Abstract
Aims
To investigate the ability of the Academic Research Consortium for High Bleeding Risk (ARC-HBR) criteria and ARC-HBR score to predict 2-year bleeding and mortality in patients undergoing transcatheter aortic valve replacement (TAVR).
Methods and results
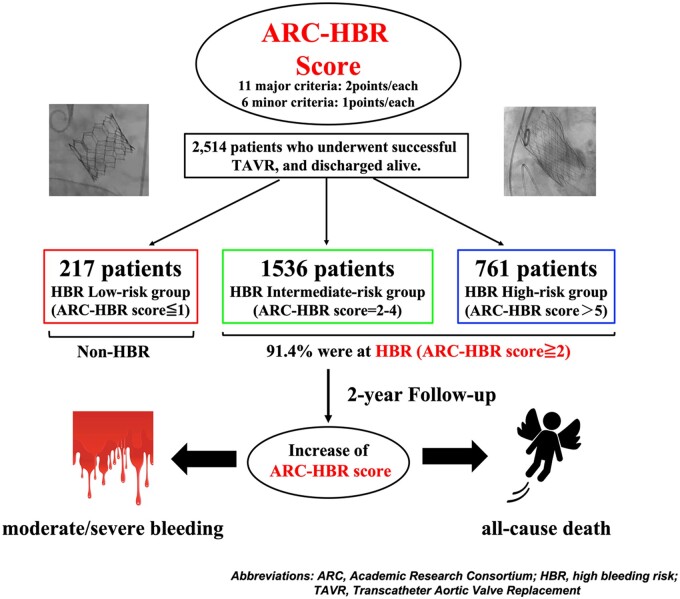
We enrolled 2514 patients who underwent successful TAVR during 2013–17. In this study, we used the ARC-HBR score for further HBR-risk stratification, and the ARC-HBR score was calculated as follows: each major criterion was 2 points and each minor criterion was 1 point. The impact of the ARC-HBR criteria and increasing ARC-HBR score on the incidence of moderate/severe bleeding events, mortality, and ischaemic stroke in the first 2 years were evaluated. We used survival classification and regression tree (CART) analysis for 2-year moderate or severe bleeding events, and patients were statistically classified into HBR low- (ARC-HBR score ≤1), intermediate- (ARC-HBR score = 2–4), or high-risk (ARC-HBR score ≥5) groups, and 91.4% were at HBR (ARC-HBR score ≥2). The rates of 2-year moderate/severe bleeding events and all-cause mortality were higher in the ARC-HBR group and highest in the HBR high-risk group. An increased HBR score was significantly associated with moderate/severe bleeding events [hazard ratio (HR) 1.19, 95% confidence interval (CI) 1.07–1.31; P = 0.001] and all-cause mortality (adjusted HR 1.24, 95% CI 1.17–1.32; P < 0.001).
Conclusions
The ARC-HBR criteria identify patients at HBR after TAVR; an increased ARC-HBR score is associated with 2-year moderate/severe bleeding events and mortality.
Keywords: All-cause mortality, High-bleeding risk, Transcatheter aortic valve replacement, Aortic stenosis
Graphical Abstract
Graphical Abstract.
Introduction
Transcatheter aortic valve replacement (TAVR) is a feasible therapeutic option for patients who require a valve replacement, regardless of the patient’s surgical risk, and provides satisfactory mid-term clinical outcomes.1–5 This trend is similar to that of percutaneous coronary intervention (PCI) using new-generation drug-eluting stents, which improved clinical outcomes as an alternative therapy for coronary artery bypass grafting in patients with ischaemic heart disease.6 The bleeding risk after PCI has been studied extensively, and several studies have reported that post-PCI bleeding negatively affected survival as significantly as the occurrence of thrombotic events.7–11 Following these reports, the Academic Research Consortium for High-Bleeding Risk (ARC-HBR) standardized the definition of high-bleeding risk (HBR) through a literature review and the consensus of experts.12 HBR was defined as a ≥ 4% risk of Bleeding Academic Research Consortium (BARC) type 3 or 5 bleeding at 1 year or a ≥ 1% risk of an intracranial haemorrhage at 1 year.13 Several studies regarding the validation of the ARC-HBR criteria after PCI in real clinical settings have verified that the definition of HBR accurately identifies patients at an increased risk not only for bleeding but also for thrombotic events.14–16 On the other hand, antithrombotic therapy is recommended after TAVR as well as after PCI, and TAVR is typically performed for older patients with a high surgical risk17,18 who are frail and have multiple comorbidities associated with HBR.19,20 Therefore, further information on the bleeding risk, and bleeding events on mortality after TAVR is warranted, although the balance between bleeding and thrombotic risks in patients who undergo TAVR has also been studied.19 However, the prevalence, expected bleeding event rate, and expected ischaemic event rate of patients with HBR, and the association of HBR and mortality after TAVR are rarely reported except post hoc analysis from POPular TAVI trial.21 Since there is no bleeding risk stratification model for TAVI patients, we applied the ARC-HBR criteria to patients who underwent TAVR to investigate the prevalence of bleeding events, ischaemic events, and mortality in the first 2 years after discharge. Furthermore, we stratified the patients based on the ARC-HBR score, as we hypothesized that nearly all of the patients who underwent TAVR would be at HBR.
Methods
Study population
We analysed data from 2514 patients who were enrolled in the Optimized Transcatheter Valvular Intervention-Transcatheter Aortic Valve Implantation (OCEAN-TAVI) registry and discharged after a successful TAVI between October 2013 and May 2017. The OCEAN-TAVI is a prospective, multicentre, observational registry of patients with severe aortic stenosis who underwent TAVR at 1 of the 14 collaborating hospitals located in Japan.18 This trial was registered with the University Hospital Medical Information Network Clinical Trials Registry (UMIN-ID: 000020423). The study protocol was developed in accordance with the Declaration of Helsinki and was approved by the ethics committee of each participating hospital. All patients provided written informed consent prior to participation in this study.
Definition of the Academic Research Consortium for High Bleeding Risk criteria and scoring
There are 11 major ARC-HBR criteria and 6 minor criteria.12 Patients are considered to be at HBR if they meet at least one major criterion or two minor criteria. In this study, we assigned each major criterion 2 points and each minor criterion 1 point. A patient’s ARC-HBR score was the sum of the points of the criteria that the patient met. The study population was classified into three groups according to the ARC-HBR score. Patients with ARC-HBR score ≥2 were considered to be at HBR, as this indicates the presence of at least one major criterion or two minor criteria. In this study, two major criteria (spontaneous bleeding event requiring hospitalization or transfusion in the past 6 months or at any time if recurrent and chronic bleeding diathesis) and one minor criterion (spontaneous bleeding event requiring hospitalization or transfusion within the past 12 months) were not captured from the registry dataset. Therefore, the major criteria were severe chronic kidney disease [estimated glomerular filtration rate (eGFR) <30 mL/min], thrombocytopenia (platelet count <100 × 109/L), severe anaemia (haemoglobin <11 g/dL), liver cirrhosis, prior haemorrhagic stroke or moderate or severe ischaemic stroke within the past 6 months, active malignancy, and anticipated use of long-term oral anti-coagulation. The minor criteria were age ≥75 years, mild anaemia [haemoglobin (men vs. women) = 11.0–12.9 vs. 11.0–11.9 g/dL], prior ischaemic stroke, and moderate chronic kidney disease (eGFR = 30–59 mL/min).
