The search was updated on October 1, 2020. Our search strategy was designed and executed by a health research librarian and peer-reviewed by a second librarian, as recommended by the Peer Review of Electronic Search Strategies (PRESS) guideline statement (McGowan et al. 2016). The strategy combined controlled vocabulary terms (e.g., MeSH) and text words (i.e., title and abstract terms) for concepts related to dairy products and outbreaks in Canada and the USA (see Appendix 1 for the full search strategy).
Additional search sources included guidelines on unpasteurized dairy consumption: the TRIP (Turning Research Into Practice) Database and the National Guidelines Clearinghouse. We also searched websites of Canadian and US government agencies for reports of outbreaks from dairy consumption: Canadian Food Inspection Agency (CFIA), Canadian Institute for Health Information (CIHI), CDC, Public Health Agency of Canada (PHAC), and the United States Department of Agriculture (USDA). These additional searches were conducted October 1–5, 2020. Finally, reports of outbreaks associated with unpasteurized and pasteurized milk/dairy products were requested from the Publicly Available International Foodborne Outbreak Database (PAIFOD) maintained by PHAC. Selected studies were limited to those written in either English or French and linked geographically to Canada or the USA. Search results were exported to EndNote X9 (Clarivate) for primary (title and abstract) and secondary (full text) screening. The reference lists of included studies were also hand-searched.
Inclusion criteria
We included any type of article that described the sequelae (e.g., hospitalizations, mortality) of an outbreak of disease in two or more people of any age epidemiologically linked to the consumption of pasteurized or unpasteurized dairy products from any animal in Canada or the USA from 2007 to October 2020. To be epidemiologically linked, the same pathogenic microbe had to be confirmed by laboratory testing to be present in at least one patient AND the suspected dairy source. Isolates had to closely match if any method of typing was performed. We did not include reports from the NORS database or reviews published since 2007 using only NORS data as we used a stricter definition of epidemiologically linked. We chose the year 2007 as US outbreak data from pasteurized and unpasteurized dairy sources from 1993 to 2006 were previously synthesized and published, and subsequent syntheses only examined unpasteurized dairy outbreaks (Langer et al. 2012; Mungai et al. 2015; Whitehead and Lake 2018). We excluded studies of human breast milk, eggs, and zoonoses not passed through dairy products. Commentaries, editorials, letters, and abstracts were also excluded.
Study selection
Study selection occurred in two phases. In the first phase, two independent reviewers screened the titles and abstracts of all the records based on pre-determined inclusion/exclusion criteria. The studies that met the inclusion criteria were then referred to the secondary screening phase, at which time two reviewers independently reviewed the full text of each article to determine eligibility. Disagreements at each stage were resolved by consensus, or by the decision of a third party.
Quality assessment
The methodological quality of the included outbreak studies was evaluated by two independent reviewers using the quantitative (non-randomized controlled trial) and quantitative (descriptive) sections of the Mixed Methods Appraisal Tool (MMAT) with consensus reached through discussion (Pluye et al. 2011).
Data extraction
Data extraction was completed by one team member with verification by another using a pre-designed and pilot-tested data extraction form. The following data were collected: study characteristics, patient demographics and outcome data including number of hospitalized patients, number and type of complications, pathogenic microbe, type of dairy product (e.g., fluid milk, cheese, ice cream, yogurt, powdered milk product), pasteurization status of dairy product, and type of microbiologic testing.
Data analysis
Studies were separated by pasteurization status and case determination (laboratory-confirmed cases vs. suspected cases) for reporting in tables. Case definitions were specific to each study. Confirmed cases were epidemiologically linked to the outbreak based on bacterial isolate testing in the patient and the outbreak source, while suspected cases were based on the patient having the same symptoms and a known link to a proven case or the proven source during the same time frame. Data for both confirmed and suspected cases were pooled to report frequencies and compare rates. Fisher’s exact test was used post hoc to compare Listeria rates between groups (i.e., unpasteurized vs. pasteurized) as Listeria was so predominant in the outbreaks despite pasteurization.
Results
Search results
The search identified 5245 unique records from which 31 studies met the inclusion criteria; 20 examined outbreaks due to unpasteurized dairy consumption while 11 reported on 12 outbreaks from pasteurized dairy sources (Figure 1). The included outbreak studies were mostly case reports/case series. Study characteristics are outlined in Table 1 (unpasteurized dairy products) and Table 2 (pasteurized dairy products) and full references are available in Appendix 2.
Fig. 1.
