Video
EUS-directed transgastric ERCP in Roux-en-Y gastric bypass revision of sleeve gastrectomy.
Abbreviations: EDGE, EUS-directed transgastric ERCP; LAMS, lumen- apposing metal stent; RYGB, Roux-en-Y gastric bypass; SG, sleeve gastrectomy
Background
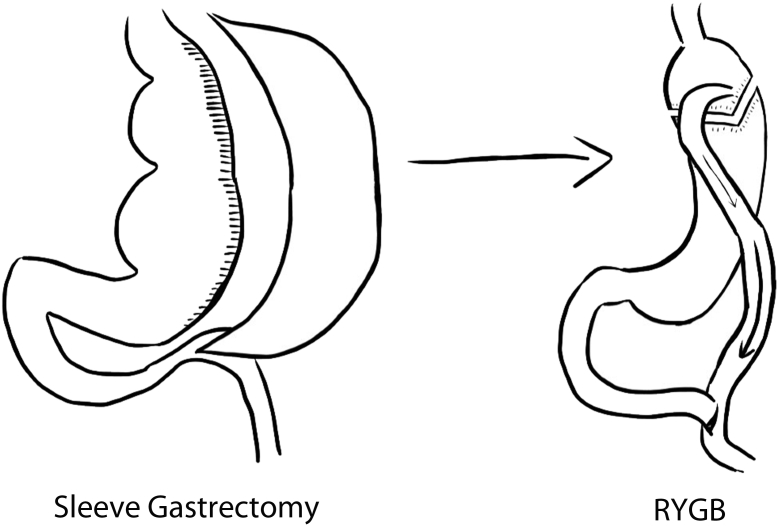
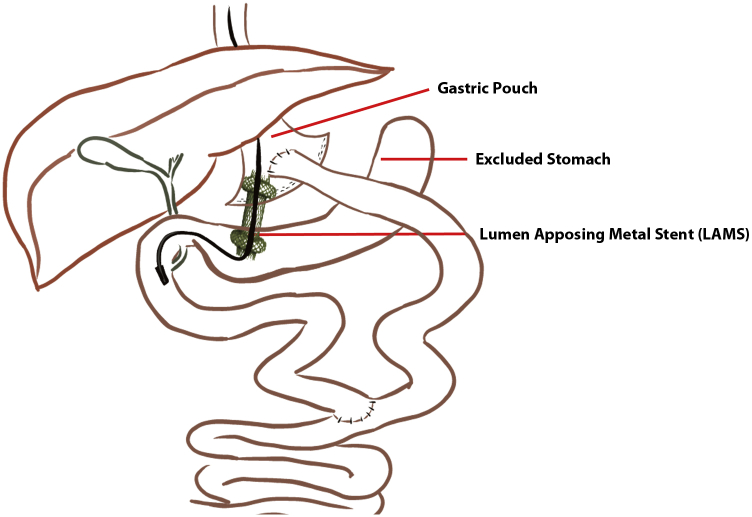
EUS-directed transgastric ERCP (EDGE) is an effective approach for the treatment of biliary adverse events of patients who have undergone Roux-en-Y gastric bypass (RYGB).1 Through deployment of a lumen-apposing metal stent (LAMS) from the gastric pouch into the excluded stomach, EDGE allows access to the bypassed stomach and duodenum in patients who have undergone RYGB (Fig. 1). However, patients who have undergone sleeve gastrectomy (SG) who undergo revision to RYGB have limited working space within both the gastric pouch and excluded stomach (Fig. 2), making therapeutic endoscopic procedures such as EDGE technically challenging.2,3
Figure 1.
EUS-directed transgastric ERCP in Roux-en-Y gastric bypass schematic diagram.
Figure 2.
Roux-en-Y gastric bypass revision of sleeve gastrectomy schematic diagram.
Case Presentation
A 54-year-old woman with a history of SG converted to RYGB was admitted to the hospital for evaluation of epigastric pain and jaundice. She had elevated liver function tests with intrahepatic and extrahepatic biliary ductal dilatation and multiple small stones within the gallbladder on MRCP. Because of concern for biliary tract disease, the patient was referred for an EDGE procedure.
