Abstract
COVID-19 is a global pandemic triggered by the severe acute respiratory syndrome-coronavirus 2 (SARS-CoV-2). The SARS-CoV-2 entry point involves the interaction with angiotensin-converting enzyme 2 (ACE2) receptor, CD147, and erythrocyte Band3 protein. Hemolytic anemia has been linked to COVID-19 through induction of autoimmune hemolytic anemia (AIHA) caused by the formation of autoantibodies (auto-Abs) or directly through CD147 or erythrocyte Band3 protein-mediated erythrocyte injury. Here, we aim to provide a comprehensive view of the potential mechanisms contributing to hemolytic anemia during the SARS-CoV-2 infection. Taken together, data discussed here highlight that SARS-CoV-2 infection may lead to hemolytic anemia directly through cytopathic injury or indirectly through induction of auto-Abs. Thus, as SARS-CoV-2-induced hemolytic anemia is increasingly associated with COVID-19, early detection and management of this condition may prevent the poor prognostic outcomes in COVID-19 patients. Moreover, since hemolytic exacerbations may occur upon medicines for COVID-19 treatment and anti-SARS-CoV-2 vaccination, continued monitoring for complications is also required. Given that, intelligent nanosystems offer tools for broad-spectrum testing and early diagnosis of the infection, even at point-of-care sites.
Supplementary Information
The online version contains supplementary material available at 10.1007/s00277-022-04907-7.
Keywords: COVID-19, SARS-CoV-2, Autoimmune hemolytic anemia
Introduction
The normal lifespan of red blood cells (RBCs) is 120 days. In hemolytic anemia, the period is shortened to a few days due to their destruction. The hemolysis may occur when RBCs are targeted by anti-RBC membrane autoantibodies (auto-Abs) leading to induction of autoimmune hemolytic anemia (AIHA) [1]. Depending on the temperature at which auto-Abs bind optimally to RBCs, AIHA is classified as warm type mediated by IgG and C3d or cold type mediated by IgM, with their maximal reactivity at 37 °C and 4 °C, relatively. However, as even warm IgM RBC auto-Abs do exist, and secondary cold agglutinin syndrome (CAS) in some cases can be mediated by cold-reactive IgG [1, 2]. The warm and cold types of AIHA lead to hemolysis through activation of phagocytic cells and the classical complement pathway. However, extra- and intravascular hemolysis may concurrently contribute to warm or cold AIHA in some cases. The complement-mediated hemolysis in cold agglutinin diseases (CAD) or CAS is mainly extravascular (phagocytosis of C3b-opsonized RBCs), although intravascular hemolysis also occurs [1, 2].
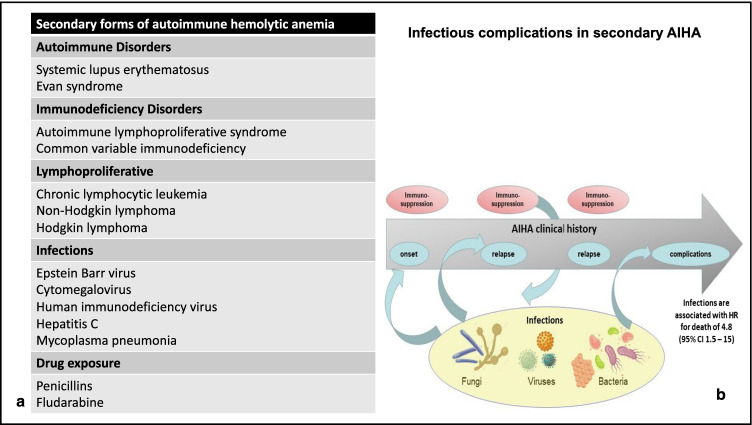
Moreover, a lack of standard diagnostic criteria makes the classification of AIHA and its subclasses is difficult [1, 3]. Depending on the presence or absence of underlying disease, AIHA is classified as primary or secondary. Primary or idiopathic type is in around 50% of cases, while the secondary type is caused by infections (mycoplasma and viral infections), lymphoproliferative disorders (lymphoma and chronic lymphocytic leukemia), and autoimmune diseases (systemic lupus erythematosus). Moreover, AIHA can also be triggered by drugs (methyldopa, antibiotics) and toxins (Fig. 1a) [2, 4, 5]. A significant risk factor for morbidity and mortality in AIHA patients is infection. Due to concurrent diseases harboring an inherent infectious risk, including immunodeficiency, autoimmune, and lymphoproliferative disorders, as well as immunosuppressive treatments, these patients are vulnerable to infectious agents (viruses, bacteria, fungi) which trigger onset or relapse of AIHA (Fig. 1b).
Fig. 1.
Secondary forms of AIHA [5] (a). Infectious complications in secondary AIHA [6] (b)
This risk is significant during the Coronavirus 2019 (COVID-19) pandemic [6]. COVID-19 is an infectious disease caused by severe acute respiratory syndrome-coronavirus 2 (SARS-CoV-2) and is considered a global issue pandemic by the World Health Organization. SARS-CoV-2 is a positive-sense single-strand RNA that shares a genetic similarity with other beta coronaviruses, like the Middle East respiratory syndrome-related coronavirus 1 (MERS-CoV-1) and SARS-CoV-1 [7]. The primary mechanism of SARS-CoV-2 entry into host cells is binding the viral spike protein to its receptor angiotensin-converting enzyme 2 (ACE2), which is highly expressed in the lung epithelial cells, proximal renal tubules, heart, and brain. The SARS-CoV-2 infection triggers an acute host immune response, inflammatory reactions, and cytokine storm leading to acute lung injury (ALI) and acute respiratory distress syndrome (ARDS) [8]. The virus can cause extra-pulmonary manifestations, like acute cardiac injury, arrhythmias, acute kidney injury, acute brain injury, endocrine failure, and multiple organ failure with fatal consequences [9]. Although AIHA is a relatively rare condition with an estimated incidence of 13/100,000 persons per year [10], there is a growing number of reported hemolytic anemia cases, mainly attributed to the development of auto-Abs, in the setting of COVID-19 [11]. Given the known risk of thrombosis in patients with cold agglutinin hemolytic anemia, Maslov et al. (2020) speculated that this might contribute to thrombosis and the unfavorable outcomes in COVID-19 patients [12]. The hemolysis of RBCs may also be caused by impairment of their morphology and functionality due to the virus infection [13], which is critical in cases of hemoglobinopathies or inherited anemias [14]. Severance et al. revealed that induction of hemolytic anemia in children with hereditary spherocytosis is due to provoking oxidative stress by SARS-CoV-2 infection [15]. On the other hand, sickle cell disease has been suggested to protect against fatal outcomes in COVID-19 because of reduced T cell-mediated immunity and related weakened immune response without cytokine storm [16]. Finally, anemia in AIHA patients represents a significant risk factor for a worse prognosis in COVID-19 patients [17]. Accordingly, the National Haemoglobinopathy Panel (NHP) has issued guidance on caring for patients with anemias regarding programmed blood transfusion and outpatients visits to reduce risk exposure to SARS-CoV-2 and related COVID-19 severity in the vulnerable group of patients [14].