Data collection and statistical analysis
All data were collected from the OCEAN-TAVI database. During the study period, the Edwards SAPIEN-XT and SAPIEN-3 (Edwards Lifesciences, Irvine, CA, USA) as balloon-expandable prosthesis and the Medtronic CoreValve and Evolut-R System (Medtronic, Minneapolis, MN, USA) as self-expandable prosthesis were available in Japan. Indication and decision for the approach route of TAVR were decided on the individual local heart team members. Dual antiplatelet therapy (DAPT) is usually recommended for 3–6 months, followed by indefinite single antiplatelet therapy (SAPT) after TAVR in patients who are not eligible for anti-coagulation, and combination therapy of oral anticoagulants (OAC) and SAPT, followed by indefinite OAC after TAVR in patients eligible for anti-coagulation. The specific antithrombotic regimen selected including when to reduce the regimen to single agent was at the discretion of each operator who considered the individual patient’s risk. The primary study endpoint was a moderate or severe bleeding event in the first 2 years after discharge, defined according to the Global Utilization of Streptokinase and Tissue Plasminogen Activator for Occluded Coronary Arteries (GUSTO).13 The secondary study endpoints were 2-year all-cause mortality and 2-year ischaemic stroke rates after hospital discharge.
Continuous variables are presented as the median and interquartile range (IQR), and categorical variables are presented as number and percentage. First, we used survival classification and regression tree (CART) analysis for 2-year moderate or severe bleeding events.22 We used the ctree function of the party package with moderate or severe bleeding events as the outcome measure and the ARC-HBR score as an independent variable to determine the cut-off values of the ARC-HBR score that define low-, intermediate-, and high-risk HBR. The study population was divided into three HBR groups: high-risk, intermediate-risk, and low-risk. We used a univariable Cox regression model to determine the impact of the ARC-HBR score on the study endpoints. Variables that were found to be significantly different between the three groups were included. We did not include variables that were already included in the ARC-HBR score (age, a history of ischaemic stroke, liver cirrhosis, or malignancy), laboratory data on admission (haemoglobin, platelet count, and eGFR), or STS score [the presence of atrial fibrillation or peripheral artery disease and New York Heart Association (NYHA) heart failure functional class]. The variables with P < 0.05 in the univariate analysis were included in the multivariate model, and the Akaike information criteria were used to select the best predictive Cox model. The incidence of each endpoint was estimated using the Kaplan–Meier method and was reported with the 95% confidence interval (CI). Differences among the three groups were evaluated using the log-rank test. Differences in continuous and categorical variables among the groups were compared using the Wilcoxon rank-sum test or the chi-square test, respectively. Statistical analyses were performed using R software packages (version 3.6.3; R Development Core Team). Statistical significance was set at P < 0.05.
Results
The patient characteristics, procedural information, and periprocedural clinical outcome data are listed in Table 1. The median ARC-HBR score was 4. Patients with ARC-HBR score ≤1, 2–4, and ≥5 were included in the HBR low- (n = 217), intermediate- (n = 1536), and high-risk (n = 761) groups, respectively, according to the survival CART analysis results. The majority of the patients (91.4%) met the definition of HBR. The evaluation items for ARC-HBR scoring are listed in Supplemental material online, TableS1. The median patient age was 85 years, and 30.6% of the patients were men. The majority of the participants (96.1%) presented with NYHA Class II or higher. The median Canadian Study of Health and Aging’s Clinical Frailty Scale score was 4. The median STS score was 6.5%. The median plasma brain natriuretic peptide level on admission was 268 (IQR 118–563) pg/mL. The majority of patients (86.9%) received the SAPIEN XT or SAPIEN 3 valve (Edwards Lifesciences, Irvine, CA, USA) with a median valve size of 23 mm. The transfemoral approach for TAVR was used in 85.7% of patients. Acute kidney injury after TAVR occurred in 9.6% of patients. Echocardiography revealed that the mean post-procedural left ventricular ejection fraction (LVEF) was 63%, the mean aortic valve pressure gradient was 10 mmHg, and the mean effective orifice area index was 1.15 cm2/m2. Over half of the patients (54.1%) were administered dual anti-platelet therapy (DAPT) (clopidogrel and aspirin) after TAVR.
Table 1.
Patient characteristics
| Total n = 2514 | Low-risk n = 217 | Intermediate-risk n = 1536 | High-risk n = 761 | P-value | |
|---|---|---|---|---|---|
| HBR | 2297 (91.4) | 0 (0.0) | 1536 (100.0) | 761 (100.0) | <0.001 |
| ARC-HBR score | 4 (2–5) | 1 (1–1) | 3 (2–4) | 6 (5–6) | <0.001 |
| Age (years) | 85 (81–88) | 82 (79–86) | 85 (82–88) | 85 (81–88) | <0.001 |
| Male sex | 768 (30.6) | 75 (34.6) | 455 (29.6) | 238 (31.3) | 0.293 |
| BSA (m2) | 1.42 (1.30–1.54) | 1.47 (1.33–1.59) | 1.41 (1.30–1.53) | 1.41 (1.31–1.53) | <0.001 |
| Atherosclerotic risks | |||||
| Hypertension | 1930 (76.8) | 167 (77.0) | 1170 (76.2) | 593 (77.9) | 0.644 |
| Dyslipidaemia | 1079 (42.9) | 112 (51.6) | 683 (44.5) | 284 (37.3) | <0.001 |
| Diabetes mellitus | 541 (21.5) | 47 (21.7) | 297 (19.3) | 197 (25.9) | 0.002 |
| Current smoking | 61 (2.4) | 8 (3.7) | 32 (2.1) | 21 (2.8) | 0.276 |
