Abstract
Introduction
Kinematic alignment (KA) has increased in popularity in recent years, becoming a viable alternative to MA with encouraging short- and mid-term follow-up results. Recently, the concept of restricted kinematic alignment (rKA) has been developed to restore native knee kinematics better, avoiding failure of coronal alignment. This systematic review aims to examine whether rKA improves outcome scores (PROMs) compared with MA and to evaluate the radiographic analysis of the lower limb alignment and the causes of complications and reoperations with the rKA approach.
Methods
A systematic literature search was conducted following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines on the Pubmed/Medline, Scopus, Cochrane Library, and Embase databases. The following key terms were used: “restricted kinematic alignment, rKA, kinematic alignment, primary total knee arthroplasty, primary total knee replacement, TKA rKA, and TKR rKA.” The initial screening identified 328 studies. Each eligible article was evaluated according to the inclusion criteria: studies with levels of evidence (LoE) 1 to 4, written in English, published through May 2022, and involving human subjects. Criteria from the Methodological Index for Non-Randomized Studies (MINORS) were used to assess the methodological quality of the articles.
Results
Six clinical studies were included in this systematic review. The study was registered in the International Prospective Registry of Systematic Reviews (PROSPERO). A total of 574 knees were included. After excluding patients due to loss of follow-up or missing data, 475 knees were analyzed. The following rKA-related data were evaluated: patient-reported outcome scores (PROMs), radiographic analysis of the lower limb alignment, and causes of complications and reoperations.
Conclusions
The rKA is an improved concept for restoring native knee kinematics, avoiding excessive coronal varus/valgus alignment. It provides equivalent or slightly better PROMs than MA without increasing the risk of short-middle-term implant failure. Clinical studies with extended follow-up are needed to confirm this trend.
Keywords: Knee, Arthroplasty, Mechanical alignment, Kinematic alignment, Restricted kinematic alignment, KA
1. Introduction
For several decades, mechanical alignment (MA) was considered the gold standard technique in total knee arthroplasty (TKA).1 The MA aims to reproduce a neutral alignment of the lower limb with a hip-knee-ankle angle (HKA) of 180° ±1.5° through orthogonal cuts on the femur and tibia, followed by soft tissue release to reach the desired gap in flexion and extension. The goal is to balance load distribution between the two knee compartments, medial and lateral, to reduce prosthetic components' wear and risk of loosening.2 Despite good overall results with more than 90% implants survival after 15 years, nearly 20% of patients remained unsatisfied after surgical treatment even if a correct prosthesis positioning was obtained.3,4 Within the last 20 years, several studies undermined the cornerstones on which knee replacement was based in previous decades. Hirschmann et al.5 described different functional knee phenotypes and underlined that neutral mechanical alignment exists preoperatively only in about 5–6% of knees. Furthermore, recent clinical and biomechanical studies demonstrated that TKA implant survivorship was not precluded in case of component alignment greater than 3° from the neutral axis.6,7 Based on these postulates, the concept of kinematic alignment (KA), theorized by Howell in the early 2010s, spread considerably in recent years, becoming a viable alternative to MA with encouraging results in short-middle-term follow-up.8, 9, 10, 11 KA should be considered as a pure “resurfacing technique” in which the natural alignment of the lower limb is reproduced, and ligament release should not be performed. First, femur cuts are made at the thickness of the implants to correct wear due to cartilage loss without changing the degree of deformity.8,9 Subsequently, a tibial cut is made to obtain a rectangular space in the extension gap and a trapezoidal one in the flexion gap with a mild external laxity in the varus knee or a mild internal laxity in the valgus knee. Both in extension and flexion, all gap corrections should be performed on the tibia.8,9
Recently, Vendittoli et al. theorized the concept of “restricted kinematic alignment” (rKA) to restore the native knee kinematics, avoiding excessive varus/valgus coronal alignment.12 The rKA is based on five principles: (1) postoperative HKA should be maintained within ± 3°; (2) lateral distal femoral angle (LDFA) and medial proximal tibial angle (MPTA) may be limited to a maximum of 5°; (3) collateral ligament balance should be restored without the gap balancing technique; (4) preservation of native femoral anatomy is recommended over tibial one because of its importance in knee biomechanics; (5) resurface resection, with a thickness equal to the width of the implant, should be performed on the unworn side; cut adjustment may be sought at the worn side.12
This systematic review aims to provide a balanced view of primary TKA performed following rKA principles.12 The following data were evaluated: (1) patient-reported outcome scores (PROMs); (2) lower limb radiographic analysis; (3) causes of complications and reoperation. Finally, in the case of comparative studies, an analysis of the outcome between rKA and MA was reported.
2. Materials and methods
2.1. Research question
The research was conducted in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines.13, 14, 15 A systematic literature review was performed independently by four authors (GC, SR, FB, FG) to search studies investigating the radiographic and clinical outcomes of patients undergoing primary TKA due to end-stage knee osteoarthritis according to the rKA alignment concept.12 In case of discordance a fifth author (LS) was consulted.