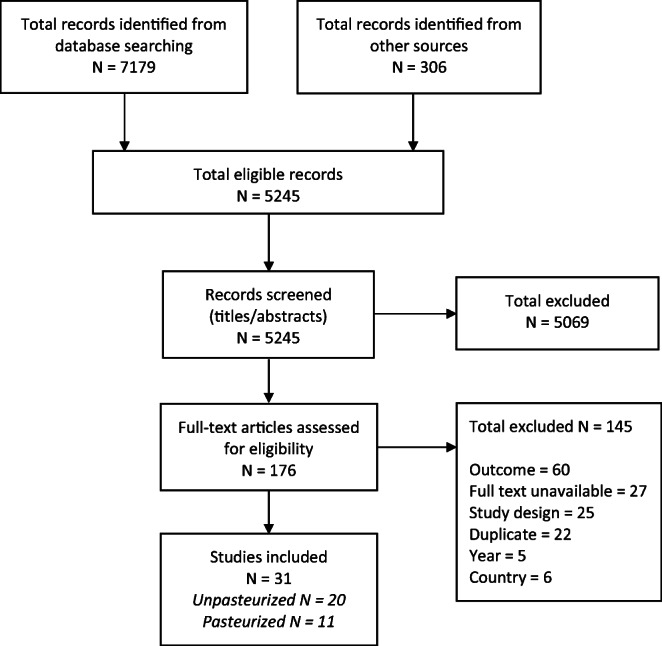
PRISMA diagram illustrating flow of citations through the screening and selection process
Table 1.
Studies reporting outbreaks linked to unpasteurized dairy products
| Study | Location | Strain | Source | Total cases | Adult cases | Peds cases | Hospitalizations | Deaths | Median age [yrs] (range) |
|---|---|---|---|---|---|---|---|---|---|
| Unpasteurized dairy products (confirmed cases only) | |||||||||
| Boyd (2021) | British Columbia | Escherichia coli O121 | Gouda-like cheese made from unpasteurized milk | 7 | 7 | 0 | 0 | 0 | 28 (22–64) |
| Burakoff (2018) | Colorado | Campylobacter jejuni | Soft cheese made from unpasteurized milk | 17 | NR | NR | 1 | 0 | 58 (12–68) |
| CDC (2017b) | 4 states (CT, FL, NY, VT) | Listeria monocytogenes | Soft cheese made from unpasteurized milk | 8 | NR | NR | 8 | 2 | 52 (<1–89) |
| Rosbach (2017) | Washington | Salmonella enterica serotype Dublin | Unpasteurized cow milk | 2 | NR | NR | 2 | 0 | NR |
| CDC (2016) | California, Florida | Listeria | Unpasteurized cow milk | 2 | 2 | NA | 2 | 1 | 77 (73–81) |
| Chen (2016) | Utah | Salmonella enterica serotype Saintpaul | Unpasteurized milk | 9 | NR | NR | 2 | 0 | NR (15–78) |
| Rosenthal (2015) | Idaho | Cryptosporidium parvum | Unpasteurized goat milk | 11 | NR | NR | 1 | NR | 11 (2 months–76 yrs) |
| Castrodale (2013) | Alaska | Campylobacter jejuni | Unpasteurized cow milk | 18 | NR | NR | NR | NR | NR |
| Longenberger (2013) | 4 states (MD, NJ, PA, WV) | Campylobacter jejuni | Unpasteurized cow milk | 81 | 56 | 25 | 10 | 0 | 31 (2–74) |
| McCollum (2012) | 5 states (AZ, CA, CO, NM, NV) | Escherichia coli O157:H7 | Aged gouda cheese made from unpasteurized milk | 41 | NR | NR | 18 (7 peds) | 0 | 16 (1–85) |
| CDC (2010) | Utah | Salmonella enterica serotype Newport | Unpasteurized milk | 10 | NR | NR | 1 | NR | 21 (2–56) |
| California Dept. Public Health (CDPH 2008) | California | Campylobacter jejuni | Unpasteurized cow milk | 16 | NR | NR | 2 | 0 | 48 (4–70) |
| CDC (2008b) | Illinois | Salmonella enterica serotype Newport | Unpasteurized Mexican-style aged cheese | 85 | NR | NR | 36 | 0 | 34 (9 days–85 yrs) |
| CDC (2007) | Pennsylvania | Salmonella enterica serotype Typhimurium | Unpasteurized cow milk and unregulated queso fresco made from the same raw milk source | 29 | NR | NR | 2 | 0 | 6 (5 months–76 yrs) |
| Unpasteurized dairy products (confirmed and suspected cases) | |||||||||
| Currie (2018) | British Columbia | Escherichia coli O157:H7 | Gouda cheese made from unpasteurized milk | 29 | NR | NR | 5 | 1 | 28 (3–82) |
| Davis (2016) | Utah | Campylobacter jejuni | Unpasteurized cow milk | 99 | 55 | 44 | 10 | 1 | 23 (1–74) |
| Weltman (2013) | Pennsylvania | Campylobacter jejuni | Unpasteurized cow milk | 8 | 4 | 4 | NR | NR | NR |
| Northlands News Center (2013) | Minnesota | Salmonella enterica serotype Typhimurium | Unpasteurized Mexican-style aged cheese | 25 | NR | NR | 15 | 0 | NR |
| Beecher (2012) | Oregon | Escherichia coli O157 | Unpasteurized cow milk | 19 | 4 | 15 | 4 | NR | NR |
| Guh (2010) | Connecticut | Escherichia coli O157:NM | Unpasteurized cow milk | 14 | 4 | 10 | 5 (4 peds) | 0 | 5 (1–81) |
Note: References for studies without hyperlinks can be found in Appendix 2
NA not applicable, NR not reported
*Primary cases only, there were 18 secondary cases not included here.
