Abstract
The coronavirus disease 2019 (COVID-19) outbreak became a worldwide pandemic in 2020. Social distancing measures, such as self-quarantine, lockdowns, and school closures, which have proven efficacy in various pandemic situations, remain in use in Korea. These measures prevented viral transmission to some extent; however, adverse effects have also resulted. First, the negative effect of social isolation on mental health is evident. This influences the psychiatric milieu of parents and children directly and indirectly. The most stressful factor among Korean youth was the restriction of outdoor activities. Increasing parenting burden result in increased screen time among youth, and social isolation created depressive mood with symptoms similar to those of attention deficit hyperactivity disorder and anxiety. Second, symptoms of posttraumatic stress disorder (PTSD) and somatization are prevalent among children and adolescents. The sense of threatened health and life during the pandemic, one symptom of PTSD, is a strong risk factor for somatization. Finally, the increased pattern of child abuse in pandemic indicates increased levels of emotional/psychological abuse and nonmedical neglect. Social isolation makes people less aware of these events. Because pediatricians evaluate pediatric patients and their families, they should regularly assess emotional/stress factors, especially when somatization is prominent during the pandemic, and cautiously recommend that families seek advice from mental health professionals when warranted. Primary physicians must understand the characteristics and aspects of child abuse in the COVID-19 pandemic, make efforts to identify signs of child abuse, and deliver accurate information and preventive strategies for child abuse to caregivers, thereby functioning as a professional guardian. To promote the mental health of parents and children during the COVID-19 pandemic, more research and cooperation among health professionals, families, governments, and schools are needed in the future.
Keywords: COVID-19, Depression, Anxiety, Posttraumatic stress disorder, Somatization, Child abuse
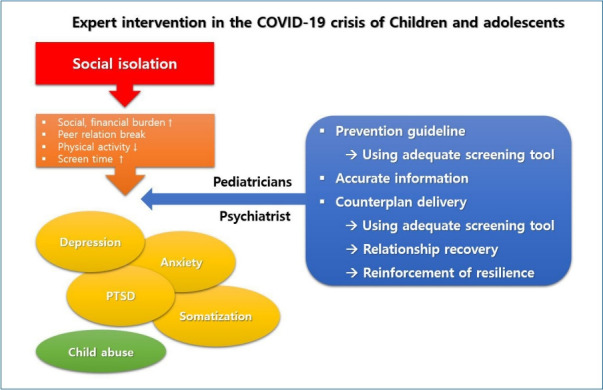
Graphical abstract
Introduction
Coronavirus disease 2019 (COVID-19), which was first reported as an infectious acute respiratory disease in Wuhan, China, in 2019, has rapidly spread worldwide. Although severe acute respiratory syndrome and Middle East respiratory syndrome outbreaks occurred in 2003 and 2013, respectively, they differed from COVID-19 in terms of infectivity. These viruses are typically contagious when an individual is symptomatic; thus, the spread rates in the community were low. In contrast, COVID-19 is highly contagious, even during symptom-free periods. This characteristic led to the COVID-19 pandemic and, ultimately, the “new normal” era that ultimately changed the daily life of humankind. Since social distancing methods such as self-quarantining, lockdowns, and school closures were effective in previous pandemic situations, many countries worldwide have implemented them during the COVID-19 pandemic [1].
In the South Korean guidelines for disease prevention published in 2020 [2], during the early phase of the COVID-19 pandemic, the prevention measure focused primarily on physical social distancing was adapted to immune-deprived adults and admitted patients in psychiatric hospitals and nursing hospitals who were at high risk of cluster infection [3]. At that point, little attention was paid to the psychological aspect of children and adolescents, particularly due to isolation from their daily social activities, peers, and teachers due to school closures. Wearing masks prevents children and adolescents from having the natural opportunity to experience and learn non-verbal communication with others in society. As reported by numerous studies, the socioeconomical, psychological, and physical aspects of the COVID-19 pandemic have been devastating on the development of children and adolescents [4]. Their cognitive development in particular was negatively affected, and their coping strategies are incomplete and emotionally immature. These features of young people make them vulnerable to stressful factors during disasters despite still experiencing critical developmental tasks. During that time, they develop their basic attitudes toward life by interacting with other people and diverse environments; these experiences give them resilience to inevitable stressful life events. Therefore, youths are especially vulnerable in disasters such as COVID-19 because high anxiety impairs their ability to learn.
A large number of psychiatric studies of the mental health of children and adolescents in this pandemic era have been published in the United States and China [4,5]. However, few of the same have been published in South Korea. The South Korean government recently aimed to expand the mental health factual survey for adults to include children and adolescents. This trial reflects the government’s concern about the mental health of those vulnerable age group.
This study aimed to review various studies of the mental health of children and adolescents during the COVID-19 pandemic including the domain of child abuse in an effort to provide direction for their further management.
Effect of COVID-19 pandemic on mental health of children and adolescents
Previous studies of the effect of COVID-19 pandemic on the mental health of children and adolescents reported increased depression, anxiety, and posttraumatic symptoms [3,4]. One study reported that parental unemployment and financial difficulties are clearly associated with their children’s emotional problems [6]. In other studies, excessive smartphone use and increased internet addictions due to increased isolation among youth were associated with depressive symptoms during the COVID-19 pandemic [5,7].