2.2. Search strategy
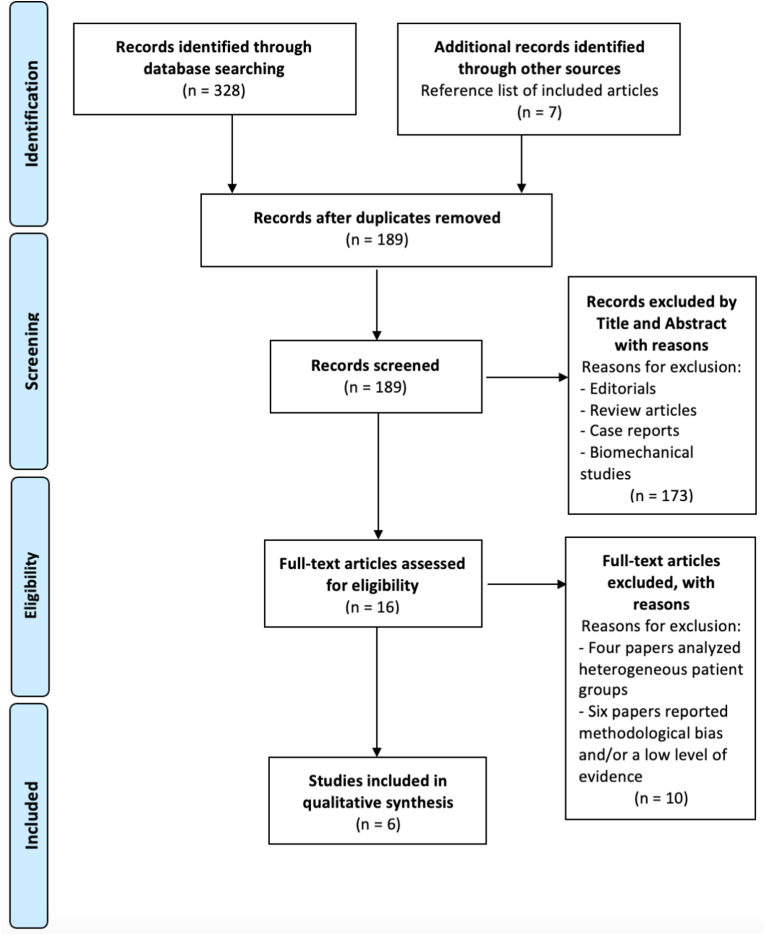
Literature research in several database (Pubmed/Medline, Scopus, Cochrane Library and Embase) was performed with the following key terms in association with Boolean Operators “AND”, “OR”: restricted kinematic alignment, rKA, kinematic alignment, primary total knee arthroplasty, primary total knee replacement, rKA TKA, and rKA TKR. Research was limited to articles published up to May 2022. A total of 328 studies were identified through the literature research. After duplicate studies were excluded, 189 studies remained, which were screened by title and abstract. After record screened, 16 studies were assessed for full text evaluation and based on the inclusion and exclusion criteria, six clinical studies16, 17, 18, 19, 20, 21 investigating radiographic and clinical outcomes of patients undergoing primary TKA due to end-stage knee osteoarthritis according to rKA alignment were included in the systematic review. A cross-check was performed in search of additional studies to be included in the analysis. The PRISMA flow chart for study selection is shown in Fig. 1.
Fig. 1.
PRISMA (Preferred Reporting Items for Systematic review and Meta-Analysis) flow diagram of articles screened, selected, and included in the systematic review and meta-analysis.
2.3. Inclusion and exclusion criteria
The inclusion criteria were original studies published in English language with Oxford Centre for Evidence-Based Medicine 2011 Levels of Evidence (LoE) 1 to 4,22 in which rKA was used in primary TKA with at least thirty patients and almost one year follow-up. No limits were set in regard of time of publications. We excluded review articles, surgical technique reports, book chapters, editorials, and abstracts from scientific meeting. Studies regarding human subjects were exclusively considered.