AZ Arizona, CA California, CO Colorado, CT Connecticut, FL Florida, MD Maryland, NM New Mexico, NJ New Jersey, NV Nevada, NY New York, PA Pennsylvania, VT Vermont, WV West Virginia
Table 2.
Studies reporting outbreaks linked to pasteurized dairy products
| Study | Location | Strain | Source | Total cases | Adult cases | Peds cases | Hospitalizations | Deaths | Median age [yrs] (range) |
|---|---|---|---|---|---|---|---|---|---|
| Pasteurized dairy products (confirmed cases only) | |||||||||
| Rosen (2020) | California | Clostridium botulinum | Pasteurized nacho cheese sauce | 10 | NR | NR | 10 | 1 | 34 (NR) |
| Hanson (2019) | Ontario | Listeria monocytogenes | Pasteurized chocolate milk | 34 | NR | NR | 12 | 4 | 73 (NR) |
| Rietberg (2016) | Washington | Listeria monocytogenes | Liquid ice cream mix from pasteurized milk | 2 | 2 | NA | 1 | 0 | NR |
| Heiman (2015) | 13 states and DC (CA, CO, MA, MD, MN, NE, NJ, NM, NY, OH, PA, VA, WA) | Listeria monocytogenes | Soft cheese made from pasteurized milk | 22 | NR | NR | 20 | 4 | 77 (30–87) |
| CDC (2014) | CA, MD | Listeria monocytogenes | Soft or semi-soft Hispanic-style cheese from pasteurized milk | 8 | 5 | 3 | 7 | 1 | NR |
| Longenberger (2014) | Pennsylvania | Yersinia enterocolitica | Improperly pasteurized cow milk | 16 | NR | NR | 7 | 1 | 27 (1–76) |
| CDC (2013) | 5 states (IL, IN, MN, OH, TX) | Listeria monocytogenes | Soft ripened cheese made from pasteurized milk | 6 | 6 | NA | 6 | 1 | 55 (30–67) |
| Gaulin (2012) | Quebec | Listeria monocytogenes P93 | Soft washed-rind cheese made from pasteurized cow milk | 38 |
38 with 16 pregnant women |
NA |
37 with 16 pregnant women |
2 | 65 (28–89) Pregnant 31 (23–36) |
| Jackson (2011) | 5 states (GA, IL, NC, TN, WI) | Listeria monocytogenes | Mexican-style cheeses produced from pasteurized milk | 8 |
7 with 5 pregnant women |
1 |
4 (1 peds, 3 pregnant women) |
NR |
Child: 3 Adult: 31.5 (21–43) |
| CDC (2008) | Massachusetts | Listeria monocytogenes | Pasteurized cow milk | 5 | 5 | NA | 5 | 3 | 75 (31–87) |
| Pasteurized dairy products (confirmed and suspected cases) | |||||||||
|
McIntyre (2015) Outbreak A |
British Columbia | Listeria monocytogenes | Soft cheese made from pasteurized cow and goat milk | 49 | NR | NR | NR | NR | 49 (4–85) |
|
McIntyre (2015) Outbreak B |
British Columbia | Listeria monocytogenes | Soft cheese made from pasteurized cow and goat milk | 86 | NR | NR | NR | NR | 46 (14–76) |
Note: References for studies without hyperlinks can be found in Appendix 2
NA not applicable, NR not reported
CA California, CO Colorado, GA Georgia, IL Illinois, IN Indiana, MA Massachusetts, MD Maryland, MN Minnesota, NC North Carolina, NE Nebraska, NJ New Jersey, NM New Mexico, NY New York, OH Ohio, PA Pennsylvania, TN Tennessee, TX Texas, VA Virginia, WA Washington, WI Wisconsin
Outbreaks linked to unpasteurized dairy products
Twenty outbreaks were reported: 14 outbreaks (70%) involving unpasteurized fluid milk (cow milk (n=11), goat milk (n=1), unknown animal (n=2)); seven (35%) involving cheese made from unpasteurized milk with one outbreak linked to both contaminated fluid milk and cheese made from the milk. One outbreak was caused by the parasite Cryptosporidium parvum while the others were caused by bacteria: Campylobacter jejuni (n=6; 30%), Salmonella enterica (n=6; 30%), enterohemorrhagic Escherichia coli (n=5; 25%) and Listeria spp. (n=2; 10%).