Given the multifaceted nature of hemolytic exacerbations associated with COVID-19 infection, the review aims to highlight challenges tackling the complexity of these conditions, diagnosis, and management.
The interplay between SARS-CoV-2 infection and AIHA
AIHA is a common hematologic autoimmune sequel in the COVID-19 patients, according to an analysis by Taherifard et al. (2021) conducted on a total reported 94 cases [18]. A cross-sectional study by Algassim et al. (2021) have revealed that COVID-19 patients with AIHA are linked with poor prognosis and prolonged hospital stay, mainly when the hemoglobin (Hb) level is below 12 g/L. The authors reported that 14.7% of patients admitted to the intensive care unit (ICU) and 9% of non-ICU patients had AIHA, with a mortality rate of 32% among the direct antiglobulin test-positive patients [17]. Lazarian et al. (2020) have reported seven cases of AIHA comprising both warm and cold types during the early COVID-19 course. Four patients had lymphoid disorders, and this per se might explain the triggering effect of SARS-CoV-2 infection in auto-immunity induction [19]. Significantly, SARS-CoV-2 infection can cause hematologic autoimmune disorders in predisposed subjects both in the elderly and children, and several cases of AIHA have been described in a pediatric setting of COVID-19 [20, 21].
AIHA and related anemia lead to reduce oxygen saturation, critical organs ischemia, and hemodynamic disorders [17]. When it coincides with the COVID-19 associated cytokine storm, SARS-CoV-2-mediated immune hemolysis became high. AbouYabis and Bell (2021) have summarized a growing number of reported cold and warm AIHA cases in the setting of COVID-19 infection presented during the SARS-CoV-2-induced cytokine storm. Although the exact mechanism of AIHA contributing to COVID-19 remains unknown, the alteration in antigen presentation creating cryptic antigens caused by SARS-CoV-2 cytokine-rich inflammatory response is suggested [22]. Moreover, as the intense acute-phase response in COVID-19 causes, the dysregulation of the complement system [23], immune complexes, and complement products found on the RBC cell surface have been suggested to affect their rheology promoting intravascular thrombosis [24]. This is consistent with observed disseminated intravascular coagulopathy with subsequent multi-organ failure from warm AIHA in a COVID-19 patient [25]. The hypercoagulability and exacerbated inflammatory response may affect RBCs, making membranes fragile with lower elasticity, leading to embolisms and clots in COVID-19 patients [26]. Finally, iron and serum ferritin resulting from hemolysis may drive oxidative stress. Hyperferritinemia and impaired iron homeostasis have been demonstrated to contribute to endothelial damage and cause ultrastructural changes in RBCs of COVID-19 patients. Moreover, AIHA may lead to pulmonary thrombosis [27]. Interestingly, thrombosis associated with cold-agglutinin AIHA could be the presenting symptoms in COVID-19 patients [28]. As well, warm type AIHA may cause a pulmonary embolism. Abnormal exposure to phosphatidylserine (PS), RBCs derived microparticles (MP), and nitric oxide scavenging could be the potential mechanism of thrombosis in warm type AIHA. The destruction of RBCs leads to increased exposure of PS on the RBCs outer surface. PS acts as a docking site for enzymatic complexes involved in coagulation pathways; it makes RBCs more adhesive and leads to antiphospholipid antibody formation. RBC-derived MPs are released during hemolysis, acting as tissue factors triggering thrombosis. MPs correlate with D-Dimer and thrombin-antithrombin complex formation as well. Nitric oxide is sequestrated by the released hemoglobin from hemolyzed RBCs leading to uninhibited platelet aggregation and vasoconstriction leading to thrombosis [29]. These findings suggest the causality between erythrocyte pathology and thrombosis in these patients [30].
SARS-CoV-2 and direct erythrocytes injury
Methemoglobinemia is a hemoglobin disorder caused by the oxidation of iron Hb from ferrous to ferric status with oxygen-carrying capacity failure, leading to hypoxia, cyanosis, and respiratory failure [28]. Methemoglobinemia can be induced by drugs such as dapsone, sulfonamide, local anesthetics, and ascorbic acid [31] or viral infections, such as influenza, due to induction of oxidative stress and oxidation of Hb iron as a result [32]. Lopes et al. (2021) have reported a case study of SARS-CoV-2 induced-methemoglobinemia and non-hemolytic anemia due to oxidative stress aggravated by glucose-6-phosphate dehydrogenase (G6PD) deficiency [33]. In a docking study, Liu and Li (2021) have identified two SARS-CoV-2 proteins, S and ORF3a, able to bind with the 1-beta chains of hemoglobin, therefore causing Hb denaturation and immunological agglutination [34]. Interestingly, in a cohort study, DeMartino et al. (2020) have demonstrated no direct RBCs and Hb damage during SARS-CoV-2 infection [35]. Regardless of the established findings, various possible pathophysiologic mechanisms have been highlighted. Cavezzi et al. (2020), in their narrative review, pointed out that SARS-CoV-2 infection is associated with direct cytopathic injury of circulating RBCs and their precursors in bone marrow or indirect RBCs by intravascular coagulopathy and cytokine storm. These pathological changes are supported by the presence of anisocytosis generated by conformational changes in both RBCs membrane proteins and lipids [36]. These conformational changes in RBC surface ankyrin-1 protein appear to be due to molecular similarity with the SARS-CoV-2 spike protein [37].