| Atrial fibrillation | 500 (19.9) | 0 (0.0) | 122 (7.9) | 378 (49.7) | <0.001 |
| History of coronary stenting | 324 (12.9) | 20 (9.2) | 212 (13.8) | 92 (12.1) | 0.124 |
| History of coronary artery bypass grafting | 157 (6.3) | 17 (7.8) | 89 (5.8) | 51 (6.7) | 0.419 |
| History of myocardial infarction | 159 (6.3) | 9 (4.1) | 94 (6.1) | 56 (7.4) | 0.200 |
| History of ischaemic stroke | 272 (10.9) | 2 (0.9) | 122 (7.9) | 148 (19.4) | <0.001 |
| History of haemorrhagic stroke | 12 (0.5) | 0 (0.0) | 4 (0.3) | 8 (1.1) | 0.020 |
| Peripheral vascular disease | 350 (13.9) | 21 (9.7) | 197 (12.8) | 132 (17.3) | 0.002 |
| Pulmonary dysfunction | 589 (23.4) | 49 (22.6) | 355 (23.1) | 185 (24.3) | 0.778 |
| Liver cirrhosis | 75 (3.0) | 0 (0.0) | 11 (0.7) | 64 (8.4) | <0.001 |
| Malignancy | 124 (4.9) | 0 (0.0) | 35 (2.3) | 89 (11.7) | <0.001 |
| NYHA class | <0.001 | ||||
| Class II | 1150 (45.7) | 126 (58.1) | 739 (48.1) | 285 (37.5) | |
| Class III | 1092 (43.4) | 68 (31.3) | 648 (42.2) | 376 (49.4) | |
| Class IV | 177 (7.0) | 7 (3.2) | 89 (5.8) | 81 (10.6) | |
| Clinical Frailty Scale | 4 (3–5) | 3 (3–4) | 4 (3–4) | 4 (3–5) | <0.001 |
| STS score | 6.5 (4.5–9.4) | 4.6 (3.0–6.6) | 6.2 (4.4–8.7) | 8.1 (5.4–12.5) | <0.001 |
| Long-term use of steroids or NSAIDs | 128 (5.1) | 2 (0.9) | 49 (3.2) | 77 (10.1) | <0.001 |
| Laboratory data on admission | |||||
| Haemoglobin (mg/dL) | 11.2 (10.1–12.4) | 13.2 (12.6–13.7) | 11.4 (10.4–12.5) | 10.3 (9.4–11.2) | <0.001 |
| Platelet count (×104/µL) | 17.6 (14.3–21.4) | 19.1 (16.0–21.8) | 17.9 (14.9–21.6) | 16.4 (11.9–20.6) | <0.001 |
| e-GFR (mL/min/1.73 m2) | 50.6 (38.0–63.1) | 70.9 (64.9–80.8) | 52.7 (42.4–63.5) | 38.0 (27.2–50.3) | <0.001 |
| BNP (pg/mL) | 268 (118–563) | 127 (58–309) | 252 (109–525) | 352 (176–703) | <0.001 |
| TAVR procedure | |||||
| Transfemoral approach | 2154 (85.7) | 191 (88.0) | 1307 (85.1) | 656 (86.2) | 0.456 |
| Valve type | 0.970 | ||||
| Edwards SAPIEN XT valve | 1349 (53.7) | 118 (54.4) | 829 (54.0) | 402 (52.8) | |
| Edwards SAPIEN 3 valve | 834 (33.2) | 72 (33.2) | 506 (32.9) | 256 (33.6) | |
| Medtronic Corevalve | 189 (7.5) | 13 (6.0) | 117 (7.6) | 59 (7.8) | |
| Medtronic EvolutR | 142 (5.7) | 14 (6.5) | 84 (5.5) | 44 (5.8) | |
| Valve size (mm) | 23 (23–26) | 26 (23–26) | 23 (23–26) | 23 (23–26) | 0.231 |
| Procedure time (min) | 69 (52–94) | 70 (52–92) | 68 (52–93) | 72 (52–97) | 0.607 |
| Periprocedural complications | |||||
| Coronary occlusion | 23 (0.9) | 1 (0.5) | 15 (1.0) | 7 (0.9) | 0.757 |
| Ischaemic stroke | 48 (1.9) | 3 (1.4) | 28 (1.8) | 17 (2.2) | 0.667 |
| Permanent pacemaker implantation | 210 (8.4) | 14 (6.5) | 133 (8.7) | 63 (8.3) | 0.544 |
| Acute kidney injury | 241 (9.6) | 9 (4.1) | 123 (8.0) | 109 (14.3) | <0.001 |
| Major bleeding | 268 (10.7) | 20 (9.2) | 153 (10.0) | 95 (12.5) | 0.141 |
| Minor bleeding | 224 (8.9) | 4 (1.8) | 116 (7.6) | 104 (13.7) | <0.00 |
| All bleeding | 492 (19.6) | 24 (11.1) | 269 (17.5) | 199 (26.1) | <0.001 |
| New-onset atrial fibrillation | 93 (3.7) | 11 (5.1) | 62 (4.1) | 20 (2.6) | 0.124 |
| Transthoracic echocardiography after TAVR | |||||
| LVEF by modified Simpson’s or Teichholz (%) | 63 (55–68) | 63 (56–67) | 64 (56–68) | 62 (54–67) | 0.001 |
| Mean aortic valve pressure gradient (mmHg) | 10 (8–13) | 11 (8–14) | 10 (8–13) | 10 (7–13) | <0.001 |
| Peak aortic valve pressure gradient (mmHg) | 19 (15–25) | 21 (15–27) | 20 (16–26) | 19 (14–25) | 0.006 |
| Effective orifice area index with Doppler (cm2/m2) | 1.15 (0.97–1.35) | 1.20 (1.02–1.43) | 1.14 (0.97–1.34) | 1.15 (0.96–1.34) | 0.008 |
| Perivalvular leakage grade ≧ moderate | 44 (1.8) | 4 (1.8) | 25 (1.6) | 15 (2.0) | 0.744 |
| Anti-thrombotic medications at discharge | <0.001 | ||||
| Anti-platelet therapy | |||||
| Clopidogrel alone | 109 (4.3) | 7 (3.2) | 68 (4.4) | 34 (4.5) | |
| Aspirin alone | 328 (13.1) | 21 (9.7) | 200 (13.0) | 107 (14.1) | |
| Clopidogrel and aspirin (DAPT) | 1361 (54.1) | 151 (69.6) | 951 (61.9) | 259 (34.0) | |
| Oral anti-coagulation therapy | |||||
| Warfarin alone | 82 (3.3) | 4 (1.8) | 34 (2.2) | 44 (5.8) | |
| DOAC alone | 110 (4.4) | 6 (2.8) | 54 (3.5) | 50 (6.6) | |
| Combination therapy | |||||
| OAC and anti-platelet therapy | 384 (15.3) | 17 (7.8) | 142 (9.2) | 225 (29.6) | |
| Triple therapy (OAC and DAPT) | 35 (1.4) | 1 (0.5) | 17 (1.1) | 17 (2.2) | |
| None | 105 (4.2) | 10 (4.6) | 70 (4.6) | 25 (3.3) | |
| Proton pump inhibitor | 1610 (64.0) | 118 (54.4) | 950 (61.8) | 542 (71.2) | <0.001 |
| H2-blocker | 148 (5.9) | 17 (7.8) | 88 (5.7) | 43 (5.7) | 0.808 |
Categorical variables are shown as numbers (percentages) and continuous variables are shown as medians (25–75 percentiles).
ARC, Academic Research Consortium; BNP, brain natriuretic peptide; BSA, body surface area; DAPT, dual antiplatelet therapy; DOAC, direct oral anticoagulant; e-GFR, estimated glomerular filtration rate; HBR, high bleeding risk; LVEF, left ventricular ejection fraction; NYHA, New York Heart Association; NSAIDs; non-steroidal anti-inflammatory drugs; OAC, oral anticoagulant; STS, Society of Thoracic Surgeons; TAVR, transcatheter aortic valve replacement.
The HBR high-risk group was significantly older (P < 0.001) with significantly higher clinical frailty (P < 0.001) and STS (P < 0.001) scores and a significantly lower LVEF (P = 0.001) than the other two groups. The HBR-high-risk group had a significantly higher incidence of acute kidney injury, periprocedural minor bleeding, and all (minor or major) bleeding events after TAVR (P < 0.001) than the other two groups. The number of anti-thrombotic medications at discharge was significantly different among the three groups (P < 0.001).