From the 20 outbreaks, 530 illnesses were reported, with 449 (85%) being confirmed and 81 (15%) being suspected, with 98 (18%) pediatric cases (confirmed and suspected). Age range was nine days to 91 years with 51% of the cases being male. There were 124 hospitalizations (124/530, 23%; 2 studies did not report hospitalizations) (Table 3). Rare, serious complications, when reported, included six cases of hemolytic uremic syndrome (HUS) (Beecher 2012; Currie et al. 2018; Guh et al. 2010; McCollum et al. 2012) and one adult case of thrombotic thrombocytopenic purpura (TTP) (Guh et al. 2010), all of which were associated with enterohemorrhagic E. coli outbreaks. One case of acute motor axonal neuropathy (AMAN) (a form of Guillain-Barre Syndrome) was reported in an outbreak of Campylobacter jejuni (California Department of Public Health 2008; Gerner-Smidt and Whichard 2009). Five deaths were reported among 530 cases (0.9%; 5 studies did not report mortality). Three were due to listeriosis (Centers for Disease Control and Prevention, 2016, 2017b), one was due to E. coli O157:H7 (Currie et al. 2018), and one was due to a combination of Campylobacter jejuni gastroenteritis and chronic medical problems (Davis et al. 2016).
Table 3.
Reported outcomes across included studies
| Outcomes | Unpasteurized (530 cases) N (%) |
Pasteurized (284 cases) N (%) |
|---|---|---|
| Hospitalizations | 124 (23.4) | 134 (47.2) |
| HUS cases | 6 (1.1) | 0 |
| TTP | 1 (0.2) | 0 |
| AMAN | 1 (0.2) | 0 |
| Deaths | 5 (0.9) | 17 (6.0) |
| Premature delivery | 0 | 12 (4.2) |
| Miscarriage | 0 | 1 (0.4) |
| Fetal deaths/stillbirths | 0 | 7 (2.5) |
HUS hemolytic uremic syndrome, TTP thrombotic thrombocytopenic purpura, AMAN acute motor axonal neuropathy
Two thirds of the infectious disease outbreaks linked to unpasteurized dairy were due to consumption of fluid milk (n=14/21; one outbreak was linked to both milk and cheese). A higher proportion of people required hospitalization if the source was cheese made from unpasteurized milk (n=82/195, 42%) than if the source was unpasteurized fluid milk (n=40/311, 13%) (p<0.001). We did not calculate the difference in proportions for deaths due to the small numbers.
Outbreaks linked to pasteurized dairy products
Eleven studies reported 12 outbreaks linked with consumption of pasteurized dairy products (Table 2). The outbreak sources were soft cheese made from pasteurized milk (n=7), pasteurized fluid milk (n=3) (the milk was improperly pasteurized in at least one outbreak), liquid ice cream mix (n=1), and gas station nacho cheese sauce (n=1). The most common pathogen was Listeria monocytogenes (n=10; 83%), with one outbreak due to Yersinia enterocolitica (8.3%) and one outbreak due to Clostridium botulinum (8.3%).
The total number of illnesses was 284 with 174 (61%) from confirmed cases and 110 (39%) from suspected cases, with four pediatric cases (confirmed and suspected). Ages ranged from less than one year to 92 years with 35% being male. There were 134 hospitalizations (47%; 134/284) and 17 deaths (6.0%; 17/284) (Table 3). Fifteen deaths were due to Listeriosis monocytogenes while one was due to Yersinia enterocolitica and one was due to Clostridium botulinum. No HUS cases were reported. Thirty-three Listeria infections of pregnant women were reported from five different Listeria outbreaks resulting in one miscarriage (Centers for Disease Control and Prevention 2013), 12 preterm deliveries (Centers for Disease Control and Prevention, 2008a; Gaulin et al. 2012), and seven fetal losses/stillbirths (Centers for Disease Control and Prevention, 2008; Gaulin et al. 2012; Heiman et al. 2015; Jackson et al. 2011).
Unpasteurized vs. pasteurized outbreaks
Listeria monocytogenes was more likely to be the causative agent in pasteurized outbreaks (Listeria: n=10/12, 83% versus non-Listeria: n=2/12, 17%; p<0.001) and the proportions of hospitalizations and deaths were higher in pasteurized than in unpasteurized outbreaks (pasteurized: n=134/284, 47% vs. unpasteurized: n=124/530, 23%, p<0.01; pasteurized: 17/284, 6% vs. unpasteurized: 5/530, 0.9%, p<0.01) respectively.