2.4. Quality assessment
Each included study was analyzed according to the Levels of Evidence (LoE) of the Oxford Centre for Evidence-Based Medicine 2011.22 MINORS criteria23 were used to assess the methodological quality of the articles. Regarding statistical analysis, categorical variables were reported as percentages (%), while continuous variables were represented as mean values. This systematic review was registered on the International Prospective Register of Systematic Reviews (PROSPERO), CRD42022335016 in June 2022.24
2.5. Data extraction and collection
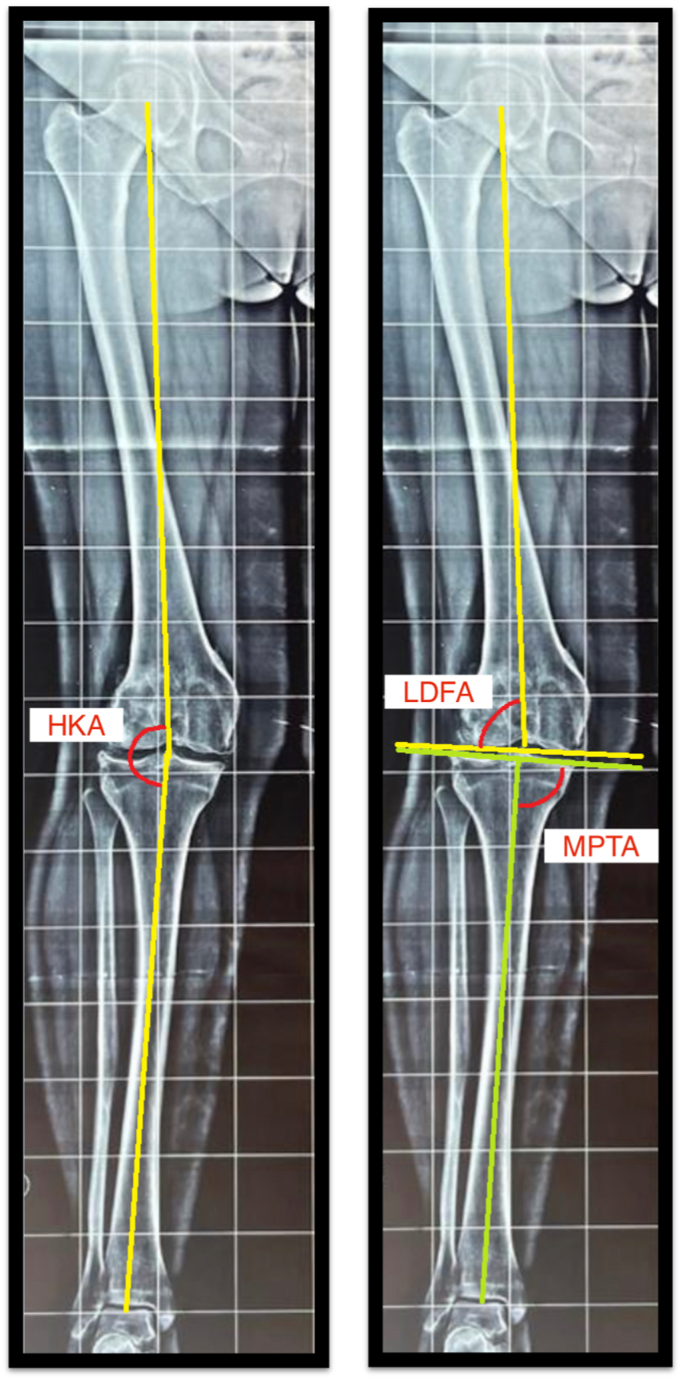
During the analysis of the included studies16, 17, 18, 19, 20, 21 the following study characteristics were inserted in a template: full title, first author, year of publication, study design, number of patients, number of knee, patients excluded due to missing data and/or lost to follow-up, surgical procedure (computer navigated, robotic assisted), implant design, average age, length of follow-up, complications, reoperations, radiographic data, and PROMs. For radiographic analysis we recorded the HKA, defined as the angle between the mechanical axis of the femur and the mechanical axis of the tibia, the LDFA, defined as the angle between the distal femur axis on the coronal plane and the mechanical axis of the femur, and the MPTA defined as the medial angle between the tangent to the tibial plateau line and the mechanical axis of the tibia line (Fig. 2).
Fig. 2.
Radiographs showing the measurements of hip-knee-ankle angle (HKA), lateral distal femoral angle (LDFA) and medial proximal tibial angle (MPTA).
3. Results
3.1. Included studies and demographic data
After applying inclusion and exclusion criteria, a total of six studies were included in the final analysis.16, 17, 18, 19, 20, 21 The number of knees initially included was 574. After excluding patients due to loss of follow-up or missing data, 475 patients were analyzed in this systematic review. The average age was 68.2 years (range, 67.4 to 70), and there were 314 women (66.1%) with an average BMI of 31.1 kg/m2 (range, 29.2 to 32.2). The average follow-up was 2.3 years (range, 1 to 4.1). Studies descriptions and demographic data are listed in Table 1. The average MINORS score for non-comparative studies was 11.1 (range, 9–14), while the average MINORS score for comparative studies was 20.8 (range, 19–23). Due to the average low quality of the included studies, we decided not to perform a meta-analysis.
Table 1.
Main demographic characteristics of patients collected in clinical studies included in the systematic review.