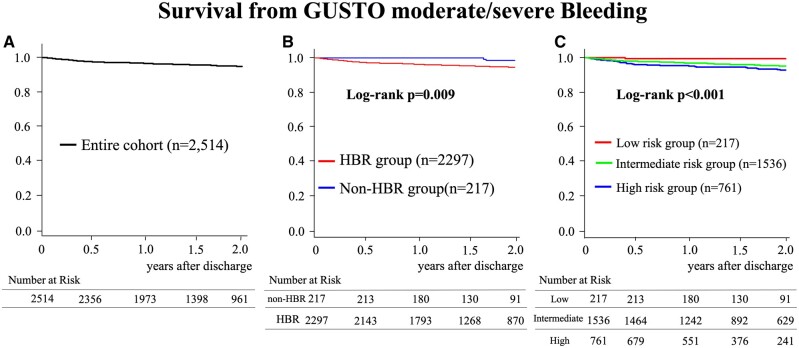
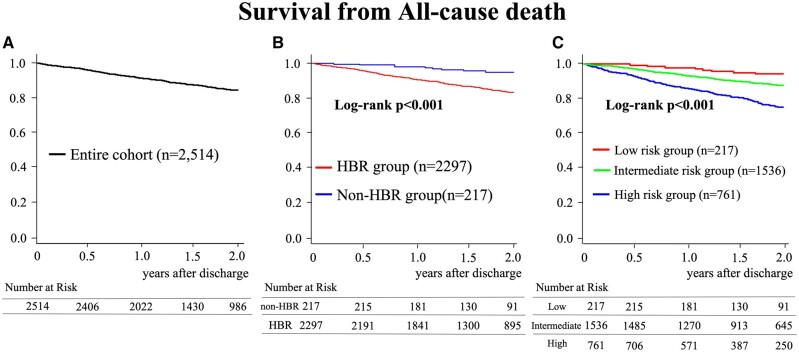
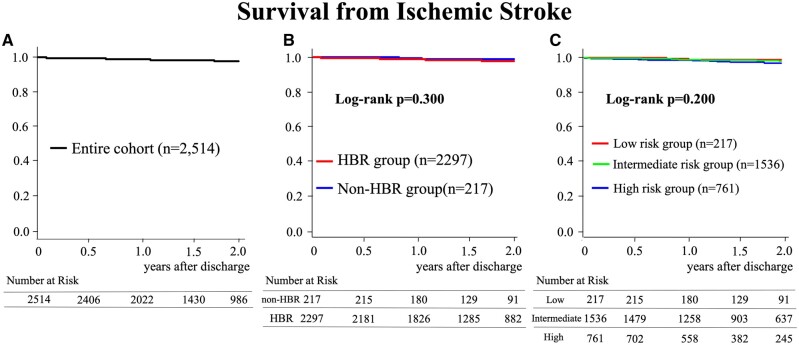
During the 2-year follow-up, 106 bleeding events, 328 deaths, and 42 ischaemic stroke events were noted. The rate of moderate/severe bleeding events was 3.3% (95% CI 2.5–4.0) at 1 year and 5.1% (95% CI 3.1–6.0) at 2 years (Figure 1). The all-cause mortality rate was 8.4% (95% CI 7.3–9.5) at 1 year and 15.5% (95% CI 13.9–17.1) at 2 years (Figure 2). The rate of ischaemic stroke was 1.2% (95% CI 0.7–1.6) at 1 year and 2.1% (95% CI 1.5–2.8) at 2 years (Figure 3).
Figure 1.
Incidence of bleeding events. (A) The rate of moderate/severe bleeding events in the entire patient population is shown. (B) The rates of moderate/severe bleeding events are compared between patients at high-bleeding risk (HBR; HBR group) and the non-HBR group. (C) The rates of moderate/severe bleeding events are compared between patients in the HBR low-, intermediate-, and high-risk groups.
Figure 2.
Incidence of mortality. (A) The mortality rate in the entire patient population is shown. (B) The mortality rates are compared between patients at high-bleeding risk (HBR; HBR group) and the non-HBR group. (C) The mortality rates are compared between patients in the HBR low-, intermediate-, and high-risk groups.
Figure 3.
Incidence of ischaemic stroke. (A) The rate of ischaemic stroke in the entire patient population is shown. (B) The rates of ischaemic stroke are compared between patients at high-bleeding risk (HBR; HBR group) and the non-HBR group. (C) The rates of moderate/severe bleeding events are compared between patients in the HBR low-, intermediate-, and high-risk groups.
The rates of moderate/severe bleeding events and all-cause mortality were higher in the patients at HBR (Figures 1B and 2B) and significantly higher in the HBR high-risk group than in the other two groups (P < 0.001) (Figures 1C and 2C). The rate of moderate/severe bleeding events at 1 and 2 years was 4.6% (95% CI 3.0–6.1), 3.1% (95% CI 2.2–4.0), and 0.7% (95% CI 0.0–2.1) and 7.2% (95% CI 5.0–9.4), 4.6% (95% CI 3.3–5.8), and 1.4% (95% CI 0.0–3.4) in the HBR high-, intermediate-, and low-risk groups, respectively. The all-cause mortality rate at 1 and 2 years was 14.2% (95% CI 11.7–16.7), 6.5% (95% CI 5.2–7.7), and 1.8% (95% CI 0.0–3.6) and 24.8% (95% CI 21.2–28.2), 12.6% (95% CI 10.7–14.4), and 5.0% (95% CI 1.7–8.3) in the HBR high-, intermediate-, and low-risk groups, respectively. The rate of ischaemic stroke was not significantly different between patients at HBR and those not at HBR or between the three groups (Figure 3B,C). The ARC-HBR group (the HBR intermediate- or high-risk group) had a higher risk of moderate/severe bleeding [hazard ratio (HR) 10.43, 95% confidence interval (CI) 1.46–74.77; P = 0.020] and death (HR 3.14, 95% CI 1.67–5.89; P < 0.001) than the non-HBR group (the HBR low-risk group) (Table 2). Furthermore, each 1-point increase in the ARC-HBR score was associated with an increased risk of moderate/severe bleeding events (adjusted HR 1.19, 95% CI 1.07–1.31; P = 0.001) and all-cause mortality (adjusted HR 1.23, 95% CI 1.15–1.31; P < 0.001) although it was not associated with an increased risk of ischaemic stroke (HR 1.16, 95% CI 0.99–1.36; P = 0.072) (Table 2). In addition, each 1-point increase in the clinical frailty scale was also associated with an increased risk of moderate/severe bleeding events (adjusted HR 1.19, 95% CI 1.07–1.31; P = 0.001) and all-cause mortality (adjusted HR 1.23, 95% CI 1.13–1.34; P < 0.001), the occurrence of AKI was associated with an increased risk of all-cause mortality (adjusted HR 1.77, 95% CI 1.32–2.36; P < 0.001), and increased STS risk score was associated with an increased risk of ischaemic stroke events (adjusted HR 1.04, 95% CI 1.01–1.06; P = 0.004) (Table 2).
Table 2.
Cox regression analysis for each endpoint
| Univariable |
Multivariable |
AIC model |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| HR | 95% CI | P-value | Adjusted HR | 95% CI | P-value | Adjusted HR | 95% CI | P-value | |
| GUSTO moderate/severe bleeding | |||||||||
| ARC-HBR (the HBR intermediate- or high-risk group vs. low-risk group) | 10.43 | 1.46–74.77 | <0.001 | ||||||
| HBR score (per 1 point increase) | 1.20 | 1.09–1.33 | <0.001 | 1.19 | 1.07–1.31 | 0.001 | 1.19 | 1.07–1.31 | 0.001 |
| Clinical Frailty Scale (per 1 point increase) | 1.23 | 1.06–1.42 | 0.006 | 1.19 | 1.03–1.38 | 0.020 | 1.19 | 1.03–1.38 | 0.020 |
| STS risk score | 1.02 | 0.99–1.04 | 0.162 | ||||||
| BNP on admission | 1.00 | 1.00–1.00 | 0.897 | ||||||
| Acute kidney injury | 1.05 | 0.55–2.01 | 0.883 | ||||||
| All-cause mortality | |||||||||
| ARC-HBR (the HBR intermediate- or high-risk group vs. low-risk group) | 3.14 | 1.67–5.89 | 0.020 | ||||||
| HBR score (per 1 point increase) | 1.30 | 1.23–1.38 | <0.001 | 1.23 | 1.15–1.31 | <0.001 | 1.24 | 1.17–1.32 | <0.001 |
| Clinical Frailty Scale (per 1 point increase) | 1.31 | 1.21–1.42 | <0.001 | 1.18 | 1.07–1.30 | 0.001 | 1.23 | 1.13–1.34 | <0.001 |
| STS risk score | 1.04 | 1.03–1.04 | <0.001 | 1.01 | 1.00–1.03 | 0.032 | 1.01 | 1.00–1.03 | 0.009 |
| BNP on admission | 1.00 | 1.00–1.00 | 0.015 | 1.00 | 1.00–1.00 | 0.658 | |||
| Acute kidney injury | 2.45 | 1.86–3.23 | <0.001 | 1.91 | 1.40–2.61 | <0.001 | 1.77 | 1.32–2.36 | <0.001 |
| Ischaemic stroke | |||||||||
| ARC-HBR (the HBR intermediate- or high-risk group vs. low-risk group) | 1.98 | 0.48–8.17 | 0.348 | ||||||
| HBR score (per 1 point increase) | 1.16 | 0.99–1.36 | 0.072 | ||||||
| Clinical Frailty Scale (per 1 point increase) | 1.08 | 0.85–1.38 | 0.513 | ||||||
| STS risk score | 1.04 | 1.01–1.06 | 0.004 | ||||||
| BNP on admission | 1.00 | 1.00–1.00 | 0.744 | ||||||
| Acute kidney injury | 1.71 | 0.72–4.07 | 0.221 | ||||||
Categorical variables are shown as numbers (percentages) and continuous variables are shown as medians (25–75 percentiles).