Besides ACE2, the virus tropism for erythrocytes is associated with the cluster of differentiation 147 (CD147), also known as basigin or extracellular matrix metalloproteinase inducer (EMMPRIN), a transmembrane glycoprotein highly expressed in RBCs [38]. CD147 mediates SARS-CoV-2 entering RBCs by endocytosis [39], leading to dysregulation of RBCs CD147-cyclophilin A signaling pathway with subsequent hemolysis [40]. So, antibodies against CD147 like mepolizumab may attenuate SARS-CoV-2 invasion and hemolysis [41]. Similarly, azithromycin and other macrolides can also inhibit the interaction between SARS-CoV-2 and CD147 on RBC membranes and other host cells. Therefore, these antibiotics can also be considered a potential therapeutic drug in COVID-19 management and associated hemolytic anemia [42]. However, Shilts et al. (2021) have demonstrated no interactions between SARS-CoV-2 and CD147. In their experiment, no changes in susceptibility to this virus were observed in human lung epithelial cells after removing by CRISPR/Cas9 basigin from their surface [43]. As a matter of fact, the CD147 expression is stimulated by hyperinflammation status [44]. Raony and Figueiredo (2020) have confirmed that in a COVID-19-induced cytokine storm, there is an overexpression of CD147 facilitating the SARS-CoV-2 spike protein binding to retinal cells [45]. Therefore, the higher expression of RBCs CD147 may mediate the interaction between RBCs and SARS-CoV-2 even in the absence of ACE2. Indeed, it has been reported that ACE2-deficient T cells can be infected with SARS-CoV-2 via CD147 [46].
Moreover, inducing intra-erythrocytic oxidative stress by viral load has been demonstrated to be detrimental to proteins in erythrocytes, including those involved in membrane function, antioxidant defense, and transport and delivery of oxygen [47]. The RBCs’ susceptibility is increased to being damaged by the associated micro-angiopathic inflammations [48]. In a case study, Lancman et al. (2021) have reported intravascular hemolysis with Coombs-negative hemolytic anemia in COVID-19 patients, suggesting direct RBCs injury due to SARS-CoV-2/CD147 interaction [49]. The latter, along with associated inflammatory reactions, is suggested to induce erythrocyte structural membrane changes and complement activations that together provoke intravascular and extravascular hemolysis [47, 50].
As regards the virus tropism to erythrocyte, Cosic et al. (2020), using the resonant recognition model, have proposed that SARS-CoV-2 might also infect RBCs via binding to the RBC Band3 protein [51]. Band3, the anion exchanger 1 protein, is most abundant in mature RBCs and controls, among others, bicarbonate/chloride homeostasis. This protein is regarded as a docking site for structural proteins necessary for membrane integrity [52] and is mandatory for oxygen release and metabolic processes [51]. Thus, SARS-CoV-2 spike protein binding to RBC Band3 protein disturbs oxygen transport function causing severe hypoxia and metabolic alterations that increase the risk of RBC injury and hemolytic effect [13, 51]. Band3 protein inhibits glycolytic enzyme function during normal oxygen saturation. However, during hypoxia, oxy-Hb competes with Band3 protein to favor the glycolytic pathway that increases RBCs ATP to promote oxygen release and prevent tissue hypoxia [53]. Moreover, Thomas et al. (2020), in an observational study involving 29 COVID-19 patients and 23 healthy controls, have revealed that RBCs from COVID-19 patients had a high glycolytic pathway with oxidation and fragmentation of membrane protein, including Band3 protein, spectrin beta, and ankyrin [47]. This alteration in membrane protein is associated with RBC lipid metabolism changes, particularly sphingolipids, acyl-carnitine, and fatty acids. High RBC glycolytic metabolite is regarded as a compensatory pathway against SARS-CoV-2 induced hypoxia to improve Hb oxygen load [54]. Because Band3 protein stabilizes deoxy-Hb and control oxygen loading, so it is shifting RBC metabolism toward hexose-monophosphate shunt and prevents the susceptibility of RBC to the effects of oxidative stress during COVID-19-induced hypoxia [55]. These findings suggest a potential impact of SARS-CoV-2 infection on the RBCs’ structural proteins and lipid metabolism. Thus, COVID-19-induced hypoxia or SARS-CoV-2 may inhibit Band3 protein, disrupting RBC metabolism, structural integrity, oxygen transport, and circulation in the bloodstream [56].
Moreover, SARS-CoV-2 reduces RBC antioxidant capacity, including G6PD activity, and causes deformability of RBCs associated with a high risk of hemolysis [47]. The reduced G6PD activity contributes to the oxidation of structural proteins resulting in RBCs deformability and their susceptibility to coagulation and thromboembolic disorders in patients with severe COVID-19 [57].
Likewise, sphingosine-1-phosphate (S1P), also known as lysosphingolipid, is a bioactive lipid mediator mainly released from RBCs and to a lesser extent from platelets and endothelial cells. S1P has immune-modulating effects in mitigation of SARS-CoV-2 and viral infection-induced inflammatory disorders. The reduction of S1P serum level correlates with COVID-19 severity and reduces RBCs production or SARS-CoV-2-induced injury [58, 59].
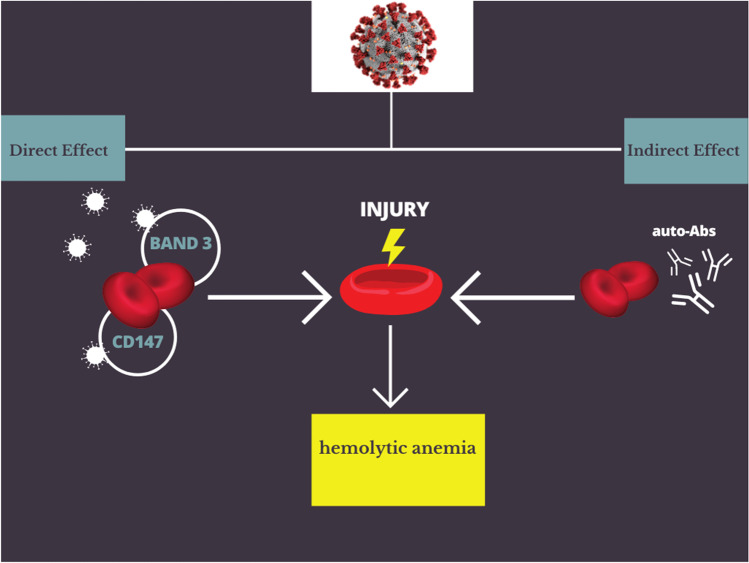
Overall, the net effect of SARS-CoV-2 infection-induced hemolytic anemia is either direct RBC injury or indirectly through induction of auto-Abs against the RBC membrane (Fig. 2).
Fig. 2.
Mechanism of SARS-CoV-2-induced hemolytic anemia
COVID-19 management in the scenario of AIHA
The rapid spread and high fatality of SARS-CoV-2 requires a rapid discovery of effective antiviral agents to control this pandemic. The lack of treatment options caused clinical trials to test existing pharmacological drugs such as remdesivir, chloroquine, hydroxychloroquine, ivermectin, lopinavir-ritonavir, azithromycin, doxycycline, rivaroxaban, and protease inhibitors to repurpose them for the treatment of COVID-19. Since some of these agents may be implicated in the pathogenesis of AIHA, the risk should be considered in evaluating the efficacy and safety of prospective repurposing drugs in the treatment of COVID-19 infections [60, 61].