Quality assessment
Using the MMAT tool and its associated scoring metrics, the methodological quality of the studies was determined to be moderate overall. The average descriptor value scored between a 2 and a 3 out of a possible 4 where a ‘yes’ was equal to 1 and a ‘no’ or ‘cannot tell’ was equal to 0 (Appendix 3). The most common study design was case report/case series where the absence of an a priori research question and concise reporting did not allow for answers to all of the quality assessment questions to be determined. Therefore, we excluded questions 3.5 and 4.5.
Discussion
In this systematic approach to identify outbreaks linked to the consumption of unpasteurized versus pasteurized dairy products in Canada and the USA from 2007 onward, two thirds of cases were linked to unpasteurized dairy products. Hospitalizations and deaths were significantly higher for infections from pasteurized dairy products, but it is important to recognize that the absolute risk of infection is markedly higher with consumption of unpasteurized products.
The higher proportion of adverse outcomes with pasteurized products differs from the 1993–2006 US study findings (Langer et al. 2012). This appears to be attributable to the emergence of Listeria as the primary pathogen in reported outbreaks from pasteurized products. Outbreaks of Listeria in pasteurized products occur because of improper pasteurization or from contamination post-pasteurization. Any bacteria present on the hands or gloves of people or the equipment that come into contact with milk or milk products can cause contamination. This is only a problem if those bacteria are human pathogens and there is sufficient time for them to multiply between contamination and consumption. Unlike most human pathogens, Listeria can multiply at refrigerator temperatures (Chan and Wiedmann, 2009). Listeria is also unlike other dairy-derived pathogens in that it is highly virulent and associated with an increased risk of hospitalization and death upon infection in pregnant women and immunocompromised hosts, and with an increased risk of meningitis in those over 50 years of age (Schlech, 2019). All of the included studies that reported premature deliveries, miscarriages, and fetal deaths in pregnant mothers had identified Listeria monocytogenes as the pathogen. It should also be noted that widespread use of biologic response modifiers over the last decade has increased the number of immunocompromised hosts, likely increasing the risk of infection by pathogens including Listeria monocytogenes (Le Saux, and Canadian Pediatric Society, Infectious Diseases and Immunization Committee, 2012).
The distribution of pathogens in the current review also differs from previous similar reviews. Norovirus was detected in 13 of 103 outbreaks with an identified pathogen in the 1993–2006 US study while none of the outbreaks in the current study were due to viruses (Langer et al. 2012). This is surprising given that the availability and scope of molecular detection of viruses have expanded over time, although this may be because norovirus is now so well recognized that outbreaks are less likely to be reported. In outbreaks linked to consumption of pasteurized dairy products from 2007 through 2020, a startling 83% were due to Listeria infection with outbreaks stemming from soft cheese, fluid milk, and ice cream. In comparison, Listeria was detected in only 3% of the 30 outbreaks involving pasteurized dairy products between 1993 and 2006 (Langer et al. 2012). Listeria can be zoonotic or can come from soil or plant matter and it appears that a bovine source is less common than post-pasteurization contamination. A recent surveillance report of listeriosis outbreaks due to soft cheeses in the USA from 1998 to 2014 also found that the proportion of outbreaks resulting from cheese made from pasteurized milk was significantly higher in the 2007–2014 period compared to 1998–2006 (33% vs. 5%, p=0.009) (Jackson et al. 2018). Some postulated reasons were increased soft cheese consumption and a desire to procure foods from smaller producers who may be at increased risk for sanitary deficiencies.
In unpasteurized foodborne outbreaks, the presence of Campylobacter spp. has been widely reported in previous studies (Oliver et al. 2009). Campylobacteriosis was reported to be the most commonly reported pathogen linked to unpasteurized milk, accounting for 69% of cases in 2005 through 2012 in Ontario, Canada (Public Health Ontario, Raw Milk Working Group, 2013), and 81% of outbreaks from 2007 through 2012 in the USA (Mungai et al., 2015). The 1993–2006 US study reported 54% of outbreaks involving unpasteurized dairy products were attributed to Campylobacter spp. (Langer et al. 2012). Our findings were similar with campylobacteriosis associated most frequently with illness due to consumption of unpasteurized dairy products, but only accounting for 33% of cases (30% of outbreaks), followed by E. coli linked to 28% of cases (25% of outbreaks).
The number of pediatric cases was not reported separately from the adult data for most outbreaks but as expected, the majority of cases of HUS (83%, 5 out of 6) occurred in children. Given the risk of acute and chronic renal failure with HUS, parents considering providing their children with unpasteurized dairy products should be educated about the risk of HUS.