The supervision and care of youth have been compromised during the COVID-19 pandemic. To prevent its transmission throughout the community, self-quarantine and school closures were implemented. These actions resulted in children being left alone at home without proper caregiving, especially those in double-income families. The increased burden of childrearing leads to parental permission for their children to use digital media, even when the parents are at home. In fact, the mean screen time of children and adolescents since the COVID-19 outbreak (3.96±2.28 hours per day) is significantly higher than that before the outbreak (2.2±1.84 hours per day) [8]. The recommended media exposure time is below 2 hours per day [9]. In a previous study, a screen time longer than 2 hours per day increased depression and suicidal ideation in children and adolescents. Depression among children and adolescents was reportedly increased according to many studies since the COVID-19 outbreak, consistent with another previous study [10,11]. This is a problematic phenomenon, especially in 3–5-yearold children in South Korea because 2.5% of that age group was already at high risk of smartphone dependency and 11.4% were at potential risk before the pandemic [12].
Moreover, sleep problems due to increased screen time exacerbate children’s negative emotions [13]. A previous study suggested that the electromagnetic fields generated by mobile phones were associated with less favorable sleep duration, nocturnal awakening, and parasomnia in 7-year-old children [14]. Furthermore, increased screen time also causes symptoms of attention deficit hyperactivity disorder (ADHD), which increases parenting burden [15,16]. These ADHD similar symptoms results in a vicious cycle through negative feedback from parents to their children that worsen children’s depression and anxiety symptoms.
In one study of the effect of COVID-19 on stress in children and adolescents in South Korea, the most stressful factor among youth was the restriction of outdoor activities, such as inability to meet friends and stay at home orders. The second most stressful factor was difficulty understanding lecture content through online classes [17]. As a result, children who perceived this kind of stress showed more intense emotional difficulties. They were also more susceptible to depressive mood, anxiety symptoms, more aggressive behavior, and greater dependency on smartphones; all of these effects negatively correlated with academic difficulties that ended up lowering self-esteem among children and adolescents [17]. On the contrary, some positive reports stated that more time spent at home with their parents prevented children and adolescents from suicidal attempt and substance use disorders, although further long-term studies are needed [18].
Some studies revealed that older adolescents show more depressive symptoms than younger adolescents and children [19]. However, the existence of differences in anxiety symptoms by age remains controversial. While 2 studies reported no difference in anxiety symptoms by age [19,20], another reported that anxiety symptoms increased with increasing age [21].
Relationship between children’s negative emotions and posttraumatic stress disorder in the COVID-19 pandemic
According to the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition [22], “experiencing repeated or extreme exposure to aversive details of the traumatic events” is a potential traumatic event. Accordingly, the COVID-19 pandemic can be defined as a traumatic disaster [23]. Like sudden acute respiratory syndrome and Middle East respiratory syndrome, COVID-19 causes posttraumatic stress disorder (PTSD) symptoms in healthcare workers such as intrusive thoughts associated with traumatic memory, persistent avoidance, negative alterations in cognition and mood, and hyperarousal [24,25]. Similarly, children and adolescents also suffer from PTSD symptoms in this pandemic situation. Recent research revealed that the prevalence of PTSD among 57,948 high school students after COVID-19 outbreak peaked at 16.9% and emphasized the long-term adverse consequences on their mental health [26]. It is also suggested that COVID- 19 pandemic itself functions as a big traumatic event to youth, causing PTSD symptoms and in turn increasing their depressive symptoms.
Because somatization is one of most prevalent symptoms in children and adolescents with mental health issues, it also should be spotlighted. Somatization is simply defined as a persistent somatic symptom with no evident organic cause even after a thorough medical evaluation. Symptoms can vary but include dizziness, pain, fatigue, and musculoskeletal manifestations [27,28]. Depressed youths often complain of somatic symptoms such as headaches and stomachaches; this is a unique feature of children versus adults with depression [29,30]. As mentioned above, children and adolescents with limited ability to recognize their emotions frequently experience negative emotions during the COVID-19 pandemic, which in turn causes somatic symptoms that negatively affect their physical and psychological well-being. Therefore, pediatricians have increased opportunities to evaluate youth in the clinic settings; moreover, it is recommended that emotional and stressful factors be addressed and evaluated by pediatricians in primary pediatric clinic settings during the COVID-19 pandemic.
In one cross-sectional study of primary school students during the early COVID-19 pandemic in China, children were asked to complete self-questionnaires of their somatization symptoms and concerns about COVID-19 [31]. In that study, primary school students with somatization symptoms reported a higher threat to their lives and health, which in turn was revealed as a strong risk factor for somatization. Interestingly, anxiety, not depression, was associated with somatization. Jowett et al. [32] suggested that the sense of threat, among the PTSD symptom cluster of the International Classification of Diseases, Eleventh Edition, also showed a strong association with somatization in adults.
In previous studies, the lower the resilience, the greater the degree of somatization. Resilience is defined as an ability to recover from stress [33,34]. Shangguan et al. [35] reported that lower resilience is a predictor of somatization, while perceived stress acts as a moderator of resilience and somatization. Perceived stress is more intense and more prevalent among women than among men, revealing a sex-based difference. Therefore, interventions that improve resilience would decrease somatization [36-38]. This is expected to be more beneficial for youths and their caretakers, mostly women, in Korea during the COVID-19 pandemic, but further investigations are required.