Endoscopic Methods
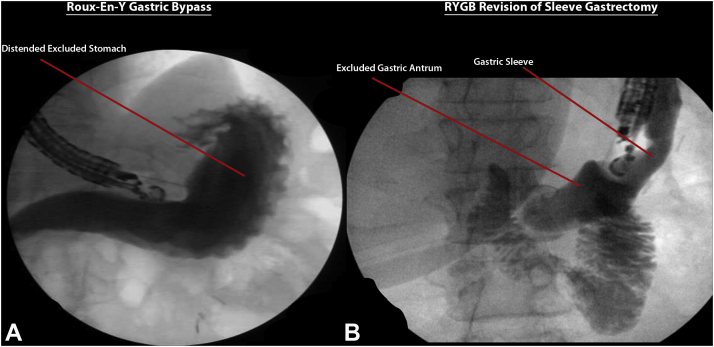
On EUS (Video 1, available online at www.giejournal.org), the excluded stomach appeared small because of earlier SG. A suitable location was identified with the EUS scope in the jejunum. From here, the excluded stomach was punctured with a 19-gauge needle, and 200 mL of a contrast/saline solution mixture was injected, opacifying the excluded stomach. Compared with patients who have undergone RYGB with no prior SG, whose excluded stomachs are often uniformly distended, this patient’s excluded stomach had suboptimal dilation on fluoroscopy, with the antrum being the most dilated part as expected (Fig. 3). A decision was thus made to target the antrum for deployment of the LAMS, even though performing an ERCP from this position can be technically challenging because of short and unstable scope position (Fig. 4). Under EUS and fluoroscopic guidance, a 20- × 10-mm LAMS was deployed from the jejunum into the antrum of the excluded stomach, creating a jejunogastrostomy. The LAMS was then dilated to 18 mm by using a dilating balloon. Then, 2 interrupted sutures were placed, securing the proximal phalange of the LAMS to the jejunal wall. A duodenoscope was then advanced through the LAMS into the second part of the duodenum for same-session ERCP. There was moderate biliary dilation, although biliary sphincterotomy followed by balloon sweeps yielded no stones. Occlusion cholangiogram confirmed no filling defects at the end of the procedure.
Figure 3.
Fluoroscopic opacification of the excluded stomach in (A) Roux-en-Y gastric bypass and (B) Roux-en-Y gastric bypass revision of sleeve gastrectomy.
Figure 4.
EUS-directed transgastric ERCP in Roux-en-Y gastric bypass revision of sleeve gastrectomy schematic diagram.
Patient Outcomes
The patient recovered well with no postprocedural adverse events. A cholecystectomy was performed, and the patient returned for LAMS removal after 14 weeks. Upper-GI series 4 weeks later showed a persistent fistula, and the patient underwent repeat EGD with fistula closure by argon plasma coagulation and a 10-mm over-the-scope clip. A repeat upper-GI series 8 weeks later confirmed closure of the fistula.
Conclusions
Although technically challenging, EDGE can be effectively and safely performed in patients with an RYGB revision of SG. Because of limited working space in the stomach and suboptimal dilation of the excluded gastric sleeve, LAMS deployment into the antrum may be necessary.
Disclosure
Dr Khashab is a consultant for Boston Scientific, Olympus America, Medtronic, GI Supply, Apollo Endosurgery, and Pentax, and receives royalties from Elsevier and UpToDate. All other authors disclosed no financial relationships.
Supplementary data
EUS-directed transgastric ERCP in Roux-en-Y gastric bypass revision of sleeve gastrectomy.
References
- 1.Runge T.M., Chiang A.L., Kowalski T.E., et al. Endoscopic ultrasound-directed transgastric ERCP (EDGE): a retrospective multicenter study. Endoscopy. 2021;53:611–618. doi: 10.1055/a-1254-3942. [DOI] [PubMed] [Google Scholar]
- 2.Yorke E., Sheppard C., Switzer N.J., et al. Revision of sleeve gastrectomy to Roux-en-Y gastric bypass: a Canadian experience. Am J Surg. 2017;213:970–974. doi: 10.1016/j.amjsurg.2017.04.003. [DOI] [PubMed] [Google Scholar]
- 3.Topart P. Comment on: Conversion of laparoscopic sleeve gastrectomy to Roux-en-Y gastric bypass: patterns predicting persistent symptoms after revision. Surg Obes Rel Dis. 2021;17:1688–1689. doi: 10.1016/j.soard.2021.06.008. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
EUS-directed transgastric ERCP in Roux-en-Y gastric bypass revision of sleeve gastrectomy.
EUS-directed transgastric ERCP in Roux-en-Y gastric bypass revision of sleeve gastrectomy.