Highlights
-
•
Nanocomplexes of siRNA can be nebulized using a miniaturizable acoustomicrofluidic nebulization device.
-
•
An aerosol mist consisting of siRNA-loaded droplets with aerodynamic diameter of approximately 3 µm is produced.
-
•
The siRNA remains intact and functional; able to knockdown the luciferase gene in model lung epithelial cells.
Keywords: Surface acoustic waves, Nebulizer, Lung delivery, siRNA, Nanoparticles
Abstract
The local delivery of therapeutic small interfering RNA or siRNA to the lungs has the potential to improve the prognosis for patients suffering debilitating lung diseases. Recent advances in materials science have been aimed at addressing delivery challenges including biodistribution, bioavailability and cell internalization, but an equally important challenge to overcome is the development of an inhalation device that can deliver the siRNA effectively to the lung, without degrading the therapeutic itself. Here, we report the nebulization of siRNA, either naked siRNA or complexed with polyethyleneimine (PEI) or a commercial transfection agent, using a miniaturizable acoustomicrofluidic nebulization device. The siRNA solution could be nebulised without significant degradation into an aerosol mist with tunable mean aerodynamic diameters of approximately 3 µm, which is appropriate for deep lung deposition via inhalation. The nebulized siRNA was tested for its stability, as well as its toxicity and gene silencing properties using the mammalian lung carcinoma cell line A549, which demonstrated that the gene silencing capability of siRNA is retained after nebulization. This highlights the potential application of the acoustomicrofluidic device for the delivery of efficacious siRNA via inhalation, either for systemic delivery via the alveolar epithelium or local therapeutic delivery to the lung.
1. Introduction
Many human diseases, including cancer, are caused by the overproduction of normal proteins, or the production of abnormal and harmful proteins. The discovery of RNA interference (RNAi) emerged as a promising therapeutic approach to stop the production of disease-causing proteins by specifically silencing the genes encoding the target protein [1]. Using small strands of ribonucleic acid (RNA) or small interfering RNA (siRNA), gene silencing is achieved when the siRNA reaches the cytoplasm and binds its complementary mRNA, which is then degraded by the appropriate cellular RNAi mechanism [2], [3], [4]. In principle, nearly every gene in the body can be targeted for silencing by RNAi. After more than two decades of research to address poor tissue delivery and siRNA stability, the translation of siRNA-based therapeutics to the clinic has been realized with three agents now approved by the US Food and Drug Administration and many others in clinical development [5].
While most of the research has focused on improving the delivery of siRNA using novel carrier materials or modification techniques, the method of administration or route of delivery of the therapeutic is equally important. Pulmonary delivery, in particular, provides a route for both systemic and local delivery of siRNA [6], [7]. The lungs have a large surface area, with the thin alveolar epithelium permitting access to a vast network of blood vessels for rapid drug absorption and high bioavailability, while bypassing first-pass metabolism. Alternatively, local delivery to the lungs provides a targeted approach for the treatment of pulmonary diseases that would benefit from the high drug concentration at the target site, reduced side effects and reduced siRNA degradation that would otherwise be prevalent in the systemic circulation. Potential applications for the targeted delivery of siRNA to the lungs are for the treatment of lung cancer, cystic fibrosis, inflammation, and infectious diseases, including tuberculosis.
Various groups have investigated the pulmonary delivery of siRNA, both in vitro and in vivo [8], [9]. A number of earlier works have used intranasal administration as the route for pulmonary delivery, including siRNA targeted against influenza [10] and respiratory syncytial virus (RSV) [11] in mice. Intratracheal administration was used in monkeys to study the pulmonary delivery of siRNA against severe acute respiratory syndrome (SARS) [12]. However, intranasal success in mice might not equate to success in humans as the breathing pattern and lung morphology differ considerably between the two species. Moreover, intratracheal administration is hardly an option for patients due to its intrusive nature. Advancement in existing technologies for administering pulmonary drugs, including nebulizers, metered-dose inhalers, and dry powder inhalers, to allow the delivery of large macromolecular drugs without aggregation, denaturation or device blockage, would therefore be key to a more patient-friendly approach to the pulmonary delivery of siRNA therapeutics.
Clinical trials for the treatment of RSV using inhaled siRNA (now discontinued) was initiated by Alnylam Pharmaceutics in 2006 using a nebulizer, which have many advantages over metered-dose and dry powder inhalers. Less complex formulation is needed for nebulizers compared to a dry powder inhaler, although significant efforts have been made in the preparation and characterization of dry powder siRNA formulations. The active aerosolization mechanism of nebulizers involves an external energy source that could allow for control of delivery, as well as negating the need for hand-breath coordination, which is the main source of patient misuse and poor compliance, particularly among children and elderly patients [13], [14].
Despite their appeal, there is room for improvement in the technological design of nebulizers, which include jet nebulizers, ultrasonic nebulizers, and the vibrating mesh nebulizer. Portability remains an issue with jet nebulizers, which can also suffer from delivery inefficiency with reports of only ∼12% delivered dose reaching the lung [15], [16]. Modern ultrasonic nebulizers have become more portable, but suffer from the susceptibility of macromolecular drugs to denature under the large cavitation [17], [18], [19] and hydrodynamic shear forces induced by the piezoelectric crystal-driven nebulization process [13], [14]. There is reduced shear stress created with vibrating mesh nebulizers, which nebulize formulations through a vibrating array of microorifices, but they are expensive and are susceptible to clogging.
An aerosol technology we are investigating for the nebulization of therapeutics is the Respite platform, which utilizes surface acoustic waves (SAW) to drive nebulization [20], [21], [22]. Surface acoustic waves (SAW), which are 10 MHz order Rayleigh waves, are a type of acoustic wave with displacement amplitudes in the nanometre range that propagates along the surface of a single-crystal piezoelectric substrate such as lithium niobate (LiNbO3 or LN). Since the wave is rapidly attenuated with increasing depth into the substrate, the energy is confined to the substrate surface. Hence, when a SAW encounters a liquid placed upon the substrate, it diffuses into it at an angle of 22°, which is known as the Rayleigh angle. When enough power is applied in the form of an electrical signal via interdigital transducer (IDT) electrodes that are patterned using photolithography techniques on the LN surface, the energy diffuses into the liquid, inducing capillary waves on the free surface of the liquid. At high enough power, the interface rapidly destabilizes, leading to the atomization of the liquid drop into a fine mist suitable for inhalation [23].