Limitations
A major limitation of our analysis is that illness is often not recognized to be food-borne; therefore, the food source is sometimes not identified. However, it appears that the pathogen is almost always identified if the source is a dairy product (Davis et al., 2016). By using a strict definition of epidemiologically linked, we will have excluded outbreaks due to pathogens that are yet to be recognized or difficult to detect; such outbreaks are likely to still be reported in the literature if they result in severe morbidity or large numbers of cases. In addition, as a minority of cases or outbreaks are reported and even fewer are published in the literature, we could not access the full text of 26 studies. Our findings are therefore undoubtedly a gross underestimate of the true burden of food-borne illness due to consumption of dairy products and may be biased toward emerging pathogens such as Listeria. Also, the majority of the studies did not report data for children and adults separately, which limits applicability of the findings. Finally, as the majority of included studies were case series/reports, information on the denominator was often not available, making it difficult to assess the overall impact of the outbreak. Very few studies calculated relative risk of illness based on the amount of dairy product consumed or by consumer demographics and therefore our review does not include a comparative risk assessment.
Conclusion
While the number of published outbreaks epidemiologically linked to dairy consumption during our study period was relatively low, the burden of illness associated with these outbreaks was high with many cases requiring hospitalization and a small number resulting in long-term sequelae or death. Listeria outbreaks even from pasteurized products may be an emerging problem. Health care professionals, particularly those who work with neonates, pregnant women, people with compromised immune systems, and people over age 50 years, must be aware of the risks inherent in consumption of unpasteurized dairy products and soft cheeses made from pasteurized milk.
Supplementary Information
(DOCX 28 kb)
(DOCX 19 kb)
(DOCX 24 kb)
Acknowledgements
The authors acknowledge the contribution of Tara Landry for her peer review of the search strategy, and those of Liza Bialy and Shelly Jun for quality assessment of the included studies. We also acknowledge Judy D. Greig and Mariola Mascarenhas with the Public Health Agency of Canada for their assistance in searching the Publicly Available International Foodborne Outbreak Database (PAIFOD).
Availability of data and material
Data are available from the corresponding author by reasonable request.
Code availability
Not applicable.
Author contributions
MS, RF, and JLR conceived the project and undertook the data collection and analysis; MS and NAB wrote the first draft; all the authors contributed toward the intellectual content of the manuscript.
Funding
This work was supported by the Alberta Strategy for Patient-Oriented Research (SPOR) SUPPORT Unit Knowledge Translation Platform, which is funded by Alberta Innovates (G201900663) and the Canadian Institutes of Health Research (201305).
Declarations
Conflict of interest
The authors declare no competing interests.
Ethics approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Consent to participate
Not applicable
Consent for publication
Not applicable
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- Beecher, C. (2012). 19 ill with E. coli in Oregon raw milk outbreak. Food Safety News. Retrieved from https://www.foodsafetynews.com/2012/04/post-5/.
- California Department of Public Health. (2008). Campylobacteriosis among persons consuming unpasteurized milk from a cow-leasing program. Retrieved from www.marlerblog.com/uploads/file/CDPH%20Report%20(Tardiff).pdf.
- Health Canada. (2013). Raw or unpasteurized milk. Retrieved from http://www.canada.ca/en/health-canada/services/milk-infant-formula/raw-or-unpasteurized-milk.html.
- Centers for Disease Control and Prevention. (2007). Foodborne Active Surveillance Network (FoodNet) population survey atlas of exposures, 2006-2007. U.S. Department of Health and Human Services, Centers for Disease Control and Prevention.
- Centers for Disease Control and Prevention Outbreak of Listeria monocytogenes infections associated with pasteurized milk from a local dairy--Massachusetts, 2007. MMWR. 2008;57(40):1097–1100. [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. (2013). Multistate outbreak of listeriosis linked to Crave Brothers Farmstead Cheeses (final update). Retrieved from https://www.cdc.gov/listeria/outbreaks/cheese-07-13/index.html.
- Centers for Disease Control and Prevention. (2015). Guide to confirming an etiology in foodborne disease outbreak. Retrieved from https://www.cdc.gov/foodsafety/outbreaks/investigating-outbreaks/confirming_diagnosis.html.
- Centers for Disease Control and Prevention. (2016). Multistate outbreak of listeriosis linked to raw milk produced by Miller’s Organic Farm in Pennsylvania (Final Update). Retrieved from https://www.cdc.gov/listeria/outbreaks/raw-milk-03-16/index.html.
- Centers for Disease Control and Prevention. (2017a). Raw milk questions and answers. Retrieved from http://www.cdc.gov/foodsafety/rawmilk/raw-milk-questions-and-answers.html#history.