COVID-19 pandemic and child abuse inside the family
It is essential to address child abuse issues in the COVID-19 pandemic. Child abuse is a huge traumatic experience to developing young minds that negatively affects an individual’s emotional and physical well-being throughout the lifespan. Social isolation in the COVID-19 pandemic is a well-known risk factor of child abuse [39,40]. Most child abuse occurs at home by parents, with whom social isolation due to COVID-19 puts children in closer contact, who are nervous and edgy because of social and financial distress [41]. This situation of home lockdown increases the likelihood of child abuse. Brown et al. suggested that parental situations including needing financial help, depression, and anxiety are strongly associated with the likelihood of child abuse [42]. Likewise, Lawson et al. [43] reported that parental unemployment is risk factor of both psychological and physical child abuse.
In 2020, Ministry of Health and Welfare of South Korea published a document entitled “Major Statistic Data of Child Abuse,” which reported a 2.1% increase in child abuse reporting compared to the 13.7% rate of 2019 [41]. Also, 92.1% of child abuse cases were reported in 2020 versus 92.7% in 2019 (Table 1, Fig. 1) [41,44]. In South Korea, among mandatory child abuse reporters, employees of primary, middle, and high schools showed the highest reporting rate (Table 2; Figs. 2, 3). However, reported cases by primary, middle, and high school employees decreased from 5,901 cases in 2019 to 3,805 cases in 2020 [41]. Online classes due to school closure in 2020 hindered teachers from observing their students directly and talking face to face with them. Although the COVID-19 pandemic is a period of a high likelihood of child abuse, teachers have difficulty noticing abuse clues among their students due to physical and temporal obstructions. On the contrary, cases reported to Child Protective Services (CPS), public officers, and child welfare workers were greatly increased. Reports by healthcare providers and physicians were also slightly increased from 293 cases in 2019 to 363 cases in 2020 [41]. It is encouraging that reports by healthcare providers and physicians were increased since it implies that the role of reporting child abuse by police officers, physicians, and CPS has become more important since the COVID-19 outbreak. These professionals are recommended to have increased knowledge and more intent to detect child abuse. However, this will be possible only with the provision of greater governmental support.
Table 1.
Child abuse case reporting in South Korea, 2010–2020
| Reported type | 2010 | 2011 | 2012 | 2013 | 2014 | 2015 | 2016 | 2017 | 2018 | 2019 | 2020 |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Suspected child abuse cases | 6,513 (80.5) | 8,325 (82.1) | 8,979 (82.1) | 10,857 (83.0) | 15,025 (84.5) | 16,651 (86.7) | 25,878 (87.2) | 30,923 (90.5) | 33,532 (92.1) | 38,380 (92.7) | 38,929 (92.1) |
| Overlapping reports of child abuse cases | 89 (1.0) | 84 (0.8) | 34 (0.3) | 43 (0.3) | 93 (0.5) | 87 (0.5) | 189 (0.6) | 292 (0.9) | 420 (1.2) | 449 (1.1) | 557 (1.3) |
| Only general consultation (no child abuse) | 1,704 (18.5) | 1,737 (17.1) | 1,930 (17.6) | 2,176 (16.6) | 2,664 (15) | 2,465 (12.8) | 3,604 (12.1) | 2,951 (8.6) | 2,464 (6.8) | 2,560 (6.2) | 2,761 (6.5) |
| Child abuse cases reported from outside of Korean territory | - | - | - | - | 9 (0.1) | 11 (0.1) | 3 (0) | 3 (0) | 1 (0) | 0 (0) | 4 (0) |
Values are presented as number (%).
Data from Child Abuse & Neglect Korea, 2018.2020. Ministry of Health and Welfare, Republic of Korea.
Fig. 1.
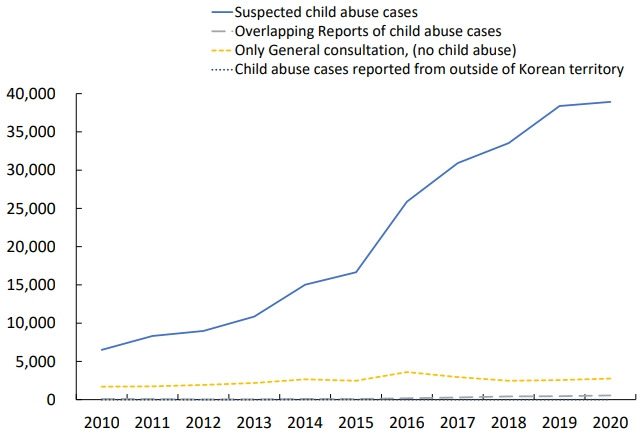
Child abuse case reporting in South Korea, 2010–2020.
Table 2.