| Author and publication year | Study design | N° of knees, initial cohort/final cohort | TKA Design | Surgical technique | Age | Gender female | BMI | Follow-up |
|---|---|---|---|---|---|---|---|---|
| N°/N° | y.o., Mean ± SD/(Range)* | (%) | Kg/m2 | y.o., Mean ± SD/(Range)* | ||||
| Winnock de Grave et al. (21) | Retrospective, comparative (MA vs rKA) | 50/40 | Triathlon, CR (Stryker) | Robotic assisted | 69.9 ± 8.3 | 25 (60%) | 29.2±4.8 | 1 |
| Sappey-Mariner et al. (20) | Retrospective, comparative (MA vs rKA) | 50/50 | GMK, PS (Medacta) | Non robotic or navigation assisted | 70 ± 8.5 | 58 (58%) | 29.7±5.2 | 3.6 (3.1–3.9) |
| Abhari et al. (19) | Restrospective, comparative (MA vs rKA) | 121/115 | Triathlon, CR (Stryker) | Robotic assisted | 68 (43–85) | 52 (45.2%) | 32 (21–51) | 1.5 (1–2.2) |
| MacDessi et al. (18) | Prospective, comparative (MA vs rKA) | 70/70 | Legion, PS (S&N) | Computer navigation | 67.5 (36–89) | 40 (63.5%) | 30.2 | 1 |
| Laforest et al. (17) | Retrospective, non-comparative (rKA) | 133/100 | Triathlon (Stryker) | Computer navigation | 67.4 ± 10 | 76 (76%) | 32.2±6.3 | 4.1 (2.7–5) |
| Hutt et al. (16) | Retrospective, non-comparative (rKA) | 100/100 | Triathlon (Stryker) | Computer navigation | 68 ± 11 | 63 (63%) | 31±6 | 2.4 ± 0.8 |
N°: numbers of knees, TKA: Total Knee Arthoplasty, BMI: Body Max Index, y.o: years old, SD: Standard Deviation, %: percentage, KG/m2: kilogram/meter2, MA: mechanical alignment, rKA: restricted kinematic alignment, CR: cruciate-retaining, GMK: Global Medacta Knee, PS: Posterior-stabilized, S&N: Smith & Nephew, *: if SD was not reported, values range were recorded.
3.2. Clinical scores
Knee society score (KSS): two studies reported the outcome based on the KSS score.19,20 Abhari et al.19 reported an increase in both subscales of KSS. For “clinical KSS,” they reported a statistically significant increase (p < 0.001) from an average of 41.9±9.4 to an average of 93±9.4. For “function KSS,” they reported a statistically significant increase from an average of 51±10 preoperatively to an average of 85±16 postoperatively. Sappey-Mariner et al.,20 reported an average increase of 52±30.4 points, increasing statistically (p < 0.001) reaching an average of 173.2±19.6.
WOMAC score: three studies reported the outcome based on WOMAC Score.16,17,19 Abhari et al.19 reported an increase in the WOMAC score from an average of 43±15 preoperatively to an average of 90±11 postoperatively. LaForest et al.17 reported an average postoperative WOMAC score of 20.1±21. Similarly, Hutt et al.16 reported a better postoperative WOMAC score in their case series. They reported values from an average of 49.4± 12.8 preoperatively to an average of 24.7± 16.5 postoperatively.
Knee Injury and Osteoarthritis Outcome Score (KOOS) score: three studies reported the outcome based on the KOOS Score.16,17,19 Abhari et al.19 reported an increase in KOOS score from 46±1.1 preoperatively to 86±1.5 postoperatively. LaForest et al.17 reported the postoperative KOOS score only, with an average of 71.5±19.8. Lastly, Hutt et al.16 reported a statistically significant (p < 0.001) increase for each subscale of the KOOS score. Specifically, the values for pain increased from an average of 38.5±17 to 74.6±18.8, for symptoms from 39.4±12.7 to 54.8±26.7, for activities of daily living from 41.2±18.7 to 76±19.3, and finally for sport from 14.2±22.7 to 46.4±30.6.
Forgotten Joint Score (FJS): Three studies evaluated the joint function after rKA TKA using the FJS.17, 18, 19 Abhari et al.19 reported an average FJS of 72±27. MacDessi et al.18 reported a statistically significant increase from an average of 15.9±13.2 preoperatively to an average of 63.9±29.6. Lastly, LaForest et al.17 reported an average postoperative of 65.9±29.6.
Other Scores: One study reported the OKS,21 with a statistically significant increase from an average of 28.3 preoperatively to an average of 44.8±4.4 (p < 0.001). The authors themselves reported the EQ-5D-5L questionnaire to assess the quality of life. The reported values increased from an average of 75.3 preoperatively to an average of 84.1 postoperatively.21
Patient satisfaction: Two studies reported the rate of satisfaction after surgery with an rKA TKA.19, 20, 21 DeGrave et al. reported satisfaction in 98% of patients.21 Abhari et al.19 reported postoperative satisfaction in 92% of patients.
3.3. Lower limb alignment
The average values of the several radiographic measurements regarding the lower limb alignment of the included studies16, 17, 18, 19, 20, 21 were calculated and recorded. The average preoperative HKA was 176.6° (range, 176°–178.6°), while the average postoperative HKA angle was 178.6° (178°–179.5°). The average preoperative LDFA was 90.6° (range, 88°–92.1°), while the average postoperative LDFA was 91.3° (range, 88.8°–92.3°). The average preoperative MPTA was 87° (range, 86.7°–87.8°), while the average postoperative MPTA was 87.7° (range, 87.1°–90°). Detailed information about the radiographic analyses is listed in Table 2.
Table 2.