The use of SAWs in the telecommunications industry is widespread, and in microfluidics, SAWs have been utilized to manipulate fluids to induce effects including pumping, jetting and mixing [6], [24], [25], [26]. The application of SAWs in the nebulization of therapeutics for pulmonary delivery is of great interest as it can be miniaturized into a low-cost, portable system powered by camera batteries due to the small dimensions of the piezoelectric chip and its efficiency in driving nebulization [27], [28], [29], [30], [31], [32], [33], [34]. Furthermore, the size of the droplets generated using SAWs are within the size range suitable for deep lung delivery (between 1 μm and 5 μm) and can be tuned by adjusting the physical properties of the liquid [23] and the input power to the device [35]. Qi et al showed that the nebulization of the asthma drug salbutamol using this device resulted in a mean aerosol size of ∼3 μm using dynamic light scattering (DLS), with approximately 80% of the drug reaching the lung, as determined through a twin-stage lung model [30].
Unlike conventional ultrasonic nebulizers, which typically run at 100 kHz order frequencies and require powers of 10 W and above, the 10 MHz order frequencies and low power (∼2–3 W) associated with the SAW nebulizer suppresses the large shear and cavitational damage inflicted on biomolecules suspended in the liquid [13], [14], [36]. As such, this makes the SAW nebulizer, and its high nebulization rate hybrid acoustic wave counterpart (HYDRA) [37], attractive candidates for the pulmonary delivery of clinically significant large macromolecules. This has been demonstrated in the SAW nebulization of biomolecules, including DNA, peptides, proteins (e.g., monoclonal antibodies and lytic enzymes), and even stem cells which showed no appreciable degradation and retained biological function after nebulization [20], [21], [22], [33], [38], [39], [40], [41], [42].
Here, we investigate the use of the SAW nebulizer for the pulmonary delivery of siRNA. At 13–15 kDa or approximately 19–23 bp in length, the siRNA duplex is relatively large compared with small molecular weight pulmonary drugs. It is particularly susceptible to hydrolysis/degradation by nucleases due to the presence of a hydroxyl group in the 2′-position of the ribose in the RNA backbone. It is also highly negatively charged, which presents a barrier to the internalization of naked or free siRNA by cells, which are also negatively charged. As a result, the structure of siRNA is often chemically modified, or the siRNA packaged within cationic vectors to improve its stability and to facilitate intracellular delivery. As proof of principle, we used siRNA against firefly luciferase in this work as the model target protein, although this could easily apply to other siRNA targeted against proteins implicated in lung diseases. The properties of the nebulized aerosols of free siRNA, as well as siRNA complexed with transfection vectors were characterized. Moreover, the stability and gene silencing activity of nebulized siRNA were investigated to demonstrate the potential application of the SAW nebulization platform for the efficient pulmonary delivery of siRNA.
2. Materials and methods
2.1. Materials
Luciferase GL2 siRNA duplex was purchased from Dharmacon (Millenium Science, Mulgrave, VIC, Australia). The Steady-Glo Luciferase assay system was from Promega Corporation (Alexandria, NSW, Australia). Dulbecco’s Modified Eagle Medium (DMEM), heat-inactivated fetal bovine serum (HI-FBS), Ultrapure water, 10x phosphate buffered saline (PBS), 0.25% Trypsin-Ethylenediaminetetraacetic acid (EDTA), 10x Tris/Borate/EDTA buffer, Alamar Blue cell viability reagent, Ultrapure TEMED and SYBR Safe DNA Gel stain were from Life Technologies Pty. Ltd. (Mulgrave, VIC, Australia). Linear PEI, 25,000 g mol−1, was from Polysciences Inc. (Warrington, PA, USA). INTERFERin transfection agent was from Polyplus transfection via VWR International (Murarrie, QLD, Australia). The siRNA molecular weight ladder was from New England Biolabs (Genesearch Pty. Ltd., Arundel, QLD, Australia). Acylamide/Bis 40% (w/v) and ammonium persulfonate (APS) were from Sigma Aldrich LLC (Castle Hill, NSW, Australia). A549 cells, a human lung carcinoma cell line, were also from Sigma Aldrich. A549-luc-C8, which are A549 cells stably expressing firefly luciferase, were from Perkin Elmer via Thermo Fisher Scientific (Scoresby, VIC, Australia). Cells were grown in DMEM supplemented with 10% HI-FBS in a humidified 37 °C incubator with 5% CO2.
2.2. SAW device fabrication
The SAW nebulizer device was fabricated as described elsewhere [43], [44]. Briefly, a focused interdigital transducer (IDT) was patterned by sputtering aluminium (1.5 µm thickness, NanochromeTM II electron beam evaporation system, Intlvac, Niagara Falls, NY) and chromium (5 nm thickness) onto a clean 128° Y-cut X-propagating lithium niobate (LiNbO3) piezoelectric substrate (Roditi, London UK), followed by standard UV photolithography and wet etching.
2.3. SAW nebulization of siRNA and siRNA/carrier complexes
Naked siRNA (10 µM) was prepared in 25 mM sodium acetate buffer, pH 5.2. Complexes of siRNA with PEI (1 mg mL−1 in MilliQ), were prepared at N/P ratios 30, 60 and 90, where N refers to nitrogen residues in PEI and P refers to the phosphate in siRNA, in 25 mM sodium acetate buffer, pH 5.2. Complexes of siRNA with INTERFERin were prepared at 1:1, 1:2 and 1:4 ratios of siRNA to INTERFERin, according to the manufacturer’s instructions. The degree of complexation at each ratio and the stability of the nebulized free or complexed siRNA were determined by native gel electrophoresis using a 10% polyacrylamide gel. Samples were run alongside a siRNA standard molecular weight marker and at 100 mV for 60 min. Gels were stained with SybrSafe and imaged using a Gel Doc imaging system (Bio-Rad Laboratories Pty. Ltd., Hercules, CA).
Nebulization of naked siRNA and complexes were carried out inside a 50 mL Falcon tube to allow for the condensation and collection of the nebulized mist for analysis. Formulations were fed to the device via a glass capillary tube (ID 1.5 mm) with a wick of polyester/cellulose cleanroom paper at the end, which provided a thin film of fluid at the focused edge of the SAW device to facilitate effective nebulization (see Fig. 1). A high frequency (29.78 MHz) electrical signal, and input power of <2 W was supplied to the IDT to generate the propagating SAW to drive nebulization of the liquid feed. Note that when handling siRNA, care was taken to minimize enzymatic degradation by RNase, by using RNase-free solutions and consumables where possible, wearing gloves, and ensuring a clean working space decontaminated with RNaseZap (ThermoFisher).