AIC, Akaike information criteria; ARC, Academic Research Consortium; BNP, brain natriuretic peptide; CI, confidence interval; GUSTO, Global Utilization of Streptokinase and Tissue Plasminogen Activator for Occluded Coronary Arteries; HBR, high-bleeding risk; HR, hazard ratio; STS, Society of Thoracic Surgeons.
Discussion
Our study found that 91% of patients who underwent TAVR were at HBR. Meeting the criteria for HBR and an increased ARC-HBR score, and clinical frailty scale were both associated with an increased 2-year risk of moderate/severe bleeding events and all-cause mortality after TAVR. This is the largest study to report the long-term bleeding risks after hospital discharge of patients who undergo TAVR and the effects of HBR on the incidence of bleeding events, mortality, and ischaemic events, as most previous studies focusing on TAVR were short-term and did not include the effects of bleeding risk.1–5,17,19
The ARC-HBR criteria have been evaluated in patients who underwent PCI;14 however, they have rarely evaluated in patients who have undergone TAVR except post hoc analysis from popular TAVI trial.21 They reported that a total of 78.5% had an ARC-HBR Score 2, and thus were considered at HBR according to the ARC-HBR definition of the 978 patients in the cohort, and there was no statistically significant increase of all bleeding, nor of major and life-threatening bleeding, associated with this definition (non-HBR 19.7% vs. HBR 24.1%; P = 0.22; and 6.6% vs. 10.8%; P = 0.08, respectively).21 Of course, the patient background for this study was quite different from that of POPular TAVI trial. In particular, median age (85 years old vs.79.5–81.0) and STS scores (6.5 vs. 2.4–3.2) were higher in patients in our study compared to patients in Popular TAVI,23,24 which may have contributed to the higher HBR rate in our study population (91.4% vs. 78.5%). However, this study from POPular TAVI trial included TAVR perioperative bleeding events as TAVR 1-year events, and did not truly assess the long-term bleeding risk after successful TAVR discharge, because TAVR has more perioperative bleeding events compared to PCI because it uses a large calibre catheter. Therefore, we evaluated the long-term prognostic impact of the ARC-HBR criteria after TAVR discharge using the data of the patients in the OCEAN-TAVI registry. The prevalence of patients at HBR was 91%, and the ARC-HBR criteria accurately identified patients with a higher risk of moderate/severe bleeding events after TAVR discharge in our study, although the previous study considered that the ARC-HBR criteria proposed for PCI patients may not be accurately assessed in TAVR patients, since the background of TAVR patients is very different from that of PCI patients.21 Furthermore, the 2-year mortality after TAVR discharge in patients who met the ARC-HBR criteria was significantly higher than that in patients who did not meet the ARC-HBR criteria. These results are consistent with those of a previous report that showed that late-onset bleeding occurring >30 days after TAVR is related to an increase in mortality.25 In addition, since most of the patients in this study met the ARC-HBR criteria, we stratified them by scoring the factors that make up the ARC-HBR criteria. As a result, patients with ARC-HBR score ≥5 had significantly higher risks of bleeding events and mortality; an increase in the ARC-HBR score significantly affected both endpoints. Patients with ARC-HBR score ≥5 had more comorbidities that are known to be associated with poor clinical outcomes after TAVR.20,26 However, an increased ARC-HBR score was independently associated with higher risks of bleeding events and mortality during the 2 years after TAVR discharge in this study, which is consistent with a previous study that reported that meeting more items of the ARC-HBR criteria was associated with an incrementally higher incidence of major bleeding events in patients who underwent PCI.14 In addition, this study showed that an increase in the clinical frailty scale was also associated with an increase in bleeding events and mortality at 2 years after TAVR. Although Frailty is not included in the ARC-HBR criteria, a recent Japanese guideline on antithrombotic therapy for ischaemic heart disease adopted frailty as bleeding risk factors that are specific to Japanese patients on the basis of the results of previous studies in East Asian patients underwent PCI.27,28 The results of our study indicate that the assessment of frailty is also important for the prediction of bleeding events in Japanese patients undergoing TAVR.
Although risk prediction models for in-hospital mortality after TAVR have been reported,29,30 these models do not include long-term clinical outcomes. The ARC-HBR criteria were developed for the long-term risk stratification of major bleeding events and include factors that have been reported to be associated with long-term mortality after TAVR, including chronic kidney disease, liver cirrhosis, and active cancer.31–33 We believe that the adaptation of the ARC-HBR criteria for patients who undergo TAVR and further risk stratification using the ARC-HBR score will help physicians predict the long-term bleeding events and mortality after TAVR. Our results suggest that patients with higher ARC-HBR scores should be carefully monitored after TAVR discharge. Furthermore, the optimal anti-thrombotic therapy after TAVR is controversial, although the use of DAPT was recommended in practice guidelines until recently.34,35 On the other hand, POPular TAVI trial showed that antithrombotic therapy after TAVR could reduce the risk of bleeding events with monotherapy.23,24 The specific anti-thrombotic medication administered was not associated with bleeding events or mortality in this study, and the specific medication used was determined on a case-by-case basis by the attending physician. More studies are required to determine the association of the ARC-HBR score and specific anti-thrombotic therapies in patients who underwent TAVR. Furthermore, blood disorders such as von Willebrand disease have also been reported as a risk of bleeding after TAVR and should be considered.36
This study has some limitations. First, some ARC-HBR criteria data were not available as the OCEAN-TAVI registry was not designed to investigate the impact of the ARC-HBR criteria. As a result, two major criteria (spontaneous bleeding event requiring hospitalization or transfusion in the past 6 months or at any time if recurrent and chronic bleeding diathesis such as von Willebrand disease) and one minor criterion (spontaneous bleeding event requiring hospitalization or transfusion within the past 12 months) were not available from the registry dataset in this study. Therefore, the prevalence of HBR and the ARC-HBR score may be underestimated in this study. Second, the GUSTO moderate/severe criteria were used to define major bleeding events, while the ARC-HBR initiative defined major bleeding as BARC type 3 or 5 bleeding events. We decided to use the GUSTO criteria based on the data available in the OCEAN-TAVI database, which does not include data regarding haemoglobin drop or the units of red blood cells transfused after each bleeding event. However, some previous PCI trials have reported that the rates of major bleeding were similar when the GUSTO criteria and BARC type 3 or 5 bleeding events were used to define major bleeding.7,37,38 Third, the specific antithrombotic regimen selected including when to reduce the regimen to single agent was at the discretion of each operator who considered the individual patient’s risk. Therefore, it is difficult to interpret the risk of bleeding and mortality with different antithrombotic regimens in this study.
Finally, this study includes only Japanese patients, whose bleeding risk may differ from that of patients in Western countries.21,27,28 It has been reported that haemorrhagic events after PCI treatment are more common in Asians treated with DAPT compared to Westerners.39 Furthermore, the risk of intracranial haemorrhage from anti-coagulation has also been found to be higher in East Asians.40,41 Therefore, the results of this study do not directly apply to Westerners and require careful interpretation.