- Centers for Disease Control and Prevention. (2017b). Multistate outbreak of listeriosis linked to soft raw milk cheese made by Vulto Creamery (Final Update). Retrieved from https://www.cdc.gov/listeria/outbreaks/soft-cheese-03-17/index.html.
- Chan YC, Wiedmann M. Physiology and genetics of Listeria monocytogenes survival and growth at cold temperatures. Crit Rev Food Sci Nutr. 2009;49(3):237–253. doi: 10.1080/10408390701856272. [DOI] [PubMed] [Google Scholar]
- Christidis T, Pintar KD, Butler AJ, Nesbitt A, Thomas MK, Marshall B, et al. Campylobacter spp. prevalence and levels in raw milk: A systematic review and meta-analysis. Journal of Food Protection. 2016;79(10):1775–1783. doi: 10.4315/0362-028X.JFP-15-480. [DOI] [PubMed] [Google Scholar]
- Committee on Infectious Diseases, Committee on Nutrition for the American Academy of Pediatrics Consumption of raw or unpasteurized milk and milk products by pregnant women and children. Pediatrics. 2014;133(1):175–179. doi: 10.1542/peds.2013-3502. [DOI] [PubMed] [Google Scholar]
- Currie A, Galanis E, Chacon PA, Murray R, Wilcott L, Kirkby P, et al. Outbreak of Escherichia coli O157:H7 infections linked to aged raw milk gouda cheese, Canada, 2013. Journal of Food Protection. 2018;81(2):325–331. doi: 10.4315/0362-028X.JFP-17-283. [DOI] [PubMed] [Google Scholar]
- Davis KR, Dunn AC, Burnett C, McCullough L, Dimond M, Wagner J, et al. Campylobacter jejuni infections associated with raw milk consumption--Utah, 2014. MMWR. 2016;65(12):301–305. doi: 10.15585/mmwr.mm6512a1. [DOI] [PubMed] [Google Scholar]
- Dewey-Mattia D, Manikonda K, Hall AJ, Wise ME, Crowe SJ. Surveillance for foodborne disease outbreaks - United States, 2009-2015. MMWR. 2018;67(10):1–11. doi: 10.15585/mmwr.ss6710a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gaulin C, Ramsay D, Bekal S. Widespread listeriosis outbreak attributable to pasteurized cheese, which led to extensive cross-contamination affecting cheese retailers, Quebec, Canada, 2008. Journal of Food Protection. 2012;75(1):71–78. doi: 10.4315/0362-028X.JFP-11-236. [DOI] [PubMed] [Google Scholar]
- Gerner-Smidt P, Whichard JM. Foodborne disease trends and reports. Foodborne Pathogens & Disease. 2009;6(1):1–5. doi: 10.1089/fpd.2008.9990. [DOI] [PubMed] [Google Scholar]
- Guh A, Phan Q, Nelson R, Purviance K, Milardo E, Kinney S, et al. Outbreak of Escherichia coli O157 associated with raw milk, Connecticut, 2008. Clinical Infectious Diseases. 2010;51(12):1411–1417. doi: 10.1086/657304. [DOI] [PubMed] [Google Scholar]
- Headrick ML, Korangy S, Bean NH, Angulo FJ, Altekruse SF, Potter ME, et al. The epidemiology of raw milk-associated foodborne disease outbreaks reported in the United States, 1973 through 1992. American Journal of Public Health. 1998;88(8):1219–1221. doi: 10.2105/AJPH.88.8.1219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heiman KE, Garalde VB, Gronostaj M, Jackson KA, Beam S, Joseph L, et al. Multistate outbreak of listeriosis caused by imported cheese and evidence of cross-contamination of other cheeses, USA, 2012. Epidemiology & Infection. 2015;144(13):2698–2708. doi: 10.1017/S095026881500117X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jackson KA, Biggerstaff M, Tobin-D'Angelo M, Sweat D, Klos R, Nosari J, et al. Multistate outbreak of Listeria monocytogenes associated with Mexican-style cheese made from pasteurized milk among pregnant, Hispanic women. Journal of Food Protection. 2011;74(6):949–953. doi: 10.4315/0362-028X.JFP-10-536. [DOI] [PubMed] [Google Scholar]
- Jackson KA, Gould LH, Hunter JC, Kucerova Z, Brendan J. Listeriosis outbreaks associated with soft cheeses, United States, 1998–2014. Emerging Infectious Disease Journal. 2018;24(6):1116–1118. doi: 10.3201/eid2406.171051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jay-Russell MT. Raw (unpasteurized) milk: Are health-conscious consumers making an unhealthy choice? Clinical Infectious Diseases. 2010;51(12):1418–1419. doi: 10.1086/657305. [DOI] [PubMed] [Google Scholar]