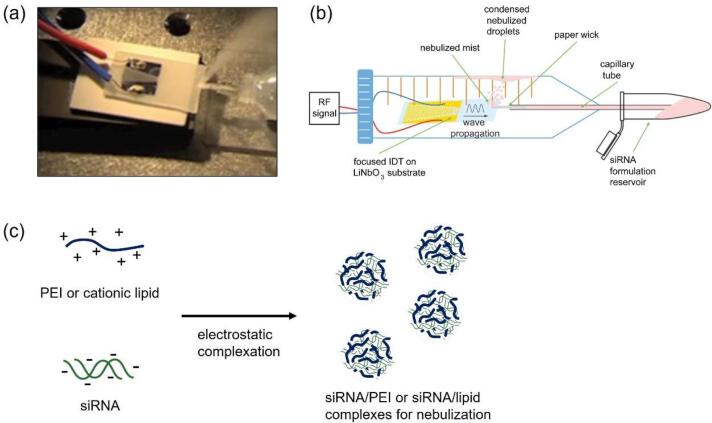
Fig. 1.
(a) Nebulization of a liquid siRNA formulation using a microfabricated SAW device consisting of a focused IDT electrode photolithographically patterned onto a single crystal piezoelectric (lithium niobate; LiNbO3) substrate. Power in the form of an oscillating electrical signal is supplied, leading to the generation and propagation of SAW, which causes the siRNA formulation to be drawn from the vial through a capillary tube and paper wick in contact with the substrate. Above a threshold power, the liquid meniscus, which forms as a consequence, is destabilized and nebulized into a fine aerosol mist suitable for inhalation. (b) Schematic depiction of the experimental mist collection setup within a 50 mL centrifugal tube. (c) Schematic representation of the complexation of siRNA with polyethyleneimine (PEI) or a cationic lipid for siRNA delivery.
2.4. Characterization of complexes in terms of size and zeta potential
The siRNA complexes were characterized in terms of size by dynamic light scattering (DLS), and zeta-potential by microelectrophoresis using a Malvern ZS Nanosizer (Malvern Instruments, Malvern, UK). Measurements for both DLS and microelectrophoresis were carried out in triplicates in 25 mM sodium acetate buffer, pH 5.2.
2.5. Aerosol characterization
The aerosol mist was characterized in terms of its droplet size distribution by laser diffraction (Spraytec, Malvern Instruments, Malvern, UK). Nebulization was performed with 1.6 W power supplied to the device. Measurements were carried out without a vacuum driven exhaust, at about 2–3 cm from the base of the mist. The aerosol diameters reported represent the median particle size (Dv50) from a volume-based size distribution.
2.6. Transfection with nebulized siRNA
Luciferase-expressing A549-luc cells were grown to 90% confluency, detached with trypsin/EDTA, then seeded in 96-well plates at 5000 cells per well 24 h prior to transfection. On the day of transfection, the media was replaced with fresh growth medium and then nebulized or non-nebulized naked siRNA, siRNA/PEI complexes or siRNA/INTERFERin complexes were added to the cells in quadruplicates to give an equivalent of 3 pmol siRNA per well. The plates were incubated at 37 °C, and after 4 h, the medium was replaced with fresh growth medium. Cells were grown over 48 h with one media change at 24 h. Luciferase activity in cells was measured using the Steady-Glo assay according to the manufacturer’s instructions, and luminescence measured using a microplate reader with luminescence capability (BioTek Synergy HTX, Winooski, VT, USA).
2.7. Cell viability assay
Cells were treated as per transfection protocol above. After 4 h incubation with the siRNA or complexes, the media was replaced with fresh media and incubated overnight. Alamar Blue reagent was added at a 1:10 (reagent:media) ratio as described in the protocol and plates incubated at 37 °C for 2 h. The fluorescence at 590 nm was measured using a standard microplate fluorometer (BioTek Synergy).
3 Results. and discussion
3.1. Effect of SAW nebulization on siRNA stability
The nanofabricated SAW nebulization device is shown in Fig. 1a. Nebulization of siRNA formulations was carried out inside 50 mL Falcon tubes, as shown schematically in Fig. 1b, to allow for the collection, via centrifugation, of the mist that condenses on the walls for analysis. Liquid formulations of siRNA make suitable reservoirs for nebulization using the SAW device. The siRNA could either be in its free form, but naked siRNA is prone to hydrolysis by nucleases and so it is often chemically modified or packaged into compact complexes with cationic molecules to improve its stability. In this work, PEI and a commercial transfection agent INTERFERin were used to form complexes with siRNA (Fig. 1c). PEI is a strongly positively charged polymer and is well studied for its ability to form stable complexes with negatively charged nucleic acids, including plasmid DNA, antisense RNA and siRNA. INTERFERin is a lipid-based transfection agent, marketed for its ability to effectively transfect A549 lung carcinoma cells. The complexation of siRNA with PEI and INTERFERin was first studied using polyacrylamide gel electrophoresis. To determine the ratio at which stable complexes were formed, complexes at various ratios of nitrogen to phosphate (N:P) were prepared and ran through a 10% polyacrylamide gel. For PEI, N:P ratio of above 30 was found to be effective in forming complexes as shown by the retardation of the siRNA band on the gel (Figure S1). For INTERFERin, a ratio of 1:1 (suggested manufacturer INTERFERin:siRNA ratio) was sufficient for siRNA to be complexed into particles, as demonstrated by the absence of the free siRNA band on the gel (not shown). The addition of heparin, a strongly negatively charged molecule that can compete for binding with the siRNA, releases the siRNA from the complexes as shown on the gel (Figure S2), confirming the presence of complexes at the N/P ratios studied.
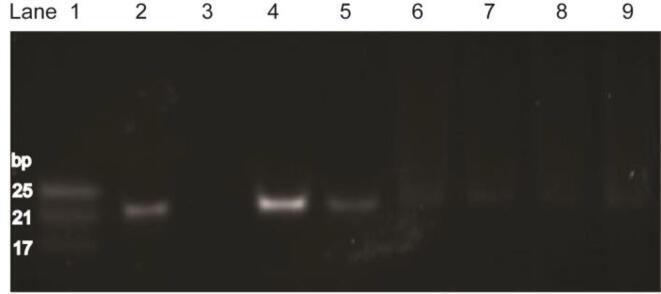
Formulations of siRNA were nebulized at powers not exceeding 2 W. Fig. 2 shows the effect of SAW nebulization on the stability of siRNA. When compared to the migration of the siRNA marker and non-nebulized siRNA, the gel shows, within the resolution of the gel imaging camera, negligible degradation of the nebulized siRNA, either in its naked free form or complexed with PEI. This suggests the potential for delivering intact siRNA within the droplets generated from the SAW device.
Fig. 2.