It has been shown that both chloroquine and hydroxychloroquine inhibit SARS-CoV-2 in Ver E6 at a micromolar concentration range through blocking of cathepsin L and PH-dependent interference with viral endocytosis. Both chloroquine and hydroxychloroquine were used to manage COVID-19 based on the preliminary data suggesting their abilities to limit viral replications [62, 63]. Doyno et al. (2020), however, have revealed that hydroxychloroquine might increase the risk of hemolysis in COVID-19 patients with G6PD deficiency. Thus, a measurement of this enzyme activity should be done before initiation of therapy [62]. Surprisingly, a large-scale study did not support these findings [63].
Despite the fact that controversy about the potential benefit of ribavirin in the management of COVID-19 [64], Eslami et al. (2020) have revealed the effectiveness of ribavirin in the inhibition of the replication of SARS-CoV-2 [65]. However, its prolonged intake can increase the risk of hemolytic anemia due to accumulation within the RBCs and induction of oxidative membrane damage [66]. Moreover, Nabil et al.’s (2020) study has disclosed that repurposing antiviral drugs such as arbidol, remdesivir, ritonavir, and lopinavir may cause hemolytic anemia by unknown mechanisms in patients with COVID-19 [67]. Finally, the World Health Organization recommended against the use of chloroquine, hydroxychloroquine, remdesivir, and lopinavir/ritonavir in the treatment of SARS-CoV-2 infection [60]. Therefore, an extensive review of used drugs in the management of COVID-19 for the potential hemolytic effect is necessary and warranted since anemia is correlated with COVID-19 severity [68].
Recently, discussion of the hematologic complications after SARS-CoV-2 vaccination has been starting. Besides developing vaccine-associated immune thrombosis with thrombocytopenia, as Fattizzo et al. (2021) reviewed, hemolytic flares occurred in patients with cold and warm AIHA who received either Moderna or Pfizer-BioNTech vaccines [69]. Fatima et al. (2022) also have reported a case of a patient who developed IgG-mediated AIHA after vaccination with the Moderna COVID-19 vaccine [70]. Overall, hemolytic exacerbations occurring during COVID-19 are more severe than those appearing after the SARS-CoV-2 vaccine [69, 70].
AIHA diagnosis in the setting of COVID-19 infection
The AIHA diagnosis is based on the detection of hemolytic anemia by Hb level and biochemical markers of hemolysis (often supported by blood smear and absolute reticulocyte count), followed by a demonstration of autoimmune pathogenesis by DAT. The further classification depends primarily on the pattern by monospecific DAT (Ig class and/or complement protein on the RBC surface) and only occasionally on autoantibodies in RBC eluate and serum, while anemia and hemolysis are identified based on complete blood count (CBC), reticulocyte count, peripheral blood smear, serum biomarkers including bilirubin, lactate dehydrogenase (LDH), haptoglobin, and urine hemoglobin level [10].
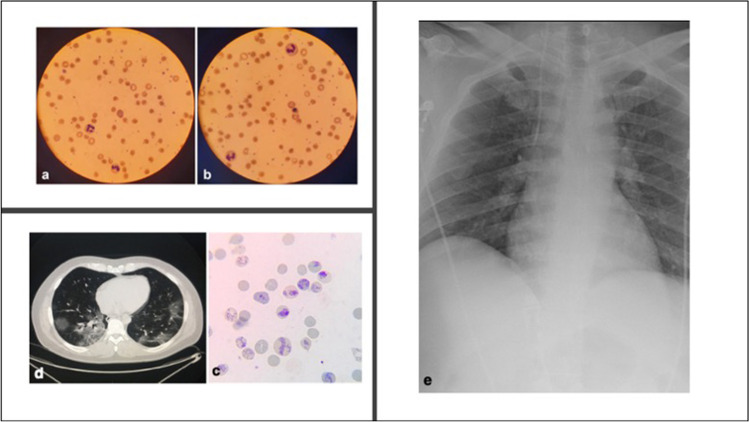
According to Lazarian et al. (2020), the time between the COVID-19 symptoms and AIHA onset with marked signs of hemolysis ranged from 4 to 13 days [19]. Positive direct DAT or Coombs tests for IgG and C3 were reported in several COVID-19 cases [71–74] and warm antibodies in four of the seven cases reported by Lazarian et al. [19]. Hemolysis markers, including anemia, defects in the red cell membrane–spherocytosis (Fig. 3a and b) [74], reticulocytosis (Fig. 3c) [75], unconjugated bilirubinemia, increased serum LDH activity, ferritin, and low haptoglobin were also observed [10, 73, 74, 76]. Moreover, increased D-dimer and C-reactive levels were reported due to hypercoagulability and hyperinflammatory response in most SARS-CoV-2-associated AIHA cases [19, 72–74, 76]. Extended examinations, including chest X-rays, showed bilateral opacities (Fig. 3d) [73, 76], while chest computed tomography showed typical COVID-19 infection changes in the lung (Fig. 3c) [74, 75].
Fig. 3.
Diagnosis of hemolysis: polychromasia (a), nucleated red blood cells (b) [74], and reticulocytosis (c) [75]. COVID-19 infection-induced changes in the lung: Computed tomography scan shows bilateral lung infiltration (d) [81]; chest X-ray shows diffuse bilateral opacities (e) [81]
Challenges and future perspectives
Challenges remain, including hemolysis diagnosis in COVID-19 patients, which may be masked by the infection-related elevated acute phase haptoglobin [74]. Given that the complexity of the pathophysiologic interplay between SARS-CoV-2 infection and hemolytic events still requires further studies, more research on developing comprehensive diagnostic approaches tailored to the individual pathophysiological features of each disease is necessary. The improved understanding of the interconnected pathogeneses will enable the development of specific biomarkers alongside exact therapy. Since hemolytic anemias are increasingly associated with COVID-19, early detection and management of these conditions may prevent poor prognostic outcomes in these patients. In this context, the emerging sensitive, rapid, selective, and at the point-of-care (POC) diagnostic systems for the virus detection are a response [77, 78]. Moreover, biomonitoring related to coagulopathy and other pathologies may be the subject of POC analyses assisting clinicians in planning clinical interventions relating to individualized management [30]. This is even more important, considering that the NHP recommended minimalization outpatient visits to limit exposure of anemia patients to SARS-CoV-2 infections. In fact, these patients are at risk of non-efficient diagnostics and withdrawal of effective trial therapy [14]. This problem is the more serious as the COVID-19 pandemic is constantly surprising healthcare systems, and continuous variations in the structures of SARS-CoV-2 contribute to newly emerged variants making the viral infection more transmissible, contagious, and severe [79]. In this context, a broader application of current knowledge on technologies that use high-performance antibacterial and antiviral nanosystems can also mitigate the SARS-CoV-2 transmission [80].