- Langer AJ, Ayers T, Grass J, Lynch M, Angulo FJ, Mahon BE. Nonpasteurized dairy products, disease outbreaks, and state laws-United States, 1993-2006. Emerging Infectious Diseases. 2012;18(3):385–391. doi: 10.3201/eid1803.111370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Le Saux N, Canadian Pediatric Society, Infectious Diseases and Immunization Committee Biologic response modifiers to decrease inflammation: Focus on infection risks. Paediatric Child Health. 2012;17(3):147–150. doi: 10.1093/pch/17.3.147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leamy RJ, Heiss SN, Roche E. The impact of consumer motivations and sources of information on unpasteurized milk consumption in Vermont, 2013. Food Protection Trends. 2014;34(4):216–225. [Google Scholar]
- Lejeune JT, Rajala-Schultz PJ. Food safety: Unpasteurized milk: A continued public health threat. Clinical Infectious Diseases. 2009;48(1):93–100. doi: 10.1086/595007. [DOI] [PubMed] [Google Scholar]
- McCollum JT, Williams NJ, Beam SW, Cosgrove S, Ettestad PJ, Ghosh TS, et al. Multistate outbreak of Escherichia coli O157:H7 infections associated with in-store sampling of an aged raw-milk Gouda cheese, 2010. Journal of Food Protection. 2012;75(10):1759–1765. doi: 10.4315/0362-028X.JFP-12-136. [DOI] [PubMed] [Google Scholar]
- McGowan J, Sampson M, Salzwedel DM, Cogo E, Foerster V, Lefebvre C. PRESS Peer Review of Electronic Search Strategies: 2015 guideline statement. Journal of Clinical Epidemiology. 2016;75:40–46. doi: 10.1016/j.jclinepi.2016.01.021. [DOI] [PubMed] [Google Scholar]
- Mungai EA, Behravesh CB, Gould LH. Increased outbreaks associated with nonpasteurized milk, United States, 2007-2012. Emerging Infectious Diseases. 2015;21(1):119–122. doi: 10.3201/eid2101.140447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oliver SP, Boor KJ, Murphy SC, Murinda SE. Food safety hazards associated with consumption of raw milk. Foodborne Pathogens & Disease. 2009;6(7):793–806. doi: 10.1089/fpd.2009.0302. [DOI] [PubMed] [Google Scholar]
- Pluye, P., Robers, E., Cargo, M., Bartlett, G., O'Cathain, A., Griffiths, F., et al. (2011). Proposal: A mixed methods appraisal tool for systematic mixed studies reviews. Retrieved from http://mixedmethodsappraisaltoolpublic.pbworks.com.
- Public Health Agency of Canada. (2012). National single day food consumption report: Analysis of the 24-hour dietary recall data from the Canadian Community Health Survey (CCHS), cycle 2.2, nutrition (2004), and assessment for food consumption frequency among Canadians. Public Health Agency of Canada.
- Public Health Ontario, Raw Milk Working Group. (2013). PHO technical report: Update on raw milk consumption and public health: A scientific review for Ontario public health professionals. Queen's Printer for Ontario.
- Schlech, W. F. (2019). Epidemiology and clinical manifestations of Listeria monocytogenes infection. Microbiol Spectr, 7(3). 10.1128/microbiolspec.GPP3-0014-2018 [DOI] [PMC free article] [PubMed]
- Shiferaw B, Verrill L, Booth H, Zansky SM, Norton DM, Crim S, et al. Sex-based differences in food consumption: Foodborne Diseases Active Surveillance Network (FoodNet) Population Survey, 2006-2007. Clinical Infectious Diseases. 2012;54(Suppl 5):S453–S457. doi: 10.1093/cid/cis247. [DOI] [PubMed] [Google Scholar]
- Steele JH. History, trends, and extent of pasteurization. Journal of the American Veterinary Medical Association. 2000;217(2):175–178. doi: 10.2460/javma.2000.217.175. [DOI] [PubMed] [Google Scholar]
- U.S. Food and Drug Administration. (1987). FDA plans to ban raw milk. U.S. Government Printing Office.
- U.S. Food and Drug Administration. (2020). Code of Federal Regulations Title 21, Chapter 1, Subchapter B - Food for human consumption, part 133 cheeses and related cheese products. Retrieved from http://www.accessdata.fda.gov/scripts/cdrh/cfdocs/cfcfr/CFRSearch.cfm?CFRPart=133.
- Whitehead, J., & Lake, B. (2018). Recent trends in unpasteurized fluid milk outbreaks, legalization, and consumption in the United States. PLoS Curr. 10.1371/currents.outbreaks.bae5a0fd685616839c9cf857792730d1 [DOI] [PMC free article] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX 28 kb)
(DOCX 19 kb)
(DOCX 24 kb)
Data Availability Statement
Data are available from the corresponding author by reasonable request.