In conclusion, the ARC-HBR criteria accurately identify patients at HBR after TAVR, and an increased ARC-HBR score is associated with 2-year GUSTO moderate/severe bleeding events and mortality after TAVR, even in cohorts that include many patients at HBR.
Lead author biography
Ka zuki Mizutani is a Japanese cardiologist, and expert of catheter interventions (percutaneous coronary intervention, structural heart disease intervention). He has reported several articles regarding transcatheter aortic valve replacement.
Supplementary material
Supplementary material is available at European Heart Journal Open online.
Supplementary Material
Acknowledgements
We would like to express our heartfelt gratitude to the Japan Society of Clinical Research for their dedicated support and to the investigators and institutions that participated in the OCEAN-TAVI registry.
Funding
The OCEAN-TAVI registry is supported by grants from Edwards Lifesciences, Medtronic, Boston Scientific, Abbott Medical, and Daiichi-Sankyo company.
Conflict of interest: Drs Yamamoto, Tada, Naganuma, Shirai, Mizutani, Tabata, Ueno, and Watanabe are clinical proctors for Edwards Lifesciences and Medtronic. Drs Takagi and Hayashida are clinical proctors for Edwards Lifesciences. The remaining authors have no conflicts of interest to disclose.
Consent: All patients provided written informed consent prior to participation in this study.
Data availability statement
The data underlying this paper cannot be shared publicly because [the data can only be provided to institutions approved by the Ethics Committee]. Upon reasonable request to the corresponding author, the data will be shared.
References
- 1. Smith CR, Leon MB, Mack MJ, Miller DC, Moses JW, Svensson LG, Tuzcu EM, Webb JG, Fontana GP, Makkar RR, Williams M, Dewey T, Kapadia S, Babaliaros V, Thourani VH, Corso P, Pichard AD, Bavaria JE, Herrmann HC, Akin JJ, Anderson WN, Wang D, Pocock SJ;. PARTNER Trial Investigators. Transcatheter versus surgical aortic-valve replacement in high-risk patients. N Engl J Med 2011;364:2187–2198. [DOI] [PubMed] [Google Scholar]
- 2. Leon MB, Smith CR, Mack M, Miller DC, Moses JW, Svensson LG, Tuzcu EM, Webb JG, Fontana GP, Makkar RR, Brown DL, Block PC, Guyton RA, Pichard AD, Bavaria JE, Herrmann HC, Douglas PS, Petersen JL, Akin JJ, Anderson WN, Wang D, Pocock SJ;. PARTNER Trial Investigators. Transcatheter aortic-valve implantation for aortic stenosis in patients who cannot undergo surgery. N Engl J Med 2010;363:1597–1607. [DOI] [PubMed] [Google Scholar]
- 3. Leon MB, Smith CR, Mack MJ, Makkar RR, Svensson LG, Kodali SK, Thourani VH, Tuzcu EM, Miller DC, Herrmann HC, Doshi D, Cohen DJ, Pichard AD, Kapadia S, Dewey T, Babaliaros V, Szeto WY, Williams MR, Kereiakes D, Zajarias A, Greason KL, Whisenant BK, Hodson RW, Moses JW, Trento A, Brown DL, Fearon WF, Pibarot P, Hahn RT, Jaber WA, Anderson WN, Alu MC, Webb JG;. PARTNER 2 Investigators. Transcatheter or surgical aortic-valve replacement in intermediate-risk patients. N Engl J Med 2016;374:1609–1620. [DOI] [PubMed] [Google Scholar]
- 4. Mack MJ, Leon MB, Thourani VH, Makkar R, Kodali SK, Russo M, Kapadia SR, Malaisrie SC, Cohen DJ, Pibarot P, Leipsic J, Hahn RT, Blanke P, Williams MR, McCabe JM, Brown DL, Babaliaros V, Goldman S, Szeto WY, Genereux P, Pershad A, Pocock SJ, Alu MC, Webb JG, Smith CR;. PARTNER 3 Investigators. Transcatheter aortic-valve replacement with a balloon-expandable valve in low-risk patients. N Engl J Med 2019;380:1695–1705. [DOI] [PubMed] [Google Scholar]
- 5. Popma JJ, Deeb GM, Yakubov SJ, Mumtaz M, Gada H, O'Hair D, Bajwa T, Heiser JC, Merhi W, Kleiman NS, Askew J, Sorajja P, Rovin J, Chetcuti SJ, Adams DH, Teirstein PS, Zorn GL, Forrest JK, Tchétché D, Resar J, Walton A, Piazza N, Ramlawi B, Robinson N, Petrossian G, Gleason TG, Oh JK, Boulware MJ, Qiao H, Mugglin AS, Reardon MJ;. Evolut Low Risk Trial Investigators. Transcatheter aortic-valve replacement with a self-expanding valve in low-risk patients. N Engl J Med 2019;380:1706–1715. [DOI] [PubMed] [Google Scholar]
- 6. Piccolo R, Giustino G, Mehran R, Windecker S.. Stable coronary artery disease: revascularisation and invasive strategies. Lancet 2015;386:702–713. [DOI] [PubMed] [Google Scholar]
- 7. Mauri L, Kereiakes DJ, Yeh RW, Driscoll-Shempp P, Cutlip DE, Steg PG, Normand SL, Braunwald E, Wiviott SD, Cohen DJ, Holmes DR Jr, Krucoff MW, Hermiller J, Dauerman HL, Simon DI, Kandzari DE, Garratt KN, Lee DP, Pow TK, Ver Lee P, Rinaldi MJ, Massaro JM;. DAPT Study Investigators. Twelve or 30 months of dual antiplatelet therapy after drug-eluting stents. N Engl J Med 2014;371:2155–2166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Costa F, van Klaveren D, James S, Heg D, Räber L, Feres F, Pilgrim T, Hong MK, Kim HS, Colombo A, Steg PG, Zanchin T, Palmerini T, Wallentin L, Bhatt DL, Stone GW, Windecker S, Steyerberg EW, Valgimigli M; PRECISE-DAPT Study Investigators. Derivation and validation of the predicting bleeding complications in patients undergoing stent implantation and subsequent dual antiplatelet therapy (PRECISE-DAPT) score: a pooled analysis of individual-patient datasets from clinical trials. Lancet 2017;389:1025–1034. [DOI] [PubMed] [Google Scholar]
- 9. Valgimigli M, Costa F, Lokhnygina Y, Clare RM, Wallentin L, Moliterno DJ, Armstrong PW, White HD, Held C, Aylward PE, Van de Werf F, Harrington RA, Mahaffey KW, Tricoci P.. Trade-off of myocardial infarction vs. bleeding types on mortality after acute coronary syndrome: lessons from the Thrombin Receptor Antagonist for Clinical Event Reduction in Acute Coronary Syndrome (TRACER) randomized trial. Eur Heart J 2017;38:804–810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Généreux P, Giustino G, Witzenbichler B, Weisz G, Stuckey TD, Rinaldi MJ, Neumann F-J, Metzger DC, Henry TD, Cox DA, Duffy PL, Mazzaferri E, Yadav M, Francese DP, Palmerini T, Kirtane AJ, Litherland C, Mehran R, Stone GW.. Incidence, predictors, and impact of post-discharge bleeding after percutaneous coronary intervention. J Am Coll Cardiol 2015;66:1036–1045. [DOI] [PubMed] [Google Scholar]
- 11. Kazi DS, Leong TK, Chang TI, Solomon MD, Hlatky MA, Go AS.. Association of spontaneous bleeding and myocardial infarction with long-term mortality after percutaneous coronary intervention. J Am Coll Cardiol 2015;65:1411–1420. [DOI] [PubMed] [Google Scholar]