Native polyacrylamide gel electrophoresis (PAGE) of both nebulized and non-nebulized siRNA and PEI:siRNA complexes. Lane 1: siRNA ladder showing 25, 21 and 17 bp duplex markers; Lane 2: nebulized free siRNA; Lane 3: nebulized PEI; Lane 4: non-nebulized PEI:siRNA complexes at N:P of 1; Lane 5: nebulized PEI:siRNA complexes at N:P of 1; Lane 6: non-nebulized PEI:siRNA complexes at N:P of 30; Lane 7: nebulized PEI:siRNA complexes at N:P of 30; Lane 8: non-nebulized PEI:siRNA complexes at N:P of 60; Lane 9: nebulized PEI:siRNA complexes at N:P of 60.
3.2. Effect of SAW nebulization on particle size
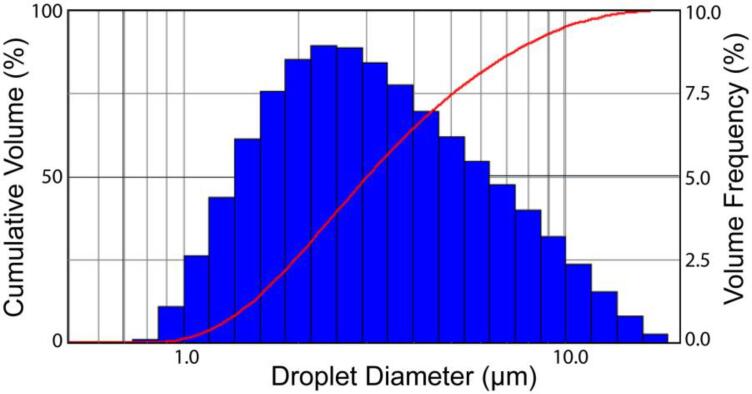
The aerodynamic size of the aerosol droplets determines their localization within the respiratory tract [45], [46]. Larger droplets > 5 μm tend to localize in the upper respiratory tract, depositing in the nose and throat upon inhalation, whereas very small droplets <1 μm are typically exhaled. It is widely accepted that aerosols of aerodynamic size 1 to 5 μm are ideal for pulmonary delivery as they are able to navigate the highly-branched network of the airways to reach the alveolar region in the deep lung, where systemic access to the body is possible [47]. At this size range, inertial impaction is low and gravitational sedimentation effects circumvent proximal airway deposition [48], [49], [50]. The results from the aerosol size measurements using laser diffraction (in the absence of a vacuum-driven inhalation cell attachment) in Fig. 3 indicate that aerosols generated using the SAW nebulizer in the presence of the siRNA have a mean diameter D of approximately 2.7 μm (based on the volume median diameter Dv50) at an input power to the device of 1.6 W. Given that the density ρ of the siRNA solution at these low concentrations is similar to the density of water, this translates into a corresponding aerodynamic diameter Da = (ρ/ρ0)1/2D of approximately 2.7 μm with ρ0 being the standard particle density (1 g cm−3). This value, given the absence of an inhalation cell attachment, exhibits the real-time aerosol sizes as the mist propagates from the device. The final size of the nebulized droplets may be influenced by a number of factors, including the resulting liquid formulation, which could be influenced by the presence of excipients and the nucleic acid concentration affecting the physical properties of the liquid. During inhalation, condensation and evaporation effects could also shift the size range of aqueous droplets [51], [52]. Previous studies with the SAW device have also indicated the tunability of droplet size as a function of input power, with the size of the droplets increasing with the magnitude of power supplied. Conversely, reduction in the aerosol size can be achieved by tuning the wettability of the substrate so as to decrease the aspect ratio of the liquid body on the substrate that is nebulized [23], [35]. Ultimately, the area of the lung where the aerosol droplets deposit will depend not only on the aerosol size, but also the inhalation or inspiration technique of the patient [47], [53]. Once deposited on the lung surface, the size and other physicochemical properties of the particles (e.g., surface charge and composition, rigidity) can become important for intracellular delivery [54], as assessed in the next section.
Fig. 3.
Volume-based droplet size (column) and cumulative size (solid curve) distribution obtained from the SAW nebulization of a liquid siRNA formulation, as measured by laser diffraction.
3.3. Characterization of nebulized complexes
The effect of nebulization on the size and zeta potential of the siRNA:PEI complexes was measured using dynamic light scattering and microelectrophoresis, respectively. Table 1 shows that the size of siRNA:PEI complexes at N:P ratios 30, 60 and 90 did not vary after nebulization. The zeta potential, which is indicative of the overall charge of the particle complex, was also not affected by nebulization (Table 1), with the particles retaining a net positive charge that is beneficial for the interaction of the complexes with cells in vitro. With complexes of size approximately 180 nm within 3 μm aerosol droplets, the results imply that the complexes do not unravel nor are they degraded as a result of nebulization. The slight heat that may be produced at the point of atomization also has negligible effect on the properties of the complexes or naked siRNA itself. The size of the INTERFERin/siRNA complexes was measured (Table S1) and the complexes, at INTERFERin/siRNA ratios of 1:1, 2:1 and 3:1, are within the size (approximately 450–620 nm) suitable for cellular uptake and encapsulation in 3 μm aerosol droplets.
Table 1.
Characterization of nebulized and non-nebulized PEI/siRNA complexes in terms of size and zeta potential.
| Sizea (nm) |
Zeta potentialb (mV) |
|||
|---|---|---|---|---|
| Non-nebulized | Nebulized | Non-nebulized | Nebulized | |
| PEI:siRNA N:P 30 | 100 | 94 | 29 | 31 |
| PEI:siRNA N:P 60 | 185 | 188 | 22 | 25 |
| PEI:siRNA N:P 90 | 181 | 186 | 30 | 30 |
aMeasured using dynamic light scattering. In 25 mM sodium acetate, pH 5.2.
bMeasured by microelectrophoresis, in 25 mM sodium acetate, pH 5.2.