Conclusions
Taken together, the data discussed here highlight that SARS-CoV-2 infection may lead to hemolytic anemia directly through cytopathic injury or indirectly through induction of auto-Abs. Therefore, extensive research on the potential mechanisms of SARS-CoV-2-induced hemolytic anemia and related specific diagnostics covering the complex etiology is required. Diagnostics tailored to the individual pathophysiological features of each disease demand comprehensive and continuous examination. Challenges remain, however, including the recommendation of limited outpatient visits. A more comprehensive application of intelligent nanosystems may contribute to broad-spectrum testing and early diagnosis of the SARS-CoV-2 infection even as well as can mitigate the SARS-CoV-2 transmission thus be part of protecting strategy of these vulnerable group of patients.
Supplementary Information
Below is the link to the electronic supplementary material.
Author contribution
HMA and AIA conceptualized the study; HMA, AIA, MK, and AK collected the data. HMA, GEB, and MK interpreted the data. AIA and MK drafted the initial version; HMA, GEB, MK, and AK revising it critically for important intellectual content approved the final version to be published. All authors remain in agreement to be accountable for all aspects of the work.
This article does not contain any studies with human participants or animals performed by any of the authors.
Data availability
Not applicable.
Declarations
Conflict of interest
The authors declare no competing interests.
Footnotes
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Hayder M. Al-kuraishy, Email: Hayderm36@yahoo.com
Ali I. Al-Gareeb, Email: Dr.alialgareeb78@yahoo.com
Małgorzata Kujawska, Email: kujawska@ump.edu.pl.
Gaber El-Saber Batiha, Email: gaberbatiha@gmail.com.
References
- 1.Al-Kuraishy HM, Al-Gareeb AI. Comparison of deferasirox and deferoxamine effects on iron overload and immunological changes in patients with blood transfusion-dependent β-thalassemia. Asian J Transfus Sci. 2017;11:13–17. doi: 10.4103/0973-6247.200768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Berentsen S, Barcellini W. Autoimmune hemolytic anemias. N Engl J Med. 2021;385:1407–1419. doi: 10.1056/NEJMra2033982. [DOI] [PubMed] [Google Scholar]
- 3.Hill QA, Hill A, Berentsen S. Defining autoimmune hemolytic anemia: a systematic review of the terminology used for diagnosis and treatment. Blood Adv. 2019;3:1897–1906. doi: 10.1182/bloodadvances.2019000036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chaudhary RK, Das SS. Autoimmune hemolytic anemia: from lab to bedside. Asian J Transfus Sci. 2014;8:5–12. doi: 10.4103/0973-6247.126681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Liebman HA, Weitz IC. Autoimmune hemolytic anemia. Med Clin North Am. 2017;101:351–359. doi: 10.1016/j.mcna.2016.09.007. [DOI] [PubMed] [Google Scholar]
- 6.Giannotta JA, Fattizzo B, Cavallaro F, Barcellini W. Infectious complications in autoimmune hemolytic anemia. J Clin Med. 2021;10(1):164. doi: 10.3390/jcm10010164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Pathak S. Convalescent plasma: Would it prove to be magic potion/boon in the current scenario of COVID pandemic? Asian J Transfus Sci. 2020;14:1–3. doi: 10.4103/0973-6247.290652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Al-kuraishy HM, A-M T, Al-Gareeb AI, Musa RA, Ali ZH. COVID-19 pneumonia in an Iraqi pregnant woman with preterm delivery. 0:1-1
- 9.Lugnier C, Al-Kuraishy HM, Rousseau E. PDE4 inhibition as a therapeutic strategy for improvement of pulmonary dysfunctions in Covid-19 and cigarette smoking. Biochem Pharmacol. 2021;185:114431 . doi: 10.1016/j.bcp.2021.114431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gehrs BC, Friedberg RC. Autoimmune hemolytic anemia. Am J Hematol. 2002;69:258–271. doi: 10.1002/ajh.10062. [DOI] [PubMed] [Google Scholar]
- 11.Abouyabis AN, Bell GT. Hemolytic anemia complicating COVID-19 infection. J Hematol. 2021;10:221–227. doi: 10.14740/jh906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Maslov DV, Simenson V, Jain S, Badari A. COVID-19 and cold agglutinin hemolytic anemia. TH Open. 2020;4:e175–e177. doi: 10.1055/s-0040-1715791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Russo A, Tellone E, Barreca D, Ficarra S, Laganà G. Implication of COVID-19 on erythrocytes functionality: red blood cell biochemical implications and morpho-functional aspects. Int J Mol Sci. 2022;23:2171. doi: 10.3390/ijms23042171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Roy NBA, Telfer P, Eleftheriou P, de la Fuente J, Drasar E, Shah F, Roberts D, Atoyebi W, Trompeter S, Layton DM, et al. Protecting vulnerable patients with inherited anaemias from unnecessary death during the COVID-19 pandemic. Br J Haematol. 2020;189:635–639. doi: 10.1111/bjh.16687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Severance TS, Rahim MQ, French J, Baker RM, Shriner A, Khaitan A, Overholt KM. COVID-19 and hereditary spherocytosis: a recipe for hemolysis. Pediatr Blood Cancer. 2021;68:e28548. doi: 10.1002/pbc.28548. [DOI] [PubMed] [Google Scholar]
- 16.Fronza Michele, F B, Stirpe Emanuele. Acute lung failure due to COVID-19 in a patient with sickle cell anemia. Minerva Pneumologica 2020. 2021;59(2):44–6. [Google Scholar]
- 17.Algassim AA, Elghazaly AA, Alnahdi AS, Mohammed-Rahim OM, Alanazi AG, Aldhuwayhi NA, Alanazi MM, Almutairi MF, Aldeailej IM, Kamli NA, et al. Prognostic significance of hemoglobin level and autoimmune hemolytic anemia in SARS-CoV-2 infection. Ann Hematol. 2021;100:37–43. doi: 10.1007/s00277-020-04256-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Taherifard E, Taherifard E, Movahed H, Mousavi MR. Hematologic autoimmune disorders in the course of COVID-19: a systematic review of reported cases. Hematology. 2021;26:225–239. doi: 10.1080/16078454.2021.1881225. [DOI] [PubMed] [Google Scholar]