Radiographic analysis of lower limb alignment before and after TKA rKA implantation.
| Author and publication year | HKA (°) |
LDFA (°) |
MPTA (°) |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Preoperative |
Postoperative |
Preoperative |
Postoperative |
Preoperative |
Postoperative |
|||||||
| Value | SD/Range | Value | SD/Range | Value | SD/Range | Value | SD/Range | Value | SD/Range | Value | SD/Range | |
| Winnock de Grave et al. (21) | 176.3 | 4.3 | 178.3 | 2.1 | 88 | 1.4 | 88.8 | 1.4 | 86.7 | 1.3 | 87.1 | 1.4 |
| Sappey-Mariner et al. (20) | 176 | 165/195 | 178.6 | 171/178 | 91.3 | 2.4 | 91.3 | 2.4 | 87 | 3 | 88.6 | 2.6 |
| Abhari et al. (19) | 176 | N/A | 178 | N/A | N/A | N/A | N/A | N/A | N/A | N/A | 87 | N/A |
| MacDessi et al. (18) | 177.2 | 161/191 | 177.8 | 173/192 | 87.5 | 3 | 90.6 | 1.5 | 87.8 | 1.8 | 90 | 1.9 |
| Laforest et al. (17) | 178.6 | 4.1 | 179.1 | 1.8 | 91.8 | 2.7 | 92.3 | 1.8 | 86.7 | 2.6 | 86.8 | 1.5 |
| Hutt et al. (16) | 175.4 | 5.9 | 179.5 | 2.3 | 92.1 | 2.5 | 91.8 | 2 | 87 | 3.2 | 87.6 | 2.2 |
| Average values | 176.6 | / | 178.6 | / | 90.6 | / | 91.3 | / | 87 | / | 87.7 | / |
HKA = Hip-Knee-Angle; LDFA = lateral distal femoral angle; MPTA = medial proximal tibial angle, N/A: not available. All value is expressed in ° (degree) with mean and SD. If SD was not reported, values range were recorded.
3.4. Complications and reoperations
The overall complication rate was 3.4% (16 knees). Three studies16,18,21 reported no postoperative complications. The follow-up was limited to one year only in two of them.18,21 Sappery-Mariner et al.20 reported a higher complication rate. A reoperation was performed in eight cases (16%) at an average follow-up of 3.6 years. Abhari et al.19 and Laforest et al.17 reported a 4.3% and 3% reoperation rate, respectively.
Aseptic loosening of the tibial component was the most frequent cause of reoperation, with an incidence of 2.3% (11 knees), followed by pain related to tibial component mispositioning (0.4%) and delayed flexion deficit (0.4%). In one case, a revision due to a deep periprosthetic joint infection was reported (0.2%).
4. Discussion
The KA aims to restore the anatomy of the pre-arthritic knee without ligamentous release. Liu et al.,10 in their recent meta-analysis, analyzed that KA results in better functional outcomes than MA in short-to-medium-term follow-up. However, the KA in patients with extreme pathologic anatomies is highly debated. In these outlier patients, rKA may be the appropriate compromise because, on the one side, it provides good restoration of the patient's anatomy by avoiding significant ligamentous release compared to MA, and, on the other side, it excludes extreme prosthetic implant positioning, avoiding deleterious effects on TKA biomechanics and wear patterns.25
Restricted KA results reported in the literature are encouraging,12 but currently, only a few low-quality studies have provided early outcomes of this novel technique for lower limb alignment.16, 17, 18, 19, 20, 21
4.1. PROMs
The most important finding of this systematic review is the optimal PROMs of patients undergoing primary TKA according to the principles of rKA, with a statistically significant improvement between preoperative and postoperative PROMs in all studies analyzed.
Sappey-Marinier et al.20 and Abhari et al.19 reported a postoperative KSS score, sum of clinical and functional score, of 173.2 and 178, respectively, in line with the average KSS score of patients undergoing primary TKA with KA or MA.
Winnock de Grave et al.21 described a mean postoperative OKS score of 44.8, while LaForest et al.17 and Hutt et al.16 reported an average postoperative WOMAC score of 20.1 and 24.7, respectively.
Discordant results are described in comparative studies between rKA and MA. Winnock de Grave et al.21 reported significantly better postoperative OKS (p < 0.025) and patient satisfaction (p < 0.002) in patients with varus knees undergoing rKA compared with MA. Abhari et al.19 described a significantly better postoperative WOMAC, FJS, and KSS in patients treated with rKA and overall satisfaction of 96%, higher than the 80% satisfaction of patients undergoing MA TKAs. Conversely, Sappey-Marinier et al.20 and MacDessi et al.18 reported no statistically significant differences in postoperative PROMs between MA and rKA. Nevertheless, the mean postoperative PROMs reported in rKA are not inferior to the clinical results obtained with MA.
4.2. Lower limb postoperative alignment
The differences between preoperative and postoperative values in lower limb alignment are probably related to “restoring” degrees of varus caused by wear of the medial femoral-tibial joint cartilage.12
Hutt et al.16 performed a navigated TKA rKA to achieve more precise coronal plane cuts and planned alignment. In their postoperative analysis, the authors observed that 12 knees, three valgus and nine varus, exceeded the safe range of ± 3° in the coronal plane. Although one of the key principles of KA alignment is that no corrections should be made on the femoral side, Hutt et al. performed femoral cuts on 15 knees with an LDFA >5° preoperatively to keep the HKA in the desired range. In 20 knees, however, the authors performed correction on the tibial side because of an MPTA angle >5°.