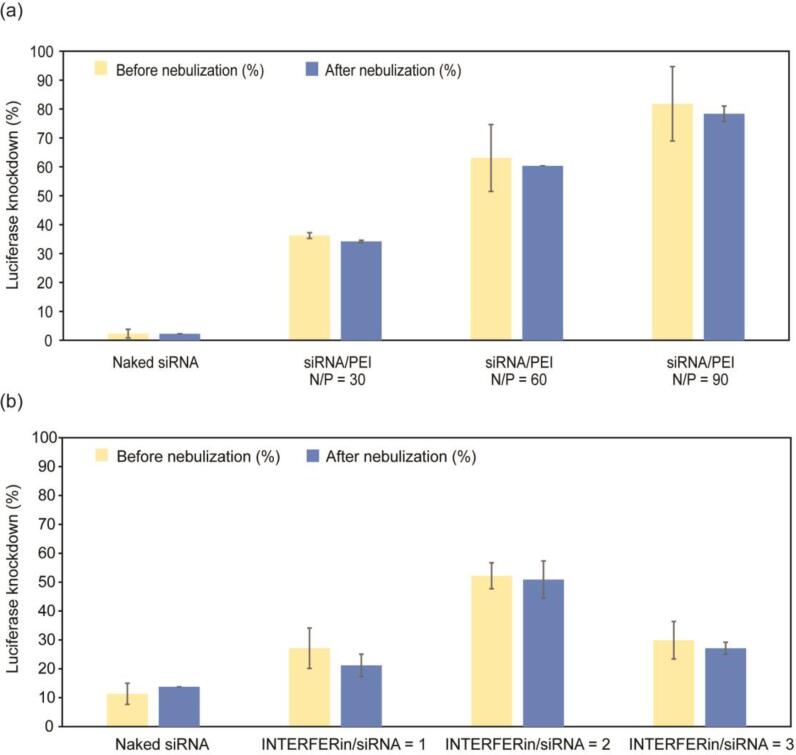
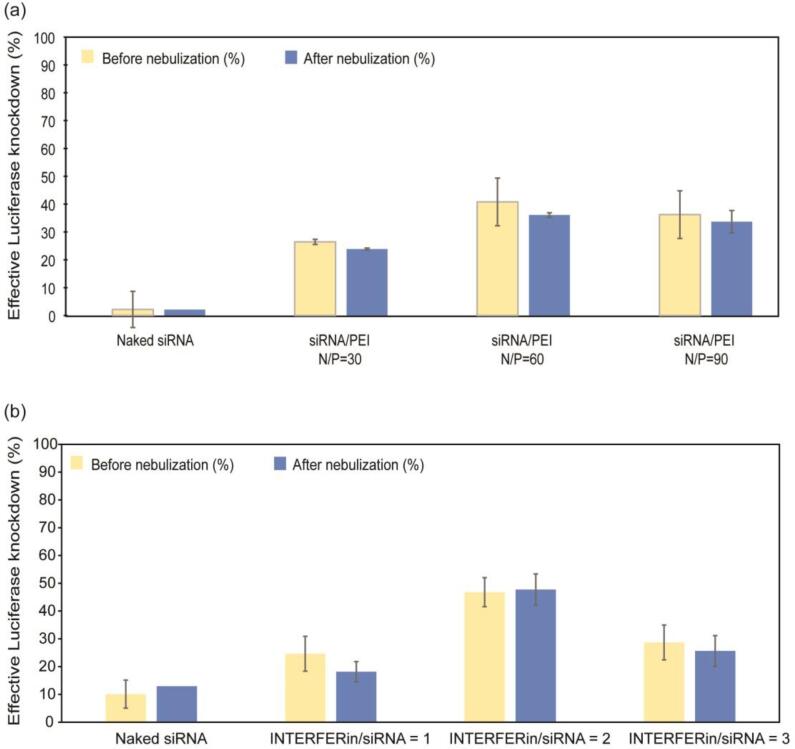
3.4. Effect of SAW nebulization on siRNA activity
While gel electrophoresis confirmed that nebulized siRNA remained intact, it was equally important that the siRNA retained its biological activity or its gene silencing capability post nebulization. To test this, siRNA was complexed with PEI and INTERFERin to mediate transfection in A549 cells, which are human lung carcinoma cells. As proof of principle, siRNA against firefly luciferase was nebulized and its gene silencing capability tested using modified A549 cells that stably express the firefly luciferase gene (A459-luc). Fig. 4 shows the gene knockdown from luciferase siRNA complexed with PEI (Fig. 4a) and INTERFERin (Fig. 4b). The data shows increasing gene knockdown as the N:P ratio of PEI to siRNA increases, with up to 80% knockdown at N:P 90. However, from a study of the concurrent viability of the cells using Alamar Blue viability assay, a portion of the knockdown can be attributed to cell death, with decreasing cell viability observed at increasing N:P ratio (Figure S2a). The cytotoxicity of 25 kDa PEI is a major drawback for the clinical use of PEI as a transfection agent for gene therapy applications. Commercially available transfection agent INTERFERin was also used to complex siRNA at ratios recommended by the manufacturer. Luciferase knockdown of up to 50% was obtained at INTERFERin:siRNA ratio of 2:1. While generally lower knockdown was obtained with INTERFERin compared with PEI, the INTERFERin was less cytotoxic than PEI, with a cell viability of 93% at ratio 2:1 (Figure S2b). Therefore, taking into consideration the toxicity of the transfection agents, which would otherwise contribute to the apparent gene knockdown, the effective luciferase knockdown from nebulized versus non-nebulized siRNA complexes are shown in Fig. 5. INTERFERin complexed with siRNA at 2:1 ratio showed the most knockdown with approximately 47% reduction in luciferase protein production.
Fig. 4.
Luciferase gene knockdown from naked siRNA and siRNA complexed with cationic PEI (a) or INTERFERin (b) at various ratios. Cells were incubated with nebulized or non-nebulized siRNA samples and incubated for 48 h at 37 °C with 5% CO2 prior to measurement of luciferase expression by luminescence. Luciferase expression or knockdown has been normalized according to the luminescence of untreated cells.
Fig. 5.
Effective luciferase gene knockdown from naked siRNA and siRNA complexed with cationic PEI (a) or INTERFERin (b) at various ratios, after normalizing against the corresponding viability of treated cells. Luciferase expression or knockdown has been normalized according to the luminescence of untreated cells.
These results suggest that complexed siRNA within the aerosol droplets emitted from the acoustomicrofluidic device remains biologically active and can cause gene silencing. The limiting factor lies mainly with the transfection agent, which suggests the need for better transfection agents that would deliver siRNA to the cell cytoplasm effectively, without toxicity. There is active research into materials for gene therapy applications and the potential for these complexes to be designed precisely for lung delivery is immense. Apart from the size of the aerosol droplet that could determine its localization within the respiratory system, the precise design of the particle complex, which was outside the scope of our study, could prove significant to improve interaction with target cells within the respiratory system, using strategies including active targeting and muco-penetration [55], [56], [57], [58]. In particular, given the clinical success of lipid-based nanoparticles in vaccination and chemotherapy, for example, strategies to deliver therapeutics to the lungs using lipid-based systems have attracted considerable interest [59], [60], [61].