- 19.Lazarian G, Quinquenel A, Bellal M, Siavellis J, Jacquy C, Re D, Merabet F, Mekinian A, Braun T, Damaj G, et al. Autoimmune haemolytic anaemia associated with COVID-19 infection. Br J Haematol. 2020;190:29–31. doi: 10.1111/bjh.16794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Vega Hernández P, Borges Rivas Y, Ortega Sánchez E, Marqués Cabrero A, Remedios Mateo L, Silvera Roig P, Infante Quintanar A, Díaz-Delgado Peñas R, Sánchez Escudero V, García-García ML. Autoimmune hemolytic anemia in a pediatric patient with severe acute respiratory syndrome coronavirus 2 infection. Pediatr Infect Dis J. 2020;39:e288. doi: 10.1097/INF.0000000000002809. [DOI] [PubMed] [Google Scholar]
- 21.Zama D, Pancaldi L, Baccelli F, Guida F, Gottardi F, Dentale N, Esposito F, Masetti R, Viale P, Pession A. Autoimmune hemolytic anemia in children with COVID-19. Pediatric Blood & Cancer. 2022;69(2):e29330. doi: 10.1002/pbc.29330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.AbouYabis AN, Bell GT. Hemolytic anemia complicating COVID-19 infection. J Hematol. 2021;10:221–227. doi: 10.14740/jh906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.D’Alessandro A, Thomas T, Dzieciatkowska M, Hill RC, Francis RO, Hudson KE, Zimring JC, Hod EA, Spitalnik SL, Hansen KC. Serum proteomics in COVID-19 patients: altered coagulation and complement status as a function of IL-6 level. J Proteome Res. 2020;19:4417–4427. doi: 10.1021/acs.jproteome.0c00365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lam LKM, Reilly JP, Rux AH, Murphy SJ, Kuri-Cervantes L, Weisman AR, Ittner CAG, Pampena MB, Betts MR, Wherry EJ, et al. Erythrocytes identify complement activation in patients with COVID-19. American J Physiol-Lung Cell Molecular Physiol. 2021;321:L485–L489. doi: 10.1152/ajplung.00231.2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Damani J. Disseminated intravascular coagulopathy from warm autoimmune hemolytic anemia in a patient with COVID-19. Chest. 2020;158:A397. doi: 10.1016/j.chest.2020.08.388. [DOI] [Google Scholar]
- 26.Grobler C, Maphumulo SC, Grobbelaar LM, Bredenkamp JC, Laubscher GJ, Lourens PJ, Steenkamp J, Kell DB, Pretorius E. Covid-19: the rollercoaster of fibrin(Ogen), D-dimer, Von Willebrand factor, P-selectin and their interactions with endothelial cells, platelets and erythrocytes. Int J Mol Sci. 2020;21(14):5168. doi: 10.3390/ijms21145168.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Solari D, Alberio L, Ribi C, Grandoni F, Stalder G. Autoimmune hemolytic anemia and pulmonary embolism: an association to consider. TH Open. 2021;05:e8–e13. doi: 10.1055/s-0040-1721733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Patil NR, Herc ES, Girgis M (2020) Cold agglutinin disease and autoimmune hemolytic anemia with pulmonary embolism as a presentation of COVID-19 infection. Hematol Oncol Stem Cell Ther. 10.1016/j.hemonc.2020.06.005 [DOI] [PMC free article] [PubMed]
- 29.Elmassry M, Vutthikraivit W, Abdelmalek J, Rahman MR, Makram J, Mortagy M, Test V. Warm autoimmune hemolytic anemia as a rare cause of pulmonary embolism. Chest. 2020;158:A2095–A2096. doi: 10.1016/j.chest.2020.08.1810. [DOI] [Google Scholar]
- 30.Venter C, Bezuidenhout JA, Laubscher GJ, Lourens PJ, Steenkamp J, Kell DB, Pretorius E. Erythrocyte, platelet, serum ferritin, and P-selectin pathophysiology implicated in severe hypercoagulation and vascular complications in COVID-19. Int J Mol Sci. 2020;21(21):8234. doi: 10.3390/ijms21218234.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kang C, Kim DH, Kim T, Lee SH, Jeong JH, Lee SB, Kim JH, Jung MH, Lee KW, Park IS. Therapeutic effect of ascorbic acid on dapsone-induced methemoglobinemia in rats. Clin Exp Emerg Med. 2018;5:192–198. doi: 10.15441/ceem.17.253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Palmer K, Dick J, French W, Floro L, Ford M. Methemoglobinemia in patient with G6PD deficiency and SARS-CoV-2 infection. Emerg Infect Dis. 2020;26(9):2279–2281. doi: 10.3201/eid2609.202353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Lopes DV, Lazar Neto F, Marques LC, Lima RBO, Brandão AAGS. Methemoglobinemia and hemolytic anemia after COVID-19 infection without identifiable eliciting drug: a case-report. IDCases. 2021;23:e01013. doi: 10.1016/j.idcr.2020.e01013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Liu Wenzhong Lh (2021) COVID-19: attacks the 1-beta chain of hemoglobin an captures the porphyrin to inhibit human heme metabolism. ChemRxiv. Cambridge: Cambridge Open Engage
- 35.DeMartino AW, Rose JJ, Amdahl MB, Dent MR, Shah FA, Bain W, McVerry BJ, Kitsios GD, Tejero J, Gladwin MT. No evidence of hemoglobin damage by SARS-CoV-2 infection. Haematologica. 2020;105:2769–2773. doi: 10.3324/haematol.2020.264267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Cavezzi A, Troiani E, Corrao S. COVID-19: hemoglobin, iron, and hypoxia beyond inflammation. A narrative review Clin Pract. 2020;10:1271. doi: 10.4081/cp.2020.1271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Angileri F, Légaré S, Marino Gammazza A, Conway de Macario E, Macario AJL, Cappello F. Is molecular mimicry the culprit in the autoimmune haemolytic anaemia affecting patients with COVID-19? Br J Haematol. 2020;190:e92–e93. doi: 10.1111/bjh.16883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Varadarajan S, Balaji TM, Sarode SC, Sarode GS, Sharma NK, Gondivkar S, Gadbail A, Patil S. EMMPRIN/BASIGIN as a biological modulator of oral cancer and COVID-19 interaction: Novel propositions. Med Hypotheses. 2020;143:110089 . doi: 10.1016/j.mehy.2020.110089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Wang K, Chen W, Zhang Z, Deng Y, Lian JQ, Du P, Wei D, Zhang Y, Sun XX, Gong L, et al. CD147-spike protein is a novel route for SARS-CoV-2 infection to host cells. Signal Transduct Target Ther. 2020;5:283. doi: 10.1038/s41392-020-00426-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Behl T, Kaur I, Aleya L, Sehgal A, Singh S, Sharma N, Bhatia S, Al-Harrasi A, Bungau S. CD147-spike protein interaction in COVID-19: get the ball rolling with a novel receptor and therapeutic target. Sci Total Environ. 2022;808:152072 . doi: 10.1016/j.scitotenv.2021.152072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Bian H, Zheng ZH, Wei D, Zhang Z, Kang WZ, Hao CQ, Dong K, Kang W, Xia JL, Miao JL et al (2020) Meplazumab treats COVID-19 pneumonia: An open-labelled, concurrent controlled add-on clinical trial. medRxiv 2020.2003.2021.20040691. 10.1101/2020.03.21.20040691.