Types of child abuse reporters, 2019 and 2020
| No. | 2019 |
2020 |
||
|---|---|---|---|---|
| Mandatory reporter of child abuse | Nonmandatory reporter of child abuse | Mandatory reporter of child abuse | Nonmandatory reporter of child abuse | |
| 1 | Primary/middle/high school employees (5,901, 15.4%) | Employers 0f Child Protection Service as nonmandatory reporters (12,389, 32.3%) | Primary/middle/high school employees (3,805, 9.8%) | Employers of child protection service as nonmandatory reporters (10,254, 26.3%) |
| 2 | Nursing staffs at schools (448, 1.2%) | Parents (6,506, 17%) | Employers of child protection service as mandatory reporters (2,394, 6.1%) | Parents (6284, 16.1%) |
| 3 | Employers of child welfare institution (337, 0.9%) | Child self (4652, 12.4%) | Public officers in the field of child welfare (984, 2.5%) | Child self (5533, 14.2%) |
| 4 | Healthcare provider/medical professionals (293, 0.8%) | Neighbors/friends (1,718, 4.5%) | Employers in institutions for child welfare (711, 1.8%) | Neighbors/friends (1,945, 5.0%) |
| 5 | Employers in institutions for adolescents’ welfare (286, 0.7%) | Others (986, 2.6%) | Public officers in the field of social welfare (632, 1.6%) | Others (1,127, 2.9%) |
| 6 | Employers in institutions for social welfare (226, 0.7%) | Public officers in the field of social welfare (959, 2.5%) | Healthcare provider/medical professionals (363, 0.9%) | Child’s relatives (653, 1.7%) |
This table shows the first top 6 ranking of types of child abuse reporters who are mandatory and nonmandatory reporters, respectively, in 2 consecutive years.
Data from Child Abuse & Neglect Korea, 2019 and 2020. Ministry of Health and Welfare, Republic of Korea.
Fig. 2.
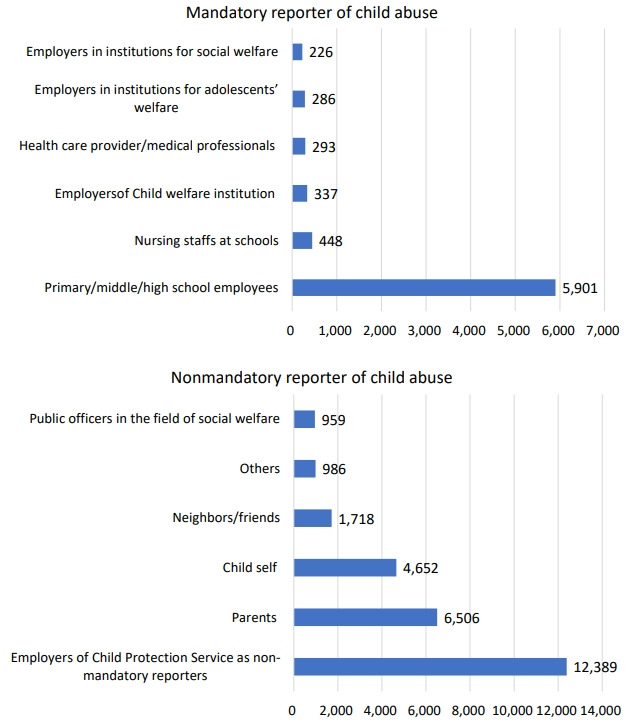
Mandatory and nonmandatory reporters of child abuse in 2019.
Fig. 3.
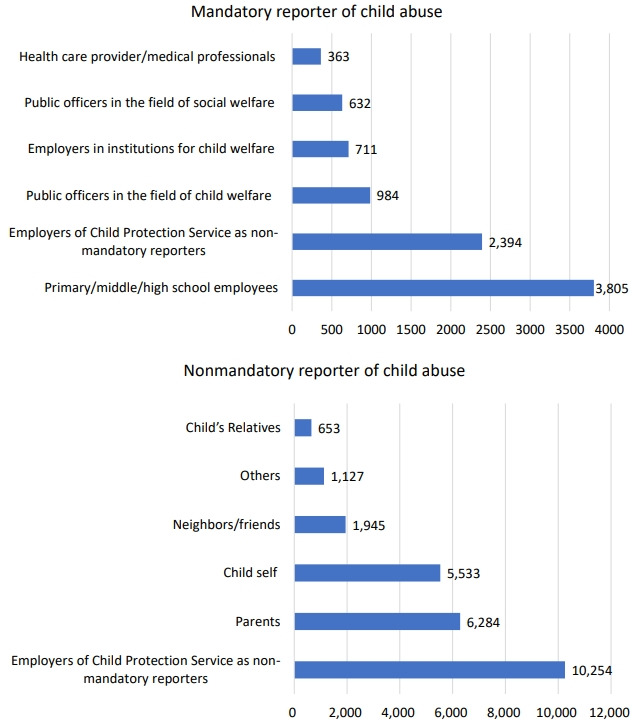
Mandatory and nonmandatory reporters of child abuse in 2020.
In addition, the pattern of child abuse in COVID-19 pandemic differs from that of pre-COVID-19 era. In the COVID-19 pandemic, emotional/psychological abuse and nonmedical neglect (any neglect that is not related with the child’s medical needs) are significantly increased [45]. Because of this changed pattern of abuse, it is seldom identified by surrounding people and might mitigate the increasing rate of case reporting of child abuse. Another difference in the COVID-19 pandemic is increased children’s self-reporting of abuse [41].
Management to improve mental health of children and adolescents
The COVID-19 pandemic created physical, social, emotional crises for many children and adolescents (Table 3). They are now more likely to experience depression and anxiety and are at greater risk of emotional disturbances during adolescence and adulthood, particularly those with less educated parents, fewer friends, and less physical activity [20]. Among these risk factors, physical activity can be modified. Rothon et al. [46] revealed that increasing physical activity by 1 hour per week was associated with an 8% decrease in the odds of depressive symptoms in adolescents. Also, a meta-analysis suggested that increased physical activity in youth is associated with decreased depressive symptoms [47]. Moreover, the number of obese children has increased due to reduced physical activity since the COVID-19 outbreak, which threatens their physical health [48]. Hence, in clinical settings, professionals who can directly assess a child’s physical health, such as a pediatrician, should educate parents and youths to increase their physical activity to improve their emotional and physical well-being and evaluate whether a child is performing adequate physical activity by referring to the 2018 Physical Activity Guidelines [49,50].