4. Conclusion
A SAW-based nebulization platform was investigated for its potential to deliver siRNA via the inhalation route. Nebulization of a liquid siRNA formulation produced aerosol droplets of mean aerodynamic diameter of 2.7 μm, which is within the range (1–5 μm) suitable for pulmonary delivery. Analysis of the nebulized siRNA by gel electrophoresis showed negligible degradation of the 21 bp nucleic acid duplex during the nebulization process. When complexed with PEI or a cationic lipid, the resulting particulate retained its size and zeta potential after nebulization. Importantly, the siRNA within the complexes retained their biological activity and were able to induce luciferase gene knockdown in luciferase-expressing A549 lung carcinoma cells. Improvements in the microfluidics and circuitry of the SAW device could enable simultaneous synthesis and delivery of siRNA poly- or lipoplexes in situ, within a low-cost, portable system for lung delivery. Moreover, the process of drug formulation becomes far simpler than with metered dose inhalers and dry particle inhalers devices that, by themselves are very simple, yet belie the years of effort and costs required in formulating the dry particles they deliver.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgments
CCJ acknowledges funding through an Australian Research Council (ARC) Super Science Fellowship through grant FS100100073. CCJ also acknowledges the Melbourne Centre for Nanofabrication for a Technology Fellowship. JRF is grateful to the Melbourne Centre for Nanofabrication for a Senior Technology Fellowship and RMIT University for a Vice-Chancellor’s Senior Research Fellowship. LYY acknowledges support for an ARC Future Fellowship through grant FT130100672. The work was also supported in part by ARC Discovery grants DP1092955, DP120100013 and DP120100835. This work was performed in part at the Melbourne Centre for Nanofabrication (MCN) in the Victorian Node of the Australian National Fabrication Facility (ANFF).
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ultsonch.2022.106088.
Contributor Information
Christina Cortez-Jugo, Email: ccortez@unimelb.edu.au.
Leslie Yeo, Email: leslie.yeo@rmit.edu.au.
Appendix A. Supplementary data
The following are the Supplementary data to this article:
References
- 1.Fire A., Xu S., Montgomery M.K., Kostas S.A., Driver S.E., Mello C.C. Potent and specific genetic interference by double-stranded RNA in Caenorhabditis elegans. Nature. 1998;391:806–811. doi: 10.1038/35888. [DOI] [PubMed] [Google Scholar]
- 2.Bumcrot D., Manoharan M., Koteliansky V., Sah D.W. RNAi therapeutics: a potential new class of pharmaceutical drugs. Nat. Chem. Biol. 2006;2:711–719. doi: 10.1038/nchembio839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Elbashir S.M., Harborth J., Lendeckel W., Yalcin A., Weber K., Tuschl T. Duplexes of 21-nucleotide RNAs mediate RNA interference in cultured mammalian cells. Nature. 2001;411:494–498. doi: 10.1038/35078107. [DOI] [PubMed] [Google Scholar]
- 4.Whitehead K.A., Langer R., Anderson D.G. Knocking down barriers: advances in siRNA delivery. Nat. Rev. Drug Discov. 2009;8:129–138. doi: 10.1038/nrd2742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zhang M.M., Bahal R., Rasmussen T.P., Manautou J.E., Zhong X.-B. The growth of siRNA-based therapeutics: updated clinical studies. Biochem. Pharmacol. 2021;189 doi: 10.1016/j.bcp.2021.114432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ding X., Li P., Lin S.-C.-S., Stratton Z.S., Nama N., Guo F., Slotcavage D., Mao X., Shi J., Costanzo F. Surface acoustic wave microfluidics. Lab Chip. 2013;13:3626–3649. doi: 10.1039/c3lc50361e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lam J.-K.-W., Liang W., Chan H.-K. Pulmonary delivery of therapeutic siRNA. Adv. Drug. Deliv. Rev. 2012;64:1–15. doi: 10.1016/j.addr.2011.02.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Dahlman J.E., Barnes C., Khan O., Thiriot A., Jhunjunwala S., Shaw T.E., Xing Y., Sager H.B., Sahay G., Speciner L., Bader A., Bogorad R.L., Yin H., Racie T., Dong Y., Jiang S., Seedorf D., Dave A., Sandu K.S., Webber M.J., Novobrantseva T., Ruda V.M., Lytton-Jean A.K.R., Levins C.G., Kalish B., Mudge D.K., Perez M., Abezgauz L., Dutta P., Smith L., Charisse K., Kieran M.W., Fitzgerald K., Nahrendorf M., Danino D., Tuder R.M., von Andrian U.H., Akinc A., Schroeder A., Panigrahy D., Kotelianski V., Langer R., Anderson D.G. In vivo endothelial siRNA delivery using polymeric nanoparticles with low molecular weight. Nat. Nanotechnol. 2014;9:648–655. doi: 10.1038/nnano.2014.84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Merkel O.M., Rubinstein I., Kissel T. siRNA delivery to the lung: what's new? Adv. Drug. Deliv. Rev. 2014;75:112–128. doi: 10.1016/j.addr.2014.05.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Tompkins S.M., Lo C.-Y., Tumpey T.M., Epstein S.L. Protection against lethal influenza virus challenge by RNA interference in vivo. Proc. Natl. Acad. Sci. USA. 2004;101:8682–8686. doi: 10.1073/pnas.0402630101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bitko V., Musiyenko A., Shulyayeva O., Barik S. Inhibition of respiratory viruses by nasally administered siRNA. Nat. Med. 2005;11:50–55. doi: 10.1038/nm1164. [DOI] [PubMed] [Google Scholar]
- 12.Li B.-J., Tang Q., Cheng D., Qin C., Xie F.Y., Wei Q., Xu J., Liu Y., Zheng B.-J., Woodle M.C. Using siRNA in prophylactic and therapeutic regimens against SARS coronavirus in Rhesus macaque. Nat. Med. 2005;11:944–951. doi: 10.1038/nm1280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Tonnis W.F., Lexmond A.J., Frijlink H.W., De Boer A.H., Hinrichs W.L. Devices and formulations for pulmonary vaccination. Expert Opin. Drug Deliv. 2013;10:1383–1397. doi: 10.1517/17425247.2013.810622. [DOI] [PubMed] [Google Scholar]