LaForest et al.17 reported a change in HKA (from 4.9° preoperative varus to 1.9° postoperative varus), LDFA (from 91.8° preoperative to 92.2° postoperative), and MPTA (from 86.7° preoperative to 86.8° postoperative), reflecting cartilage restoration due to arthritic changes in the joint.
MacDessi et al.18 reported lower limb alignment within 3° in 94% of navigated TKA rKA, describing a postoperative LDFA in rKA with more valgus (89.2° SD 1.8) than in MA (90.6° SD 1.5°). Similar data on postoperative lower extremity alignment were also described by Sappey-Marinier et al.20 The authors also reported that the femoral component was slightly valgus in patients treated with rKA compared with MA (91.3°SD 2.4° and 89.8° SD 1.3°, respectively), and the tibial component was slightly more varus (88.6° SD 1.4° and 89.5° SD 0.9°, respectively).
Winnock de Grave et al.21 analyzed patients with varus and valgus knees before surgery, reporting the difference in lower limb alignment between these two categories of patients. The authors described that the net change in constitutional varus for HKA was less than that for constitutional valgus knee (3.8° SD 0.9 and 5.2° SD 1.4°, respectively).
4.3. Complications
The overall revision rate of rKA was 3.4% (16 TKAs, after an average follow-up period of 2.3 years). The revision rate aligns with data reported in MA TKAs and KA TKAs.9,26, 27, 28, 29 Three studies reported no complications.16,18,21 Sappey-Marinier et al.20 reported the highest complications rate, with eight TKAs (16%) revised at an average follow-up of 3.6 years, all due to tibial component loosening. The authors observed that the revision rate due to aseptic loosening as the endpoint was significantly higher in the rKA than in the MA group (84% versus 98%, p < 0.001). Sappey-Marinier et al. reported no statistically significant differences in lower limb alignment between patients managed with rKA alignment with and without tibial component loosening. Abhari et al.19 reported no statistically significant differences in revision rate between patients managed by rKA and MA. The authors revised three TKAs due to tibial component loosening within one year from primary TKA (4.3%). Laforest et al.17 performed TKA revisions (3%) in three cases: tibial component shift after a fall due to persistent pain, periprosthetic joint infection, and persistent pain secondary to flexion instability.
4.4. Limitations
Several limitations should be analyzed in this systematic review. First, this is a novel kinematic concept developed in 2016, and there are only a few studies with a small sample size and short follow-up period. Second, one of the main concerns ascribed to KA and rKA is the increased risk of aseptic loosening at mid-term and long-term follow-up that could not be evaluated in a short period as reported in the included studies (average follow-up 2.3 years). Third, different surgical protocols were used. In some cases, TKAs were performed with robotic assistance, while in others, with computer-assisted navigation. Fourth, different implants and fixation types that may play a key role in TKA survival were used in the studies. For instance, it has been demonstrated that new polyethylene insert designs could result in better knee kinematics, better clinical scores, and longer life of TKA.30, 31, 32, 33, 34 Lastly, there was no standardization in the PROMs used to evaluate patients (WOMAC, KOOS, and FJS were used in three studies, KSS in two studies, OKS and EQ-5D-5L in one study).
5. Conclusion
This systematic review highlighted that rKA provides equivalent or slightly improved PROMs reporting no increased risk of implant failure at a short follow-up period. More studies with a greater number of patients and a longer follow-up period need to be performed to confirm this tendency. Finally, considering low-quality studies included, randomized controlled trials may be useful to compare rKA outcomes with KA or MA.
Authors contribution
Risitano Salvatore: Conceptualization, Methodology. Cacciola Giorgio: Data curation, Writing- Original draft preparation. Sabatini Luigi: Data curation. Capella Marcello: Visualization, Investigation. Bosco Francesco: Software. Giustra Fortunato: Software, Validation. Masse' Alessandro: Supervision. Vaishya Raju: Supervision, Writing- Reviewing.
Funding
This research received no external funding.
Ethical standard
This article does not contain any studies with human participants or animals performed by any of the authors.
Informed consent
For this type of study formal consent is not required.
Data availability statement
Data is contained within the article.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Declaration of competing interest
The authors declare that they have no conflicts of interest.
Acknowledgement
None.