Table 3.
Studies of various COVID-19 pandemic effects on children and adolescents
| Study | Country | Study design | Age of participants | Major findings |
|---|---|---|---|---|
| Marques de Miranda et al., 2020 [3] | China, United states, Europe, South America | Nonsystematic review | 6–21 Years | Depression↑ |
| Anxiety↑ | ||||
| PTSD symptom↑ | ||||
| Meherali et al., 2021 [4] | West Africa, Australia, United States, Canada, Italy, China, India | Systematic review | 5–19 Years | Depression↑ |
| Anxiety↑ | ||||
| Frasquilho et al., 2020 [6] | China | Cross-sectional online questionnaire survey | 7–18 Years | Depression↑(smartphone/internet addiction is associated with depressive symptoms) |
| Anxiety↑ | ||||
| Xiang et al., 2020 [7] | China | Natural experimental longitudinal study | 6–17 Years | Physical activity↓ |
| Sedentary behavior ↑ | ||||
| Screen time↑ | ||||
| Park et al., 2022 [8] | South Korea | Cross-sectional online questionnaire survey | Parents with at least one child aged between 1– 12 years | Average time spent on childcare ↑ |
| Parental stress ↑ | ||||
| Children’s stress ↑ | ||||
| Child’s screen time↑ | ||||
| Berchtold et al., 2018 [9] | Switzerland | Retrospective study | 13–15 Years | Justification for setting a limit to 2 hours of screen time per day. |
| Bignardi et al., 2020 [11] | United Kingdom | Longitudinal study | 7.6–11.6 Years | Depression↑ |
| Cao et al., 2022 [26] | China | Cross-sectional online questionnaire survey | 11–20 Years | Rate of anxiety, depression and PTSD symptoms was 7.1%, 12.8% and 16.9%. |
| Adverse family relationship, lack of social support - most important predictor for mental health outcome. | ||||
| Liu et al., 2020 [31] | China | Cross-sectional study | Primary school student: 11–12 years | Incidence of somatization in primary school student is 2.39% (lower than college student). |
| College student: 19–23 years | Threat of life and health is significant risk factor for somatization. | |||
| Shangguan et al., 2021 [35] | China | Cross-sectional online questionnaire survey | Average age: 30.56± 10.78 | Resilience↓→somatization↑ |
| Perceived stress is mediator in the context of sex difference. | ||||
| Brown et al., 2020 [42] | Western United States | Cross-sectional online questionnaire survey | Parents with a child under the age of 18 years | Parental perceived stress↑→ child abuse potential ↑ |
| Rothon et al., 2010 [46] | United Kingdom | Prospective cohort study | 11–14 Years | Physical activity↑→ Depressive symptoms↓ |
| Kang et al., 2021 [48] | South Korea | retrospective cohort study | 4–14 Years | Childhood obesity↑ |
| Vitamin D deficiency↑ |
PTSD, posttraumatic stress disorder.
Pediatricians should carefully pay attention to the burden of childcare and social and financial issues of caregivers and evaluate their mental health state using the Korean version of the Patient Health Questionnaire-9, a short and validated self-reported screening tool for major depressive disorder with a sensitivity of 86.5% and specificity of 52.9% [51]. If the total score exceeds 10, a pediatrician should actively connect them with mental health professionals to ensure proper treatment for their depression. This ultimately promotes the mental health of their children and adolescents and helps decrease their screen time by decreasing the subjective parental burden at home. Likewise, pediatricians should assess their psychosocial problems, including behavioral and emotional problems, using the Korean version of the Pediatric Symptom Checklist, a simple and useful screening tool for children 7–18 years of age. If the total score exceeds 14 (sensitivity, 91.8%; specificity, 89.9%) [52], pediatricians should refer them to child psychiatrists.
In the COVID-19 pandemic, social isolation and school closures prevent the proper surveillance of youth by others. Therefore, child abuse cases might be underdetected and occur secretly behind closed doors. Moreover, the pattern of child abuse in the COVID-19 pandemic mainly involves emotional/psychological and nonmedical neglect. Primary physicians who can directly evaluate children and adolescents, such as pediatricians, are among the few important person who can be aware of childhood abuse. Hence, pediatricians must understand the characteristics and aspects of child abuse during the COVID-19 pandemic and aim to identify signs of child abuse, thereby functioning as a professional guardian [53].
Moreover, during the COVID-19 pandemic, children and adolescents feel threats to their lives and health or concern about being infected or passing viruses to others, which can cause somatization. Thus, providing accurate information, prevention guidelines, and mental health referrals is very important to preventing somatization in children and adolescents. Together, when children and adolescents finally return to school after any period of lockdown, it is important to remember that they already have experienced much adversity, which may result in PTSD. Thus, physicians, teachers, and parents should be told that they definitely need more time to adjust than usual and helped in many directions. Previous research suggested a cooperative model to overcome the COVID-19 pandemic [54]. This model suggested that psychological service should be provided to the social, school, and family systems; this approach is important to solving the psychological problems of children and adolescents. Since the physical health of children and adolescents is reciprocal and inseparable from their mental health, pediatricians should routinely evaluate the emotional state of children and adolescents and help at-risk children obtain proper attention and help from mental health professionals.