- 14.Yeo L.Y., Friend J.R., McIntosh M.P., Meeusen E.N., Morton D.A. Ultrasonic nebulization platforms for pulmonary drug delivery. Expert Opin. Drug Deliv. 2010;7:663–679. doi: 10.1517/17425247.2010.485608. [DOI] [PubMed] [Google Scholar]
- 15.Lewis R.A., Fleming J.S. Fractional deposition from a jet nebulizer: how it differs from a metered dose inhaler. Br. J. Dis. Chest. 1985;79:361–367. doi: 10.1016/0007-0971(85)90069-5. [DOI] [PubMed] [Google Scholar]
- 16.O'Callaghan C., Barry P.W. The science of nebulised drug delivery. Thorax. 1997;52:S31. doi: 10.1136/thx.52.2008.s31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Taylor K.M., McCallion O.N. Ultrasonic nebulisers for pulmonary drug delivery. Int. J. Pharm. 1997;153:93–104. [Google Scholar]
- 18.Tsai C., Mao R., Lin S., Zhu Y., Tsai S. Faraday instability-based micro droplet ejection for inhalation drug delivery. Technology. 2014;2:75–81. doi: 10.1142/S233954781450006X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Tsai C.S., Mao R.W., Lin S.K., Wang N., Tsai S.C. Miniaturized multiple Fourier-horn ultrasonic droplet generators for biomedical applications. Lab Chip. 2010;10:2733–2740. doi: 10.1039/c005262k. [DOI] [PubMed] [Google Scholar]
- 20.Cortez-Jugo C., Qi A., Rajapaksa A., Friend J.R., Yeo L.Y. Pulmonary monoclonal antibody delivery via a portable microfluidic nebulization platform. Biomicrofluidics. 2015;9 doi: 10.1063/1.4917181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Marqus S., Lee L., Istivan T., Chang R.Y.K., Dekiwadia C., Chan H.-K., Yeo L.Y. High frequency acoustic nebulization for pulmonary delivery of antibiotic alternatives against Staphylococcus aureus. Eur. J. Pharm. Biopharm. 2020;151:181–188. doi: 10.1016/j.ejpb.2020.04.003. [DOI] [PubMed] [Google Scholar]
- 22.Rajapaksa A.E., Ho J.J., Qi A., Bischof R., Nguyen T.-H., Tate M., Piedrafita D., McIntosh M.P., Yeo L.Y., Meeusen E. Effective pulmonary delivery of an aerosolized plasmid DNA vaccine via surface acoustic wave nebulization. Respir. Res. 2014;15:1–12. doi: 10.1186/1465-9921-15-60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Qi A., Yeo L.Y., Friend J.R. Interfacial destabilization and atomization driven by surface acoustic waves. Phys. Fluids. 2008;20 [Google Scholar]
- 24.Destgeer G., Sung H.J. Recent advances in microfluidic actuation and micro-object manipulation via surface acoustic waves. Lab Chip. 2015;15:2722–2738. doi: 10.1039/c5lc00265f. [DOI] [PubMed] [Google Scholar]
- 25.Go D.B., Atashbar M.Z., Ramshani Z., Chang H.-C. Surface acoustic wave devices for chemical sensing and microfluidics: a review and perspective. Anal. Methods. 2017;9:4112–4134. doi: 10.1039/C7AY00690J. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Yeo L.Y., Friend J.R. Surface acoustic wave microfluidics. Annu. Rev. Fluid Mech. 2014;46:379–406. [Google Scholar]
- 27.Guo Y., Dennison A., Li Y., Luo J., Zu X.-T., Mackay C., Langridge-Smith P., Walton A., Fu Y.Q. Nebulization of water/glycerol droplets generated by ZnO/Si surface acoustic wave devices. Microfluid Nanofluidics. 2015;19:273–282. [Google Scholar]
- 28.Ju J., Yamagata Y., Ohmori H., Higuchi T. High-frequency surface acoustic wave atomizer. Sens. Actuator A Phys. 2008;145:437–441. [Google Scholar]
- 29.Kurosawa M., Watanabe T., Futami A., Higuchi T. Surface acoustic wave atomizer. Sens. Actuator A Phys. 1995;50:69–74. [Google Scholar]
- 30.Qi A., Friend J.R., Yeo L.Y., Morton D.A., McIntosh M.P., Spiccia L. Miniature inhalation therapy platform using surface acoustic wave microfluidic atomization. Lab Chip. 2009;9:2184–2193. doi: 10.1039/b903575c. [DOI] [PubMed] [Google Scholar]
- 31.Winkler A., Harazim S., Collins D., Brünig R., Schmidt H., Menzel S. Compact SAW aerosol generator. Biomed. Microdevices. 2017;19:1–10. doi: 10.1007/s10544-017-0152-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Winkler A., Harazim S., Menzel S., Schmidt H. SAW-based fluid atomization using mass-producible chip devices. Lab Chip. 2015;15:3793–3799. doi: 10.1039/c5lc00756a. [DOI] [PubMed] [Google Scholar]
- 33.Alvarez M., Friend J., Yeo L.Y. Rapid generation of protein aerosols and nanoparticles via surface acoustic wave atomization. Nanotechnology. 2008;19 doi: 10.1088/0957-4484/19/45/455103. [DOI] [PubMed] [Google Scholar]
- 34.Friend J.R., Yeo L.Y., Arifin D.R., Mechler A. Evaporative self-assembly assisted synthesis of polymeric nanoparticles by surface acoustic wave atomization. Nanotechnology. 2008;19 doi: 10.1088/0957-4484/19/14/145301. [DOI] [PubMed] [Google Scholar]
- 35.Collins D.J., Manor O., Winkler A., Schmidt H., Friend J.R., Yeo L.Y. Atomization off thin water films generated by high-frequency substrate wave vibrations. Phys. Rev. E. 2012;86 doi: 10.1103/PhysRevE.86.056312. [DOI] [PubMed] [Google Scholar]
- 36.Rezk A.R., Ahmed H., Brain T.L., Castro J.O., Tan M.K., Langley J., Cox N., Mondal J., Li W., Ashokkumar M. Free radical generation from high-frequency electromechanical dissociation of pure water. J. Phys. Chem. Lett. 2020;11:4655–4661. doi: 10.1021/acs.jpclett.0c01227. [DOI] [PubMed] [Google Scholar]
- 37.Rezk A.R., Tan J.K., Yeo L.Y. HYbriD resonant acoustics (HYDRA) Adv. Mater. 2016;28:1970–1975. doi: 10.1002/adma.201504861. [DOI] [PubMed] [Google Scholar]
- 38.Alhasan L., Qi A., Rezk A.R., Yeo L.Y., Chan P.P. Assessment of the potential of a high frequency acoustomicrofluidic nebulisation platform for inhaled stem cell therapy. Integr. Biol. 2016;8:12–20. doi: 10.1039/c5ib00206k. [DOI] [PubMed] [Google Scholar]