References
- 1.Rivière C., Iranpour F., Auvinet E., et al. Alignment options for total knee arthroplasty: a systematic review. Orthop Traumatol Surg Res. 2017;103(7):1047–1056. doi: 10.1016/j.otsr.2017.07.010. Nov. [DOI] [PubMed] [Google Scholar]
- 2.Hohman D.W., Jr., Nodzo S.R., Phillips M., Fitz W. The implications of mechanical alignment on soft tissue balancing in total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2015;23(12):3632–3636. doi: 10.1007/s00167-014-3262-4. Dec. [DOI] [PubMed] [Google Scholar]
- 3.Bourne R.B., Chesworth B.M., Davis A.M., Mahomed N.N., Charron K.D. Patient satisfaction after total knee arthroplasty: who is satisfied and who is not? Clin Orthop Relat Res. 2010;468(1):57–63. doi: 10.1007/s11999-009-1119-9. Jan. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gunaratne R., Pratt D.N., Banda J., Fick D.P., Khan R.J.K., Robertson B.W. Patient dissatisfaction following total knee arthroplasty: a systematic review of the literature. J Arthroplasty. 2017;32(12):3854–3860. doi: 10.1016/j.arth.2017.07.021. Dec. [DOI] [PubMed] [Google Scholar]
- 5.Hirschmann M.T., Moser L.B., Amsler F., Behrend H., Leclerq V., Hess S. Functional knee phenotypes: a novel classification for phenotyping the coronal lower limb alignment based on the native alignment in young non-osteoarthritic patients. Knee Surg Sports Traumatol Arthrosc. 2019;27(5):1394–1402. doi: 10.1007/s00167-019-05509-z. May. [DOI] [PubMed] [Google Scholar]
- 6.Parratte S., Pagnano M.W., Trousdale R.T., Berry D.J. Effect of postoperative mechanical axis alignment on the fifteen-year survival of modern, cemented total knee replacements. J Bone Joint Surg Am. 2010;92(12):2143–2149. doi: 10.2106/JBJS.I.01398. Sep. 15. [DOI] [PubMed] [Google Scholar]
- 7.Morgan S.S., Bonshahi A., Pradhan N., Gregory A., Gambhir A., Porter M.L. The influence of postoperative coronal alignment on revision surgery in total knee arthroplasty. Int Orthop. 2008;32(5):639–642. doi: 10.1007/s00264-007-0391-0. Oct. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Howell S.M., Hull M.L. Kinematic alignment in TKA: definition, surgical technique, and challenging cases. Orthop Knowl Online. 2012;10 Number 7. [Google Scholar]
- 9.Howell S.M., Howell S.J., Kuznik K.T., Cohen J., Hull M.L. Does a kinematically aligned total knee arthroplasty restore function without failure regardless of alignment category? Clin Orthop Relat Res. 2013;471(3):1000–1007. doi: 10.1007/s11999-012-2613-z. Mar. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Liu B., Feng C., Tu C. Kinematic alignment versus mechanical alignment in primary total knee arthroplasty: an updated meta-analysis of randomized controlled trials. J Orthop Surg Res. 2022;17(1):201. doi: 10.1186/s13018-022-03097-2. Apr 4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Malavolta M., Compagnoni R., Mezzari S., Calanna F., Pastrone A., Randelli P. Good clinical results using a modified kinematic alignment technique with a cruciate sacrificing medially stabilised total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2022;30(2):500–506. doi: 10.1007/s00167-020-06196-x. Feb. [DOI] [PubMed] [Google Scholar]
- 12.Vendittoli P.A., Martinov S., Blakeney W.G. Restricted kinematic alignment, the fundamentals, and clinical applications. Front Surg. 2021;8 doi: 10.3389/fsurg.2021.697020. Jul 20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Moher D., Liberati A., Tetzlaff J., Altman D.G., PRISMA Group Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med. 2009;151(4):264–269. doi: 10.7326/0003-4819-151-4-200908180-00135. Aug 18. W64. [DOI] [PubMed] [Google Scholar]
- 14.Cacciola G., Mancino F., De Meo F., et al. Mid-term survivorship and clinical outcomes of the medial stabilized systems in primary total knee arthroplasty: a systematic review. J Orthop. 2021;24:157–164. doi: 10.1016/j.jor.2021.02.022. Feb 22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cacciola G., Mancino F., De Meo F., Bruschetta A., De Martino I., Cavaliere P. Current reconstruction options in periprosthetic fractures around the knee. Geriatr Orthop Surg Rehabil. 2021;12 doi: 10.1177/21514593211023996. Aug 27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hutt J.R., LeBlanc M.A., Massé V., Lavigne M., Vendittoli P.A. Kinematic TKA using navigation: surgical technique and initial results. Orthop Traumatol Surg Res. 2016;102(1):99–104. doi: 10.1016/j.otsr.2015.11.010. Feb. [DOI] [PubMed] [Google Scholar]
- 17.Laforest G., Kostretzis L., Kiss M.O., Vendittoli P.A. Restricted kinematic alignment leads to uncompromised osseointegration of cementless total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2022;30(2):705–712. doi: 10.1007/s00167-020-06427-1. Feb. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.MacDessi S.J., Griffiths-Jones W., Chen D.B., et al. Restoring the constitutional alignment with a restrictive kinematic protocol improves quantitative soft-tissue balance in total knee arthroplasty: a randomized controlled trial. Bone Joint Lett J. 2020;102-B(1):117–124. doi: 10.1302/0301-620X.102B1.BJJ-2019-0674.R2. Jan. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Abhari S., Hsing T.M., Malkani M.M., et al. Patient satisfaction following total knee arthroplasty using restricted kinematic alignment. Bone Joint Lett J. 2021;103-B(6 Supple A):59–66. doi: 10.1302/0301-620X.103B6.BJJ-2020-2357.R1. Jun. [DOI] [PubMed] [Google Scholar]