- 12. Urban P, Mehran R, Colleran R, Angiolillo DJ, Byrne RA, Capodanno D, Cuisset T, Cutlip D, Eerdmans P, Eikelboom J, Farb A, Gibson CM, Gregson J, Haude M, James SK, Kim H-S, Kimura T, Konishi A, Laschinger J, Leon MB, Magee PFA, Mitsutake Y, Mylotte D, Pocock S, Price MJ, Rao SV, Spitzer E, Stockbridge N, Valgimigli M, Varenne O, Windhoevel U, Yeh RW, Krucoff MW, Morice M-C.. Defining high bleeding risk in patients undergoing percutaneous coronary intervention. Circulation 2019;140:240–261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. GUSTO Investigators. An international randomized trial comparing four thrombolytic strategies for acute myocardial infarction. N Engl J Med 1993;329:673–682. [DOI] [PubMed] [Google Scholar]
- 14. Natsuaki M, Morimoto T, Shiomi H, Yamaji K, Watanabe H, Shizuta S, Kato T, Ando K, Nakagawa Y, Furukawa Y, Tada T.. Application of the Academic Research Consortium High Bleeding Risk Criteria in an All-Comers Registry of Percutaneous Coronary Intervention. Circ Cardiovasc Interv 2019;12:e008307. [DOI] [PubMed] [Google Scholar]
- 15. Ueki Y, Bär S, Losdat S, Otsuka T, Zanchin C, Zanchin T, Gragnano F, Gargiulo G, Siontis GCM, Praz F, Lanz J, Hunziker L, Stortecky S, Pilgrim T, Heg D, Valgimigli M, Windecker S, Räber L.. Validation of the Academic Research Consortium for High Bleeding Risk (ARC-HBR) criteria in patients undergoing percutaneous coronary intervention and comparison with contemporary bleeding risk scores. EuroIntervention 2020;16:371–379. [DOI] [PubMed] [Google Scholar]
- 16. Cao D, Mehran R, Dangas G, Baber U, Sartori S, Chandiramani R, Stefanini GG, Angiolillo DJ, Capodanno D, Urban P, Morice M-C, Krucoff M, Goel R, Roumeliotis A, Sweeny J, Sharma SK, Kini A.. Validation of the Academic Research Consortium High Bleeding Risk definition in contemporary PCI patients. J Am Coll Cardiol 2020;75:2711–2722. [DOI] [PubMed] [Google Scholar]
- 17. Grover FL, Vemulapalli S, Carroll JD, Edwards FH, Mack MJ, Thourani VH, Brindis RG, Shahian DM, Ruiz CE, Jacobs JP, Hanzel G, Bavaria JE, Tuzcu EM, Peterson ED, Fitzgerald S, Kourtis M, Michaels J, Christensen B, Seward WF, Hewitt K, Holmes DR Jr; STS/ACC TVT Registry. 2016 Annual Report of the Society of Thoracic Surgeons/American College of Cardiology Transcatheter Valve Therapy Registry. J Am Coll Cardiol 2017;69:1215–1230. [DOI] [PubMed] [Google Scholar]
- 18. Yamamoto M, Watanabe Y, Tada N, Naganuma T, Araki M, Yamanaka F, Mizutani K, Tabata M, Ueno H, Takagi K, Higashimori A, Shirai S, Hayashida K;. OCEAN-TAVI investigators. Transcatheter aortic valve replacement outcomes in Japan: Optimized CathEter vAlvular iNtervention (OCEAN) Japanese multicenter registry. Cardiovasc Revasc Med 2019;20:843–851. [DOI] [PubMed] [Google Scholar]
- 19. Mangieri A, Montalto C, Poletti E, Sticchi A, Crimi G, Giannini F, Latib A, Capodanno D, Colombo A.. Thrombotic versus bleeding risk after transcatheter aortic valve replacement: JACC review topic of the week. J Am Coll Cardiol 2019;74:2088–2101. [DOI] [PubMed] [Google Scholar]
- 20. Shimura T, Yamamoto M, Kano S, Kagase A, Kodama A, Koyama Y, Tsuchikane E, Suzuki T, Otsuka T, Kohsaka S, Tada N, Yamanaka F, Naganuma T, Araki M, Shirai S, Watanabe Y, Hayashida K, Yashima F, Inohara T, Kakefuda Y, Arai T, Yanagisawa R, Tanaka M, Kawakami T, Maekawa Y, Takashi K, Yoshitake A, Iida Y, Yamazaki M, Shimizu H, Yamada Y, Jinzaki M, Tsuruta H, Itabashi Y, Murata M, Kawakami M, Fukui S, Sano M, Fukuda K, Hosoba S, Sato H, Teramoto T, Kimura M, Sago M, Tsunaki T, Watarai S, Tsuzuki M, Irokawa K, Shimizu K, Kobayashi T, Okawa Y, Miyasaka M, Enta Y, Shishido K, Ochiai T, Yamabe T, Noguchi K, Saito S, Kawamoto H, Onishi H, Yabushita H, Mitomo S, Nakamura S, Yamawaki M, Akatsu Y, Honda Y, Takama T, Isotani A, Hayashi M, Kamioka N, Miura M, Morinaga T, Kawaguchi T, Yano M, Hanyu M, Arai Y, Tsubota H, Kudo M, Kuroda Y, Kataoka A, Hioki H, Nara Y, Kawashima H, Nagura F, Nakashima M, Sasaki K, Nishikawa J, Shimokawa T, Harada T, Kozuma K; OCEAN-TAVI Investigators. Impact of the clinical frailty scale on outcomes after transcatheter aortic valve replacement. Circulation 2017;135:2013–2024. [DOI] [PubMed] [Google Scholar]
- 21. Bor WL, Chan Pin Yin DRPP, Brouwer J, Nijenhuis VJ, Peper J, Timmers L, Rensing BJWM, Swaans MJ, Ten Berg JM.. Assessment of the Academic Research Consortium for High Bleeding Risk Criteria in Patients Undergoing TAVR. JACC Cardiovasc Interv 2021;14:1265–1267. [DOI] [PubMed] [Google Scholar]
- 22. Mizutani K, Hara M, Iwata S, Murakami T, Shibata T, Yoshiyama M, Naganuma T, Yamanaka F, Higashimori A, Tada N, Takagi K.. Elevation of B-type natriuretic peptide at discharge is associated with 2-year mortality after transcatheter aortic valve replacement in patients with severe aortic stenosis: insights from a multicenter prospective OCEAN-TAVI (Optimized Transcatheter Valvular Intervention-Transcatheter Aortic Valve Implantation) Registry. J Am Heart Assoc 2017;6:e006112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Brouwer J, Nijenhuis VJ, Delewi R, Hermanides RS, Holvoet W, Dubois CLF, Frambach P, De Bruyne B, van Houwelingen GK, Van Der Heyden JAS, Toušek P, van der Kley F, Buysschaert I, Schotborgh CE, Ferdinande B, van der Harst P, Roosen J, Peper J, Thielen FWF, Veenstra L, Chan Pin Yin DRPP, Swaans MJ, Rensing BJWM, van ’t Hof AWJ, Timmers L, Kelder JC, Stella PR, Baan J, ten Berg JM.. Aspirin with or without clopidogrel after transcatheter aortic-valve implantation. N Engl J Med 2020;383:1447–1457. [DOI] [PubMed] [Google Scholar]
- 24. Nijenhuis VJ, Brouwer J, Delewi R, Hermanides RS, Holvoet W, Dubois CLF, Frambach P, De Bruyne B, van Houwelingen GK, Van Der Heyden JAS, Toušek P, van der Kley F, Buysschaert I, Schotborgh CE, Ferdinande B, van der Harst P, Roosen J, Peper J, Thielen FWF, Veenstra L, Chan Pin Yin DRPP, Swaans MJ, Rensing BJWM, van 't Hof AWJ, Timmers L, Kelder JC, Stella PR, Baan J, Ten Berg JM.. Anticoagulation with or without clopidogrel after transcatheter aortic-valve implantation. N Engl J Med 2020;382:1696–1707. [DOI] [PubMed] [Google Scholar]