Conclusion
The COVID-19 pandemic enormously changed the daily lives of humankind by restricting social contacts and increasing depression, anxiety, and somatization. It also increased the screen time of children and adolescents. All of these factors jeopardize youth since they are still making crucial developmental steps and are vulnerable to adversity. This is a direct and negative effect of COVID-19 pandemic, but indirect effects also play a role, including increased parenting burden, parental unemployment, financial struggles, less supervision, more time alone, more familial conflicts, and a higher risk of child abuse. Therefore, primary physicians should pay more attention to these issues and assess their patients’ mental and physical health. In the continuing COVID-19 pandemic, pediatricians are becoming more important and function as professional guardians. More research should be done to promote an evidence-based approach and government policy should help the family, school, and social systems cooperate to protect the mental health of children and adolescents.
Key message
· The coronavirus disease 2019 (COVID-19) pandemic has required preventive measures like self-quarantine, school closures, and lockdown, which ultimately make youth directly and indirectly vulnerable to depression, anxiety, posttraumatic stress disorder, and somatization.
· Child abuse is more common in the COVID-19 era than previously.
· Pediatricians should carefully examine parental and child mental health to directly and indirectly aid their physical and mental health.
Footnotes
Conflicts of interest
No potential conflicts of interest relevant to this article was reported.
References
- 1.Cauchemez S, Van Kerkhove MD, Archer BN, Cetron M, Cowling BJ, Grove P, et al. School closures during the 2009 influenza pandemic: national and local experiences. BMC Infect Dis. 2014;14:207. doi: 10.1186/1471-2334-14-207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kim J, Ashihara K. National disaster management system: COVID-19 case in Korea. Int J Environ Res Public Health. 2020;17:6691. doi: 10.3390/ijerph17186691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Marques de Miranda D, da Silva Athanasio B, Sena Oliveira AC, SimoesE-Silva AC. How is COVID-19 pandemic impacting mental health of children and adolescents? Int J Disaster Risk Reduct. 2020;51:101845. doi: 10.1016/j.ijdrr.2020.101845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Meherali S, Punjani N, Louie-Poon S, Abdul Rahim K, Das JK, Salam RA, et al. Mental health of children and adolescents amidst COVID-19 and past pandemics: a rapid systematic review. Int J Environ Res Public Health. 2021;18:3432. doi: 10.3390/ijerph18073432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Duan L, Shao X, Wang Y, Huang Y, Miao J, Yang X, et al. An investigation of mental health status of children and adolescents in china during the outbreak of COVID-19. J Affect Disord. 2020;275:112–8. doi: 10.1016/j.jad.2020.06.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Frasquilho D, de Matos MG, Marques A, Neville FG, Gaspar T, Caldas-de-Almeida JM. Unemployment, parental distress and youth emotional well-being: the moderation roles of parent-youth relationship and financial deprivation. Child Psychiatry Hum Dev. 2016;47:751–8. doi: 10.1007/s10578-015-0610-7. [DOI] [PubMed] [Google Scholar]
- 7.Xiang M, Zhang Z, Kuwahara K. Impact of COVID-19 pandemic on children and adolescents' lifestyle behavior larger than expected. Prog Cardiovasc Dis. 2020;63:531–2. doi: 10.1016/j.pcad.2020.04.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Park JH, Park JY, Jin KS. What did COVID-19 Change? The impact of COVID-19 on Korean parents' and children's daily lives and stress. Child Psychiatry Hum Dev. 2022;53:172–82. doi: 10.1007/s10578-021-01262-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Berchtold A, Akre C, Barrense-Dias Y, Zimmermann G, Surís JC. Daily internet time: towards an evidence-based recommendation? Eur J Public Health. 2018;28:647–51. doi: 10.1093/eurpub/cky054. [DOI] [PubMed] [Google Scholar]
- 10.Courtney D, Watson P, Battaglia M, Mulsant BH, Szatmari P. COVID-19 impacts on child and youth anxiety and depression: challenges and opportunities. Can J Psychiatry. 2020;65:688–91. doi: 10.1177/0706743720935646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bignardi G, Dalmaijer ES, Anwyl-Irvine AL, Smith TA, Siugzdaite R, Uh S, et al. Longitudinal increases in childhood depression symptoms during the COVID-19 lockdown. Arch Dis Child. 2020;106:791. doi: 10.1136/archdischild-2020-320372. –7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Seoul (Korea): National Information Society Agency; 2015. Survey on internet overdependence [internet] [cited 2021 Nov 29]. Available from: http://www.nia.or.kr/ [Google Scholar]
- 13.Lissak G. Adverse physiological and psychological effects of screen time on children and adolescents: Literature review and case study. Environ Res. 2018;164:149–57. doi: 10.1016/j.envres.2018.01.015. [DOI] [PubMed] [Google Scholar]