- 20.Sappey-Marinier E., Shatrov J., Batailler C., et al. Restricted kinematic alignment may be associated with increased risk of aseptic loosening for posterior-stabilized TKA: a case-control study. Knee Surg Sports Traumatol Arthrosc. 2021;23 doi: 10.1007/s00167-021-06714-5. Aug. [DOI] [PubMed] [Google Scholar]
- 21.Winnock de Grave P., Luyckx T., Claeys K., et al. Higher satisfaction after total knee arthroplasty using restricted inverse kinematic alignment compared to adjusted mechanical alignment. Knee Surg Sports Traumatol Arthrosc. 2022;30(2):488–499. doi: 10.1007/s00167-020-06165-4. Feb. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Burns P.B., Rohrich R.J., Chung K.C. The levels of evidence and their role in evidence-based medicine. Plast Reconstr Surg. 2011;128(1):305–310. doi: 10.1097/PRS.0b013e318219c171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Slim K., Nini E., Forestier D., Kwiatkowski F., Panis Y., Chipponi J. Methodological index for non-randomized studies (minors): development and validation of a new instrument. ANZ J Surg. 2003;73(9):712–716. doi: 10.1046/j.1445-2197.2003.02748.x. Sep. [DOI] [PubMed] [Google Scholar]
- 24.Sideri S., Papageorgiou S.N., Eliades T. Registration in the international prospective register of systematic reviews (PROSPERO) of systematic review protocols was associated with increased review quality. J Clin Epidemiol. 2018;100:103–110. doi: 10.1016/j.jclinepi.2018.01.003. Aug. [DOI] [PubMed] [Google Scholar]
- 25.Blakeney W.G., Vendittoli P.A. In: Personalized Hip and Knee Joint Replacement [Internet] Rivière C., Vendittoli P.A., editors. Springer; Cham (CH): 2020. Restricted kinematic alignment: the ideal compromise? 2020 jul 1. (Chapter 17). PMID: 33347126. [DOI] [PubMed] [Google Scholar]
- 26.Khan M., Osman K., Green G., Haddad F.S. The epidemiology of failure in total knee arthroplasty: avoiding your next revision. Bone Joint Lett J. 2016;98-B(1 Suppl A):105–112. doi: 10.1302/0301-620X.98B1.36293. Jan. [DOI] [PubMed] [Google Scholar]
- 27.Iyengar K.P., Gowers B.T.V., Jain V.K., Ahluwalia R.S., Botchu R., Vaishya R. Smart sensor implant technology in total knee arthroplasty. J Clin Orthop Trauma. 2021;22 doi: 10.1016/j.jcot.2021.101605. Sep. 22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Vishwanathan K., Kambhampati S.B.S., Vaishya R. Equivalent outcomes of ultra-congruent and standard cruciate-retaining inserts in total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2022;11 doi: 10.1007/s00167-021-06833-z. Jan. Epub ahead of print. PMID: 35013748. [DOI] [PubMed] [Google Scholar]
- 29.Mishra A.K., Vaish A., Vaishya R. Effect of Body mass index on the outcomes of primary total knee arthroplasty up to one year - a prospective study. J Clin Orthop Trauma. 2022;27 doi: 10.1016/j.jcot.2022.101829. Mar 8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Cacciola G., De Martino I., De Meo F. Does the medial pivot knee improve the clinical and radiographic outcome of total knee arthroplasty? A single centre study on two hundred and ninety seven patients. Int Orthop. 2020;44(2):291–299. doi: 10.1007/s00264-019-04462-3. Feb. [DOI] [PubMed] [Google Scholar]
- 31.Sabatini L., Bosco F., Barberis L., et al. Kinetic sensors for ligament balance and kinematic evaluation in anatomic Bi-cruciate stabilized total knee arthroplasty. Sensors. 2021;21(16):5427. doi: 10.3390/s21165427. Aug 11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Bistolfi A., Giustra F., Bosco F., et al. Comparable results between crosslinked polyethylene and conventional ultra-high molecular weight polyethylene implanted in total knee arthroplasty: systematic review and meta-analysis of randomised clinical trials. Knee Surg Sports Traumatol Arthrosc. 2022;19 doi: 10.1007/s00167-022-06879-7. Feb. Epub ahead of print. PMID: 35182171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Bistolfi A., Giustra F., Bosco F., et al. Ultra-high molecular weight polyethylene (UHMWPE) for hip and knee arthroplasty: the present and the future. J Orthop. 2021;25:98–106. doi: 10.1016/j.jor.2021.04.004. Apr 23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Risitano S., Sabatini L., Barberis L., Fusini F., Malavolta M., Indelli P.F. Combining kinematic alignment and medial stabilized design in total knee arthroplasty: basic rationale and preliminary clinical evidences. J Orthop. 2020;21:427–431. doi: 10.1016/j.jor.2020.08.025. Aug 27. PMID: 32943829; PMCID: PMC7479312. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data is contained within the article.