- 25. Généreux P, Cohen DJ, Mack M, Rodes-Cabau J, Yadav M, Xu K, Parvataneni R, Hahn R, Kodali SK, Webb JG, Leon MB.. Incidence, predictors, and prognostic impact of late bleeding complications after transcatheter aortic valve replacement. J Am Coll Cardiol 2014;64:2605–2615. [DOI] [PubMed] [Google Scholar]
- 26. Balan P, Zhao Y, Johnson S, Arain S, Dhoble A, Estrera A, Smalling R, Nguyen TC.. The Society of Thoracic Surgery Risk Score as a predictor of 30-day mortality in transcatheter vs surgical aortic valve replacement: a single-center experience and its implications for the development of a TAVR risk-prediction model. J Invasive Cardiol 2017;29:109–114. [PubMed] [Google Scholar]
- 27. Nakamura M, Iijima R.. Implications and characteristics of high bleeding risk in East Asian patients undergoing percutaneous coronary intervention: Start with what is right rather than what is acceptable. J Cardiol 2021;78:91–98. [DOI] [PubMed] [Google Scholar]
- 28. Nakamura M, Kadota K, Nakao K, Nakagawa Y, Shite J, Yokoi H, Kozuma K, Tanabe K, Iijima R, Harada A, Kuroda T, Murakami Y.. High bleeding risk and clinical outcomes in East Asian patients undergoing percutaneous coronary intervention: the PENDULUM registry. EuroIntervention 2021;16:1154–1162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Edwards FH, Cohen DJ, O'Brien SM, Peterson ED, Mack MJ, Shahian DM, Grover FL, Tuzcu EM, Thourani VH, Carroll J, Brennan JM, Brindis RG, Rumsfeld J, Holmes DR Jr; Steering Committee of the Society of Thoracic Surgeons/American College of Cardiology Transcatheter Valve Therapy Registry. Development and validation of a risk prediction model for in-hospital mortality after transcatheter aortic valve replacement. JAMA Cardiol 2016;1:46–52. [DOI] [PubMed] [Google Scholar]
- 30. Iung B, Laouénan C, Himbert D, Eltchaninoff H, Chevreul K, Donzeau-Gouge P, Fajadet J, Leprince P, Leguerrier A, Lièvre M, Prat A, Teiger E, Laskar M, Vahanian A, Gilard M; FRANCE 2 Investigators. Predictive factors of early mortality after transcatheter aortic valve implantation: individual risk assessment using a simple score. Heart 2014;100:1016–1023. [DOI] [PubMed] [Google Scholar]
- 31. Généreux P, Kodali SK, Green P, Paradis J-M, Daneault B, Rene G, Hueter I, Georges I, Kirtane A, Hahn RT, Smith C, Leon MB, Williams MR.. Incidence and effect of acute kidney injury after transcatheter aortic valve replacement using the new valve academic research consortium criteria. Am J Cardiol 2013;111:100–105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Peeraphatdit TB, Nkomo VT, Naksuk N, Simonetto DA, Thakral N, Spears GM, Harmsen WS, Shah VH, Greason KL, Kamath PS.. Long-term outcomes after transcatheter and surgical aortic valve replacement in patients with cirrhosis: a guide for the hepatologist. Hepatology 2020;72:1735–1746. [DOI] [PubMed] [Google Scholar]
- 33. Bendary A, Ramzy A, Bendary M, Salem M.. Transcatheter aortic valve replacement in patients with severe aortic stenosis and active cancer: a systematic review and meta-analysis. Open Heart 2020;7:e001131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Dangas GD, Tijssen JGP, Wöhrle J, Søndergaard L, Gilard M, Möllmann H, Makkar RR, Herrmann HC, Giustino G, Baldus S, De Backer O, Guimarães AHC, Gullestad L, Kini A, von Lewinski D, Mack M, Moreno R, Schäfer U, Seeger J, Tchétché D, Thomitzek K, Valgimigli M, Vranckx P, Welsh RC, Wildgoose P, Volkl AA, Zazula A, van Amsterdam RGM, Mehran R, Windecker S; GALILEO Investigators. A controlled trial of rivaroxaban after transcatheter aortic-valve replacement. N Engl J Med 2020;382:120–129. [DOI] [PubMed] [Google Scholar]
- 35. Kosmidou I, Liu Y, Alu MC, Liu M, Madhavan M, Chakravarty T, Makkar R, Thourani VH, Biviano A, Kodali S, Leon MB.. Antithrombotic therapy and cardiovascular outcomes after transcatheter aortic valve replacement in patients with atrial fibrillation. JACC Cardiovasc Interv 2019;12:1580–1589. [DOI] [PubMed] [Google Scholar]
- 36. De Larochellière H, Puri R, Eikelboom JW, Rodés-Cabau J.. Blood disorders in patients undergoing transcatheter aortic valve replacement: a review. JACC Cardiovasc Interv 2019;12:1–11. [DOI] [PubMed] [Google Scholar]
- 37. Watanabe H, Domei T, Morimoto T, Natsuaki M, Shiomi H, Toyota T, Ohya M, Suwa S, Takagi K, Nanasato M, Hata Y, Yagi M, Suematsu N, Yokomatsu T, Takamisawa I, Doi M, Noda T, Okayama H, Seino Y, Tada T, Sakamoto H, Hibi K, Abe M, Kawai K, Nakao K, Ando K, Tanabe K, Ikari Y, Hanaoka KI, Morino Y, Kozuma K, Kadota K, Furukawa Y, Nakagawa Y, Kimura T; STOPDAPT-2 Investigators. Effect of 1-month dual antiplatelet therapy followed by clopidogrel vs 12-month dual antiplatelet therapy on cardiovascular and bleeding events in patients receiving PCI: the STOPDAPT-2 randomized clinical trial. JAMA 2019;321:2414–2427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Costa F, Van Klaveren D, Feres F, James S, Räber L, Pilgrim T, Hong MK, Kim HS, Colombo A, Steg PG, Bhatt DL, Stone GW, Windecker S, Steyerberg EW, Valgimigli M;. PRECISE-DAPT Study Investigators. Dual antiplatelet therapy duration based on ischemic and bleeding risks after coronary stenting. J Am Coll Cardiol 2019;73:741–754. [DOI] [PubMed] [Google Scholar]
- 39. Kang J, Park KW, Palmerini T, Stone GW, Lee MS, Colombo A, Chieffo A, Feres F, Abizaid A, Bhatt DL, Valgimigli M, Hong MK, Jang Y, Gilard M, Morice MC, Park DW, Park SJ, Jeong YH, Park J, Koo BK, Kim HS.. Racial differences in ischaemia/bleeding risk trade-off during anti-platelet therapy: individual patient level landmark meta-analysis from seven RCTs. Thromb Haemost 2019;119:149–162. [DOI] [PubMed] [Google Scholar]
- 40. Shen AY, Yao JF, Brar SS, Jorgensen MB, Chen W.. Racial/ethnic differences in the risk of intracranial hemorrhage among patients with atrial fibrillation. J Am Coll Cardiol 2007;50:309–315. [DOI] [PubMed] [Google Scholar]
- 41. Yamaguchi T. Optimal intensity of warfarin therapy for secondary prevention of stroke in patients with nonvalvular atrial fibrillation: a multicenter, prospective, randomized trial. Japanese nonvalvular atrial fibrillation-embolism secondary prevention cooperative study group. Stroke 2000;31:817–821. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data underlying this paper cannot be shared publicly because [the data can only be provided to institutions approved by the Ethics Committee]. Upon reasonable request to the corresponding author, the data will be shared.