- 42.Ulrich H, Pillat MM. CD147 as a target for COVID-19 treatment: suggested effects of azithromycin and stem cell engagement. Stem Cell Rev Rep. 2020;16:434–440. doi: 10.1007/s12015-020-09976-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Shilts J, Crozier TWM, Greenwood EJD, Lehner PJ, Wright GJ. No evidence for basigin/CD147 as a direct SARS-CoV-2 spike binding receptor. Sci Rep. 2021;11:413. doi: 10.1038/s41598-020-80464-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Miao J, Zhang K, Zheng Z, Zhang R, Lv M, Guo N, Xu Y, Han Q, Chen Z, Zhu P. CD147 expressed on memory CD4. Front Immunol. 2020;11:545980. doi: 10.3389/fimmu.2020.545980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Raony Í, Saggioro de Figueiredo C (2020) Retinal outcomes of COVID-19: possible role of CD147 and cytokine storm in infected patients with diabetes mellitus. Diabetes Res Clin Pract 165:108280. 10.1016/j.diabres.2020.108280.London [DOI] [PMC free article] [PubMed]
- 46.Tan L, Wang Q, Zhang D, Ding J, Huang Q, Tang YQ, Miao H. Lymphopenia predicts disease severity of COVID-19: a descriptive and predictive study. Signal Transduct Target Ther. 2020;5:33. doi: 10.1038/s41392-020-0148-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Thomas T, Stefanoni D, Dzieciatkowska M, Issaian A, Nemkov T, Hill RC, Francis RO, Hudson KE, Buehler PW, Zimring JC, et al. Evidence of structural protein damage and membrane lipid remodeling in red blood cells from COVID-19 patients. J Proteome Res. 2020;19:4455–4469. doi: 10.1021/acs.jproteome.0c00606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Østergaard L. SARS CoV-2 related microvascular damage and symptoms during and after COVID-19: consequences of capillary transit-time changes, tissue hypoxia and inflammation. Physiol Rep. 2021;9(3):e14726. doi: 10.14814/phy2.14726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Lancman G, Marcellino BK, Thibaud S, Troy K. Coombs-negative hemolytic anemia and elevated plasma hemoglobin levels in COVID-19. Ann Hematol. 2021;100:833–835. doi: 10.1007/s00277-020-04202-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Bhardwaj N, Singh A. Splenectomy modulates the erythrocyte turnover and Basigin (CD147) expression in mice. Indian J Hematol Blood Transfus. 2020;36:711–718. doi: 10.1007/s12288-020-01272-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Cosic I, Cosic D, Loncarevic I. RRM prediction of erythrocyte band3 protein as alternative receptor for SARS-CoV-2 virus. Appl Sci. 2020;10:4053. doi: 10.3390/app10114053. [DOI] [Google Scholar]
- 52.Nemkov T, Reisz JA, Xia Y, Zimring JC, D'Alessandro A. Red blood cells as an organ? How deep omics characterization of the most abundant cell in the human body highlights other systemic metabolic functions beyond oxygen transport. Expert Rev Proteomics. 2018;15:855–864. doi: 10.1080/14789450.2018.1531710. [DOI] [PubMed] [Google Scholar]
- 53.Reisz JA, Wither MJ, Dzieciatkowska M, Nemkov T, Issaian A, Yoshida T, Dunham AJ, Hill RC, Hansen KC, D'Alessandro A. Oxidative modifications of glyceraldehyde 3-phosphate dehydrogenase regulate metabolic reprogramming of stored red blood cells. Blood. 2016;128:e32–42. doi: 10.1182/blood-2016-05-714816. [DOI] [PubMed] [Google Scholar]
- 54.Zhou Y, Ding N, Yang G, Peng W, Tang F, Guo C, Chai X. Serum lactate dehydrogenase level may predict acute respiratory distress syndrome of patients with fever infected by SARS-CoV-2. Ann Transl Med. 2020;8:1118. doi: 10.21037/atm-20-2411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Del Vecchio L, Locatelli F. Hypoxia response and acute lung and kidney injury: possible implications for therapy of COVID-19. Clin Kidney J. 2020;13:494–499. doi: 10.1093/ckj/sfaa149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Aguiar JA, Tremblay BJ, Mansfield MJ, Woody O, Lobb B, Banerjee A, Chandiramohan A, Tiessen N, Cao Q, Dvorkin-Gheva A et al (2020) Gene expression and. Eur Respir J 56. 10.1183/13993003.01123-2020. [DOI] [PMC free article] [PubMed]
- 57.D'Alessandro A, Fu X, Kanias T, Reisz JA, Culp-Hill R, Guo Y, Gladwin MT, Page G, Kleinman S, Lanteri M, et al. Donor sex, age and ethnicity impact stored red blood cell antioxidant metabolism through mechanisms in part explained by glucose 6-phosphate dehydrogenase levels and activity. Haematologica. 2021;106:1290–1302. doi: 10.3324/haematol.2020.246603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Marfia G, Navone S, Guarnaccia L, Campanella R, Mondoni M, Locatelli M, Barassi A, Fontana L, Palumbo F, Garzia E, et al. Decreased serum level of sphingosine-1-phosphate: a novel predictor of clinical severity in COVID-19. EMBO Mol Med. 2021;13:e13424. doi: 10.15252/emmm.202013424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Selim S, Sunkara M, Salous AK, Leung SW, Berdyshev EV, Bailey A, Campbell CL, Charnigo R, Morris AJ, Smyth SS. Plasma levels of sphingosine 1-phosphate are strongly correlated with haematocrit, but variably restored by red blood cell transfusions. Clin Sci (Lond) 2011;121:565–572. doi: 10.1042/CS20110236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Alam S, Kamal TB, Sarker MMR, Zhou JR, Rahman SMA, Mohamed IN. Therapeutic effectiveness and safety of repurposing drugs for the treatment of COVID-19: position standing in 2021. Front Pharmacol. 2021;12:659577. doi: 10.3389/fphar.2021.659577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Ha F, John A, Zumwalt M. The Southwest Respiratory and Critical Care Chronicles. 10.12746/swrccc.v9i37.795