- 39.Alvarez M., Yeo L.Y., Friend J.R., Jamriska M. Rapid production of protein-loaded biodegradable microparticles using surface acoustic waves. Biomicrofluidics. 2009;3 doi: 10.1063/1.3055282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Qi A., Yeo L., Friend J., Ho J. The extraction of liquid, protein molecules and yeast cells from paper through surface acoustic wave atomization. Lab Chip. 2010;10:470–476. doi: 10.1039/b915833b. [DOI] [PubMed] [Google Scholar]
- 41.A.E. Rajapaksa, L.A.H. Do, D. Suryawijaya Ong, M. Sourial, D. Veysey, R. Beare, W. Hughes, W. Yang, R.J. Bischof, A. McDonnell, Pulmonary deposition of radionucleotide-labeled palivizumab: proof-of-concept study, Front. Pharmacol., (2020) 1291. [DOI] [PMC free article] [PubMed]
- 42.Wang Y., Rezk A.R., Khara J.S., Yeo L.Y., Ee P.L.R. Stability and efficacy of synthetic cationic antimicrobial peptides nebulized using high frequency acoustic waves. Biomicrofluidics. 2016;10 doi: 10.1063/1.4953548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Li H., Friend J.R., Yeo L.Y. Surface acoustic wave concentration of particle and bioparticle suspensions. Biomed. Microdevices. 2007;9:647–656. doi: 10.1007/s10544-007-9058-2. [DOI] [PubMed] [Google Scholar]
- 44.Tan M.K., Friend J.R., Yeo L.Y. Microparticle collection and concentration via a miniature surface acoustic wave device. Lab Chip. 2007;7:618–625. doi: 10.1039/b618044b. [DOI] [PubMed] [Google Scholar]
- 45.Heyder J.J.G.C.F.W., Gebhart J., Rudolf G., Schiller C.F., Stahlhofen W. Deposition of particles in the human respiratory tract in the size range 0.005–15 μm. J. Aerosol Sci. 1986;17:811–825. [Google Scholar]
- 46.Darquenne C. Deposition mechanisms. J. Aerosol Med. Pulm. Drug Deliv. 2020;33:181–185. doi: 10.1089/jamp.2020.29029.cd. [DOI] [PubMed] [Google Scholar]
- 47.Patton J.S., Byron P.R. Inhaling medicines: delivering drugs to the body through the lungs. Nat. Rev. Drug Discov. 2007;6:67–74. doi: 10.1038/nrd2153. [DOI] [PubMed] [Google Scholar]
- 48.Darquenne C. Aerosol deposition in health and disease. J. Aerosol Med. Pulm. Drug Deliv. 2012;25:140–147. doi: 10.1089/jamp.2011.0916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Sznitman J. Respiratory microflows in the pulmonary acinus. J. Biomech. 2013;46:284–298. doi: 10.1016/j.jbiomech.2012.10.028. [DOI] [PubMed] [Google Scholar]
- 50.Sznitman J. Revisiting airflow and aerosol transport phenomena in the deep lungs with microfluidics. Chem. Rev. 2021;122:7182–7204. doi: 10.1021/acs.chemrev.1c00621. [DOI] [PubMed] [Google Scholar]
- 51.Grasmeijer N., Frijlink H.W., Hinrichs W.L. An adaptable model for growth and/or shrinkage of droplets in the respiratory tract during inhalation of aqueous particles. J. Aerosol Sci. 2016;93:21–34. [Google Scholar]
- 52.Haddrell A.E., Lewis D., Church T., Vehring R., Murnane D., Reid J.P. Pulmonary aerosol delivery and the importance of growth dynamics. Ther. Deliv. 2017;8:1051–1061. doi: 10.4155/tde-2017-0093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Byron P.R. Prediction of drug residence times in regions of the human respiratory tract following aerosol inhalation. J. Pharm. Sci. 1986;75:433–438. doi: 10.1002/jps.2600750502. [DOI] [PubMed] [Google Scholar]
- 54.Liu Q., Guan J., Qin L., Zhang X., Mao S. Physicochemical properties affecting the fate of nanoparticles in pulmonary drug delivery. Drug Discov. Today. 2020;25:150–159. doi: 10.1016/j.drudis.2019.09.023. [DOI] [PubMed] [Google Scholar]
- 55.Osman G., Rodriguez J., Chan S.Y., Chisholm J., Duncan G., Kim N., Tatler A.L., Shakesheff K.M., Hanes J., Suk J.S. PEGylated enhanced cell penetrating peptide nanoparticles for lung gene therapy. J. Control. Release. 2018;285:35–45. doi: 10.1016/j.jconrel.2018.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Schneider C.S., Xu Q., Boylan N.J., Chisholm J., Tang B.C., Schuster B.S., Henning A., Ensign L.M., Lee E., Adstamongkonkul P. Nanoparticles that do not adhere to mucus provide uniform and long-lasting drug delivery to airways following inhalation. Sci. Adv. 2017;3:e1601556. doi: 10.1126/sciadv.1601556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Zierden H.C., Josyula A., Shapiro R.L., Hsueh H.T., Hanes J., Ensign L.M. Avoiding a sticky situation: bypassing the mucus barrier for improved local drug delivery. Trends Mol. Med. 2021;27:436–450. doi: 10.1016/j.molmed.2020.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Osman N., Kaneko K., Carini V., Saleem I. Carriers for the targeted delivery of aerosolized macromolecules for pulmonary pathologies. Expert Opin. Drug Deliv. 2018;15:821–834. doi: 10.1080/17425247.2018.1502267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Artzy-Schnirman A., Raviv S.A., Flikshtain O.D., Shklover J., Korin N., Gross A., Mizrahi B., Schroeder A., Sznitman J. Advanced human-relevant in vitro pulmonary platforms for respiratory therapeutics. Adv. Drug Deliv. Rev. 2021;176 doi: 10.1016/j.addr.2021.113901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Lokugamage M.P., Vanover D., Beyersdorf J., Hatit M.Z., Rotolo L., Echeverri E.S., Peck H.E., Ni H., Yoon J.K., Kim Y., Santangelo P.J. Optimization of lipid nanoparticles for the delivery of nebulized therapeutic mRNA to the lungs. Nat. Biomed. Eng. 2021;5:1059–1068. doi: 10.1038/s41551-021-00786-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Xue W., Dahlman J.E., Tammela T., Khan O.F., Sood S., Dave A., Cai W., Chirino L.M., Yang G.R., Bronson R., Crowley D.G. Small RNA combination therapy for lung cancer. Proc. Natl. Acad. Sci. 2014;111:E3553–E3561. doi: 10.1073/pnas.1412686111. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.