- 14.Moon JH. Health effects of electromagnetic fields on children. Clin Exp Pediatr. 2020;63:422–8. doi: 10.3345/cep.2019.01494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Thoma VK, Schulz-Zhecheva Y, Oser C, Fleischhaker C, Biscaldi M, Klein C. Media use, sleep quality, and ADHD symptoms in a community sample and a sample of ADHD patients aged 8 to 18 years. J Atten Disord. 2020;24:576–89. doi: 10.1177/1087054718802014. [DOI] [PubMed] [Google Scholar]
- 16.Nikkelen SW, Valkenburg PM, Huizinga M, Bushman BJ. Media use and ADHD-related behaviors in children and adolescents: a meta-analysis. Dev Psychol. 2014;50:2228–41. doi: 10.1037/a0037318. [DOI] [PubMed] [Google Scholar]
- 17.Choi HJ, Kim HK. Effects of COVID-19 stress on children’s emotion and academic development. J Welf Counsel Educ. 2021;10:83–105. [Google Scholar]
- 18.Meade J. Mental health effects of the COVID-19 pandemic on children and adolescents: a review of the current research. Pediatr Clin North Am. 2021;68:945–59. doi: 10.1016/j.pcl.2021.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Xie X, Xue Q, Zhou Y, Zhu K, Liu Q, Zhang J, et al. Mental health status among children in home confinement during the coronavirus disease 2019 outbreak in Hubei Province, China. JAMA Pediatr. 2020;174:898–900. doi: 10.1001/jamapediatrics.2020.1619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Chen F, Zheng D, Liu J, Gong Y, Guan Z, Lou D. Depression and anxiety among adolescents during COVID-19: a cross-sectional study. Brain Behav Immun. 2020;88:36–8. doi: 10.1016/j.bbi.2020.05.061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Zhou SJ, Zhang LG, Wang LL, Guo ZC, Wang JQ, Chen JC, et al. Prevalence and socio-demographic correlates of psychological health problems in Chinese adolescents during the outbreak of COVID-19. Eur Child Adolesc Psychiatry. 2020;29:749–58. doi: 10.1007/s00787-020-01541-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.American Psychiatric Association . Diagnostic and statistical manual of mental disorders. 5th ed. Washington, DC: American Psychiatric Association; 2013. [Google Scholar]
- 23.Hickerson WL. COVID-19 disaster response assessment. J Burn Care Res. 2020;41:918. doi: 10.1093/jbcr/iraa068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Yuan K, Gong YM, Liu L, Sun YK, Tian SS, Wang YJ, et al. Prevalence of posttraumatic stress disorder after infectious disease pandemics in the twenty-first century, including COVID-19: a meta-analysis and systematic review. Mol Psychiatry. 2021;26:4982–98. doi: 10.1038/s41380-021-01036-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Carmassi C, Foghi C, Dell'Oste V, Cordone A, Bertelloni CA, Bui E, et al. PTSD symptoms in healthcare workers facing the three coronavirus outbreaks: what can we expect after the COVID-19 pandemic. Psychiatry Res. 2020;292:113312. doi: 10.1016/j.psychres.2020.113312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Cao C, Wang L, Fang R, Liu P, Bi Y, Luo S, et al. Anxiety, depression, and PTSD symptoms among high school students in china in response to the COVID-19 pandemic and lockdown. J Affect Disord. 2022;296:126–9. doi: 10.1016/j.jad.2021.09.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Vassend O, Roysamb E, Nielsen CS, Czajkowski NO. Musculoskeletal complaints, anxiety-depression symptoms, and neuroticism: a study of middle-aged twins. Health Psychol. 2017;36:729–39. doi: 10.1037/hea0000484. [DOI] [PubMed] [Google Scholar]
- 28.Russo J, Katon W, Sullivan M, Clark M, Buchwald D. Severity of somatization and its relationship to psychiatric disorders and personality. Psychosomatics. 1994;35:546–56. doi: 10.1016/S0033-3182(94)71723-0. [DOI] [PubMed] [Google Scholar]
- 29.Portegijs PJ, Jeuken FM, van der Horst FG, Kraan HF, Knottnerus JA. A troubled youth: relations with somatization, depression and anxiety in adulthood. Fam Pract. 1996;13:1–11. doi: 10.1093/fampra/13.1.1. [DOI] [PubMed] [Google Scholar]
- 30.Masi G, Favilla L, Millepiedi S, Mucci M. Somatic symptoms in children and adolescents referred for emotional and behavioral disorders. Psychiatry. 2000;63:140–9. doi: 10.1080/00332747.2000.11024905. [DOI] [PubMed] [Google Scholar]
- 31.Liu S, Liu Y, Liu Y. Somatic symptoms and concern regarding COVID-19 among Chinese college and primary school students: a cross-sectional survey. Psychiatry Res. 2020;289:113070. doi: 10.1016/j.psychres.2020.113070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Jowett S, Shevlin M, Hyland P, Karatzias T. Posttraumatic stress disorder and persistent somatic symptoms during the COVID-19 pandemic: the role of sense of threat. Psychosom Med. 2021;83:338–44. doi: 10.1097/PSY.0000000000000890. [DOI] [PubMed] [Google Scholar]
- 33.Sağaltıcı E, Sönmez O, Karcı E, Şahin ŞK, Ertürk A. Somatic distress, mental health and psychological resilience among cancer patients during the pandemic. Int J Res Counsel Educ. 2021;5:116–27. [Google Scholar]