- 62.Doyno C, Sobieraj DM, Baker WL. Toxicity of chloroquine and hydroxychloroquine following therapeutic use or overdose. Clin Toxicol (Phila) 2021;59:12–23. doi: 10.1080/15563650.2020.1817479. [DOI] [PubMed] [Google Scholar]
- 63.Mohammad S, Clowse MEB, Eudy AM, Criscione-Schreiber LG. Examination of hydroxychloroquine use and hemolytic anemia in G6PDH-deficient patients. Arthritis Care Res (Hoboken) 2018;70:481–485. doi: 10.1002/acr.23296. [DOI] [PubMed] [Google Scholar]
- 64.Khalili JS, Zhu H, Mak NSA, Yan Y, Zhu Y. Novel coronavirus treatment with ribavirin: groundwork for an evaluation concerning COVID-19. J Med Virol. 2020;92:740–746. doi: 10.1002/jmv.25798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Eslami G, Mousaviasl S, Radmanesh E, Jelvay S, Bitaraf S, Simmons B, Wentzel H, Hill A, Sadeghi A, Freeman J, et al. The impact of sofosbuvir/daclatasvir or ribavirin in patients with severe COVID-19. J Antimicrob Chemother. 2020;75:3366–3372. doi: 10.1093/jac/dkaa331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Sato S, Moriya K, Furukawa M, Saikawa S, Namisaki T, Kitade M, Kawaratani H, Kaji K, Takaya H, Shimozato N, et al. Efficacy of L-carnitine on ribavirin-induced hemolytic anemia in patients with hepatitis C virus infection. Clin Mol Hepatol. 2019;25:65–73. doi: 10.3350/cmh.2018.0070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Nabil A, Uto K, Elshemy MM, Soliman R, Hassan AA, Ebara M, Shiha G. Current coronavirus (SARS-CoV-2) epidemiological, diagnostic and therapeutic approaches: an updated review until June 2020. EXCLI J. 2020;19:992–1016. doi: 10.17179/excli2020-2554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Tao Z, Xu J, Chen W, Yang Z, Xu X, Liu L, Chen R, Xie J, Liu M, Wu J, et al. Anemia is associated with severe illness in COVID-19: a retrospective cohort study. J Med Virol. 2021;93:1478–1488. doi: 10.1002/jmv.26444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Fattizzo B, Pasquale R, Bellani V, Barcellini W, Kulasekararaj AG. Complement mediated hemolytic anemias in the COVID-19 era: case series and review of the literature. Front Immunol. 2021;12:791429. doi: 10.3389/fimmu.2021.791429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Fatima Z, Reece BRA, Moore JS, Means RT. Autoimmune hemolytic anemia after mRNA COVID vaccine. J Investig Med High Impact Case Rep. 2022;10:232470962110732. doi: 10.1177/23247096211073258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Lopez C, Kim J, Pandey A, Huang T, Deloughery TG. Simultaneous onset of COVID-19 and autoimmune haemolytic anaemia. Br J Haematol. 2020;190:31–32. doi: 10.1111/bjh.16786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Nair LJ, Regukumar A, Baalamurugan KT. COVID-19-associated severe autoimmune hemolytic anemia: a rare case report. Saudi J Med Med Sci. 2021;9:276–279. doi: 10.4103/sjmms.sjmms_203_21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Brazel D, Eid T, Harding C. Warm and cold autoimmune hemolytic anemia in the setting of COVID-19 disease. Cureus. 2021;13:e18127. doi: 10.7759/cureus.18127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Hindilerden F, Yonal-Hindilerden I, Akar E, Yesilbag Z, Kart-Yasar K. Severe autoimmune hemolytic anemia in COVID-19 infection, safely treated with steroids. Mediterr J Hematol Infect Dis. 2020;12:e2020053. doi: 10.4084/MJHID.2020.053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Campos-Cabrera G, Mendez-Garcia E, Mora-Torres M, Campos-Cabrera S, Campos-Cabrera V, Garcia-Rubio G, Jose-Luis CV (2020) Autoimmune hemolytic anemia as initial presentation of COVID-19 infection. Blood 136:8. 10.1182/blood-2020-139001.
- 76.Huda Z, Jahangir A, Sahra S, Rafay Khan Niazi M, Anwar S, Glaser A (2021) A Case of COVID-19-associated autoimmune hemolytic anemia with hyperferritinemia in an immunocompetent host. Cureus 13(6):e16078. 10.7759/cureus.16078. [DOI] [PMC free article] [PubMed]
- 77.Ahmadivand A, Gerislioglu B, Ramezani Z, Kaushik A, Manickam P, Ghoreishi SA. Functionalized terahertz plasmonic metasensors: femtomolar-level detection of SARS-CoV-2 spike proteins. Biosens Bioelectron. 2021;177:112971. doi: 10.1016/j.bios.2021.112971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Kaushik AK, Dhau JS, Gohel H, Mishra YK, Kateb B, Kim NY, Goswami DY. Electrochemical SARS-CoV-2 sensing at point-of-care and artificial intelligence for intelligent COVID-19 management. ACS Appl Bio Mater. 2020;3:7306–7325. doi: 10.1021/acsabm.0c01004. [DOI] [PubMed] [Google Scholar]
- 79.Mostafavi E, Dubey AK, Teodori L, Ramakrishna S, Kaushik A (2020) SARS‐CoV‐2 Omicron variant: A next phase of the COVID‐19 pandemic and a call to arms for system sciences and precision medicine. MedComm 3. 10.1002/mco2.119. [DOI] [PMC free article] [PubMed]
- 80.Tiwari S, Juneja S, Ghosal A, Bandara N, Khan R, Wallen SL, Ramakrishna S, Kaushik A. Antibacterial and antiviral high-performance nanosystems to mitigate new SARS-CoV-2 variants of concern. Curr Opin Biomed Eng. 2022;21:100363. doi: 10.1016/j.cobme.2021.100363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Campos D, Navarro S, Llamas-González YY, Sugasti M, González-Santamaría J. Broad antiviral activity of ginkgolic acid against chikungunya, Mayaro, Una, and Zika Viruses. Viruses. 2020;12(4):449. doi: 10.3390/v12040449. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Not applicable.