- 34.Southwick SM, Charney DS. The science of resilience: implications for the prevention and treatment of depression. Science. 2012;338:79–82. doi: 10.1126/science.1222942. [DOI] [PubMed] [Google Scholar]
- 35.Shangguan F, Zhou C, Qian W, Zhang C, Liu Z, Zhang XY. A conditional process model to explain somatization during coronavirus disease 2019 epidemic: the interaction among resilience, perceived stress, and sex. Front Psychol. 2021;12:633433. doi: 10.3389/fpsyg.2021.633433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Franck E, Haegdorens F, Goossens E, van Gils Y, Portzky M, Somville F, et al. The role of coping behavior in healthcare workers' distress and somatization during the COVID-19 pandemic. Front Psychol. 2021;12:684618. doi: 10.3389/fpsyg.2021.684618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Osofsky HJ, Weems CF, Graham RA, Osofsky JD, Hansel TC, King LS. Perceptions of resilience and physical health symptom improvement following post disaster integrated health services. Disaster Med Public Health Prep. 2019;13:223–9. doi: 10.1017/dmp.2018.35. [DOI] [PubMed] [Google Scholar]
- 38.Malarkey WB, David P, Gouin JP, Edwards MC, Klatt M, Zautra AJ. REMAP-a resilience resources measure for prediction and management of somatic symptoms. Int J Behav Med. 2016;23:738–45. doi: 10.1007/s12529-016-9559-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Rosenthal CM, Thompson LA. Child abuse awareness month during the coronavirus disease 2019 pandemic. JAMA Pediatr. 2020;174:812. doi: 10.1001/jamapediatrics.2020.1459. [DOI] [PubMed] [Google Scholar]
- 40.Seddighi H, Salmani I, Javadi MH, Seddighi S. Child abuse in natural disasters and conflicts: a systematic review. Trauma Violence Abuse. 2021;22:176–85. doi: 10.1177/1524838019835973. [DOI] [PubMed] [Google Scholar]
- 41.Ministry of Health and Welfare . Sejong (Korea): Ministry of Health and Welfare; 2020. Child abuse & neglect Korea 2020 [internet] [cited 2021 Nov 29]. Available from: http://www.mohw.go.kr/ [Google Scholar]
- 42.Brown SM, Doom JR, Lechuga-Peña S, Watamura SE, Koppels T. Stress and parenting during the global COVID-19 pandemic. Child Abuse Negl. 2020;110(Pt 2):104699. doi: 10.1016/j.chiabu.2020.104699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Lawson M, Piel MH, Simon M. Child maltreatment during the COVID-19 pandemic: consequences of parental job loss on psychological and physical abuse towards children. Child Abuse Negl. 2020;110(Pt 2):104709. doi: 10.1016/j.chiabu.2020.104709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Ministry of Health and Welfare . Sejong (Korea): Ministry of Health and Welfare; 2019. Child abuse & neglect Korea 2019 [internet] [cited 2021 Nov 29]. Available from: http://www.mohw.go.kr/ [Google Scholar]
- 45.Sharma S, Wong D, Schomberg J, Knudsen-Robbins C, Gibbs D, Berkowitz C, et al. COVID-19: differences in sentinel injury and child abuse reporting during a pandemic. Child Abuse Negl. 2021;116(Pt 2):104990. doi: 10.1016/j.chiabu.2021.104990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Rothon C, Edwards P, Bhui K, Viner RM, Taylor S, Stansfeld SA. Physical activity and depressive symptoms in adolescents: a prospective study. BMC Med. 2010;8:32. doi: 10.1186/1741-7015-8-32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Korczak DJ, Madigan S, Colasanto M. Children's physical activity and depression: a meta-analysis. Pediatrics. 2017;139:e20162266. doi: 10.1542/peds.2016-2266. [DOI] [PubMed] [Google Scholar]
- 48.Kang HM, Jeong DC, Suh BK, Ahn MB. The impact of the coronavirus disease-2019 pandemic on childhood obesity and Vitamin D status. J Korean Med Sci. 2021;36:e21. doi: 10.3346/jkms.2021.36.e21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.U.S. Department of Health and Human Services . Physical activity guidelines for Americans. 2nd ed. Washington, DC: U.S. Department of Health and Human Services; 2018. [Google Scholar]
- 50.Lobelo F, Muth ND, Hanson S, Nemeth BA, Council on Sports Medicine and Fitness. Section on Obesity Physical activity assessment and counseling in pediatric clinical settings. Pediatrics. 2020;145:e20193992. doi: 10.1542/peds.2019-3992. [DOI] [PubMed] [Google Scholar]
- 51.Lee SH, Huh YJ, Kim JH, Han CS. Finding optimal cut off points of the Korean version of the Patient Health Questionnaire-9 (PHQ-9) for screening depressive disorders. Mood Emot. 2014;12:32–6. [Google Scholar]
- 52.Han DH, Woo J, Jeong JH, Hwang S, Chung US. The Korean version of the Pediatric Symptom Checklist: psychometric properties in korean school-aged children. J Korean Med Sci. 2015;30:1167–74. doi: 10.3346/jkms.2015.30.8.1167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Chung US. It is time for doctors to start seeing the signs and hearing the cries of abused children as professional guardians. J Korean Med Sci. 2015;30:351–2. doi: 10.3346/jkms.2015.30.4.351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Zhou X. Managing psychological distress in children and adolescents following the COVID-19 epidemic: a cooperative approach. Psychol Trauma. 2020;12(S1):S76–8. doi: 10.1037/tra0000754. [DOI] [PubMed] [Google Scholar]